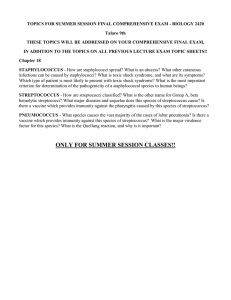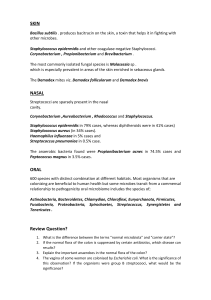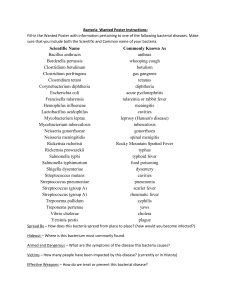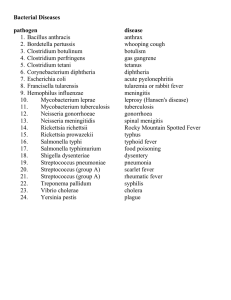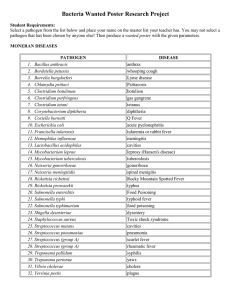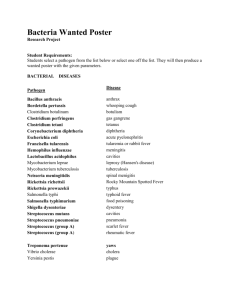
Gram positive and gram negative cocci Gram + Staphylococci, Streptococci and Enterococci Gram - Gonococci and Meningococci Jawetz-Medical microbiology Chapter 13,14,20 Domain: Phylum: Class: Order: Family: Genus: Bacteria Firmicutes Cocci Coccus Staphylococcaceae Staphylococcus The staphylococci are gram-positive spherical cells, Common inhabitant of the skin and mucous membranes, usually arranged in grapelike irregular clusters. They fermenting carbohydrates and producing pigments that vary from white to deep yellow. Staphylococci are nonmotile and do not form spores. The genus Staphylococcus has at least 40 species. The four most frequently encountered species of clinical importance are • • • • Staphylococcus aureus- S. aureus produces a carotenoid pigment called staphyloxanthin, which imparts a golden color to its colonies Staphylococcus epidermidis Staphylococcus lugdunensis Staphylococcus saprophyticus Staphylococci produce catalase, which converts hydrogen peroxide into water and oxygen. The catalase test differentiates the staphylococci, which are positive, from the streptococci, which are negative. Two species are commonly associated with staphylococcal diseases in humans • Staphylococcus aureus-The more virulent strain that can produce a variety of conditions depending on the site of infection • S. aureus is distinguished from the others primarily by coagulase production. Coagulase is an enzyme that causes plasma to clot by activating prothrombin to form thrombin • Staphylococcus epidermidis-Normal microbiota of human skin that can cause opportunistic infections in immunocompromised patients or when introduced into the body Pathogenicity of Staphylococcus infections result of produced enzymes and toxins. Virulence factors of Staphylococcus aureus Staphylococcus diseases • Furuncles (boils) are skin abscesses, which involve a hair follicle and surrounding tissue. • Carbuncles are clusters of furuncles connected subcutaneously, causing deeper suppuration and scarring. • folliculitis – superficial inflammation of hair follicle; usually resolved with no complications but can progress • impetigo – bubble-like swellings that can break and peel away; most common in newborns Toxin mediated disease • Staphylococcal food poisoning-is a gastrointestinal illness caused by eating foods contaminated with toxins produced by the bacterium. ✔ can contaminate food by people who carry it ✔ can also be found in unpasteurized milk and cheese products ✔ Because Staph is salt tolerant, it can grow in salty foods like ham Symptoms: • vomiting • nausea • stomach cramps • Diarrhea The illness cannot be passed to other people and typically lasts for only 1 day. Severe illness is rare. Staphylococcal Food Poisoning syndrome gastrointestinal illness caused by eating foods contaminated with toxins produced by Staph. Diagnosis based on • Clinical evaluation- group of cases and symptoms characteristic to GI infections • Laboratory evaluation-Toxin-producing Staph can be identified in stool or vomit The toxins can also be detected in foods. Toxic shock Syndrome (TSS)- was first described in children but came to public attention during the early 1980s, when hundreds of cases were reported in young women using intravaginal tampons. • • • • • high fever vomiting Diarrhea Sore throat muscle pain. Treatment • Aggressive Therapy -antibiotics • Blood Transfusions • Corticosteroids • Electrolyte replacements • Ventilator if lungs are damaged • Scalded Skin Syndrome (SSS) also known as Ritter von Ritterschein disease- results from the production of toxin exfoliatin , SSS characterized by red blistering skin that looks like a burn or scald The disease is most common in neonates and children less than 5 years of age. Symptoms: • Fussiness (irritability) • Tiredness • Fever • Redness of the skin • Fluid-filled blisters that break easily and leave an area of moist skin that soon becomes tender and painful • Large sheets of the top layer of skin may peel away Treatment may include: Intravenous antibiotic therapy Fluids to prevent dehydration Nasogastric feeding Use of skin creams or ointments and bandages Pain medicines Principles of Microbiology Diagnosis • • • • • Culture Test Catalase Test Coagulase Test- To detect Coagulase –positive Staphylococci as it is considered pathogenic for humans; Susceptibility Testing-Broth Serologic and Typing Test Treatment ⮚ Bacteremia, endocarditis, pneumonia, and other severe infections caused by S aureus require prolonged intravenous therapy with a β-lactamase-resistant penicillin. ⮚ Vancomycin is often reserved for use with nafcillin-resistant staphylococci. ⮚ Novobiocin: S. epidermidis is sensitive, whereas S. saprophyticus is resistant. ⮚ Because of the frequency of drug-resistant strains, meaningful staphylococcal isolates should be tested for antimicrobial susceptibility to help in the choice of systemic drugs. Domein: Bacteria Phylum: Firmicutes Class: Bacilli Order: Lactobacillales Family: Streptococcaceae Genus: Streptococcus Streptococci are Gram-positive, nonmotile, catalase-negative, facultatively anaerobic cocci that occur in chains or pairs. They are widely distributed in nature. Some are members of the normal human microbiota; others are associated with important human diseases. The genus Streptococcus includes three of the most important pathogens of humans. • S. pyogenes- β-hemolytic group A streptococci the cause of “strep throat,” which can lead to rheumatic fever and heart disease; • S. agalactiae, the most frequent cause of sepsis in newborns. • S. pneumoniae, a leading cause of pneumonia and meningitis in persons of all ages. Streptococcus diagnostic laboratory test Specimen • A throat swab • pus for culture identification • blood test • Serum for antibody determinations. Smears Culture Antigen Detection Tests Serologic Tests • Determination of ASO,anti-ASO titer • anti-DNase B and antihyaluronidase test • Antistreptokinase test • anti-M type-specific antibodies test Streptococcus pyogenes-Group A streptococci Erysipelas—It is an infection of the upper dermis and superficial lymphatics. symptoms typically include: Cellulitis—is an acute, rapidly spreading infection of the skin and subcutaneous tissues. Necrotizing fasciitis (streptococcal gangrene)- is very rare but serious infection, It can destroy skin, fat, and the tissue covering the muscles within a very short time. The disease sometimes is called flesh-eating bacteria. Scarlet Fever Scarlet fever or scarlatina – is a bacterial infection caused by group A Streptococcus. It is usually a mild illness, but people with scarlet fever need treatment to prevent rare but serious health problems. Common Symptoms of Scarlet Fever: • very red, sore throat • fever (101° F or above) • red rash with a sandpaper feel • Bright red skin in underarm, elbow • whitish coating on the tongue • “strawberry” (red and bumpy) tongue • Headache or body aches • Nausea, vomiting, or abdominal pain • Swollen glands Long-term Health Problems from Scarlet Fever • • • • • • • Rheumatic fever (an inflammatory disease that can affect the heart, joints, skin, and brain) Kidney disease (inflammation of the kidneys, called post-streptococcal glomerulonephritis) Otitis media (ear infections) Skin infections Abscesses (pockets of pus) of the throat Pneumonia (lung infection) Arthritis (joint inflammation) Diagnosis: Diagnosis is very easy, but sometimes milder forms can be confused with Rubella, Roseola, Kawasaki disease, drug eruption. • Swab test • Blood test • Blood test for bacterial identification Treatment: Group A strep is sensitive to penicillin. penicilin is drug of choice except in patient allergic to penicillin(narrow-spectrum cephalosporin). Treatment with oral antibiotic for 10 days is recommended Glomerulonephritis Post streptococcal Glomerulonephritis is an immune mediated disease is characterized by the sudden appearance of • Hematuria • proteinuria • red blood cell casts in the urine • Edema • hypertension with or without oliguria. Diagnosis Laboratory studies in acute poststreptococcal glomerulonephritis (APSGN) include tests to provide evidence of preceding streptococcal infection, renal function studies, and serologic studies. • Antibody titer in blood • Urine Analysis • Imagine studies (Chest radiographs may show findings of congestive heart failure.Renal ultrasound images usually reveal normal-sized kidneys bilaterally) • Histologic tests • Renal biopsy Treatment • Anti-infection treatment, antibiotic therapy • Immunosupresant Group B Streptococcus Growth on Granada/columbia sheep blood agar Growth characteristics Microaerophilic/ aerobic condition β-hemolysis Small grey or white colonies 2-4 mm in diameter Group B Streptococcus S. Agalactiae Group B Streptococcus GBS is cause of postpartum infection and as the most common cause of neonatal sepsis. Diagnosis: staining, culturing on selective medium, latex agglutination, biochemical test, molecular test (PCR) Treatment: mainly with beta-lactams, which includes penicillin and ampicillin. Streptococcus pneumonia Growth characteristics Facultative anaerobic α-hemolysis Small grey mucoidal colonies Streptococcus pneumonia Virulence factors Pneumococcal Disease Symptoms of pneumococcal disease depend on the part of the body that is infected. • • • • • • • • • • Fever Cough shortness of breath chest pain stiff neck confusion and disorientation sensitivity to light joint pain, chills, ear pain hearing loss brain damage, and death. Diagnosis • • Blood test Cerebrospinal fluid test Treatment • • • The pneumococcal vaccine can protect you from pneumococcal disease. Antibiotic therapy with broad spectrum antibiotic Levofloxacin is rapidly becoming a popular choice in pneumonia; this agent is a fluoroquinolone used to treat CAP caused by, S pneumoniae (including penicillinresistant strains) Symptoms: Nausea Vomiting Photophobia Altered mental status (confusion) Diagnosis: Identification of causative agent from blood or cerebrospinal fluid It is important to start treatment as soon as possible. The most effective way to protect against certain types of bacterial meningitis is VACTINATION. There are vaccines for three types of bacteria that can cause meningitis: Neisseria meningitidis Streptococcus pneumoniae Hib Streptococcus mutans Gram-positive coccus that is a major inhabitant of the oral cavity is considered a significant contributor of tooth decay and cavities. Facultative anaerobic α-hemolytic or nonhemolytic 0.5–1.0 mm in diameter colonies Streptococcus in oral cavity DIAGNOSIS •Lab diagnosis of Streptococcus mutans is based on the identification of the organism by its microscopic, cultural, and biochemical characteristics. Dental plaque and swabs from the cavities and taken as samples for laboratory identification. TREATMENT •Chlorhexidine, ofloxacin, doxycycline, tetracycline, chlortetracycline, erythromycin, vancomycin, clindamycin, methicillin, and gentamycin Enterococcus ⮚ Facultative anaerobic, catalase-negative Gram- positive cocci ⮚ Arranged individually, in pairs, or short chains. ⮚ Optimal temperature for growth 23-30 C ⮚ They are normal inhabitants of the intestinal tract, female genital tract, and (less commonly) oral cavity. ⮚ There are at least 47 species of enterococci, but associated with disease in humans are Enterococcus faecalis and Enterococcus faecium. Gram negative Cocci Neisseria Domain: Bacteria Phylum: Proteobacteria Class: Cocci “kidney bean” appearance Order: Coccus Family:Neiseriaceae Genus: Neiseria, Kingella, Eikenella, Simonsiella, and Alysiella NEISSERIA GONORRHEA Pathogenesis Gonococci exhibit several morphologic types of colonies but only piliated bacteria appear to be virulent. Gonococci are not normal inhabitants of the respiratory or genital flora. When introduced onto a mucosal surface adherence ligands such as pili and Opa proteins allow initial attachment of the bacteria to receptors on epithelial cells. Gonococci attack mucous membranes of the genitourinary tract, eye, rectum, and throat, producing acute suppuration that may lead to tissue invasion; Genital gonorrhea Signs & Symptoms • Painful or burning sensation when urinating; • Vaginal bleeding. • A burning sensation during urination • A white, yellow, or green discharge from the penis • Painful or swollen testicles Gonococcal ophthalmia neonatorum infection of the eye in newborns Infected during passage through an birth canal. The initial conjunctivitis rapidly progresses and, if untreated, result is blindness. To prevent Gonococcal ophthalmia neonatorum, instillation of tetracycline, erythromycin, or silver nitrate into the conjunctival sac of newborns is compulsory in the United States. Laboratory Diagnosis Specimens- Pus and secretions are taken from the urethra, cervix, rectum, conjunctiva, throat, or synovial fluid for culture and smear. Smear- Gram-stained smears of urethral or endocervical exudates reveal many diplococci within pus cells. These give a presumptive diagnosis. Culture- after collection, pus or mucus is streaked on enriched selective medium (modified Thayer-Martin medium [MTM]) and incubated in an atmosphere containing 5% CO2 at 37°C. Nucleic Acid Amplification Tests- detect gonococci in genital and urine specimens without culture. Important method for screening population. Treatment Because of the problems with antimicrobial resistance in N. gonorrhea CDC recommended: ceftriaxone (250 mg) intramuscularly as a single dose or 400 mg of oral cefixime as a single dose. Additional therapy with 1 g of azithromycin orally in a single dose or with 100 mg of doxycycline orally twice a day for 7 days. Patients who do not complete a course of treatment once they begin to feel better present a risk of continued transmission and selection of resistant strains NEISSERIA MENINGITIDIS Meningococci produce mediumsized smooth colonies on blood agar plates after overnight incubation. Thirteen serogroups have been defined on the basis of the antigenic specificity of their polysaccharide capsule. The most important diseaseproducing serogroups are A, B, C, W-135, and Y. Antigenic structure Pathogenesis Clinical Manifestation The meningococcus is spread horizontally (person to person) by respiratory droplets or direct contact. Acute Purulent MeningitisThe most common form of meningococcal infection Fulminant meningococcemia Common symptoms are: • sudden fever • Purplish rash • Headache • stiff neck • Nausea • Vomiting • increased sensitivity to light • confusion Laboratory diagnosis Specimens- blood and spinal fluid for smear and culture Smear - Gram-stained smears of the sediment of centrifuged spinal fluid or of petechial aspirate often show typical neisseriae within polymorphonuclear leukocytes or extracellularly. Culture - Culture media without sodium polyanethol sulfonate are helpful in culturing blood specimens. Cerebrospinal fluid specimens are plated on chocolate agar and incubated at 37°C in an atmosphere of 5% CO2. Treatment Penicillin G is the drug of choice for treating patients with meningococcal disease. Either chloramphenicol or a third generation cephalosporin such as cefotaxime or ceftriaxone is used in persons who are allergic to penicillins. Epidemiology, Prevention and Control Meningococcal meningitis occurs in epidemic waves -called “meningitis belt” military encampments Meningococcal Conjugate religious pilgrims Vaccine Quadravalent (MCV4) sub-Saharan Africa stimulates T-cell–dependent Recently, vaccine 4CMenB (Bexsero®) was licensed in the European Union. Three vaccines against serogroups A, C, Y, and W-135 and one that contains only C and Y available in the United States. responses. Use is recommended beginning at age 11 with boosters at 16 years. It is also recommended down to the age of 9 months for anyone at high risk for meningococcal disease