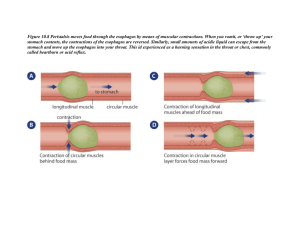
Dzholdosheva A.N EMBRYOGENESIS OF GASTROINTESTINAL TRACT • As a result of cephalocaudal and lateral folding of Embryo , endoderm lined yolk sac is incorporated into The embryo to form primitive gut. • Primitive gut is blind ended however midgut is connected To yolk sac by means of vitelline duct / yolk stalk. Pharyngeal gut : buccopharngeal membrane to tracheo Bronchial diverticulum. Foregut : caudal to pharyngeal tube extends upto Liver outgrowth. Midgut :caudal to liver upto right 2/3rd to left 1/3rd of Transverse colon. Hindgut :left 1/3rd of transverse colon to cloacal Membrane Endoderm forms lining of git , perenchyma of glands ; Liver and pancreas Splanchnic mesoderm forms muscle , connective tissue & peritoneal components. Mesoderm dictates type of struture i.E. Lung in thorax Via hox code. Mesentry is double layers of peritoneum that enclose An organ and connect it to body wall (intraperitoneal) At 5 wks gut is suspended by dorsal mesentry which Extends from lower esophagus to cloaca. Ventral mesentry is derived from septum transversum Imaging Barium is contraindicated in the immediate postoperative period, following recent rectal biopsy, or any other circumstance in which an intraperitoneal or mediastinal leak could occur. It should also be avoided in patients at high risk of aspiration In neonates ,it is advisable to use water soluble contrast agents rather than barium for both upper and lower gastrointestinal studies. Low osmolar water-soluble contrast agents include iohexol (Omnipaque 240, 300) and iopamidol (Niopam 200, 300). They have little adverse effect if extravasated into the peritoneum or mediastinum, or aspirated into the respiratory tract. generally used undiluted or mildly diluted for a contrast meal and diluted approximately 1 in 2 for an enema. Earlier hyperosmolar water-soluble agents such as meglumine/sodium (Gastrografin) and iothalamate meglumine (Conray) were associated with considerable fluid shifts, drawing water into the bowel lumen with the risk of severe dehydration and haemodynamic compromise in infants. If aspirated,they may result in severe pulmonary oedema. The only remaining indication for Gastrograffin, used in dilution, is in the enema treatment of meconium ileus, when hyperosmolarity is beneficial. For a contrast meal examination, barium or watersoluble contrast can be administered via a cup-andstraw, feeding bottle, or cautiously syringed directly into the mouth if necessary. Contrast should be introduced just over the base of the tongue so that the infant still will have to swallow. Contrast should not be delivered with the patient in the supine position. The infant should be in the lateral or right anterior-oblique position, because this guards against aspiration. With contrast enema examinations in newborn and young infants, the most important practical point is to have adequate occlusion of the anus. A Foley catheter is preferred and should be inserted before taping of the buttocks. When one is looking for low rectal pathology, such as Hirschsprung's disease, it is best not to blow up the balloon. In many cases, extensive preparation of the colon is not required and, in Hirschsprung's disease, is contraindicated. Omit the feeding before the examination. Overnight fasting is not required and is detrimental. In the neonate and young infant, fluid and electrolyte balance is delicate, and it is most important that these infants not be dehydrated for prolonged periods FOREGUT ESOPHAGUS AT 4th WK RESPIRATORY DIVERTICULUM APPEARS AT VENTRAL WALL OF FOREGUT. ESOPHAGOTRACHEAL SEPTUM RESPIRATORY PRIMORDIUM (VENTRAL) ESOPHAGUS (DORSAL) MUSCULAR COAT IS FORMAD BY SPLANCHNIC MESENCHYME STRIATED IN UPPER 2/3rd (VAGUS) SMOOTH IN LOWER 1/3rd (SPLANCHNIC PLEXUS) In neonatal esophagus mucosal folds are not as prominent as in adults, but indentations by the aortic arch, left main stem bronchus, and normal left atrium are frequently noted, even in the neonate Normal peristaltic activity usually is evident at birth but may not be as pronounced as in later life. Normal esophagus. Latera view showing normal indentations produced by aortic arch (A) and left main bronchus (B). In the recumbent position, emptying of the esophagus may be somewhat prolonged. In the neonate, the esophagus is flexible and can assume peculiar configurations during various phases of the respiratory cycle. The resulting bizarre, tortuous configuration of the esophagus at any level may at first appear startling, but repeat study usually demonstrates a normal esophagus Tortuous esophagus. A. Bizarre, tortuous-appearing esophagus in young infant. B. Moments later, the esophagus appears normal. Air in the Esophagus (Pneumoesophagus) Many infants demonstrate small amounts of air in the esophagus on regular chest films, and the finding is entirely normal. some infants demonstrate massive collections of air in the esophagus, or so-called mega-aeroesophagus . Such air collections are readily visible on plain chest films and can be startling In most of these cases, the underlying problem usually is gastroesophageal reflux , but excessive air in the esophagus also can be a sign of the presence of a tracheoesophageal fistula. Massive pneumoesophagus (i.e .. mega-aero esophagus). A. Note the marked distention of the air-filled esophagus (arrows). This air is much more voluminous than that seen under normal circumstances. Most often, such massive distention of the esophagus is the result of gastroesophageal reflux. B. Premature infant. Supine position with air reflux from the stomach into the esophagus (arrows). Transient Esophageal Hypotonia of the Neonate In some newborn infants, the esophagus appears almost totally inactive, and even with prolonged examination, little peristaltic activity is noted These infants frequently have difficulty with swallowing, and regurgitation is common. This is why they are referred to the radiologist for examination. No obstructing lesions are found, and the phenomenon is transient. Within a week or less, normal peristaltic activity prevails, feeding difficulties disappear, and the infant has no further problems. This lack of normal motility is simply a reflection of normal, but transient, neuromuscular immaturity. Transient esophageal hypotonia of the neonate. On these four spot films, taken in rapid sequence, note that there is no suggestion of peristaltic activity of the esophagus. Anyone of the spot films could be interpreted as normal, but when it is noted that on none is there evidence of peristalsis of the esophagus, transient hypotonia should be suspected. Most Common Causes of GI Tract Obstruction by Age Age Cause of Obstruction 0 -1 month Congenital anomalies Atresia/stenosis Malrotation/volvulus Hirschsprung disease Meconium plug/small left colon syndrome Meconium ileus 1-5 months Hernias 5 months-3 years Intussusception 3 years and older Perforated appendicitis Adhesions Regional enteritis Causes of Esophageal Obstruction Congenital atresia/stenosis Web/diverticulum Foreign body Stricture (peptic, caustic) Extrinsic compression (cysts, neoplasms, vascular) Achalasia ESOPHAGEAL ATRESIA & TRACHEOESOPHAGEAL FISTULA The trachea and oesophagus arise from the common foregut. Anomalies in the separation of these two structures by the oesophagotracheal septum result in oesophageal atresia, with or without an associated tracheooesophageal fistula, with an incidence of 1 in 2-4000 live births. Diagnosis may be suspected on antenatal ultrasound if the gastric bubble is small or not visualised, or if a distended proximal oesophageal pouch is seen. Polyhydramnios is commonly associ-ated. Postnatally, infants present with drooling, choking, coughing and episodes of cyanosis on feeding. When attempts to pass a naso-gastric tube are made, resistance is met and a chest radiograph will show the tube coiled in a dilated air-filled proximal oesophageal pouch Since air usually is seen in the stomach within 1 5 minutes afrer birth, an airless abdomen in the neonate should suggest the strong possibility of esophageal atresia with no tracheoesophageal fistula. ESOPHAGEAL ANOMALIES ESOPHAGEAL ATRESIA & TRACHEOESOPHAGEAL FISTULA : TYPES: •O.A. With trachea and distal esophageal fistula (85%) •O.A. Without fistula (10%) •Isolated tracheoesophageal fistula,h-type (5%) •O.A. With proximal fistula (rare) •O.A. With proximal & distal fistula (rare) Atretic segment usually at the junction of proximal & middle 1/3rd. If TOF is present , found proximal to carina. Mortality with esophageal atresia is due to congenital Anomalies. ANTENATAL DIAGNOSIS • Polyhydroamnios • Absent fundic bubble NEONATAL DIAGNOSIS •Excessive salivation , coughing and choking •Orogastric tube curls in proximal esophageal pouch Plain radiography •Air filled proximal esophageal pouch • Gasless abdomen in isolated O.A. Or O.A. With proximal fistula. •Gas in abdomen means distal fistula •Aspiration pneumonia •Vertebral anomalies (vater) Contrast study for proximal fistulas 1 ml OF LOCM TO BE USED IN LATERAL POSITION . H - TYPE FISTULA DEMONSTATED IN PRONE POSITION Figure 2: ( a) Contrast swallow showing an oesophageal atresia, overflow of contrast into the bronchial tree and a distal tracheooesophageal fistula with contrast in the stomach Figure 2: (b) Lateral chest X-ray demonstrating a contrast-fi lled blind ending proximal oesophagus and trachea outlined by aspirated contrast Oesophageal atresia with tracheooesophageal fistula. A coiled tube is seen in the dilated proximal oesophageal pouch (top arrow). The presence of distal air-filled bowel implies an associated tracheooesophageal fistula. Thirteen pairs of ribs are noted, compatible with VATER syndrome (lower arrow H-type fistulas generally present later in infancy or childhood with episodes of choking or apnoeas during feeding or recurrent lower respiratory tract infections. If suspected clinically, a 'tube oesophagram' should be performed. A nasogastric tube is passed and water-soluble contrast instilled while the tube is slowly withdrawn the oesophagus. Most fistulas involve the proximal third of the oesophagus and care should he taken to distend this segment well in order to maximise visualisation of a fistula which passes anteriorly and superiorly between the oesophagus and the trachea, in more of an `N' than an `H' configuration Contrast oesophagram demonstrating oblique track (arrows) of a tracheo-oesophageal fistula with contrast filling the tracheobronchial tree. It is important for the surgeon to know whether the aortic arch is right or left sided to facilitate surgical repair. This can be difficult to demonstrate in neonates, and magnification, high-kilovoltage techniques, and CTand MR examinations have been used to meet this end. Ultrasonography also can identify the aortic arch and determine whether it is left or right sided, but the study is not always easy to accomplish. ESOPHAGEAL STENOSIS Congenital esophageal stenosis is a far less common cause of congenital esophageal obstruction. As in esophageal atresia, esophageal stenosis arises from faulty tracheal and esophageal separation, where tracheobronchial cartilage remnants remain in the wall of the esophagus. On barium swallow, small diverticula (mucous glands) can be seen in the areas of stenosis Congenital esophageal stenosis without • Tracheobronchial remnants • Intraluminal membranes O.A. Is associated: TRACHEOBRONCHIAL REMNANTS represent abnormal rests of Respiratory tissue in esophageal wall. Localized narrowing of distal esophagus with proximal Dilatation. Multiple small diverticulum like structures (Tracheobronchial glands) perpendicular to esophagus INTRALUMINAL MEMBRANE Thin radioluscent defect that traverses esophageal Lumen at rt. Angle. Degree of obstruction depends upon size of aperture. ESOPHAGEAL BRONCHUS Abnormal origin of bronchus from esophagus Cause:incomplete cleavage b/w trachea and esophagus In utero. Recurrent , persistent infection in the area supplied by Abnormal esophagus FOREGUT CYSTS CLASSIFIED AS : •BRONCHOGENIC •GASTROENTERIC •NEURENTERIC BRONCHOGENIC CYSTS : Cause : Abnormal ventral branching of tracheobronchial tree Lined by respiratory epithelium Symptomatic due to compression of trachea or incidental Plain radiography Oval or round mediastinal mass in subcarinal or right Paratracheal region. Foregut cysts push the carina forward and esophagus Backward; thyroidal masses and aberrant left pulmonary Artery behave similarly ON BARIUM EXTRINSIC COMPRESSION OF ESOPHAGU S BY MASS CT : THIN WALLED WATER DENSITY MASSES OR SOFT TISSUE MASSES (CONFUSED WITH TUMOUR) GASTROENTERIC CYST Known as esophageal duplication cyst Cause : arise from diverticulum of primitive foregut or Abnormal recanalization of gut. Clinically silent or may cause dysphagia , pain Imaging similar to bronchogenic cyst except •Posterior mediastinum •Thick wall •On barium extrinsic or intramural compression Variety of enteric cysts communicate with esophagus. Tc 99m identifies enteric duplication cysts if they contain gastric mucosa. Cyst behind the carina deviating the esophagus to the right side. Extrinsic mass causes displacement of esophagus towards the right and mass effect on the esophagus. NEURENTERIC CYST Incomplete seperation of foregut from notochord Cyst wall contains gastrointestinal Neural elements Round or oval lobulated mass in posterior mediastinum b/w Esophagus and spine. Associated with congenital anomalies of spine i.e. Hemivertebra, spina bifida. MRI to delineate intraspinal anomalies. VASCULAR ANOMALIES • Double aortic arch • Right aortic arch with aberrant left subclavian a. • Aberrant left pulmonary artery Clinical presentation •Dysphagia •Recurrent respiratory infection •Dyspnea Suspicion (aortic) • Trachea deviated to left side • Tracheal indentation on right or posteriorly • Absent aortic arch on left Barium swallow • Posterior indentation of esophagus(lateral view) • Unilateral/ bilateral indentation (frontal view) Preoperative ct/ mri/ dsa for vascular anatomy ABERRANT ORIGIN OF LEFT PULMONARY ARTERY Known as pulmonary sling Left pulmonary arise from right pulmonary artery Diagnosis Plain radiograph Normal Obstructive emphysema rt. Lung Barium swallow Indentation on anterior wall of esophagus at the level Of carina ABERRANT SUBCLAVIAN A. ABERRANT PULMONARY A. STOMACH FUSIFORM DILATION OF FOREGUT IN 4th wk. Longitudinal axis rotation Rotates 90 degree clockwise Left side face anteriorly(left vagus) Right side face posteriorly(rt. Vagus) Posterior wall grows faster (greater curvature) Dorsal mesogastrium pulled towards rt. Side forming Lesser peritoneal sac or omental bursa Anteroposterior axis rotation Pyloric part moves to right& upwards Cardiac portion to left & downwards CONGENITAL ANOMALIES Situs solitus : stomach bubbble on left side Situs invesus : stomach bubble on rt. Side Situs ambigus :associated with polysplenia/ asplenia Duplication of stomach Bowel has additional loop or cystic component Antrum esp. Along greater curvature F>m Infant with vomiting , fever , pain Diagnosis : Usg:echogenic bowel wall surrounded by hypoechoic muscle with cyst full of echofree fluid Tc99m: TUBULAR OR COMMUNICATING CYSTS MICROGASTRIA & AGASTRIA ABSENT STOMACH (AGASTRIA) SMALL UNDERDEVELOPED STOMACH (MICROGASTRIA)ASSOCIATED WITH: •MALROTATION •CHD •AGANGLIONOSIS •ASPLENIA GASTRIC ATRESIA / WEB •FAILURE OF LUMEN TO DEVELOP IN STOMACH • PARTIAL / COMPLETE • SECONDARY TO ISCHAEMIA DIAGNOSIS PLAIN RADIOGRAPHY: COMPLETE: DISTENDED STOMACH WITH NO SMALL BOWEL GAS BARIUM STUDY RARELY INDICATED PARTIAL : BARIUM STUDY WITH TANGENTIAL PROJECTION Gastric diaphragm. A, Note the thin membrane (arrows) crossing the fluid-filled gastric antrum. B, The same diaphragm seen during a contrast upper GI series (arrows). ECTOPIC PANCREAS Small areas of ectopic pancreas may be found anywhere in GIT Gastric antrum with rudimentary duct(commonest) Diagnosis •Asymptomatic •Smooth , sessile polyp- type mass projecting into Gastric antrum below pylorus on greater curvature •Duct system on barium study seen as central niche Mimics ulcer •USG : FOCAL ANTRAL THICKNING UPTO 5 mm(unreliable) HYPERTROPHIC PYLORIC STENOSIS •Pyloric muscle hypertrophy •Unknown etiology •First born male •PRESENTS SOON AFTER BIRTH UPTO 10 wks Clinical features: •Projectile vomiting •Palpable lump Diagnosis: Palpation of olive shaped tumour,rarely radiology Required for diagnosis Usg : •Fill stomach with dextrose •Failure of passage of gastric contents •Marked gastric peristalsis •Shouldering & beaking •Single / double curved echogenic structures on Long. Section(central mucosa) •LENGTH >15mm ABNORMAL •12 – 15 mm BORDERLINE The classic appearance of pyloric stenosis on ultrasound is that of (a)elongation of the pyloric canal; (b)persistent spasm of the pyloric canal with little, if any, fluid passing into the duodenum; (c)persistent thickening of the circular muscle in the elongated canal; and (d) a sonolucent donut (thickened muscle) on cross section BARIUM MEAL •USG CAN MISS 8 % OF CASES •LONG, CURVING SINGLE OR DOUBLE PYLORIC CANAL (STRING SIGN) •SHOULDERING TO ANTRUM •MUSHROOM SHAPED APPEARANCE OF DUODENUM •DELAY UPTO 20min. CAN BE NORMAL The thickness at which the muscle is considered hypertrophied is 3 mm or greater. Pyloric canal length of 1.5 cm is considered diagnostic of pyloric stenosis when seen in conjunction with thickened pyloric muscle. In practice, however,normal canal length is much shorter than this and is often impossible to measure. Measurement of canal length is more problematic than measurement of muscle thickness and therefore a less reliable criterion. Pylorospasm and Minimal Muscular Hypertrophy In some vomiting infants, sonography shows a persistently contracted and elongated canal, but the degree of muscular thickening is less than the criterion of 3 mm for surgically correctible HPS. With extended observation, eventually the canal opens and fluid is seen to pass into the duodenum,but the periods of spasm predominate In the vast majority of cases, there is no thickening of the pyloric muscle or mucosa, and the problem is primarily nonspecific pylorospasm (antral dyskinesia) This condition can accompany milk allergy or other forms of gastritis. In some cases the pyloric muscle is mildly thickened, measuring 2 to 3 mm. Such patients should be distinguished from those with normal muscle thickness(<2 mm) because some patients with minimal muscle hypertrophy can eventually progress to classic pyloric Stenosis Many of these infants will respond to medical therapy and require no surgery Normal stomach. Normal antrum of Pyloric stenosis. AXR showing distendsetdomach (S), pyloric canal (P), and proximal duodenum (D). Four gastric air bubble. hypoechoic outer circular muscle. gastric wall layers are visible (from inside out): echogenic mucosa, hypoechoic muscularis mucosae, echogenic submucosa, Pyloric muscle tangential imaging artifacts. A, When imaging the antrum in cross section, the muscle will appear thickened if obtained through plane 1, but will show normal thickness if HPS A, Longitudinal scan shows markedly thickened, hypoechoic gastric antral muscle (arrows). Elongated canal is nearly 2 cm in length. B, Transverse scan shows typical, hypoechoic “doughnut” (arrows). Central echogenic mucosa with anechoic fluid-filled crevices. Pylorospasm. A, The pylorus remained contracted early in the examination of this infant, but the muscle is normal in thickness (arrows). B, After slightly extended period of viewing,the pylorus relaxed and appeared normal (arrows) Pyloric stenosis. Barium meal showing an elongated pyloric canal and shouldering of the antrum due to the hypertrophied pyloric muscle. Empty stomach artifact. A, Before fluid is administered, the antrum is contracted and the pyloric muscle appears thickened (arrows). B, When fluid distends the antrum, the true normal thickness of the muscle is seen (arrows). Midgut & hindgut MIDGUT 5 wks embryo suspend by short dorsal mesentry Rapid elongation of gut &mesentry form primary Intestinal loop. Cephalic limb: • Distal part of duodenum • Jejunum • Part of ileum Caudal limb : • Lower portion of ileum • Caecum , appendix • Asc. COLON & PROX 2/3 rd OF TR. Colon Malrotation and midgut volvulus is one of the major paediatric surgical emergencies and the role of radiology in its diagnosis critical. Delay in diagnosis can result in infarctive necrosis of the entire small bowel and is potentially fatal. At approximately week 6 of gestation the duodenojejunal and ileocolic segments of the primitive gut herniate into the extraembryonic coelom in the umbilical cord. Both loops elongate and rotate 270° anticlockwise around the axis of the superior mesenteric artery. By the end of the third month of gestation the bowel loops are returned to their final positions in the abdominal cavity, with their mesenteries becoming fixed to the parietal peritoneum at several sites. The duodenal loop is fixed with the duodenojejunal junction (DJJ) in the left upper quadrant at the ligament of Treitz and the ileocaecal junction fixed in the right lower quadrant. The normal DJ flexure lies to the left of the midline (at least over the vertebral pedicle) at the level of the pylorus. In malrotation, it is displaced medialy, inferiorly or both The normal small bowel mesentery therefore has a broad diagonal base across the abdomen. Physiological hernia : During 6 th wk. Rapid elongation of cephalic limb Rapid growth of liver Abdominal cavity is small so contents herniate into extraembronic cavity Rotation of midgut Around SMA axis 270 degree counterclockwise Rotation viewed from front •Rotation during herniation (90 deg.) •Return of intestinal loops(rem. Of 180 deg.) •Caecum forms during herniation Elongation of intestinal loops continue Retraction of herniated loops At 10 wks • Regression of mesonephric kidney • Reduced growth of liver • Expansion of abdominal cavity Proximal jejunum first part to enter (lies on left) Caecal bud last part to enter back(below rt. Lobe of Liver) Appendix develops during descent of caecum, Frequently retrocaecal/ retrocolic MALROTATION Any child with bilious vomiting considered to have Malrotation unless proved otherwise Malrotation is associated with malfixation so GI study to locate DJ junction Normally to the Lt. of left vertebral pedicle at the Level of duodenal cap DJ junction is mobile in children less than 4 months SMV is ventral or to the Lt. of artery in malrotation SMV spirals around SMA , artery shows hyperdynamic Circulation Band of ladd’s gives z-configuration of DJ junction TYPE I MALROTATION (NONROTATION) STOP ROTATING AFTER 90 DEG. COUTERCLOCKWISE DJ JUNCTION LIES ON RT. SIDE CAECUM LIES ON LT. SIDE CLINICALLY INSIGNIFICANT BECAUSE OF GOOD FIXATION TYPE II MALROTATION (REVERSED MALROTATION) B/W 6WKS– 10WKS AFFECTS DUODENUM ONLY DUODENUM ENDS UP IN FRONT OF SMA OR OBSTRUCTED BY LADD’S BAND MIMICKS DUODENAL ATRESIA DJ JUNCTION ON RT. & CAECUM ON RT. SIDE TYPE III MALROTATION ERROR IN ROTATION AFTER 10 WKS DJ JUNCTION & CAECUM USUALLY MIDLINE MOST DANGEROUS FORM OF MALROTATION VOLVULUS , GANGRENE & DEATH COMMON. VOLULUS GIVES BEAKED APPERENCE(COMPLETE OBST.) CORKSCREW (INCOMPLETE OBST.) LATE PRESENTATION Midgut volvulus presenting as a classic 'corkscrew' appearance of the duodenum and proximal jejunum on lateral view on ultrasound in a patient with volvulus, vigorous peristalsis of the obstructed duodenal C-loop is seen with characteristic tapering of the distal, twisted end When color Doppler ultrasound is used, the twisted mesenteric vessels are seen swirling in a clockwise direction (whirlpool sign), and this finding is highly suggestive of midgut volvulus Midgut volvulus. Vigorous peristaltic activity fails to empty the duodenum, and the third portion of the duodenum has beak deformity (arrow); S, stomach Midgut volvulus: altered relationship of mesenteric vessels. A, Normal superior mesenteric vein (V) lies to the right of the superior mesenteric artery (A). B, Intestinal malrotation and midgut volvulus; the vein (V) lies to the left of the artery (A). C, Color Doppler shows a clockwise whirlpool of vessels (arrows) around a volvulus. DUODENAL ATRESIA & STENOSIS • 1 IN 6000 LIVE BIRTHS • ATRESIA MORE COMMON THAN STENOSIS • ASOCIATED WITH DOWN’S SYNDROME, ESOPHAGEAL ATRESIA ,ARM, LADD’S BAND, RENAL ANOMALIES,BILIARY ATRESIA TYPES : TYPE I WEB (DIAPHRAGM OCCLUDING LUMEN) TYPE II BLIND END CONNECTED BY FIBROUS CORD TYPE III (MOST COMMON) NO CONNECTING CORD WITH DEFICIT OF MESENTERY TYPE IV MULTIPLE ATRESIAS ANTENATAL DIAGNOSIS •DOUBLE BUBBLE •POLYHYDROAMNIOS CLINICAL FEATURES BILIOUS VOMITING(DAY 1) PLAIN RADIOGRAPHY •DOUBLE BUBBLE APPERENCE •GAS DISTAL S/O INCOMPLETE ATRESIA Because an abdominal fluid collection can have other etiologies, it is important to demonstrate a continuum between the stomach and the cystic mass on ANC scan. A prominent incisura angularis of the stomach may be mistaken for a “double bubble” if these are in different planes, but a careful real-time longitudinal examination of the stomach can eliminate this possibility. Duodenal atresia in a fetus with trisomy 21. A, Transverse fetal pelvis at 18 weeks with echogenic bowel (arrow E). B, Same fetus at 21 weeks. Transverse view of abdomen with stomach (arrow S) on left and fluid-filled duodenum (arrow D). C, Same fetus at 25 weeks. There is a “double bubble.” The stomach is visible inferiorly (S), with the dilated proximal duodenum (D) visible crossing the midline. DUODENAL ATRESIA DOUBLE BUBBLE APPEARENCE DUODENAL WEB ANNULAR PANCREAS most common congenital anomaly of the pancreas . Pancreatic tissue encircles the descending duodenum and narrows its lumen. the bilobed ventral component of the pancreas fuses with the dorsal pancreas on both sides of the duodenum. often presents in childhood, especially in children with Down syndrome, about half of cases do not present until adulthood. Symptoms in adults nausea, vomiting, abdominal pain, and occasionally jaundice. PREOPERATIVE DIFFERENTIATION FROM DUODENAL ATRESIA IS DIFFICULT DIAGNOSIS The UGI series typically demonstrates eccentric or concentric narrowing of the descending duodenum CT pancreatic tissue seen surrounding 2nd part of Duodenum ERCP a segment of pancreatic duct encircling the Duodenum Annular Pancreas. Upper GI series demonstrates a 3-cm long circumferentially narrowed segment (arrows) of the descending duodenum. No ulceration was evident. CT confirmed an annular pancreas. Db, duodenal bulb. Annular pancreas. A, Axial T1-weighted fat- suppressed MR image demonstrates pancreatic tissue completely circumscribing the descending portion of the duodenum B, Corresponding MRCP shows the extrinsic compression around the second portion of the duodenum PREDUODENAL PORTAL VEIN PRESENTS AS DUODENAL ATRESIA/ STENOSIS PORTAL VEIN LIES ANTERIOR DUODENUM ASSOCIATED WITH •SPLENIC ANOMALIES •MALROTATION USG CAN DEMONSTRATE VEIN ANT. TO DUODENUM Pre-duodenal portal vein seen anterior to duodenum, and posterior to intraperitoneal pancreas (arrow) Jejunal /ileal atresia Commonest bowel atresia Etiology Intrauterine ischaemic insult Primary Secondary : due to antenatal volvulus Severity of ischaemia determines extent of atresia Proximal jejunum & distal ileum are common sites Clinical features •Bilious vomiting •Abdominal distention •Meconium passage depends upon time of insult & Site of obstruction Diagnosis •Dilated bowel loops to the level of atresia •Meconium peritonitis with calcification present if Intrauterine perforation has occured BARIUM ENEMA Preoperative enema is required to exclude Distal atresias Locm is preferred Microcolon is normal finding except High obstruction Low obstruction with late intrauterine insult Apple peel syndrome Intrauterine occlusion of distal sma •Proximal jejunal atresia •Agenesis of mesentery •Absence of mid small bowel Distal ileum spirals around it’s narrow vas. Pedicle Malrotated microcolon usually present •multiple sites of severe stenosis and a spiral configuration of the atretic segment. This condition tends to be familial JEJUNAL ATRESIA TRIPLE BUBBLE APPEARENCE Jejunal Atresia. Plain film shows distention of the stomach (S), duodenum (D), and loops of the upper intestine (arrows). No air is present distal to the proximal jejunum ILEAL ATRESIA DILATED BOWEL LOOPS MICROCOLON WITH REFLUX INTO TERMINAL ILEUM MECONIUM ILEUS High protein content of meconium cause distal bowel Obstruction 90%have cystic fibrosis Clinical features • Bilious vomiting • Abdominal distention • Failure of passage of meconium Antenatal diagnosis Multiple echogenic foci Meconium cysts Plain radiography Bubbly pattern of bowel gas in rt. Iliac fossa Dilatation of small bowel Usg : dilated loops with echogenic material Barium enema To determine true nature of obstruction In uncomplicated therapeutic as well as diagnostic Isoosmolar contrast medium Gastrograffin diluted half strenght with saline or water Barium sulphate inspissates & risk of perforation 1/3rd pt. Too sick--require surgery 1/3rd pt. Enema unsuccessful 1/3rd pt. One or more enema req. To remove sticky meconium Complicated meconium ileus Intraabdominal calcification Bowel wall calcification Soft tissue mass In utero perforation causes chemical peritonitis (Snow storm appearance) on usg Meconium pseudocyst is due to vascular compromise MECONIUM ILEUS BUBBLY APPEArance Meconium Ileus. A. Plain film shows the soap-bubble effect of air mixed with meconium in the numerous distended loops of intestine. B. Contrast enema demonstrates a typical microcolon with reflux into the terminal ileum, which is filled with pellets of meconium (arrows). Meconium plug syndrome misleading name for a condition caused by functional immaturity and abnormal peristalsis of the distal colon. Also known as small left colon syndrome , this condition should not be confused with meconium ileus. a normal to dilated proximal colon filled with meconium and an empty distal descending colonic segment are characteristic The meconium in infants with this condition is normal and is not the cause of obstruction. more common in normal large infants and infants of diabetic mothers. functional obstruction is transient and can often be treated by rectal stimulation or saline enemas Normal ganglion cells are present in these infants, and once the meconium has passed, the patient will defecate Normally. Meconium Plug Syndrome (Small Left Colon Syndrome). A. Numerous loops of intestine are distended with air. Also, note air in the relatively narrow rectosigmoid colon (arrow). B. Contrast enema demonstrates a small left colon with the characteristic transition zone (arrow). These findings mimic VITELLINE DUCT ANOMALIES Meckel's diverticulum •2--4 % population vitelline duct persist •40--60 cm FROM IC JUNCTION CLINICAL FEATURES •BRIGHT RED PAINLESS RECTAL BLEEDING •Obstruction secondary to intussusception Vitelline cyst / enterocystoma cause strangulation or volvulus Vitelline fistula : duct patent entire length (fecal discharge) Tc pertechnate scan dignostic for heterotrophic pancreatic tissue ,gastric mucosa Meckel Diverticulum. A scan performed with technetium99m-pertechnate shows an abnormal collection of tracer in the right lower quadrant (arrow), whose intensity parallels that of the stomach (S). Gastric mucosa within the Meckel diverticulum is responsible for the tracer localization. B, bladder. HINDGUT HINDGUT GIVE RISE TO DISTAL 1/3rd OF TR. Colon,descending colon Sigmoid , rectum & upper part of rectal canal Terminal portion of hindgut enters posterior reg. Of cloaca (Primitive anorectal canal ) Allantois enters anterior portion ,primitive urogenital sinus Urorectal septum forms perineum Ectodermal proliferation closes distal most part of anal canal which is recanalized Junction b/w ectoderm & endoderm , pectinate line Normal appearance in neonate Haustral patterns are hardly developed Large bowel is redundant, sigmoid reaching upto hepatic Flexures Caecum can appear higher Lymphoid follicles , tiny nodular filling defect,upto 2mm Upto 5 yrs is s/o good coating Lymphoid hyperplasia >3 mm ,found in • dysgammaglobulinemia • Ibd • Lymphoma Lymphoid hyperplasia Large bowel atresia Rarer than small bowel atresia Clinical features •Failure to pass meconium •Abd. Distention •Vomiting Types :type I -- web Type II -- gap bridged by atretic cord Type III -- complete seperation (most com.) Right colon is mostly involved Diaphragm prolapse in retrograde fashion into dilated prox. Segment, windsock appearence Functional motility disorder Hischprung's disease 1 in 5,000 live births, m>f Absence of myenteric ganglion in distal large bowel Hypertonic aganglionic segment Zone of transition gradual change from ganglionosis to aganglionosis Rectosigmoid region is most common (70%), 25% extend to the splenic flexure or transverse colon (long segment) and 5% involve the entire colon (total colonic Hirschsprung's disease). Cause : due to arrest in the normal cranial-to caudal neural cell migration, resulting in absence of ganglion cells within the myenteric plexus of the bowel wall Clinical features failure to pass meconium within the first 48 h of life. A smaller number present with intractable constipation later in childhood and occasionally into adulthood. Enterocolitis occurs in 15% of patients and can be the initial presentation, with fever and diarrhoea. Diagnosis Biopsy is definitive Radiology and manometery helpful Plain radiography OBSTRUCTION ( >3 cms) Cross table lateral with pt . prone for zone of transition Contrast enema No bowel prepration Water soluble contrast media preferred Lateral position to recognize zone of transition Absence of tr. Zone does not exclude disease Delayed film showing retention is also s/o disease Reversal of rectosigmoid ratio Irregular saw tooth contractions in aganglionic seg. The normal neonatal rectum is of greater calibre than the sigmoid colon. Inversion of the rectosigmoid index, often in association with irregular contractions of the aganglionic rectum and difficulty in obtaining good rectal distension, is indicative of Hirschsprung's disease Hirschsprung's disease. An abrupt transition zone is seen at the rectosigmoid junction on this lateral rectal view from a contrast enema performed on a 2-day-old boy with failure to pass meconium. The rectum was difficult to distend well and showed irregular contractions. Enteric duplication cyst Additional portion of gut develops Non communicating with bowel except tubular type Mesenteric side of iileum , common site Muscle layer continuous with bowelwall Clinical features • Vomiting due to obstruction • Abdominal pain • Palpable abdominal mass Usg : • Unilocular anechoic cystic mass • Double layered • Tc 99m req. In tubular & communicating cyst Mesenteric cyst / lymphangioma Sequestration of lymphatic vessels Omental cysts ( in omentum) Intermitent symptoms Soft & mobile , difficult to palpate Usg : •Uniloculated / multiloculated •Thin or thick septations Anechoic or echogenic debris Anorectal malformation Absence of normal anus, First day presentation with obstruction 1 in 5,000 live births Male > female Cause : abnormality in formation of cloaca Posterior portion of cloaca is small so hindgut opening Shifts anterioly Classification : On basis of rectum above or below puborectalis sling •High •Intermediate •Low Low variety No communication with gu tract Visible perineal opening anterior (ectopic anus) High variety No visible perineal opening Comm. With gu tract present Imperforate anus No anal opening , lack of recanalization of lower Portion of anal canal. Associations: Oeis (5%) omphalocele-exstrophy-imperforate anus-spinal defects) Vacterl (45%) Down syndrome (2-8%) Currarino's triad;anorectal stenosis Scimitar sacrum Presacral mass lesions Plain radiograph Distal bowel obstruction Invertogram no more used , cross table lateral taken. Intravesicle air s/o high variety Calcified intraluminal meconium (high variety) Vertebral anomalies (vater) Usg : Renal tract anomalies( ectopic, horseshoe) Spinal usg to rule out cord tethering Transperineal for distance b/w anal dimple & distal large bowel Loopogram : Size of bowel distal to colostomy Any fistula To look for leaks or obstruction after pull through surgery or Before colostomy closure Ct/ mri ; Indicated if incontinence or constipation after operation BODY WALL DEFECTS Omphalocele Herniation of abdominal viscera covered by amnion through enlarged umblical ring Cause : failure of bowel to return to body cavity from physiological herniation 2.5/ 10,000 live births Mortality 25% Cardiac anomalies 50% Antenatal presence of sac with umblical insertion Gastroschisis 1/ 10,000 live birts Increased incidence with cocaine use Herniation of bowel contents directly into amniotic cavity Right lateral to umblicus (regression of rt. Umblical vein) Not covered by amnion or peritonium No chromosomal anomalies Bowel are short, edematous & coated with fibrocollagenous Coating Excellent survival Gastroschisis. Several air-filled extra-abdominal loops of bowel are seen in this infant of 26 weeks gestation. A small left congenital diaphragmatic hernia was also present . THANK YOU