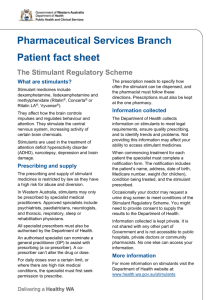
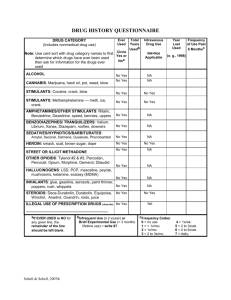
Managing Stimulant Use Disorder Stimulants are “uppers”, they speed the body up Stimulants include: amphetamines, cocaine, crack, MDMA, Ritalin, Dexedrine, caffeine, nicotine Can be ingested, snorted, injected, or smoked Often used as a survival strategy (eg to stay awake all night to protect themselves or their belongings) No evidence based pharmacological approach to treatment at present, although trials have occurred with a number of drugs including Ritalin, Dexedrine, topiramate, modafinil and meth amphetamine Evidence supports the use of contingency management, motivational interviewing and CBT as well as other psychosocial approaches Patients can be referred to the contingency management group at RAAC by AMCT SW Substance Food Sex Morphine Nicotine Cocaine Amphetamines Crack Initial Effects Lasts 5-30 mins Feelings of intense euphoria Warm skin, dry mouth Feeling thirsty, not hungry Rapid HR and RR Auditory hallucinations Withdrawal Feeling restless, sweaty and twitchy Sensitive to light and noise Feelings of paranoia Strong cravings for more crack Dopamine increase (relative to baseline) 150% 200% 200% 225% 350% 1000% Crystal Meth Initial Effects Lasts 4-24+ hours Feeling alert and energetic Not feeling hungry or tired Dry mouth Rapid HR and RR Feeling restless, anxious, paranoid, unable to sleep Withdrawal Feeling extremely tired, unable to sleep, anxious, Hungry and thirsty Clenched jaw Strong cravings for more meth Stimulant Overdose Tachycardia Tachypnia Hypertension hyperthermia Diaphoresis, tremors Chest pain Anxiety, paranoia, agitation Confusion, hallucinations Loss of consciousness Vomiting Seizures Severe headache Jerking limbs, involuntary body movements Sleep deprivation There is no antidote to stimulant overdose, treatment requires supportive management. Naloxone will not work for a stimulant overdose, but should still be used if presentation cannot be differentiated form opiate overdose Stimulant withdrawal is often confused with over sedation from opioids. Patients who use both opioids and stimulants should still have their opioid withdrawal treated even if they are in bed sleeping as a result of withdrawal from stimulants. Patients withdrawing from stimulants will likely have a POSS score of “S”, patients over sedated from opioids will have a POSS score of 3 or 4 If the patient has no pulse, call code blue and initiate CPR Stimulants can be contaminated with opioids and this has resulted in inadvertent opioid overdoses If alert and can safely swallow, encourage hydration Encourage them not to take any more substances until the current substance has worn off Low stimulation environment if possible (eg. private room or semi-private room) Reassurance and support Consider need for medications such as anxiolytics and antipsychotics If overheated, cool them down with cold towels or ice packs Always offer harm reduction strategies and supplies to patients who use stimulants and inform them of OPS hours and location Drug testing is available at the OPS for fentanyl and benzodiazepines, this can be especially life-saving for people who only use stimulants as they do not have a tolerance for opioids