Histology - introduction
advertisement
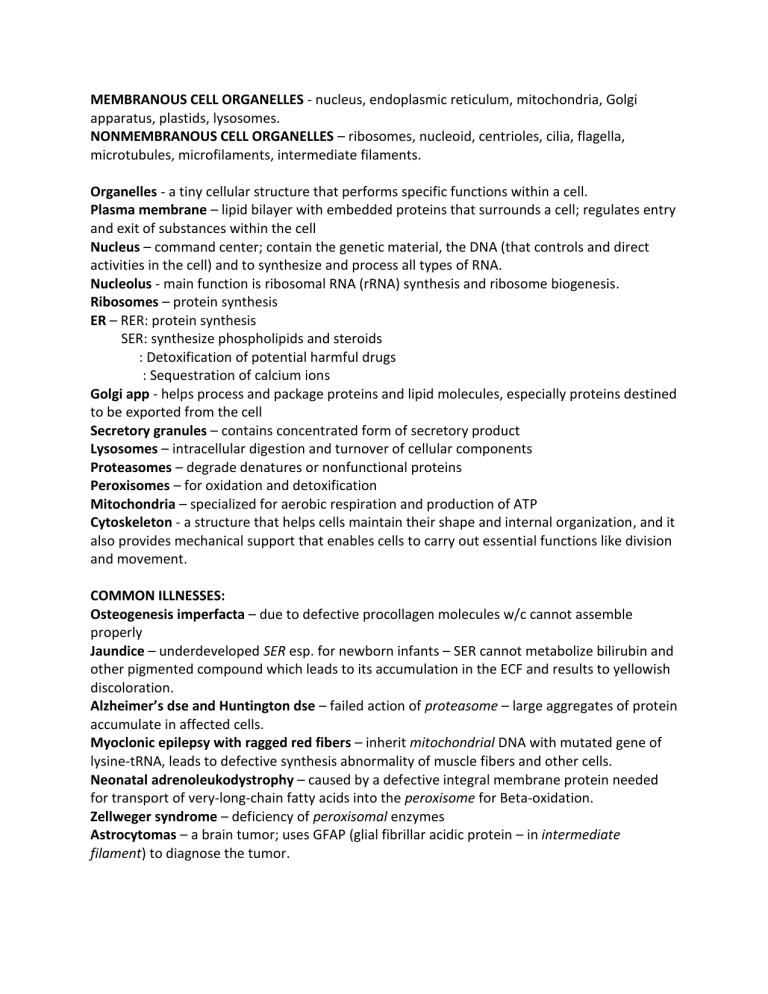
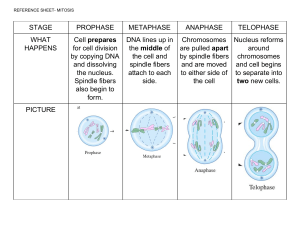
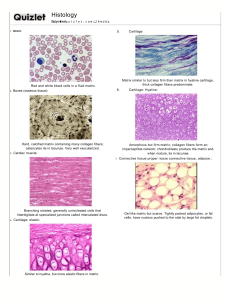
MEMBRANOUS CELL ORGANELLES - nucleus, endoplasmic reticulum, mitochondria, Golgi apparatus, plastids, lysosomes. NONMEMBRANOUS CELL ORGANELLES – ribosomes, nucleoid, centrioles, cilia, flagella, microtubules, microfilaments, intermediate filaments. Organelles - a tiny cellular structure that performs specific functions within a cell. Plasma membrane – lipid bilayer with embedded proteins that surrounds a cell; regulates entry and exit of substances within the cell Nucleus – command center; contain the genetic material, the DNA (that controls and direct activities in the cell) and to synthesize and process all types of RNA. Nucleolus - main function is ribosomal RNA (rRNA) synthesis and ribosome biogenesis. Ribosomes – protein synthesis ER – RER: protein synthesis SER: synthesize phospholipids and steroids : Detoxification of potential harmful drugs : Sequestration of calcium ions Golgi app - helps process and package proteins and lipid molecules, especially proteins destined to be exported from the cell Secretory granules – contains concentrated form of secretory product Lysosomes – intracellular digestion and turnover of cellular components Proteasomes – degrade denatures or nonfunctional proteins Peroxisomes – for oxidation and detoxification Mitochondria – specialized for aerobic respiration and production of ATP Cytoskeleton - a structure that helps cells maintain their shape and internal organization, and it also provides mechanical support that enables cells to carry out essential functions like division and movement. COMMON ILLNESSES: Osteogenesis imperfacta – due to defective procollagen molecules w/c cannot assemble properly Jaundice – underdeveloped SER esp. for newborn infants – SER cannot metabolize bilirubin and other pigmented compound which leads to its accumulation in the ECF and results to yellowish discoloration. Alzheimer’s dse and Huntington dse – failed action of proteasome – large aggregates of protein accumulate in affected cells. Myoclonic epilepsy with ragged red fibers – inherit mitochondrial DNA with mutated gene of lysine-tRNA, leads to defective synthesis abnormality of muscle fibers and other cells. Neonatal adrenoleukodystrophy – caused by a defective integral membrane protein needed for transport of very-long-chain fatty acids into the peroxisome for Beta-oxidation. Zellweger syndrome – deficiency of peroxisomal enzymes Astrocytomas – a brain tumor; uses GFAP (glial fibrillar acidic protein – in intermediate filament) to diagnose the tumor. Mitosis G1 – cell growth S phase – DNA replication G2 – cell development M Phase - cell division begins (Karyogenesis) Interphase (S-phase) – cell prepares to develop Prophase – chromosome condensed, nuclear envelop disassembled and spindle fiber emerge from centrosome, centrosome move toward opposite poles Metaphase – sister chromatids aligned at metaphase plate, each sister chromatid are attached to the spindle fiber originating form opposite poles Anaphase – sister chromatids are pulled toward opposite poles, certain spindle fiber elongates the cell Telophase – spindle fiber breaks down, chromosome de-condense, nuclear envelop reforms around the chromosome, cytoplasm starts to divide Cytokinesis – division of 2 daughter cells (diploid) Meiosis Interphase (S-phase) – Chromosomes are duplicated Prophase 1 – chromosome condensed, chromosome pair up and exchange bits of DNA called recombination or crossing over Metaphase 1 – paired chromosome are lined in the metaphase plate, centrioles are at the opposite side of the poles with spindle fibers extending from it Anaphase 1 – chromosomes are pulled apart (sister chromatids are still attached to centromere), by spindle fiber, toward the opposite side of the poles Telophase 1 – sister chromatids arrive at the pole and begin to condense, nuclear envelope forms around its nucleus and cytoplasm is divided by cleavage furrow Cytokinesis 1 - divides 2 daughter cells (diploid) Prophase 2 – sister chromatids condensed, nuclear envelop disassembles, spindle fiber begins to form Metaphase 2 – sister chromatids aligns at the metaphase plate, centrioles are at the opposite side of the poles with spindle fiber extending from it Anaphase 2 – sister chromatid are pulled to the opposite side of the poles due to the action of spindle fibers Telophase 2 – each pole gathers full set of chromosome, create 2 new nuclei Cytokinesis – divides 4 daughter cells (haploid) Connective tissue is comprised of cells, formed fibers, and amorphous extracellular matrix (ground substance). Both the fibers and ground substance are secreted by the connective tissue cells that are interspersed and embedded in the matrix. Functions of the connective tissue include support and binding together of the other tissues; providing a medium for the passage of metabolites; serving as a storage site for lipids, water and electrolytes; aiding in protection against infection by an inflammatory reaction mediated by cells that have migrated into the connective tissue from the blood; and repair by the formation of scar tissue. Connective tissues are derived from the embryonic connective tissue or mesenchyme which is derived primarily from the mesodermal germ layer of the developing embryo. 1. What is a hypertrophic scar? A hypertrophic scar is a thick raised scar that's an abnormal response to wound healing. They more commonly occur in taut skin areas following skin trauma, burns or surgical incisions. There are increased numbers of myofibroblasts in hypertrophic scars. Transforming growth factor-beta (TGF-beta) stimulates differentiation of both local and bone fibroblasts into myofibroblasts, which then creates tension on the wound. It is hypothesized that existing tension on a wound may exacerbate this pathway, creating a vicious cycle. Deep wounds stimulate dermal fibroblasts to produce collagen and inflammatory mediators like transforming growth factor-beta 1 (TGF-beta1). TGF-beta1 further stimulates fibroblasts to deposit elastin and collagen, potentially leading to increased deposition in wounds predisposed to hypertrophic scarring. Hypertrophic scars show the deposition of collagen type III fibers that are arranged parallel to the epidermis. 2. What type of tissue predominates the scar? Collagen Tissue 3. What is a connective tissue? It is the tissue that provides supports and physically connects other tissues and cells together to form the organs of the body. 4. What are the different connective tissues and to which part of the body are they abundantly deposited? a. Loose (Areolar) – a layer beneath the epithelial lining of many organs and fillinf the spaces between fibers of muscle and nerve. Common areas are: lamina propria beneath epithelial lining od digestive tract; blood vessels b. Dense Regular – mostly type 1 collagen bundles and fibroblasts aligned in parallel for great resistance to prolonged or repeated stresses from the same direction. Areas are: ligaments, tendons, aponeurosis and corneal stroma c. Dense irregular – bundles of collagen fibers appear randomly interwoven, with no definite orientation. Areas are: dermis of sin, organ capsules, submucosa layer of digestive tract d. Reticular – abundant fibers of type 3 collagen forming a delicate network that supports various type of cells. Areas are: bone marrow, liver, pancreas, adrenal glands, all lymphoid organs except thymus e. Mucoid – or Wharton’s jelly, a principal component of fetal umbilical cord; abundant ground substance composed chiefly of hyaluronan, mucoid tissue is gelatinous, with sparse collagen fibers and scattered fibroblasts. 5. What is the difference between a hypertrophic scar and a keloid? Hypertrophic and keloid scars are two types of raised, abnormal scars. The distinction between hypertrophic scars and keloid scars can be seen histologically. Both hypertrophic scars and keloids show thick bundles of collagen on histopathology. Hypertrophic scars show the deposition of collagen type III fibers that are arranged parallel to the epidermis. Keloid scars show haphazard sheets of type-1 and type-2 collagen with random directional orientation. This is sometimes termed “keloid collagen,” and tends to be much more histologically disorganized. There also tend to be more blood vessels and neocapillary ingrowth histologically in keloid scars than in hypertrophic scars. (https://www.ncbi.nlm.nih.gov/books/NBK470176/) Respiratory System Case #1 1. What is a pulmonologist and what is the pulmonary system? A pulmonologist is a physician who specializes in the respiratory system. The pulmonary system consists of upper and lower pulmonary structures, bronchial/systemic circulation, and gas exchange at the level of the lungs and tissue cells. 2. What is the main function of the Pulmonary system? These anatomical structures work together to achieve two main goals: delivery of oxygen and removal of carbon dioxide. 3. What are the divisions of the Pulmonary System and what organs comprise each division? Conducting portion – comprises of nasal cavities, pharynx, larynx, trachea, bronchi, bronchioles and terminal bronchioles. Respiratory portion – system’s main function of gas exchange occurs, consisting of respiratory bronchioles, alveolar ducts and alveoli. 4. What is the major lining epithelium of the organs in the Pulmonary system? Lined with mucosa having ciliated pseudostratified columnar epithelium (respiratory epithelium). 5 major cell types: Ciliated columnar cells, goblet cells. Brush cells,small granule cells, basal cells 5. What is dyspnea? And what role does the respiratory system play in persons with acute shortness of breath? Dyspnea is the medical term for shortness of breath (air hunger). Dyspnea affects the level of oxygen delivered in the body. Without the proper amount of oxygen delivered in the body, hypoxia or hypoxemia occur leading to symptom of decrease level of consciousness. This may be due to certain illnesses originating from the respiratory system (e.g. COPD, asthma, pneumonia), cardiovascular (pulmonary edema, myocardial infarction, angina), GI/Hepatic (ascites, acute liver failure), renal (acute renal failure, pericardial effusion), hematological (anemia) and neuromuscular (myasthenia gravis, trauma to phrenic nerves). It could be allergic reactions and anxiety. Understanding and learning about the respiratory system will aid health care professionals in identifying the cause of dyspnea. Case #2 1. Identify the parts of the respiratory system and their different histologic characteristics. Vestibules of nasal cavities – stratified squamous(keratinized to nonkeratinized) Most areas of nasal cavity – respiratory epithelium (Pseudostratified Ciliated Columnar epithelium) Superior areas of nasal cavities – olfactory epithelium, with bipolar neurons Nasopharynx and posterior Oropharynx – respiratory epithelium and stratified squamous epithelium Larynx – respiratory and stratified squamous epithelium Trachea – respiratory epithelium 2. Describe the pulmonary circulation and contrast it with the systemic circulation. Low oxygen blood carried by the SVC and IVC will enter the right atrium, passing thru the tricuspid valve, gets in to the right ventricle. The right ventricle will pump blood to the pulmonary artery and into the lungs for the exchange of gases, this will occur at the alveoli wherein there is capillary exchange of oxygen and carbon dioxide. Blood becomes oxygenated and goes into the pulmonary vein and then to the left atrium. Oxygenated blood then goes to the left ventricles thru the mitral valve and pumps into the aorta. Blood will then travel to the aortic arch and into the body’s system. 3. Discuss the Blood- Gas Barrier and its function. The blood–air barrier (alveolar–capillary barrier or membrane) exists in the gas exchanging region of the lungs. It exists to prevent air bubbles from forming in the blood, and from blood entering the alveoli. The barrier is permeable to molecular oxygen, carbon dioxide, carbon monoxide and many other gases. The barrier between capillary blood and alveolar air comprising the alveolar epithelium and capillary endothelium with their adherent basement membrane and epithelial cells cytoplasm. Pulmonary gas exchange occurs across this membrane. Failure of the barrier may occur in a pulmonary barotrauma. This can be a result of several possible causes, including blast injury, swimming-induced pulmonary edema, and breathing gas entrapment or retention in the lung during depressurization, which can occur during ascent from underwater diving or loss of pressure from a pressurized vehicle, habitat or pressure suit.