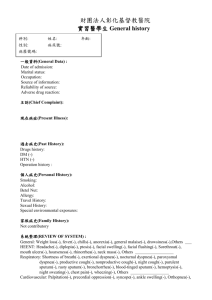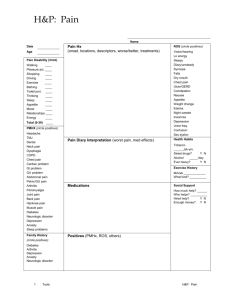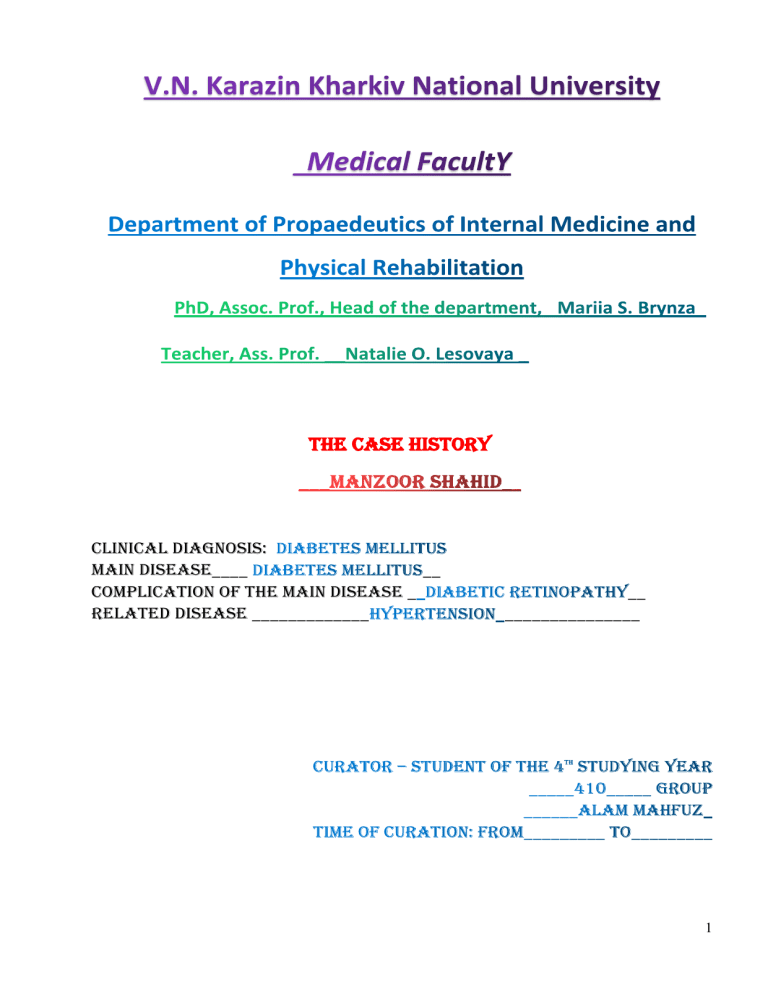
THE CASE HISTORY Clinical diagnosis: Main disease____ __ Complication of the main disease _ Related disease _____________ __ _______________ 1 2 Surname, name, patronic_____MANZOOR SHAHID_____________ Age___60________ Sex___MALE______ Family status____MARRIED________________ Education (primary, secondary, tertiary) Occupation_BUISNESSMAN___Post__OWNER_________________ Place of employment___BIHAR____________________ Permanent address______PATNA , BIHAR, INDIA___ Date of admission to the hospital__18/05/2022_ The patient complains of dizziness and headache for 3 days. The patient has a history of Hypertension for 6 months under medication (Amlodipine 5 mg OD). Diabetes under insulin therapy. Feeling of weakness, difficulty in walking for 3 days. The patient was a known case of Hypertension for 6 months. He had CVA ( Cerebral vascular accident) before 6 months, he got weakness of right limbs after CVA. No history of COPD. No history of any surgical illness. No history of drug and food allergies. 3 The patient is happily married , has 2 sons and a daughter. There is no history of Diabetes, HTN, Asthama Or TB in famiy. Is a middle class family. Smoking:- No Alcohol:- No Food habbit:- 3 times a day, Non-vegetarian. Bowel an bladder :- Regular and normal. Sleep :- 8 hours at night. Characteristics of the general status: overall health, weakness, fever, weight loss, presence of edema (localization, time of appearance, etc.). The review should be started from the system which desturbances predominated in the clinical manifestation of the disease. 1. 2. 3. 4. Pain (dolor) in pericardial zone: No pain on palpation. Palpatation : Non- tender. Shortness of breath (dyspnoe): NO. Edema (edema): NO 1. Breathing quality assessment:- NORMAL 2. Cough (tusis): NONE 3. Sputum (sputum): NONE. 4. Shortness of breath (dyspnoe) and suffocation (astma. asphyxia): NO. 5. Pain (dolor) in the chest: NO 6. Hemoptysis (haemoptoe) (blood spitting): NO. 7. Fever (febris):- NO. 4 8. 1. 2. 3. 4. 5. 6. 7. 8. Voice: normal. Pain: NO Appetite (orexis): Increased appetite .(Polyphagia ) Diarrheal effects: No . Dysphagia (dysphagia) -No. Abdominal bloating (metcorismus):- No Excrements (liming) (feces), Normal. Constipation (obstipatio):- NO. diarrhoea (diarrhoea):- No . 1. Pain: NO; 2. nature of urination: Frequent urination with daily volume of more than 3 litres, Polyurea, 3. colour of urine : straw-yellow, , urine turbid with trace of suger 4. the presence of blood in the sediment:- Nil 5. assessment of urine smell:- Fruity smell; 6. Edema:- No. 1. Headache: Mild headache 2. Dizziness: dizziness and difficulty in walking, uncoordinated gait 3. 4. 5. 6. 7. Loss of consciousness: No. Memory :-normal, The mood- Anxious, job satisfaction :- okay, retired . aggression :- sometimes aggressive usually due to poor relation with elder son. 1. The pain :- No 2. change of gait:- uncoordinated gait. 5 3. 4. 5. 6. stiffness in the joints, morning stiffness in movements, tremor of limbs, convulsions:- No. Muscle strength:- weak muscle power in right limb. Sensory:- Normal. Overall condition: Moderate. General appearence of the patient:- Anxious Consciousness: clear, . Facial expression: normal, Gait: slow, spastic, paretic, ataxic, fast, etc. Posture: direct. Body type: type asthenic), height:- 172 cm, weight:- 90 kg waist circumference:- 40 inch Skin: color - Hyperpigmentation(Shin spots)humidity (normal, dry, wet), humidity of palms, sweating general or local anesthesia (indicate the degree (mild, strong) and time of appearance), skin turgor (saved, increase, decrease). Visible mucous: Normal Skin appendages: normal hair growth. The hypodermic cellulose: presence of fat on waist and belly area. Edema: Absent. Head: normal shape , size and hair growth, without any injury. Eyes: Absence of any discharge or readness, but Vision is Blurry Nose: Normal shape an breathing without any discharge or disturbence of smell. Neck: normal shape with normal mobility . Lymph nodes: no enlaregement with normal mobility. The muscular system: Satisfactory muscle development, muscle weakness in right limb. Bone system: Normal 6 Joints: Normal 1 Examination of the chest. 1. Static inspection. The shape of the chest: normal ( asthenic), with symmetry. 2. Dynamic examination. Symmetric motion of both halves of the chest in breathing,:- normal. the number of respiratory movements per minute;:- 16 , type of breathing:-combined, Rhythm:-rhythmic , Shortness of breath: Absent, Palpation of the chest: No tenderness or mass found. Percussion of the chest: Resonant on all lung field Lung auscultation: normal vesicular breath sound on both sides Of The Sternum _________________________________ 7 ____________________________________________________________________ __ Left Midclavicular Line. ____________________________________________________________ – __120 Beats____Per 1 Min,. (Ir)Regular____ Filling___Normal____________, Strain____High_____________, Contour_____Visible_________, (Un)Equal On Both Arms. Arteries Palpation And Auscultation_____Pulse Is Prominent Bp On The Left Arm__140/90__________Mm Hg, On The Right Arm_140/90____________Mm Hg.. tive. Central Venous Pressure___6mm Of Hg_________ 8 Inspection:- No abdominal distention, symmetrical movement of abdomen with respiration, do dilated superficial veins, no scar marks. Palpation:- Non- tender Normal liver and spleen Percussion:- Dulness present. Ascultation:- Bowel sounds present(Normal) Lumbar area examination: No tenderness or mass found, Pasternatskiy symptom (on both sides):- Negative, palpation along the renal ducts (detection of points of pain):no pain; palpation and percussion of the suprapubic section (bladder) :- no tenterness or mass found, Gynecomasty:- no Scrotum, testicles:- normal without tenderness or any abnormal mass. the pateint is well oriented in time and space good , - have some family issues , finds difficult to control his emotions . had conflict with elder son, slightly hot temered, its persistence and pattern. thyroid gland, its swelling:- normal , without tenderness ; thyroid dysfunction symptoms :- none , 9 Stroke Cardiovacular embolism Diabetes Diabetic retinopathy Hematoogical:BSR- 210 mg/dl. Sodium- 139 mg/dl Potassium:- 4.6mmol/dl Creatinine:-1.0 mg/dl Blood urea:-30 mg/dlgm :- light yellow Acidic Nil trace Clear 0-2 /HPF - 0-2 /HPF :- 8.2 mmol/L 11.5 mmol/L 6.8 % For suspiscion of diabetic retinopathy following tests were performed Fluorescein angiography- some microvessels were seen to be blocked. 10 Optical coherence tomography (OCT) Based on all the gathered information , Diebetes mellitus has been diagnosed in this patient with the complication of diabetic retinopathy. Inj. Human insulin -3.o.7ou Amlodipine 5 mg OD continue 1. 2. 3. 4. 5. 6. . 1. Lifestyle modification:- exercise, healthy diet Diabetic diet Regular blood sugar level monitoring Regular eye check up Diffrent site of injection Foot care. - as this is a chronic condition, with diet modification and lifestyle changes combined with insulin therapy, the prognosis is good and person can lead a normal life with proper health monitoring); 11 2. usually 70 % of the population is not at fatal risk , only in severe untreated the person may die due to diabetic ketoacidosis and other cardiovascular diseases. 3. person can do daily works with some limitations if severe obesity is present. 12