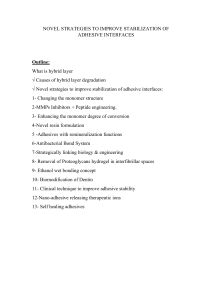
NOVEL STRATEGIES TO IMPROVE STABILIZATION OF ADHESIVE INTERFACES Outline: What is hybrid layer √ Causes of hybrid layer degradation √ Novel strategies to improve stabilization of adhesive interfaces: 1- Changing the monomer structure 2-MMPs Inhibitors + Peptide engineering. 3- Enhancing the monomer degree of conversion 4-Novel resin formulation 5 -Adhesives with remineralization functions 6-Antibacterial Bond System 7-Strategically linking biology & engineering 8- Removal of Proteoglycans hydrogel in interfibrillar spaces 9- Ethanol wet bonding concept 10- Biomodification of Dentin 11- Clinical technique to improve adhesive stability 12-Nano-adhesive releasing therapeutic ions 13- Self healing adhesives Adhesion of composite restorations occurs as a result of hybrid layer formation … What is hybrid layer? Hybrid means→ composed of different materials or phases. * It is a layer of dentin penetrated by a bonding agent forming resin tags. (Dentin collagen + bonding agent) Causes of hybrid layer degradation 1- Degradation of Adhesive-Dentin Interface 1.1.Proteolytic Enzymes *Matrix metalloproteinases especially MMP-8, and cysteine cathepsins attack type I collagen (the most abundant type of dentin collagen). *These enzymes are activated by: √ proteinases, chemical agents, low pH, heat treatment and mechanical stress . √ Acid-etchants and bacterial acids. √ Incomplete resin infiltration NB: Exposed dentin collagen express binding sites for MMPs and cathepsins. 1.2. Chemical/Biochemical Interactions pulpal pressure results in: pumping dentin fluid through dentinal tubules →hydrolysis of hydrophilic resins→ reducing sealing ability & bond durability. methacrylate adhesives contain ester bonds subjected to chemical and/or enzymatic hydrolysis. Human saliva contains cholesterol esterase →degrade dimethacrylates. 1.3. Mechanical Loading Masticatory forces can affect the bonding interface. Masticatory forces → tooth bending → gap formation → microleakage and recurrent caries. 2- Microleakage It occurs due to: 2.1 polymerization shrinkage: (Contraction stresses bond strength) → marginal gaps → microleakage → recurrent caries. 2.2 Bacterial enzymes: Ex: Collagenases →increase nano-leakage Lactic acid →activate MMPs 3. Hydrolysis of resin by water sorption Adhesives with hydrophilic monomers like HEMA (Hydroxy ethylmethacrylate: ✓ Enhances the wettability and impregnation of adhesives to dentin. ✓ Increase hybrid layer permeability →increase water sorption→ separations between hydrophilic and hydrophobic polymerized resins →bond degradation 4.Incomplete resin infiltration → leaves unprotected collagen and porosities in the hybrid layer. Results in : Incomplete water removal from interfibrillar spaces (between collagen fibers) →water accumulation → hydrolysis → decreased bond strength & increased nano leakage. Consequences of bonding failure: HYBRIDLAYER STABILIZATION (1) Changing monomer structure Aim : Change the monomer structure to increase the hydrophobicity → decrease water sorption. The hydrophobicity of the monomers can be increased by incorporating: ✓ Urethane group. ✓ Branched methacrylate linkage. ✓ Ethoxylated BisGMA. (2) MMPs inhibitors What are MMPs ? ✓ Proteolytic enzymes ✓ synthesized by odontoblasts and trapped within mineralized dentin matrix. ✓ calcium-and zinc dependent NB: Exposed dentin collagen express recognizable cleavage sites for MMPs. MMPs inhibitors: 1- chlorhexidine : Cationic-anionic reaction ✓ ✓ ✓ ✓ has a +ve charge. electrostatically binds to –ve charged catalytic sites of MMPs. blocks active sites. Chelates with zinc or calcium in catalytic domain. This leads to: 1-loss of catalytic activity of MMPs . 2-with better bond durability☺ 2- Alcohols: ⁎Alcohols can inhibit MMPs by forming a covalent bond between MMP’s catalytic zinc and alcohol’s oxygen atom. 3-Protein cross-linking: Cross-linker function: 1-produce conformational changes in MMPs 3D structure 2-hinder molecular mobility → interfere with enzyme activity. 3-Stabilize hybrid layer → improve bond strength. Ex: Glutaraldehyde, Hesperidin, Riboflavin, Grape seed extract & tannic acid. a) Glutaraldehyde *cross-linking by covalent bonds between amino groups of proteins and the aldehyde groups of glutaraldehyde. *5% glutaraldehyde for 1 min after acid etching →better bond stability. * Disadvantage: toxic at high concentrations b) Hesperidin (Extracted from citrus fruits) → increase mechanical properties of hybrid layer & immediate bond strength of self-etching adhesive c) Riboflavin *cross-linking agent in used with dental blue light *Better bond stability. *Biocompatible d) Grape seed extract *(GSE) is a natural cross-linker. *Inhibit MMPs activity and production. 4-Galardin: -Synthetic MMP inhibitor -Attack the active sites and chelate the zinc ion in MMP -Reduce nano-leakage 5-Peptide engineering : ✓ Strong inhibition of MMP-8 by small metal binding peptide (metal abstraction peptide MAP). ✓ MAP is a small peptide capable of robbing transition metal ions, ex: Zn from chelators. ✓ MAP is grafted into amine-containing polymers. ✓ MAP bind to zinc at the catalytic domain of MMP-8. (3) Enhancing the monomer degree of conversion Monomer degree of conversion can be improved by: 1-Water-soluble photo-initiators → resist cleavage by esterase. 2-Photo-initiators that are compatible with the hydrophobic and hydrophilic parts of adhesive. 3-Increasing the light-curing time. EX: sulfinates or sulfonates are added to SEA: Why? because CQ is adversely affected by presence of acidic monomers in Self-etch adhesives. How do they act? ✓ promote the photopolymerization of self-etch adhesive SEAs → improve the DC & μTBS. ✓ promote polymerization by scavenging oxygen (O2 is an inhibitor). (4)Novel resin formulation (BisGMA) is the most common crosslinking monomer in dental adhesives… ➔ Drawbacks: high susceptibility to hydrolysis → affect durability. Modified formulations: ✓ Silyl-functionalized BisGMA. ✓ Resin containing γ-methacryloxyproyl trimethoxysilane (MPS). 1- Silyl-functionalized BisGMA Ex: methoxysilyl-functionalized BisGMA. silyl-BisGMA provide: ✓ higher crosslinking compared to BisGMA/HEMA formulations. ✓ hydrolysis resistance during aqueous aging. Leading to…. ➢ Decreased degradation ➢ Decreased leached HEMA by 90% ➢ Retain mechanical properties 2- Resin containing γ-methacryloxyproyl trimethoxysilane (MPS) → Has intrinsic self-strengthening properties Basis: photoacid-induced sol-gel reaction + free radical photo-polymerization reaction of methacrylate ➢ ➢ ➢ ➢ Mechanism: light curing → free radical polymerization of methacrylate monomers (HEMA, BisGMA, and MPS). After that, photoacid-induced sol-gel reaction continues ″without light″ After 48 h, 65% of silyl groups undergo hydrolysis. After exposure to water or lactic acid→ the hydrolysis continues, and new crosslinked points are formed. *Also, the silanol groups react with the hydroxyl groups of HEMA or BisGMA forming covalent bonds (Si−O−C). Example for commercially available adhesive : Clearfil Porcelain Bond Activator → can be mixed with the adhesive (5) Adhesives with remineralization functions ✓ NB: Protease and cariogenic bacteria cause demineralization of dentin in hybrid layer. ➔ Remineralizing adhesives action mechanism: ✓ Promote microcracks healing and acids neutralization by raising the pH. ✓ Provide alkaline ions like Ca and P→ acids neutralization . ✓ Promote the epitaxial growth of the remaining HA crystals in partially demineralized dentin. Example for commercially available adhesive : fluoride-releasing adhesives (OptiBond Solo and Reactmer Bond) This can be achieved by addition of bioactive glass (BAG), calcium phosphate , and HA. ✓ Source of Ca and P ions. ✓ Allow deposition of calcium phosphate on crystals surfaces. ✓ Protect collagen fibrils → MMPs is fossilized by the crystal growth. • Bioactive glass ❖ ☺ anti-microbial activity→ increase the pH by release of alkaline ions: Na+ or K+ exchanged with H+ or H3O+ ions. ❖ ☺ Inhibit MMP due to alkaline ions → MMP act at pH 7. • calcium phosphate ❖ ☺ α tricalcium phosphate (-TCP) nanofiller improve bond strengths. ❖ ☺ amorphous calcium Phosphate nanoparticles (NACP) up to 40 wt% provide Ca and P ion without affecting bond strength. • Hydroxyapatite ❖ ☺ 7 wt% nano HA improve the immediate micro-tensile bond strength. (6)Antibacterial Bond System Bacteria→ secrete enzymes → demineralization → microleakage and recurrent caries 1- Silver nanoparticles (NAg): Ag ion role: a) inhibit bacterial enzymes . b) alter bacterial DNA leading to cell death. 2-Chitosan -Antibacterial agent that can be incorporated in dental adhesives -But: bond strength decreases as chitosan content increases . Ex: methacrylate-modified chitosan primer , possessed both hydrophilic and hydrophobic features, and can interact with the restorative material and tooth structure. → A higher value of bond strength was recorded at chitosan 0.2 % compared to 2.5 %. 3- Quaternary Ammonium Salts (QAS) : √ Positively charged → bind to negatively charged bacteria cell → alter membrane permeability → cytoplasmic leakage → bacterial death. 4- Chlorohexidine (CHX): √Antibacterial agent even at low concentration (0.05–0.2%). √ Inhibit bacterial proteolytic enzymes. √ Electrostatically binds to demineralized dentin. √ Can be added to the primer or bond. 5- Doxycycline (DOX): √ A tetracycline derivative √ Inhibit cariogenic bacteria such as S. mutans & Lactobacillus Ex: - Doxycycline (DOX)-encapsulated nanotubes incorporated into the dentin bonding agent Provide sustained release of DOX inhibit MMPs & cariogenic bacteria. ➔ Example for commercially available adhesive: - G-ænial Bond *Generally, Self-etch adhesives showed higher antibacterial activity than total etch adhesives. (7) Strategically linking biology & engineering ✓ ✓ ✓ ✓ 1- Proton Sponge Adhesives: Recurrent caries results from cariogenic plaque at restoration margins. Cariogenic plaque→ (pH < 5) →acid demineralization & enzymatic degradation of methacrylate ester groups in adhesives. degradation of methacrylate ester groups produces carboxylic acids, → the same functional group in lactic acid → induce caries. Cariogenic plaque at restoration margin can be reduced by neutralizing the acidic microenvironment. This can be done by : Incorporating a neutralizing agent→ act as a neutralizing proton sponge. Incorporating amine-containing monomers: Ex: 2-(dimethylamino) ethyl methacrylate (DMAEMA) → buffering effect . But …. Drawback → leaching of amine-containing cytotoxic species. So… the alternative strategy involves the use of biomolecules. 2-Modulating pH with biomolecules: ❖ Lysine- based dental adhesives. -Essential amino acid. - Act as a weak base. -Antibacterial properties →Buffer the micro-environment without leaching amine-containing cytotoxic species. ❖ arginine-based dental (8) Removal of Proteoglycans hydrogel in interfibrillar spaces ✓ Dentin → collagen + glycosaminoglycan / proteoglycan. ✓ GAGs /proteoglycans → bind to collagen → prevent adhesive infiltration into interfibrillar spaces → accumulation of water in HL. ✓ Moreover, GAGs (ex: Chondroitin sulfate) → highly polar and-ve charged → high tendency to attract water into interfibrillar spaces. ✓ Water → hydrolysis & degradation . Removal of proteoglycans by enzymatic treatment: Examples: ✓ Chondrotiniase ✓ Trypsin → It was found that, removal of PGs (chondrotin sulphate) leads to: √ Change surface energy √ help in water displacement √ improved resin infiltration √ improve TBS √ reduce nano-leakage (9) Ethanol wet bonding Severe drying leads to collagen collapse → So, we need moist dentin for bonding. Problems of water wet bonding ??? *Water tree formation … Acts as a semi-permeable membrane → osmotic effect and fluid movement → trapped moisture → ↓ composite curing → hydrolysis and degradation at interface. This can be overcome by: Ethanol wet bonding Ethanol wet bonding ✓ This technique replaced water wet technique. ✓ It is used to dehydrate the exposed collagen without collapsing. ✓ The water in DT is replaced by ethanol. In addition, ✓ Ethanol dissolves hydrophobic resin such as TEGDMA (Tri Ethyl Glycidyl Di Methacrylate) making them more hydrophilic. ✓ When HEMA is used as a primer; HEMA/alcohol, it shows better infiltration compared to HEMA/water. Advantages: 1-Better dentin wettability. 2-Better bond penetration and sealing with DT. 3-Better bond durability. Disadvantages: 1-Technique sensitive 2-Additional steps & more time Ayar et.al 2014 found that, Ethanol-wet-bonding increase the Microtensile bond strength from 17.4 MPa to 28.7 Mpa compared to Water wet bonding. (10) Biomodification of Dentin Dentin biomodification improves mechanical properties through nonenzymatic collagen cross-linking. (1) Physical Agents. Using photo-oxidative techniques. By the action of (UV) light → requires the presence of oxygen free radical (reactive & unstable). Ex: Vitamin B2 (riboflavin) ✓ Source of oxygen free radicals, ✓ Activated by UV light → induce covalent bonds formation between the amino group of glycine of collagen and the carbonyl groups of hydroxyproline of side chains (cross-linking) (2) Nonspecific Synthetic Cross-Linking Agents : Cross-linking agents: √ Stabilizes the structure. √ Make it more resistant to enzymatic degradation. Ex: 1) Glutaraldehyde 5% 2) Carbodiimide (EDC) 0.1; 0.3, 0.5 M: Less cytotoxic→ activation → reacts with the amino groups in collagen→ cross linking ⁎Limitation: release of urea → delay cross-linking (1h) → limit the clinical use. 3) Biomimetic Remineralization: The use of amorphous calcium phosphate nanoprecursors for biomineralization of dentin. (4) Cross-Linking Agents of Natural Origin. Antioxidant materials √ Promote cross-linking with collagen √ Inhibit MMPs. Ex: Grape seeds derivative (oligomeric proanthocyanidin). limitations: 1-Long application times (10 min to 1h) not clinically applicable. 2-Reduced degree of conversion (inhibiting polymerization). 3- Brown pigmentation in dentin. (11) Clinical technique to minimize nano-leakage & improve adhesive stability 1-Prolonged Curing Time -extending curing time beyond 20 seconds results in: √improve polymerization √improve degree of conversion √reducing the permeability 2- scrubbing action Scrubbing action of self-etch adhesives results in: improve smear layer removal→ improve resin infiltration → improve enamel and dentinal bonding →less nano leakage 3- Multiple layer adhesive application Hashimoto et al. (2006) found that: ➢ Bond strength can be improved by applying three -coats of adhesive. ➢ Increasing the number of coats → minimize nano-leakage. NB: Application of several coats without curing→ better resin impregnation →minimize adhesive thickness 4-High-pressure air blowing ➢ Enhance solvent evaporation & resin penetration. ➢ More extended resin tags →Improve Bond strength. (12) nano-adhesive releasing therapeutic ions - Application of adhesives or pre-treatments doped with antiMMPs → reduce proteolytic enzymes & hydrolysis. Ex: nano bioactive glasses (BGn) doped with specific functional and therapeutic ions, such as Ag, F, Fe,Ca, and Cu. 1- Incorporation of bioactive glass doped with fluoride within adhesives results in: ✓ Better remineralization. ✓ Better MMP inhibition. ➔ compared to bioglass 2- Incorporation of bioactive glass doped with copper CuBGn (2%) within adhesives results in: ✓ Induce remineralization. Inhibit MMP without affecting the bond strength. (13) Self healing adhesives ✓ Act by closing micro- or nanocracks. ✓ nanocapsules/ microcapsules filled with healing agent→ Crack → rupture of nanocapsules/ microcapsules → release of their content → contacts the catalyst in the matrix → polymerization → healing . Example: Poly(urea-formaldehyde) (PUF) microcapsules containing TEGDMA and N,N-dihydroxyethyl-p-toluidine (DHEPT) These capsules are incorporated into a matrix containing nanoparticles of amorphous calcium phosphate NACP to obtain crack-healing, antibacterial, and remineralization Thank you