Haemolytic Anaemia(1)
advertisement

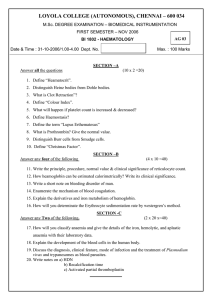
ANAEMIA – III Dr GangadharDr Vaishali Jain Classification of Anemia According to Underlying Mechanism Desired Learning Outcomes 1. 2. 3. 4. 5. 6. 7. Discuss aplastic anaemia in terms of etiopathogenesis, clinical features and investigations Briefly describe causes of pancytopenia Outline the diagnostic approach for normocytic anaemia Discuss pathogenesis of hereditory spheocytosis and G6PD deficiency anaemia Explain thalassemia in terms of pathogenesis, types clinical features and investigations Describe sickle cell anaemia with emphasis on pathogenesis, clinical features and investigations Explain etiopathogenesis and lab investigations for Paroxysmal nocturnal haemoglobinuria Lesson contents 1. 2. 3. 4. 5. 6. 7. 8. Aplastic anaemia: Etiopathogenesis, clinical features, investigations Pancytopenia: Causes Diagnostic approach for normocytic anaemia Hereditory spherocytosis G6PD deficiency anaemia Thalassemia: Pathogenesis, types, clinical features, investigations Sickle cell anaemia: Pathogenesis, clinical features, investigations Paroxysmal nocturnal haemoglobinuria(PNH): Etiopathogenesis, lab investigations APLASTIC ANEMIA • The bone marrow is “empty” (scattered lymphocytes and a rare hematopoietic precursor) and the blood shows pancytopenia (cells are of normal size and shape) • In bone marrow: No abnormal infiltrate (leukaemia) or increase in fibrous tissue • In blood : Not only an anemia, but a thrombocytopenia and neutropenia too…………..aplastic anaemia is misnomer Aplastic anemia : Etiology • • • • • • Idiopathic (50%) Drugs (Chloramphenicol, alkylating agents, antithyroid) Chemicals (Benzene, insecticides) Radiation; Pregnancy Viruses (CMV, EBV, hepatitis) Fanconi anemia (autosomal recessive, charecterized by defect in DNA repair leading to aplasia) Pathogenesis • • • • Affects quality or quantity of stem cells in bone marrow Defective haematopoietic microenvironment Deficiency of factors stimulating haematopoiesis Inhibition of hematopoiesis by immunological mechanisms Aplastic anemia : Clinical features • • • • Insidious onset Fatigue and tachycardia (from the anemia) Petechiae and bruising (from the thrombocytopenia) Infections (from the neutropenia) ** Lymph nodes, liver or spleen are not enlarged. If enlarged, diagnosis other than aplastic anaemia should be considered Aplastic anemia : Investigations • Peripheral blood examination: Any 2 of the following are diagnostic Hb < 10 gm/dl Neutrophil count <1,500/cmm Platelet count < 50,000/cmm • Normocytic normochromic red blood cells • Bone marrow examination: 1. Bone marrow aspiration: Dry tap Hypocellular marrow Erythroid and myeloid precursors and megakaryocytes – reduced Abundant lymphocytes and red blood cells 2. Bone marrow biopsy: Necessary for diagnostic confirmation Hypocellularity Fat cells and sparse haematopoietic element Bone marrow biopsy Fat cells Bony trabeculae Aplastic anaemia Aplastic anaemia: Bone marrow biopsy PANCYTOPENIA : CAUSES • Aplastic anaemia • Megaloblastic anaemia • Infiltration of bone marrow – leukaemia, lymphoma, storage disorders • Miliary tuberculosis • Hypersplenism Aplastic anaemia Vs Pancytopenia • Comparing a distinct disease (aplastic anemia) with a generalized blood finding (pancytopenia) • Pancytopenia is decrease in all cell lines (white cells, red cells, and platelets) in the blood • Pancytopenia indicates that something serious is going on in the marrow: Either the marrow isn’t making enough cells, or it’s so full of other stuff (like the fibrosis) Bone marrow biopsy : Fibrosis resulting in pancytopenia Fibrosis Bony trabeculae Diagnostic approach HAEMOLYTIC ANAEMIA HEREDITARY SPHEROCYTOSIS • Pathogenesis: Defective spectrin (a protein which attaches the red cell membrane to the cytoskeleton) The red cell membrane is unstable, leading to increased fragility and the formation of spherocytes, which get eaten by macrophages Hereditary Spherocytosis: Peripheral blood smear Normal RBCs Spherocytes • Morphology • Mild normochromic, normocytic anemia • Numerous spherocytes G6PD DEFICIENCY ANAEMIA • Pathogenesis: Glucose-6-phosphate dehydrogenase (G6PD) helps to reduce free radicals formed during cell metabolism Without G6PD, free radicals attack the molecular bonds between heme and globin, and globin becomes denatured, forming a little blob called a Heinz body The spleen bites out Heinz bodies, leaving bite marks in the cell Oxidizing substance (like a drug, or fava beans) triggers free radical formation G6PD deficiency anaemia :Peripheral blood smear Bite cell • • Schistocytes Bite cells(caused by recent pitting of Heinz bodies) Schistocytes (cell fragments) G6PD deficiency anaemia : Peripheral blood smear Bite cell THALASSEMIA Introduction Thalassemia is a quantitative abnormality of hemoglobin Haemoglobin structure Relative proportion of normal haemoglobin Adults Newborn HbA (α2β2) - 97%, HbA (α2β2) - 20% HbA2 (α2δ2) - 2.5% HbF (α2γ2) - 80% HbF (α2γ2) - 0.5% In healthy adult, • 2β genes encodes 2β globin chains • 4α genes encodes 2α globin chains Thalassemia • Pathogenesis: It is inherited single gene disorder characterized by quantitative decrease in one of the globin chains In α-thalassemia (deletion of α gene) - decreased amount of α chain—manifest in fetal and adult life In β-thalassemia (point mutation in β gene) - decreased amount of β chain – manifest in childhood and adult life • Problem: 1. Decreased hemoglobin production (as decrease in globin chains) 2. Excess unpaired α chains (in β thalassemia) or β, γ, and δ chains (in α thalassemia), which form tetramers and lead to premature red cell destruction β Thalassemia Type Genotype β -Thalassemia β/β+, β/β0 minor Anaemia RBC morphology Hb Clinical electrophoresis features Mild Hb A2>3.5%; Hb F < 10% Hb A- Normal Microcytic Hypochromic; Occ.Target cells; Basophilic stippling Asymptomatic β –Thalassemia Intermedia β -Thalassemia β0/β+, β0/β0 Severe Major (Cooley’s anaemia) Microcytic Hb A2 - Normal Hypochromic; Hb F = 10-95% Many target cells; Hb A- reduced Basophilic stippling; Many normoblasts; Severe anisopoikilocytosis Onset in infancy; Splenomegaly +++; Marked skeletal & facial changes; Transfusion dependent β Thalassemia major: Peripheral blood smear Normoblast Target cell β Thalassemia major: Peripheral blood smear β Thalassemia major : Clinical features Malar prominence Splenomegaly . • Malar prominence is due to erythroid hyperplasia in bone marrow • Splenomegaly due to extramedullary haematopoiesis β Thalassemia major : Radiological findings Erythroid hyperplasia in bone marrow result in, • Skull bones Separation of the table and thickening of the skull vault Bony trabeculae develop at right angles to the tables of the skull bone giving rise to ‘hair on end’/ ‘brush appearance’ Medulla - less dense • Tubular Bones of Extremities Corterx – thinned Medulla – less dense Widening of the marrow cavity α Thalassemia Type Silent carrier Genotype αα/α- α thalassemia α_/α_, trait αα/- - Hb H disease α-/- - Hydrops foetalis - -/- - Anaemia RBC Hb Clinical morphology electrophoresis features Absent None Absent/ mild Microcytic Hypochromic Moderate Microcytic Hypochromic; Target cells Severe Numerous erythroblasts Normal Asymptomatic Normal Asymptomatic Hb H (β4) Splenomegaly Hb Bart’s (γ4) Splenomegaly α Thalassemia: Clinical features Hydrops foetalis Thalassemia : Investigations • • • • Hb - reduced MCV; MCH – microcytic hypochromic RDW – normal (In IDA- RDW increased) Osmotic fragility test – red cells in thalassemia are resistant to osmotic lysis • Hb electrophoresis • X-ray – skull; long bones Prenatal diagnosis: • Chromatography – globin chain synthesis studies • Foetal DNA analysis – amniocentesis, chorionic villus biopsy SICKLE CELL ANAEMIA • Pathogenesis: Sickle cell anemia is a qualitative abnormality of hemoglobin It is a type of hemoglobinopathy (diseases with point mutations in one of the globin chain genes) The abnormal hemoglobin (called HbS) in sickle cell anemia changes shape when it releases oxygen The HbS molecules then aggregate and polymerize, forming the cell into a fragile, non-deformable, sickle shape . glutamic acid is replaced by valine at 6th position in the globin chains Sickle cells bust open more easily; they also stick together in small vessels, leading to ischemia (often occurring in hands, feet, lungs, and spleen) The spleen may undergo massive enlargement (due to red cell sequestration) in early childhood By early adulthood, however, the spleen is reduced to a small, fibrotic remnant (due to recurrent hemorrhage and fibrosis); this is called “autosplenectomy Sickle cell anaemia : clinical features Leg ulcer Dactylitis Sickle cell anaemia : Investigations Hb : reduced Peripheral blood examination ESR: low (inability of red cells to form rouleaux) Identification of HbS: 1. Sickling test Addition of reducing agent (2% sodium metabisulphite) triggers polymerisation of HBS 2. Hb electrophoresis 3. High performance liquid chromatography (HPLC) Sickle cell anemia : Periphral blood smear During crises (acute events) Sickle cells are seen in the peripheral blood After autosplenectomy (Post-splenectomy blood picture) - Nucleated red blood cells, - Target cells, - Howell- Jolly bodies, and - Increased platelet count Sickle cell anaemia Sickle cell Sickling test Peripheral blood smear Sickle cell anaemia : Peripheral blood smear Sickle cells Paroxysmal nocturnal haemoglobinuria (PNH) • Acquired haematopoietic stem cell disorder • Defective stem cells arise in case of aplastic anaemia • Stem cell in PNH give rise to RBCs, WBCs and platelets which are abnormally sensitive to complement • In PNH, cell membrane proteins (CD55, CD59) are deficient which normally inhibit lytic action of complement • Red cell destruction is more at night (as more complement is activated at night) so haemoglobinuria is observed in first voided urine in morning Paroxysma nocturnal haemoglobinuria (PNH) Laboratory investigations: Pancytopenia Reticulocyte count – increased Haemoglobinuria Haemosiderinuria Acidified serum test (Ham test) - acidification of serum activates complement and causes haemolysis of red cells Flow cytometric analysis of membrane proteins PNH: Investigations Mechanism of intravascular haemolysis Mechanism of extravascular haemolysis in macrophages