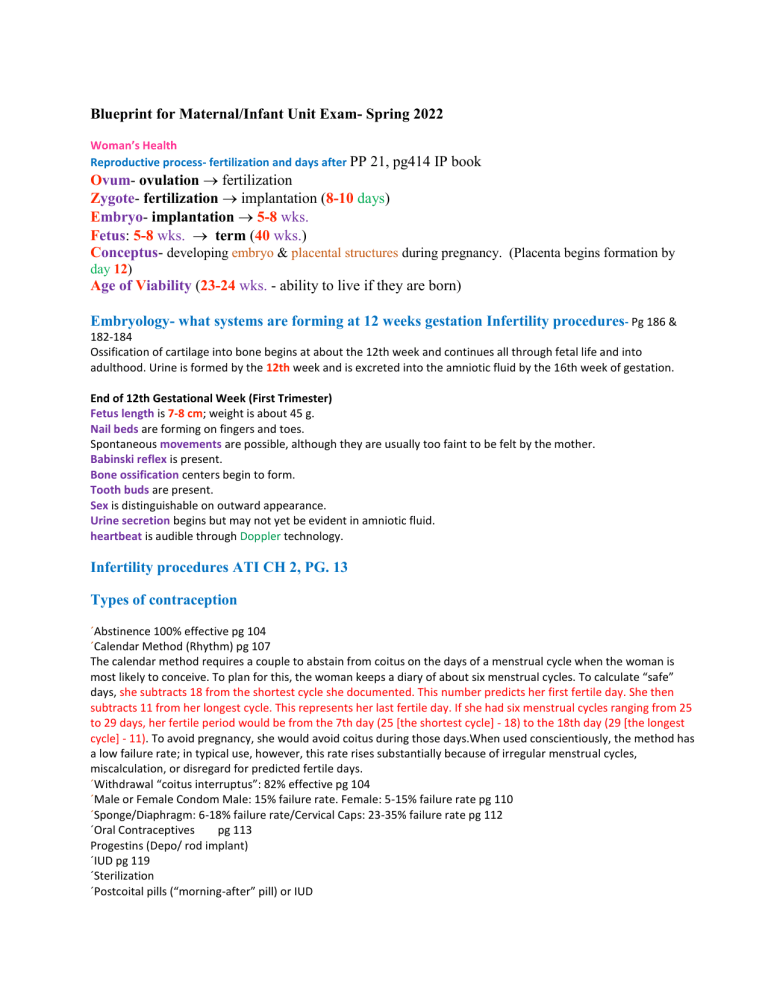
Blueprint for Maternal/Infant Unit Exam- Spring 2022 Woman’s Health Reproductive process- fertilization and days after PP 21, pg414 IP book Ovum- ovulation fertilization Zygote- fertilization implantation (8-10 days) Embryo- implantation 5-8 wks. Fetus: 5-8 wks. term (40 wks.) Conceptus- developing embryo & placental structures during pregnancy. (Placenta begins formation by day 12) Age of Viability (23-24 wks. - ability to live if they are born) Embryology- what systems are forming at 12 weeks gestation Infertility procedures- Pg 186 & 182-184 Ossification of cartilage into bone begins at about the 12th week and continues all through fetal life and into adulthood. Urine is formed by the 12th week and is excreted into the amniotic fluid by the 16th week of gestation. End of 12th Gestational Week (First Trimester) Fetus length is 7-8 cm; weight is about 45 g. Nail beds are forming on fingers and toes. Spontaneous movements are possible, although they are usually too faint to be felt by the mother. Babinski reflex is present. Bone ossification centers begin to form. Tooth buds are present. Sex is distinguishable on outward appearance. Urine secretion begins but may not yet be evident in amniotic fluid. heartbeat is audible through Doppler technology. Infertility procedures ATI CH 2, PG. 13 Types of contraception ´Abstinence 100% effective pg 104 ´Calendar Method (Rhythm) pg 107 The calendar method requires a couple to abstain from coitus on the days of a menstrual cycle when the woman is most likely to conceive. To plan for this, the woman keeps a diary of about six menstrual cycles. To calculate “safe” days, she subtracts 18 from the shortest cycle she documented. This number predicts her first fertile day. She then subtracts 11 from her longest cycle. This represents her last fertile day. If she had six menstrual cycles ranging from 25 to 29 days, her fertile period would be from the 7th day (25 [the shortest cycle] - 18) to the 18th day (29 [the longest cycle] - 11). To avoid pregnancy, she would avoid coitus during those days.When used conscientiously, the method has a low failure rate; in typical use, however, this rate rises substantially because of irregular menstrual cycles, miscalculation, or disregard for predicted fertile days. ´Withdrawal “coitus interruptus”: 82% effective pg 104 ´Male or Female Condom Male: 15% failure rate. Female: 5-15% failure rate pg 110 ´Sponge/Diaphragm: 6-18% failure rate/Cervical Caps: 23-35% failure rate pg 112 ´Oral Contraceptives pg 113 Progestins (Depo/ rod implant) ´IUD pg 119 ´Sterilization ´Postcoital pills (“morning-after” pill) or IUD Antepartum TORCH infections- signs/symptoms •Toxoplasmosis: caused by a protozoan parasite (Toxoplasma gondii), spread through cat feces, uncooked meat, & contaminated soil. Passed through the placenta to fetus. Infection higher during 3rd trimester. Maternal infections with fever, malaise, hepatosplenomegaly. Can cause spontaneous abortion in first trimester. Infants have damage to brain, retina, skeletal muscle, cardiac muscle. No universal screening. Maternal testing with igg antibodies treatment with antibiotics prenatally. NB treated for 12 months after birth. •Other- Syphilis (see previous discussion) •Rubella: RNA virus spread by inhalation of infected particles. Low rates now due to vaccines. Risk of congenital rubella occurs in first trimester, decreases in 2nd trimester, and rises again in 3rd trimester. Maternal symptoms mild, fetal infection can result in miscarriage, stillbirth, or congenital rubella syndrome. NB can have a “blueberry muffin rash” No specific treatment for newborns and remain contagious for up to a year. Vaccinate mother postpartum. •Cytomegalovirus (CMV): the most common congenital viral infection, and a leading cause of long-term disabilities in infants (hearing, ocular, cardiac). Most common cause of non-hereditary hearing loss.. Risk of vertical transmission 30-40% in primary infection in pregnancy. There is no treatment for maternal or fetal CMV. Acyclovir has many toxic side effects. •Herpes simplex: STI, double-stranded DNA virus in 2 types: HSV-1 and HSV-2. in-utero transmission rare, neonatal infections low. The risk of vertical transmission is highest in primary infection during pregnancy. Most pregnant women are asymptotic, but if present painful external genital lesions are present. They quickly convert to vesicles & resolve. Neonatal infections involve a rash, CNS involvement and disseminated disease (sepsis, Rds, dic). Acyclovir to treat. Complications of pregnancy- signs to report to the provider (list of complications on PP #38) (Page 251-253) Report: vaginal bleeding, persistent vomiting, chills & fever or pain on urination, sudden escape of clear fluid from the vagina, abdominal or chest pain, gestational hypertension (Rapid weight gain (over 2 lb/week in the second trimester, over 1 lb/week in the third trimester), Swelling of the face or fingers, Flashes of light or dots before the eyes, Dimness or blurring of vision, Severe, continuous headache, Decreased urine output, Right upper quadrant pain unrelated to fetal position, Blood pressure increased above 140/90 mmHg), Increase or decrease in fetal movement, and uterine contractions before 37 weeks of pregnancy. Placenta previa- risk factors: CH 21 Pg 537 in the textbook Pg 44 in ATI: Risk factors: previous placenta previa, uterine scarring (previous cesarean birth, curettage, endometritis), maternal age greater than 35 y/o, multifetal gestation, multiple gestations, & smoking Abruptio placentae- s/s Pg 46 ATI: sudden onset of intense localized uterine pain w/ dark red vaginal bleeding. Area of uterine tenderness can be localized or diffuse over uterus & board like. Contractions w/ hypertonicity Fetal distress Clinical findings of hypovolemic shock Nagel’s rule- calculations for EDB Take the first day of the last menstrual period, subtract 3 months, add 7 days and 1 year as needed. Preeclampsia (Gestational Hypertension) – ATI pg. 62 S/S HTN, proteinuria, lower extremities pitting edema, epigastric pain, scotoma (a partial loss of vision or blind spot), RUQ pain, seizures. Preeclampsia: is GH with the addition of proteinuria of greater than or equal to 1+. Report of transient headaches might occur along w/ episodes of irritability. Edema can be present. Severe preeclampsia: BP 160/110 or greater, proteinuria greater than 3+, oliguria, elevated blood creatinine greater than 1.1 mg/dL, cerebral or visual disturbances (HA & blurred vision), hyperreflexia w/ possible ankle clonus, pulmonary or cardiac involvement, extensive peripheral edema, hepatic dysfunction, epigastric & right upper-quadrant pain, & thrombocytopenia. Pregnant teens- education techniques (textbook pg 104) Many sex education classes for adolescents advocate abstinence as the only contraceptive measure, so teenagers and young adults who take these courses may know little about other options. When discussing abstinence as a contraceptive method, be certain to provide information not only on the method but also suggestions for ways to comply with this method (Box 6.4). A worry is adolescents who make “abstinence pledges” to not have sexual intercourse until they are married may “tune out” not only additional information on contraception but also on safer sex practices. Then, if they break their pledge (about 50% do), that could leave them more vulnerable to STIs and pregnancy than others Infertility procedures ´Male: ´Semen Analysis ´Ultrasound: of testes,scrotum, ejaculatory ducts, seminal vesicles, vas deferens ´Female. ´Pelvic Exam ´Hormone analysis ´Postcoital test ´Ultrasound: female reproductive organs ´Hysterosalpingography- visualize fallopian tubes ´Hysteroscopy- uterus examined ´Laparoscopy- check internal organs (Eneida) Amniotic fluid- characteristics and functions of Slide 25/(pg 179 Brunner’s) ´Amniotic membranes: amnion, chorion ´Amniotic fluid- 800-1200 mL at term, changed almost every hour, filters, swallowed by the fetus, mostly made up fetal urine. Oligohydramnios (<300 mL, polyhydramnios or hydramnios (>2000 mL). Amniotic fluid never becomes stagnant because it is constantly being newly formed and absorbed by direct contact with the fetal surface of the placenta. The major method of absorption, however, happens within the fetus. Because the fetus continually swallows the fluid, it is absorbed from the fetal intestine into the fetal bloodstream. From there, it goes to the umbilical arteries and to the placenta and is exchanged across the placenta to the mother’s bloodstream. At term, the amount of amniotic fluid has grown so much it ranges from 800 to 1,200 ml. If for any reason the fetus is unable to swallow (esophageal atresia or anencephaly are the two most common reasons), excessive amniotic fluid or hydramnios (more than 2,000 ml in total or pockets of fluid larger than 8 cm on ultrasound) will result (Ghionzoli, James, David, et al., 2012). Hydramnios may also occur in women with diabetes because hyperglycemia causes excessive fluid shifts into the amniotic space (Perovic´, Garalejic´, Gojnic´, et al., 2012). Early in fetal life, as soon as the fetal kidneys become active, fetal urine adds to the quantity of the amniotic fluid. A disturbance of kidney function, therefore, may cause oligohydramnios or a reduction in the amount of amniotic fluid. Oligohydramnios can be detected by ultrasound. The amniotic fluid index is measured, and it should be at least 5 cm. The vertical pocket of amniotic fluid should be greater than 2 cm (American Congress of Obstetricians and Gynecologists [ACOG], 2014). The appropriate amount of amniotic fluid ensures adequate kidney function. The most important purpose of amniotic fluid is to shield the fetus against pressure or a blow to the mother’s abdomen. Because liquid changes temperature more slowly than air, it also protects the fetus from changes in temperature. Another function is that it aids in muscular development, as amniotic fluid allows the fetus freedom to move. Finally, it protects the umbilical cord from pressure, thus protecting the fetal oxygen supply. Even if the amniotic membranes rupture before birth and the bulk of amniotic fluid is lost, some will always surround the fetus in utero because new fluid is constantly being formed. Amniotic fluid is slightly alkaline, with a pH of about 7.2. Checking the pH of the fluid at the time membranes rupture and amniotic fluid is released helps to differentiate amniotic fluid from urine because urine is acidic (pH 5.0 to 5.5). Preterm labor- risks for (pg 67 ATI) Infections of the urinary tract or vagina, HIV, active herpes infection, or chorioamnionitis (infection of the amniotic sac) Previous preterm birth, multifetal pregnancy, smoking, substance abuse, violence or abuse, lack of prenatal care, uterine abnormalities, & low pregnancy weight (maura) Tuberculosis (TB)- treatment during pregnancy-book pg. 505 Women with active tuberculosis need treatment during pregnancy. Isoniazid (INH), rifampin (RIF), and ethambutol hydrochloride (Myambutol)——may be given without apparent teratogenic effects. INH, however, may result in a peripheral neuritis if a woman does not also take supplemental pyridoxine (vitamin B6). Ethambutol has the side effect of causing optic atrophy and loss of green color recognition in the woman. To detect this, test the woman’s ability to recognize green at prenatal visits using the color section of a Snellen (eye test) chart. If symptoms develop, inform her health provider about possibly discontinuing the drug. A woman who had tuberculosis earlier in life must be especially careful to maintain an adequate level of calcium during pregnancy to ensure the calcium tuberculosis pockets in her lungs are not broken down and the disease is not reactivated. A woman is usually advised to wait 1 to 2 years after the infection becomes inactive before attempting to conceive as pressure on the diaphragm from the enlarging uterus changes the shape of the lung and can break open recently calcified pockets more readily than well-calcified lesions. Pockets may also break open during labor from the increased intrapulmonary pressure of pushing. Recent inactive tuberculosis may also become active during the postpartum period as the lung returns to its more vertical prepregnant position following birth. Although tuberculosis can be spread by the placenta to the fetus, if it is active, it usually is spread to the infant after birth by the mother’s coughing. Obtaining a negative sputum culture after birth rules out active tuberculosis. Urge the woman to continue taking her tuberculosis medications as prescribed during breastfeeding as only small amounts of these are secreted in breast milk and so are safe for her infant GTPAL classification system-PP-SLIDE •G- gravida, # of pregnancies • P- para, # pregnancies that were > 20 weeks, live or not = (TPAL) • T- # term pregnancies, > 37 weeks •P- # preterm pregnancies, < 37 weeks •A- # of abortions, loss at < 20 weeks •L- # of living children •* A multigestatonal pregnancy is counted as one para •G- 3 •P – 2 (term) 0 (preterm), 0 (abortions), 2 (living children •Written G3P2002 •Primagravida- pregnant for the first time •Nulligravida- never been and not currently pregnant •Multigravida- pregnant previously •Primapara- carried one child at least 20 weeks •Grand multipara- carried 5 or more pregnancies > 20 wks HIV infection- risks for infection during pregnancy Intrapartum Maternal infections slide 9 •Human immunodeficiency virus (HIV): in the u.s. 8700 with Hiv give birth yearly •Organism: a retrovirus that attacks t lymphocytes. Causes immunosuppression. •Mode of transmission: Perinatal transmission occurs ,2% with prenatal care and treatment. Transmitted also through breast milk •Clinical Presentation: fatigue & influenza-type feelings, fever, anemia, lymphadenopathy, diarrhea and weight loss. •Testing: Universal screening at first prenatal visit & 3 months. Rapid hiv antibody tests, Elisa & western blot •Treatment: mothers should be treated during pregnancies and newborns of HIV positive mothers should also be treated. Antiretroviral agent or nucleoside reverse transcriptase inhibitor (Retrovir) at 14 weeks of pregnancy. Infant receives Retrovir for 6 weeks starting at birth. •Effect on fetus/newborn: HIV infection possible if untreated, other infections due to a weak immune system and possible death. Second stage of labor- physiological needs-LVN BOOK PG 248 Instruct the woman to bear down with the urge to push ■ More progress is made and fewer traumas are noted to mother and fetus with spontaneous pushing efforts. Monitor for fetal response to pushing; check FHR every 5–15 minutes or after each contraction. ■ Assessing fetal heart rate response to pushing efforts Provide comfort measures. Support and encourage woman’s spontaneous pushing efforts. Attend to perineal hygiene as needed, as the woman may pass stool with pushing. Provides a cleaner pathway Give praise and encouragement of progress made. Support and empowerment of woman’s efforts Encourage rest between contractions by breathing with the patient and therapeutic touch. Decreases fatigue and hypoxia in fetus by providing increased oxygenation Review and reinforce pushing technique by: Maintaining eye contact. Developing a rhythm and pushing style to deal with each contraction that maximizes the woman’s urge to push. Using direct, simple, and focused communication, avoiding unnecessary conversation. Advocate on the woman’s behalf for her desires of the delivery plan. Assist the support person and partner. ■ Role model supportive behaviors. ■ Offer support, praise, and encouragement. ■ Assist with food and rest and provide breaks. EFM- steps when placing on a laboring woman-book pg. 355-356 The presence and duration of uterine contractions is gained by means of a pressure transducer or tocodynamometer strapped to the woman’s abdomen or held in place by stockinette Place the transducer snugly over the uterine fundus or the area where contractions are most easily felt. The transducer works to convert the pressure originated by the contraction into an electronic signal that is then recorded on graph paper. The FHR is monitored with the use of an ultrasonic sensor or monitor also strapped against a woman’s abdomen at the level of the fetal chest. The small Doppler unit converts fetal heart movements into audible beeping sounds and also records them on graph paper. Epidural anesthesia- nursing interventions during ATI pg. 83 Assess and record FHR and vital signs. Assist with obtaining an ultrasound to determine whether a cesarean birth is indicated. ● Position the client in a supine position with a wedge under one hip to prevent compression of the vena cava. ● Insert an indwelling urinary catheter. ● Ensure the client has signed the informed consent form. ● Apply a sequential compression device. ● Administer preoperative medications. ● Prepare the surgical site. ● Insert an IV catheter, and initiate administration of IV fluids. ● Determine whether the client has had nothing by mouth since midnight before the procedure. If the client has, notify the anesthesiologist. ● Ensure that preoperative diagnostic tests are complete, including an Rh-factor test. ● Explain the procedure to the client and their partner. ● Provide emotional support. ● ● Intrapartum continuedPain management in labor- nonpharmacological Support from a doula of coach Complementary and alternative therapies: Relaxation Focusing and imagery Spirituality Breathing techniques Herbal preparations Aromatherapy and essential oils Heat and cold application Bathing or hydrotherapy Therapeutic touch and massage Yoga and meditation Reflexology Hypnosis Biofeedback Transcutaneous Electrical Nerve Stimulation Intracutaneous Nerve Stimulation Acupuncture and Acupressure Determining labor status- exams needed Spontaneous rupture of the membranes (SROM) may occur before the onset of labor but typically occurs during labor. Once the membranes have ruptured, the protective barrier to infection is lost, and ideally the woman should deliver within 24 hours to reduce the risk of infection to herself and her fetus. Assessing the Status of Membranes Different techniques may be used to confirm ROM: ■ A speculum exam may be done to assess for fluid in the vagi- nal vault (pooling) ■ Nitrazine paper: The paper turns blue when in contact with amniotic fluid. Can be dipped in the vaginal fluid or fluid- soaked Q-tip can be rolled over the paper ■ Ferning: During a sterile speculum exam a sample of fluid in the upper vaginal area is obtained.he fluid is placed on a slide and assessed for “ferning pattern” under a microscope A ferning pattern confirms ROM. AmniSure testing kit. The AmniSure ROM Test is a rapid, non-invasive immunoassay that aids clinicians with the diagnosis of ROM in pregnant women with signs and symptoms suggestive of the condition. According to published data it is ~99% accurate. Preparation for a C-section birth- lvn pg 349 The major maternal medical indications for a cesarean birth are: Previous cesarean birth Placental abnormalities Dystocia, difficult childbirth, or dysfunctional labor that is caused by: Ineffective uterine contractions that lead to the prolonged first stage of labor Cephalopelvic disproportion Complete the appropriate admission assessments and required preoperative forms. ■ Expected findings ■ Couplesandfamiliesmayhaveanincreasedlevelofanxiety related to the surgery and method of anesthesia. ■ Anxietymayberelatedtothisbeingthewoman’sfirstsurgical experience and fears of the unknown for self and fetus. ■ The expectant father may have concerns about injury to his partner and/or child. Couples are excited about the upcoming birth of their child. Couples have questions and concerns regarding the cesarean birth and method of anesthesia. Vital signs are within normal limits, with a mild increase in blood pressure related to increased anxiety. Obtain baseline vital signs Obtain laboratory testing as per orders, CBC, platelets, and type and screen. A delay in lab results can result in a delay in surgery. Obtain a baseline fetal heart rate monitor strip before and after administration of regional anesthesia. ■ Expected findings ■ Category I fetal heart rate Review the prenatal chart for factors that place the woman at risk during or after cesarean birth and ensure that physician and anesthesiologist or CRNA are aware of risk factors such as low platelet count. Assess womens’ knowledge and educational needs. Provide preoperative education. Identify and respect the cultural values, choices, and preferences of the woman and her family. Individualize care to meet needs of patient and family. Ensure that all required documents, such as prenatal record, current laboratory reports, and consent forms, are in the woman’s chart. Verify that the woman has been NPO for 6–8 hours before surgery. Women without complications undergo- ing scheduled cesarean birth may have limited amounts of clear liquids up to 2 hours prior to induction of anes- thesia (American Society of Anesthesiologists Task Force, 2007). Follow hospital policy for NPO status. Complete the surgery checklist, which includes removal of jewelry, eyeglasses/contact lenses, and dentures. Eyeglasses can be given to the support person to bring into the operating room so the woman can use them to see her newborn baby. Explain to the couple what they can expect before, dur- ing, and after the cesarean birth. Fetal station- how to assess for Station refers to the relationship of the presenting part of the fetus to the level of the ischial spines. When the presenting fetal part is at the level of the ischial spines, it is at a 0 station (synonymous with engagement). If the presenting part is above the spines, the distance is measured and described as minus stations, which range from −1 to −4 cm. If the presenting part is below the ischial spines, the distance is stated as plus stations (+1 to +4 cm). At a +3 or +4 station, the presenting part is at the perineum and can be seen if the vulva is separated (i.e., it is crowning). interventions for fetal distress -LVN BOOk Pg. Respiratory distress syndrome (RDS) is a life-threatening lung disorder that results from underdeveloped and small alveoli and insufficient levels of pulmonary surfactant. These two combined factors can cause an alteration in alveoli surface ■ Lecithin/sphingomyelin (L/S) ratio: Lecithin and sphingomyelin are two phospholipids that are detected in the amniotic fluid. The ratio between the two phospholipids provides information on the level of surfactant. A L/S ratio greater than 2:1 in a nondiabetic woman indicates the fetus’s lungs are mature. A L/S ratio of 3:1 in a diabetic woman indicates the fetus’s lungs are mature. Assessment Findings ■ Respiratory distress varies based on degree of prematurity. ■ Respiratory difficulty begins shortly after delivery and the neonate must work progressively harder at breathing to maintain open terminal airways ■ Tachypnea is present. ■ Intercostal retractions; seesaw breathing patterns occur. ■ Expiratory grunting. ■ Nasal flaring is present. ■ Increased oxygen requirements are increased to maintain a PaO2 and PaCO2 within normal limits. ■ The normal range of PaO2 is 60–70 mm Hg. ■ The normal range of PaCO2 is 35–45 mm Hg. ■ Skin color is gray or dusky. ■ Breath sounds on auscultation are decreased. Rales are present as RDS progresses. ■ The neonate is lethargic and hypotonic. ■ X-ray exam shows a reticulogranular pattern of the peripheral lung fields and air bronchograms ■ Hypoxemia may occur (PaO2 <50 mm Hg). ■ Acidosis may result from sustained hypoxemia. Nursing Actions Nursing actions for neonates with RDS are similar to actions for preterm neonates, with additional emphasis on the following: ■ Provide respiratory support. ■ Maintain a patent airway. ■ Assess for correct placement of endotracheal tube. ■ Listen for equal breath sounds bilaterally, assess for equal chest rise, use commercial end tidal CO2 detector. ■ Administer oxygen as ordered to maintain oxygen satura- tion within ordered parameters. ■ Hypoxemia and acidosis may further decrease surfactant production. ■ Short-term oxygen administration may be given using a mask or tubing. ■ Long-term oxygen administration may be given using a nasal cannula or oxygen hood. ■ Oxygen is humidified and warmed. ■ Warmed oxygen aids in thermoregulation for the infant. ■ Administer and monitor continuous positive airway pressure (CPAP), mechanical ventilation, high-frequency oscillatory ventilation, and/or ECMO as per order. ■ Minimize oxygen demand by maintaining a neutral thermal environment, clustering care to decrease stress, and treating acidosis as clinically indicated and ordered. ■ Suction airway as needed for removal of secretions as neonates have a smaller airway diameter, which increases the risk of obstruction. ■ Suctioning may stimulate the vagus nerve, causing bradycardia, hypoxemia, or bronchospasm. First stage of labor- therapeutic interventions for Perform admission Procedures and orient patient to setting. Review prenatal records. Assess FHR and uterine activity. Assess maternal vital signs and pain. Assist with ambulation and maternal position changes. Provide comfort measures. Discuss pain management options. Administer pain meds PRN. Monitor I&O and provide oral and/or IV hydration as indicated. Provide ongoing assessment of labor progress. Request an immediate bedside evaluation by a physician ( eneida) Oxytocin induction- when to discontinue (slide22 high risk drugs) •Uses in the obstetrical patient: •1. Induction of labor •Rationale; Pitocin is a uterine stimulant. It works by causing uterine contractions by changing calcium concentrations in the uterine muscle cells (increases intracellular calcium). The dose may need to be higher in a preterm mother as there are less oxytocin receptor cells in the uterine muscle cells. Preterm induction may require higher doses as there are less receptor cell in the preterm uterus •2. Augmentation of labor •Rationale; Helps make contractions stronger and more effective. Ineffective labor can be augmented with Pitocin. Can also be used during the third stage of labor to help with expulsion of the placenta. •Use in obstetrical patients-continued •3. Help abort the fetus in cases of incomplete abortion or miscarriage. •Rationale; Stimulates contractions of the uterus to help expel all the fetal tissues & placenta in an incomplete abortion to prevent infection, disseminated intravascular coagulation (DIC), or bleeding In the mother. Doses are much higher with this use- 10-20 mU/min. •4. Stop postpartum hemorrhage/bleeding. •Rationale; Uterine contractions cause blood vessels to clamp down & prevent bleeding (control of atony). Pitocin causes uterine contractions. Doses of 20-40 mU/min used. •5. Could be helpful in postpartum depression (nasal spray). (slide 34 of high risk dros… when to stop oxytocin) •Consider turning Pitocin drip off during the 2nd stage of labor. Dilation of the vagina and pelvic floor is a strong stimulus of natural release of oxytocin, so the drip may be stopped, (pg 664 brunners) Oxytocin induction Induction of labor means labor is started artificially. Augmentation of labor refers to assisting labor that has started spontaneously but is not effective. Although induction may be necessary to initiate labor before the time when it would have occurred spontaneously because a fetus is in danger, it is not used as an elective procedure until the fetus is at term (over 39 weeks). At one time, induction could be completed if a fetus was proven to have adequate lung surfactant by amniocentesis at term but less than 39 weeks. However, the American College of Obstetricians and Gynecologists (ACOG) has issued a statement (ACOG, 2013) indicating that fetal lung maturity should not be used and inductions should be avoided until 39 weeks unless medically indicated. Conditions that might make induction necessary before that time include preeclampsia, eclampsia, severe hypertension, diabetes, Rh sensitization, prolonged rupture of the membranes, and intrauterine growth restriction. Postmaturity (a pregnancy lasting beyond 42 weeks) is yet another situation that makes it more potentially dangerous for a fetus to remain in utero than to be born. Because either augmentation or initiation of labor carries a risk of uterine rupture or premature separation of the placenta, it must be used cautiously in women with multiple gestation, polyhydramnios, grand parity, who are older than 40 years, or have previous uterine scars (Norman, 2012). Oxytocin is an effective uterine stimulant, but there is a thin line between adequate stimulation and hyperstimulation, so careful observation during the entire infusion time is an important nursing responsibility (Bor, Ledertoug, Boie, et al., 2016). Before induction of labor is begun in term and postterm pregnancies, the following conditions should be present: The fetus is in a longitudinal lie. The cervix is ripe, or ready for birth. The presenting part is the fetal head (vertex) and is engaged. There is no CPD. The fetus is estimated to be mature by date (over 39 weeks). Oxytocin is always administered intravenously, so that, if uterine hyperstimulation should occur, it can be quickly discontinued The danger of hyperstimulation is that a fetus needs 60 to 90 seconds between contractions in order to receive adequate oxygenation from placenta blood vessels. Hyperstimulation (i.e., tachysystole) is usually defined as five or more contractions in a 10-minute period or contractions lasting more than 2 minutes in duration or occurring within 60 seconds of each other, situations that have the potential to interfere with placenta filling and fetal oxygenation. If uterine hyperstimulation should occur, several interventions such as asking the woman to turn onto her left side to improve blood flow to the uterus, administering an IV fluid bolus to dilute the level of oxytocin in the maternal blood stream, and administering oxygen by mask at 8 to 10 L are all helpful. In addition, a primary care provider may prescribe terbutaline to relax the uterus. The surest method to relieve tachysystole, however, is to immediately discontinue the oxytocin infusion. oxytocin (Pitocin) is commonly mixed in the proportion of 10 International Units in 1,000 ml of Ringer’s lactate. Possible Adverse Effects: nausea, vomiting, cardiac arrhythmias, uterine hypertonicity, tetanic contractions, uterine rupture (with excessive dosages), severe water intoxication, and fetal bradycardia After cervical dilatation reaches 4 cm, artificial rupture of the membranes may be performed to further induce labor, and the infusion may be discontinued at that point. A side effect of oxytocin is that it causes peripheral vessel dilation, and peripheral dilation can lead to extreme hypotension. To ensure safe induction, therefore, take the woman’s pulse and blood pressure every hour. A second side effect of oxytocin is that it can result in decreased urine flow, possibly leading to water intoxication. This is first manifested by headache and vomiting. If you observe these danger signs in a woman during induction of labor, report them immediately and halt the infusion. Water intoxication in its most severe form can lead to seizures, coma, and death because of the large shift in interstitial tissue fluid. Keep an accurate intake and output record and test and record urine specific gravity throughout oxytocin administration to detect fluid retention. Limit the amount of IV fluid being given to that prescribed (usually 150 ml/hr by ensuring the main IV fluid line is infusing at a rate not greater than 2.5 ml/min). Contractions should occur no more often than every 2 minutes, should not be stronger than 50 mmHg pressure, and should last no longer than 70 seconds. The resting pressure between contractions should not exceed 15 mmHg by monitor (Fig. 23.4). If contractions become more frequent or longer in duration than these safe limits, or if signs of fetal distress occur, stop the IV infusion and seek help immediately. Anticipate oxygen administration may be needed to maintain fetal oxygenation. If stopping the oxytocin infusion does not stop the hyperstimulation, a tocolytic such as terbutaline may be prescribed to decrease myometrial activity. After birth, observe the infant closely for hyperbilirubinemia and jaundice because these are associated with oxytocin induction. Amniotomy procedure- nursing assessment during ATI Pg. 103 (pg 610 brunner’s) In rare instances, the cord may be felt as the presenting part on an initial vaginal examination during labor or can be visualized on ultrasound if one of these is taken during labor. More often, however, cord prolapse is first discovered only after the membranes have ruptured, when the FHR is discovered to be unusually slow or a variable deceleration FHR pattern suddenly becomes apparent on a fetal monitor. On inspection, the cord may be visible at the vulva. To rule out cord prolapse, always assess fetal heart sounds immediately after rupture of the membranes, whether this occurs spontaneously or by amniotomy. (ATI pg 90, 91, 92) Fetal Bradicardia (FHR less than 110/min for 10 min or more) d/c oxytocin Late Decelerations (slowing of FHR at the start of contractions with return of FHR to baseline at the end of contractions), d/c oxytocin Variable decelerations FHR (Transitory, abrupt slowing of FHR 15/min or more below baseline for at least 15 seconds, variable in duration, intensity and timing in relation to uterine contraction) d/c oxytocin Vertical lie- position of fetus (slide 43 welcome rnsg 1327 ppp) ´Fetal Lie- relationship of maternal spine to fetal spine (parallel or transverse) (pg331 brunner’s) Vertical (longitudinal) position Approximately 96% of fetuses assume a longitudinal lie (with their long axis parallel to the long axis of the woman) Longitudinal lies are further classified as cephalic, which means the fetal head will be the first part to contact the cervix, or breech, with a foot or the buttocks as the first portion to contact the cervix. Magnesium Sulfate- adverse and side effects of (slide 7,8, of high risk dros ppp) •Side Effects (Maternal) •Flushing/hot flashes •Headache/dizziness •Blurred vision Side Effects (Fetus/Newborn) Low APGAR scores Poor muscle tone Low calcium levels/osteopenia •Lethargy/tiredness •Muscle weakness/ decreased DTR’s •Nausea/vomiting/constipation (paralytic ileus) •Respiratory depression/ cardiac arrest •Decreased urine output •Signs of Magnesium Toxicity: •Visual changes (even temporary blindness) •Somnolence (drowsiness) •Flushing •Muscle paralysis/ loss of deep tendon reflexes •Pulmonary edema •Urine output < 30 mL/hr (Mg is only exceted in the kidneys) EFM- frequency and duration on a strip Bold line to bold line = 1 min, small box = 10 seconds Fetal positioning- frank breech (pg 332 brunner’s) Breech presentation can cause a difficult birth, with the presenting point influencing the degree of difficulty. Three types of breech presentation (complete, frank, and footling) are possible Longitudinal Moderate Attitude is moderate because the hips are flexed, but the knees are extended to rest on the chest. The buttocks alone present to the cervix Stage 3 of labor- placental separation characteristics (slide 48 of welcome ppp)´Stage III (birth of baby to expulsion of placenta) (pg 369 brunner’s) The third stage of labor is the time from the birth of the baby until the placenta is delivered. For most women, this is a time of great excitement because the infant has been born, but this can also be a time of feeling anticlimactic because the infant has finally arrived after being anticipated for so long a time. (pg 342 brunner’s) Placental Separation As the uterus contracts down on an almost empty interior, there is such a disproportion between the placenta and the contracting wall of the uterus that folding and separation of the placenta occur. Active bleeding on the maternal surface of the placenta begins with separation, which helps to separate the placenta still further by pushing it away from its attachment site. As separation is completed, the placenta sinks to the lower uterine segment or the upper vagina. The placenta has loosened and is ready to deliver when: There is lengthening of the umbilical cord. A sudden gush of vaginal blood occurs. The placenta is visible at the vaginal opening. The uterus contracts and feels firm again. If the placenta separates first at its center and lastly at its edges, it tends to fold on itself like an umbrella and presents at the vaginal opening with the fetal surface evident. Approximately 80% of placentas separate and present in this way. Appearing shiny and glistening from the fetal membranes, this is called a Schultze presentation. If, however, the placenta separates first at its edges, it slides along the uterine surface and presents at the vagina with the maternal surface evident. It looks raw, red, and irregular, with the ridges or cotyledons that separate blood collection spaces evident; this is called a Duncan presentation. Although there is no difference in the outcome, record which way the placenta presented. A simple trick of remembering the presentations is remembering that, if the placenta appears shiny, it is a Schultze presentation. If it looks “dirty” (the irregular maternal surface shows), it is a Duncan presentation (Fig. 15.12). This stage can take anywhere from 1 to 30 minutes and still be considered normal. Because bleeding occurs as the placenta separates, before the uterus contracts sufficiently to seal maternal capillaries, there is a blood loss of about 300 to 500 ml, not a great amount in relation to the extra blood volume that was formed during pregnancy. (ATI pg 97) Placental separation findings Fundus firmly Swift gush of dark blood from introitus Umbilical cord appears to lengthen as placenta descends Vaginal fullness on exam Assignment of 1 and 5 min Apgar scores to the neonate Stage 1-4 of labor, behavioral expectations of mother in each stage Postpartum (pg 341, 342)CH 15 Stage 1 – LAT Latent phase Cervical dilation: 0-3 cm Contractions: Irregular Mild-moderate Mother: talkative/ eager managed by controlled breathing. (teaching/ instructions time) Active phase Cervical dilation:4-7 cm Contractions: More regular moderate-strong Mother: This phase can be difficult for a woman because contractions grow so much stronger and last so much longer than they did in the latent phase that she begins to experience true discomfort. It is also both an exciting and a frightening time because it is obvious something dramatic is definitely happening. In a few hours, a woman will have a new baby. Her life will never be the same again. Transition phase Cervical dilation:8-10 cm Contractions: Mother: Woman may experience intense discomfort that is so strong, it might be accompanied by nausea and vomiting. She may also experience a feeling of loss of control, anxiety, panic, and/or irritability. Because of the intensity and duration of the contractions, it may seem as though labor has taken charge of her. A few minutes before, she may have enjoyed having her forehead wiped with a cool cloth or her back rubbed. Now, she may knock a partner’s hand away from her. Her focus turns entirely inward to the task of birthing her baby. As a woman reaches the end of this stage at 10 cm of dilatation, unless she has been administered epidural anesthesia, a new sensation, the irresistible urge to push, usually begins. Second Stage A woman typically feels contractions change from the characteristic crescendo– decrescendo pattern to an uncontrollable urge to push or bear down with each contraction as if to move her bowels. She may experience momentary nausea or vomiting because pressure is no longer exerted on her stomach as the fetus descends into the pelvis. She pushes with such force that she perspires and the blood vessels in her neck become distended.The fetus begins descent and, as the fetal head touches the internal perineum to begin internal rotation, her perineum begins to bulge and appear tense. The anus may become everted, and stool may be expelled. As the fetal head pushes against the vaginal introitus, this opens and the fetal scalp appears at the opening to the vagina and enlarges from the size of a dime, to a quarter, then a half-dollar. This is termed crowning. It takes a few contractions of this new type for a woman to realize everything is all right, just different, and to appreciate it feels better and less frightening, to push with contractions. As she concentrates on pushing, she may become unaware of the conversation in the room. Pain may disappear as all of her energy and thoughts are directed toward giving birth. As the fetal head is pushed out of the birth canal, it extends and then rotates to bring the shoulders into the best line with the pelvis. The body of the baby is then born. Third Stage The third stage of labor, the placental stage, begins with the birth of the infant and ends with the delivery of the placenta. Two separate phases are involved: placental separation and placental expulsion. After the birth of the infant, the uterus can be palpated as a firm, round mass just below the level of the umbilicus. After a few minutes of rest, uterine contractions begin again, and the organ assumes a discoid shape. It retains this new shape until the placenta has separated, approximately 5 minutes after the birth of the infant. Placental Separation As the uterus contracts down on an almost empty interior, there is such a disproportion between the placenta and the contracting wall of the uterus that folding and separation of the placenta occur. Active bleeding on the maternal surface of the placenta begins with separation, which helps to separate the placenta still further by pushing it away from its attachment site. As separation is completed, the placenta sinks to the lower uterine segment or the upper vagina. Once separation has occurred, the placenta delivers either by the natural bearing-down effort of the mother or by gentle pressure on the contracted uterine fundus by the primary healthcare provider (a Credé maneuver) Fourth Stage he first 1 to 4 hours after birth of the placenta is sometimes termed the “fourth stage” to emphasize the importance of close maternal observation needed at this time. Episiotomy after vaginal delivery- nursing diagnosis for (pg 412 brunner’s) Nursing Diagnosis: Risk for fluid volume deficit related to uterine atony Outcome Evaluation: Patient maintains vital signs within normal range; fundus is firm to palpation; lochia discharge is small to moderate with a minimum of clot formation. In order to assess if uterine atony is present, frequently assess vital signs, lochia amount, and fundal height. Teach patient the usual involution process and how to check her fundus and evaluate lochia so she can do this after she returns home. Nursing Diagnosis: Pain related to perineal discomfort, uterine cramping (afterpains), or muscular aches Outcome Evaluation: Patient states that degree of pain is tolerable; patient demonstrates knowledge of measures for adequate pain relief. (Erica) Uterine atony- interventions for pg 650 book is a serious condition that can occur after childbirth occurs when the uterus fails to contract after delivery of the baby and can lead to a potentially life-threatening condition known as the first part of hemorrhage. Interventions: uterine/ fundal massage followed by oxytocin. remain with the mother after massaging her, fundus, and assess to be certain her uterus is not relaxing again.. Be on guard for signs of uterine bleeding. Methylergonovine – assessment before use ati pg.140 Assess uterine tone and vagina bleeding. Do not administer to clients who have hypertension. Monitor for adverse reactions including hypertension, nausea, vomiting, and headache Signs of hemorrhage- early & late pg book528,529 Early: vaginal bleeding, confusing late: Increase pulse rate Decrease blood pressure Increase respiration rate Cold, clammy skin Decrease urine output Dizziness or decreased level of consciousness Decrease central venous pressure. PP hemorrhage- interventions for pg book 528 Omit vaginal examination, order type and cross-match of 2 units of whole blood, measure intake and output, monitor uterine contractions and fetal heart rate by external monitor, administer oxygen as necessary at 6 to 10 L min by face masks, place women flat in bed on her side, alert Healthcare team of emergency situation, begin intravenous fluid such as ringers lactate with a 16 or 18 gauge angiocath, withhold oral fluid, assess Vital Signs pulse respiration blood pressure every 15 minutes apply pulse oximeter and automatic blood pressure cuff necessary. Breastfeeding- instructions to mother:p468 Educating all pregnant women about the benefit and management of breastfeeding helping women initiate breastfeeding within half an hour after birth Assisting mothers to breastfeed and maintain lactation even if they should be separated from their infant not giving newborns food or drink other than breast milk unless medically indicated, so they are hungry to breastfeed. advise woman they need not introduce solid food until at least 4 months not giving newborn pacifiers to quite them as this can reduce the sucking initiative supporting rooming-in such as allowing mother and infant to remain together 24 hours a day encouraging breastfeeding on demand fostering the establishment of breastfeeding support groups and referring mother's to them on discharge from the birthing center of Hospital Vulvar hematoma- interventions for page144 ati Lacerations that occurred during labor and birth consists of tearing of soft tissues in the birth canal and adjacent structures including the vulvar, cervical. Pain rather than noticeable bleeding is the distinguishable clinical finding of hematoma. The client Risk for hemorrhage or infection due to laceration or hematoma pain. assess pain visually or manually inspect the vulva, perineum, and rectum of lacerations and or hematomas evaluate lochia continue to assess Vital Signs and hemodynamic status Attempt to identify the source of bleeding Assist the provider with repair procedures use ice packs to treat small hematomas administer pain medication Encourage sitz baths and frequent perineal hygiene Newborn Post dates infant with asphyxia- interventions for book 673. Infants who experienced severe asphyxia at birth should receive intravenous fluids so they do not become exhausted from sucking or until necrotizing enterocolitis has been ruled out which can result when there is a temporary reduction of oxygen to the bowel Care of newborn under phototherapy- nursing interventions Maintain eye mask over the newborn eyes for protection of cornea retina keep a newborn undressed. For a male newborn, a surgical mask should be placed like a bikini over the genitalia to prevent possible testicular damage from heat and light waves. Be sure to remove the metal strip from the mask to prevent burning Avoid applying lotions or ointments to the skin because ther absorb heat and can cause burns. Remove the newborn from phototherapy every 4 hours, and mask the newborns eyes,checking for inflammation or injury. Reposition the newborn every 2 hours to expose all of the body surface to the phototherapy lights and prevent pressure sores Check the lamp energy with a photometer per facility protocol Turn off the phototherapy lights before drawing blood for testing. Observe the newborn for effects of phototherapy Bronze discoloration: not a serious complication. Infant of diabetic mother (IDM)- priority care Should be tested fo low blood sugar( hypoglycemia). Even if asymptomatic and feeding soon after birth. AN INFANT OF A WOMAN WHO HAS DIABETES MELLITUS Infants of women who have diabetes mellitus whose illness was poorly controlled during pregnancy are typically longer and weigh more than other babies (macrosomia). The baby also has a greater chance of having a congenital anomaly such as a cardiac anomaly because hyperglycemia is teratogenic to a rapidly growing fetus. Most such babies have a cushingoid (i.e., fat and puffy) appearance. They tend to be lethargic or limp in the first days of life as a result of hyperglycemia. The macrosomia results from overstimulation of pituitary growth hormone and extra fat deposits created by high levels of insulin during pregnancy. This infant’s large size is deceptive, however, because, like all LGA babies, they are often immature. RDS occurs at a higher rate than usual in these infants because they may be born preterm or, if born at term, lecithin pathways may not be mature. High fetal insulin secretion during pregnancy to counteract the hyperglycemia can interfere with cortisol release. This could block the formation of lecithin and further prevent lung maturity (Murphy, Janzen, Strehlow, et al., 2013). A term frequently used for these infants is “fragile giant.” An infant of a woman with diabetes loses a greater proportion of weight in the first few days of life than does the average newborn because of the loss of extra fluid accumulated. Observe such an infant closely to be certain this weight loss actually represents a loss of extra fluid and that dehydration is not occurring. Complications A macrosomic infant has a greater chance of birth injury, especially shoulder and neck injury. A cesarean birth may be necessary to avoid cephalopelvic disproportion. Immediately after birth, the infant tends to be hyperglycemic because the mother was at least slightly hyperglycemic during pregnancy and excess glucose transfused across the placenta. During pregnancy, the fetal pancreas responded to this high glucose level with islet cell hypertrophy, resulting in matching high insulin levels. After birth, as an infant’s glucose level begins to fall because the mother’s circulation is no longer supplying glucose, the overproduction of insulin will cause the development of severe hypoglycemia. Hyperbilirubinemia also may occur in these infants because, if immature, they cannot effectively clear bilirubin from their system. Hypocalcemia also frequently develops because parathyroid hormone levels are lower in these infants due to hypomagnesemia from excessive renal losses of magnesium. Although infants of women with diabetes are usually LGA, an infant born to a woman with extensive blood vessel involvement may be SGA because of poor placental perfusion. The problems of hypoglycemia, hypocalcemia, and hyperbilirubinemia remain the same. Therapeutic Management In a newborn, hypoglycemia is defined as a serum glucose level of less than 45 mg/dl. To avoid a serum glucose level from falling this low, infants of women with diabetes need to be fed early; if they are unable to suck, a continuous infusion of glucose can be prescribed. It is important the infant not be given only a bolus of glucose; otherwise, rebound hypoglycemia (accentuating the problem) can occur. Some infants of women with diabetes have a smaller than usual left colon, apparently another effect of intrauterine hyperglycemia, which can limit the amount of oral feedings they can take in their first days of life. Signs of an inadequate colon include vomiting or abdominal distention after the first few feedings. Careful monitoring for any vomiting and normal bowel movements can help identify this condition. Heat loss in newborn- evaporation, radiation, convection, conduction ati 172, book429 Conduction; loss of body heat resulting from direct contact with a cooler surface. Preheat a radiant warmer, warm a stethoscope and other instruments, and pad scale before weighing the newborn. The newborn should be placed directly on the parents chest and converted with a warm blanket. Convention: flow of heat from he body surface to cooler environmental air. Place the bassinet out of the direct line of a fan or air conditioning vent, swaddle a newborn in a blanket, and keep the head covered. Any procedure done with a newborn uncovered should be performed under a radiant heat Source. Keep ambient temperature of the nursery or clients room at 22 to 26 degrees Celsius (72 to 78 degrees F) Evaporation loss of heat a surface liquid converted to Vapor. gently rub the newborn drive with a warm sterile blanket adhering to standard precautions immediately after delivery. Is thermoregulation is unstable postpone the initial back until the newborn skin temperature is 36.5 degrees C. When bathing expose only one body part at a time washing and drying thoroughly Radiation: loss of heat from the body surface to a cooler solid surface that is close to, but not in direct contact keep a newborn and examine tables away from Windows and air conditioners Newborn assessment- normal head, caput succedaneum, cephalohematoma Caput succedaneum is a swelling of the scalp in a newborn that usually disappears within 3 to 5 days . ati page 104 Cephalohematoma: a collection of blood under the periosteum of the skull bone caused by pressure at Birth. Book p.441,445 Interventions for feeding a term infant pg book 454 “On demand” schedule (are fed when they are hungry) . need to be fed as often as every 1.5 to 2 hours in the first few days ad weekd of life.