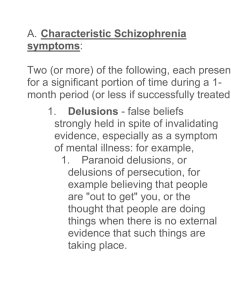
Psychiatry Lectures Lecture 1: Introduction to Psychiatry What Is Psychiatry? Psychiatry is the branch of medicine focused on the diagnosis, treatment and prevention of mental, emotional and behavioral disorders. A psychiatrist is a medical doctor who specializes in mental health, including substance use disorders. Psychiatrists are qualified to assess both the mental and physical aspects of psychological problems. People seek psychiatric help for many reasons. The problems can be sudden, such as a panic attack, frightening hallucinations, thoughts of suicide, or hearing "voices." Or they may be more long-term, such as feelings of sadness, hopelessness, or anxiousness that never seem to lift or problems functioning, causing everyday life to feel distorted or out of control. Psychiatrists use a variety of treatments – including various forms of psychotherapy, medications, psychosocial interventions and other treatments (such as electroconvulsive therapy or ECT), depending on the needs of each patient. Terminology Neurosis: Former name of a class of mental disorders characterized by anxiety and avoidance behavior, with symptoms distressing to the patient, intact reality testing, no violation of social norms, and no apparent organic etiology. Psychosis: Impaired reality testing (means that patient is unable to distinguish personal subjective experience from the reality of the external world). They experience hallucinations and/or delusions. Psychosis is a one of the criteria to diagnose schizophrenia and related disorder, but it also can occur in mood disorders, substance use disorders and cognitive disorders (delirium and dementia). Insight: The patient’s awareness and understanding of the origins and meaning of his attitudes, feelings, and behavior and of his disturbing symptoms; self-understanding. It can be lost, partial, or intact. Disorders of perception: illusions and hallucinations. Illusions are defined as misperception of real external sensory stimuli. If occur in delirium (=confusion). E.g.: elderly patient, at night, in the intensive care unit sees the wires attached to his chest to take ECG as snakes. The treatment is to reassure the patient and open the lights at night. Illusion can occur in normal people. Hallucinations are false sensory perception not associated with real external stimulus. Hallucinations could occur in schizophrenia, substance use disorders bipolar disorder, and major depressive disorder with psychotic feature in which they are usually auditory hallucinations. Page 1 Visual hallucinations occurs more in organic cases (brain tumor, wilson's disease, Lewy-Body dementia, etc...). Olfactory hallucinations occur in partial complex epilepsy (e.g.: smelling burning and تذوقيّة ّ rubber in temporal lobe epilepsy (TLE)). Hallucinations can be gustatory and somatic. An example of somatic hallucinations is the feeling that there are worms or bugs on the skin of the patient (occur in cocaine withdrawal and called cocaine bug). Disorders of thought: it can be disorder of content, or form, or stream of thought. Disorders of thought Content: these include delusions, obsessions, and overvalued ideas. We can add here also suicidal thoughts and homicidal thoughts. Delusions are false beliefs, based on incorrect conclusion about external reality, not consistent with patient's culture. Delusions do not occur in normal people. There are different types of delusions for different types of mental illnesses: bizzare delusion: an impossible strange belief(e.g.: invaders from the space have implanted electrodes into my brain). This occurs usually in schizophrenia. Paranoid delusions: includes persecutory delusions, delusions of reference , and grandiose delusions. In persecutory delusions the patient believes that there is a plan to hurt him (e.g. poisons put in food, police try to kill him etc..). In delusions of reference the patients believe that people are watching or following him, or refer to him (e.g. people in the TV or radio are talking about the patient). In grandiose delusions the patient exaggerates his importance, power, or identity. Paranoid delusions usually occur in schizophrenia (paranoid subtype), or delusional disorder, but also can occur in other disorders like grandiose delusions in bipolar disorder (in manic episodes). Grandiose delusion in a manic episode is mood-congruent . Nihilistic delusion: false feeling that self, others, or the world is nonexistent or coming to an end. Nihilistic delusion in major depressive disorder with psychot ic features is mood-congruent. Delusion of infidelity (delusional jealousy): false belief derived from pathological jealousy about a person's partner being unfaithful. Occur in delusional disorder and schizophrenia. This delusion is dangerous and lead sometimes to violence. Geographical separation is sometimes advised. Erotomania: delusional belief, more common in women than in men, that someone is deeply in love with them. Occur in delusional disorder, schizophrenia, and bipolar disorder. Delusion of guilt: false feeling of guilt. This is a mood-congruent delusion when occur in major depressive disorder with psychotic features. • Delusions of control: false feeling that a person's will, thought, or feelings are being controlled by external forces and include: thought withdrawal, thought insertion, and thought broadcasting. Occur usually in schizophrenia. Page 2 There are other types of delusions. Under the term "Thought Content" we can also put: suicidal ideas, and homicidal ideas, as these two ideas are dangerous and we must ask about them when the patient seems to have risk of them: e.g. risk of suicide in depression, and risk of homicide in morbid jealousy. Disorder of form of thought (also called Formal Thought Disorders) appears in the patient's speech and the most important type is called: loosening of association, in which there is a lack of meaningful connection between sequential ideas. Disorders of stream or speed of thoughts include mainly what is called as: "Pressure of thought" which is the subjective experience of one's thoughts occurring rapidly, each thought being associated with a wider range of consequent ideas than normal and with inability to remain on one idea for any length of time. Usually Occur in manic illness. And the speech is called "pressured (or pressure of speech)". Mood: sustained emotional state reported by the patient (subjective ). Affect: emotional state reported by observer (doctor ). Disorders of mood: it can be normal or depressed or euphoric. Depressed in depression and euphoric (or called elated) in mania. Sometimes there is what is called as restricted, or blunted affect, which means a reduction in the intensity of emotions and it occurs in schizophrenia and in depression. In severe forms of blunted affect, the affect is called flat "flat affect". The affect is also can be described as appropriate, or inappropriate. Other common signs and symptoms: Psychomotor retardation: this is characterized by slowing of thought and activity. This occurs in depression and is one of the criteria of it. Psychomotor agitation: characterized by a dysphoric restlessness of speech and motor behavior. This is also a criterion of depression. Stereotypies: repeated, purposeless, and sometimes bizarre movements. It occurs in schizophrenia, mental retardation, and in autism. Catatonic symptoms: catatonia is defined as an increase in resting muscle tone to distinguish it from rigidity. One of the catatonic symptoms is posturing which is characterised by taking a posture (sometimes bizarre posture) and maintaining it for minutes. It occurs In schizophrenia and in depression. Another catatonic feature is negativism which is resistance to requests and commands. And this occurs in chronic schizophrenia. Some catatonic patients are totally immobile "stupor" and this occurs in schizophrenia and depression. All catatonic features respond well to electroconvulsive therapy (ECT). History and Metal Status Examination (MSE): History: 1. Name, age, and marital status. Current occupation. Route of referral. Page 3 2. Chief complaints 3. History of presenting complaints 4. Past psychiatric and medical history 5. Drug history 6. Family history 7. Personal history: Birth, Childhood, School, Work, Marriage. 8. Forensic Hx. 9. Social background information 10. Premorbid personality Mental Status Examination (MSE): 1. Appearance: Style of dress. Level of cleanliness. General physical condition. 2. Behaviour: Appropriateness of behaviour. Level of motor activity. Apparent level of anxiety. Eye contact. Rapport. Abnormal movement or posture. Episodes of aggression. 3. Speech: Volume, rate, and tone. Quantity and fluency. Abnormal associations, clang and punning. Flight of ideas. 4. Mood: Subjective and objective assessment of mood. 5. Perception: Hallucinations or illusions. 6. Thought Form: formal thought disorder. 7. Thought Content: delusions, obsessions, suicidal and homicidal intents. 8. Cognition: Orientation. Attention and Concentration. Short-term and long term memory. 9. Insight: Does the patient feel his experiences are as the result of illness? Will he accept medical advice and treatment? The End Page 4