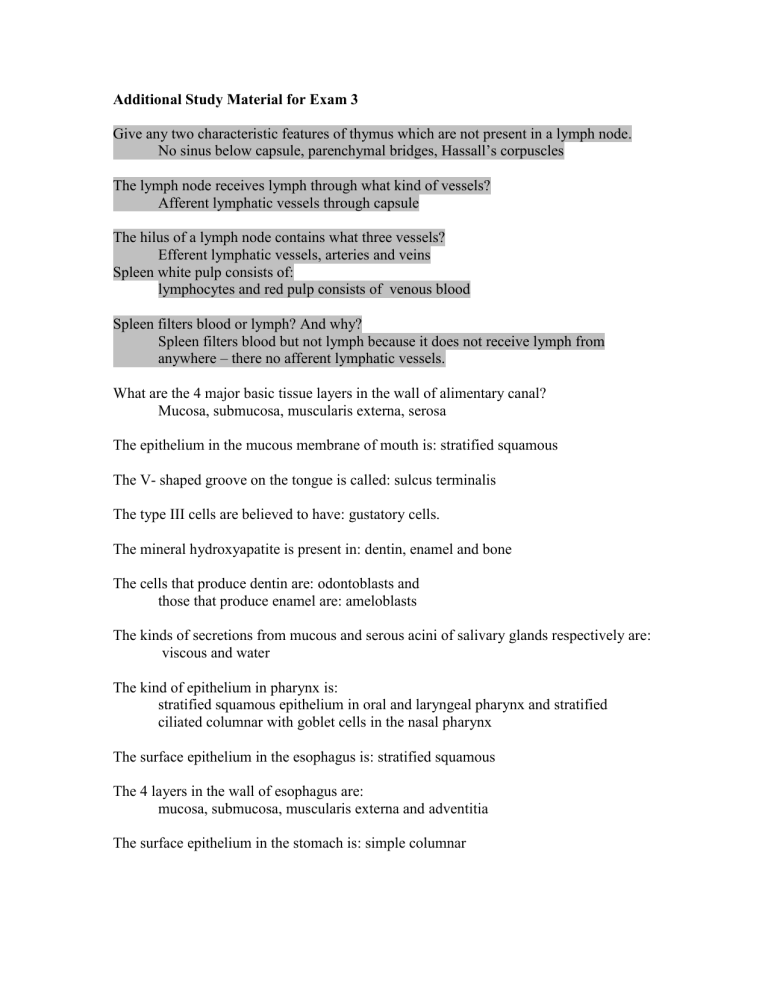
Additional Study Material for Exam 3 Give any two characteristic features of thymus which are not present in a lymph node. No sinus below capsule, parenchymal bridges, Hassall’s corpuscles The lymph node receives lymph through what kind of vessels? Afferent lymphatic vessels through capsule The hilus of a lymph node contains what three vessels? Efferent lymphatic vessels, arteries and veins Spleen white pulp consists of: lymphocytes and red pulp consists of venous blood Spleen filters blood or lymph? And why? Spleen filters blood but not lymph because it does not receive lymph from anywhere – there no afferent lymphatic vessels. What are the 4 major basic tissue layers in the wall of alimentary canal? Mucosa, submucosa, muscularis externa, serosa The epithelium in the mucous membrane of mouth is: stratified squamous The V- shaped groove on the tongue is called: sulcus terminalis The type III cells are believed to have: gustatory cells. The mineral hydroxyapatite is present in: dentin, enamel and bone The cells that produce dentin are: odontoblasts and those that produce enamel are: ameloblasts The kinds of secretions from mucous and serous acini of salivary glands respectively are: viscous and water The kind of epithelium in pharynx is: stratified squamous epithelium in oral and laryngeal pharynx and stratified ciliated columnar with goblet cells in the nasal pharynx The surface epithelium in the esophagus is: stratified squamous The 4 layers in the wall of esophagus are: mucosa, submucosa, muscularis externa and adventitia The surface epithelium in the stomach is: simple columnar The gastric mucosa is thrown into large folds called: rugae which in turn have smaller pits called: foveolae The three kinds of glands in gastric mucosa are: cardiac, oxyntic and pyloric Give the names and secretion(s) / function(s) of 5 kinds of cells in the gastric glands: Mucous Neck Cells - Columnar, lodged between large rounded oxyntic cells, Nucleus displaced in the base of the cell PAS+ secretory granules in cytoplasm with mucigen Stem Cells - Responsible for continuous renewal of gastric mucosa, Surface mucous cells are replaced every four days Oxyntic or Parietal Cells - Most conspicuous, pyramidal with large spherical nucleus, produce HCl, have broad rounded bases and large mitochondria, apical surface has invaginations called secretory canaliclui, microvilli project into the lumen of secretory canaliculi, cytoplasm has no secretory granules, active oxyntic cells have five fold increase in secretory canaliculi and microvilli, 60-80 % of the increase is due to H+ / K+ ATPase for acid secretion, Oxyntic cells also produce gastric intrinsic factor (GIF) for absorption of vitamin B 12, Deficiency of GIF results in erythrocyte immaturity and Pernicious anemia, Deficiency of acid results in achlorhydria Chief or Zymogenic Cells - found in lower third of oxyntic glands, absent in cardia, sparse in fundus and rare in pylorus, Numerous apical secretory granules containing pepsinogen, Well developed Golgi complex, rough ER and lysosomes, Enteroendocrine cella - found scattered individually among the cells of all glands, are called argentaffin or enterochromaffin cells, produce biogenic amines and peptide hormones • G cells – gastrin for gastric motility and acid secretion • EC cells – secretin for gastric motility • D cells – somatostatin – inhibits other enteroendocrine cells • A cells – enteroglucagon – raises blood sugar level • ECL cells – histamine for gastric secretions The enzyme localized in the membranes of oxyntic cells is: H+ / K+ ATPase What is the pH of the gastric secretions? 0.9 -2.0 The three specializations that increase surface area in small intestine are: plicae circulares, villi and microvilli What are the names and functions of the secretions from the following cells in small intestine? A or α cells in pancreas and stomach; produce glucagon for carbohydrate metabolism B or β cells in pancreas; produce insulin for carbohydrate metabolism D or δ cells in pancreas, stomach and intestine; produce somatostatin which inhibits secretion of glucagon and insulin D1 cells in pancreas, stomach and intestine; produce vasoactive intestinal polypeptide for vasoconstriction EC cells in pancreas, stomach and intestine; produce serotonin for vasoconstriction ECL cells in fundic stomach; produce histamine for vasodilation G cells in duodenum and pyloric stomach; produce gastrin for gastric secretions I cells in jejunum and ileum; produce cholecystokinin which inhibits secretion of gastric juices and stimulates pancreatic juices and bile ejection from gallbladder S cells in jejunum and ileum; produce secretin which inhibits secretion of gastric juices and stimulates pancreatic juices The kind of epithelium is small intestine is: simple columnar What are kinds of cells / glands present in SI epithelium? And their functions? Absorptive cells - Simple columnar with microvilli and surface coat made of glycoproteins, Microvilli have actin and myosin that are responsive to ATP and Ca++, Lateral walls of cells are widened for absorption of fat and accumulation of chylomicra, Digestion occurs at the surface, Disaccharides to monosaccharides by disaccharidases, Polypeptides to amino acids by proteases Goblet cells - Unicellular exocrine cells secreting PAS+ mucus Enteroendocrine cells, Scattered at the base of epithelium, Also called enterochromaffin or argentaffin cells, Secrete hormones into lamina propria, Common in duodenum, fewer in jejunum – see above for all details of enteroendocrine cells Crypts of Lieberkuhn - Are intestinal glands at the base of the villi, Produce watery intestinal juices which serve as solvent for digested nutrients Paneth Cells - Are small group of cells at the base of crypts of Lieberkuhn, Produce and release antibacterial lysozyme and phospholipase A2 What are lacteals and where are they located? What is their function? lacteals are lymphatic capillaries in SI villi for absorption of lymph loaded with ats. The specific location for Peyer’s patches is: lamina propria of ileum What are M cells? Cells that help capture microorganisms in Peyer’s patches What is the function of Paneth cells? They produce antibacterial lysosomes and phospholipase 2 - and where are they located? Bottome of crypts of Lieberkuhn Give the specific location for the Brunner's glands: Submucosa of duodenum Give the names of a protein digesting enzymes secreted from small intestine: leucine amino peptidase Give any 2 specific characteristic features of appendix that are not present in the rest of the large intestine? Cross section of appendix shows angular outline, Villi are absent in appendix but crypts of Lieberkuhn are present What change in epithelium occurs in rectum and anus? Becomes stratified squamous The three nerve plexus that form deeper intrinsic system in the intestines are: GI is innervated by divisions of autonomic nervous system - Parasympathetic, sympathetic and enteric, Parasympathetic and sympathetic constitute extrinsic division and enteric constitutes intrinsic division The Intrinsic Division - Located within the walls, is autonomous and can work without CNS - Superficial in subserous area Deeper and most conspicuous Myenteric (Auerbach’s) plexus between longitudinal and circular muscles, Deep muscular plexus – mucosal aspect of circular muscles Submucosal (Meissner’s) plexus Give the special features of colon and cecum mucosa Simple columnar epithelium, No plicae circulares, No villi beyond ileocecal sphincter, Numerous crypts of Lieberkuhn, No Paneth cells, Abundant goblet cells Hepatic sinusoids are branches of: hepatic portal vein What vessels are expected to be found in a portal canal – arteries, veins, lymphatic vessels and bile ducts The blood capillaries in the liver are called: sinusoids A classical liver lobule is defined as: cells radiate around central veins What kind of cells are found in sinusoidal lining? endothelial and Kupffer What is space of Disse and what is its function? space between endothelium and hepatocytes, the function is formation of lymph Give specific features of a hepatocyte - Cells are polyhedral (6 or more sides) with three surfaces, One side is exposed to space of Disse, A second side is exposed to bile canaliculi, A third one in contact with the adjacent cell, Large single nuclei, most cells single nucleated; about 25 % are binucleate, One or more nucleoli per nucleus, rich in rough ER, fat, glycogen, mitochondria and peroxisomes with enzymes uricase The walls of bile canaliculi are rich in: ATPase activity Order of bile duct branching is - Bile canaliculi terminal ductules (canals of Hering) drain into interlobular bile ducts right and left hepatic ducts common bile duct after joining with cystic duct from gallbladder Functions of liver include: It filters and cleans blood – Kupffer cells involved It is a blood storage site - sinusoids have enormous volume ~ 400 ml Resistance to blood flow in liver causes development of ascites and leads to cirrhosis It processes and transfers nutrients Maintains normal blood sugar level by glycogenesis and glycogenolysis Maintains normal lipid levels by transporting or transforming It is the site of synthesis of plasma proteins - Substantial rate of production of albumin, alpha and beta globulins, glycoproteins, lipoproteins, prothrombin, fibrinogen etc. It is the site of detoxication of lipid soluble drugs such as barbiturates (sleep inducers) Enzymes in the smooth endoplasmic reticulum (microsomes) called microsomal enzymes are responsible Administration of drugs such as barbiturates stimulates activities of microsomal enzymes Has excretory function - Bilirubin from the breakdown of red blood cells is eliminated by Kupffer cells, Bilirubin urobilinogen feces, Accumulation of bilirubin hyperbilirubinemia jaundice, Causes of jaundice include increased production of bilirubin, decreased uptake of blood by liver, disturbance in conjugation of bilirubin with other substances and interference with its secretion Major function of liver concerned with the digestive system is the secretion of bile Bile consists of: Cholesterol, Lecithin, Fatty acids, Electrolytes, Bile salts, Bile salts emulsify fat molecules The function of bile is – emulcification of fats The important histological features of gallbladder are: Gallbladder wall consists of distinct Mucosa – see below, Submucosa – dense connective tissue, Muscularis – all smooth muscles, Subserosa – loose connective tissue, Serosa – loose connective tissue Epithelium is tall simple columnar with microvilli and is thrown into folds called Rugae, Outpouchings called Rockitansky-Aschoff sinuses cross lamina propria and muscles – this is a pathological condition, Lamina propria has loose connective tissue with mucosal glands, Smooth muscles are longitudinal, transverse and oblique, Frequently dense connective tissue with Luschka ducts are found among smooth muscles, Luschka ducts are embryonic bile ducts which never established connection with lumen – a histological feature Junction of gallbladder with pancreas consists of A portion of duodenum wall, The common bile duct, The pancreatic duct, The ampulla of Vater, The sphincter of Oddi Bile concentration by gallbladder is by which process? Active transport of NA= followed by water by osmosis. Describe the release and actions of small intestinal hormone for pancreatic stimulation and secretion: Hormonal stimuli are through the release of two hormones both from small intestinal mucosa Secretin – causes release of large volumes of bicarbonates solution to neutralize acidic chyme Cholecystokinin – causes release of large volumes of enzyme solution and activates gallbladder for bile release Pancreatic exocrine secretion contains Pancreatic amylase for starch and glycogen digestion Pancreatic lipase for digestion of lipids Trypsinogen, chymotrypsinogen, procarboxypeptidases and trypsin inhibitor for protein digestion Also DNAse and RNAse Pancreatic endocrine cells are located in – islets of Langerhans Hormones from pancreatic endocrine cells and their secretions are Alpha Beta Delta cells cells cells F cells Location Periphery Throughout Throughout Scattered %/# next to beta 70 % third least Granules large/dense less dense heterogeneous - Mitochondria smaller larger - - Golgi Complex less prominent more prominent - Hormones glucagon insulin somatostatin pancreatic Polypeptide Names of cartilages in larynx are Three unpaired – thyroid, cricoid and epiglottis Three paired – arytenoid, corniculate and cuneiform Gradual changes that appear when trachea branches include Cartilage ring to cartilage plates to complete disappearance Epithelium columnar to low columnar or cuboidal to suamous in alveoli Appearance of smooth muscles in bronchioles What specific kinds of epithelium are found in the following locations? Olfactory - pseudostratified columnar ciliated Trachea – pseudostratfied columnar ciliated with goblet cells Primary bronchi – ciliated columnar with goblet cells Bronchiole – ciliated low columnar to cuboidal Respiratory bronchioles – cuboidal to low cuboidal Alveolar ducts – simple squamous What are two chemical substances produced in type 2 alveolar cells? Pulmonary surfactant consisting mainly of dipalmitoyl phosphatidyl-choline – reduces surface tension of water Also dense secretory granules called lamellar bodies rich in phospholipids Also have alkaline phosphatase activity with clinical What is the significance of Clara cells? Are specialized cells which populate the epithelium of the respiratory tree from the level of terminal bronchiole to alveolar duct. Are polyhedral, non-ciliated with cytoplasmic biosynthetic organelles Clara cells are known to have a role in: • Surfactant production; their product is not the same as that produced by the type II alveolar cells, but it may form one constituent of surfactant • Detoxification; the number of Clara cells increases in response to increased exposure to pollutants e.g. chronic cigarette inhalation • Clara cells have secretory granules and produce guanylin for the control of water an electrolyte transport in the GI Barrier to diffusion of gases in alveoli consists of • A layer of fluid surfactant • A thin slender epithelium • A basal lamina of the epithelium • A thin interstitium • A basal lamina of the capillaries • A capillary endothelium What are the kinds of pressure that help regulate breathing? • Atmospheric Pressure – 760 mm Hg • Intrapulmonary Pressure in the alveoli • Intrapleural Pressure - 4 mm Hg lower than atmospheric pressure – negative pressure is important for keeping lungs inflated What are the muscles of inspiration? – diaphragm and external internalcostals What are the muscles of expiration – for normal expiration just the relaxation of muscles of inspiration is sufficient. For forced expiration the required muscles are abdominals and internal intercostals. Non-respiratory functions of respiratory system include Metabolism - Monoamine oxidase and P450 microsomal enzymes Endocrine function - Prostaglandin and histamine secretions Speech - Vocal cords Smell - Olfactory cells of nose