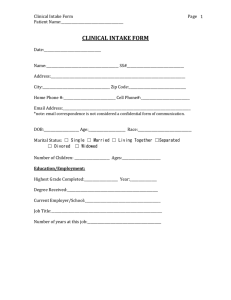
1 Initial Clinical Intake This is an example of what you may utilize when doing a clinical intake. There are various of often more personalized templates which different clinics, organization and practices utilize to conduct an initial intake assessment. Personal Information Basics: Name, age, gender, sexual orientation, marital or relationship status, ethnicity/race, religious affiliation, current housing situation, highest level of education Personal History 1. What is your current occupation? How long have you been in your current position? How long have you been in this field? If student: Where do you go to school? Academic grade level/college/grad school, etc. 2. How many significant romantic relationships have you had? (In any of the relationships, did you experience any physical, sexual, verbal abuse or was substance abuse an issue)? 3. Have you had prior therapy? YES / NO If yes: a. Tell me about your previous therapy experience: b. Reason therapy ended: 4. Suicidality: Do you have current thoughts, or have you had thoughts in the past of hurting yourself? If yes to past but not current, collect more info: When? Hospitalization? Ideation or Plan? Attempt? If yes to current, will have to do further assessment for: Ideation, Plan, Access to Means - How often do you have these thoughts? - When was the last time? - Scale 0-10 (10 being strongest) how strong is your desire not to live currently? - Would anything make it better? 2 - Have you ever thought about how or when you would harm yourself? - Is the method you would use readily available? - Is there anything that would stop you from harming yourself? Resources to utilize: Further assessment (per site/practice policy), creating a safety-plan, providing client with resources, phone numbers you may need (i.e., for hospitalization) 5. What does your support system look like: Emotionally, Physically, Spiritually, and Financially? 6. How do you spend your down time (leisure, interest, hobbies)? Family History/Cultural History 7. Describe your relationship with family of origin members. (Explore parental/sibling relationships, both past and present) a. Marital/relationship status of parents b. Living/passed away? c. Any family mental health hx? 8. Is there anything significant about your culture that your therapist should know about? 9. In a sentence or two, please describe your childhood and upbringing. Medical History 10. When was your last physical check-up? (month/year) anything significant? (if not within 2 years offer client at least 2 physician referrals) 11. Have you ever been treated by a psychiatrist? 12. Have you received any mental health diagnoses (past or present)? 3 13. Are you currently taking any medications (including psychotropic)? 14. Do you have allergies to medications or foods? YES / NO If yes, please have them describe what happens when in contact with allergen. 14. Do you currently have problems with pain? YES / NO If yes: a. Where is your pain located? ________________________________________ b. How long have you had this pain problem? __________________________________ c. What things help your pain? ______________________________________________ d. How intense is your pain today? (none) 0 1 2 3 4 5 6 7 8 9 10 (worst) e. Are you currently being treated for your pain? Yes/No If yes, who is your provider? __________________________________________________________ Nutrition 15. Do you purge, restrict intake, or overeat? If yes, please describe: 16. Has your appetite changed recently? If yes, please describe: 17. Have you lost or gained at least 10lbs in the last 30 days? If yes, please describe: 18. How many hours of sleep do you get? Do you have any issues with sleep (too much, too little, insomnia, apnea)? 19. How often do you exercise? 20. Alcohol and drug intake a. Do you drink alcohol? How often? b. Drug use – if yes, what and how often c. Tobacco use d. Nicotine use e. Caffeine use 4 MENTAL STATUS EXAMINATION (Utilize MSE form if preferred) Orientation: Appearance: Behavior: Speech: Mood and Affect: Insight and Judgment: Perceptual/Thought Disturbances: PRELIMINARY TREATMENT PLAN: Preliminary dx, goals, recommendations/referrals (1) PROVISIONAL DIAGNOSIS: N/A – to be further assessed (2) GOAL FOR THERAPY (AT LEAST 1 GOAL FOR THERAPY): (3) RECOMMENDATIONS OR REFERRALS