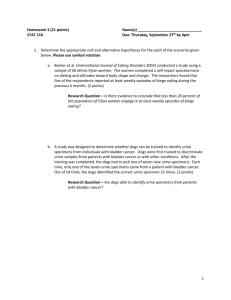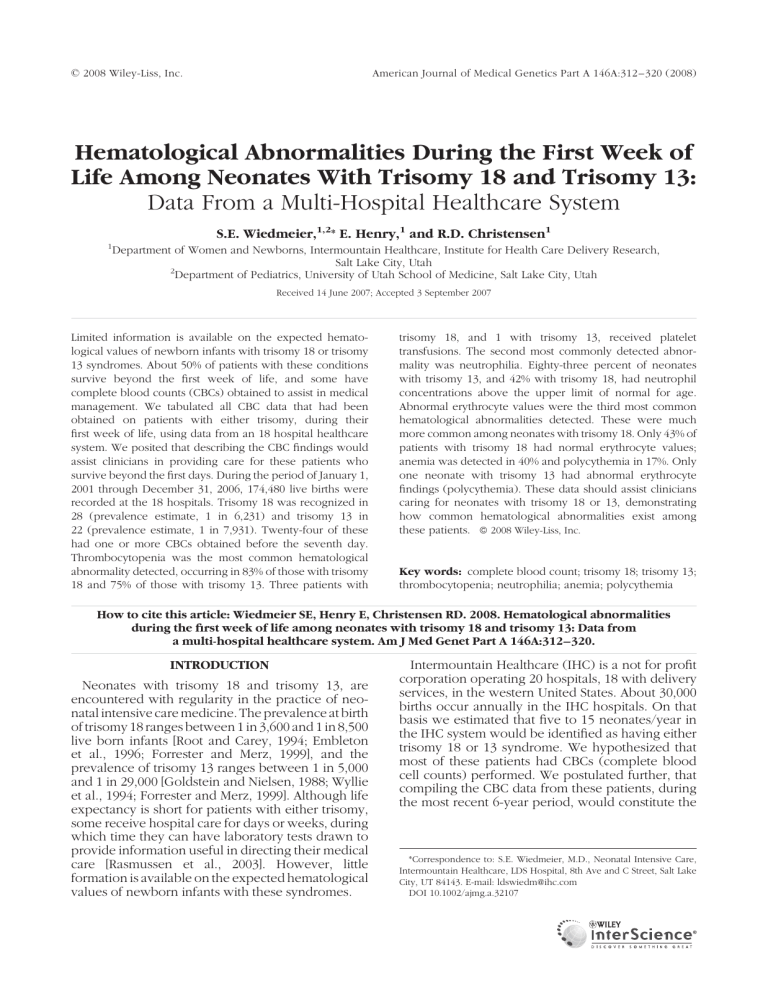
ß 2008 Wiley-Liss, Inc. American Journal of Medical Genetics Part A 146A:312 – 320 (2008) Hematological Abnormalities During the First Week of Life Among Neonates With Trisomy 18 and Trisomy 13: Data From a Multi-Hospital Healthcare System S.E. Wiedmeier,1,2* E. Henry,1 and R.D. Christensen1 1 Department of Women and Newborns, Intermountain Healthcare, Institute for Health Care Delivery Research, Salt Lake City, Utah 2 Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, Utah Received 14 June 2007; Accepted 3 September 2007 Limited information is available on the expected hematological values of newborn infants with trisomy 18 or trisomy 13 syndromes. About 50% of patients with these conditions survive beyond the first week of life, and some have complete blood counts (CBCs) obtained to assist in medical management. We tabulated all CBC data that had been obtained on patients with either trisomy, during their first week of life, using data from an 18 hospital healthcare system. We posited that describing the CBC findings would assist clinicians in providing care for these patients who survive beyond the first days. During the period of January 1, 2001 through December 31, 2006, 174,480 live births were recorded at the 18 hospitals. Trisomy 18 was recognized in 28 (prevalence estimate, 1 in 6,231) and trisomy 13 in 22 (prevalence estimate, 1 in 7,931). Twenty-four of these had one or more CBCs obtained before the seventh day. Thrombocytopenia was the most common hematological abnormality detected, occurring in 83% of those with trisomy 18 and 75% of those with trisomy 13. Three patients with trisomy 18, and 1 with trisomy 13, received platelet transfusions. The second most commonly detected abnormality was neutrophilia. Eighty-three percent of neonates with trisomy 13, and 42% with trisomy 18, had neutrophil concentrations above the upper limit of normal for age. Abnormal erythrocyte values were the third most common hematological abnormalities detected. These were much more common among neonates with trisomy 18. Only 43% of patients with trisomy 18 had normal erythrocyte values; anemia was detected in 40% and polycythemia in 17%. Only one neonate with trisomy 13 had abnormal erythrocyte findings (polycythemia). These data should assist clinicians caring for neonates with trisomy 18 or 13, demonstrating how common hematological abnormalities exist among these patients. ß 2008 Wiley-Liss, Inc. Key words: complete blood count; trisomy 18; trisomy 13; thrombocytopenia; neutrophilia; anemia; polycythemia How to cite this article: Wiedmeier SE, Henry E, Christensen RD. 2008. Hematological abnormalities during the first week of life among neonates with trisomy 18 and trisomy 13: Data from a multi-hospital healthcare system. Am J Med Genet Part A 146A:312–320. INTRODUCTION Neonates with trisomy 18 and trisomy 13, are encountered with regularity in the practice of neonatal intensive care medicine. The prevalence at birth of trisomy 18 ranges between 1 in 3,600 and 1 in 8,500 live born infants [Root and Carey, 1994; Embleton et al., 1996; Forrester and Merz, 1999], and the prevalence of trisomy 13 ranges between 1 in 5,000 and 1 in 29,000 [Goldstein and Nielsen, 1988; Wyllie et al., 1994; Forrester and Merz, 1999]. Although life expectancy is short for patients with either trisomy, some receive hospital care for days or weeks, during which time they can have laboratory tests drawn to provide information useful in directing their medical care [Rasmussen et al., 2003]. However, little formation is available on the expected hematological values of newborn infants with these syndromes. Intermountain Healthcare (IHC) is a not for profit corporation operating 20 hospitals, 18 with delivery services, in the western United States. About 30,000 births occur annually in the IHC hospitals. On that basis we estimated that five to 15 neonates/year in the IHC system would be identified as having either trisomy 18 or 13 syndrome. We hypothesized that most of these patients had CBCs (complete blood cell counts) performed. We postulated further, that compiling the CBC data from these patients, during the most recent 6-year period, would constitute the *Correspondence to: S.E. Wiedmeier, M.D., Neonatal Intensive Care, Intermountain Healthcare, LDS Hospital, 8th Ave and C Street, Salt Lake City, UT 84143. E-mail: ldswiedm@ihc.com DOI 10.1002/ajmg.a.32107 American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a 313 HEMATOLOGICAL ABNORMALITIES IN NEONATES WITH TRISOMY 18 AND TRISOMY 13 largest series to date dealing with these issues, and that such data would be of value to clinicians caring for neonates with these conditions. managed and accessed by authorized data analysts. The Intermountain Healthcare Institutional Review Board approved this study. METHODS RESULTS Data were collected as a de-identified limited data set from archived IHC electronic records of all newborn infants where the diagnosis of either trisomy 18 or trisomy 13 was made either prenatally or during the first month after birth. The newborn services provided within the 18 IHC hospitals with delivery services include eight Level 1, six Level 2, and four Level 3 nurseries. The information collected for analysis was limited to demographics and the data contained in the CBCs. Demographic characteristic included gestational age, birth weight, gender, race, Apgar score at 5 min, level of neonatal care available at delivery hospital, in-hospital mortality, length of initial hospital stay for all patients, and discharge disposition. Data were collected only for CBCs obtained <7 days after birth, and only on neonates with a date of birth from January 1, 2001 through December 31, 2006, who within the first month of life had a karyotype analysis confirming the diagnosis of either trisomy 18 or 13. The program used for data collection is a modified subsystem of ‘‘clinical workstation.’’ The 3M Company (Minneapolis, MN) approved the structure and definitions of all data points for use within the program. The data were collected from the electronic medical record, case mix, and laboratory systems. Trained and designated clinical personnel enter additional data. Data are Between January 1, 2001 and December 31, 2006, 174,480 live births were recorded at the 18 IHC hospitals. Twenty-eight of these neonates were identified as having trisomy 18 (prevalence at birth estimate, 1/6231) and 22 were identified as having trisomy 13 (prevalence at birth estimate, 1/7,931). Twenty-four of these 50 (12 with trisomy 18, and 12 with trisomy 13) had one or more CBCs obtained during the first 144 hr after birth and recorded in the IHC electronic database. Karyotype analysis of these 24 included three with an unbalanced Robertsonian translocation trisomy 13, and 1 with mosaic trisomy 13. The chromosomal abnormality of the remaining 20 was not specified in the electronic records, although all were stated to have either ‘‘trisomy 18’’ or ‘‘trisomy 13.’’ Demographic features of the 50 neonates are listed in Table I. The patients with trisomy 18 or 13 who had a CBC obtained during the first week of life and the group of patients with trisomy 18 who did not, were of similar gestational age, term or near-term, and the majority were small for gestational age (SGA). The group of patients with trisomy 13 who did not have a CBC obtained during the first week were slightly more preterm and a smaller percentage were SGA compared to the patients in the other three groups. The distribution of Apgar scores at 1 min was different for the patient groups. A higher proportion TABLE I. Demographic Features and Outcomes of 50 Neonates With Trisomy 18 or Trisomy 13 Neonates with trisomy 18 who had one or more CBCs during the first week (n ¼ 12) Gestational age (weeks) SD Birth weight (g) mean SD Percent who were SGAa Gender (% male) Born in hospital with Level III NICU Apgar score of <4 at 5 min Race White nonhispanic Hispanic Other Outcomes Died in the hospital—never discharged home Died in the hospital within 24 hr of birth Discharged home from the hospital Transferred to a non-IHC hospital Discharged to a long-term care facility Mean length of the initial hospital stay—hours Neonates with trisomy Neonates with trisomy 13 Neonates with 18 who had no CBCs who had one or more trisomy 13 who during the first CBCs during the had no CBCs during week (n ¼ 16) first week (n ¼ 12) the first week (n ¼ 10) 36.1 3.7 2,007 66 83% (10/12) 25% 50% (6/12) 8% (1/12) 36.8 2.4 1,624 518 100% (16/16) 44% 69% (11/16) 38% (6/16) 37.3 2.1 2,627 704 83% (10/12) 58% 67% (8/12) 8% (1/12) 32.4 6.3 1,752 1,040 40% (4/10) 50% 90% (9/10) 70% (7/10)* 8 2 2 16 0 0 8 3 1 9 0 1 42% (5/12) 81% (13/16)* 50% (6/12) 100% (10/10)* 8% (1/12) 50% (6/12) 8% (1/12) 0% 43.5 (median 11.0) 75% (12/16)* 19% (3/16) 0% 0% 20.8 (median 4.5) 8% (1/12) 42% (5/12) 0% 8% (1/12) 114.5 (median 7.5) 100% (10/10)* 0%* 0% 0% 1.6 (Median 1.0)* a SGA, small for gestational age (weight <10th centile). *P < 0.05 versus ‘‘had CBC’’ group. American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a 314 WIEDMEIER ET AL. of patients with either trisomy who did not have a CBC during the first week had an Apgar score of less than 4 recorded at 5 min of age compared to the group of patients who did have a CBC. In addition, when compared to patients who did have a CBC, a significantly higher proportion of neonates with trisomy 18 or 13 who did not have a CBC died during their initial hospitalization, most within 24 hr of delivery. Fifty percent (12/24) of the patients who had a CBC survived the initial neonatal period and were ultimately discharged from the hospital. In contrast only 12% (3/26) of the patients who did not have a CBC survived long enough to eventually be discharged (Table I). The number of CBCs obtained from each of the 50 neonates, during the first week after birth, ranged from 0 to 9 (median, 2). Blood neutrophil concentrations of the 12 with trisomy 18 and the 12 with trisomy 13 are shown in Figure 1. Using the criteria of Manroe et al. [1979], 26% of the blood neutrophil counts of those with trisomy 18 were in the neutrophilic range, 54% were in the normal range, and 20% were in the neutropenic range. Blood neutrophil counts of those with trisomy 13 included 64% in the neutrophilic range, 33% in the normal range, and 3% in the neutropenic range. Platelet counts are shown in Figure 2. Fifty-two platelet counts were obtained on the 12 neonates with trisomy 18, with values ranging from 21,000 to 240,000/ml. Seventy-six percent of the counts were in the thrombocytopenic range (<150,000/ml). Fortyfive percent were in the moderately severe thrombocytopenic range (50,000–100,000/ml), and 6% were <50,000/ml. Thirty-seven platelet counts were obtained on the 12 neonates with trisomy 13, with values ranging from 45,000 to 235,000/ml. Fifty-one percent of the counts were in the thrombocytopenic range (<150,000/ml). Twenty-two percent were in the moderately severe thrombocytopenic range, and 3% were <50,000/ml. The mean platelet volume for patients with Trisomy 18 was 8.95 fL with 30% of values above 10 fL and 14% of values below 7.5 fL. The mean platelet volume for patients with Trisomy 13 was 9.2 fL with 15% of values above 10 fL and 1.5% of values below 7.5 fL. Three patients with trisomy 18 and 1 patient with trisomy 13 received one or more platelet transfusions. Hematocrit and hemoglobin values are shown in Figure 3 (panels A and B). Polycythemia (hematocrit >65% or hemoglobin >22g/dl) was identified in 1% of the CBCs of neonates with trisomy 18. Seventy-five percent of the hematocrit and hemoglobin values of neonates with trisomy 18 were normal (40–65% and 13–22 g/dl), while a hematocrit <40% or hemoglobin <13 g/dl was identified in 14%. Polycythemia was identified in 3% of the CBCs of neonates with trisomy 13. One underwent a reduction transfusion. Ninety-five percent of the hematocrit and hemoglobin values of neonates with trisomy 13 were normal, and no low values were identified. Nucleated erythrocyte counts (NRBC) ranged from zero to 584/ml for neonates with trisomy 18 and zero to 402/ml for those with trisomy 13 (Fig. 3, panel C). By three days (60 hr) all NRBC concentrations were <100/ml. As shown in Figure 3 (panel D), the mean corpuscular volume for neonates with trisomy 18 (109 8 fl) and with trisomy 13 (109 þ 6) were in the normal range (108 8 fl), [Christensen, 1999]. DISCUSSION The trisomy 18 and 13 syndromes are two of the most common multiple congenital anomaly syndromes in live born infants, with a combined prevalence of approximately 1 in 4,000 births. Although numerous reports describe the structural defects associated with both of these conditions, there is limited information on the prevalence of their hematological abnormalities during the neonatal period. The current study was undertaken to evaluate the CBC findings of neonates with trisomy 18 or 13 in the first week of life, using electronically archived data from an 18 hospital healthcare system, in a manner similar to our recent study of the hematological abnormalities of neonates with Down syndrome [Henry et al., 2007]. Thrombocytopenia was the most common hematological abnormality identified, having been detected in over 75% of cases (Table II). Smith’s latest catalog reports that thrombocytopenia occurs in TABLE II. Hematological Problems Recognized in the First 7 Days After Birth, Among Neonates With Trisomy 18 or Trisomy 13 Hematological problem Neutrophiliaa Thrombocytopeniab Polycythemiac Anemia Neutropenia a Trisomy 18 proportion with this problem recognized (n ¼ 12) Trisomy 13 proportion with this problem recognized (n ¼ 12) P-value (5) 42% (10) 83% (2) 17% (5) 42% (3) 25% (10) 83% (9) 75% (1) 8% (0) 0% (1) 8% 0.040 0.500 0.500 0.019 0.295 Blood neutrophil concentration > upper limit of normal for postnatal age [Manroe et al., 1979]. Platelet concentration <150,000/ml. Hemoglobin >22 g/dl or hematocrit >65%. b c American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a HEMATOLOGICAL ABNORMALITIES IN NEONATES WITH TRISOMY 18 AND TRISOMY 13 315 FIG. 1. Blood concentration of neutrophils during the first 144 hr after birth among 12 neonates with trisomy 18 (squares) and 12 neonates with trisomy 13 (circles). Heavy lines are drawn to estimate the upper and lower limit of anticipated values for neonates (normal values from Manroe et al. [1979]). FIG. 2. Blood concentration of platelets, and mean platelet volume, during the first 144 hr after birth among 12 neonates with trisomy 18 (squares) and 12 neonates with trisomy 13 (circles). Panel A: Platelet concentration per microliter of blood. Heavy lines are drawn at 150,000/ml and 450,000/ml, as estimates of the upper and lower limits of normal for platelet concentrations of neonates. Panel B: Mean platelet volume (fL). American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a 316 WIEDMEIER ET AL. FIG. 2. (Continued ) FIG. 3. Hematocrit, hemoglobin concentration, nucleated erythrocyte concentration, and mean corpuscular volume, during the first 144 hr after birth among 12 neonates with trisomy 18 (squares) and 12 neonates with trisomy 13 (circles).Panel A: Hematocrit (%). Heavy lines are drawn at 40% and at 65%, as estimates of the lower and upper limit of normal values in neonates [Christensen, 1999]. Panel B: Hemoglobin (g/dl). Heavy lines are drawn at 13 and 22 g/dl, as estimates of the lower and upper limit of normal values in neonates [Christensen, 1999]. Panel C: Nucleated erythrocytes (cells/ml). Panel D: Mean corpuscular volume (fL). Heavy lines are drawn at 100 and 116 fL, as estimates of two standard deviations from the normal mean value of 108 fL among normal neonates [Christensen, 1999]. American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a HEMATOLOGICAL ABNORMALITIES IN NEONATES WITH TRISOMY 18 AND TRISOMY 13 FIG. 3. (Continued ) 317 American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a 318 WIEDMEIER ET AL. FIG. 3. (Continued ) <10% of patients with trisomy 18 and in <50% of patients with trisomy 13 [Jones, 2006]. Consistent with our data, Kosho et al. [2006] reported thrombocytopenia in 83% (20/24) of patients with trisomy 18. In addition, Hohlfeld et al. [1994] reported that 87% of fetuses with trisomy 18, and 54% of fetuses with trisomy 13, had platelet counts <150,000/ml. While collectively these data indicate that thrombocytopenia is common in this group of neonates, we know of no studies that delineate the responsible mechanism. Thrombocytopenia is commonly seen in preterm SGA infants, however it is relatively less common in term SGA infants [Sola et al., 2000]. In the current study we noted that while 83% of the neonates who had one or more CBCs obtained during the first week after birth were SGA they were all term or near-term at the time they were delivered making it unlikely that their SGA status was the single underlying explanation for their thrombocytopenia. Birth asphyxia also appears to be a significant risk factor for neonatal thrombocytopenia [Sola and Christensen, 1999]. Only two of the 24 patients on whom CBCs were obtained in the current study had an Apgar score of less that four recorded at 5 min of age making it unlikely that hypoxia contributed significantly to the pathogenesis of thrombocytopenia in this group of neonates. Thrombocytopenia also commonly accompanies systemic infections in neonates. The thrombocytopenia accompanying neonatal sepsis is the kinetic result of accelerated platelet destruction, and results in a high MPV from a compensatory release of immature platelets from the marrow [Patrick and Lazarchick, 1990]. Our patients with trisomy 18 and 13 did not have a high MPV, suggesting that the kinetic mechanism in these patients was not infectious. Decreased platelet production as a consequence of reduced megakaryocytes or impaired platelet production from megakaryocytes has been identified as the mechanism responsible for the neonatal thrombocytopenia associated with a variety of syndromes and congenital disorders. While it is tempting to hypothesize a similar cause for the thrombocytopenia noted in neonates with trisomies 18 or 13 much more investigation will be needed to definitively identify the responsible mechanism. Potential approaches might include measuring plasma thrombopoietin concentrations, reticulated platelet counts, and marrow biopsies [Sola-Visner et al., 2007]. The second most common hematological abnormality observed was neutrophilia (Table II). Eighty three percent of neonates with trisomy 13, and 42% of those with trisomy 18, had blood neutrophil concentrations above the upper limits of normal American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a HEMATOLOGICAL ABNORMALITIES IN NEONATES WITH TRISOMY 18 AND TRISOMY 13 [Manroe et al. 1979]. Structural anomalies of neutrophils of patients with trisomy 13 have been reported by several investigator [Huehns et al., 1964; Salama et al., 2004], but we are unaware of previous studies documenting the high prevalance of neutophilia in neonates with trisomy 18 or 13. Normal neutrophil counts were observed in only 33% of those with trisomy 18 and in fewer than 10% of those with trisomy 13, suggesting the possibility of neutrophil dysregulation in these patients. Abnormal erythrocyte values were the third most common hematological abnormalities detected (Table II). These were much more common among neonates with trisomy 18. In fact, only about 40% of those with trisomy 18 had normal erythrocyte values, with anemia present in 40%, polycythemia in 17%, and an abnormally high or low MCV in 40%. Perhaps, similar to their wide range of neutrophil concentrations, this finding suggests dysregulation of erythropoiesis among patients with trisomy 18. In contrast, anemia was not detected in any of the patients with trisomy 13; however one had polycythemia diagnosed, with a hematocrit of 69%, and underwent a reduction transfusion. Werner also reported an increased incidence of polycythemia in patients with trisomy 18 or 13 [Werner, 1995]. We recognize that our study has several shortcomings. For instance, the results are limited by a relatively small sample size, and also by the potential for selection bias, because CBCs were obtained on only about half of the 50 affected neonates. We were unable to definitively determine whether fewer CBCs were obtained if the diagnosis of trisomy had been made prenatally. One would anticipate that the medical care provided to neonates in whom the diagnosis of either trisomy 18 or 13 had been made prenatally would have been influenced by parenteral decisions regarding resuscitation and previously agreed upon therapeutic interventions. We speculate that this was the case as compared to patients who had CBCs, a significantly higher proportion of patients who did not, had Apgar scores of less than 4 at 5 min and died during their initial hospitalization, most within 24 hr. Another shortcoming is that the anatomic site of the blood drawn for testing is not listed in our electronic records, and therefore the results we report surely contain some venous, some capillary, and perhaps some arterial sources. While platelet counts, and determinations of the MPV and MCV, do not vary significantly with the anatomic source, capillary values tend to run somewhat higher than vascular sources when assessing a neonate’s hemoglobin and hematocrit [Christensen, 1999]. Arterial blood tends to have a lower leukocyte count than simultaneously obtained venous or capillary samples [Christensen and Rothstein, 1979]. An additional shortcoming is that we did not determine the mechanistic explanations for the 319 hematological abnormalities found. Erythropoiesis and myelopoiesis are multifaceted dynamic processes regulated by cell–cell and cell–matrix interactions, stimulatory and inhibitory cytokines, and an assortment of transcription factors. Clearly, more extensive studies will be necessary to determine the precise impact of genomically unbalanced changes, such as trisomy 18 or 13, on the developing hematopoietic system. Despite these limitations, our findings illustrate that CBC abnormalities are very common among neonates with trisomy 18 and 13, and if our study is representative, one or more CBCs are obtained on about half of these patients during their first week following birth. Many complex medical and ethical issues arise in the management of neonates with trisomy 18 or 13 [Carey, 2001]. While the neonatal mortality rates for patients with either of these conditions is high, it is important to recognize that a number of these patients will have longer-term survival [Baty et al., 1994; Root and Carey, 1994; Brewer et al., 2002; Rasmussen et al., 2003; Duarte et al., 2004; Kosho et al., 2006]. We maintain that our present report can assist clinicians directing the medical care of neonates with trisomy 18 or 13, by heightening their awareness of the common hematological abnormalities to be anticipated in these neonates. REFERENCES Baty BJ, Blackburn BL, Carey JC. 1994. Natural history of trisomy 18 and trisomy 13: Growth, physical assessment, medical histories, survival, and recurrence risk. Am J Med Genet 49: 175–188. Brewer CM, Holloway SH, Stone DH, Carothers AD, FitzPatrick DR. 2002. Survival in trisomy 13 and trisomy 18 cases ascertained from population based registers. J Med Genet 39:e54. Carey JC. 2001. Trisomy 18 and trisomy 13 syndromes. In: Cassidy SB, Allenson JE, editors. Management of genetic syndromes. 2nd edition. New York: Wiley-Liss. p 417–436. Christensen RD. 1999. Expected hematologic values for term and preterm neonates. In: Christensen RD, editor. Hematologic problems of the neonate. Philadelphia: W.B. Saunders. p 122– 123. Christensen RD, Rothstein G. 1979. Pitfalls in the interpretation of leukocyte counts of newborn infants. Am J Clin Path 72:608– 611. Duarte AC, Menezes AJC, Devens ES, Roth JM, Garcias GL, Martino-Roth MG. 2004. Patau syndrome with a long survival. A case report. Genet Mol Res 3:288–292. Embleton ND, Wyllie JP, Wright MJ, Burn J, Hunter S. 1996. Natural history of trisomy 18. Arch Dis Child 75:38–41. Forrester MB, Merz RD. 1999. Trisomies 13 and 18: Prenatal diagnosis and epidemiologic studies in Hawaii, 1986–199. Genet Test 3:335–340. Goldstein H, Nielsen KG. 1988. Rates and survival of individuals with trisomy 18 and 13. Clin Genet 34:366–372. Henry E, Walker D, Wiedmeier SE, Christensen RD. 2007. Hematological abnormalities during the first week of life among neonates with Down syndrome. Am J Med Genet Part A 143A:42–50. Hohlfeld P, Forestier F, Kaplan C, Tissot J-D, Daffos F. 1994. Fetal thrombocytopenia: A retrospective survey of 5,194 fetal blood samplings. Blood 84:1851–1856. American Journal of Medical Genetics Part A: DOI 10.1002/ajmg.a 320 WIEDMEIER ET AL. Huehns ER, Lutzner M, Hecht F. 1964. Nuclear abnormalities of the neutrophils in D1 (13–15) trisomy syndrome. Lancet 13: 589–590. Jones KL. 2006. Smith’s recognizable patterns of human malformation. 6th edition. Philadelphia: WB Saunders Co. p 13–14 and 18–19. Kosho T, Nakamura T, Kawame H, Baba A, Tamura M, Fukushima Y. 2006. Neonatal management of Trisomy 18: Clinical details of 24 patients receiving intensive treatment. Am J Med Genet Part A 140A:937–944. Manroe BL, Weinberg AG, Rosenfield CR, Browne R. 1979. The neonatal blood count in health and disease. I. Reference values for neutrophilic cells. J Pediatr 95:89–98. Patrick CH, Lazarchick J. 1990. The effect of bacteremia on automated platelet measurements in neonates. Am J Clin Pathol 93:391–394. Rasmussen SA, Wong LYC, Yang Q, May KM, Friedman JM. 2003. Population-based analyses of mortality in trisomy 13 and trisomy 18. Pediatrics 111:777–784. Root S, Carey JC. 1994. Survivial in trisomy 18. Am J Med Genet 49:170–174. Salama ME, Shah V, Lebel RR, VanDyke DL. 2004. Aberrant nuclear projections of neutrophils in trisomy 13. Arch Pathol Lab Med 128:243–244. Sola MC, Christensen RD. 1999. In: Christensen RD, editor. Hematologic problems of the neonate. Philadelphia: W. B. Saunders. p 281–291. Sola MC, Del Vecchio A, Rimsza LM. 2000. Evaluation and treatment of thrombocytopenia in the neonatal intensive care unit. Clin Perinatol 27:655–660. Sola-Visner MC, Christensen RD, Hutson AD, Rimsza LM. 2007. Megakaryocyte size and concentration in the bone marrow of thrombocytopenic and nonthrombocytopenic neonates. Pediatr Res 61:479–484. Werner EJ. 1995. Neonatal polycythemia and hyperviscosity. Clin Perinatol 22:693–710. Wyllie JP, Wright MJ, Burn J, Hunter S. 1994. Natural history of trisomy 13. Arch Dis Child 71:343–345.