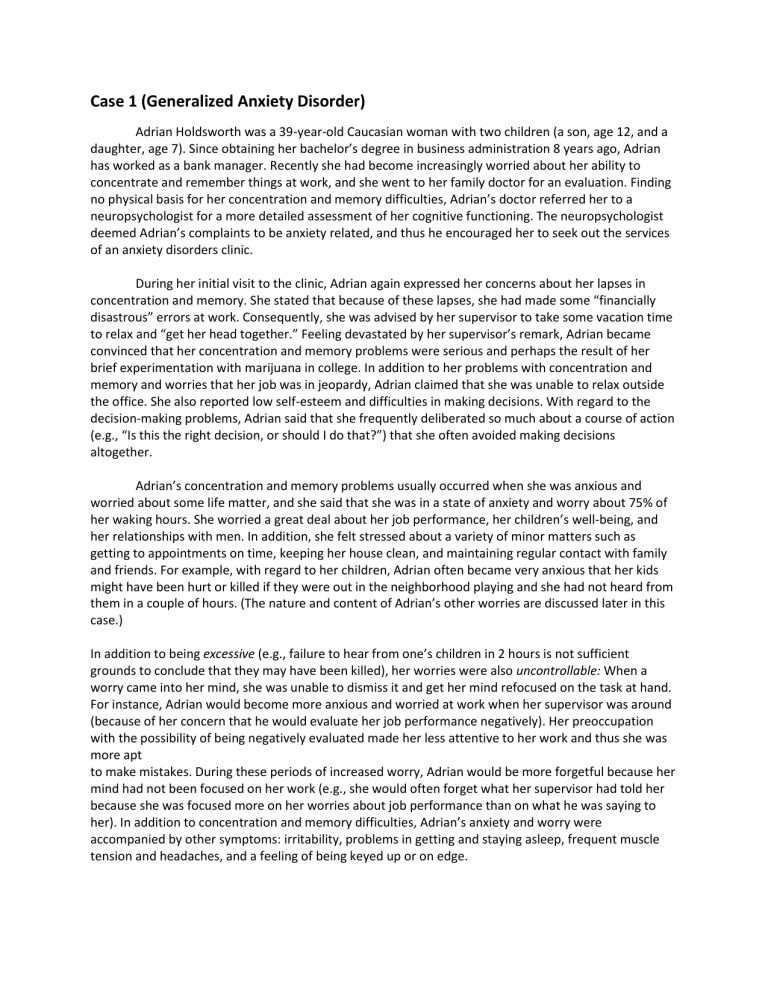
Case 1 (Generalized Anxiety Disorder) Adrian Holdsworth was a 39-year-old Caucasian woman with two children (a son, age 12, and a daughter, age 7). Since obtaining her bachelor’s degree in business administration 8 years ago, Adrian has worked as a bank manager. Recently she had become increasingly worried about her ability to concentrate and remember things at work, and she went to her family doctor for an evaluation. Finding no physical basis for her concentration and memory difficulties, Adrian’s doctor referred her to a neuropsychologist for a more detailed assessment of her cognitive functioning. The neuropsychologist deemed Adrian’s complaints to be anxiety related, and thus he encouraged her to seek out the services of an anxiety disorders clinic. During her initial visit to the clinic, Adrian again expressed her concerns about her lapses in concentration and memory. She stated that because of these lapses, she had made some “financially disastrous” errors at work. Consequently, she was advised by her supervisor to take some vacation time to relax and “get her head together.” Feeling devastated by her supervisor’s remark, Adrian became convinced that her concentration and memory problems were serious and perhaps the result of her brief experimentation with marijuana in college. In addition to her problems with concentration and memory and worries that her job was in jeopardy, Adrian claimed that she was unable to relax outside the office. She also reported low self-esteem and difficulties in making decisions. With regard to the decision-making problems, Adrian said that she frequently deliberated so much about a course of action (e.g., “Is this the right decision, or should I do that?”) that she often avoided making decisions altogether. Adrian’s concentration and memory problems usually occurred when she was anxious and worried about some life matter, and she said that she was in a state of anxiety and worry about 75% of her waking hours. She worried a great deal about her job performance, her children’s well-being, and her relationships with men. In addition, she felt stressed about a variety of minor matters such as getting to appointments on time, keeping her house clean, and maintaining regular contact with family and friends. For example, with regard to her children, Adrian often became very anxious that her kids might have been hurt or killed if they were out in the neighborhood playing and she had not heard from them in a couple of hours. (The nature and content of Adrian’s other worries are discussed later in this case.) In addition to being excessive (e.g., failure to hear from one’s children in 2 hours is not sufficient grounds to conclude that they may have been killed), her worries were also uncontrollable: When a worry came into her mind, she was unable to dismiss it and get her mind refocused on the task at hand. For instance, Adrian would become more anxious and worried at work when her supervisor was around (because of her concern that he would evaluate her job performance negatively). Her preoccupation with the possibility of being negatively evaluated made her less attentive to her work and thus she was more apt to make mistakes. During these periods of increased worry, Adrian would be more forgetful because her mind had not been focused on her work (e.g., she would often forget what her supervisor had told her because she was focused more on her worries about job performance than on what he was saying to her). In addition to concentration and memory difficulties, Adrian’s anxiety and worry were accompanied by other symptoms: irritability, problems in getting and staying asleep, frequent muscle tension and headaches, and a feeling of being keyed up or on edge. Adrian was very concerned about her excessive worry and anxiety: “I hate feeling this way all day. I just want to feel normal and in control of what’s going on in my life!” In addition to the distress they caused, Adrian’s symptoms interfered a great deal with her life. For example, she spent many extra hours at the office, arriving 30 minutes early every day to “make sure that I have my day all planned out as much as possible” (to decrease the likelihood of committing errors in her work). It took her much longer than necessary to accomplish tasks or to make decisions because she would question the accuracy of every step in the process. In addition, Adrian reported that her symptoms had a negative impact on her social and family life. She claimed that her children often complained that she was always in a bad mood. She knew that she was spending little time with her friends and had noticed that the few men she dated never seemed to call her back after the first or second date: “They can sense that I’m not a fun person.” Moreover, her worry and anxiety had affected her physically. She reported having “borderline hypertension” (moderately elevated blood pressure), which her family doctor had attributed to stress. Adrian also had a history of migraine headaches that were fairly well controlled with prescription medication but seemed more likely to occur after she worried excessively. In addition to her worry and anxiety over various life matters (e.g., job performance, children’s wellbeing), Adrian reported some discomfort in social situations in which she might be observed or evaluated by others. Specifically, Adrian said that dating, being assertive, participating in meetings, and public speaking were situations that she tended to endure with moderately high levels others, however, Adrian stated that she rarely avoided these social situations. She noted that some of her apprehension of these social situations was related to her concern that she would lose her train of thought during the interaction and be embarrassed. Clinical History: Adrian reported a fairly typical middle-class upbringing. She got along quite well with her two younger brothers and her parents. Although she regarded her parents as “uptight and serious,” she did not believe that either of them had a history of an emotional disorder (e.g., anxiety, depression). In fact, the only family member that Adrian could recall who had such difficulties was her paternal grandfather, who had alcoholism. Adrian thought of herself as being shy throughout childhood; nevertheless, she reported several enduring friendships and hobbies. She had been an A student until high school (age 14), when she and her family moved to another city and she started attending a new school where she did not know anyone. On the basis of her past grades and test scores, Adrian was advised to take honors classes at her new school. At this time, she began to worry excessively—specifically, that she would fail these classes. She began to have trouble sleeping the night before an exam and noticed some trouble concentrating in her more challenging classes. Her fear of failure emerged at this time, and she began to procrastinate on homework assignments, completing them at the last minute. She also recalled that her shyness increased during this period; she felt more anxious around boys and more hesitant to speak up in class. Adrian’s parents and friends tried to reassure her that everything was fine and not to worry. Her teachers also tried to help her relax, and some offered to read rough drafts of her papers to provide reassurance that she would ultimately receive a passing grade for her work. However, Adrian’s worries and insomnia increased even more when she started getting Bs in a few of her classes. She feared that because she was no longer a straight-A student, she might not be able to get into college. Her increasing sleep problems contributed to her worries as well—she was concerned that if she did not get enough sleep, her schoolwork would suffer even more. Adrian’s symptoms tended to wax and wane throughout her high school and college years. She noticed that she slept better and had fewer concentration and memory problems during summer vacations and holidays. However, the symptoms returned with the new school year and during exam periods. Dating often increased Adrian’s anxiety as well, based on her worries that her date would not like her or would evaluate her negatively. As a result of this, and because her parents, whom she regarded as strict, had not permitted her to date until she was 17, Adrian dated infrequently. Nevertheless, during her senior year of college, she met the man she eventually married, at age 22. During the first few years of her marriage, Adrian noticed that she felt less anxious. Yet, problems arose in her marriage after the birth of her two children. Her husband, who was a biochemist and a native of Hungary, wanted to move the family back to his homeland so that he could take an academic position in Budapest. Adrian wanted her children to be raised in the United States and had no desire to live outside the country herself. This conflict eventually led to divorce, and her husband moved back to Budapest alone. At first, he visited the children over the holidays and during summers. However, as the children got older, they began to travel during vacations to visit their father in Hungary. During these visits, Adrian worried excessively about her children’s safety and well-being. This worry, along with her concerns about job performance, minor matters, and her relationships with men, spiraled to higher and higher levels of frequency and intensity. As noted earlier, Adrian also worried about her brief experimentation with marijuana during college. Although she had tried marijuana on only a handful of occasions when she was 20, Adrian was concerned that these experiences had killed some of her brain cells, causing her persistent problems with her memory and concentration. Her family doctor had reassured her that her past marijuana use had most likely not permanently altered her memory and concentration. Adrian was able to accept this reassurance, but her confidence in her doctor’s words usually eroded over the course of a few days, or as soon as she perceived that she was having trouble concentrating or remembering. Case 2 (Post-Traumatic Stress Disorder) Cindy Oakley responded to a community advertisement for a university-based research clinic that was evaluating treatments for victims of sexual assault. At the time of her first contact with the clinic, Cindy was a 26-year-old Caucasian woman with two children. She was not employed outside her home, although she had recently been hired to do some freelance work that was scheduled to start in a few weeks. During her first interview at the clinic, Cindy reported that she had been depressed for the last 3 months. The depression had started shortly after Cindy had ended a 5-week extramarital affair. During the affair, Cindy began to have flashbacks of events from 10 years in the past. These events centered around a series of repeated rapes that had occurred when she was 16 years old. In addition to distressing images of these events that seemed to come into her mind out of nowhere, these flashbacks included times when Cindy would momentarily feel as if the past were occurring all over again. When Cindy realized that this affair coincided with the exact time of year that she had been raped, she broke off the affair. Nevertheless, Cindy became increasingly depressed and agitated as more memories surfaced. It was only now, a decade later, that Cindy began to label what had occurred then as rape. At the initial interview, Cindy stated that she had been raped repeatedly over a 5-week period by a close friend of the family. This boy, who was the same age as Cindy (16 years old), lived across the street. Because the boy came from an abusive family, Cindy’s family “adopted” him. He was best friends with her brother, and so he spent a lot of time at their home. Cindy’s parents were also quite fond of him. Prior to the rape, Cindy said that she had had a “brother-sister” relationship with the boy, whose name was Mark. Cindy gave only a sketchy account of these incidents during the first interview and made very little eye contact with the interviewer. The interviewer did not press for details during this session but rather focused on standardized questions from a structured clinical interview that was part of the research program. During the interview, Cindy reported that she had been a virgin prior to the rape and had trusted Mark quite a bit before the assault. She was verbally threatened by him, although no weapons or physical injuries were involved. Cindy was subjected to a range of sex acts, including oral, vaginal, and anal intercourse. During the assaults, her most prominent reactions were feeling detached and numb, guilty, and embarrassed. The incidents were not reported to the police, and she never received medical care. During the initial interview, Cindy stated that she often smoked marijuana. She was defensive about her use of it and said that she did not want to quit. In addition, Cindy stated that one of her previous therapists had made a big deal over her marijuana use. When Cindy had told this therapist that she felt that she was using marijuana as a crutch, he informed her that marijuana was her main problem. She disagreed, told the therapist that she did not want to make marijuana the focus of her treatment, and quit therapy. In fact, besides the single session with this therapist, Cindy had sought therapy two previous times; however, each of these contacts had lasted only one session. Clinical History: Cindy described her childhood as a happy one. She characterized her house as the safe house in the neighborhood, where all the kids could come to play and where some found refuge from problems in their own homes. Cindy’s father was a Vietnam veteran who continued to have posttraumatic stress disorder from events he had experienced during the war. She described her father as emotionally shut off, yet spoke very fondly of him. She described her mother as a self-help fanatic who kept the house filled with self-help books. Cindy also stated that she had a close and supportive relationship with her mother. As noted earlier, Cindy had one older brother who was best friends with the boy who had raped her. Cindy claimed that she was close to her brother until the rape; since the rape, they rarely interacted with each other. After describing her childhood before the rape, Cindy told the therapist about how drastically things had changed since these incidents. Cindy said that she had told her mother what had happened and that her mother stopped the abuse. After the therapist questioned her a bit further, however, Cindy recalled that she had told her mother that Mark had been “coming on” to her, that it had gotten out of control, and that she needed help getting out of the situation. The abuse ended after Cindy’s mother told Mark to leave Cindy alone. Cindy never told her mother that she had been raped. Therefore, her family did not understand why she had changed. After the rape, Cindy withdrew from her normal high school activities and began to hang out with troubled kids. Over the year following the assaults, Cindy lied often and began drinking. She described herself as floating in and out of reality. She and her mother fought frequently. A year after the rape, a friend of hers was driving recklessly and crashed the car in which Cindy was a passenger. Cindy was out of school for 2 months with a broken back. She recalled that over the next few years she became a “total rebel” and dated a “wild guy who was totally bad news.” She became pregnant by him and, not knowing what to do, consulted her father. Her father took over and arranged for an abortion. Cindy said that although she might have ultimately made the same decision, she now regretted that she had relinquished her right to decide. Cindy did not have the selfconfidence to go to college. Her mother talked her into taking classes at a business school for secretarial training. She had worked as an executive secretary until the current year. At the time of this initial interview, Cindy had been unemployed for 6 months. Cindy stated that fortunately she had had the “good sense” 5 years ago to marry a fine man with whom she had two children. Cindy said that her husband was very supportive of her and did not give up on her after the affair. Cindy’s husband was also very supportive of her efforts to receive therapy. Other than her husband, however, her social support was rather poor. In fact, Cindy reported receiving negative reactions to her disclosure about the assault from others who were closest to her. For example, Cindy recalled that she had once told one of her best friends that she was having a difficult week because the memories of the rape were surfacing. Her friend, a woman she had known since high school, responded by saying, “Get over it.” Case 3 (Major Depressive Disorder) Janet called the mental-health center to ask if someone could help her 5-year-old son, Adam. He had been having trouble sleeping for the past several weeks, and Janet was becoming concerned about his health. Adam refused to go to sleep at his regular bedtime and also woke up at irregular intervals throughout the night. Whenever he woke up, Adam would come downstairs to be with Janet. Her initial reaction had been sympathetic, but as the cycle came to repeat itself night after night, Janet’s tolerance grew thin, and she became more argumentative. She found herself engaged in repeated battles that usually ended when she agreed to let him sleep in her room. Janet felt guilty about giving in to a 5yearold’s demands, but it seemed like the only way they would ever get any sleep. The family physician was unable to identify a physical explanation for Adam’s problem; he suggested that Janet contact a psychologist. This advice led Janet to inquire about the mental-health center’s series of parent-training groups. Applicants for the groups were routinely screened during an individual intake interview. The therapist began by asking several questions about Janet and her family. Janet was 30 years old and had been divorced from her husband, David, for a little more than a year. Adam was the youngest of Janet’s three children; Jennifer was 10, and Claire was 8. Janet had resumed her college education on a parttime basis when Adam was 2 years old. She had hoped to finish her bachelor’s degree at the end of the next semester and enter law school in the fall. Unfortunately, she had withdrawn from classes 1 month prior to her appointment at the mental-health center. Her current plans were indefinite. She spent almost all of her time at home with Adam. Janet and the children lived in a large, comfortable house that she had received as part of her divorce settlement. Finances were a major concern to Janet, but she managed to make ends meet through the combination of student loans, a grant-in-aid from the university, and child-support payments from David. David lived in a nearby town with a younger woman whom he had married shortly after the divorce. He visited Janet and the children once or twice every month and took the children to spend weekends with him once a month. Having collected the necessary background information, the therapist asked for a description of Adam’s sleep difficulties. This discussion covered the sequence of a typical evening’s events. It was clear during this discussion that Janet felt completely overwhelmed. At several points during the interview, Janet was on the verge of tears. Her eyes were watery, and her voice broke as they discussed her response to David’s occasional visits. The therapist, therefore, suggested that they put off a further analysis of Adam’s problems and spend some time discussing Janet’s situation in a broader perspective. Janet’s mood had been depressed since her husband had asked for a divorce. She felt sad, discouraged, and lonely. This feeling had become even more severe just prior to her withdrawal from classes at the university (1 year after David’s departure). When David left, she remembered feeling “down in the dumps,” but she could usually cheer herself up by playing with the children or going for a walk. Now she was nearing desperation. She cried frequently and for long periods of time. Nothing seemed to cheer her up. She had lost interest in her friends, and the children seemed to be more of a burden than ever. Her depression was somewhat worse in the morning, when it seemed that she would never be able to make it through the day. Janet was preoccupied with her divorce from David and spent hours each day brooding about the events that led to their separation. These worries interfered considerably with her ability to concentrate and seemed directly related to her withdrawal from the university. She had been totally unable to study assigned readings or concentrate on lectures. Withdrawing from school precipitated further problems. She was no longer eligible for student aid and would have to begin paying back her loans within a few months. In short, one problem led to another, and her attitude became increasingly pessimistic. Janet blamed herself for the divorce, although she also harbored considerable resentment toward David and his new wife. She believed that her return to school had placed additional strain on an already problematic relationship, and she wondered whether she had acted selfishly. The therapist noted that Janet’s reasoning about her marriage often seemed vague and illogical. She argued that she had been a poor marital partner and cited several examples of her own misconduct. These included events and circumstances that struck the therapist as being very common and perhaps expected differences between men and women. For example, Janet spent more money than he did on clothes, did not share his enthusiasm for sports, and frequently tried to engage David in discussions about his personal habits that annoyed her and the imperfections of their relationship. Of course, one could easily argue that David had not been sufficiently concerned about his own appearance (spending too little effort on his own wardrobe), that he had been too preoccupied with sports, and that he had avoided her sincere efforts to work on their marital difficulties. But Janet blamed herself. Rather than viewing these things as simple differences in their interests and personalities, Janet saw them as evidence of her own failures. She blew these matters totally out of proportion until they appeared to her to be terrible sins. Janet also generalized from her marriage to other relationships in her life. If her first marriage had failed, how could she ever expect to develop a satisfactory relationship with another man? Furthermore, Janet had begun to question her value as a friend and parent. The collapse of her marriage seemed to affect the manner in which she viewed all of her social relationships. The future looked bleak from her current perspective, but she had not given up all hope. Her interest in solving Adam’s problem, for example, was an encouraging sign. Although she was not optimistic about the chances of success, she was willing to try to become a more effective parent. Clinical History: Janet was reserved socially when she was a child. She tended to have one or two special friends with whom she spent much of her time outside of school, but she felt awkward and self-conscious in larger groups of children. This friendship pattern persisted throughout high school. She was interested in boys and dated intermittently until her junior year in high school, when she began to date one boy on a regular basis. She and her boyfriend spent all of their time together. Janet remembered that the other kids teased them about acting as if they were married. Unfortunately, she and her boyfriend broke up during Janet’s first year in college. Janet met David a few weeks afterward, and they were married the following summer. Janet later wondered whether she had rushed into her relationship with David primarily to avoid the vacuum created by her previous boyfriend’s sudden exit. Whatever her motivation might have been, her marriage was followed shortly by her first pregnancy, which precipitated her withdrawal from the university. For the next seven years, Janet was occupied as a full-time mother and homemaker. When Adam was 2 years old and able to attend a day-care center, Janet decided to resume her college education. Her relationship with David became increasingly strained. They had even less time than usual to spend with each other. David resented his increased household responsibilities. Janet was no longer able to prepare meals for the family every night of the week, so David had to learn to cook. He also had to share the cleaning and drive the children to many of their lessons and social activities. A more balanced and stable relationship would have been able to withstand the stress associated with these changes, but Janet and David were unable to adjust. Instead of working to improve their communications, they bickered continuously. The final blow came when David met another woman to whom he was attracted and who offered him an alternative to the escalating hostility with Janet. He asked for a divorce and moved to an apartment. Janet was shaken by David’s departure, despite the fact that they had not been happy together. Fortunately, she did have a few friends to whom she could turn for support. The most important one was a neighbor who had children of approximately the same ages as Janet’s daughters. There were also two couples with whom she and David had socialized. They were all helpful for the first few weeks, but she quickly lost contact with the couples. It was awkward to get together as a threesome, and Janet had never been close enough with the women to preserve their relationships on an individual basis. That left the neighbor as her sole adviser and confidante, the only person with whom Janet felt she could discuss her feelings openly. For the next few months, Janet was able to continue her studies. With the children’s help, she managed the household chores and kept up with her work. She even found time for some brief social activities. She agreed to go out on two blind dates arranged by people with whom she and David had been friends. These were generally unpleasant encounters; one of her dates was boring and unattractive, and the other was obnoxiously aggressive. After the latter experience, she discontinued the minimal efforts she had made to develop new friendships. As time wore on, Janet found herself brooding more and more about the divorce. She was gaining weight, and the children began to comment on her appearance. To make matters worse, Claire became sick just prior to Janet’s midterm exams. The added worry of Claire’s health and her concern about missed classes and lost studying time contributed substantially to a decline in Janet’s mood. She finally realized that she would have to withdraw from her classes to avoid receiving failing grades. By this point, 1 month prior to her appointment at the mental-health center, she had lost interest in most of her previous activities. Even casual reading had come to be a tedious chore. She did not have any hobbies because she never had enough time. She also found that her best friend, the neighbor, was becoming markedly aloof. When Janet called, she seldom talked for more than a few minutes before finding an excuse to hang up. Their contacts gradually diminished to an occasional wave across the street or a quick, polite conversation when they picked up their children from school. It seemed that her friend had grown tired of Janet’s company. This was Janet’s situation when she contacted the mental-health center. Her mood was depressed and anxious. She was preoccupied with financial concerns and her lack of social relationships. Adam’s sleeping problem, which had begun about a week after she withdrew from her classes, was the last straw. She felt that she could Case 4 (Oppositional Defiant Disorder) As she stood outside her son’s bedroom door holding the handle shut, trying to keep him inside for his punishment, Nicole Helms fought back her tears. She felt like such a failure, and she had no idea what to do. Her 4-year-old son’s horrible temper tantrums scared her badly, and she felt both helpless and angry. Her mother-in-law, Mrs. Helms, would be home soon, and Nicole wanted her son, Tyler, to calm down before she arrived. He stopped screaming, kicking at the door, and pulling on the door knob, and she breathed a sigh of surprise and relief, hoping maybe he was going to stop. Then she heard a loud crashing noise that made her jump and fling open the door, fearing for Tyler’s safety. To her horror, she saw that he had climbed up on the bookshelf and ripped the curtains off the wall, knocking the bookshelf down in the process. She shouted at him, swatted his bottom, and then started to cry. He ran past her into the living room and flipped on the TV while she sat down on the floor in despair. At that point, she decided she had to get help, or her son would surely end up like his father. The next morning, she called Tyler’s pediatrician, and his nurse arranged an appointment with a child clinical psychologist, Dr. Bell. Two weeks later, Nicole and Mrs. Helms brought Tyler for his appointment. Dr. Bell met them in the waiting room, calling Tyler’s name. She then kneeled down to his height level, smiled at him, and said hello. She introduced herself to Nicole and to Mrs. Helms, shaking their hands. She brought all three into her office, where she invited Tyler to play with the toys while she talked with his mother and grandmother to gather information about the presenting problem, symptoms, and family history. When he was younger, Tyler’s behavior seemed like that of other children his age, but in the past year or so, his first symptoms had appeared, and his behavior had become quite different from that of other children. He had become very mouthy and angry and said mean things to his mother and grandparents. He would call his mother fat and tell his grandparents he hated them. His mother and grandparents found themselves tiptoeing around him, hoping he would stay in a good mood, because when he was mad, nobody around him could be happy. Tyler’s behavior was mostly unmanageable. Nicole could not control it, nor could her husband’s parents. They had tried spanking him, reasoning with him, pleading with him, and taking away his toys. They had even tried rewarding him with candy or ice cream if he stopped having a fi t. When he didn’t get his way, he would have a temper tantrum until he did. During his temper tantrums, his mother and grandmother had the impression that he was trying to get his way manipulatively, rather than really losing control of his emotions. He would start crying, screaming, fall to the ground, kick and hit the floor, and if that didn’t work, he would knock things off the coffee table or tip over a kitchen chair. He would also hit or kick an adult if they tried to stop him. When Nicole tried to spank him for misbehaving, he would laugh at her and say it didn’t hurt. Then she would hit him harder until she scared herself and stopped, clutching him close and begging his forgiveness. He wouldn’t go to bed when asked to and fell asleep most nights in front of the television. He wouldn’t clean up his toys and even argued about brushing his teeth. When his mother was talking on the telephone, even if it was something important, he would come over and start making clicking noises with his tongue at her over and over, louder and louder, to annoy her until she paid attention to him. Basically, if he got his way, he acted happy and could be very sweet, but he didn’t act happy that much anymore. Even when they took him somewhere fun, like Chuck E. Cheese, he wanted more game tokens than he was given or didn’t like his pizza. He would argue about which booth they chose to sit in or who should sit next to him. When he was arguing, his tone of voice was harsh and bossy. On occasions that she tried to discipline him, he would do something to get her back. Once when they were eating lunch at home, he said he wanted a cookie. Nicole told him he could have one when he finished half his sandwich. He looked at her defiantly, then picked up his glass of milk and slowly poured it all over his sandwich and the table. When closed in his room, he would throw his toys everywhere, pull the sheets off the bed, and empty all the clothing out of the drawers until she opened the door and relented. She had stopped trying to take him to church or the grocery store because it was so embarrassing when he acted that way. She dreaded what would happen when he started school next fall. Clinical History: Tyler was the only child of Billy and Nicole Helms. They were married the summer after they graduated from high school, and a year and a half later, Tyler was born. Tyler was the product of an uncomplicated, full-term pregnancy, and there were no problems during his birth. He met his early developmental milestones— such as crawling, walking, and talking—on time and had no health problems. He was affectionate, talkative, inquisitive, and curious as a toddler. He loved being read to and could sit for long periods of time listening to a book his mother read to him when he was only 2 years old. Nicole and Tyler developed a close, warm relationship. Nicole was a full-time homemaker, and Billy worked as a welder. They lived in their own apartment in the same part of town as Billy’s parents. Nicole’s parents were divorced, and her father lived in another state. She hadn’t seen him since she was 8 years old. Nicole’s mother did not have a very close relationship with Nicole, and they frequently argued over Nicole marrying Billy, over Nicole’s disapproval of her mother’s boyfriend, and over how she was raising Tyler. Nicole had pretty much stopped spending time with her. Billy was very close with his parents, though, and they got along well with Nicole. Nicole spent a lot of time with his mother when Billy and Mr. Helms, his father, were at work, and Mrs. Helms would often babysit for Tyler. Nicole and Billy’s relationship were mostly loving and positive, but Billy had episodes of “moodiness,” which was probably clinically significant depression. This “moody streak” seemed to run in his father’s family, striking the men: His father also had bouts of depression from time to time. Neither Billy nor his father had been treated for their depression. Members of Billy’s family worried about all their male children being affected with this affliction, and Mrs. Helms was constantly watching Tyler as a young toddler for early signs that he was going to inherit the moody streak, too. Billy had begun smoking marijuana when he was in middle school. He used it fairly regularly throughout high school and occasionally after he and Nicole married. Nicole occasionally smoked it with him when she was in high school, but after they married, she stopped using it. They sometimes drank alcohol, but Billy drank more than Nicole. After she got pregnant, Nicole didn’t like Billy using drugs and pressured him to keep marijuana out of their home. He mostly complied. He would hang out with his friends and sometimes get high, but he didn’t bring it into their apartment anymore. He was an involved father and was close to Tyler, who was his pride and joy. He loved “play wrestling” with his son, and Tyler loved watching him play video games. He would give Tyler a set of controls and let him pretend he was playing, too. Tyler seemed to worship his father and followed him around, imitating him. Just after Tyler turned 3 years old, Billy began sinking into one of his depressions. He spent less and less time with the family and more time away, with friends or off by himself. He started smelling like marijuana smoke all the time again. Nicole was worried but didn’t know what she could do beyond begging him to stop smoking. After 2 months of this behavior, one day he took off. While Nicole and Tyler were at Walmart, he packed up all of his clothes, his video games, and music and left in his pickup truck. He didn’t write a note of explanation, didn’t say goodbye, and didn’t say anything to his friends, parents, or coworkers. Nicole and his parents had not heard anything from him since then. For the first several weeks, Nicole was sure he would come back. When their minimal savings ran out, she and Tyler had to move in with Billy’s parents and let their apartment go. Mr. and Mrs. Helms were very loyal to Nicole and ashamed that their son had deserted his family. They were determined to take care of her and Tyler. Mrs. Helms, however, harbored secret fears that this abandonment of Tyler by Billy cemented Tyler’s fate of having the moody streak, too. Case 5 (Depression) Anna Thompson was a 16-year-old African American female referred to the adolescent unit of an inpatient psychiatric hospital. Her mother, Mrs. Thompson, referred Anna after discovering her daughter in her bedroom bleeding from her wrists. The amount of blood was not substantial, but Mrs. Thompson brought Anna to a hospital emergency room for treatment. The attending physician said Anna was not seriously injured, but recommended commitment to an inpatient psychiatric hospital for evaluation. Mrs. Thompson consented to a short-term commitment of her daughter given Anna’s recent depressive behaviors. A psychiatrist who specialized in adolescent behavior disorders interviewed Anna the next day. Anna was initially hesitant about talking to the psychiatrist and was angry with her mother for committing her. She was more forthcoming after some initial discussion, however. Anna said she recently moved to a new school following her mother’s divorce and that no one seemed to like her. She was upset about being in the racial minority and having few friends. When asked if a specific recent event upset her, Anna said she felt other teenagers made derogatory remarks about her weight as she ate alone during lunch (Anna was quite overweight). Anna could not be more specific, however, so whether remarks were actually made about her was unclear. Anna also said that the past 13 months were difficult. Her parents separated and eventually divorced following some marital conflict. For reasons Anna did not completely understand, her mother moved out of state with Anna and separated her from her father and 13-year-old brother. This was traumatic for Anna because she was close to her father and brother, but could no longer contact them. Anna enrolled in her new school in August and began attending in September. She missed about onethird of the school days in the first 2 months and had not attended school in the past 2 weeks. Anna said she was lonely because her mother often worked and because she had no new friendships. Anna’s mood worsened over the past 2 weeks. She greatly missed her entire family and complained she could not spend Thanksgiving with her father and brother (her mother already said this was impossible). She thus became less active, lying around the house, watching television, and surfing the Internet to chat with others. She left the house only twice in the past week and was overeating and oversleeping. Her mother worked a lot and did not talk to Anna much in the past 2 weeks. When they did converse, she tried to persuade Anna to go back to school. The psychiatrist also raised the topic of Anna’s injuries from the day before. Anna said she was feeling bad and wondered what it would be like if she committed suicide. She wondered how her family would feel and who would come to her funeral. She said she was not optimistic about the future and that suicide sometimes seemed preferable to living. Anna insisted, however, that her behavior was not an actual suicide attempt. She claimed she made a few scrapes with a butter knife to see what would happen. She did get herself to bleed but did not feel her injuries were serious (the medical report confirmed Anna’s statements). Anna said her mother came into her room, saw blood, and “freaked out.” Anna’s mother told her to get into the car and enter the emergency room. The attending physician asked about her injuries and Anna told him truthfully what happened. She was then transferred to her current unit with a person sitting outside her room to watch her. The psychiatrist asked Anna if she had current thoughts about harming herself, and Anna said no. She said again she did not want to kill herself the day before and that she now wanted to leave the unit. She also asked to see her mother and was told she would see her that evening. Anna promised the psychiatrist not to harm herself and to speak with him immediately if she had suicidal thoughts or impulses. The psychiatrist gave Anna a mild sedative and she slept for the remaining afternoon. The psychiatrist also interviewed Anna’s mother, Mrs. Thompson, who provided more information about the family situation. Mrs. Thompson said she and her husband had many past arguments about several issues, most notably his alcohol use and the family’s financial status. The last straw came, however, when Mrs. Thompson caught her husband leaning over Anna as she slept. Mrs. Thompson suspected Anna’s father of sexual abuse, though this was unproven. Anna denied this in conversations with her mother, but Mrs. Thompson felt she and Anna should leave the state. Mrs. Thompson said she parted company with her son as well because he was unruly and because they had a poor relationship. Mrs. Thompson confirmed some of Anna’s reports with respect to recent events. She confirmed she was busy at work and unable to devote the kind of attention to Anna her daughter was used to. The two did share time together on the weekends, however, though not in the past 3 weeks, and had good rapport. Mrs. Thompson also confirmed that she and Anna had little contact with Anna’s father and brother. She said this would continue with the upcoming holiday season. Mrs. Thompson also verified that Anna missed a lot of school in the past 2 months and did not make new friends. Both women were concerned about Anna’s weight and Mrs. Thompson knew this was a major source of embarrassment and frustration for her daughter. Despite these situations, Mrs. Thompson said she was shocked to find Anna bleeding in her bedroom. Mrs. Thompson never considered the possibility of suicide, but the apparent seriousness of the situation led her to agree to the inpatient commitment. The psychiatrist also spoke with Anna’s guidance counselor at school with Mrs. Thompson’s permission. The counselor, Mrs. Deetz, was upset about Anna’s condition and said Anna commented about suicide 1 month earlier. Anna came to Mrs. Deetz’s office and complained that students in her physical education class ridiculed her weight. Anna cried, complained she could not make friends, and said, “I wish I was dead.” Mrs. Deetz then changed Anna’s schedule so she would not have to attend that particular physical education class. She also made several recommendations regarding extracurricular activities, but Anna dismissed them because she would be in the racial minority. Mrs. Deetz insisted, however, that Anna’s concerns about social rejection were unfounded. She remained concerned about Anna and offered to assist the psychiatrist in any way possible. The psychiatrist reinterviewed Anna the next day to confirm she had no current suicidal thoughts or impulses. He placed her on a low dose of antidepressant medication and asked her to attend group therapy sessions that morning and evening. Anna agreed and the psychiatrist noted that her mood improved somewhat from the day before. Given information received so far, however, the psychiatrist suspected Anna just experienced a major depressive episode and should remain on suicide watch. Case 6 (Social Anxiety and Withdrawal) Bradley Mavin was a 12-year-old Caucasian male referred to a specialized clinic for youths with social anxiety and withdrawal. Bradley was in seventh grade at the time of his initial assessment. His stepfather and mother, Mr. and Mrs. Nelson, referred Bradley to the clinic after reading a newspaper advertisement calling for participants in a group therapy project. The project involved testing an assessment and treatment protocol for youths with social problems. During the telephone screening interview, Mrs. Nelson said Bradley was having trouble adjusting to his new middle school and seemed depressed and withdrawn. He also seemed upset about her recent divorce and remarriage. Bradley was thus missing more school than usual and his grades were suffering. An advanced doctoral student in clinical child psychology interviewed Bradley during the intake session. Bradley was initially cautious and unsure of himself, avoiding eye contact and speaking softly. The doctoral student, who had experience with shy and socially anxious children, first talked to Bradley about various topics he seemed to enjoy. These included his pets, school projects, and sisters. Bradley seemed more relaxed following this development of rapport. The student then questioned Bradley about his recent social problems. Bradley said his new middle school was quite different from the elementary school he was in since kindergarten. He said many of his friends from elementary school now went to a different middle school, so he did not know many people at his current location. He wanted to transfer to the other middle school to be with his old friends. Bradley also claimed that few of his new classmates spoke to him or invited him for lunch or other activities. The interviewer discovered that Bradley rarely initiated contact with others in school, however. Bradley also said he “hated” physical education class where everyone “made fun of him” for his size; he was slightly smaller than his peers. He generally felt lonely, sad, and “left out.” Bradley also complained about oral presentations in his English class, an assignment he never had before. He said his first oral presentation went badly. He was supposed to give a presentation on the history of automobiles, but became anxious when asked to stand before his classmates. Bradley said he trembled and had trouble breathing, which made his hands and voice shake noticeably. He saw some of his classmates snicker and decided then not to give another presentation. Unfortunately, he was required to give three other presentations; not doing so would result in a failing grade. Bradley started refusing school because of these experiences. He began by occasionally skipping his physical education class, but in the past month missed 1-2 full days of school per week. Bradley would stay home, do homework, and watch television when skipping school. He already asked his parents to transfer him to a new middle school or place him in home schooling. The interview also focused on other areas of Bradley’s social life. Bradley said he was active with neighborhood friends but avoided anyone new. He also had a good relationship with his mother and two sisters. His relationship with his stepfather was strained, however. Bradley said his stepfather was strict and not afraid to spank him for various offenses. His stepfather was livid about his refusal to go to school and his parents often fought about this issue. They immediately called the number in the newspaper when they saw it was for children with social problems. Mr. and Mrs. Nelson largely confirmed Bradley’s report during their interview. Mrs. Nelson said Bradley was a well-behaved son until about 2 years ago when she and her first husband separated (Bradley’s biological father was currently out of state and had no contact with the family). Bradley then became withdrawn and unwilling to play with other children in his neighborhood. Contrary to Bradley’s report, he still avoided many of his old neighborhood friends and spent much of his free time doing homework or playing video games. He did participate in family dinners and outings, but generally preferred to stay close to his mother and sisters. Mrs. Nelson said Bradley’s situation worsened during the past 3 months. She confirmed Bradley’s fears about his physical education class and oral presentations and agreed he made few, if any, new friends. She also confirmed that Bradley wanted to be placed in home schooling and she was about to do so when she saw the clinic’s advertisement. Mrs. Nelson then decided Bradley might benefit more from therapy than home schooling and she wanted the advice of clinic staff members on this matter. Mrs. Nelson said Bradley was an excellent student who was generally shy. He enjoyed working on his school projects as much as other kids enjoyed playing baseball. He was a “loner” who rarely interacted with other children his age and who preferred to play with his two younger sisters. Otherwise, he was a normal child who was compliant, polite, and dutiful regarding his household responsibilities. Mr. Nelson added that his relationship with Bradley was difficult and that the two “just didn’t seem to connect.” Mr. Nelson was adamant about Bradley’s return to school but deferred to his wife when she recommended therapy. He said he wanted to help Bradley with his problems, but was not sure he could. Mr. Nelson hoped therapy would help Bradley become more self-confident and improve their relationship. The therapist secured Mr. and Mrs. Nelson’s permission to interview Bradley’s teachers at school. All said Bradley was a fine student with excellent potential, but was shy and withdrawn. Bradley’s English teacher, Mrs. Arnot, said he did well on all assignments up to the oral reports. His first oral report had not gone badly, but Bradley clearly had physical symptoms of anxiety. She also said she had a strict class rule that students could not make jokes or laugh when anyone gave an oral report, and no one did during Bradley’s report. Bradley approached her after class and cried profusely, however, asking to be relieved of his remaining oral presentations. Bradley’s physical education teacher echoed this report, but said Bradley was teased to some extent. The teacher said Bradley needed to “grow up,” interact more with other kids, and become more assertive. Conversations with Bradley’s other teachers and guidance counselor confirmed that Bradley avoided many social situations, especially those that required meeting new people, working cooperatively with others, and performing before an audience. The therapist preliminarily concluded that Bradley was moderately socially withdrawn and met criteria for social phobia/social anxiety disorder.