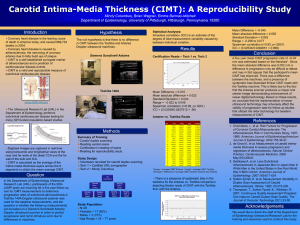
Review Article Carotid Intima Media Thickness and Its Utility as a Predictor of Cardiovascular Disease A Review of Evidence Mark Carpenter, MChem,* Hannah Sinclair, BSc, MB ChB, MRCP,†‡ and Vijay Kunadian, MBBS, MD, FRCP†‡ Abstract: Cardiovascular (CV) disease is still the leading cause of death in the developed world, despite the considerable progress in CV medical and surgical therapeutics. Many risk factors are associated with the development of future adverse CV events, such as age, hypertension, body mass index, and other comorbidities. Carotid intima media thickness (CIMT) is one method of calculating plaque burden by assessing the level of arterial thickening present. CIMT can be used as a noninvasive marker of atherosclerotic disease with increasing CIMT linked to an increased risk of subsequent CV events. In this review, the association of CIMT with CV disease is explored. Current literature on the role of CIMT in predicting CV outcomes is reviewed to determine whether it is a predictor of CV events, both in the general population and in the high-risk groups, such as those with hypertension, diabetes mellitus, and chronic kidney disease. Key Words: coronary artery disease, atherosclerosis, carotid intima media thickness, cardiovascular risk, cardiovascular outcomes. (Cardiology in Review 2016;24: 70–75) C ardiovascular disease (CVD) is still the leading cause of death in the developed world, despite the considerable progress in cardiovascular (CV) medical and surgical therapeutics. Many risk factors are associated with the development of future adverse CV events, such as age, hypertension (HTN), body mass index (BMI), and other comorbidities. Carotid intima media thickness (CIMT) is one method of calculating plaque burden by assessing the level of arterial thickening present. CIMT can be used as a noninvasive marker of atherosclerotic disease with increasing CIMT linked to an increased risk of subsequent CV events.1 CIMT is a combined measure of both the intimal and the medial layers of the arterial wall, which may limit its use in predicting early atherosclerosis where intimal thickening predominates.1 Nonetheless, whether a change in CIMT over time affects the risk of CV events has not been thoroughly investigated, with different studies describing CIMT as equally a good and poor predictor of future adverse CV events. In the United States, the Intersocietal Accreditation Commission (IAC) has developed standards and methods for the evaluation of the quality of care delivered in vascular testing. From the *Faculty of Medical Sciences, Newcastle University Medical School, UK; †Institute of Cellular Medicine, Newcastle University, Newcastle upon Tyne, UK; and ‡Freeman Hospital, Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK. Disclosure: The authors have no conflicts of interest to report. This work was supported by the National Institute for Health Research (NIHR) Newcastle Biomedical Research Centre based at Newcastle-upon-Tyne Hospitals National Health Service (NHS) Foundation Trust and Newcastle University. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. Correspondence: Vijay Kunadian, MBBS, MD, FRCP, FACC, FESC, Institute of Cellular Medicine, Faculty of Medical Sciences, Newcastle University, 3rd Floor William Leech Building, Newcastle upon Tyne NE2 4HH UK. E-mail: vijay.kunadian@ncl.ac.uk. Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. ISSN: 1061-5377/16/2402-0070 DOI: 10.1097/CRD.0000000000000077 70 | www.cardiologyinreview.com In this review, the association of CIMT with CVD is explored. The potential for CIMT to be used as a predictor of future CV risk is assessed. Current literature on the role of CIMT in predicting CV outcomes is reviewed, to determine whether it is a predictor of CV events, both in the general population and in high-risk groups such as those with HTN, diabetes mellitus (DM), and chronic kidney disease (CKD). METHODS The literature review was conducted on PubMed, NICE evidence, and Medline using the following search terms: “acute coronary syndrome,” “atherosclerosis,” “arterial stiffness,” “carotid intima media thickness,” “coronary artery disease,” “cardiovascular disease outcomes,” “myocardial infarction,” and “future cardiac risk.” Studies assessing the relationship between CIMT and CV events were included. First, we searched for research that assessed the “use of carotid intima media thickness in cardiology.” Second, we searched for studies investigating the “relationship between carotid intima media thickness and cardiovascular events.” Third, we evaluated the “role of carotid intima media thickness in predicting cardiovascular outcomes,” both in the general population and in high-risk groups. References for all included studies were also searched and evaluated. UTILITY OF CIMT IN THE PREDICTION OF ADVERSE EVENTS IN THE GENERAL POPULATION Previous studies suggest that CIMT is a good predictor of future adverse CV events (Fig. 1). In addition to being a noninvasive measurement, CIMT has no known adverse biological effects, which may enable it to be used in studies including young populations. CIMT is reproducible and quick to use2 and can be used to assess CV risk in terms of disease progression and regression. CIMT was first described as a predictor of future CV events in a study based on the Rotterdam Cohort.3 A sample of 1683 subjects from the Rotterdam Study (7983 subjects) was cross-sectionally assessed by measuring CIMT, among other variables such as the presence of plaque, BMI, and cholesterol levels, to estimate the absolute risk of coronary artery disease (CAD) within 10–12 years for each participant.3 The 10-year absolute risk of CAD rose by 3.7% per 0.15-mm increase in CIMT. The subsequent risk of death increased by 10.5% per 0.15-mm increase in CIMT within a 11.5-year period. This study demonstrated that, when viewed cross-sectionally, CIMT is a marker of risk of CAD and death within 10–12 years. The results were detected when a significant level of stenosis was absent, suggesting that CIMT could help predict and detect the risk of CV events earlier than other more traditionally used measurements. Lorenz et al4 followed 37,197 subjects for a mean period of 5.5 years, demonstrating that an increase in CIMT of 0.1 mm increased the future risk of myocardial infarction (MI) by 10–15% and stroke by 13–18%. Supplementing this finding, another study examined CIMT in relation to future risk of MI and stroke in 4476 subjects with a mean age of 72.5 years with no history of CVD.5 After a median follow-up of 6.2 years, participants in the higher quintiles of maximal CIMT had Cardiology in Review • Volume 24, Number 2, March/April 2016 Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Cardiology in Review • Volume 24, Number 2, March/April 2016 CIMT and Cardiovascular Disease FIGURE 1. Carotid intima media thickness. A, Normal CIMT; (B) CIMT measurement; (C) diffuse thickening of intima media; and (D) atheroma in the carotid bulb. an increased relative risk (RR) for MI or stroke compared with those in the lower quintiles. A linear increase in RR of MI or stroke was apparent across all quintiles, with the highest risk evident in the highest quintile compared with the lowest risk in the lowest quintile.5 In the Carotid Atherosclerosis Progression Study (CAPS),6 5056 subjects had CIMT measurements and were followed up for MI, stroke, and death over an average of 4.2 years. An increased unadjusted hazard ratio (HR) for CIMT was found for all outcomes, and following modification for age, sex, and vascular risk factors, CIMT was predictive for MI (HR, 1.16; 95% confidence interval [CI], 1.05–1.27) and for MI, stroke, or death (HR, 1.16; 95% CI, 1.05–1.28). In a 10-year cohort study of over 5000 participants living in Malmo, Sweden, CIMT, carotid plaque, and carotid stenosis were associated with future adverse CV outcome (ST elevation MI and non-ST elevation MI or death).7 These relationships persevered after correction for the risk factors (0.15-mm increase in CIMT HR 1.23; 95% CI, 1.07–1.41). In the Kuopio Ischaemic Heart Disease Study, 1288 Finnish men were followed for 2.5 years, where an increase in CIMT by 1 mm or more demonstrated a 2.2-fold increased risk of MI.8 In another study (Atherosclerosis Risk in Communities [ARIC]) 15,792 subjects aged 45–65 years were monitored across 4 communities in the United States for 4–7 years after carotid ultrasound. It was found that an increased CIMT was associated with an increased risk of CAD (HR of 1.13 for MI per 0.1-mm increase in CIMT).9 The Cardiovascular Health Study observed 5888 adults aged ≥65 years for © 2015 Wolters Kluwer Health, Inc. All rights reserved. CV events for up to 12 years; 5020 of the subjects had no previous history of CVD.10 It was demonstrated that the risk of CV adverse outcome increased on migrating from low to high CIMT values. The highest third had an 84% increased risk of CVD and a twofold increased risk of death because of CVD.10 The Individual PROGgression of carotid Intima media Thickness as a surrogate of vascular risk (PROG-IMT Project) evaluated CIMT in a population of 36,984 subjects with the following inclusion criteria: individuals who had at least 2 CIMT assessments and a clinical follow-up after the second ultrasound with records of any MI, stroke, and death.11 Participants were followed up for a mean of 7 years. The mean CIMT was found to be associated with CV risk (HR, 1.16), but the study as a whole discovered no association between CIMT progression and CV risk. This suggested that a one-off baseline CIMT measurement can help predict future adverse CV events, with CIMT progression not as effective, therefore limiting the use of this technique for CV screening.11 UTILITY OF CIMT IN THE PREDICTION OF ADVERSE EVENTS IN HIGH-RISK GROUPS Increased CIMT occurs in relation to various CV risk factors, including HTN, smoking, hypercholesterolemia, and DM.12 Furthermore, an increased CIMT has been linked to future MI/CV death and can be used as a screening tool for CV risk in high-risk patients beyond information from recognized risk factors.12 www.cardiologyinreview.com | 71 Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Cardiology in Review • Volume 24, Number 2, March/April 2016 Carpenter et al In Patients With Vascular Risk Factors In Patients With Diabetes Mellitus A longitudinal cohort study performed in 7 centers across 5 European countries recruited 3482 participants with a median age of 64.1 years. The cohort consisted of individuals with ≥3 vascular risk factors (47.8% men) who were observed over 21.5 months.13 The aim was to investigate whether measures of CIMT progression were associated with subsequent risk of adverse CV events. During this time, 129 subjects experienced a first vascular event, and all CIMT measurements showed significant progression during the first 15 months (P < 0.001), but only those with maximal progression (>1.5 mm) were significantly associated with the risk of future CV events.13 This study demonstrated that large increases in CIMT, in contrast to other progression variables, could be associated with CV risk. CVD is the main cause of death in patients with type 2 DM (T2DM).17 Identifying patients with a high probability of developing CV complications is therefore important for early prevention and intervention, which could reduce their morbidity and mortality. A recent review demonstrated that people with T2DM have a higher CIMT than comparable non-diabetic people, with an average estimated difference of 0.13 mm after correction for risk factors, such as age, risk of MI, and stroke.17 Another study on 150 subjects with DM revealed a link between CIMT and CVD determined by CT coronary angiography. Those with normal coronary arteries had the lowest CIMT measurements (mean of 0.58 mm) and those with coronary stenosis had the highest CIMT values (mean of 0.75 mm).12 A retrospective study assessed the relationship of CIMT progression with the risk of future CV events in 342 Japanese subjects with T2DM who had no medical history of CV events.18 With at least 2 CIMT measurements carried out, these patients were followed for a mean period of 7.6 years: 27 coronary events were recorded, with a coronary event defined as a MI, unstable, or stable angina. Analysis using the Cox proportional hazard model identified CIMT progression as a strong predictor of future CV events (HR, 2.24; P < 0.01). Kaplan-Meier curves were also used in the multivariate analysis showing a significantly higher rate of CV events in patients with high CIMT progression (>0.03 mm) compared with those with low CIMT progression (<0.01 mm). In addition, those with an initial high CIMT baseline (>1.1 mm) who later had a high CIMT progression were shown to be at a substantial risk of future adverse CV outcomes (HR, 5.89; P < 0.001) compared with those with a low initial CIMT baseline (<1.1 mm).18 In Patients With Prior CVD The Rotterdam Study determined the influence of CIMT in predicting future CAD in 374 subjects with a previous stroke or MI history, aged 55 years and above, who were followed up over a mean period of 4.2 years.14 These subjects were evaluated to see whether CIMT contributed to the prediction of a new MI. Receiver operating characteristic (ROC) curves were used to measure the prognostic value of the traditional risk factors added to the CIMT measurements. The ROC area with age and sex was 0.65 (95% CI, 0.62–0.69). Risk factors included previous MI, stroke, DM, smoking, systolic blood pressure (BP), diastolic BP, total, and HDL cholesterol levels, which augmented the ROC area from 0.65 to 0.72 (95% CI, 0.69–0.75). When CIMT was added to the previous model, the ROC area increased to 0.75 (95% CI, 0.72–0.78). Data from the Second Manifestations of ARTerial Disease study (SMART), a prospective cohort study following patients with pre-existing arterial disease, have demonstrated that CIMT can aid in the prediction of new vascular events.15 Patients (n = 2374), primarily male (76%) with a mean age of 60 years, were studied over a period of 2.8 years. CIMT values ranged from 0.36 to 4.52 mm, with a mean of 0.95 mm. Of the initial cohort, 225 patients experienced a new CV event (MI, unstable angina, or stable angina), with 125 of those dying from it. An increase in CIMT was related to an increased risk of future CV events (HR, 1.18; 95% CI, 1.04–1.32). The risk of stroke (RR, 1.35; 95% CI, 1.16–1.59) associated with an increase in CIMT was higher in comparison with RR in association with CV events (RR, 1.19; 95% CI, 1.02–1.38). The value of age-normalized CIMT in predicting future adverse CV events was evaluated in the University of Virginia Study16 where CIMT was measured in 727 patients with an intermediate risk of atherosclerosis, who ranged from age 16 to 85 years, with an average age of 57.5 years. Of those patients, 706 were followed up over a mean period of 4.78 years to determine clinical CV outcomes, with their details entered into a database where age-specific quartiles and odds ratios (ORs) in relation to CIMT were calculated. Twenty patients had major adverse CV events: 7 patients had MI with another 7 requiring revascularization. Carotid bulb and internal carotid artery (ICA) intima media thickness (IMT) measurements were considerably higher in patients who experienced a CV event compared with those who did not. The OR for future adverse CV outcomes was 5.8 (95% CI, 1.3–26.6) in the highest quartile compared with the bottom quartile in relation to CIMT measurements. Similar results were seen with ICA IMT (P =0.03) with the OR for future CV events being 7.4 when comparing highest with lowest quartile in terms of thickness.16 However, the limitations of this study include small sample size in comparison with other studies based on CIMT. Therefore, further investigation using larger sample sizes could improve the reliability and validity of CIMT findings. 72 | www.cardiologyinreview.com In Patients With Chronic Kidney Disease Given CVD is a leading cause death in patients with CKD, it is important to evaluate the possible links between CIMT and the future risk of poor CV outcomes in this category of patients.19 The increased risk of CV death may be due to progressive atherosclerotic vascular changes, which can be assessed by CIMT. CIMT was increased in patients with CKD (mean 0.81 mm), particularly those who have concomitant DM.19,20 A prospective cohort study examined whether CIMT could predict CV mortality in patients with CKD.19 Subjects with CKD (n = 438) who were treated with hemodialysis had their CIMT measured by B-mode ultrasound. They were followed up over 30 months, during which time there were 82 deaths and 44 others who experienced CV events, including MI, abdominal aortic aneurysm, and cerebral hemorrhage. Subjects with a range of CIMT values were compared (<1.0 mm, 1.0–2.0 mm, >2.0 mm). Those with severe CIMT (>2.0 mm) had a significantly greater risk of CV-related death (P < 0.0001). Another study aimed to determine the predictive value of CIMT and indicators of arterial stiffness, such as aortofemoral pulse wave velocity [PWV (a-f)], with CVD outcomes in CKD patients. The study consisted of 315 subjects with stage 4 to 5 CKD, aged 24 to 79 years, with a mean follow-up of 3.6 years.21 During this follow-up, 95 CV events occurred, and through analysis by the Cox proportional hazard model, it was found that mean maximum CIMT and PWV (a-f) were predictive of these CV events. However, after adjustment for age, sex, BP, and risk factors such as DM, cholesterol level, and smoking, PWV (a-f) was shown to be an independent predictor of CV events, whereas CIMT was not. The higher prevalence of CV risk factors in the CKD population could overshadow any independent role exhibited by CIMT as CIMT does not replicate the complex arterial processes and mechanisms that can lead to CV events in CKD patients.21 In Patients With Hypertension Zielinski et al22 examined CIMT as a marker of CV risk in high-risk patients with existing HTN and CAD, to determine the risk © 2015 Wolters Kluwer Health, Inc. All rights reserved. Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Cardiology in Review • Volume 24, Number 2, March/April 2016 of future CV events. Subjects (n = 297) with a mean age of 57 years were followed up for a mean of 41 months: 99% of the patients with a low CIMT (<1.13 mm) survived for 5 years compared with 78% of those with a high CIMT (>1.13 mm; P < 0.001). In those with low CIMT, event-free survival was 95% compared with 74% in subjects with high CIMT (P < 0.008), indicating that CIMT is a predictor of death and CV events in patients with HTN and CAD. These results highlight the possibility of using this method for CV risk, and even though these patients were on optimal medical therapy for high BP and cholesterol, increased CIMT could still be detected. However, it must be noted that there were limitations to these findings. A sample size of <300 using consecutive patients receiving coronary angiography is not representative, as it was not a random sample. The followup period was short in duration with the cutoff value for high CIMT arbitrary and not necessarily used in other studies. UTILITY OF CIMT IN THE PREDICTION OF SEVERITY OF ATHEROSCLEROSIS Forty-five subjects (41% female) with a mean age of 61.4 years underwent a neck computed tomography scan to determine the magnitude of atherosclerotic disease present, followed by CIMT analysis using B-mode ultrasound.23 The results were initially categorized for the presence or absence of carotid calcification, with approximately 50% of the sample having a diagnosis of HTN or hypercholesterolemia. The average CIMT in the right common carotid artery (CCA) was 0.95 mm for those with calcification present compared with 0.86 mm in those with no calcification (P = 0.14), whereas the average CIMT in the left CCA was 0.95 mm for those with calcification compared with 0.75 mm in those without (P < 0.01). Mean CIMT was 0.91 mm with the median total carotid calcium score being 48.4. The mean CIMT was 0.14 mm greater in subjects with carotid calcification, with a 0.05-mm increase in the CIMT associated with a 3 times higher risk of the presence of atherosclerosis.23 A significant correlation between CIMT and atherosclerosis was demonstrated in this study with the extent of calcification expressively associated with CIMT after adjustment for age. In addition, an increase in CIMT of 0.05 mm was associated with an increased risk for the presence of calcification. An increase in sample size would have provided additional validity and reliability to the results. CIMT AS A SCREENING TOOL IN CARDIOVASCULAR PREVENTION Subjects from Spain (n = 325) over 30 years of age with low or intermediate CV risk had their CIMT and subsequent 10-year risk of CVD calculated in comparison with a reference population of French citizens with a low CV risk.24 It was found that 18.4% of subjects had CIMT values higher than the 75th percentile of the reference population, indicating subclinical atherosclerosis which was not detected by traditional CV risk factors, such as BP, age, BMI, and a previous history of hypercholesterolemia. The percentage detected by B-mode ultrasound demonstrates that CIMT improves the stratification of risk in relation to future CV events by highlighting its potential use in detecting subclinical atherosclerosis. However, one particular limitation was that there were no CIMT reference values available in Spain; the CIMT reference values used were those of the population of France, with the study assuming both regions would have the same level of CV risk, which cannot yet be proven because of the aforementioned lack of data.24 IS CIMT A SOLITARY PREDICTOR OF CARDIOVASCULAR EVENTS OR BETTER WITH ADDITIONAL RISK SCORES? The American Heart Association currently advises that CIMT should be included in the assessment of atherosclerotic risk.25 Solitary © 2015 Wolters Kluwer Health, Inc. All rights reserved. CIMT and Cardiovascular Disease CV risk factors have a limited capacity to predict the progression of CVD, but risk stratification can be improved by integrating risk factors into models of risk, such as the Framingham risk score.26 CVD, which has a relatively prolonged asymptomatic phase, has been in need of fresh ways to categorize the stages of arterial disease from subclinical to clinical form. Presently, CVD risk is evaluated by using the Framingham or Systematic Coronary Risk Evaluation (SCORE) risk scores based on an individual’s lipids, BP, and smoking results, with those who score poorly at a higher risk of CV complications and treatment.27 Whether CIMT as a predictor of future adverse CV events is better when added to such predictive scores, or is more useful as a solitary biomarker, is examined below. Framingham Offspring Cohort Study In total, 2965 members of the Framingham Offspring Cohort Study had their CIMT measured and their CV outcomes evaluated over a 7-year period.28 Of those participants, 296 had a CV event (MI, angina, or stroke) with risk factors from the Framingham Score predicting this (C statistic of 0.748). A tool called “net reclassification” was used, where reclassification assigned those in whom CVD developed to a higher risk category and those in whom CVD did not develop to a lower risk category. The net reclassification index also acknowledges movement between categories in the reverse direction than predicted (high to low risk). Reclassifying these scores to include the intimal thickness of the ICA and CCA showed an increase in net reclassification index of 7.6% with the ICA (P < 0.001) but not with CIMT (0%, P = 0.99), showing that only ICA IMT improves the classification of CV risk when added to the Framingham Score.28 CIMT is safe, causing no radiation exposure, and is relatively inexpensive. With results from CIMT measurements being highly reproducible, it can be used as an independent predictor of CV events. In addition, CIMT can add supplementary information to established risk assessment processes such as the Framingham Score.29 The Paroi Arterielle et Risque Cardiovasculaire Study This study based on 6416 patients demonstrated that despite a large amount of similarity between the Framingham Risk Score and CIMT, there was a significant variation in one parameter, suggesting that CIMT provides supplementary information to the Framingham Risk Score.30 CIMT measurements were performed along with the Framingham score for each individual, and a significant positive correlation was found between CIMT and all components of the Framingham score (P < 0.005). For example, a Framingham score of 20 was matched with a CIMT value of 0.9 mm, with Framingham risk score increasing as CIMT increased, suggesting that CIMT provides information to complement the Framingham score.30 The Multi-Ethnic Study of Atherosclerosis The Multi-Ethnic Study of Atherosclerosis (MESA) aimed to determine whether CIMT could provide additional prognostic information to traditional risk scores such as Framingham, to predict future adverse CV events.31 Subjects aged 45 to 84 years who had no history of CVD were monitored for 5.3 years. The data were collected using ROC curves, showing a value of 0.77 for risk factors alone (HTN and plaque presence) and a value of 0.78 for CIMT added to the risk factors, demonstrating that adding CIMT to risk factors did not significantly enhance the prediction of CV disease.31 The Strong Heart Study Studies examining the prognostic value of CIMT in predicting future CV risk have not always assessed CIMT and the presence of plaques separately. A plaque is a direct demonstration of the presence of atherosclerosis, whereas CIMT is thought to be a measure of early atherosclerosis. Because of this discrepancy, the Strong Heart Study aimed to assess the individual prognostic value of CIMT and plaque www.cardiologyinreview.com | 73 Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Cardiology in Review • Volume 24, Number 2, March/April 2016 Carpenter et al progression in a population with widespread HTN and DM.32 Subjects (n = 2441) with no history of CVD and a mean age of 63 years were followed up for a mean period of 7.7 years: 65% of the participants were female, with a mean BMI of 31.3 kg/m2. The prediction of CV events was assessed by the presence and extent of atherosclerosis, along with the CIMT. Of the 2441 subjects, 495 (20.3%) experienced a CV event [101 MIs, 204 CAD (defined as presence of atheroma), 98 strokes and 98 with congestive heart failure] with 21.4% of these events leading to death. Both CIMT and the presence of plaques were strongly associated with the prediction of stroke, but CIMT showed a weak correlation in predicting future CV risk in those with HTN and DM. In fact, CIMT was only predictive of CV outcomes in those without CV risk factors present.32 However, there are some limitations to the Strong Heart Study. CIMT was only measured in the distal section of the CCA, and not the ICA or the bifurcation, and the study consisted of a specific patient group (American Indians) and therefore cannot be generalized to other populations. LIMITATIONS OF CIMT Despite the plethora of data providing evidence for the effectiveness of CIMT as a marker for CV events, there are some limitations of CIMT that need to be highlighted. Along with the extent of the atherosclerosis, the existence or absence of lesions with a necrotic core might be reflected upon as a key indicator of future risk.33 CIMT measurements do not distinguish between normal tissue and a necrotic core. Thus, measurements of the plaque composition are generally thought to be better predictors of atherosclerotic disease rather than CIMT.34 However, it needs to be realized that CIMT and plaque do not necessarily reflect the same stage of the atherosclerotic disease process. CIMT abnormalities could be seen in early atherosclerosis, when no plaques are present, and therefore be a valuable asset in assessing CV risk.34 IMT is generally acquired and measured in the CCA, but advanced atherosclerotic disease occurs predominantly in the ICA.33 Having a necrotic core indicates advanced disease, with a necrotic core defined as areas in which the extracellular matrix was lacking, causing loss of collagen and replacement by dead cellular debris.35 CIMT struggles to distinguish between a simple lesion and a necrotic core. This diagnostic investigation cannot tell how advanced the disease process is, and therefore how long the intimal thickening has been present, with the accuracy of CIMT being hindered by the fact that age-related thickening of intimal and medial layers of CCAs also occur in the absence of atherosclerosis.36,37 Carotid atherosclerosis occurs mainly in the bulb region, which is not easily visible with B-mode ultrasound.38 CIMT can also be viewed as crude in its measurements as it fails to show the complex process of plaque evolution. A plaque grows 2.4 times faster along the length of the carotid than it thickens, so CIMT may lack the sensitivity to detect plaque progression soon enough.38 The question remains whether a rise in CIMT corresponds to the level of atherosclerosis present. CIMT might simply reflect changes in vessel wall because of stress.39 B-mode ultrasound cannot distinguish between intima and medial layers. Pathological changes of medial and intimal hypertrophy of the CCA can occur in the absence of atherosclerosis, meaning there is potential for false-positive results and emotional distress for patients and their families, questioning the fact whether CIMT truly reflects the atherosclerotic process.40 CONCLUSIONS CIMT is used increasingly as a marker for atherosclerotic disease. Whether CIMT is useful in predicting CV risk is still open to debate. Currently, there is contradicting evidence that CIMT measurements improve CV disease prediction. Some evidence has indicated a 74 | www.cardiologyinreview.com relationship between CIMT and a future risk of adverse CV events, but this evidence is incomplete and requires further investigation. Methods for measuring CIMT differ among studies, which could account for the inconsistencies in published results. Most studies have reported results using the mean CIMT, with others using the mean maximum CIMT instead. These differences in methodology can limit the interpretation of results and until a standard unit of measurement for CIMT is agreed upon, discrepancies in findings may persist. The overall evidence has only suggested that CIMT is a modest predictor of future adverse CV events and not the revolutionary tool many had hoped. There is the need for CIMT to be tested, established, and reviewed in relation to traditional risk factors and high-risk populations. REFERENCES 1. Sibal L, Agarwal SC, Home PD. Carotid intima-media thickness as a surrogate marker of cardiovascular disease in diabetes. Diabetes Metab Syndr Obes. 2011;4:23–34. 2. O’Leary DH, Bots ML. Imaging of atherosclerosis: carotid intima-media thickness. Eur Heart J. 2010;31:1682–1689. 3. Bots ML, Hoes AW, Hofman A, et al. Cross-sectionally assessed carotid intima-media thickness relates to long-term risk of stroke, coronary heart disease and death as estimated by available risk functions. J Intern Med. 1999;245:269–276. 4. Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and metaanalysis. Circulation. 2007;115:459–467. 5. O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. 6. Lorenz MW, von Kegler S, Steinmetz H, et al. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke. 2006;37:87–92. 7. Rosvall M, Janzon L, Berglund G, et al. Incident coronary events and case fatality in relation to common carotid intima-media thickness. J Intern Med. 2005;257:430–437. 8. Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11:1245–1249. 9. Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. 1997;146:483–494. 10. Cao JJ, Arnold AM, Manolio TA, et al. Association of carotid artery intimamedia thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study. Circulation. 2007;116:32–38. 11. Lorenz MW, Polak JF, Kavousi M, et al; PROG-IMT Study Group. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet. 2012;379:2053–2062. 12. Robertson CM, Gerry F, Fowkes R, et al. Carotid intima-media thickness and the prediction of vascular events. Vasc Med. 2012;17:239–248. 13. Baldassarre D, Veglia F, Hamsten A, et al; IMPROVE Study Group. Progression of carotid intima-media thickness as predictor of vascular events: results from the IMPROVE study. Arterioscler Thromb Vasc Biol. 2013;33:2273–2279. 14. del Sol AI, Moons KG, Hollander M, et al. Is carotid intima-media thickness useful in cardiovascular disease risk assessment? The Rotterdam Study. Stroke. 2001;32:1532–1538. 15. Dijk JM, van der Graaf Y, Bots ML, et al. Carotid intima-media thickness and the risk of new vascular events in patients with manifest atherosclerotic disease: the SMART study. Eur Heart J. 2006;27:1971–1978. 16. Ali YS, Rembold KE, Weaver B, et al. Prediction of major adverse cardiovascular events by age-normalized carotid intimal medial thickness. Atherosclerosis. 2006;187:186–190. 17. Brohall G, Odén A, Fagerberg B. Carotid artery intima-media thickness in patients with type 2 diabetes mellitus and impaired glucose tolerance: a systematic review. Diabet Med. 2006;23:609–616. 18. Okayama KI, Mita T, Gosho M, et al. Carotid intima-media thickness progression predicts cardiovascular events in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract. 2013;101:286–292. © 2015 Wolters Kluwer Health, Inc. All rights reserved. Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Cardiology in Review • Volume 24, Number 2, March/April 2016 19. Nishizawa Y, Shoji T, Maekawa K, et al. Intima-media thickness of carotid artery predicts cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2003;41(3 suppl 1):S76–S79. 20. Szeto CC, Chow KM, Woo KS, et al. Carotid intima-media thickness predicts cardiovascular diseases in Chinese predialysis patients with chronic kidney disease. J Am Soc Nephrol. 2007;18:1966–1972. 21. Zoungas S, Cameron JD, Kerr PG, et al. Association of carotid intima-medial thickness and indices of arterial stiffness with cardiovascular disease outcomes in CKD. Am J Kidney Dis. 2007;50:622–630. 22. Zielinski T, Dzielinska Z, Januszewicz A, et al. Carotid intima-media thickness as a marker of cardiovascular risk in hypertensive patients with coronary artery disease. Am J Hypertens. 2007;20:1058–1064. 23. Allison MA, Tiefenbrun J, Langer RD, et al. Atherosclerotic calcification and intimal medial thickness of the carotid arteries. Int J Cardiol. 2005;103:98–104. 24. Aguilar-Shea AL, Gallardo-Mayo C, Garrido-Elustondo S, et al. Carotid intima-media thickness as a screening tool in cardiovascular primary prevention. Eur J Clin Invest. 2011;41:521–526. 25. Smith SC Jr, Greenland P, Grundy SM. AHA Conference Proceedings. Prevention conference V: Beyond secondary prevention: Identifying the high-risk patient for primary prevention: executive summary. American Heart Association. Circulation. 2000;101:111–116. 26. Law MR, Wald NJ. Risk factor thresholds: their existence under scrutiny. BMJ. 2002;324:1570–1576. 27. Wilson PW, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. 28. Polak JF, Pencina MJ, Pencina KM, et al. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–221. 29. Hurst RT, Ng DW, Kendall C, et al. Clinical use of carotid intimamedia thickness: review of the literature. J Am Soc Echocardiogr. 2007;20:907–914. 30. Touboul PJ, Vicaut E, Labreuche J, et al; PARC Study Participating Physicians. Correlation between the Framingham risk score and intima-media thickness: © 2015 Wolters Kluwer Health, Inc. All rights reserved. CIMT and Cardiovascular Disease 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. the Paroi Artérielle et Risque Cardio-vasculaire (PARC) study. Atherosclerosis. 2007;192:363–369. Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2008;168:1333–1339. Roman MJ, Kizer JR, Best LG, et al. Vascular biomarkers in the prediction of clinical cardiovascular disease: the Strong Heart Study. Hypertension. 2012;59:29–35. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. 2010;30:177–181. Peters SA, Grobbee DE, Bots ML. Carotid intima-media thickness: a suitable alternative for cardiovascular risk as outcome? Eur J Cardiovasc Prev Rehabil. 2011;18:167–174. Thim T, Hagensen MK, Wallace-Bradley D, et al. Unreliable assessment of necrotic core by virtual histology intravascular ultrasound in porcine coronary artery disease. Circ Cardiovasc Imaging. 2010;3:384–391. Spence JD. Technology Insight: ultrasound measurement of carotid plaque– patient management, genetic research, and therapy evaluation. Nat Clin Pract Neurol. 2006;2:611–619. Beere PA, Glagov S, Zarins CK. Experimental atherosclerosis at the carotid bifurcation of the cynomolgus monkey. Localization, compensatory enlargement, and the sparing effect of lowered heart rate. Arterioscler Thromb. 1992;12:1245–1253. Barnett PA, Spence JD, Manuck SB, et al. Psychological stress and the progression of carotid artery disease. J Hypertens. 1997;15:49–55. Glagov S, Vito R, Giddens DP, et al. Micro-architecture and composition of artery walls: relationship to location, diameter and the distribution of mechanical stress. J Hypertens Suppl. 1992;10:S101–S104. Stary HC, Blankenhorn DH, Chandler AB, et al. A definition of the intima of human arteries and of its atherosclerosis-prone regions. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1992;85:391–405. www.cardiologyinreview.com | 75 Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.