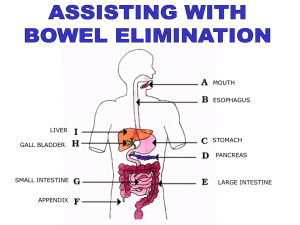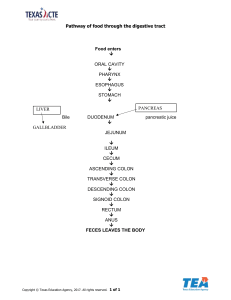
ENEMA ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ o Very sluggish and thought to move the chyme very little. ❖ Mass Peristalsis o Wave of powerful muscular contraction that moves over large areas of colon. o Occurs after eating stimulated by the presence of food in the stomach and small intestine. Course Outline DEFECATION PHYSIOLOGY DEFECATION/ BOWEL MOVEMENT FACTORS THAT AFFECT DEFECATION FECAL ELIMINATION PROBLEMS FACTORS THAT CONTRIBUTE CONSTIPATION NURSING DIAGNOSIS FOR FECAL ELIMINATION PROBLEMS MEDICATIONS ADMINISTERING ENEMA CLEANSING ENEMA COMMON ENEMA SOLUTION CLASSIFICATION OF ENEMA Rectum & Anal Canal - DEFECATION [BOWEL MOVEMENT] PHYSIOLOGY ➢ ➢ - - Elimination of waste is very essential. Excreted waste = feces/stool Large Intestine Extends from ileocecal valve to the anus Colon: 125 to 150cm long [50 to 60 inches] Cecum, transverse, descending colon, sigmoid colon, rectum and anus Haustra: pouches of large intestine due to short longitudinal muscles Absorption of water and nutrients, mucoid protection of the intestinal wall and fecal elimination Contents: food ingested over previous 4 days Lumen > flatus/feces Chyme: stomach > small intestine > ileocecal valve Ileocecal: prevents backflow of chyme and regulates the flow of chyme. Colon: serves as protective function in that its secreted mucus. It also acts to transport along its lumen the products of digestion. Mucus: serves to protect the wall of the large intestine from trauma by the acids formed in the feces, and it serves as an adherent for holding the fecal material together. Mucus also protects the intestinal wall from bacterial activity. TYPES OF MOVEMENT IN LARGE INTESTINE ❖ Haustral churning o Movement of chyme back and forth within the haustra. o Mixing the contents, aids the absorption of water & moves to the next haustra. ❖ Colon peristalsis o Wavelike movement produced by longitudinal muscle fibers. o Propels intestinal contents forward. R: 10 to 15cm [4 to 6 inches] A: 2.5 to 5cm [1 to 2 inches] Anal canal: external and internal sphincter Hemorrhoids occur when veins are distended due to the repeated pressure. Each vertical folds of rectum have a vein and an artery and these folds keeps retaining the feces within the rectum. DEFECATION/ BOWEL MOVEMENT ▪ ▪ ▪ ▪ ▪ ▪ ▪ Expulsion of feces from the anus. When peristaltic waves move the feces into the sigmoid colon and the rectum, the sensory nerves in the rectum are stimulated and the individual becomes aware of the need to defecate. It is facilitated by thigh flexion, that increases pressure within the abdomen and sitting position, that increases the downward pressure on the rectum. Normal feces 75% water 25% solid Brown due to presence of stercobilin and urobilin which derived from bilirubin Odor: action of bacteria (Escherichia coli or staphylococci) Microorganisms + chyme = odor Flatus: largely air and the by-products of digestion of CHO An adult usually forms 7 to 10L of flatus in the large intestine q24h. FACTORS THAT AFFECT DEFECATION (1) DEVELOPMENT ▪ Newborn & Infants Meconium: black tarry, odorless, and sticky Transitional stool: greenish yellow Breast-fed: light yellow to golden feces. Formula: dark yellow or tan stool. - ▪ ▪ ▪ Intestine is immature, water is not well absorbed and stool is soft, liquid, and frequent. Toddlers Desire to control during daytime bowel movements Toilet training Childs starts to become aware, feeling of discomfort by soiled diaper and sensation that need to go to toilet. School-Age & Adolescent SA: may delay defecation during d/t playing Similar bowel movement to adults Older Adults 50% suffer from constipation Due to less activity, low fiber and fluid intake, and muscle weakness MUST: adequate roughage in diet, adequate exercise, and 6 to 8 glasses of fluid daily. Gastrocolic reflex [increase peristalsis to the colon] (2) DIET ▪ Inadequate fiber intake increases the risk for having obesity, diabetes mellitus type 2, coronary artery disease and colon cancer. ▪ Diarrhea and flatus: spicy and high sugar ▪ Works with plenty of water ▪ Bland and low fiber diets are lack in bulk and it moves more slowly so it needs to increase fluid intake to increase their rate of movement. ▪ Insoluble Fiber Promotes movement Increase stool bulk Whole-wheat flour, wheat bran, nuts, many vegetables ▪ Soluble Fiber Dissolves in water = gel like Decrease blood cholesterol Decrease glucose level Oats, peas, beans, apples, citrus fruits, carrots, barley and psyllium (3) FLUID INTAKE & OUTPUT ▪ 2000 to 3000 mL/day ▪ The body continues to reabsorb fluid from the chyme as it passes along the colon. ▪ Reduced fluid intake slows the chyme’s passage along the intestines, further increasing the reabsorption of fluid from the chyme. ▪ Abnormal quick movement of chyme in the large intestine makes the feces soft or even watery due to less time of fluid absorption. (4) ACTIVITY ▪ Stimulates peristalsis (Movement of chyme to colon) ▪ Weak muscles can result from lack of exercise, immobility, or impaired neurologic functioning. ▪ Bed ridden: risk for constipation/ constipated (5) PSYCHOLOGICAL ▪ Angry/Anxious Increase peristaltic activity Subsequent nausea and vomiting ▪ Depressed Slow intestinal motility Constipation (6) DEFECATION HABITS ▪ Establish habit of defecating at a regular time. ▪ Ignores defecating can result to constipation. (7) MEDICATIONS ▪ Large doses of tranquillizers, repeated administration of morphine and codeine decrease the GI motility and can make the patient constipated. ▪ Iron tablets have an astringent effect that act more locally on the bowel mucosa to cause constipation. ▪ Laxatives stimulate bowel activity and assist fetal elimination. ▪ Iron salts can make the stool black as well as PeptoBismol, a common OTC drug. ▪ Antibiotics may cause gray-green discoloration ▪ Antacids can cause whitish discoloration or specs in the stool. (8) DIAGNOSTIC PROCEDURE ▪ Sigmoidoscopy/ colonoscopy: the patient is restricted from ingesting food or fluid. ▪ The patient will be given cleansing enema prior to the procedure. (9) ANESTHESIA & SURGERY ▪ General Anesthetics Cause normal colonic movements to cease or to slow by blocking the parasympathetic stimulation. ▪ Ileus [cessation of intestinal movement] that lasts 24-48 hours ▪ Listening for bowel sounds that reflect intestinal motility is important nursing assessment following surgery. (10) PATHOLOGIC CONDITIONS ▪ Spinal cord and head injuries can decrease sensory stimulation of defecation ▪ (11) Impaired mobility can limit pt to respond to urge and experience constipation. PAIN ▪ Pt who experienced pain during defecating often suppress the urge to defecate ▪ Resulting into constipation ▪ Narcotic analgesic can make the client constipation FECAL ELIMINATION PROBLEMS CONSTIPATION ▪ ▪ ▪ Less than 3 bowel movements. Bowel movement to the large intestine is slow + the reabsorption of water. Fecal Impaction Mass collection of hardened feces in folds of rectum. Oil retention enema is given if fetal impaction is suspected. Causes: poor defecation habits and constipation resulting into prolonged retention and accumulation of fetal material, administration of anticholinergics & antihistamine, and barium used in radiologic examination of GI tract. DIARRHEA ▪ ▪ ▪ ▪ ▪ Liquid feces Increase frequency if defecation Spasmodic cramps Increase bowel sounds Fatigue, weakness, malaise and emaciation BOWEL INCONTINENCE ▪ ▪ Loss of voluntary control of fecal and gaseous discharge Impaired anal sphincter or nerve supply FACTORS THAT CONTRIBUTE CONSTIPATION (1) Insufficient Fiber Intake (2) Insufficient fluid intake (3) Immobility (4) Irregular defecation Habits (5) Change in Daily Routine (6) Lack of Privacy (7) Chronic use of laxative or enema (8) IBS (9) Pelvic floor dysfunction/ muscle damage (10) Poor motility (11) Neurologic Conditions (12) Emotional Disturbances (13) Medications (14) Habitual ignoring the urge NURSING DIAGNOSIS FOR FECAL ELIMINATION PROBLEMS ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ ❖ Bowel incontinence Constipation Risk for constipation Perceived constipation Diarrhea Dysfunctional G.I. motility Risk for deficient fluid volume or Risk for Electrolyte Imbalance Risk for Impaired Skin Integrity Situational Low Self Esteem Disturbed body image Deficient knowledge Anxiety MEDICATIONS CATHARTICS ▪ ▪ Drugs that induce defecation They can have strong, purgative effect LAXATIVE FLATULENCE ▪ ▪ ▪ Intestinal distention Excessive flatus that leads to stretching and inflation of infection. Three primary sources of flatus: (1) Action of bacteria on the chyme (2) Swallowed air (3) Gas diffuses between bloodstream and intestine ▪ ▪ ▪ ▪ ▪ Produces soft or liquid stools Sometimes accompanied by abdominal cramps Contraindicated in the client who has nausea, cramps, colic, vomiting, or undiagnosed abdominal pain. Continual use of laxatives to encourage bowel evacuation weakens the bowel’s natural responses to fecal distention, resulting in chronic constipation. Teach the client about dietary fiber, regular exercise, taking sufficient fluids, and establishing regular defecation habits. ANTIDIARRHEALS ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Slow the motility of the intestine Absorb excess fluid in the intestine Using a medication such as an opiate when the cause is an infection, toxin, or poison may prolong diarrhea. Longer use of OTC antidiarrheals can produce dependence. Some drugs can cause drowsiness and should not me used when driving or running machinery. Kaolin-pectin preparations may absorb nutrients. Bulk laxatives 7 other absorbents may use to help bind toxins & absorb excess bowel liquid. Pepto-Bismol used to treat “traveler’s diarrhea” it may contain aspirin so it’s should not be given to children or teens with chicken pox, influenza, and other viral infection. ANTIFLATULENCE ▪ ▪ ▪ Do not decrease flatus formation but they coalesce the gas bubbles. Facilitate their passage by belching through mouth or anus. Combination of simethicone & loperamide [Imodium Advance] is effective in abdominal bloating & gas associated with acute diarrhea. ADMINISTERING ENEMA COMMON ENEMA SOLUTIONS HYPERTONIC Draws water in the colon HYPOTONIC Distends colon, stimulates peristalsis, softens feces ISOTONIC Distends colon, stimulates peristalsis, softens feces. SOAP SUDS OIL Irritates mucosa, distends colon Lubricates the feces and the colonic mucosa. CLASSIFICATION OF ENEMA ▪ CLEANSING ▪ ▪ CARMINATIVE ▪ ▪ To expel flatus Adult: 60 to 80mL RETENTION ▪ ▪ Oil or medication Retained for 1 to 3 hours ▪ ▪ ▪ Harris flush Expel flush 100 to 200mL fluid into & out rectum & sigmoid colon Repeated 5 to 6 times ENEMA – solution introduced to the rectum and large intestine Action: distend the intestine and irritate the intestinal mucosa that increase peristalsis = excretion of feces and flatus. Prevent escape of feces during pregnancy Prepare intestine for certain diagnostic tests Remove feces in instances of constipation or impaction. Temperature: 37.7 degrees Celsius or 100 degrees Fahrenheit ▪ The force of solution is controlled by: o Height of solution container o Size of tubing o Viscosity of fluid o Rectum resistance (a) HIGH ENEMA – give cleanse as much of the colon as possible. (b) LOW ENEMA – rectum and sigmoid colon only left lateral position. CLEANSING ENEMA ▪ ▪ ▪ ▪ Intended to remove feces. Prevent escape of feces during surgery. Preparation for diagnostic tests. Remove feces in occurrence of constipation or impaction. RETURN-FLOW ENEMAS ▪