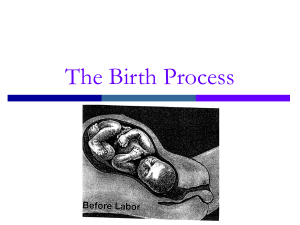
Labor and Delivery Preparation Questions: 1. Describe the signs of true labor. The signs of true labor are: 1. Contractions that occur regularly and are stronger, longer, and closer together a. Are more intense with walking b. Felt in the lower back and radiate to the lower portion of the abdomen c. Continue despite the use of comfort measures 2. Cervix shows the progressive changes of: a. Softening b. Effacement c. Dilation signaled by the appearance of bloody show d. Moves to an increasingly anterior position (baby’s head facing mom’s back) 3. Fetus’ presenting parts become engaged in the pelvis a. Increased ease of breathing (more room to breathe) b. Presenting part presses downward and compresses the bladder leads to increased urinary frequency 2. What is the length of each stage of labor? The length of each stage of labor is: 1. Stage One (Cervix dilates from 0 to 10cm) – Longest stage and differs from each person/pregnancy, can last 12 to 19 hours 2. Stage Two (The baby is delivered) – Starts when the cervix is fully dilated and effaced and ends after the baby is delivered, can last 20 minutes to two hours 3. Stage Three (The placenta is delivered) – Occurs 5 to 30 minutes after birth; greater than 30 minutes indicates a retained placenta 4. Stage Four (Recovery) – Occurs the first 1 to 4 hours after delivery of the placenta 3. What assessments should be made to evaluate the progress of labor? Assessments that should be made to evaluate the progress of labor are how many centimeters dilated the patient is, how effaced her cervix is, and the presentation of an involuntary urge to push in the expulsion of the fetus. 4. How will you meet the emotional needs of a laboring patient? The nurse can meet the emotional needs of a laboring patient by providing a quiet environment, encouraging participation in care and keep them informed, encouraging effective breathing patterns and rest between contractions, and providing praise and encouragement to the mother throughout the process. 5. How is pain managed during labor? Pain is managed during labor in a variety of ways. For pharmaceutical interventions, an anesthetic is injected into the epidural space in the spine to stop pain signals from reaching the brain; some women choose not to have this done. For non-pharmaceutical measures, the nurse can promote comfort by offering a warm shower when appropriate or a massage. 6. How are the frequency and duration of uterine contractions determined? The frequency and duration of uterine contractions are determined by stages: 1. Latent (early): Contractions are 15 to 30 minutes apart 2. Active: Contractions are 3 to 5 minutes apart (30 to 60 seconds in duration) 3. Transition: Contractions are 2 to 3 minutes apart (60 to 90 seconds in duration) 7. What is a reassuring fetal heart rate pattern? A reassuring fetal heart rate pattern is 120 to 160 beats per minute. Early decelerations are normal and mirror the image of mom’s contractions (they don’t technically come early). 8. How will you recognize when birth is imminent? The nurse will recognize when birth is imminent by the patient experiencing uterine contractions that are stronger and closer together, the sensation of pressure in the lower back and rectum, and an involuntary urge to push. 9. How will you prepare the patient and the room for birth? The nurse will prepare the patient and the room for birth by maintaining privacy and encouraging rest between contractions, placing the patient’s feet in stirrups and instruct her to move further down in the bed, and prepare any necessary instruments for when the baby is delivered. 10. What are signs of placental separation? Signs of placental separation are abdominal pain, uterine contractions that are longer and more intense than average labor contractions, uterine tenderness, backache or back pain, and decreased fetal movement.