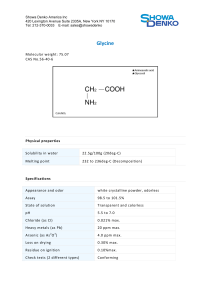
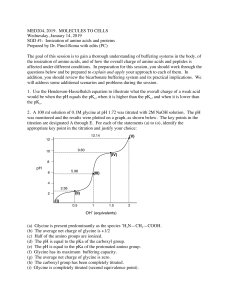
Protein metabolism By Dr. Sahar A. Helmy Lecturer of Biochemistry Special pathways for individual amino acids 1- Glycine amino acid Characters: It is glucogenic, non-essential Why glycine is nonessential AA? because it can be formed from threonine and from serine: Threonine glycine + acetaldehyde (Irreversible) Serine glycine + formaldehyde (reversible) Why glycine is glucogenic AA? because it can form pyruvate. + Formaldehyde A. Anabolic reactions of Glycine A- Glycine enters in the formation of: creatine Bile salts purines Glycine porphyrins glutathione serine 1.Porphyrins (Hb & Mb): Glycine + succinyl CoA -amino--ketoadipic acid Pyridoxal. P porphyrins 2.Bile Salts: Glycine + cholic acid Glycocholic acid NaCl or KCl Na or K glycocholate (bile salt) 3. Purines: Carbons 4 and 5 and nitrogen 7 are derived from glycine 4-Serine synthesis 5. Creatine and creatine phosphate of muscles: • Creatine synthesis requires glycine, arginine and methionine. • Creatine phosphate is the main store of energy in muscle used for muscle contraction. • Creatinine is produced either from dephosphorylation of creatine phosphate or from dehydration of creatine itself. • Creatinine is excreted in urine. -H2O 6. Glutathione(G-SH): • It is a tripeptide formed from 3 amino acids (-glutamylcysleinyl-glycine). It is formed in the liver by the help of ATP. • Glutathione can exist in 2 forms: A- Reduced form containing free –SH group (G-SH) B- Oxidised form (G-S-S-G) containing disulfide linkage. • Glutathione (G-SH) has the following functions: 1. It protects haemoglobin against oxidation by hydrogen peroxide: • Keep iron of Hb in Fe++ state. • Keep globin in native state. 2. It protects the red blood cells from haemolysis by various agents. 3. It maintains the reduced (–SH) group, which is the active and essential group of many enzymes. 4. It inactivates insulin in the liver by reductive cleaving of the 2 disulfide linkages of insulin into 2 separate polypeptide chains. Insulin glutathione transhydrogenase Insulin 2 separate polypeptide chains (inactive insulin) 4GSH 2GS-SG 5. It protects the -cells of pancreas from the degenerative action of alloxan or dehydroascorbic acid. This protective action is due to the (–SH) group of glutathione which reduces alloxan to inactive substance and reduces dehydroascorbic acid to ascorbic acid. 6. It is a cofactor of maleylacetoacetate isomerase enzyme in the synthesis of acetoacetate from tyrosine or phenylalanine. Maleylacetoacetate isomerase Maleylacetoacetate G–SH Fumaryl acetoacetate 7. Glutathione in the oxidized form (G–S–S–G) acts as a hydrogen carrier and so it is considered as a tissue respiratory enzyme. G–S–S–G +2H 2G–SH. -2H 8.Glutathione plays an important role in -glutamyl cycle (absorption of a.a). Mechanism of antioxidant function of GSH • Glutathione is maintained in the reduced form (G–SH) in red blood cells by the help of a reductase enzyme needing NADPH+ H+ as a coenzyme. • In red blood cells, this NADPH+H+ is produced in the first reaction of HMP-shunt which needs the presence of glucose -6- phosphate dehydrogenase enzyme : Glucose6-phosphate Glucose-6-phosphate Glucose-6-phosphate Dehydrogenase (G-6-PD) NADP+ 2GSH 6-Phospogluconate NADPH+H+ GS-SG Favism and primaquine sensitivity Congenital deficiency of glucose-6-phosphate dehydrogenase enzyme, NADPH+H+ is not produced and as a result glutathione (G-SH) becomes deficient in red blood cells resulting in increased tendency to haemolysis especially after the intake of some foods e.g. Fava beans, or some drugs e.g. sulfa drugs, anti-malaria drugs. Glycineis in detoxification B.B.Glycine used in detoxication: Being conjugated with benzoic acid giving hippuric acid which is excreted in urine. Glycine + Benzoic acid (Toxic) Toxic) urine Hippuric acid (Less C. Catabolic reactions of glycine • Glycine by oxidative deamination or by transamination gives glyoxylic acid which by oxidative decarboxylation gives formic acid. Primary hyperoxaluria The overproduction of a substance called oxalate (also called oxalic acid). In the kidneys, the excess oxalate combines with calcium to form calcium oxalate, a hard compound that is the main component of kidney stones. Deposits of calcium oxalate can lead to kidney damage, kidney failure, and injury to other organs. Cause of primary hyperoxaluria: • Genetic defect leads to loss of specific enzyme and the normal metabolic pathway is blocked. • Failure of oxidation of glyoxylic acid to formic acid will lead to oxidation of glyoxylic acid to oxalic acid which is excreted in great amounts in urine. • Congenital absence of glycine transaminase is the main cause of such disease. (2) Alanine • It is non-essential glucogenic amino acid because it can be formed in the body from pyruvic acid by transamination with any amino acid e.g. glutamate. L-glutamic acid+ pyruvic acid Pyr.P GPT (ALT) L-alanine+α-ketoglutaric acid Protein metabolism By Dr. Sahar A. Helmy Lecturer of Biochemistry (3) Serine • It is a non-essential amino acid formed from glycine and formaldehyde. • It is glucogenic amino acid giving pyruvic acid and ammonia by non-oxidative deamination. + Formaldehyde Functions of serine Serine Cysteine phospholipids phosphoproteins 1- formation of Phospholipids: Sphigomyelins Palmityl CoA aldehyde Cephalins Serine Co2 Ethanolamine Cephalins 3(-CH3) Choline Lecithins 2- Formation of phosphoproteins The phosphate group is usually attached to (–OH) group of serine or threonine present in phosphoproteins as caseinogen. 3- Cysteine formation Cysteine is formed from methionine and serine as follows. Cystathioninase (4) Threonine • It is essential, glucogenic amino acid. It can give glycine and acetaldehyde in the body + Formaldehyde (5) Tryptophan • • It is essential and both glucogenic and ketogenic amino acid. It has 3 main pathways: 1- Nicotinic acid pathway. 2- Serotonin and Melatonin pathway. 3- Indole and skatole pathway (putrefaction). 1)Nicotinic acid pathway: This is the main and most important pathway of tryptophan. (NAD+) (NADP+) (Nicotinamide ribose diphosphate) • Pyridoxal phosphate is necessary as a coenzyme. So vitamin B6 necessary for synthesis of nicotinic acid. • Nicotinamide formed enters in the formation of coenzymes I, II and III. • Tryptophan is both: glucogenic because it produces alanine that can form pyruvate. ketogenic because it produces acetoacetic acid. 2)Serotonin and Melatonin Pathway: •Serotonin is a substance stored in platelets, gastrointestinal mucosa and CNS. •It is formed from tryptophan as follows: (Tryptophan hydroxylase) (Serotonin) (urine) • Tryptophan metabolism is greatly deviated to serotonin pathway in malignant tumors. Function of serotonin 1- It mediates gut movement. 2- a mood regulator in vertebrate animals • Abnormal serotonin levels are also associated with problems such as suicidal tendency, obsessive compulsive disorder, and anxiety. • Tryptophan can give melatonin which is secreted by the pineal body and peripheral nerves. N-acetylation N-Acetyl transferase Serotonin N-acetylserotonin HIOMT Melatonin • HIOMT: Hydroxyindole O-methyltransferase. • Melatonin is a hormone used as a sleep aid and in the treatment of sleep disorders. 3- Indole and skatole pathway: • These are produced normally by the action of bacteria in large intestine on tryptophan. It is an example of putrefaction. • Indole and skatole give the foul odour of stool. • In case of constipation, Indole is reabsorbed by intestinal mucosa to be oxidized into indoxyl which reaches liver, conjugated with sulfuric acid and excreted in urine as indoxyl potassium sulfate (indican). So indican is one of the abnormal constituents of urine. -CO2