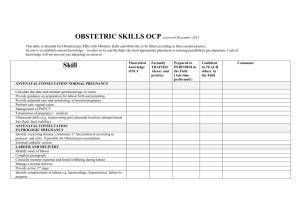
care of woman with abnormal pregnancy labour and puerperium
advertisement

THE UNITED REPUBLIC OF TANZANIA MINISTRY OF HEALTH, COMMUNITY DEVELOPMENT, GENDER, ELDERLY AND CHILDREN DIRECTORATE OF HUMAN RESOURCE DEVELOPMENT FACILITATOR’S GUIDE FOR ORDINARY DIPLOMA IN NURSING AND MIDWIFERY NTA LEVEL 6 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium © Ministry of Health, Community Development, Gender, Elderly and Children, Department of Human Resources Development Nursing Training Section 2018, Dodoma, Tanzania NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium ii Table of Contents Acronyms................................................................................................................................................. v Preamble ................................................................................................................................................ vi Acknowledgement ..................................................................................................................................vii Background ........................................................................................................................................... viii Rationale ............................................................................................................................................... viii Goals and Objectives of the Training Manual ......................................................................................... ix 1.1. Overall Goal for Training Manual ............................................................................................ ix 1.2. Objectives for Training Manual ............................................................................................... ix Introduction ............................................................................................................................................. ix 1.3. Module Overview .................................................................................................................... ix 1.4. Who is the Module For?........................................................................................................... x 1.5. How is the Module Organized? ................................................................................................ x 1.6. How Should the Module be Used? ......................................................................................... xi SESSION 1: CARE OF A WOMAN WITH ABORTION ............................................................................ 1 SESSION 2: CARE OF A WOMAN WITH ECTOPIC PREGNANCY ....................................................... 8 SESSION 3:CARE OF A WOMWN WITH HYDATIDIFORM MOLE ...................................................... 16 SESSION 4: CARE OF A WOMAN WITH BLEEDING IN LATE PREGNANCY .................................... 20 (ANTEPARTUM HAEMORRHAGE) ...................................................................................................... 20 SESSION 5:CARE OF A WOMAN WITH PLACENTA PREVIA ............................................................ 26 SESSION 6:CARE OF A WOMAN WITH ABRUPTIO PLACENTA ....................................................... 33 SESSION 7:CARE OF A WOMAN WITH UTI IN PREGNANCY ........................................................... 39 SESSION 8: CARE OF A WOMAN WITH MALARIA IN PREGNANCY ................................................ 44 SESSION 9: CARE OF A PREGNANT WOMAN WITH PULMONARY TUBERCULOSIS .................... 53 SESSION 10: CARE OF A PREGNANT WOMAN WITH SYPHYLIS .................................................... 58 SESSION 11 :CARE OF A WOMAN WITH ANAEMIA IN PREGNANCY .............................................. 62 SESSION 12: HYPERTENSIVE DISORDERS IN PREGNANCY .......................................................... 68 SESSION 13: PRINCIPLES OF CARE OF A WOMAN WITH PRE-ECLAMPSIA AND ECLAMPSIA ACCORDING TO GUIDELINES AND PROTOCOLS ............................................................................ 73 SESSION 14: CARE OF PREGNSNT WOMAN WITH DIABETES MELLITUS AND CARDIAC DISEASE ............................................................................................................................................... 82 SESSION 15:CARE OF A WOMAN WITH HYPEREMESIS GRAVIDARUM ........................................ 90 SESSION 16: CARE OF A WOMAN WITH DISORDERS OF AMNIOTIC FLUID (POLYHYDRAMIOUS AND OLIGOHYDRAMNIOS) ................................................................................................................. 94 SESSION 17:CARE OF A WITH ABNOMAL UTERINE ACTION .......................................................... 99 SESSION 18: CARE OF A WOMAN WITH PROLONGED LABOUR .................................................. 107 SESSION 19: CARE OF A WOMAN WITH OBSTRUCTED LABOUR ................................................ 112 SESSION 20:CARE OF A WOMAN UNDERGOING VACUUM ASSISTED DELIVERY AND CAESAREAN SECTION...................................................................................................................... 117 SESSION 21: CARE OF A PREGNANT WOMAN DURING INDUCTION AND AUGMENTATION OF LABOUR .............................................................................................................................................. 124 SESSION 22: CARE OF A WOMAN WITH PRETERM LABOUR ....................................................... 130 SESSION 23: CARE OF A WOMAN WITH PREMATURE RUPTURE OF MEMBRANE (PROM) ...... 135 SESSION 24: CARE OF A WOMAN WITH BREECH PRESENTATION ............................................. 140 SESSION 25: CARE OF A WOMAN WITH BROW PRESENTATION ................................................ 150 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium iii SESSION 26: CARE OF A WOMAN WITH FACE PRESENTATION .................................................. 156 SESSION 27: CARE OF A WOMAN WITH SHOULDER PRESENTATION ........................................ 162 SESSION 28: CARE OF A PREGNANT WOMAN WITH OCCIPITAL POSTERIOR PRESENTATION 172 SESSION 29: CARE OF A WOMAN WITH UNSTABLE LIE AND COMPOUND PRESENTATION .... 166 SESSION 30:CARE OF A WOMAN WITH MULTIPLE PREGNANCY ................................................ 180 SESSION 31: CARE OF A WOMAN WITH PUERPERAL SEPSIS ..................................................... 186 SESSION 32: CARE OF A WOMAN WITH PUERPERAL PSYCHOSIS ............................................. 191 SESSION 33: CARE OF A WOMAN WITH BREAST INFECTION AND MASTITIS ............................ 196 SESSION 34: CARE OF A WOMAN WITH UTERINE SUB-INVOLUTION ......................................... 200 SESSION 35:CARE OF A WOMAN WITH VENOUS THROMBOSIS IN PREGNANCY ..................... 205 SESSION 36: CARE OF A WOMAN WITH URINE INCONTINENCE ................................................. 211 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium iv Acronyms AGYW AIDS AIHA ARV VMMC WHO Adolescents Girl and Young Women Acquired Immune Deficiency Syndrome American International Health Alliance Antiretroviral Voluntary Medical Male Circumcision World Health Organization NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium v Preamble The Ministry of Health Community Development Gender Elderly and Children among other roles ensures that Tanzanians receive quality health care and service. This can be achieved through production of competent nurses and midwives amongst other health cadres. The training of competent nurses and midwives can be achieved through various teaching and learning materials; one of them being facilitator’s guides and student’s manual . Dr. Loishook Saitori Director for Human Resource Development Ministry of Health, Community Development, Gender, Elderly and Children NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium vi Acknowledgement Ministry of Health, Community Development, Gender, Elderly and Children through the Directorate of Human Resource Development, Nursing training section has reviewed Facilitator’s guide for Nursing and Midwifery training program. The review was informed by revised curriculum of the same. The successfully completion of this facilitator’s guide has been made possible by the commitment of the technical team through a series of writers’ workshops. Understanding the crucial role of the team, the Ministry would like to express sincere appreciation to all those who involved in the completion of this task. Special gratitude goes to coordinators of Nursing and Midwifery training, technical expert from NACTE and other facilitators who tirelessly supported the development of this guide whose names are listed with appreciation:- SN 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. FULL NAME Nassania Shango Professor Eliezer Tumbwene Ramadhani Samainda Dr. Patrick Mwidunda Lupyana Kahemela Joseph Pilot Mary Kipaya Paul Magessa Dominic Daudi Dr. Beatrice Mwilike Lilian Wilfred Upendo Mamchomy Tito William Sixtus Ruyumbu Dr Lenatus Kalolo Emmanuel Mwakapasa Salma Karim Athanas Paul Dr. Jiyenze Mwangu Kini Joseph Mayunga Elizabeth Kijugu Charles Magwaza Meshaki Makojijo Stellah Kiwale Evance Anderson Juliana Malingumu Rehema Mtonga Masunga Isassero Mbaruku Luga INSTITUON/ ORGANIZATION CDNT -MOHCDGEC-Dodoma Lecturer -Aga Khan University NACTE-Dodoma Program Manager-Amref Health Africa Program Officer-Amref Health Africa Program Officer- Amref Hhealth Africa Principal- Kahama School of Nursing Ag. Principal –Newala School of Nursing Tutor –Newala School of Nursing Lecturer-MUHAS Tutor KCMC School of Nursing Tutor KCMC School of Nursing Nurse Officer Muhimbili National Hospital Nurse Officer- Mbeya Refferal Medical Specialist-Mbeya Regional Refferal Principal Mbeya –OTM Tutor- Mirembe School of Nursing Principal- Mirembe School of Nursing Tutor –CEDHA Tutor- Kisare Principal-Kairuki School of Nursing Principal Njombe School of Nursing Tutor Bugando School of Nursing Tutor- PHN Morogoro Tutor Geita School of Nursing Tutor Mchukwi School of Nursing Tutor Assistant Lecturer –MUHAS Driver-Mirembe School of Nursing Lastly would like to thank the collaboration and financial support from Amref Health Africa who made this task successfully completed. Ndementria Arthur Vermand NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium vii Assistant Director Nursing Training Section, Ministry of Health, Community Development, Gender, Elderly and Children Background In 2015 the Ministry of Health, Community Development, Gender, Elderly and Children through the Directorate of Human Resource Development, Nursing training section started the process of reviewing the nursing curricula NTA level 4-6. The process completed in the year 2017 and its implementation started in the same year. The rationale for review was to comply with the National Council for Technical award (NACTE) Qualification framework which offers a climbing ladder for higher skills opportunity. Amongst other rationale was to meet the demand of the current health care service delivery. The demand is also aligned with human resource for health strategic plan and human resource for health production plan which aims at increasing number of qualified human resource for health. The process of producing qualified human resource for health especially nurses and midwives requires the plentiful investment of resources in teaching at the classroom and practical setting and the achievement of clinical competence is acquired in step wise starting from classroom teaching to skills laboratory teaching. In addition, WHO advocates for skilled and motivated health workers in producing good health services and increase performance of health systems (WHO World Health Report, 2006). Moreover, Primary Health Care Development Program (PHCDP) (2007-15) needs the nation to strengthen and expand health services at all levels. This can only be achieved when the Nation has adequate, appropriately trained and competent work force who can be deployed in the health facilities to facilitate the provisions of quality health care services. In line with the revised curricula, the MOHCDGEC in collaboration with developing partners and team of technical staff developed quality standardized training materials to support the implementation of urricula. These training materials address the foreseen discrepancies in the implementation of the curricula by training institutions. This facilitator’s guide has been developed through a series of writers’ workshop (WW) approach. The goals of Writer’s Workshop were to develop high-quality, standardized teaching materials and to build the capacity of tutors to develop these materials. The new training package for NTA Level 4-6 includes a Facilitator Guide and Student Manual. There are 33 modules with approximately 520 content sessions Rationale The vision and mission of the National Health Policy in Tanzania focuses on establishing a health system that is responsive to the needs of the people, and leads to improved health status for all. Skilled and motivated health workers are crucially important for producing good health through increasing the performance of health systems (WHO, 2006). With limited resources (human and nonhuman resources), the MOHSW supported tutors by developing standardized training materials to accompany the implementation of the developed CBET curricula. These training manuals address the foreseen discrepancies in the implementation of the new curricula. Therefore, this training manual for Certificate and Diploma program in Nursing (NTA Levels 4-6) aims at providing a room for Nurses to continue achieving skills which will enable them to perform competently. These manuals will establish conducive and sustainable training environment that will allow students and graduates to perform efficiently at their relevant levels. Moreover, this will enable them to aspire for attainment of higher knowledge, skills and attitudes in promoting excellence in nursing practice. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium viii Goals and Objectives of the Training Manual 1.1. Overall Goal for Training Manual The overall goal of these training manuals is to provide high quality, standardized and Competence-based training materials for Diploma in nursing (NTA level 4 to 6) program. 1.2. Objectives for Training Manual • To provide high quality, standardized and competence-based training materials. • To provide a guide for tutors to deliver high quality training materials. • To enable students to learn more effectively. Introduction 1.3. Module Overview This module content has been prepared as a guide for tutors of NTA Level 6 for training students. The session contents are based on the sub-enabling outcomes of the curriculum of NTA Level 6 Ordinary diploma in Nursing and Midwifery. The module sub-enabling outcome as follows: 2.1.1 Provide care to a pregnant woman with bleeding conditions due to abortion, ectopic pregnancy and hydatidiform mole according to standards 2.1.2 Provide care to a pregnant woman with Antepartum Haemorrhage (placenta praevia and abruption) according to guidelines and protocols 2.1.3 Provide care to a pregnant woman with Urinary Tract Infections (UTIs) and syphilis according to protocols and guidelines 2.1.4 Provide care to a pregnant woman with anaemia, cardiac diseases and diabetes mellitus according to standards and protocols 2.1.5 Provide care to a pregnant woman with Pulmonary Tuberculosis (PTB) and malaria according to protocols and guidelines 2.1.6 Provide care to a pregnant woman with disorders of amniotic fluid according to guidelines and standards 2.1.7 Provide care to a pregnant woman with hypertensive disorders of pregnancy according to guidelines and standards 2.1.8 Provide care to a pregnant woman with Hyperemesis gravidarum according to standards and guidelines 2.2.1 Provide care to a woman with abnormal uterine action according to standards and guidelines 2.2.2 Provide care to a woman with prolonged labour according to standards and guidelines 2.2.3 Provide care to a woman with obstructed labour according to standards and protocols 2.2.4 Provide care to a woman with precipitate labour according to standards 2.2.5 Conduct vacuum extraction delivery according to standards and guidelines 2.2.6 Provide care to a woman undergoing caesarean section according to standards and protocols 2.2.7 Provide care to a woman during induction, augmentation and trial of labour according to standards and guidelines NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium ix 2.2.8 2.3.1 2.3.2 2.3.3 2.3.4 2.3.5 2.3.6 2.3.7 2.5.1 2.5.2 2.5.3 2.5.4 2.5.5 2.5.6 Provide care to a woman with preterm labour and premature rupture of membranes according to standards Provide care to a woman with breech presentation according to standards Provide care to a woman with face presentation according to standards Provide care to a woman with brow presentation according to standards Provide care to a woman with shoulder presentation according to standards Provide care to a woman with unstable lie and compound presentation according to standards Provide care to a woman with occipital posterior position according to standards Provide care to a woman with multiple pregnancy according to standards Provide care to a woman with puerperal sepsis according to standards and guidelines Provide care to a woman with puerperal psychosis according to guidelines and protocols Provide care to a woman with breast infections according to guidelines and protocols Provide care to a woman with sub-involution of uterus according to guidelines and protocols Provide care to a woman with venous thrombosis according to guidelines and protocols Provide care to a woman with urine incontinence according to guidelines and protocols 1.4. Who is the Module For? This module is intended for use primarily by tutors of NTA Level 4 certificate and diploma in nursing schools. The module’ sessions give guidance on the time and activities of the session and provide information on how to teach the session to students. The sessions include different activities which focus on increasing students’ knowledge, skills and attitudes. 1.5. How is the Module Organized? The module is divided into 36 sessions; each session is divided into sections. The following are the sections of each session: Session Title: The name of the session. Learning Tasks – Statements which indicate what the student is expected to learn at the end of the session. Session Content – All the session contents are divided into steps. Each step has a heading and an estimated time to teach that step. Also, this section includes instructions for the tutor and activities with their instructions to be done during teaching of the contents. Key Points – Each session has a step which concludes the session contents near the end of a session. This step summarizes the main points and ideas from the session. Evaluation – The last section of the session consists of short questions based on the learning objectives to check the understanding of students. Handouts are additional information which can be used in the classroom while teaching or later for students’ further learning. Handouts are used to provide extra information related to the session topic that cannot fit into the session time. Handouts can be used by the participants to study material on their own and to reference after the session. Sometimes, a handout will have questions or an exercise for the participants. The answers to the questions are in the Facilitator Guide Handout, and not in the Student Manual Handout. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium x 1.6. How Should the Module be Used? Students are expected to use the module in the classroom and clinical settings and during self-study. The contents of the modules are the basis for learning Care of a Woman with Abnormal Pregnancy, Labour and Puerperium. Students are therefore advised to learn each session and the relevant handouts and worksheets during class hours, clinical hours and self-study time. Tutors are there to provide guidance and to respond to all difficulty encountered by students. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium xi SESSION 1: CARE OF A WOMAN WITH ABORTION Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define abortion State causes of abortion Explain the classifications of abortion Explain signs and symptoms of abortion Give care to a woman with abortion and MVA Explain complications of abortion Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 5 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 5 Brainstorming/presentation 3 10 Lecture discussion Definition of abortion Causes of abortion 4 20 Lecture discussion Classification of abortion 5 10 Presentation Signs and symptoms of abortion NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 1 6 45 Small group discussion/Lecture discussion Care of a woman with abortion and MVA 8 15 Lecture/discussion Complications of abortion 9 5 Presentation Key Points 10 5 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and LearningTasks (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Definition of abortion (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm and give a definition of abortion. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Abortion is defined as termination of pregnancy before 24 weeks of gestation or when the fetus weighs 500 g or less. In Tanzania, abortion is termination of pregnancy before 28 weeks of gestation or viability. STEP 3: Causes of abortion (10 Minutes) Chromosomal abnormalities: cause at least 50% of early abortions e.g. trisomy, monosomy X (XO) and triploidy. Blighted ovum (anembryonic gestational sac): where there is no visible foetal tissue in the sac. Maternal infections: e.g. treponema pallidum , listeria monocytogenes, mycoplasma hominis, ureaplasma urealyticum, chlamydia trachomatis, neisseria gonorrhoeae, streptococcus agalactiae, herpes simplex virus cytomegalovirus and toxoplasma gondii which causes abortion if there is acute infection early in pregnancy. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 2 Acute fever for whatever the cause can induce abortion. Trauma: external to the abdomen or during abdominal or pelvic operations. Endocrine causes: o Progesterone deficiency (causes abortion between 8-12 weeks). o Diabetes mellitus. o Hyperthyroidism. o Hypertensive disorders Drugs and environmental causes: e.g. quinine, ergots, severe purgatives, tobacco, alcohol, arsenic, lead, formaldehyde, benzene and radiation. Maternal anoxia and malnutrition. Immunological causes: e.g. systemic lupus erythematosus, antiphospholipid antibodies, isoimmunization Uterine defects e.g. Septum, Asherman's syndrome (intrauterine adhesions) and submucous myomas. Nervous, psychological conditions and over fatigue. Idiopathic. STEP 4: Classification of abortion (20 Minutes) The abortion can either be induced or spontaneous. Induced abortion Induced abortion is that abortion in which pregnancy was terminated intentionally. There are two types of induced abortion; criminal and therapeutic abortion. Spontaneous abortion Spontaneous abortion occurs without medical or mechanical means to empty the uterus. Others prefer the term miscarriage to mean spontaneous abortion. Classification of abortion Threatened abortion o If the blood loss is less than a normal menstrual flow and is not accompanied by pain of uterine contraction there is a reasonable chance for continuing pregnancy. This occurs in 50% of cases while other half will proceed to inevitable or missed abortion. Inevitable abortion o The patient complains of considerable bleeding and severe lower abdominal pain referred to the back. o On examination, the products of conception are felt through the dilated cervix. Incomplete abortion o Retention of a part of the products of conception inside the uterus. It may be the whole or part of the placenta which is retained. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 3 Complete abortion o All products of conception have been expelled from the uterus. Missed Abortion o Retention of dead products of conception for 4 weeks or more. Blighted ovum o Also called anembryonic pregnancy represents a failed development of the embryo so that only a gestational sac, with or without a yolk sac, is present STEP 5: Signs and Symptoms of Abortion (10 Minutes) The following table summarizes the signs and symptoms of abortion (columns) for each type of abortion (rows). Table 1.1: Signs and symptoms of abortion TYPE OF VAGINAL ABDOMINAL ABORTION BLEEDING PAIN CERVICAL DILATION TISSUE PASSAGE PREGNANCY TEST Threatened Slight Mild cramping No No positive Inevitable Moderate Moderate cramping Yes No positive Incomplete Heavy Severe cramping Yes Yes Positive Complete Decreased; slight Mild cramping No Yes Positive Missed None; slight None No No Negative Blighted ovum None; slight Mild cramping No No Positive NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 4 STEP 6: Care of a Woman with Abortion and MVA (45 minutes) Activity: Small Group Activity (20 minutes) DIVIDE students depending on the size of the class. ASK students to explain how to care for a woman with abortion, each group to explain the care of one category from these: Threatened abortion Inevitable abortion Incomplete abortion Complete abortion Missed abortion Blighted ovum ALLOW the groups to work together to come up with answers to the question above, focusing on their assigned category. GIVE students an example, if necessary. For example, say “Encourage the woman to rest in bed until one week after stoppage of bleeding”; “Advice the woman not to engage in sexual intercourse as it may disturb pregnancy by the mechanical effect and the effect of semen prostaglandins on the uterus.” ALLOW groups 10 minutes for this exercise. ASK students to report back the care plan per group. The following part of the presentation has more details on each of these categories. APPRAISE the students Care of a woman with abortion for each category PROVIDE feedback by summarizing the students’ answers Threatened abortion o Encourage the woman to rest in bed until one week after stoppage of bleeding. o Advice the woman not to engage in sexual intercourse as it may disturb pregnancy by the mechanical effect and the effect of semen prostaglandins on the uterus. o Give sedatives if the patient is anxious. o Medical treatment is usually not necessary but Progestogens: e.g. hydroxy progesterone is given by some if there is evidence of progesterone deficiency. o If bleeding stops, advice the woman to continue with follow-up in antenatal clinic. o Reassess the woman if bleeding recurs. Inevitable abortion NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 5 o Any attempt to maintain pregnancy is useless. o Resuscitation and oxytocin 10 IU is given by IV route to induce tetanic uterine contraction and stop bleeding. If pregnancy is less than 12 weeks: Termination is done by vaginal evacuation and curettage or suction evacuation under general anaesthesia. If pregnancy is more than 12 weeks: - Oxytocin is given by intravenous drip to expel the uterine contents. - If the placenta is retained it is removed under general anaesthesia. Counseling before and after the procedure is very important. Incomplete abortion o If pregnancy is less than 12 weeks: Evacuation is done by suction evacuation Manual Vacuum Aspiration under general anaesthesia. o If pregnancy is more than 12 weeks: evacuation by sharp curettage o Counselling and reassurance Complete abortion o No further medical intervention is required as the products of conception are completely expelled. o Mothers should be advised to seek advice if the bleeding recurs or pyrexia develops. o Counseling and follow-up. Missed abortion o The dead conceptus is expelled spontaneously in the majority of cases. o Evacuation of the uterus is indicated in the following conditions: spontaneous expulsion does not occur within four weeks there is bleeding infection or DIC developed patient is anxious. o It is important to check bleeding indices as this condition may complicate to DIC Blighted ovum o A blighted ovum eventually leads to abortion. o Counseling and reassurance o Manage accordingly Perform Manual Vacuum Aspiration(MVA) as evacuation to less than 12 weeks abprtion Reffer to Handout no1.1 STEP 7: Complications of Abortion (15 minutes) Severe bleeding that may eventually lead to shock, anemia, and renal failure Sepsis-septicaemia-infertility-ectopic pregnancy Depression that may result into marital disharmony Blood transfusion may predispose patient to HIV or hepatitis Uterine perforation Bowel injury Amniotic fluid embolism- DIC Bladder injuries RhD-sensitization Menstrual irregularities NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 6 STEP 8: Key Points (5 minutes) The abortion can either be induced or spontaneous. The term ‘miscarriage’ is used to describe spontaneous loss of pregnancy before 24 weeks Grieving is an essential part of the recovery process following abortion Bed rest will not prevent abortion Blood loss and pain associated with abortion can be profuse and profound and overwhelming for the mother Counseling and reassurance is very important for woman who has experienced abortion STEP 9: Session Evaluation (5 minutes) What is abortion? What are the causes of abortion? What are the signs and symptoms of abortion? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 7 Handout No 1.1 Step by Step in Performing MVA Step by Step in Performing MVA Ensure sterility Ensure that part of the instrument required to enter in the uterus is sterile. No part of tip of the tube should be allowed to touch the vaginal wall. Steps for performing MVA 1. Explain the procedure to the client. 2. Position the patient in lithotomy position. 3. Clean vulva and perineum with antiseptic e.g. savlon. 4. Drape patient with sterile towel . Perform bimanual pelvic examination to ascertain; Size, position of the uterus and extent of cervical dilatation. . . Insert bivalve speculum into the vagina and remove blood tissue from the vagina and cervical os using sponge holding forceps. . Clean vagina and cervix with povidone using gauze or cotton wool swabs. . Hold the anterior lip of the cervix using a single Tenaculum/volsellum at position 12 o’clock. . Select appropriate cannula according to the cervical os. . 10. Gently apply traction on cervix to straighten/align the cervical canal and uterine cavity. . Create vacuum in the syringe. . Gently insert the cannula into the uterine cavity while holding the cervix steady until it touches the fundus Note the depth by the dots visible on the cannula . Withdraw the cannula slightly . Attach the prepared syringe to the cannula by holding the end of the cannula in one hand and the syringe in the other hand; ensure the cannula is properly attached to the syringe. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 8 . Release the valve(s) on the syringe to transfer the vacuum through the cannula to the uterine cavity. . Evacuate the contents of the uterus by moving the cannula gently back and forth and rotating within the uterine cavity. . Check for signs of complete evacuation; . Red or pink form, . No more tissue in the cannula, . Gritty sensations, . The uterus contracts around the cannula. . 17. If the syringe is full with products of conception and no signs of complete evacuation close the valve, disconnect syringe from the cannula and empty the products. Repeat the evacuation procedure. 18. If there are signs of complete evacuation, close the valve, detach syringe from the cannula, withdraw syringe and remove the cannula. 19. Clean and inspect the cervix for bleeding, if there is bleeding apply pressure using a gauze for 5-10 minutes, then remove. . Give Oxytocin 10 IU IM or Ergometrine 0.2 mg IM or Misoprostol 600mcg orally. 20. remove the tenaculum/volsellum and speculum 20. Remove the patient from lithotomy position to rest for 10 to 20 minutes. 21. Inspect the tissue for product of conceptions, complete evacuation and molar pregnancy. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 9 SESSION 2: CARE OF A WOMAN WITH ECTOPIC PREGNANCY Total Session Time: 120 minutes Prerequisite :None Learning Tasks At the end of this session learner is expected to be able to: Define ectopic pregnancy State the risk factors for ectopic pregnancy Identify and explain the common sites for ectopic pregnancy Explain the sign ,symptoms and the diagnosis of an ectopic pregnancy Give care to a woman with ectopic pregnancy Explain the complications of ectopic pregnancy Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Content 1 05 Presentation Presentation of session title and learning objectives 2 05 Presentation Definition of ectopic pregnancy 3 10 Lecture/discussion Risk factors for ectopic pregnancy 4 35 Lecture /discussion Common sites for ectopic pregnancy 5 15 Presentation Sign , symptoms and the diagnosis of an ectopic pregnancy 6 30 Lecture/discussion Care of a woman with ectopic pregnancy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 10 7 10 Lecture/discussion Complication of ectopic pregnancy 8 05 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Definition of ectopic pregnancy (5 Minutes) An ectopic pregnancy is one where implantation occurs at a site other than uterine cavity. E.g. uterine tube, ovary, cervix and abdomen. o Common site (95%):the tubes. o Rare sites (5%):The ovaries, a rudimentary horn of a bicornuate uterus, broad ligaments, peritoneum and cervix. o In other words it is known as extra-uterine pregnancy STEP 3: Risk factors forectopic pregnancy (10 Minutes) Any alteration of the normal function of the uterine tube in transporting the gametes contributes to the risk of ectopic pregnancy; o Congenital abnormities of the tube. o Previous infections including Chlamydia, gonorrhea and pelvic inflammatory diseases o Previous pelvic surgery,particularly reconstructive tubal surgery o History of infertility or Assisted Reproductive Therapy (ART) o Failed sterilization i.e. Tubal ligation o Previous ectopic pregnancy o Uses of intrauterine contraceptive device o Smoking o Adjacent tumors especially in the broad ligament o Premature implantation of the fertilized ovum in the tube which may occur due premature shedding of the zona pellucida orPresence of ectopic endometrium in the tube. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 11 STEP 4: Common sites for ectopic pregnancy (35Minutes) Activity: Brainstorming (4 minutes) ASK students to outline the common sites of ectopic pregnancy ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Fallopian tube 95% (Tubal pregnancy) Cervix <2% Ovary < 2% Abdomen < 2% 1.1 A diagram showing the sites for ectopic pregnancy Tubal pregnancy o In tubal pregnancy, implantation can occur at any point along the tube, although the ampulla is the most common site, the isthmus is the next in frequency, and the interstitial site being the least common. o Tubal pregnancy can either be ruptured or unruptured Physiology of tubal pregnancy o The blastocyst rapidly erodes the epithelium and becomes attached to the muscle layer. o It grows and expands within the wall,distending the tube. o Maternal vessels are exposed and the pressure caused by the resultant blood flow can destroy the embryo. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 12 o The uterus increases in size and changes associated with early pregnancy occur in the body. o The endometrium undergoes some degree of change under the influence of hormones. o Vaginal bleeding associated with ectopic pregnancy is derived from degeneration of the decidua Outcome of tubal pregnancy o Tubal abortion The developing conceptus separate and is expelled through the fimbriated end of the uterine tube .this outcome is more common in ampullary implantation o Tubal mole Bleeding around the embryo results in its death, and then the blood clots around the conceptus enclosing it to form a mole, product retain in the tubes and may need to be removed. o Tubal rupture The wall is distended by the pregnancy and penetrated by the trophoblast to such an extent that it ruptures. This can be gradual or acute o Abdominal pregnancy Abdominal pregnancy o Is always the result of an early tubal pregnancy rupture or abortion into the peritoneal cavity. o The fertilized ovum makes the abdomen the site of its primary implantation. o The fetus develops within the peritoneal cavity but rarely survives o Pregnancy may proceed to term but very rare o The placenta remains attached to the uterine tube but expands and attaches neighboring organs Ovarian pregnancy o Is rare o Vaginal bleeding or sporting may be the presenting complaint. o Symptoms relate to rupture into the peritoneal cavity and are similar to those of tubal rupture. o On examination the midwife may palpate an enlarged ovary or ovarian mass which may or may not nor be painful. o Uterus may be slightly enlarged from endometrial response to progesterone and hCG . Cervical pregnancy o Is rare o Sign and symptoms include painless bleeding soon after the time of implantation. o Cervical mass may be palpated with distension and thriving of the cervical wall, partial dilation of the external cervical os. o Slightly enlarged uterine fundus. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 13 STEP 5: Signs, Symptoms and the diagnosis of ectopic pregnancy (15 Minutes) Sign and of ectopic pregnancy Typical sign and symptoms o Localised/abdominal pain o Amenorrhoea o Vaginal bleeding Atypical sign and symptoms o Shoulder pain o Abdominal distension o Nausea ,vomiting o Dizziness,fainting o Apyrexia Diagnosis of ectopic pregnancy o Careful history about last normal menstrual period(LNMP) its timing and appearance. o Always think of tubal pregnancy women with lower abdomen pain in whom there is possibility of pregnancy should be regarded as having an ectopic until proved otherwise o Ultrasound - the most reliable method of verification of ectopic pregnancy o Levels of β-hCG - more often levels are lower than in normal pregnancy o Laparascopy o Laparatomy STEP 6: Care a Woman with ectopic pregnancy(30 minutes) Nursing management PRE—OP& POST OP o If hemorrhage and shock present restore blood volume by the transfusion of red cells or volume expander o Or may give the woman normal saline IV and prepare for operation o Counsel the woman about her condition o The earlier diagnosis of tubal pregnancy has allowed a more conservative approach to management where the tube is less damage Medical Management o o o o o o Surgical Management Salpingostomy (incision in tube) hopefully to retain tubal function Salpingectomy (removal of tube) Open abdominal incision or laparoscopy (depending on stability of patient abdominal pregnancy they rarely reach term , and there delivery is by laparatomy For cervical pregnancy evacuation can be done. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 14 STEP 7: Complications of Ectopic pregnancy (10 minutes) Severe bleeding Sepsis Maternal death Recurrence of ectopic Infertility Shock Tubal rupture & organ damage Psychological STEP 8: Key Points (5 minutes) Ectopic pregnancy is a life threatening condition Women need prompt diagnosis and treatment Not all cases present with a classical picture Always suspect ectopic pregnancy in a woman of a child-bearing age with abdominal pain and/or per vaginal bleeding Information about ectopic pregnancy should be widely available and accessible to all social and cultural group STEP 9: Session Evaluation (5 minutes) What is ectopic pregnancy? What are the risk factors for ectopic pregnancy? State the common sites for ectopic pregnancy What are the signs and symptoms of ectopic pregnancy? How will you manageectopic pregnancy? What are the complications of ectopic pregnancy? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar esSalaam. Varny H. (2004) , Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666-667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 15 SESSION 3:CARE OF A WOMAN WITH HYDATIDIFORM MOLE Total Session Time: 60 minutes Prerequisite: None Learning Tasks At the end of this session a learner is expected to be able to: Define hydatidiform mole State the risk factors of hydatidiform mole Explain the types of hydatidiform mole Explain signs and symptoms of hydatidiform mole Explain the management of hydatidiform mole Explain complications of abortionhydatidiform mole Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Content 1 05 Presentation Presentation of session title and learning objectives 2 05 Presentation Definition of abortion 3 05 Lecture/discussion Risk factors of hydatidiform mole 4 10 Lecture/discussion Types of hydatidiform mole NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 16 6 05 Presentation Signs and symptoms of hydatidiform mole 7 15 Lecture/discussion Management of hydatidiform mole 8 05 Lecture/discussion Complications of hydatidiform mole 9 05 Presentation Key Points 10 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Definition of hydatidiform mole(5 Minutes) Hydatidiform mole is a benign neoplasm of the trophoblast often the precursor of choriocarcinoma It appears like a collection of hydropic vesicles STEP 3: Risk factors for hydatidiform mole (5 Minutes) Previous molar pregnancy Maternal age o Increasing in women under 20 and over 40 years old Ovular defect Nutritional deficiency STEP 4 : Types of hydatidiform mole (10 Minutes) Types of hydatidiform mole Complete mole: o The whole conceptus is transformed into a mass of vesicles hence contain no evidence of embryo. o It is the result of fertilization of anucleated ovum (has no chromosomes) with a sperm which will duplicate giving rise to 46 chromosomes of paternalorigin only. Partial mole: o A part of trophoblastic tissue only shows molar changes. o There is a fetus or at least an amniotic sac. o It is the result of fertilization of an ovum by 2 sperms so the chromosomalnumber is 69 chromosomes. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 17 STEP 5: Signs,symptoms and diagnosis of hydatidiform mole (5 Minutes) Sign and symptoms of hydatidiform mole Amenorrhea: usually of short period (2-3 months). Exaggerated symptoms of pregnancy especially vomiting Vaginal bleeding which is usually dark brown and may be associated with passage of vesicles and light pink or brown vaginal discharge due to rupture of the vesicles. Abdominal pain : may be , o dull-aching due to rapid distension of the uterus, o colicky due to starting expulsion, o Sudden and severe due to perforating mole. Pre-eclampsia develops in 20% of cases, usually before 20 weeks’ gestation. Hyperthyroidism develops in 10% of cases manifested by o Enlarged thyroid gland, o Tachycardia and elevated plasma thyroxin level. Diagnosis of hydatidiform mole On abdominal examination o The uterus is larger than the period of amenorrhea o The uterus is doughy in consistency Urine pregnancy test: is positive in high dilution. Serum b -hCG level: is highly elevated ( > 100.000 mIU/m1). Ultrasonographyreveals: o The characteristic intrauterine " snow storm" appearance STEP 7: Care of a Woman with hydatidiform mole (15 minutes) Resuscitate the woman with IV Ringers lactate or normal saline 3L or more Emotional support of this patient is very important. Vacuum aspiration or dilation and curettage is necessary if the mole does not abort spontaneously Hysteroctomy may be needed in a large mole to minimise and facilitate control of bleeding Hysterectomy may be considered to a woman older the 40 years of age to avoiddeveloping Choriocarcinoma Advice the woman to avoid o Getting pregnant during the follow up period o The use of intrauterine contraceptive device because of the risk of perforation and infection o The use of hormonal methods of contraception until the level of HCG have returned to normal NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 18 The woman should be couselled on the condition and to adhere to the follow up clinic. STEP8: Complication of hydatidiform mole Haemorrhage. Infection due to absence of the amniotic sac. Perforation of the uterus. Pregnancy induced hypertension Hyperthyroidism. Subsequent development of choriocarcinoma STEP 9: Key Points (5 minutes) Gestational trophoblastic disease is a general term covering both bening hydatidiform mole and choriocarcinoma. Choriocarcinoma is a malignant neoplasm which can develop as a consequence of a molar pregnancy. As soon as the diagnosis of vesicular mole is established the uterus shouldbe evacuated. Bleeding or blood stained vaginal discharge after a period of amenorrhea is the commonest symptom STEP 10: Session Evaluation (5 minutes) What is hydatidiform mole? What are the sign and symptoms of hydatidiform mole? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar esSalaam. Varny H. (2004) , Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666-667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 19 SESSION 4: CARE OF A WOMAN WITH BLEEDING IN LATE PREGNANCY (ANTEPARTUM HAEMORRHAGE) Total Session Time: 120 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define the term Antepartum Haemorrhage Explain the causes of Antepartum Haemorrhage Identify the classifications of Antepartum Haemorrhage Outline the signs and symptoms and Effects of APH Identify factors that aid in differential diagnosis in APH Explain the assessment of physical condition of the mother and foetus in APH Describe the care of a woman with APH Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning objectives 2 10 3 10 Brainstorming Lecture/discussion Lecture/discussion 4 10 Lecture/discussion Signs and Symptoms of Antepartum Haemorrhage 5 05 Lecture/discussion Factors that aid Differential Diagnosis in APH Definition of Antepartum Haemorrhage Classification of Antepartum Haemorrhage NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 20 6 10 Lecture/discussion Assessment of Physical Condition of the Mother and Fetus 7 60 Lecture/discussion Care of a Woman with APH Case study 8 05 9 05 Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Definition of Antepartum Haemorrhage (10 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the definition of Antepartum Haemorrhage (APH) ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Antepartum haemorrhage refers to bleeding from the vaginal tract in late pregnancy after the 24th week of gestation and before the onset of labour. This may place the life of the mother and unborn child at risk. STEP 3: Classification of Antepartum Haemorrhage (10 Minutes) Placental site bleeding o Placenta previa:Bleeding from separation of a placenta wholly or partially implanted in the lower uterine segment. o Abruptio placenta: Premature separation of a normally implanted placenta. o Marginal separation: Bleeding from the edge of a normally implanted placenta. Non-placental site bleeding NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 21 o o o o o Vasa previa: Bleeding from ruptured foetal vessels. Rupture uterus. Bloody show. Cervical ectopy, polyp or cancer. Vaginal varicosity. STEP 4: Signs and Symptoms of Antepartum Haemorrhage (10 Minutes) Table 4.1 Signs and Symptoms of APH Diagnosis Placenta previa Abruptio placenta Signs and symptoms always present Painless vaginal bleeding Painful vaginal bleeding (may be retained in the uterus) Intermittent or constant abdominal pain Signs and symptoms sometimes present Shock Bleeding may be precipitated by intercourse Relaxed uterus High presenting part Normal fetal condition Shock Tense/tender uterus Decreased/absence foetal movements Fetal distress or absence fetal sound Step 5: Factors that aid Differential Diagnosis in APH (5 minutes) Location of the placenta is the most critical information which will be needed to make a correct diagnosis, using ultrasound scans. Proper history taking Pain Onset of bleed, the amount of visible blood loss, colour of the blood Degree of shock Consistency of the abdomen Lie, presentation and the level of engagement Tenderness of the abdomen Audibility of the fetal heart Ultrasound scan Step 6: Assessment of Physical Condition of the Mother and Fetus (10 minutes) The midwife will assess the condition of the mother and fetus as follows: Maternal condition o The midwife will look for any pallor or breathlessness which may indicate shock NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 22 o She will weigh up the woman’s emotional state as she greets her and begins to ask for a history of events and remain calm. o She must generate the trust of both partners o Observation of pulse rate, respiration, blood pressure and temperature will be made and recorded. o The midwife must assess the amount of blood loss in order to ensure adequate fluid replacement. o She will discuss with couples how much has been lost earlier and ask to see all soiled articles, retained for doctor’s inspection. o Abdominal examination is made, observing for signs of labour. Fetal condition o The mother should be asked if baby is moving as much as normal o The midwife must attempt to auscultation of fetal heart and may use ultrasound apparatus to obtain the information Step 7: Care of the Woman wit Antepaturm Haemorrhage (60 minutes) A woman with APH can be managed as follows depending on the severity of bleeding. Mild bleeding o The women must be kept as quick as possible in a bed o Regular observation of the women’s condition o Obtain blood group and cross match and blood for full blood count o The midwife should try to distinguish the type whether placental abruption or placentaprevia o The diagnosis should be confirmed by an ultrasound scan Severe to moderate bleeding o Continue to monitor the maternal condition o Set up an intravenous infusion as soon as possible to treat shock o Draw blood for hemoglobin and grouping and cross match, if the HB is less than10mg/100ml a blood transfusion is to started immediately o Give analgesic or sedatives if necessary o Catheterize the patient and obtain midstream urine specimen o Administer oxygen to increase oxygen concentration in the maternal and fetalcirculation o Record intake and output chart o Note the blood loss and the paleness o Check fetal heart rate and movement every 10-15 minutes o Other subsequent management will depend on the definite diagnosis NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 23 Activity: Case Study (50 minutes) DIVIDE students in small manageable groups GIVE them the case study on Vaginal Bleeding in Later Pregnancy with clear instructions (20 minutes) ALLOW them time to present their responses for each group Refer Handout 4.1: Antepartum Haemorrhage key answer APPRAISE the students CLARIFY and summarize using the key answer Step 8: Key Points (5 minutes) Antepartum heamorrhage is a bleeding from the placental site due to premature separationof the placenta which occurs after 28thweeks of pregnancy and prior to the birth of thebaby and it is life threatening condition to both mother and fetus The major causes of bleeding in late pregnancy are placenta previa and premature separation of the placenta (abruptio placenta or placental abruption). Rapid assessment for and diagnosis of the cause of bleeding are essential to reduce maternal and perinatal morbidity and mortality. Step 9: Evaluation (5 minutes) What is antepartum haemorrhage? What are the signs and symptoms of Antepartum haemorrhage? What factors that aid in differential diagnosis in Antepartum haemorrhage? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13thed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14thed.). London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15thed.). London: Churchill Livingston. MOHSW. (2005). Advanced lifesaving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar esSalaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 24 Handout 4.1: Case study key answer for APH Bahati, who is 32 weeks pregnant, gravida three, has two healthy children. She has attended antenatal clinic regularly and all findings were within normal limits until her clinic visit 10 days ago. At that visit her blood pressure was noted to be 120/96 mm Hg; there were no other signs or symptoms of pregnancy-induced hypertension. Bahati was counselled about danger signs and what to do if they occur and asked to return to the clinic in two weeks. She presents herself at the health centre two days before her next visit, accompanied by her mother-in-law, with vaginal bleeding, abdominal pain and a bad headache. Initial Assessment o History, Physical Examination, Screening Procedures/Laboratory Tests) What will you include in your initial assessment of Bahati, and why? o Bahati and her mother-in-law should be greeted respectfully and with kindness. o They should be told what is going to be done and listened to carefully. o In addition, their questions should be answered in a calm and reassuring manner. o A rapid assessment should be done to check for the following signs to determine ifshe is in shock and in need of emergency treatment/resuscitation: rapid, weak pulse;systolic blood pressure less than 90 mm Hg; pallor; sweat or cold, clammy skin; rapidbreathing and confusion. o She should also be assessed to determine when vaginal bleeding started, the amountof blood lost, and whether the blood is bright and contains clots. o It will also be important to determine: When abdominal pain started (e.g., at the same time as vaginal bleeding) and thenature of the pain Whether foetal movement has been felt since the onset of bleeding and pain When headache started and whether there has been/is any visual disturbance(abruptio placenta can be associated with pregnancy-induced hypertension) What particular aspects of Bahati’s physical examination will help you make a diagnosisand identify her problems/needs, and why? o Palpation should be kept to a minimum, however, to avoid exacerbating thesymptoms. o An abdominal examination should be done to establish the location and nature ofpain, to feel the consistency of the uterus and check for guarding, and to detect foetalmovement (a tense/tender uterus and decreased foetal movements are signs ofabruptio attempt should be made to detect foetal heart sounds, which may be absentwith an abruption. What screening procedures/laboratory tests will you include (if available) in yourassessment of Bahati, and why? o No laboratory tests are required to make a diagnosis. However, an ultrasound scanmay be performed if possible to locate placenta if placenta previa is suspected. o Diagnosis (Identification of Problems/Needs) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 25 You have completed your assessment of Bahati and your main findings include thefollowing: o Pulse rate is 120 beats/minute and weak, o Blood pressure is 110/60 mm Hg. o Respiration rate is 20 breaths/minute o Temperature is 37º C. o Her skin is pale and sweaty. o Constant abdominal pain, o Uterus is tender on palpation, o Foetal heartbeat could not be heard. o Heavy vaginal bleeding containing some old clotted blood. o Coagulopathy was not detected. Based on these findings, what is Bahati’s diagnosis, and why? o Bahati’s signs and symptoms (e.g., signs of shock, constant abdominal pain, uterinetenderness, vaginal bleeding and absent foetal heart sounds) are consistent withabruptio placenta. o Care Provision (Planning and Intervention) Based on your diagnosis, what is your plan of care for Bahati, and why? o Bahati should be treated for shock immediately: Position her on her side. Ensure that her airway is open. Give her oxygen at 6–8 L/minute by mask or cannula. Keep her warm. Elevate her legs. Monitor her pulse, blood pressure, respiration and temperature. Start an IV using a large bore needle for rapid infusion of fluids (1 L of normal salineOr Ringer’s lactate in 15–20 minutes) SESSION 5:CARE OF A WOMAN WITH PLACENTA PREVIA Total Session Time: 120 minutes Prerequisites: None Learning Tasks At the end of this session learner is expected to be able to: Define placenta previa. Explain the physiology of placenta previa. Identify the degrees and causes of placenta previa. Outline the risk factors for placenta previa. Assess maternal and foetal condition of a woman with placenta previa. Describe the care of a woman with placenta previa. Outline the complications of placenta previa. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 26 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 5 Activity/ Method Presentation 2 10 Brainstorming/Presentation Content Presentation of session title and learning objectives 3 30 Lecture/discussion Definition and physiology of placenta previa Causes and degrees of placenta previa 4 10 Brainstorming Risk factors and indicators for placenta previa 5 20 Lecture/discussion 6 30 Lecture/discussion Assessment of maternal and foetal condition of a woman with placenta previa. Care of a woman with placenta previa 7 5 Presentation Complications of placenta previa 8 5 Presentation Key Points 9 5 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 27 STEP 2: Definition and Pathophysiology Of Placenta Previa (10 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the definition placenta previa. ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Definition o Placenta previa is the malposition of the placenta inthe lower uterine segment, either anteriorly or posteriorly. o The placenta is partially or totally attached to the lower uterine segment. Pathophysiology of Placenta Previa o The lower uterine segment grows and stretches progressively after the 12th week. o In later weeks this may cause the placenta to separate and severe bleeding can occur. o The bleeding is caused by shearing stress between the placental trophoblast and maternal venous blood sinuses. STEP 3: Causes and Degrees of Placenta Previa (30 Minutes) Causes of placenta previa It occurs in 0.5% of all pregnancy. It is more common in multgravida with an incidence of 1 in 90 deliveries and 1 in 250 deliveries in primigravida. The cause is unknown, but the incidence increase with advancing age and parity. It may be due to: o Low implantation of the blastocyst. o Development of the chorionic villi in the decidua capsularis o Leading to attachment to the lower uterine segment. o Large placenta as in twin pregnancy. Degrees of placenta previa The degree of placenta previa are classified into four types: o The 1stand 2nddegrees are marginal o The 3rddegree is partial placenta previa o The 4thdegree is total placental previa (see figure 5.1 below) Figure 5.1: Types of Placenta Previa NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 28 Type 1 Type 2 Type 3 Type 4 Source: https://www.ambulance.qld.gov.au/clinical.html (retrieved on 25th September 2018) Type 1 Placenta Previa o The large part of the placental tissue is situated in the upper uterine segment. o In this case vaginal delivery is possible, usually blood loss is mild and the mother and the fetus remains in good condition Type 2 Placenta Previa o The placenta is partially located in the lower uterine segment near the internal cervical os. o Vaginal delivery is possible particularly if the placenta is anterior. o Blood loss is usually moderate, although the conditions of the mother and fetus can vary, fetal hypoxia is likely to be present than maternal shock. Type 3 Placenta Previa o The placenta is located over the internal cervical os but not centrally. o Bleeding is likely to be severe particularly when the lower segment stretches and the cervix begin to efface and dilate in late pregnancy. o Vaginal delivery is inappropriate because the placenta preceded the fetus Type 4 Placenta Previa o The placenta is located centrally over the internal cervical os and torrential hemorrhage is very likely. o Vaginal delivery should not be considered. o Caesarean section is essential in order to save the life of the mother and fetus STEP 4: Risk factors and indicators for Placenta Previa (10 Minutes) Activity: Brainstorming (10 minutes) ASK students to brainstorm on the risk factors for placenta previa. ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 29 Risk factors for placenta previa Multiparity Maternal age greater than 35 Previous placenta previa Previous uterine surgery, including cesarean section (risk increases with increased number of cesarean sections) Multiple pregnancy (larger placenta covering the oss) Smoking (possible larger placenta) Indicators of placenta previa Painless per vaginal bleeding Non tender and tense uterus The fetal head remain unengaged in a primigravida There is malpresentation, usually breech The lie is transverse or oblique The lie is unstable, usually in a multigravida Localization of the placenta using ultrasonic scanning will confirm the existence of the placenta previa and establish it’s degree Step 5: Assessing the Maternal and Foetal Condition (20minutes) Assessing Maternal Condition The amount of vaginal bleeding is variable Some mother may have a history of a small repeated blood loss at intervals throughoutpregnancy whereas other may have a sudden episodes of vaginal bleeding after the 20thweek Severe hemorrhage occurs after 34th weeks of pregnancy The color of the blood is bright red denoting fresh blood All the blood loss should be quantified General Examination o If the bleeding is slight, the blood pressure, respiratory rate and pulse rate may be normal o In severe bleeding blood pressure is low and raised pulse rate due to shock o The degree of shock correlates with the amount of blood lost from the vagina o Rapid respiration. o The mother looks pale and her skin cold and moist. Abdominal Examination o The midwife may find the lie of the fetus is oblique or transverse and fetal may be highin primigravida near term o No pain felt by the mother during palpation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 30 NB:Vagina examination should never be performed because torrential hemorrhage may resultand worsen the situation Assessing the Fetal Condition Ask the mother if the fetal activity are normal In severe fetal hypoxia fetal movements may be diminished or ceased. An ultrasound fetal monitor such as cardiotocograph (CTG) may be used Pinard fetal scope may also be used If fetal hypoxia is marked medical assistance should be called urgently as this is anemergency condition If the facility has no services for resuscitation refer the woman immediately Step 6: Care of a Woman with Placenta Previa (30 minutes) The management depends on: o The amount of bleeding o The condition of the mother and the fetus o The location of the placenta o The stage of the pregnancy Conservative Management ( NURSING CARE) It is appropriate if bleeding is slight and the condition of the mother and fetus are well Keep the mother in hospital and rest the mother in bed until bleeding is stopped It is usual for the woman to remain in hospital for the rest of her pregnancy Monitor placental function by a means of fetal kick chart and antenatal CTG. Ultrasound scan to observe the position of the placenta in relation to the cervical os as thelower segment grows Insure physical, social and psychological support is important for those who are admittedfor some weeks If she have other children allow them to visit their mother regularly as they may beanxious Some occupational therapy are important to alleviate boredom in long stay to hospital The midwife, the obstetrician and the woman may plan for how the birth will bemanaged. Vaginal delivery is possible with type 1 and 2, unless the placenta is situated immediatelyabove the sacral promontory where is vulnerable to pressure from advancing fetal headand may impede decent Correct anemia with oral iron Ensure blood is available for transfusion Active Management Severe vaginal bleeding will necessitate immediate delivery by caesarean sectionregardless of the location of the placenta. Take blood for full blood count, cross matching and clotting studies. Blood transfusion may be needed to be transfused quickly, blood group O may benecessary Insert an intravenous fluids. Keep input and output chart and record. Reassure the patient all the time as she will be anxious, the partner should be involvedand supported. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 31 Prepare the patient for theatre but if the condition is worsen the patient will be examinedin the operating theatre and the caesarean section is done, “double set up”. In major degree of placenta previa (3rd& 4th) caesarean section is required even if thefetus is died in utero. The aim is to prevent torrential hemorrhage and possible maternal death. Step 7: Complications of Placenta Praevia (5 minutes) The major maternal complication associated with placenta previa is hemorrhage. Another serious complication is development of an abnormal placental attachment (e.g., placenta accreta, increta, or percreta) Maternal shock resulted from blood loss and hypovolaemia Maternal death. Fetal death. Step 8: Key Points (5 minutes) Placenta previa is life threatening emergency obstetric especially for type 3 and 4 Assessment of maternal and fetal condition is important in order to make appropriatedecision for the management as well as prevention of complication. Step 9: Evaluation (5 minutes) What are the degrees of placenta previa? How will you care a woman with placenta previa? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar esSalaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 32 SESSION 6:CARE OF A WOMAN WITH ABRUPTIO PLACENTA Total Session Time: 120 minutes Prerequisites: None Learning Tasks At the end of this session learner is expected to be able to: Define the term Abruptio placenta State the etiology of abruption placenta Explain the types of Abruptio placenta Assess maternal and fetal condition in abruptio placenta Describe the management of a woman with placental abruption Outline the complications of placental abruption Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 2 10 3 10 4 50 5 6 Activity/ Method Presentation Brainstorming Presentation Presentation Content Presentation of session title and learning objectives Definition and etiology of abruptio placenta Types of abruptio placenta Assessment of maternal and foetal condition of a woman with abruptio placenta. 30 Lecture/discussion Small group discussion Lecture/discussion 05 Lecture/discussion Complications of abruptio placenta Management of a woman with abruptio placenta NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 33 7 05 8 05 Presentation Key Points Presentation Session Evaluation SESSION CONTENTS Step 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK student to the Learning Tasks and clarify ASK student if they have any question before proceeding Step: 2 Definition and Etiology of Abruptio Placenta (10 minutes) Activity: Brainstorming (5minutes) ASK students to brainstorm on: Definition of abruptio placenta The etiology of abruptio placenta ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Definition Abruptio placenta (placental abruption) is the premature separation of the placenta, or is the detachment of part or all of a normally implanted placenta from the uterus. Separation occurs in the area of the decidua basalis after 20 weeks of gestation and before the birth of the infant. Etiology The true cause of this type of hemorrhage is unclear but is associated with: o Severe pre-eclampsia o Sudden reduction in the uterine size. e.g. when the membranes ruptured or after birth of the first twin, and rare in direct trauma to the abdomen perhaps through road traffic accident ,seat belt injury o Previous caesarean section increase the risk of placental abruption o Cigarette smoking o Poor maternal nutrition o Chorioamnionitis o Maternal blunt abdominal trauma o History of previous abruptio placenta o External cephalic version NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 34 o Cocaine, particularly crack cocaine, usage Step 3: Types of Abruptio Placenta (10 minutes) These can be classified as follows: o Revealed hemorrhage This when the blood escape from the placenta site separates the membranes fromthe uterine wall and drain through the vagina o Concealed hemorrhage This when blood is retained behind the placenta may be forced into themyometrium and it infiltrates the muscle fibers of the uterus This extravasations cause marked damaged of observed at operation the uterusappear bruised edematous this is termed as couvelaire uterus or uterine apoplexy. Partial separation of the placenta causes bleeding from the venous sinuses in the placenta bed Further separation continue to separate the placenta to a greater or lesser degree No vaginal bleeding, but the mother will have all sign of hypovolemic shockcaused by conceal bleeding into the uterine muscle The hemorrhage causes uterine enlargement and extreme pain It accounts for 20-35% of abruptions o Mixed hemorrhage The combination of both type of hemorrhage Figure 6.1: Abruptio Placenta (Concealed and Revealed) Concealed Hemorrhage Revealed Hemorrhage Source: Perry et al., (2013). Maternal Child Nursing Care. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 35 Step 4: Assessing Maternal and Fetal Conditions (30 minutes) Maternal condition The following should be adhered in assessing the mother history taking, o Ask the mother any history of accident o Headache, nausea, vomiting, epigastric pain, and visual disturbance may be the feature o Mother may feel a slight localized pain or pain free in mildest degree of placentaabruption General examination o The woman may look anxious, has abdominal pain, and the skin may look pale if themother is in shock. o Edema of the face, fingers and pretibial area of the lower limbs. o The blood pressure and pulse rate should be taken immediately. o Lowered blood pressure and raised pulse rate are signs of shock. o Temperature may remain normal and respiration may be rapid or normal, but if thereis reduced oxygenation may lead to air hunger. o Observe and estimate the visible blood loss, the colour should also be noted. o Blood that has been retained in utero for any length of time changes to brown colour Abdominal examination o Concealed hemorrhage may lead to uterine enlargement in excess of gestation o The uterus has a hard consistency and there is guarding on palpation of the abdomen o Palpation may be difficult and should not be attempted if the uterus is rigid andexcessively painful o In less severe cases, palpation should be kept to minimum to avoid further pain anddamage o Establish the nature and the location of the pain o Fetal heart is unlikely to be heard with fetal stethoscope o An ultrasound scanner to confirm the fetal survival o Fetal parts may not be palpable Assessing the fetal condition Ask the mother if she feels the fetal movements A CTG records will give more complete information about the fetal condition as well asultrasound scan Failure to elicit fetal heart sound with a Pinard stethoscope is not confirmation of a fetal death NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 36 Step 5: Management of a Woman with Placenta Abruption (50 minutes) Activity: Small Group Discussion (20 minutes) DIVIDE students into small manageable group. ASK them to discuss in groups on the management of a woman with abruption placenta for 5 minutes. AFTER small group discussion, ask students to provide their responses. CLARIFY and summarize using the contents below. Any women with history of placental abruption needs urgent medical attention, she shouldbe transferred to obstetric unit for emergency obstetric care. The mother should be admitted to labour ward and consultant obstetrician is informed. The midwife should provide physical and emotional comfort to the mother, and keep herinformed all the time with information’s concerning her condition and progress Managing Pain Pain which exacerbates shock should be alleviated. If it is so extreme morphine 15mg or pethidine 100-150mg may be given The midwife should differentiate the pain from concealed hemorrhage to that of labourpain The nature of the pain should be discussed because labour pain may supervene followingplacental abruption Managing Shock Set IV line of normal saline or ringer’s lactate Maintain Airway, Breathing and Circulation Shock may be due to hypovolaemia, to extravasations and consequent pain or toconsumptive coagulopathy. Whole blood is traditionally used to restore the blood volume An infusion of fresh frozen plasma for every 4-6 units of blood to replenish the clottingfactors (i.e. a ratio of 1 FFP to 4-6 units of blood). The mother should rest on her side to prevent vena cava occlusion and aortic compressionby the gravid uterus. The legs may be elevated but the body should remain horizontal. The foot of the bed may be elevated. Observations Vital signs should be monitored frequently depending on the severity of her condition. Check blood pressure 2-hourly or as frequently as necessary. Insert an indwelling catheter and monitor urine output. The urine should be tested for protein, which may also be linked to pregnancy inducedhypertension. Prepare an intake and output chart and record all fluids. Fundal height and abdominal girth are measured hourly, an increase indicate continuebleeding behind the placenta. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 37 If the fetus is alive, fetal heart rate should be taken continuously with the aid ofcardiotograph. Any deterioration in the maternal or fetal condition must be reported immediately to theobstetrician. Investigations Clotting studies should be carried out because of the risk of coagulation defects. Blood sample may be needed at intervals in order to monitor the progress of thecondition. Specific Management of Different Degrees of Placenta Abruption Mild separation of the placenta. o In this case the placental separation and the haemorrhage are slight. o Mother and the fetus are in a stable condition. Moderate separation of the placenta. o This describes placental separation of about one quarter. o Up to 1000ml of blood may be lost, some may remain behind the placenta as retroplacental clot or extravasations into the uterine muscles and some will remain per vaginum. o The mother will be shocked with raised pulse rate and lowered blood pressure o There may be uterine tenderness and abdominal guarding. o The fetus may alive but hypotoxic; intrauterine death is a probability o The fluid replacement should be monitored. o The fetal condition should be monitored with an electronic fetal monitor, if the fetusis alive, immediate caesarian section may be indicated. o Vaginal delivery may be contemplated if the fetus is in good condition or has alreadydied. Severe separation of the placenta. o This is an acute obstetric emergency; at least two-third of the placenta has becomedetached and 2000 ml of blood or more are from the circulation. o The mother will be severely shocked to the degree far beyond what might be expectedfrom the amount of viable blood loss. o Whole blood 1500ml should be transfused rapidly and subsequent amounts calculatedin accordance with the woman’s central venous pressure. o Labour may begin spontaneously in advance of amniotomy (intentionally breaking ofamniotic sac with a sterile amnion hook, allis forceps to stimulate or augment labour). Psychological care The patient and her partner should be kept informed for what is happening at all time. Step 6: Complications of Abruptio Placenta (5 minutes) Disseminated intravascular coagulation is complication of moderate severe to placentalabruption. Postpartum hemorrhage. Renal failure occur as a result of hypovolemia and consequent poor perfusion of thekidneys Pituitary necrosis due to prolonged and severe hypotension. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 38 Step 7: Key Points (5 minutes) Abruptio placenta (placental abruption) is the premature separation of the placenta, or is the detachment of part or all of a normally implanted placenta from the uterus. The blood loss from a placenta abruption may be revealed, concealed or mixedhaemorrhage Any woman with history suggestive of placenta abruption needs urgent medical attention. Assessment of maternal and fetal conditions is important in order to provide appropriatemanagement of a woman with abruptio placenta thus to minimize complications. Step 8: Evaluation (5 minutes) What are the types of abruptio placenta? What is the management of a woman with abruptio placenta References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.). London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. SESSION 7:CARE OF A WOMAN WITH URINARY TRACT INFECTION (UTI) IN PREGNANCY Total Session Time: 120 minutes Prerequisite: Learning tasks At the end of this session a learner is expected to be able: Outline risk factors of UTIs Detect signs and symptoms of UTIs in pregnancy Management of UTIs in pregnancy Explain the prevention of UTIs Explain the impact of UTIs in pregnancy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 39 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Lecture/discussion Content Presentation of session title and learning tasks 2 10 Brainstorming 3 20 Lecture/discussion Definition of UTI Causes and Risk factors of UTI 4 15 Lecture/discussion Signs and symptoms of UTI in pregnancy 5 35 Lecture/ discussion Management of UTI in pregnancy 6 15 Lecture /discussion Prevention of UTI 7 15 Brainstorming Complications of UTI in pregnancy 8 05 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 40 STEP 2: Definition of UTI (10 Minutes Activity: Brainstorming (5 minutes) ASK students to brainstorm Definition of UTI ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as below: Is infection of the urinary tract occurring due to ascending microorganisms due to urine stasis or trauma during labour or inadequate hygiene leading to ascending infection Step 3: Causes And Risk Factors Of Uti (20 Minutes) Causes: The common causative organism is usually Escherichia coli. E. coli is the offending organism in over 90% cases. Other pathogens are Klebsiella pneumonae and Proteus. To exclude pre-existent asymptomatic Bacteriuria, all pregnant women should ideally have a urine test at their first antenatal visit. The overall incidence during pregnancy ranges between 2 and 10%. Risk factors Apparently stasis of urine occurs during pregnancy, which results from; o Hormonal ureteral dilation, o Hormonal ureteral hypoperistalsis, o Pressure of the expanding uterus against the ureters Trauma during labour Inadequate vulval hygiene Apparently PH change of vagina to alkalinity reduces clearance of microorganism. STEP 4: Signs and symptoms of UTI in pregnancy (15 Minutes) Mild o o Severe o o Mild general body malaise aches and pains in the back and loins. In some cases painful urination may be apparent. Acute cystitis- characterized by scalding on urination Pyelonephritis- causing a sharp raised temperature, pain over the kidney and haematuria. o Lower abdominal pain, nausea, vomiting and Dehydration NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 41 STEP 5: Management of UTI in pregnancy (35 Minutes Investigations: The diagnosis of UTI reached by clinical symptoms and sings and investigations. o Urinalysis, culture and sensitivity of the midstream upper urine (MUS) .Urinalysis and culture are routinely done at initial evaluation to check for asymptomatic bacteriuria. Diagnosis of symptomatic UTI is not changed by pregnancy. Treatment: o Treatment of symptomatic UTI is not changed by pregnancy, except drugs that may harm the fetus are avoided. o Because asymptomatic bacteriuria may lead to pyelonephritis, it should be treated with antibiotics similar to an acute UTI. o Antibacterial drug selection is based on individual and local susceptibility and resistance patterns, but good initial empiric choices include the following: Cephalexin Amoxycilin Nitrofurantoin Trimethoprim/sulfamethoxazole o A patient with severe symptoms and signs like fever, vomiting and dehydration Iv antibiotics may be a best option with iv fluids and hospitalization. General Nursing care: o 4 hourly observation of vital signs specifically temperature and pulse rate o Observation of uterine contractions for preterm labour o Nursing care should include mobility of the patient and if possible wearing antithrombotic stocking to avoid deep veins thrombosis(DVT) o Counselling and reassurance of the patient. STEP 6: Prevention of Urinary Tract Incfetion (UTI) in Pregnancy (15 Minutes Routine screening of asymptomatic pregnant mother at first visit to antenatal clinic by doing urinalysis and if possible doing culture and sensitivity. Maintaining of vulva hygiene to avoid ascending infections Enough and regular drinking of water that will help to wash out and clear bacteria in the Urinarr tract Prompt treatment at the first indication of the UTI and ensuring that the woman completes the course of prescribed antibiotic Re–assessment and repeated treatment is essential until the bacterial count is satisfactory. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 42 STEP 7: Complications of UTI in pregnancy (15 minutes Activity: Brainstorming (5 minutes) ASK students to brainstorm on Complications of UTI in pregnancy ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as shown below Complications o Miscarriages o Preterm labour then to premature deliveries o Anaemia in pregnancy o Acute renal disease e.g. pyelonephritis o Chronic renal diseases e.g. Nephritis and Nephrotic Syndrome o Proteinuria STEP 8: Keys Points (5 minutes The causative organism is commonly Escherichia coli. Prompt treatment at the first indication of the UTI and ensuring that the woman completes the course of prescribed antibiotic. Routine screening of asymptomatic pregnant mother at first visit to antenatal clinic by doing urinalysis and if possible doing culture and sensitivity STEP 7: Session Evaluation (5 minutes What are risk factors of UTI in pregnancy? What are the symptoms and signs of UTI in pregnancy? How do we prevent UTI in pregnancy? What are the complications of UTI in pregnancy? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.). London: Churchill Livingston Duttas .D.C,Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contarceptives( 7th ed). New Delh: India NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 43 SESSION 8: CARE OF A WOMAN WITH MALARIA IN PREGNANCY Total Session Time: 120 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define malaria in pregnancy List clinical features of uncomplicated and severe malaria Describe the treatment of uncomplicated malaria Describe the pre referral management of severe malaria in pregnancy Monitor maternal and foetal conditions Explain the impact of malaria in pregnancy Teach a pregnant woman on prevention and control of malaria Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content 2 05 Presentation Introduction and Definition of malaria in pregnancy 3 10 Lecture/discussion Clinical features of uncomplicated and severe malaria 4 20 Lecture/discussion Treatment of uncomplicated malaria Presentation of session title and learning objectives NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 44 5 30 Brainstorming Lecture/discussion Lecture/discussion Management of severe malaria in pregnancy 6 10 7 15 Group discussion Presentation Health education for prevention and control of malaria in pregnancy 8 15 Presentation How to Reduce Morbidity and Mortality from Malaria in Pregnancy 9 05 Presentation Key Points 10 05 Presentation Session Evaluation Impact of malaria in pregnancy SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Introduction and Definition of Malaria in Pregnancy (5 minutes) Malaria in pregnancy is a parasitic infection, the most common causative organism being plasmodium which is carried by mosquitoes. The malaria parasites hide in the placenta; therefore routine finger prick blood sample testing may not detect the parasites. The parasites may thus still be present and cause damage to the placenta and foetus. The parasites rarely pass into the blood circulation of the baby but can obstruct the passage of nutrients and oxygen to the unborn baby hence slowing down its normal growth. Initially malaria infection can occur without symptoms. Anaemia may be the only recognizable clinical feature. Why Pregnant Women are More Vulnerable to Malaria o The effects of malaria on pregnancy are dependent on the malaria epidemiology and the immunity of the women. o There is a decline in immunity which is most pronounced in the first and second pregnancies and teenage pregnancies. o Pregnant women tend to get malaria more easily than women who are not pregnant because of the loss of ability to fight malaria infection (low immunity). NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 45 o Low birth weight prevalence in primigravida adolescents is doubles that of adult primigravidae. STEP 3: Clinical Features of Uncomplicated and Severe Malaria(10 minutes) Uncomplicated malaria o Headache o Fever o Joint pains and malaise o Poor appetite o Nausea and/or Vomiting o Diarrhoea o Chest pain o Pallor o Note: some patients may be asymptomatic Severe malaria o Severe malarial anaemia o Haemoglobinuria o Cerebral malaria o Pulmonary oedema. STEP 4: Treatment of Uncomplicated Malaria(20 minutes) Case Management of Uncomplicated Malaria Early diagnosis and effective management are important to prevent progression of uncomplicated to severe malaria or death Whenever malaria is suspected laboratory confirmation of the parasite should be performed Treatment should be commenced immediately if laboratory test is not possible based on clinical presentation A negative result does not exclude malaria infection Blood slide can be negative even if parasites are present, as they may be hidden in the placenta. Note: o During the first trimester of pregnancy Oral Quinine should be used as drug of choice for treatment of uncomplicated malaria o Quinine is safe during pregnancy o Artemether/Lumefantrine (ALu) is not recommended in the first trimester, however if quinine is not available and the patient is in danger then ALu tablets may still be used. o During second and third trimesters of pregnancy Artemether/Lumefantrine (ALu) shouldbe used as drug of choice for treatment of uncomplicated malaria o ALu is an oral fixed combination tablet of 20 mg Artemether - a derivate of artemisinin, and120 mg Lumefantrine. o ALu has a rapid action against Plasmodium falciparum with clearance of the parasites fromthe blood within 2 days. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 46 o Due to the long body elimination time of Lumefantrine (up to 10 days), ALu is notrecommended to mothers who are breastfeeding children below 5 kgs ALu Administration The first dose of ALu should be administered at the health facility as DOT The second dose should be strictly given 8 hours after the first dose. Subsequent doses could be given twice daily (morning-evening) in the second and third day of treatment until completion of 6 doses. Give Paracetamol tablets 1gram 6 hourly for three days to relieve pain and fever when giving ALu. Note: o If the drug is vomited or spat out within 30 minutes after administration, the dose should be repeated o ALu should be taken with meals or drinks such as milk to enhance its absorption. Side Effects and Contraindications of ALu Side effects o Incidence is low Contraindication o Patients with hypersensitivity to ALu Not recommended o 1st trimester of pregnancy o Lactating mothers with a child below 5 kgs o Children below 5 kgs body weight o Patients with severe malaria. Management of Failed Response to Malaria Treatment with ALu If within 4 to 14 days after treatment with ALu a patient returns to you complaining ofcontinued symptoms of malaria, a blood smear (and not RDT as does not reveal parasitecount) should be examined. If malaria parasites are not found, other causes of symptoms should be investigated. If malaria parasites are present, this indicates drug failure. Quinine should be started immediately with strict follow up after a full history andexamination. Malaria cases should be followed up on the third day if symptoms persist or immediately ifthe condition worsens, and cases that fail to respond should be referred. Note o Quinine tablets should be given for 7-10 days, at a dose of 10mg/kg every 8 hours NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 47 STEP 5: Management of Severe Malaria in Pregnancy(30 minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the management of severe malaria in pregnancy. ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Management of Severe Malaria in Pregnancy Severe malaria is a medical emergency and demands early diagnosis based on a completehistory, physical examination and blood smear/RDT General Management Clear and maintain the airway to ensure breathing Place the patient in semi-prone position or on her side Take vital signs (pulse rate, respiration, blood pressure and temperature) Take blood slide for malaria parasites in order to initiate immediate treatment (do not waitfor results) Take blood for urgent Hb estimation and blood for sugar if possible. Injectable Quinine is the drug of choice for treatment of severe malaria duringpregnancy Quinine does not cause abortion at therapeutic doses Severe malaria can cause abortion or premature delivery Give quinine injection without delay Hypoglycaemia is a common problem in severe malaria. Use of quinine may worsen thecondition. Therefore, give 5ml/kg of 10% dextrose solution as bolus, OR give 2.5 ml/kg of 25%dextrose as bolus, OR give 50ml of water by mixing 20 gm of sugar (4-level teaspoons) with200 ml of safe water. Give glucose solution orally or by Naso-gastric tube if unconscious. Intra-Muscular (IM) Quinine If administration of IV Quinine is not possible, Quinine can be administered intramuscularlyafter appropriate dilution. Use Quinine dihydrochloride injection (300 mg/ml) Give a dose of 10 mg of salt/kg bodyweight (maximum 600 mg) every 8 hours until thepatient is able to take oral therapy. Dilute in four-fold of water for injection or normal-saline (1:4) to a concentration of 60mg/ml Note: o Give paracetamol tablets 1 gram 6 hourly for 3 days. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 48 Administration of Intravenous (IV) Quinine Quinine dihydrochloride salt 10 mg/kg weight Diluted in 5-10 ml/kg weight of 5% dextrose Infused over a period of 4 hours, rest for 4 hours, but keep the IV line open, then continuewith IV Quinine until the patient is able to take orally Change to Quinine tablets 10 mg/kg every 8 hours to complete 7 days of treatment or if notin 1st trimester give full course of ALu to complete treatment (ALu administration should bestarted 12 hours after the last dose of quinine) Also give 1 gram of paracetamol tablets 6 hourly for 3 days to lower fever and relieveheadache/pain Administration of I/V Quinine may cause hypoglycaemia, therefore close monitoring is vital Refer the patient if necessary. The drop rate is calculated as follows; o Drop rate per minute = amount of fluid to be infused (in ml) x 20 (drop factor)time period to be infused (in minutes) Note o It is important to monitor the rate of Infusion because Quinine if allowed to run toorapidly may cause hypotension and hypoglyecaemia may develop. o On the other hand if the Infusion is too slow, inadequate blood levels of the drug may beachieved. o Quinine drip (Infusions) should be discontinued as soon as the patient is able to take oralquinine medication. o Patients should be properly instructed to complete the 7-day treatment. o Alternatively, a full course of ALu may be administered to complete treatment Management of Failed Response to Quinine Therapy Persistence of clinical features of severe malaria o Failure of clearance of parasites after 5 days of treatment o Other possible causes of illness which have not been investigated. Note o Patients with malaria who have not responded to quinine therapy should be givenparenteral Artemether 3.2mg/kg weight (loading dose) IM followed by 1.6mg/kg weightdaily for 6 days. STEP 6: Impact of Malaria in Pregnancy (10 minutes) Adverse consequences of malaria during pregnancy On the pregnant woman o Anemia o Hypoglycaemia o Cerebral malaria o Febrile illness o Puerperal sepsis o Death On the foetus o Abortion o Intrauterine growth restriction NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 49 o Stillbirth o Congenital infection On the newborn o Low birth weight o Premature o Growth retardation o Congenital neonatal malaria o Death STEP 7: Health education for prevention and control of malaria in pregnancy (15 minutes) Activity: Small Group Discussion (10 minutes) DIVIDE students into small manageable group. ASK them to discuss in groups on the health education for prevention and control of malaria in pregnancy. AFTER small group discussion, ask students to provide their responses. CLARIFY and summarize using the contents below. Health education messages should focus on the following: o If malaria symptoms persist after taking right dose of quinine therapy the patient might be having no response to the treatment. The patient MUST thus go to a higher level of care for re-evaluation and further management. o Use of IPTp among pregnant women o Advise on the use of ITNs o Advise on environmental sanitation and Indoor Residual Spray (IRS) to control mosquitoes. o Closing windows and doors before dark o Use of mosquito gauze to windows and doors o Advise pregnant women, family members and other support persons to seek early treatment when they feel sick. o Continue with food and fluid intake. o Importance of compliance to finish the dose. STEP 8: How to Reduce Morbidity and Mortality from Malaria in Pregnancy (15 minutes) Intermittent Preventive Treatment (IPT) of malaria with Sulfadoxine/Pyrimethamine (SP) Preventing malaria transmission due to mosquito bites by using Insecticide Treated Nets(ITNs) Early diagnosis of malaria and prompt case management Quality focused antenatal care (ANC) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 50 Intermittent Preventive Treatment (IPTp) Intermittent Preventive Treatment (IPT) is the administration of drug (medicine) therapy in full therapeutic doses at predetermined intervals during pregnancy even if individuals have no signs of malaria The aim of IPT is to prevent the worst effects of malaria infection in pregnancy rather than to cure a potentially life-threatening illness. Women taking IPT can still become sick with malaria IPT is not chemoprophylaxis Currently SP is the drug of choice for IPT IPT assumes that pregnant women in malarial areas are infected with malaria, therefore SP should be given to reduce the adverse effects of malaria The recommended schedule for IPT is four doses that are given four weeks apart from 14 weeks of gestation. The health provider should devise an individual schedule for the pregnant woman that ensures that IPT is given during the second and third trimester and the doses are not given less than 4 weeks apart. To get a single dose is better than nothing. Some pregnant women start ANC during the last trimester of pregnancy. They can be protected from a single dose of SP SP can be given at any point in pregnancy between 14 weeks and the last trimester as long as they are four weeks apart. Evidence shows that, if used as recommended, SP is safe and effective for both the pregnant woman and foetus. Sulfadoxine/Pyrimethamine (SP) Is a combination of two different drugs - Sulfadoxine and Pyrimethamine which act synergistically. One tablet contains 500 mg of sulfadoxine and 25 mg of pyrimethamine. Fansidar® (SP) is the most common brand name, but other brands with the same medicine are: Falcidin®, Laridox®, Malostat®, Orodar®, and Metakelfin®. SP remains the drug of choice for IPTp even though it is no longer the first line drug for uncomplicated malaria treatment. Note o Chloroquine remains the recommended drug of choice for chemoprophylaxis for pregnant women with sickle cell disease Administering SP to Pregnant Woman during ANC Visits Always ask about allergy to sulfa drugs before giving SP In cases of known allergy to sulfa drugs and no available alternatives to SP for IPT, the use of ITNs is strongly advised. Pregnant women should take SP with clean and safe drinking water, under Direct Observed Treatment (DOT) at the antenatal clinic. Infection Prevention measures should be adhered to (use clean cups for each client) If the pregnant woman vomits SP within 30 minutes, the dose should be repeated After giving SP record on the antenatal card and in the register MTUHA Book 6. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 51 Explain to the woman the importance of returning for the second dose, four weeks apart being the minimum period required. SP and Tetanus Toxoid may be given during the same visit. If malaria is confirmed any time after administration of IPTp with SP, a full treatment with antimalarials should be given according to the national guidelines. Insecticide Treated Nets Insecticide treated nets (ITN) prevent physical contact with mosquitoes through either killingor repelling them. Use of ITN is effective because mosquitoes usually bite at night when the client is asleep. ITN kill or repel other insects like: o Lice, ticks, bedbugs and cockroaches STEP 9: Key Points (5 minutes) Early diagnosis and effective case management of malaria are crucial in preventing the progression to severe disease and death. Pregnant women with uncomplicated malaria are likely to develop severe malaria. Treatment should be commenced immediately based on clinical presentation if laboratory test is not possible During the first trimester of pregnancy Oral Quinine should be used as drug of choice for treatment of uncomplicated malaria During second and third trimesters Artemether/Lumefantrine (ALu) should be used as drug of choice for treatment of uncomplicated malaria Injectable Quinine (IM/IV) is the drug of choice for treatment of severe malaria during pregnancy. Most pregnant women tend to get malaria more easily than women who are not pregnant because of the loss of ability to fight malaria infection (low immunity) In order to reduce malaria in pregnancy, ITN, IPT, early diagnosis of malaria and prompt case management through quality focused ANC and community health education and promotion are recommended. Step10: Session Evaluation (5 minutes) Why pregnant women are vulnerable to malaria? What are the effects of malaria in pregnancy to the pregnant woman and the newborn? What are the strategies to reduce morbidity and mortality from malaria in pregnancy? How can you prevent malaria in pregnancy? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 52 Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. SESSION 9: CARE OF A PREGNANT WOMAN WITH PULMONARY TUBERCULOSIS Total Session Time: 60 minutes Prerequisite: Learning Tasks At the end of this session a learner is expected to be able: Outline the causes of pulmonary tuberculosis (PTB) in pregnancy Outline the risk factors pulmonary tuberculosis in pregnancy Explain the signs and symptoms of pulmonary tuberculosis (PTB) in pregnancy Describe the management and prevention of pulmonary tuberculosis (PTB) in pregnancy Discuss the maternal and fetal effects of pulmonary tuberculosis (PTB) in pregnancy Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 53 Session Overview Box Step Time (min) Activity/ Method Presentation Content 1 05 Presentation of Session Title and Learning tasks Brainstorming/presentation The causes of pulmonary tuberculosis (PTB) in pregnancy 2 05 3 05 Lecture discussion Risk factors for contacting PTB 4 10 Lecture discussion Symptoms and signs of PTB and Diagnosis of PTB 5 15 Lecture discussion Care of a woman with PTB and prevention in pregnancy 6 10 Lecture discussion Maternal and foetal effects of PTB in pregnancy 7 05 Presentation Key Points 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: The Causes of Pulmonary Tuberculosis (PTB) In Pregnancy (5 Minutes) Activity: Brainstorming (3 minutes) ASK students to tell the causes of pulmonary tuberculosis in pregnancy ALLOW time for them to respond CLARIFY and provide summary using the content below Pulmonary Tuberculosis (TB) infection is caused by inhalation of viable bacilli, which may persist in an inactive state (known as latent TB infection [LTBI]) or progress to active TB disease NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 54 o Individuals with LTBI are asymptomatic and not contagious. Latent TB bacilli remain viable and may reactivate, causing active symptomatic TB disease, which can be transmitted via airborne spread. o This can happen when someone with the untreated, active form of tuberculosis coughs, speaks, sneezes, spits, laughs or sings STEP 3: Risk Factors for Contacting PTB (5 Minutes) Positive family history or past history Low socioeconomic status Area with high prevalence of tuberculosis HIV infection Alcohol addiction Intravenous drug abuse STEP 4: Symptoms and signs of PTB and Diagnosis (10 Minutes) Symptoms and Signs of active TB include: Coughing (productive) that lasts two or more than two weeks Coughing up blood Chest pain, or pain with breathing or coughing Unintentional weight loss Fatigue Fever mostly in the evening Night sweats Chills Loss of appetite DIAGNOSIS: Tuberculin skin test with Purified Protein Derivative (PPD) when > 10 mm is considered positive speciallyin presence of risk factors X-ray chest (after 12 weeks) Early morning sputum (three samples) for acid-fast bacilli Gastric washings Diagnostic bronchoscopy Extrapulmonary sites—lymph nodes, bones (rare in pregnancy) Direct amplification tests for 16 S ribosomal DNA and gene probe can detect M. tuberculosis with greater sensitivity and specificity. ( Currently GN expert) STEP 5: Care of a woman with PTB and prevention in pregnancy (15 Minutes) Prophylaxis-a pregnant woman with no evidence of evidence of active disease or HIV positive are given Isoniazid prophylaxis 300 mg/day is started after the first trimester and continued for 6–9 months and Pyridoxin (Vit B6) 50 mg/ day is added to prevent peripheral neuropathy. No major adverse fetal or neonatal effects are seen with these anti-tuberculous drugs. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 55 Treatment: Pregnant women with active tuberculosis should receive the following drugs orally daily for a minimum period of 9 months. (Isoniazid, Rifampicin, Ethambutol , Pyrazinamide) in fixed dose combination. Streptomycin is not used in pregnant as it causes damage to facial nerve. Place of therapeutic termination: Tuberculosis per se is not an indication for termination of pregnancy. Obstetric management is no different from other pregnant women, once tuberculosis is well managed. Breastfeeding: Breastfeeding is not contraindicated when a woman is taking anti-tuberculous drugs. Breastfeeding should be avoided if the infant is also taking the drugs (to avoid excess drug level). In active lesion, however, not only is breastfeeding contraindicated but the baby is to be isolated from the mother following delivery. Baby should be given prophylactic isoniazid 10–20 mg/kg/day for 3 months when the mother is suffering from the active disease. However, if the mother is on effective chemotherapy for at least 2 weeks, there is no need to isolate the baby. BCG should be given to the baby as early as possible. CONTRACEPTION: o Pregnancy is to be avoided until quiescence is assured for about two years. o Spacing can be achieved by any methods acceptable to the couple. o Oral contraceptives should be avoided when rifampicin is used. o sterilization should be seriously considered, if the family is completed. Nutrition assessment and counselling; individuals with active tuberculosis (TB) should receive o an assessment of their nutritional status o appropriate counselling based on their nutritional status at diagnosis and throughout treatment. o Pregnant women with active TB and moderate undernutrition, or with inadequate weight gain, should be provided with locally available nutrient-rich or fortified supplementary foods, as necessary to achieve an average weekly minimum weight gain of approximately 300 g in the second and third trimesters. All pregnant women with TB should be under care of physician who manages the clinical aspect of the women’s treatment and a specialist midwife with full training in the disease. It is also important that they collaborate with the obstetrician and HIV specialist to promote continuity of care. The key to a successful outcome is to ensure that the woman adheres to the prescribed treatment. Postnatal Care If negative, the neonate BCG vaccination should be given and drug therapy discontinued Antituberculin drugs are considered to be compatible with breastfeeding. Caring for a child at home makes great demand on the woman and extra help should be arranged if possible. Long term medical and social follow up is necessary in order to monitor the progress of the disease and the respond to treatment, also to provide help for the socially and economically disadvantaged. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 56 STEP 6: Maternal and foetal effects of PTB in pregnancy (10 Minutes) Feotal effects o In active disease, fetus can be affected by transplacental route or by aspiration of amniotic fluid. o Neonatal affection is mainly by postpartum maternal contact. o In untreated patients, the incidence of preterm labor, IUGR and perinatal mortality is high. o Low birth from untreated mother o Increased rate of spontaneous abortion Maternal effects o Low weight gain in pregnancy o Preterm labour o Puerperal sepsis o The onset of primary TB is often insidious and the symptoms are non-specific fatigue,malaise, loss of appetite, loss of weight alteration in bowel habit and low grade fever, can be interpreted as usual symptoms occurring in pregnancy STEP 7: Key Points (5 minutes) Tuberculosis (TB) infection is caused by inhalation of viable bacilli, which may persist in an inactive state (known as latent TB infection [LTBI]) or progress to active TB disease. This can happen when someone with the untreated, active form of tuberculosis coughs, speaks, sneezes, spits, laughs or sings. The cardinal symptoms and signs for pulmonary tuberculosis are productive cough for two weeks or more, sweating and evening fever and un intentional weight loss Prophylaxis-a pregnant woman with no evidence of evidence of active disease or HIV positive are given Isoniazid prophylaxis 300 mg/day. STEP 8: Session Evaluation (5 minutes) What are the risk factors for contacting PTB? What are the maternal effects of PTB ? Why contraception is important to a woman with PTB? References WHO. Guideline: Nutritional care and support for patients with tuberculosis. Geneva, World Health Organization; 2013 Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. WHO. (2006). Pregnancy, childbirth, postpartum and newborn care: A guide for essential practice (2nd ed.). Geneva: WHO. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 57 SESSION 10: CARE OF A PREGNANT WOMAN WITH SYPHYLIS Total Session Time: 60 minutes Prerequisite: Learning Tasks At the end of this session a learner is expected to be able: Outline the causes of syphilis in pregnancy Explain the signs and symptoms of syphilis in pregnancy Describe the management of syphilis in pregnancy Explain the prevention of syphilis in pregnancy Discuss the maternal and fetal effects of syphilis in pregnancy Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content 1 05 2 05 Presentation of Session Title and Learning tasks Brainstorming/presentation The causes of syphilis in pregnancy 3 05 Lecture discussion Risk factors for contacting syphilis 4 10 Lecture discussion Symptoms and signs of syphilis and Diagnosis of syphilis 5 15 Lecture discussion Care of a woman with syphilis and prevention in pregnancy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 58 6 10 7 5 8 5 Lecture discussion Maternal and foetal effects of syphilis inpregnancy Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: The Causes of Syphilis In Pregnancy (5 Minutes Activity: Brainstorming (3 minutes) ASK students to tell the causes of syphilis in pregnancy ALLOW time for them to respond CLARIFY and provide summary using the content below Syphilis is a systemic infection caused by the spirochete bacteria called Treponema pallidum, is a sexually transmitted disease which is of particular concern during pregnancy because of the risk of transplacental infection of the fetus. Congenital infection can be associated with several adverse outcomes, including perinatal death. Incidence is rising due to upsurge of HIV infection and the IV drug abuse STEP 3: Risk Factors for Acquiring Syphilis (5 Minutes) those having unprotected sex woman who have sex with men who sex with other men woman with HIV at high risk woman with numerous sexual partners STEP 4: Symptoms and signs of Syphilis and Diagnosis (10 Minutes) Primary symptom o syphilis are one or many painless, firm, and round syphilitic sores called chancres. These appear about 3 weeks after exposure. o Chancres disappear within 3 to 6 weeks, but, without treatment, the disease may progress to the next phase. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 59 Secondary symptoms o a non-itchy rash that starts on the trunk and spreads to the entire body, including the palms of the hands and soles of the feet. It may be rough, red, or reddish-brown in color o oral, anal, and genital wart-like sore o muscle aches,fever, sore throat ,swollen lymph nodes , o patchy hair loss, headaches, weight loss, fatigue Diagnosis o Having obstetric performances with classic history shows—late abortion → macerated stillbirth → fresh stillbirth o Serological test—This should be done as a routine in the first antenatal visit. VDRL Blood tests: These can detect a current or past infection, as antibodies to the disease will be present for many years. Bodily fluid: Fluid from a chancre during the primary or secondary stages can be evaluated for the disease. Cerebrospinal fluid: This may be collected through a spinal tap and examined to test for any impact on the nervous system. If there is a diagnosis of syphilis, any sexual partners must be notified of and tested for the disease. STEP 5: Care of a woman with Syphilis and prevention in pregnancy (15 Minutes) Syphilis can be treated successfully in the early stages. Early treatment with penicillin is important, as long-term exposure to the disease can lead to life-threatening consequences. So early screening to a pregnant woman during antenatal is very important protection even if the treatment is begun late in pregnancy. For primary or secondary or latent syphilis : benzathine penicillin 2.4 million units intramuscularly single dose. When the duration is more than a year—benzathine penicillin 2.4 million units IM weekly for 3 doses is given. If the patient is allergic to penicillin, oral azithromycin 2 gm as a single dose is given. Baby: Positive serological reaction without clinical evidences of the disease —The baby is treated with a single intramuscular dose of penicillin G 50,000 units per kg body weight Infected baby with positive serological reaction: o Isolation with the mother o Intramuscular administration of aqueous procaine penicillin G 50,000 units per kg body weight each day for 10 days. An apparently healthy child of a known syphilitic mother: Serological reaction should be tested weekly for the first month and then, monthly for 6 months. STEP 6: Maternal and foetal effects of Syhilis in pregnancy (10 Minutes) Feotal effects o Abortion o Preterm birth NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 60 o Intrauterine deaths leading to either a macerated or a fresh stillbirth o Nonimmune fetal hydrops (ascites, hepatomegaly) o Delivery of a highly infected baby with early neonatal death o Survival with congenital syphilis. Maternal effects o Infertility o Recurrent pregnancy losses o Preterm deliveries o Dementia o Numbness of extremities o Visual loss STEP 7: Key Points (5 minutes) Syphilis is a systemic infection caused by the spirochete bacteria called Treponema pallidum, It is a sexually transmitted disease which is of particular concern during pregnancy because of the risk of transplacental infection of the fetus. Serological test—this should be done as a routine in the first antenatal visit.( VDRL) Early screening to a pregnant woman during antenatal is very important An apparently healthy child of a known syphilitic mother: Serological reaction should be tested weekly for the first month and then, monthly for 6 months. STEP 8: Session Evaluation (5 minutes) What are the risk factors syphilis infections? How does syphilis diagnosed? List the feotal effects of syphilis. References WHO. Guideline: Nutritional care and support for patients with tuberculosis. Geneva, World Health Organization; 2013 Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. WHO. (2006). Pregnancy, childbirth, postpartum and newborn care: A guide for essential practice (2nd ed.). Geneva: WHO. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 61 SESSION 11 :CARE OF A WOMAN WITH ANAEMIA IN PREGNANCY Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define anaemia State the factors contributing to anaemia in pregnancy Outline the clinical features of anaemia Care of a woman with mild, moderate and severe anaemia Explain the impact of anaemia, to a pregnant woman and foetus Explain the prevention of anaemia in pregnancy Resources Needed: Give care to a woman with abortion Explain complications of abortion Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Brainstorming/presentation Definition of anaemia in pregnancy Factors contributing to anaemia in pregnancy 3 10 Lecture discussion 4 15 Presentation Clinical features and diagnosis of anaemia in pregnancy 5 45 Lecture discussion Care of a pregnant woman with mild, moderate and severe anaemia 6 15 Lecture discussion Explain the impact of anaemia, to a pregnant NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 62 woman and foetus 8 15 9 05 10 05 Buzzing/presentation Explain the prevention of anaemia in pregnancy Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning objectives ASK participants if they have any questions before continuing STEP 2: Definition of anaemia in pregnancy (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on the defition of anaemia in pregnancy. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Anaemia is defined as the reduction of red blood cells or haemoglobin concentration or both below the normal range. A pregnant woman with haemoglobin (Hb) less than 11g/dl or haemotocrit less than 33% is considered anaemic. Anaemia can be ; o Moderate anaemia Hb(7.0-10.9)g/dl o Severe anaemia Hb<7g/dl o Very severe anaemia Hb<4g/dl STEP 3: Factors Contributing To Anaemia In Pregnancy (10 Minutes) Increased nutritional demand for o Growing foetus and placenta NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 63 o Increased maternal Red blood cell mass o Nutrients include mainly iron, and folic acid, and other vitamins. Plasma volume increases by 50%, and RBC mass 25% this leads haemodilution which reaches maximum about 32-34 weeks. Inadequate dietary intake –nutritional deficiency o Poor diet lacking essential nutrients for haemopesis- i.e iron and folic acid o Poor appetite- e.g. o excessive vomiting o Acute & chronic infections o Inadequate absorption (malabsorption this is rare) Excessive iron loss ( blood loss) o parasitic infestations- mainly hookworm, schistosmiasis o heavy menstrual loss prior to pregnancy Malaria pregnancy women are more susceptible to malaria especially during first pregnancy Chronic nutrient depletion high parity especially frequent closely spaced births Multiple pregnancy increased demand of nutrients (iron, folic acid vitamin B ) Underlying infections e.g. UTI,HIV,TB Blood disorders like sickle cell anaemia and leukaemia STEP 4: Clinical Features And Diagnosis Of Anaemia In Pregnancy (15 Minutes) Anaemia may be asymptomatic and symptoms appear when the anaemia is already severe Symptoms and signs are not very specific The general complaints are o fatigue, o lestlessness, o dizziness, o palpitations, o dyspnoea, o And orthopnoea, Signs include o palor of the conjunctiva, tongue, bucalmucosa,palms, and nail beds etc, Palor of the mucous membranes, and palms Koilonychia in long standing severe anaemia of iron deficiency type May be jaundiced NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 64 tachycardia,tachypnoea , gallop rhythm Diagnosis Through history taking Through physical examination Through laboratory investigation o Full blood count and RBC indices o Haemoglobin-determine the severity of anaemia o peripheral blood smear o Red cell indices- microcytosis, hypochromia- reflects iron deficiency anaemia. megaobablastic- folic acid deficiency o Blood slide for malaria parasites STEP 5: Care Of A Pregnant Woman With Mild, Moderate And Severe Anaemia (45 Minutes) Mild to Moderate Anaemia (7-10.9g/dl) o Find and treat the cause of anaemiaGive the following drugs: Ferrous sulphate 200 mg three times a day Folic acid 5 mg daily Antihelminthics : Mebendazole 500 mg (DOT) once after the first trimester o Treat schistosomiasis after delivery Severe anaemia o Severe at any gestation is an emergency; the pregnant woman should be admitted. o Thorough history and examination o Exclude cardiac failure o Give the pregnant woman blood transfusion Precautions-give diuretic before transfusion Transfuse slowly NB blood transfusion may precipitate cardiac failure o Monitor vital sign of the mother and fetal heart rate o Continue with ferrous sulphate and folic acid up to 3 months after delivery o Follow up patient every 14 days until Hb reaches 11g/dl. Very severe anaemia Very severe anaemia – in Cardiac failure is an obstetric emergency o Transfusion is necessary and urgent o Use packed cells or sediment cell and discard the serum o Give a fast acting diuretic- e. g furosemide or ethacranic acid before transfusion o Monitor the maternal and fetal vital sign STEP 6: Impacts Of Anaemia To Mother And Foetus(20 Minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 65 Mother o Severe anaemia may cause cardiac failure and death Dangerous time is during labour when there is increased work of the heart After delivery when shunting of the blood from placental bed results in volume overload o Poor weight gain o Reduced tolerance to blood loss. Minimal blood loss may precipitate hypovolaemia and collapse o Reduced resistance to infection especially during the puerperium, and thus susceptible to puerperal infections. o Decreased work capacity Poor ability to lactate Foetus o Abortion o Premature delivery o Intrauterine growth retardation o Stillbirth o Thus anemia in pregnancy causes increased maternal morbidity and mortality and perinatal morbidity and mortality STEP 7: Prevention of anaemia in pregnancy(15 minutes) Activity: Buzzing (2 minutes) TELL students to pair up and outline the clinical features of anaemia in pregnancy for 2inutes ALLOW few students to respond and let other pairs provide unmentioned responses CLARIFY and summarize by using the information below. PROVIDE possible answers as indicated in the notes below Prophylactic treatment to all pregnant women o Iron- ferrous sulphate 1 tablet twice a day o Folic acid 1 tablet once a day o Intermittent presumptive treatment (IPT) for malaria with SP twice during pregnancy o De-worming once during the second trimester Treatment of any underlying condition Give nutritional education o All pregnant women should be advised to take diversified diet and promote use of food richin iron which are locally available. Advise the woman on personal malaria protection using ITN Advise on family planning Advice pregnant women on the importance of antenatal clinic follow ups General environmental measures NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 66 o Control malaria, and hookworm o Promote and ensure adequate nutrition to all women in reproductive age o Promote adequate food production and thus household food security at national level STEP 9: Key points (5 minutes) Anaemia in pregnancy is preventable In order to treat anaemia treat the underlying cause first Aetiological type of anaemia includes o Iron deficiency o Folic acid deficiency o Combined deficiencies o Hemolytic anaemia - due to malaria o Anaemia of chronic infections e.g. HIV/AIDS,pyelonephritis and TB o Hemoglobinopathies, eg sickle cell anaemia STEP 10: Session Evaluation(5 minutes) What are the contributing factors for anemia in pregnancy? What are the clinical symptoms and signs of anemiain pregnancy? What are the complications or effects of anemia to pregnant woman? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 67 SESSION 12: CARE OF A WOMAN HYPERTENSIVE DISORDERS IN PREGNANCY Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session a learner is expected to be able to: Define hypertensive disorders of pregnancy Describe different classes of hypertensive disorders of pregnancy Explain etiology of hypertensive disorders of pregnancy Explain pathophysiology of hypertensive disorders of pregnancy Explain signs and symptoms of imminent eclampsia Describe haemolysis elevated liver enzymes and low platelets count (HELLP) syndrome Identify principles of managing pre-eclampsia and eclampsia Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 05 Activity/ Method Presentation Content 1 2 10 Brainstorming/presentation Definition hypertension in pregnancy 3 10 Lecture discussion classes of hypertensive disorders of pregnancy 4 30 Lecture discussion etiology of hypertensive disorders of pregnancy 5 20 Lecture discussion pathophysiology of hypertensive disorders of Presentation of session title and learning tasks NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 68 pregnancy 6 20 Presentation signs and symptoms of imminent eclampsia 7 10 Lecture discussion Haemolysis elevated liver enzymes and low platelets count (HELLP) syndrome 8 10 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Hypertensive Disorders of Pregnancy (10 Minutes Activity: Brainstorming (5 minutes) ASK students to brainstorm on the definitions of hypertension, hypertensive disorders of pregnancy, pregnancy-induced hypertension, chronic hypertension. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Hypertension is one of the medical condition that is diagnosed when a BP is ≥140/90 mmHG measured 2times apart with at least 4hours or more apart. The hypertensive disorders of pregnancy include pregnancy induced-hypertension and chronic hypertension. Pregnancy induced-hypertension is that occurs after 20 weeks of gestation, during labour and/or within 48hours of delivery. Hypertension occurs before 20 of gestation age it is classified as chronic hypertension. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 69 STEP 3: Different Classes of Hypertensive Disorders Of Pregnancy (10 Minutes) The term, ‘Pregnancy-induced hypertension (PIH)’ is defined as the hypertension that develops as a direct result of the gravid state. It includes—(i) gestational hypertension, (ii) pre-eclampsia, and (iii) eclampsia. Gestational hypertension: BP ≥ 140/90 mm Hg for the first time in pregnancy after 20 weeks, without proteinuria Pre-eclampsia: Gestational hypertension with proteinuria Severe pre-eclampsia(imminent eclampsia): Diastollic pressure of 110mmHG or above after 20 weeks of gestation age with protein in urine of +3 or above, severe headache, blurred vision, epigastric pain, dizziness but no convulsions and no loss of consciousness. Eclampsia: Women with pre-eclampsia complicated with convulsions and/ or coma Chronic hypertension: Known hypertension before pregnancy or hypertension diagnosed first time before 20 weeks of pregnancy Superimposed pre-eclampsia or eclampsia: Occurrence of new onset of proteinuria in women with chronic hypertension. STEP 4: Aetiology of Hypertensive Disorders of Pregnancy (30 Minutes) Pregnancy induced hypertension is a multisystem disorder of unknown aetiology characterized by development of hypertension to the extent of 140/90 mm Hg or more with proteinuria after the 20th week in a previously normotensive and non-proteinuric woman. Some amount of edema is common in a normal pregnancy. Edema has been excluded from the diagnostic criteria unless it is pathological. The risk factors can be explained rather the causes of pregnancy induced hypertension; o Primigravida: Young or elderly (first time exposure to chorionic villi) o Family history: Hypertension, pre-eclampsia o Placental abnormalities: Hyperplacentosis: Excessive exposure to chorionic villi (molar pregnancy twins, diabetes) Placental ischemia. o Obesity: BMI >35 kg/M2, Insulin resistance. o Pre-existing vascular disease o New paternity. Changing of paternity has been associated with PIH o Thrombophilias (antiphospholipid syndrome, protein C, S deficiency, o Preexisting medical conditions such as hypertension, renal disease, thrombophilias o Age (teens and women older than 35 years) The common causes of chronic hypertension: o Essential hypertension o Chronic renal disease (reno vascular disease) o Coarctation of aorta o Endocrine disorders (diabetes mellitus, pheochromocytoma, thyrotoxicosis o Connective tissue diseases (Lupus erythematosus). STEP 5: Pathophysiology Of Hypertensive Disorders Of Pregnancy (20 Minutes) In pre-eclampsia and eclampsia, the following pathophysiologic changes are noted o BP begins to rise after 20 weeks of pregnancy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 70 o o o o o o Blood flow is decreased to virtually all organs, which is secondary to intense vasospasm due to an increased sensitivity of the vasculature to any pressor agent Blood flow to the kidneys is decreased, resulting in sodium retention that leads to loss of intravascular plasma volume, increased extracellular volume (oedema) and increased sensitivity to pressor agents. Permeability increases and serum albumin filters through into the urine(Tubular reabsorption is simultaneously depressed) Leading to protein in urine. Loss of normal vasodilation of uterine arterioles results in decreased placental perfusion and can affect fetal growth and wellbeing The liver is affected in severe cases where intravascular haemorrhages and necrosis occur Oedema of the liver cells produces epigastric pain and impaired liver function may results in jaundice Decreased intravascular volume results in increased viscosity of the blood and a corresponding rise in hematocrit, as well as activation of the coagulation cascade, especially platelets, with microthrombi formation. STEP 6: Signs and Symptoms Of Imminent Eclampsia (20 Minutes) Imminent eclampsia or severe pre-eclapmsia is classified when the diastolic blood pressure is above 110mmHG on two readings at least 20minutes apart. The following are the symptoms and signs of immnent eclampsia;o A sharp rise in blood pressure o Diminished in urine output which is due to acute vasospam o Increase in proteinuria +3 or more o Headache which is usually severe persistent and frontal in location( throbbing in nature) usually does not respond to analgesic o Drowsiness or confusion due to cerebral edema o Visual distabances such as blurring vision or flushing lights, due to retinal edema o Epigastric pain which denotes liver edema and impairment of liver function o Nausea and vomiting. STEP 7: Haemolysis , Elevated Liver Enzymes And Low Platelets Count (HELLP) Syndrome (10 Minutes) HELLP Syndrome: This is an acronym for Hemolysis (H), Elevated Liver enzymes (EL) and Low Platelet count (LP)(<100,000/mm3). o This is a rare complication of pre-eclampsia (10–15%). o HELLP syndrome may develop even without maternal hypertension. o This syndrome is manifested by nausea, vomiting, epigastric or right upper quadrant pain, along with biochemical and hematological changes. o Parenchymal necrosis of liver causes elevation in hepatic enzymes (AST and ALT >70 IU/L, LDH>600 IU/L) and bilirubin (>1.2 mg/dL). o There may be subcapsular hematoma formation (which is diagnosed by CT scanning) and abnormal peripheral blood smear. o Eventually liver may rupture to cause sudden hypotension, due to hemoperitoneum. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 71 STEP 8: Key Points (10minutes) Hypertension is one of the medical condition that is diagnosed when a BP is ≥140/90 mmHG measured 2times apart with at least 4hours or more apart. The hypertensive disorders of pregnancy include pregnancy induced-hypertension and chronic hypertension. Pregnancy induced hypertension is a multisystem disorder of unknown aetiology characterized by development of hypertension to the extent of 140/90 mm Hg or more with proteinuria after the 20th week in a previously normotensive and non-proteinuric woman. Some amount of edema is common in a normal pregnancy. Imminent eclampsia or severe pre-eclapmsia is classified when the diastolic blood pressure is above 110mmHG on two readings at least 20minutes apart with proteinuria of +3 or above, headache and visual disturbance HELLP Syndrome: This is an acronym for Hemolysis (H), Elevated Liver enzymes (EL) and Low Platelet count (LP)(<100,000/mm3). STEP 8: Session Evaluation (5 minutes) What are hypertensive disorders of pregnancy? What is pregnancy induced hypertension? How can you classify pregnancy induced hypertension? How can you describe the word HELLP syndrome? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Duttas .D.C, Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contraceptives ( 7th ed). New Delh: India MOHSW. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 72 SESSION 13: CARE OF A WOMAN WITH PRE-ECLAMPSIA AND ECLAMPSIA Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session a learner is expected to be able: Identify principles of managing eclampsia Assess a woman to diagnose hypertensive disorders of pregnancy Give care to a pregnant woman with mild pre-eclampsia during antenatal Give care to a pregnant woman with severe pre-eclampsia/eclampsia during antenatal Give care to a pregnant woman with severe pre-eclampsia/eclampsia during itrapartum and after delivery Complications following severe pre-aclampsia and eclampsia intra-partum and after delivery. Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation 2 10 Brainstorming 3 15 Demonstration/ Content Presentation of Session Title and Learning Objectives principles of managing eclampsia Assessment of a pregnant woman to diagnose hypertensive disorders of pregnancy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 73 4 10 Lecture discussion Care of a pregnant woman with Pre-eclampsia during antenatal 5 15 Lecture discussion Care of a pregnant woman with severe preeclampsia & eclampsia during antenatal 6 30 Lecture discussion Care of a pregnant woman with severe preeclampsia and eclampsia during intra-partum and after delivery 7 20 Lecture discussion Complications following severe pre-aclampsia and eclampsia intra-partum and after delivery. 8 10 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Principles Of Caring A Pregnant Woman With Eclampsia (10Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the principles of care a woman with severe preeclampsia /eclampisa. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below The management of severe Pre-eclampsia and eclampsia is based on the following principles: o Antenatal care and recognition of hypertension o Identification and treatment of Pre-eclampsia/Eclampsia by skilled attendant o Timely delivery The treatment objectives ; NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 74 o Control convulsion by giving appropriate drugs. o Control hypertension by giving antihypertensive accordingly o The delivery as expectant management should be within 12hrs. STEP 3: Assessment Of A Pregnant Woman To Diagnose Hypertensive Disorders Of Pregnancy (15 Minutes) Activity: Demonstration (10 minutes) DIVIDE: students in medium-sized manageable group DEMONSTRATE on how to manage a woman with pre-eclampsia for 5 minutes Refer students to Handout 13.1: Checking blood pressure ALLOW one student from each group to do return demonstration and let others comment on it CLARIFY and summarize by using the information below STEP 4: Care Of A Pregnant Woman With Pre-Eclampsia During Antenatal (10 Minutes) Women with PIH or mild Pre-eclampsia can be advised to rest at home and continue to monitor maternal and fetal condition Attend Antenatal clinic weekly ensuring that the woman has a birth plan and continue with antihypertensive If a woman cannot have Treatment is aimed at managing symptoms and preventing worsening of the condition and complications. Bed rest has the added advantages of reducing oedema by improving the renal circulation, facilitating kidney filtration and producing a diuresis Advice diet rich in protein, fibre and vitamins may be recommended and fluids should be encouraged. STEP 5: Care Of A Pregnant Woman With Severe Pre-Eclampsia & Eclampsia During Antenatal (15 Minutes) Severe pre-eclampsia and eclampsia are managed similarly with the exception that delivery must occur within 24 hours of onset of severe pre-eclampsia versus 12 hours of onset of convulsions in eclampsia All cases of severe pre-eclampsia should be managed actively. Symptoms and signs of “impending eclampsia” (blurred vision, hyperreflexia) are unreliable and expectant management is not recommended. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 75 The management depends upon the severity of the disease so a woman with severe preeclampsia or eclampsia should be admitted for care to multibeded room or single room. Treatment is aimed at managing symptoms and preventing worsening of the condition and complications. She must have continuous care so if staff is few encourage a relative to stay with her who can alert staff in the event of convulsions. o Bed rest The mother should be nursed in bed and will be encouraged to adopt a sitting position or to lie on her side in order to encourage uterine blood flow. Bed rest has the added advantages of reducing oedema by improving the renal circulation, facilitating kidney filtration and producing a diuresis. Except in severe cases the mother may get up for toilet facilities. o Diet Advice diet rich in protein, fibre and vitamins may be recommended and fluids should be encouraged. o Urine Urine should be tested for protein daily and a specimen should be sent to the laboratory if possible so that the levels of protein can be estimated. o Fluid intake and output Fluid should be conscientiously measured. Adequate urine output signifies good renal function; oliguria or urinary suppression may occur if the disease becomes severe. o Blood pressure Blood pressure is ascertained 4 hourly, but will be taken hourly or more frequently if mother is severely affected. o Abdominal examination It will be carried out at least twice daily. Any discomfort, tenderness, or pain experienced by the mother should be recorded and reported immediately to the doctor. o The fetal heart rate The fetal heart should be elicited when abdominal examination is performed. Kicks charts Are maintained to monitor the degree of fetal movement and serial ultrasonic scans are undertaken to assess fetal growth and amounts of liquor if available. STEP 6: Care Of A Pregnant Woman With Severe Pre-Eclampsia And Eclampsia During Intra-Partum And After Delivery (30 Minutes) Once the diagnosis of severe pre-eclampsia (imminent eclampsia) is made, manage as for eclampsia o Shout for help o Keep her in left lateral position o Protect from injury o Ensure the airway is clear—insert an airway if needed NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 76 Give oxygen 4–6 Lts/minutes if available Conduct a rapid evaluation of the general condition including vital signs (pulse, blood pressure and respiration) o Administer magnesium sulphate Give 4 gms (20 ml of 20% solution) IV slowly over 20 minutes; then draw up 10 gms of 50% magnesium sulphate (2 syringes with 10 ml of 50% solution in each) and 1ml of 2% lignocaine injection in the same syringe (loading dose) Give by deep IM injection in each buttock, ensuring sterile technique. If it is not possible to give IV dose, the IM dose should be sufficient. o Commence IV of normal saline solution.(Do not give Ringer’s Lactate) o If diastolic BP is > 110 give Hydralazine 10mg IV slowly over 3–5 minutes, if not possible to give IV, give IM. If hydralazine is not available, give nifedipine 10 mg sub lingual, recheck BP after 30minutes. o If diastolic Blood Pressure remains elevated ≥ 110, repeat IV hydralazine 10mg (can be repeated up to maximum of three doses of hyralazine) continue monitoring BP closely. o Aim for diastolic Blood Pressure between 90–100 mm Hg. o Catheterize with indwelling urethral catheter and commence intake/output chart. o Quick assessment of the foetus, delivery should be done regardless of gestation age, mode of delivery SVD is preferred but if following assessment the cervix is unfavourable caesarean section can be opted. Deliver the baby by the quickest and easiest method, within 6–8 hours of onset of fits. Give magnesium sulphate 5 gm (i.e., 10 ml of 50%) solution as deep IM injection in alternate buttocks with 1 ml of 2% lignocaine in the same syringe every 4 hours or iv 1gm hourly for 24hrs(maintenance dose) Monitor vital signs, respiratory rate, reflexes and foetal heart rate every half an hour. o Note; Before repeating administration of medicine, check that: Respiratory rate is at least 16 per minute Patellar reflexes are present Urinary output is at least 25 ml per hour over 4 hours Assist second stage of labour by doing vacuum extraction if possible Specific management of Pre-eclampsia and Eclampsia o During labour The midwife should remain with the mother throughout labor and delivery The mother should be made as comfortable as possible which will necessitate attention to oral, and body hygiene at regular intervals at regular intervals. The bed linen should be changed frequently as amniotic fluid usually drain throughout Position the mother on her side will prevent supine hypotension o o NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 77 The midwife should encourage the mother to move her legs. If she unable to do so, passive leg exercises will stimulate the circulatory return to the heart The partograph should be strictly followed with increased monitoring of BP (1/2 hrly); fluid output and checking fetal condition Consideration of assisting delivery by vacuum extraction After Delivery o The blood pressure will be recorded after delivery according to BP. o The goal is for the diastolic BP to be maintained between 90-100 mmHg. o If BP is within normal range check at least 4 hourly for 24 hours o If proteinuria has been present the urine should be tested once or twice daily until it is clear and urinary output should be recorded o Any other treatment prescribed should be carried out o Postnatal care will be as normal o The woman and her family should be fully informed of what happened and reassured, answering questions as needed o She should be counseled on maternal and newborn danger signs and family planning. STEP 7: Complications Following Severe Pre-Aclampsia And Eclampsia IntraPartum And After Delivery (20 Minutes) The Effects on the Woman o Respiratory problems (pulmonary edema, asphyxia, aspiration of vomit, bronchopneumonia) o Cardiac problems (heart failure) o Effects on the brain (hemorrhage, thrombosis, edema, stroke) o Renal complications (acute kidney failure) o Hepatic disease (liver failure or subcapsular hematoma/hemorrhage) o HELLP syndrome (hemolysis, elevated liver enzymes, low platelet count) o Coagulopathy (clotting/coagulation failure) o Visual disturbances (temporary blindness, lasting a few hours to up to a week, due to oedema of the retina) o Injuries during convulsions/fits (fractures, aspiration) o Abruption placenta. o Risk of severe pre-eclampsia/eclampsia in subsequent pregnancies o Long-term cardiovascular morbidity. o Death o Note; The main causes of maternal death in eclampsia are intracerebral hemorrhage, pulmonary complications, kidney failure, liver failure and multi-organ system failure (e.g., heart + liver + kidney) Fetal: The perinatal mortality is very high to the extent of about 30–50%. o The causes are: Prematurity for spontaneous or induced, Intrauterine asphyxia due to placental insufficiency arising out of infarction, retroplacental hemorrhage and spasm of uteroplacental vasculature, NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 78 Effects of the drugs used to control convulsions, Trauma during operative delivery. STEP 8: Key Points (10 minutes) Pre-eclampsia and eclampsia are main cause of maternal death and require quality Antenatal care as well as increased community awareness The main two signs and symptoms of Pre-eclampsia and eclampsia includes hypertension and proteinuria All cases of severe pre-eclampsia should be managed actively Treatment is aimed at managing symptoms and preventing worsening of the condition and complications Midwife must give continuous care to the woman so, if number of staff is few encourage a relative to stay with her who can alert staff in the event of convulsions STEP 9: Session Evaluation (5 minutes) What are the principles of caring a woman with eclampsia? What is the drug of choice to control hypertension in mild pre-eclampsia? How do we administer magnesium sulphate in a pregnant woman with eclampsia? What are the maternal complications following eclampsia? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Duttas .D.C, Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contraceptives ( 7th ed). New Delh: India MOHSW. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Handout No. 13.1 How to measure Blood Presure Sphygmomanometers NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 79 There are three types of sphygmomanometersused to measure blood pressure: mercury, aneroid, and digital. Reading blood pressure by auscultation is considered the gold standard . Subject Position: supine, seated, standing. In seated position, the subject's arm should be flexed. The flexed elbow should be at the level of the heart. If the subject is anxious, wait a few minutes before taking the pressure. Procedures To begin blood pressure measurement, use a properly sized blood pressure cuff. The length of the cuff's bladder should be at least equal to 80% of the circumference of the upper arm. Wrap the cuff around the upper arm with the cuff's lower edge one inch above the antecubital fossa. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 80 Lightly press the stethoscope's bell over the brachial artery just below the cuff's edge. Some health care workers have difficulty using the bell in the antecubital fossa, so we suggest using the bell or the diaphragm to measure the blood pressure. Rapidly inflate the cuff to 180mmHg. Release air from the cuff at a moderate rate (3mm/sec). Listen with the stethoscope and simultaneously observe the sphygmomanometer. The first knocking sound (Korotkoff) is the subject's systolic pressure. When the knocking sound disappears, that is the diastolic pressure (such as 120/80). Record the pressure in both arms and note the difference; also record the subject's position (supine), which arm was used, and the cuff size (small, standard or large adult cuff). If the subject's pressure is elevated, measure blood pressuretwo additional times, waiting a few minutes between measurements. A BLOOD PRESSURE OF 180/120mmHg OR MORE REQUIRES IMMEDIATE ATTENTION! Precautions Aneroid and digital manometers may require periodic calibration. Use a larger cuff on obese or heavily muscled subjects. Use a smaller cuff for pediatric patients. For pediatric patients a lower blood pressure may indicate the presence of hypertension. Don't place the cuff over clothing. Flex and support the subject's arm. In some patients the Korotkoff sounds disappear as the systolic pressure is bled down. After an interval, the Korotkoff sounds reappear. This interval is referred to as the "auscultatory gap." This pathophysiologic occurrence can lead to a marked under-estimation of systolic NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 81 pressure if the cuff pressure is not elevated enough. It is for this reason that the rapid inflation of the blood pressure cuff to 180mmHg was recommended above. The "auscultatory gap" is felt to be associated with carotid atherosclerosis and a decrease in arterial compliance in patients with increased blood pressure. Practice Use our aneroid and mercury sphygmomanometers simulators to practice your blood pressure measurement skills. Then take one of our courses that feature blood pressure, auscultation, and other physical examination skills. For pediatric patients, the NIH provides tables which use age, sex and height to interpret blood pressure findings. View our pediatric blood pressure drills for more information. SESSION 14: CARE OF PREGNSNT WOMAN WITH DIABETES MELLITUS AND CARDIAC DISEASE Total Session Time: 120 minutes Prerequisites None NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 82 Learning Tasks At the end of this session a learner is expected to be able: Define diabetes mellitus and cardiac disease Explain the risk factors of diabetes mellitus and cardiac diseases Explain the management of pre-existing diabetes mellitus and gestational diabetes Describe the management of a pregnant woman with cardiac disease Explain the maternal and fetal complications of diabetes mellitus and cardiac diseases Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content 2 40 Brainstorming Definitions diabetes mellitus and cardiac disease 3 10 Lecture discussion risk factors of diabetes mellitus and cardiac diseases 4 10 Lecture discussion Care of pregnant woman with pre-existing diabetes mellitus and gestational diabetes 5 15 Lecture discussion Care of a pregnant woman with cardiac disease 6 30 Lecture discussion maternal and fetal complications of diabetes mellitus and cardiac diseases 7 05 Presentation Key Points 8 05 Presentation Session Evaluation Presentation of session title and learning tasks SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 83 READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definitions Of Diabetes Mellitus And Cardiac Disease (15 Minutes Activity: Brainstorming (5 minutes) ASK students to brainstorm on definition of diabetes mellitus and cardiac disease. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Diabetes mellitus is a chronic metabolic disorder due to either insulin deficiency (relative or absolute) or due to peripheral tissue resistance (decreased sensitivity) to the action of insulin. o The pathophysiology involved are: decreased sensitivity of skeletal muscles and liver to insulin (insulin resistance) Inadequate secretion of insulin (β cell dysfunction). o The defect lies both in insulin secretion and action. o The ultimate effect is the hyperglycemia. o Gestation Diabetes Mellitus is defined as carbohydrate intolerance of variable severity with onset or first recognition during the present pregnancy. The entity usually presents late in the second or during the third trimester. Previously, the definition stipulated that the GTT should come down to normal following delivery. Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. o Cardiovascular disease includes coronary artery diseases (CAD) such as angina Myocardial infarction (commonly known as a heart attack). o Other CVDs include stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, heart arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis. Peripartum cardiomyopathy is defined as cardiac failure occurring in the last month of pregnancy or within five months of delivery, in the absence of any identifiable cause of heart failure. STEP 3: Risk Factors Of Diabetes Mellitus And Cardiac Diseases (15 Minutes) Diabetes Mellitus in pregnancy(GDM) Positive family history of diabetes (parents or sibling). o Family history should include uncles, aunts and grandparents Having a previous birth of an overweight baby of 4 kg or more NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 84 Previous stillbirth with pancreatic islet hyperplasia revealed on autopsy Unexplained perinatal loss Presence of polyhydramious or recurrent vaginal candidiasis in present pregnancy Persistent glycosuria Age over 30 years Obesity Ethnic group (East Asian, Pacific island Cardiovascular Disease The cardiac failure occurs during pregnancy around 30 weeks, during labor and mostly soon following delivery. Factors responsible for cardiac failure: o Advanced age o Cardiac arrhythmias or left ventricular hypertrophy o History of previous heart failure o Appearance of ‘risk factors’ in pregnancy are: infection, anemia hypertension, excessive weight gain and multiple pregnancy o Inadequate supervision. STEP 4: Care Of Pregnant Woman With Pre-Existing Diabetes Mellitus And Gestational Diabetes (30 Minutes) Screening of GDM: Screening strategy for detection of GDM are: o Low risk—Absence of any risk factor as mentioned, blood glucose testing is not routinely required o Average risk—Some risk factors ;perform screening test High risk—Blood glucose test as soon as feasible. o The method employed is by using 50 gm oral glucose challenge test without regard to time of day or last meal, between 24 and 28 weeks of pregnancy. A plasma glucose value of 140 mg percent or that of whole blood of 130 mg percent at 1 hour is considered as cut off point for consideration of a 100 gm (WHO – 75 gm) glucose tolerance test. Figure 8.1. Criteria for Screening Diabetes and Glucose tolerance in g/dl Criteria for diagnosis of impaired glucose tolerance and diabetes with 75 gm oral glucose Time Normal Tolerance Impaired Glucose Tolerance Diabetes Fasting <100 ≥100 and <126 ≥126 2 hours post glucose <140 ≥140 and <200 ≥200 Pre Pregnancy and Pre Natal Care NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 85 Diabetes Mellitus increases chances of complications for both mother and foetus and its incidence is increasing globally. o It is important therefore that good metabolic control is established before and throughout pregnancy. o Women should have access to pre-pregnancy counseling services and ideally meet a diabetic specialist before becoming pregnant. o Insulin dosage is reviewed and an explanation given of the adjustment that will be require during pregnancy. o Women with Type 2 diabetic mellitus (DM) on oral hypoglycemic will need transfer to insulin to prevent the possibility of teratogenesis. o Dietary advice, including weight control and folic acid supplementation, and general health measures are important throughout pregnancy. o This woman needs special ANC and will require more frequent visits in particular: Close monitoring of BP Testing urine at each visit for protein & glucose Monitoring foetal growth and wellbeing noting when the foetus is large for dates which can indicate poor diabetic control Counselling for birth preparedness and complication readiness Intrapartum Care o Ideally labour should be commenced spontaneously at term for women with uncomplicated DM during pregnancy. o Poor diabetes control or deterioration in the maternal or foetal condition may necessitate earlier, planned birth. o Induction of labour may be considered where the foetus is judged to be microsomic or small for dates. o Routine induction of labour at 37-38 weeks gestation is no longer recommended as it does not reduce prenatal mortality rate and is more likely to results in respiratory morbidity. o It may also contribute to high caesarean section rates for diabetic pregnancies compared with normal pregnancies. o The aim of intra-partrum care is to maintain normal-glycaemia in labour (i.e. < 7.0mmol/L). o Maternal hyperglycemia leads to an increase in foetal insulin production, which will cause neonatal hypoglycaemia. o Dehydration must be avoided and a strict input/output chart maintained. o Foetal distress is more common as placental blood flow is reduced and glycosylated haemoglobin decreases oxygen carriage in diabetes pregnancies. o In addition, maternal ketoacidosis may result from dehydration and unstable diabetes. If mother becomes acidotic, ketones will cross the placenta and affect the foetal acidbase status. o Continuous electronic foetal monitoring is recommended if available however the most important activity is close monitoring of the mother and foetus using the partograph. o If the baby is large care must be taken during birth to prepare for possible complications such as shoulder dystocia, also ensure equipment and supplies for newborn resuscitation are available. Postpartum o NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 86 o Immediately after the third stage labour insulin requirements will fall rapidly to prepregnancy levels. o The insulin infusion rate should be reduced by at least 50%. o Carbohydrate metabolism returns to normal very quickly and women can assume their pre-pregnancy insulin regime. o Women with type 2 DM who were previously on oral hypoglycaemia or dietary control need to be controlled prior to recommencing therapy. o Monitoring of blood glucose levels should continue during this interim period. o Breastfeeding should be encouraged in all women with diabetes. o An additional carbohydrate intake may be needed therefore adjust insulin accordingly. o Operative /assisted delivery, together with diabetes, predisposes these women to infection and delayed healing. o The administration of antibiotics may be a useful preventive measure in this instance. o All women should be offered contraceptive advice so that optimum metabolic control is achieved prior to planning next pregnancy. o The issue governing choices of contraception for women with DM are similar to those non-diabetic women. o Women with DM, gestational diabetes should be reviewed at 6 weeks, ideally as a combined diabetes clinic or alternatively by their GP (General Practitioner). STEP 5 Care Of A Pregnant Woman With Cardiac Disease (15 Minutes) Prenatal Care o Women with known heart disease should preconception counseling before becoming pregnant to discuss the risks of condition to pregnancy. o General health advice can be given by a midwife with regard to diet, weight, exercise, rest, and the prevention of anaemia and the avoidance of tobacco, drugs and alcohol. Intra-Partum Care o The first stage of labour In view of the increased cardiac output during labour and immediately after the birth, it is important to plan for and manage labour carefully Optimal management involves monitoring the maternal condition closely; this includes the measurement of vital signs and urine output The partograph must be used to monitor labour and support decision making Fluid balance o Women with significant heart disease require care concerning fluid balance in labour indiscriminate use of intravenous crystalloid fluids will lead to an increase in circulating blood volume, which women with heart disease will find difficult to cope with and they may easily develop pulmonary oedema. o Positioning; Cardiac output is influenced by the position of the labouring woman It is important to remember that woman with heart disease are particularly sensitive to aortocarval compression by the gravid uterus in the supine position This decreases the cardiac output by inhibiting venous return to the heart resulting in maternal hypotension and foetal bradycardia It is preferably that all labouring women, as well as those with heart disease, adopt prop-up or left lateral position in labour that is comfortable. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 87 Second stage of labour o This should be short without undue exertion on the part of mother. o A vacuum extraction should be considered. o Prolonged pushing with breath holding such as the valsalva manoeuvre, which is undesirable for healthy women, may be dangerous for women with heart disease. o It raises the intrathoracic pressure, pushes the blood out of the thorax and impedes venous return, with the results that cardiac output falls. o The midwife should encourage the woman to breathe normally and follow her natural desire to push; giving several short pushes during each contraction. o Care should be taken when the woman in lithotomy, where the lower part of the body is higher than trunk, as this produces a sudden increase in venous return to the heart, which may result in heart failure. Third stage of labour o This is actively managed with oxytocin as the drug of choice due to increased risk of PPH. ergometrine is contraindicated as this act on smooth muscles and will have a direct effect on the heart as well as producing a tonic uterine contraction. o Misoprostol can be used if oxytocin not available. Post-natal care o During the first 48 hours following birth the heart must cope with the extra blood from the uterine circulation and it is important that the midwife monitors the woman’s condition during this time. o Close observation should identify early signs of infection, thrombosis or pulmonary edema. o Breast feeding is encouraged as cardiac output is not affected by lactation although drug therapy for specific heart conditions may need to be reviewed for safety during breastfeeding. o The midwife provides support with breast feeding similar to that with other women, and the importance of rest and adequate diet. o Discharge planning is particularly important for women with heart disease. o The midwife can evaluate the help and support that will be available in the home during postnatal period. o The woman and her partner will need to discuss the implications of a future pregnancy with the cardiologist and obstetrician. o Following this, the midwife can provide advice to the woman and her partner about contraception. STEP 6: Maternal and Fetal Complications Of Diabetes Mellitus And Cardiac Diseases (20 Minutes) Complications of diabetes (Hyperglycemia and adverse pregnancy outcome): o Maternal :During pregnancy: Abortion: Recurrent spontaneous abortion may be associated with uncontrolled diabetes. Preterm labor, may be due to infection or polyhydramious Infection: Urinary tract infection and vulvo vaginitis. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 88 Increased incidence of pre-eclampsia Polyhydramious is a common association with Large baby, large placenta, fetal hyperglycemia leading to polyuria, increased glucose concentration of liquor irritating the amniotic epithelium or increased osmosis, are some of the probabilities. Maternal distress may be due to the combined effects of an oversized fetus and polyhydramious. Diabetic retinopathy, microaneurysms, hemorrhages and proliferative retinopathy Diabetic nephropathy—may lead to renal failure Ketoacidosis o During labor: There is increased incidence of: Prolongation of labor due to big baby. Shoulder dystocia (Shoulder dystocia is due to disproportionate growth with increased shoulder/head ratio. Perineal injuries. Postpartum hemorrhage. Operative interference. o Puerperium: Puerperal sepsis Lactation failure. o Foetal and neonatal complications: Foetal macrosomia (30-40%) due to maternal hyperglycaemia and elevated free fatty acids Congenital malformation due genetic susceptibility and hyperglycemia Abortion Intrauterine foetal death Birth injuries (Shoulder dystocia leads to brachial plexus injury) Cardiac dieses Complications o Mternal Congenital cardiac failure Pulmonary oedema Pulmonary Embolism Aenaemia Maternal Death o Foetal complication Abortion Intrauterine growth restriction (IUGR) Premature delivery Intra-uterine death(IUFD) Neonatal death Foetal congenital heart disease STEP 7: Key Points (5 minutes) Gestation Diabetes Mellitus is a carbohydrate intolerance of variable severity with onset or first recognition during the present pregnancy. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 89 The entity usually presents late in the second or during the third trimester. Previously, the definition stipulated that the GTT should come down to normal following delivery. Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. Peripartum cardiomyopathy is a cardiac failure occurring in the last month of pregnancy or within five months of delivery, in the absence of any identifiable cause of heart failure. Diabetes Mellitus increases chances of complications for both mother and foetus and its incidence is increasing globally. It is important therefore that good metabolic control is established before and throughout pregnancy. Women should have access to pre-pregnancy counseling services and ideally meet a diabetic specialist before becoming pregnant. STEP 8: Session Evaluation (5 minutes) What are the roles of midwife in caring for a woman with cardiac disease in labour? What are the aspects of antenatal care need to be adapted for a woman with diabetes mellitus? What are foetal complications in woman with gestational diabetes? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Duttas .D.C, Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contraceptives ( 7th ed). New Delh: India MOHSW. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. SESSION 15:CARE OF A WOMAN WITH HYPEREMESIS GRAVIDARUM Total Session Time: 60 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define hyperemesis gravidarum Explain causes and diagnosis of hyperemesis gravidarum Outline signs and symptoms of hyperemesis gravidarum Describe the management of a pregnant woman with hyperemesis gravidarum NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 90 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Brainstorming/presentation Definition of hyperemesis gravidarum Causes and diagnosis of hyperemesis gravidarum 3 10 Lecture discussion 4 10 Presentation Outline the sign and symptoms of hyperemis gravidarum 5 20 Lecture discussion Care of a pregnant women with hyperemesis gravidarum 6 05 Presentation Key Points 7 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition Of Hyperemesis Gravidarum (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on the defition of hyperemesis gravidarum time them with to respond NMT ALLOW 06101: Care of for a Woman Abnormal Pregnancy, Labour and Puerperium WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below 91 Hyperemesis gravidarum Is an excessive nausea and vomiting that start between 4-10 weeks gestation, and resolvebefore 20 weeks. STEP 3: Causes And Diagnosis Of Hyperemesis Gravidarum (10 Minutes) The causes of hyperemesis is uncertain, with multi-factorial causes such as: o Hormonal /Endocrine High human chorionic ganadotrophin (hCG) stimulates the chemoreceptor trigger zone in the brain stem including the vomiting center. o Allergy to the corpus luteum or the released hormones. o Nervous and psychological due psychological rejection of an unwanted pregnancy o Deficiency of: adrenocortical hormone and /or, vitamin B6 and B1 o Hyperemesis occur more often where mothers have a multiple pregnancy, or a hydatidiform o Simultaneously occurrence of hyperthyroidism and hyperemesis suggest transient thyroid dysfunction as a possible cause STEP 4: Sign And Symptoms (10 Minutes) The patient cannot retain anything in her stomach. o Vomiting occurs through the dayand night even without eating. Thirst, constipation and oliguria. In severe cases, vomitus is bile and/ or blood stained. Finally, there are manifestations of Werniche’s encephalopathy as drowsiness,nystagmus and loss of vision then coma. Manifestations of starvation and dehydration: o Loss of weight. o Sunken eyes. o Dry tongue and inelastic skin. o Pulse: rapid and weak. o Blood pressure: low. o Temperature: slight rise STEP 5: Care Of A Pregnant Woman With Hyperemesis Gravidarum (20 Minutes) The woman should be hospitalized for observation and fluid therapy NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 92 Calm reassurance and sensitive information-giving should be accompanied by competent attention to physical needs. On arrival in hospital blood will be taken to determine the plasma electrolytes. The potassium and sodium levels will be corrected by intravenous infusion( Ringers lactate) The infusion will continue until hydration and electrolytes return to normal. Vitamins B12 and C, folic acid and iron will be required to correct anaemia. The pregnant woman should be given promethazine if vomiting persists and a sedative may be given to produce rest. Advice the woman to take small quantity of meals frequently. Monitor vital sign at least 4 hourly Test urine twice for specific gravity, acetone, sugar and protein The intake and output of fluids including vomitus will need insidious monitoring andrecording. Once vomiting has ceased for a period of 24 hrs, oral fluids may be commenced and if these are tolerated a light diet may follow. Normal food is gradually introduced and intravenous therapy discontinued. Note o Very occasional the disorder fails to improve with the treatment outlined above and o The mother will subside into coma and be in danger of dying. STEP 6: Key Points (5 minutes) Without dehydration the woman can be treated as an outpatient with the same drugs. If not Responding admit to the hospital Morning sickness is the nausea felt by about 50% of pregnant women on getting up in the morning, actual vomiting is called emesis gravidarum. These two conditions usually start between the 4th and 6th weeks of pregnancy and improve or disappear about the 12th week. In hyperemesis gravidarum the vomiting is not confined to the morning but it is repeated throughout the day until it affects the general condition of the patient STEP 7: Session Evaluation (5 minutes) What is hyperemesis gravidarum What are the possible causes or aetiology of hyperemesis gravidurum References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 93 Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. SESSION 16: CARE OF A WOMAN WITH DISORDERS OF AMNIOTIC FLUID (POLYHYDRAMIOUS AND OLIGOHYDRAMNIOS) Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define the terms polyhydramious and oligohydramnios State causes and predisposing factors of polyhydramious and oligohydramnios Explain the diagnostic measures for polyhydramious and oligohydramnios Describe the management of a pregnant woman with polyhydramious and oligohydramnios State the complications associated with polyhydramious and oligohydramnios Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Content NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 94 1 05 Presentation Presentation of session title and learning objectives 2 05 Definition of polyhydramious and oligohydramnios 3 05 Brainstorming Presentation Lecture/discussion 4 15 Lecture/discussion Management of a woman with polyhydramious 5 15 Lecture/discussion Management of a woman with oligohydramnios 6 05 Presentation Complications associated with polyhydramious and oligohydramnios 7 05 Presentation Key Points 8 05 Presentation Session Evaluation Causes and predisposing factors of polyhydramious and oligohydramnios SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition Of Polyhydramious And Oligohydramnios (5 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the definitions of polyhydramnious and oligohydramnios ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 95 Polyhydramious (hydramnios) is an excessive amount of amniotic fluid. o Is defined as the amount of amniotic fluid which exceeds 1500 ml. o It may not be clinically apparent until it reaches 3000 ml. Oligohydramnios is an abnormally small amount of amniotic fluid. STEP 3: Causes And Predisposing Factors Of Polyhydramious And Oligohydramnios (5 Minutes) Causes and predisposing factors of polyhydramious Most polyhydramious is of unknown etiology. The following conditions are likely to result in a higher incidence of polyhydramious: o Multiple pregnancy (especially with monozygotic twins) o Diabetes o Erythroblastosis o Fetal malformations (especially of the gastrointestinal tract—e.g., tracheoesophageal fistula—or central nervous system—e.g., anencephaly, meningomyelocele) Causes and predisposing factors of oligohydramnios The condition is frequently caused by uteroplacental insufficiency, which thereby means that a decreased fluid volume may be associated with a marked increase in perinatal mortality. The following conditions have a higher incidence of oligohydramnios: o Congenital anomalies (e.g., renal agenesis, Potter’s syndrome) o Viral diseases o Intrauterine growth restriction (IUGR) o Uteroplacental insufficiency o Early rupture of the fetal membranes (24 to 26 weeks) o Response to indocin as a tocolytic o Fetal hypoxia o Meconium-stained fluid and meconium aspiration o Postmaturity syndrome STEP 4: Care of a Woman with Polyhydramious (15 minutes) Assessing the woman thourough On history taking the woman will complain of o Breathlessness and discomfort o Abdominal pain in severe cases o Exacerbation of associated symptoms of pregnancy such as; indigestion, heartburns and constipation. o Lower swelling and varicosities of vulva and lower limbs Abdominal examination o Inspection The uterus is larger than expected for the period of gestation and is globular in shape NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 96 Abdominal skin appears stretched and shiny with marked stripe gravidarum and obvious superficial blood vessels o Palpation Uterus feels tense and is difficult to feel the Fetal parts Fetal ballottement between the two hands Fluid thrill may be elicited by placing a hand on one side of the abdomen and taping the other side with fingers Measurement of abdominal girth In cases of acute hydramnios it is done in order to observe the rate of increase o Auscultation May be difficult if the quantity of fluid allows the foetus to move away from the stethoscope o Ultrasound Is used to confirm the diagnosis of polyhydramious Management of polyhydramious The aim of management is to relieve maternal symptoms and optimize the length ofgestation, prolonging it if safe. When the cause is already determined o The mother will usually be admitted to a consultant obstetric unit. o Subsequent care will depend on the mother’s condition, the cause of thepolyhydramious and the stage of pregnancy. o The mother should rest in bed. An upright position will help to relieve any dyspnea and she may be given antacids to relieve heartburn and nausea. o Acute polyhydramious is managed by amniocentesis but the outlook is very poor. o The mother may need to have labour induced in late pregnancy if the symptomsbecome worse. o Labour is usually normal but the midwife should be prepared for the possibility ofpostpartum haemorrhage. o The baby should be carefully examined for abnormalities and a wide orogastric tubemust be passed for about 10-12cm. in order to confirm the patency of theoesophagus. STEP 5: Care of a Woman with Oligohydramnios (15 minutes) Assessment of the mother History taking o The woman who had a previous normal pregnancy may have noticed a reduction in fetal movements. o History of vagina leakage Abdominal Examination o Inspection The uterus appears smaller than expected for the period of gestation. o Palpation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 97 The uterus is small and compact and fetal parts are easily felt Breech presentation is possible. o Auscultation is normal Diagnosis o Ultrasonic scan will exclude Intra-uterine growth restriction. Renal abnormality. Coexisting fetal or placental conditions or complications. o Screen for diabetes and Rh iso-oimmunization. Care of woman with oligohydramnios The woman should be admitted for investigations which will include placental function tests. If there is no foetal abnormality the pregnancy will be allowed to continue Labour may begin early or may be induced because of the possibility of placental insufficiency. Epidural analgesia may be indicated because uterine contractions may be very painful. Impairment of placental circulation may result in foetal hypoxia. Constriction rings are a possibility due to the small amount of amniotic fluid. In rare cases the membranes may adhere to the foetus. Reassure the woman and the patner on the condition STEP 6: Complications of Polyhydramious and Oligohydramnios (5 minutes) Polyhydramious complications o Preterm labor (due to over distention of the uterus) o Maternal dyspnea and shortness of breath o Fetal malpresentations o Abruptio placenta o Cord prolapse o Uterine dysfunction during labor (due to over distention of the uterus) o Immediate postpartum hemorrhage as a result of uterine atony from over distention Oligohydramnios complications o Lack of amniotic fluid reduces the intra-uterine space and causes compression deformities. o The baby has a squashed-looking face, flattening of the nose, micrognathia and talipes. o The skin is dry and leathery in appearance. STEP 7: Key points (5 minutes) Polyhydramious (hydramnios) is an excessive amount of amniotic fluid. When polyhydramious is diagnosed, consultation with a consulting physician is indicated. The woman especially needs emotional support if congenital anomalies are present. Women with severe polyhydramious have a number of mechanical difficulties and discomforts for which the midwife can provide relief measures. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 98 Oligohydramnios is an abnormally small amount of amniotic fluid. Oligohydramnios is a significant finding suggestive of post-maturity syndrome in a postdate pregnancy. STEP 8: Session Evaluation (5 minutes) What are the differences between polyhydramious and oligohydramnios? What are the predisposing factors of polyhydramious? What are the complications of polyhydramious? What are the complications of Oligohydramnios? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. Varney, H., Burst, V., Kriebs, J. M., &Gegor, C. L. (2004). Varney's midwifery. Jones & Bartlett Learning. SESSION 17: CARE OF A WOMAN WITH ABNORMAL UTERINE ACTION Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define abnormal uterine action Describe types of abnormal uterine action Describe causes of abnormal uterine action Care of a pregnant woman with abnormal uterine action NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 99 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Presentation Defintion of abnormal uterine action 3 15 Brainstorming/presentation Types of Abnormal Uterine action 4 50 Lecture discussion Care of Woman with Abnormal Uterine Action 5 35 Small group discussion/ Lecture discussion Cervical dystocia 6 05 Presentation Key Points 7 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definitio of Uterine Action (5 Minutes) Abnormal uterine action is any deviation from normal pattern of uterine contractions affecting the normal course of labour. Its one of the factors causing dystocia (difficult labor) in which uterine forces are insufficiently strong orinappropriately coordinated to efface and dilate the cervix (uterinedysfunction). NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 100 STEP 3: Types of Abnormal Uterine Action (15 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm describe the types of anormal uterine action. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Classifications or Types of abnormal uterine action Over-efficient uterine action o Precipitate labour in absence of obstruction o Exessive contraction and retraction in presence of obstruction Inefficient uterine Action o Hypotonic inertia o Hyprtonic inertia Colyky uterus Hyperctive lower segment o Constriction ring Cervical Dystocia STEP 4: Care of Woman with Abnormal Uterine Action( 50 minutes) Over-efficient uterine action Precipitate labour Is the type of labour due to strong coordinate uterine contractions from the onset of labour, which results in abnormally rapid progress and delivery within three hours of its commencement (excessive with or without obstruction) Causes of precipitate labour o It is more common in multiparas when there are; Strong uterine contractions Small sized baby Roomy pelvis Minimal soft tissue resistance Diagnosis o It is a retrospective diagnosis as the patient is usually seen in the second or third stages of labor NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 101 o If seen during the 1st stage of the labor, the partograph will show rapid progress of cervical dilation and effacement o If seen after delivery, examination of the mother and infant should be perfomed Care of a woman with precipitate labour o The with past history of precipitate labour, should be admitted to the hosp at the first perception of labour pain o Inhalation anaesthesia as nitrous oxide and oxygen is given to slow the course of labour. o Tocolytic agents as ritodrine may be effective o Episiotomy may be preformed to avoid perineal lacerations and intracranial haemorrhage o After delivery exploration of the birth canal for any injury should be done and manage accordingly o Give the mother prophylactic antibiotics if delivery occurred in unsuitable conditions o Proper examination of the fetus for detection of injury and any complications Complication of precipitate labour o Maternal Lacerations of the cervix, vagina and perineum Shock Inversion of the uterus Postpartum haemorrhage Sepsis due to lacerations and inappropriate surroundings o Foetal Foetal Intracranial haemorrhage due to sudden compression and decompression of the head Foetal asphyxia due to strong frequent uterine contractions reducing placental perfusion and lack of immediate resuscitation Avulsion of the umbilical cord Foetal injury Overstimulation of the uterus Excessive use of syntocinon or prostaglandin may result in titanic contractions with inadequate periods of relaxation between them Complications o Fetal hypoxia due to uterine spasm which reduces the placento-fetal oxygen o Precipitate labour due to overstimulation of the uterus o Progress of labour may be slow due to lots of retraction o Uterine rupture in cases of some degrees of disproportion Management o Inform the doctor for immediate management o The administration of syntocinon or prostaglandins must be stopped at once o Nurse the mother on her left side and monitor fetal heart rate frequently o Puffs of a ventolin inhaler to reduce severe contraction o Administer oxygen in case fetal bradycardia NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 102 Inefficient uterine contraction Definition Uterine action is said to be inefficient when the contractions do not effectively dilate the cervix. Progress in labour is slow and length of labour is prolonged Classification Hypotonic uterine inertia o The contractions are weak, short and infrequent o The result is slow dilatation of the cervix or non o Hypotonic uterine action may be primary; occurring from the onset of labour or secondary; developing during the course of the previously normal labour o The cause of primary hypotonic is unknown but it is most commonly found in primgravida o Secondary hypotonic uterine actionmay be due to cephalopelvic disproportion, malpresentation or malposition of the fetal occiput. o Management of hypotonic uterine action Encouragement and support from the midwife is necessary Perform vaginal examination to exclude disproportion or malpresentation or malposition and manage according to the case Proper management of the first stage Prophylactic antibiotics in prolonged labour particularly if the membranes are ruptured. Artificial rupture of membrane can be done if still intact providing that; Vaginal delivery is amenable The cervix is more than 3 cm dilatation The presenting part occupying well the lower uterine segment. Set intravenous infusion of cyntocinon, providing that there is no contraindication for it. Maintain fluid and electrolyte balance and give analgesia as required Perform vaginal examination 2-4hourly interval to assess cervical dilatation and use the partograph to monitor labour progress You can perform operative delivery vaginally either by forceps, vacuum or breech extraction according to the presenting part and its level providing that:Cervix is fully dilated and vaginal delivery is amenable. o Complication of hypertonic inertia Nervousness and anxiety Exhaustion and starvation ketoacidosis Prolonged second stage Increased liability for instrumental delivery and C/S Retention of placenta and postpartum haemorrhage NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 103 Subinvolution of the uterus Risks of abuse of uterine stimulants Hypertonic uterine inertia ( Incoordinate Uterine action ) o There are of two types o Colicky uterus: incoordination of the different parts of the uterus in contractions. o Hyperactive lower uterine segment: so the dominance of the upper segment is lost. The condition is more common in primigravidae and characterized by: Labour is prolonged. Uterine contractions are irregular and more painful. The pain is felt before and throughout the contractions with marked low backache often in occipitoposterior position Slow cervical dilatation. Premature rupture of membranes. Foetal and maternal distress. o Care of a woman with hypertonic inertia Inform the doctor Reassurance to the women is important to promote comfort as possible Perform vaginal examination to exclude disproportion or malpresentation or malposition Proper management of the first stage Prophylactic antibiotics in prolonged labour particularly if the membranes are ruptured Give intravenous infusion such as Hartmann’s solution to correct ketoacidoci’s. Fluid balance chart is kept and all specimens of urine are tested for presence of ketones. Frequent mouth wash is given so that woman’s mouth remains moist and fresh. Pain relief is essential to rest the woman from pain. Monitor fetal heart and uterine contractions continuously to exclude fetal distress. Membranes may be ruptured artificially, and a low-dose of syntocinon infusion may be commenced to stimulate normal uterine contractions if the patient is eligible. Virginal examinations are performed at 2-4 hourly intervals to assess the progress Plot the findings on the partograph Caesarean section may be performed in case of poor progress with syntocinon, disproportion or foetal distress before full cervical dilatation STEP 5: Cervical dystocia (35Minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 104 Activity: Small Group Activity (10 minutes) DIVIDE students depending on the size of the class. ASK students to explain about cervical dystocia based on the following questions each group working on one question. What is cervical dystocia Types of cervical dystocia Care of a woman with cervical dystocia Complication of cervical dystocia ALLOW the groups to work together to come up with answers to the question above. ALLOW groups 5 minutes for this exercise. ASK students to report back the care plan per group. The following part of the presentation has more details on cervical dystocia APPRAISE the students PROVIDE feedback by summarizing the students’ answers Cervical dystocia is the failure of the cervix to dilate within a reasonable time despite of good uterine contractions Types of cervical dystocia o Organic (secondary) which is due to Cervical stances as a sequel to previous amputation, scarring, cone biopsy, extensive cauterization or obstetric trauma. Organic lesions as cervical myoma or carcinoma o Functional (primary) In spite of the absence of any organic lesion and the well effacement of the cervix, the external os fails to dilate. This may be due to lack of softening of the cervix during pregnancy or cervical spasm resulted from overactive sympathetic tone. Also may be due to previous history of failure of external os to dilate in previous birth, rigid cervix, insufficient uterine contractions, malpresentations and malposition Care of a woman with cervical dystocia o All cases of dystocia are an obstetric emergency o The woman should be admitted in the labour unit and the obstetrician should be present. o Anesthetist and pediatrician should be informed o Oxytocin can be used if abnormal uterine contraction are the cause of dystocia NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 105 o Assisted delivery may be required. o The mother may need urgent cesarean section Complication of cervical dystocia o Perinatal morbidity and mortality from hypoxia and acidosis o Brachial plexus injury o Postpartum haemorrhage o Perineal tear STEP 6: Key points(5 minutes) • Uterine action is said to be inefficient when the contractions do not effectively dilate the cervix. • Progress in labour is slow and length of labour is prolonged. • In hypertonic uterine action the fundal dominance is lost and the contractions start and last longer in the lower segment. • Progress in labour is slow and length of labour is prolonged • Cervical dystocia means failure of the cervix to dilate despite good uterine contraction • Excessive use of syntocinon or prostaglandin may result in titanic contractions with inadequate periods of relaxation between them STEP 6: Evaluation (5 minutes) What is the classification of abnormal uterine action? What is the most common complication in all the classifications of abnormal uterine action? What are the general care you can give to a pregnant woman with any abnormal uterine action? References Advanced life saving skills (2005) reproductive child health section Dar-es -Salaam: Tanzania, volume 2 Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dares Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 106 Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. SESSION 18: CARE OF A WOMAN WITH PROLONGED LABOUR Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define prolonged labour Explain prolonged first stage of labour State the possible causes of prolonged first stage of labour Describe prolonged second stage of labour State causes of prolonged second stage of labour Explain the management of prolonged labour Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Partograph Anatomical chart Session Overview Box Step Time (min) Activity/ Method Content NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 107 1 05 Presentation Presentation of session title and learning objectives 2 05 Definition of prolonged labour 3 25 Brainstorming Presentation Lecture/discussion 4 15 Lecture/discussion Prolonged second stage of labour (causes and care) 5 05 Presentation Key Points 5 05 Presentation Session Evaluation Prolonged first stage of labour(causes and care) SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Prolonged Labour (5 minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on definition of prolonged labour ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Definition of prolonged labour The labor is said to be prolonged when the combined duration of the first and second stage is more than the arbitrary time limit of 18 hours. The prolongation may be due to protracted cervical dilatation in the first stage and/or inadequate descent of the presenting part during the first or second stage of labor. Labor is considered prolonged when the cervical dilatation rate is less than 1 cm/hr and descent of the presenting part is < 1 cm/hr for a period of minimum 4 hours observation. STEP 3: Care of a Woman with Prolonged First Stage of Labour (25 minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 108 Causes of prolonged labour in the first stage Any one or combination of the factors in labor could be responsible. Failure to dilate the cervix is due to: o Fault in power: Abnormal uterine contraction such as uterine inertia (common) or incoordinate uterine contraction o Fault in the passage: Contracted pelvis, cervical dystocia, pelvic tumor, or even full bladder o Fault in the passenger: Malposition (OP) and malpresentation (face, brow), congenital anomalies of the fetus (hydrocephalus). o Too often deflexed head, minor degrees of pelvic contraction and disordered uterine action have got sinister effects in causing non-dilatation of the cervix. Early administration of sedatives and analgesics before the active labor begins. The first stage of labour is divided into a latent and active phase. Prolonged latent phase o Mean duration of latent phase is about 8 hours in a primi and 4 hours in a multi. o A latent phase that exceeds 20 hours in primigravidae or 14 hours in multiparae is abnormal. o During the latent phase the uterus contracts regularly, and the mother experiences discomfort and pain. o The cervix effaces and dilation occurs. o The duration of the latent phase will vary according to each individual and with parity. o A prolonged latent phase of labour can be inaccurately diagnosed when the mother is in false labour. o The causes include: Unripecervix malposition and malpresentation cephalopelvic disproportion premature rupture ofthe membranes. Prolonged active phase o The active phase is distinguished by an increased rate of dilatation of the cervix, with descent of the presenting part. o Slow progress may be defined either as total duration of hours in labour or as failure of the cervix to dilate at a fixed rate per hour. o A prolonged active phase is caused by a combination of factors including the cervix, the uterus, the fetus and the mother’s pelvis. o An interval of 4 hours is allowed to diagnose delay in active phase and then appropriate intervention is done. o Prolonged active phase may be divided into: Protracted active phase: When the rate of cervical dilatation is < 1.2 cm/hr in a primipara and < 1.5 cm/hr in a multipara. A protracted active phase may be due to: Inadequate uterine contractions Cephalopelvic disproportion Malposition (OP) or malpresentation (brow) Epidual anesthesia. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 109 Arrest disorder: Arrest of dilatation is defined when no cervical dilatation occurs after 2 hours in the active phase of labor. It is commonly due to inefficient uterine contractions. No descent for a period of > 1 hour is called arrest of descent. It is commonly due to CPD. Care of a woman with prolonged first stage of labour Vaginal examination is done to verify the fetal presentation, position and station. The causes of slow labour must be identified before deciding on management. Oxytocin infusion may be used to stimulate uterine contraction. If no progress despite good uterine contraction caesarean section must be done. The midwife should help the woman to adopt comfortable position. Reassurance and support is necessary. Effective pain relief is given by intramuscular pethidine or by regional (epidural) analgesia. Give Intravenous infusion to correct fluid and electrolyte balance and to give energy. Encourage the woman to empty bladder regularly Test urine for ketones Monitor Intake and output chart. Give sips of water only especially if general anaesthesia is required for delivery Observation of Vital signs is Significant. High vaginal swab may be taken for laboratory Investigation (if membrane ruptured). Broad – Spectrum antibiotics may be offered prophylactically in the hope of preventingmaternal uterine infection. Fetal Condition Monitor fetal heart continuously. Observe the amniotic fluid for the presence of meconeum. Prevent aspiration during delivery. STEP 4:Care of a Woman with Prolonged Second Stage of Labour (15 minutes) Mean duration of second stage is 50 minutes for nullipara and 20 minutes in multipara. Prolonged second stage is diagnosed if the duration exceeds 2 hours in nullipara and 1 hour in a multipara when no regional anesthesia is used. One hour or more is permitted in both the groups when regional anesthesia is used during labor Causes of prolonged labour in the second stage Ineffective contractions Poor maternal effort Loss of or absence of a desire to push cause by epidural analgesia A full bladder or a full rectum can also impede progress A large fetus, malpresentation or malposition may account for delay A reduced pelvic outlet, in association with an occipitoposterior position, may result in deep transverse arrest. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 110 Care of a woman with prolonged second stage of labour A vaginal examination should be carried out to confirm position, attitude and station of the presenting part. The fetal heart should be auscultated after every contraction or electronic monitoring used. In the presence of inefficient uterine contractions an infusion of oxytocin should be commenced. Assisted delivery (ventouse) will be utilized where the pelvic outlet is adequate and vaginal birth can be safely carried out. Operative delivery may be necessary where there is evidence of CPD. Continue monitoring of maternal and fetal condition Complications Oedema and lacerations caused by prolonged pressure of the fetal head on the vaginal walls and pelvic floor muscle. Uterine prolapse, cystocele or rectocele may occur. STEP 5: Key points (5 minutes) The labor is said to be prolonged when the combined duration of the first and second stage is more than the arbitrary time limit of 18 hours. The prolongation may be due to protracted cervical dilatation in the first stage and/or inadequate descent of the presenting part during the first or second stage of labor. Labor is considered prolonged when the cervical dilatation rate is less than 1 cm/hr and descent of the presenting part is < 1 cm/hr for a period of minimum 4 hours observation. Prolonged labor is not synonymous with inefficient uterine contraction. Inefficient uterine contraction can be a cause of prolonged labor but labor may also be prolonged due to pelvic or fetal factor. Step 6: Session Evaluation (5 minutes) What is prolonged labour? What are the causes of prolonged labour? What is prolonged first stage of labour? What is prolonged second stage of labour? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 111 Dutta, D. C. (2013). Text Book of Obstetrics: Including Perinatology and Contraception 7 th Edition. New central book agency.Jaypee Brothers Medical Publishers (P) Ltd. India. SESSION 19: CARE OF A WOMAN WITH OBSTRUCTED LABOUR Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define obstructed labour List causes of obstructed labour Identify signs and symptoms of obstructed labour Explain the management and prevention of obstructed labour State complications of obstructed labour Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Pelvic model and fetus Partograph Session Overview Box Step Time (min) 1 05 2 05 3 05 Activity/ Method Presentation Content Brainstorming Presentation Lecture/discussion Definition of obstructed labour Presentation of session title and learning objectives Causes of obstructed labor NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 112 4 10 Lecture/discussion Signs and symptoms of obstructed labour 5 20 Buzzing Lecture/discussion Management and prevention of obstructed labour 6 05 Presentation Complications of obstructed labour 7 05 Presentation Key Points 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Obstructed Labour (5 minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on the defition of obstruced labour ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Definition of obstructed labour Obstructed labor is one where in spite of good uterine contractions, the progressive descent of the presenting part is arrested due to mechanical obstruction. This may result either due to factors in the fetus or in the birth canal or both, so that further progress is almost impossible without assistance. The obstruction usually occurs at the pelvic brim but may occur at the outlet-for example deep transverse arrest in an android pelvis. STEP 2: Causes of Obstructed Labour (5 minutes) The common causes of obstructed labour include: Cephalopelvic Disproportion NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 113 o The fetus may be large e.g. in diabetes mellitus mothers. o Pelvis may be contracted or previously fractured pelvis. Malpresentation o Brow presentation o Persistent mentoposterior position o Shoulder presentation or arm prolapse Deep Transverse Arrest o Outcome of an occipito posterior position Fetal Abnormalities o A hydrocephalic fetus o Conjoin twins (abdominal wall of twins attached together) o After coming head in breech presentation. o Locked Twins Pelvic mass o Cervical fibroids o An ovarian tumour o Tumor of the bony pelvis Stenosis of the cervix or vagina Tight perineum Step 4: Signs and Symptoms of Obstructed Labour (10 minutes) Early Signs The presenting part does not enter the pelvic brim despite of good contractions The midwife should exclude full bladder, a loaded rectum and large amount of amnioticfluids; causes non – engagement. The Cervix dilates slowly, hangs loosely like an empty sleeve and presenting part cannotdescend. Late Signs A woman admitted late in labour ward from home or arise only in a badly management orneglected labour On general examination the woman is: o Dehydrated-dry tongue and cracked lips o Ketotic o Severe pain o Rapid pulse rate o Has pyrexia o Low urine output – contain ketones or blood stained. o Fetal heart sound cannot be heard. o Rupture of the uterus can cause maternal shock. o Signs of fetal distress. o Uterus mouldedround the fetus and it fails to relax properly between contractions. o Lower segment becoming progressively thinner and longer, upper segment shorterand thicker. o A physiological retraction ring, or Bandl’s ring, it is similar to a full bladder. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 114 Vaginal examination o a prolapsed arm or shoulder presentation o The vagina is hot and dry the presenting part is high and feels wedged and immovable and oedematous o Excessive molding of the fetal skull and a large caput succedaneum is present o Cervix is fully or partially dilated, oedematous and hanging. o The membranes are ruptured. o The presenting part is high and not engaged or impacted in the pelvis. Step 5: Care and Prevention of a woman with Obstructed Labour (20 minutes) Activity: Buzzing (10 minutes) TELL the students to pair up and discuss on the management and prevention of Obstructed labour (5 minutes) ALLOW few students to respond and let other pairs provide unmentioned responses CLARIFY and summarize by using the information below Care of a woman with obstructed labour The underlying principles of management are: o To relieve the obstruction at the earliest by a safe delivery procedure o To combat dehydration and ketoacidosis o To control sepsis. Midwife should start resuscitating the patient; the doctor who is responsible for the further management should be called at once. Resuscitation o Put up an IV drip with a large (No 18) needle or cannula o If she is mainly dehydrated and exhausted give sodium lactate or normal saline one or two litres in about 6 hours. o If she is shocked run in saline or sodium lactate as fast as possible. Antibiotics o Most patients will need antibiotics for examples: X-pen 5 MU IV stat, continue 2 MU IV 6 hourly plus streptomycin 1 g IM stat, continue 1 g IM daily or chloramphenicol 1 g IV stat, followed by 0.5 g IV 6 hourly. Delivery o If the obstruction cannot be overcome by manipulation or instrumental delivery. o Caesarean section should be performed as soon as possible if the baby is alive; pre operation and nursing management (To see C/S emergency). o If ruptured uterus or seems likely do laparatomy. It is lifesaving whether baby alive or dead. o If uterus seems intact but the baby is dead, cephalic presentation – cervix 7 cm craniotomy. Prevention of obstructed labour NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 115 Proper history taking of previous deliveries e.g. prolonged labour, difficult deliveries babies with weight over 4.5 kg.at birth. Antenatal detection of the factors likely to produce prolonged labor (big baby, small women, malpresentation and position). Continuous vigilance, use of partographand timely intervention of a prolonged labor due to mechanical factors can prevent obstructed labor. Failure in progress of labor in spite of good uterine contractions for a reasonable period (2–4 hours) is an impending sign of obstructed labor. If the presenting part fails to advance during second stage of labour despite of good contractions medical aid should be summoned. Step 5: Complications of Obstructed Labour (5 minutes) Maternal : o Maternal distress and ketoacidosis. o Rupture uterus. o Necrotic vesico -vaginal fistula. o Infections as chorioamnionitis and puerperal sepsis. o Postpartum haemorrhage due to injuries or uterine atony. Foetal: o Asphyxia. o Intracranial haemorrhage from excessive moulding. o Birth injuries. o Infections. Step 6: Key Points (5 minutes) Obstructed labor is one where in spite of good uterine contractions, the progressive descent of the presenting part is arrested due to mechanical obstruction. Effects of obstructed labor are both on the mother and the fetus. Management is primarily aimed in prevention. The actual management is to relieve the obstruction and to deliver the fetus safely . Step 7: Session Evaluation (5 minutes) What is obstructed labour? What are the signs and symptoms of obstructed labour? What are the complications of obstructed labour? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 116 MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. Dutta, D. C. (2013). Text Book of Obstetrics: Including Perinatology and Contraception 7th Edition. New central book agency. Jaypee Brothers Medical Publishers (P) Ltd. India. SESSION 20:CARE OF A WOMAN UNDERGOING VACUUM ASSISTED DELIVERY AND CAESAREAN SECTION Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define the term vacuum extraction. Explain the indications and contraindications for vacuum extraction. Explain the procedure of vacuum extraction. List the complications of vacuum extraction Define caesarean section Describe the types of caesarean section Explain the indication and contraindication of caesarean section Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Equipment for vacuum extractions NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 117 Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Brainstorming/presentation Definition of vacuum extraction The indication and contraindication of vacuum delivery 3 10 Lecture discussion 4 50 Presentation /demonstration Procedure of vacuum extraction 5 10 Presentation Complication of vacuum extraction 6 30 Lecture discussion Caesarean section 7 05 Presentation Key Points 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of vacuum extraction (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on the defition of vacuum extraction. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 118 Vacuum assisted birth or vacuum extraction is a method of birth involving the attachment of a vacuum cup to the fetal head and using negative pressure to assist in the birth of the head. o Vacuum extraction (ventouse delivery) is used when there is delay in the second stage of labour when the head is engaged and no cephalo pelvic disproportion. o The cup cleaves to the baby’s scalp by suction and is used to assist maternal effort. STEP 3: Indication and contraindication of vacuum extraction (10 Minutes) Indication Mild fetal distress Delay in second stage of labour Maternal exhaustion Malposition: occipitolateral and occipitoposterior position Prerequisites for use Vertex presentation Ruptured membranes Cervix full dilated No fetal head palpable above symphysis pubis Empty bladder Absence of CPD The woman is prepared in a lithotomy position to allow sufficient traction. Contraindications No contractions Cephalo-pelvic disproportion Foetal skull moulding 2+ or more Excessive caput Non-vertex presentation Incomplete cervical dilatation Premature fetus STEP 4: Procedure Of Vacuum Extraction (20 Minutes) Watch the following link for video showing the demonstration of vacuum extraction (https://www.youtube.com/watch?v=8Fq_JR_5vCo) Equipment o A delivery tray o Vacuum extractor tray with various size of cups o Episiotomy tray Steps/method o Ensure bladder is emptied prior to vacuum extraction NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 119 o The woman is positioned in lithotomy o The position of the fetal head is determined and an appropriately sized cup is selected o The cup is placed against the fetal head as near to the occiput as possible, ensuringthat no cervix is trapped beneath Assess position of fetal head by identifying the sagittal suture line and fontanelles Identify posterior fontanelle Apply largest possible cup Place centre of the cup as close to the posterior fontanelle as possible Check no maternal soft tissue in rim of cup The cup is applied to the fetal head, and a caput develops inside the cup as the pressure is initiated. create a vacuum of 0.2kg/cm2(Yellow ) check application of cup Increase vacuum to 0.8kg/cm2 (Green) check application of cup start traction in line of pelvic axis and perpendicular to cup Vacuum suction pressures of 500 to 600 mmHg have been recommended during traction. . Between contractions, suction pressure can be fully maintained or reduced to <200 mmHg. With each contraction ask the mother to push Place finger on scalp next to cup to assess descent and potential slippage Between contractions check fetal heart and application of cup Do not pull if no contraction Episiotomy if needed Continue pulls for maximum of 30 minutes When head delivered release the vacuum and remove cup Failed vacuum extraction Classify as ‘failed’ if o Fetal head does not advance with each pull o Fetus undelivered after three pulls or after 30 minutes o Cup slips off the head twice at proper direction of pull with maximum negative pressure If vacuum extraction is not successful a forceps assisted or CS is then performed Post procedure Examine perineum and repair episiotomy/tear Write up procedure Observe baby for complications (12-24hrs) Neonatal review where available Inform mother STEP 5: Complication Of Vacuum Extraction (10 Minutes) Maternal complication o Perineal trauma o Vaginal lacerations NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 120 o Cervical lacerations o Soft-tissue hematomas Fetal complication o Cephalohematoma o Scalp lacerations o Subdural hematoma o Retinal hemorrhage STEP 6: Caesarean Section (45 Minutes) Definition of caesarean section An operative procedure to deliver a viable foetus or morethrough an abdominal and uterine incision Indications of caesarean section Maternal indication o Contracted pelvis and cephalopelvic disproportion o Pelvic tumors especially if impacted in the pelvis or cancercervix. o Antepartum haemorrhage o Hypertensive disorders with pregnancy o Abnormal uterine action. o Previous uterine scar as hysterotomy or metroplasty. o Previous successful repair of vesico-vaginal fistula o Previous caesarean section Fetal indication o Malpresentations and malposition ( see before) o Prolapsed pulsating cord or foetal distress before full cervicaldilatation. o Diabetes mellitus (see before). o Bad obstetric history as recurrent intrauterine foetal death in lastweeks of pregnancy or repeated intranatal foetal death. o Post-mortem C.S. done within 10 minutes of maternal death tosave a living baby. Contraindication of caesarean section Dead foetus: except in; o Extreme degree of pelvic contraction. o Neglected shoulder o Severe accidental haemorrhage. Extensive scar or pyogenic infection in the abdominal wall e.g. in burn Disseminated intravascular coagulation: to minimize blood loss . Types of caesarean section According to time o Elective caesarean section: The operation is done at apre-selected time before onset of labour, usually at completed 39weeks. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 121 o Selective caesarean section: The operation is done after onset oflabour. According to the site of uterine incision: o Upper segment caesarean section (classical C.S.): The incisionis done in the upper uterine segment and it is always vertical. o Lower segment caesarean section (LSCS) It is the commonertype, the incision is done in the lower uterine segment and maybe transverse ( the usual) or vertical in the followingconditions Presence of lateral varicosities. Constriction ring to cut through it. Deeply engaged head. Pre and post operative care of a pregnant woman undergoing caesarean section Preoperative care o Inform the mother about the procedure and reassure to allay anxiety o Check vital signs such as Blood pressure, pulse and respiration o Intravenous infusion should be in situ o Give iv ceftriaxone 1 g and iv metronidazole 500 mls. o Insert an indwelling catheter to empty the bladder. o Any valuables items are placed in safe keeping according to hospital policy o Laboratory investigation such as hemoglobin, Grouping and cross matching o Check urea and electrolyte levels and clotting factors Postoperative care o Blood pressure and pulse every ¼ hour o Temperature every 2 hours o Inspect the wound every ½ an hour o Inspect lochia (normally it should be small in amounts) o Nurse the woman in the left lateral or recovery position until fully conscious since the risk of regurgitation and silent aspiration of stomach contents is still present. o Give analgesics as prescribed. o If the mother opts to breastfeed, put the baby to the breast as soon as she recovers. o Breast feeding can be achieved with minimal disturbance to the mother Complication of caesarean section o Uterine rupture in subsequent pregnancy. o Post-operative infection: Endometritis, wound sepsis, peritonitis and secondarily pelvic adhesions. o Paralytic ileus(intestinal obstruction). o Injury to the urinary system: Bladder, ureters, and secondarily vesico-vaginal fistula o Injury to the uterine vessels with massive haemorrhage. o Embolism: Pulmonary, thrombophlebitis and deep venous thrombosis . o Atelectasis.Partial collapse or incomplete inflation of lung. o Respiratory distress. o Prolonged hospitalization. o Caesarean hysterectomy STEP 7: Key points (5 minutes) Precaution during vacuum derivery NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 122 o Care should be taken to ensure that no vaginal skin is trapped in the edges of the cup. o Prolonged or excessive traction should not be used. Vacuum is also called ventose delivery Antiseptic measures for vagina , vulva and perineum is important STEP 8: Session Evaluation (5 minutes) What is vacuum extraction? What are the indication and contraindication of vacuum extraction? What are the types of caesarean section? What are the contraindications of caesarean section? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 123 SESSION 21: CARE OF A PREGNANT WOMAN DURING INDUCTION AND AUGMENTATION OF LABOUR Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define induction of labour Explain the indications and contraindications of induction of labour Explain the methods of induction of labour Explain pre-induction assessment Explain the care of a woman during induction of labour Explain about augmentation of labour Resources Needed: Explain complications of abortion Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Content 1 05 Presentation Presentation of session title and learning tasks 2 05 Presentation Definition of induction of labour 3 05 Lecture discussion Indication and contraindication of induction of labour 4 05 Lecture discussion Pre-induction assessment NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 124 5 15 Brainstorming/Lecture discussion Methods of induction of labour 6 10 Lecture discussion Care of a woman during induction of labour 7 05 Lecture discussion Augmentation of labour 8 05 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of induction of labour (5 Minutes) Induction of labour is the initiation of contractions for the purpose of achieving a vaginal birth in a pregnant woman who is not in labour. STEP 3: Indication And Contraindication (5 Minutes) Indication of induction of labour Maternal o Hypertensive disorders in pregnancy o Diabetes o Medical problem Renal ,respiratory or cardiac diseases may require induction of labour o Placenta abruption after the mother’s condition is stabilised o Post term pregnancy (defined at or after 42 weeks) o Premature rupture of membrane o Previous stillbirth o Unexplained oligohydramnios Foetal indications o Post-term pregnancy. o Intrauterine growth retardation. o Intrauterine foetal death. o Rh- isoimmunization. o Gross congenital anomalies Contraindication of induction of labour NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 125 o o o o o o o o o o o o o Placenta Praevia Transverse or compound fetal presentation Cord presentation or cord prolapsed Active genital herpes Previous caesarean section High parity Cephalopelvic disproportion Multiple pregnancy Polyhydramious Maternal cardiac disease Grand multiparty Breech presentation Presenting part above pelvic inlet STEP 4: Pre-Induction Assessment (5 Minutes) In order to decide on the methods of induction the assessment of the cervix is required by using the bishop score. The key elements in the assessment are the dilatation, effacement (cervical canal length) ,position, consistency and the station of the presenting part. The five different features are considered and each is awarded a score of between 0 and 3 When a total of 6 or over is reached the prognosis for induction is good. Figure: Showing the bishop score NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 126 STEP 5: Method Of Induction Of Labour (15 Minutes) Activity: Brainstorming (3 minutes) ASK students to brainstorm on the methods of induction of labour ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Methods Medical induction Prostaglandins o These induce ripening of the cervix and uterine contractions o Misoprostol (cytotec) is a synthetic prostaglandin E1 which is the most common used. o Prostaglandins are more effective when administered by intravaginal route. o Labour will result in 30 to 50% of cases o Fetal heart rate and uterine contraction should be monitored continuously. o The side effects of prostaglandins includes Uterine hyperstimulation and ruptured uterus Systemic side effects includes pyrexia ,diarrhoea and vomiting Oxytocin o The cyntocinon is given intravenously as the oral route is ineffective and the intramuscular route is dangerous in case of over dosage o It is used intravenously ,diluted in an isotonic solution such as normal saline o The infusion should be controlled o Dosage should be recorded in milli-units per minutes with the suggested dilution being 30 IU in IV 500ml of normal saline. o Rate of infusion must be titrated against the assessment of strength and frequency of uterine contractions o The infusion rate may be reduced as labour becomes established o It may be used in conjunction with amniotomy and may be commenced at the same times as ARM or after delay in several hours o The use of oxytocin for induction of labour has the following side effects Hyperstimulation of the uterus Prolonged use may predispose to uterine atony postpartum Water retention may occur in prolonged use Systemic side effects including direct vascular smooth muscle relaxation leading to transient vasodilatation and hypotension Mechanical Induction Sweeping or stripping of membrane. o Membrane sweeping means detaching the amniotic membranes of the fore waters from the lower segment of the uterus. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 127 o This can be effective method of inducing labour where there is an uncomplicated pregnancy Amniotomy o It is the artificial rupture of membrane (ARM) resulting in drainage of liquor o However ARM possesses the following hazards: Intrauterine infection Early deceleration of fetal heart Cord prolapsed Bleeding from the fetal vessels in the membrane ( vasa praevia) the triable vessel in the cervix or slow lying placental site (placenta praevia) Surgical induction can cause vertical transmission of HIV Ballooning, a urinary catheter is inserted intracervical and ballooned by 40 cc of water for injection; the catheter is attached to the thigh by a plaster. The ballon is remained intracervical until it drop and labour starts. STEP 5: Care Of A Woman During Induction Of Labour (10 Minutes) The midwife should discuss with woman and obtain consent prior to induction of labour Written information should be available A record of the woman and partners wishes should be made in the maternity notes Reassure the woman Assess the position of the fetus and relationship of the presenting part to the pelvic brim before commencing the oxytocin Then induction is done if the cervix is favourable by the appropriate method. Observe maternal and fetal condition and record on the partograph Assess the progress of labour and possible side effects Observe maternal pulse, blood pressure, and temperature and record on the partograph Observe contraction for frequency, duration and strength every 15 minutes and keep record Fetal heart should be recorded in the partograph every 15 minutes Observe for signs of fetal distress such as meconeum stained liquor which may indicate the presence of fetal distress Observe and note the mother’s reaction to pain caused by the contraction Give support and encouragement to the woman to help her cope with the contractions. Vaginal examination performed to assess the length, consistency position and station of the presenting part usually in every 4 hours. STEP 6: Augmentation Of Labour (5 Minutes) Augmentation of labour refers to interventions to correct the slow progress in labour. Correction of ineffective uterine contraction includes o Amniotomy o Administration of oxytocin Care of a woman during augmentation includes o Obtain consent from the mother prior to augmentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 128 o o o o o Written information should be available Reassure the mother and her partner Monitor the progress of labour and the condition of the mother Monitor the maternal’s vital signs and record in the partograph Observe for any sign of fetal distress such as meconeum stained liquor which may indicate the presence of fetal distress STEP 8: Key Points (5 minutes) Induction of labour is the initiation of contractions for the purpose of achieving a vaginal birth in a pregnant woman who is not in labour. Augmentation of labour refers to interventions to correct the slow progress in labour Oxytocin should not be started within 6hours of administration of prostaglandins Continuous fetal monitoring is recommended when oxytocin is used for inducing or augmenting labour STEP 9: Session Evaluation (5 minutes) What is the difference between induction and augmentation of labour? What are the indications and contraindications of induction of labour? What are the methods of induction of labour? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 129 SESSION 22: CARE OF A WOMAN WITH PRETERM LABOUR Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define preterm labour Explain causes of preterm labour Explain signs and symptoms of preterm labour Explain the conservative management of a woman with preterm labour Explain complications of preterm labour Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content Definition of preterm labour 1 05 Presentation of session title and learning objectives 2 05 3 05 Brainstorming Presentation Lecture/discussion 4 05 Lecture/discussion Signs and symptoms of preterm labour 5 25 Brainstorming Lecture/discussion Conservative management of a woman with preterm labour 6 05 Presentation Complications of preterm labour 7 05 Presentation Key Points Causes of preterm labor NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 130 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Preterm Labour (5 minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on defition of preterm labour ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Definition of preterm labour Preterm labor is defined as one where the labor starts before the 37th completed week (< 259 days), counting from the first day of the last menstrual period. o The lower limit of gestation is not uniformly defined; whereas in developed countries it has been brought down to 20 weeks, in developing countries it is 28 weeks. o Preterm birth is the significant cause of perinatal morbidity and mortality. STEP 3: Causes of Preterm Labour (5 minutes) Maternal causes o Medical disorders Pre-eclampsia Chronic nephritis Anaemia malnutrition o Antepartum haemorrhage Placenta praevia Abruptio placenta o Uterine anomalies Septate uterus Incompetent cervix Fibroid uterus NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 131 o Psychological or hormonal. Foetal causes o Congenital anomalies o Intrauterine foetal death o Polyhydramious o Multiple pregnancy o Rh- isoimmunization o Premature rupture of membranes. Idiopathic STEP 4: Signs and Symptoms of Preterm Labour (5 minutes) Signs and symptoms Painful menstrual-like cramps-may be confused with round ligament pain Dull low backache-different from the usual low backache a pregnant woman may have Suprapubic pain or pressure-may be confused with urinary tract infection Sensation of pelvic pressure or heaviness Change in character or amount of vaginal discharge (thicker, thinner, watery, bloody, brown, and colorless) Diarrhea Unpalpated uterine contractions (painful or painless) felt more often than every 10 minutes for 1 hour or more and not relieved by lying down Premature rupture of the membranes The diagnosis of preterm labour(Assessment of a woman with preterm labour) History taking on the pain,Vital signs are very important General Examination from head to toe including abdominal examination,Vaginal examination and Laboratory investigation Regular uterine contractions with or without pain (at least one in every 10 minute); Dilatation (> 2 cm) and effacement (80%) of the cervix; Pelvic pressure, backache and or vaginal discharge or bleeding. STEP 5: Conservative management to a woman with Preterm Labour (25 minutes) The management includes: o To prevent preterm onset of labor, if possible o To arrest preterm labor, if not contraindicated o Appropriate management of labor o Effective neonatal care. Principles of management of women with preterm labour: o Glucocorticoids to the mother to reduce neonatal Respiratory distress syndrome o Antenatal transfer of the mother with fetus in utero to a center equipped with NICU o Tocolytic drugs to the mother for a short period unless contraindicated o Antibiotics to prevent neonatal infection with Group B Streptococcus (GBS) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 132 o Careful intrapartum monitoring, minimal trauma and presence of a neonatologist during delivery o Vaginal delivery is preferred, unless otherwise indicated for cesarean birth Conservative management Prophylactic management: o Adequate rest for high risk patients. o Improve health and nutrition. o Discourage cigarette smoking. o Treatment of cervical incompetence by circulage in the second quarter of pregnancy. Preventive management: o The aim is to inhibit labour till completed 37 weeks’ gestation or at least till the foetal lung maturity is ensured. This may be achieved by acting on one or more of the following theories of labour. o Neuromuscular: Sedation such as diazepam. Ethyl alcohol (Ethanol). Sympathomimetic drugs such as ritodrine and isoxuprine. receptor blockers: as phenoxybenzamine o Hormonal : Betamethazone:4 mg betamethazone IM every 8 hours for 48 hours can cause: Decreaseoestrogen synthesis by depressing the production of its precursor from thefoetal adrenal gland. Inhibition of prostaglandin synthesis. Acceleration of foetal lung maturity. Prostaglandin inhibition: e.g. endomethacin. Oxytocin inhibition by : Hydration with a rapid IV infusion of 0.9% Nacl (normal saline) in a rateof 120 ml/hour. This will decrease the release of oxytocins as well asantidiuretic hormone from the posterior pituitary. Ethyl alcohol. o Mechanical: Rest in bed: to reduce the mechanical stimuli from the pressure of the presentingpart on the lower uterine segment. Cervical cerclage: it is of value in prevention of abortion and preterm labour ifdone at 14-16 weeks’ gestation but not so later on. Amniocentesis: was advocated by some authors to reduce the mechanicaldistension of the uterus in polyhydramious. Management in the first stage The patient is put to bed to prevent early rupture of the membranes To ensure adequate fetal oxygenation by giving oxygen to the mother by mask Epidural analgesia is of choice Labor should be carefully monitored prefer-ably with continuous EFM Cesarean delivery is done for obstetric reasons only NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 133 Management in the second stage The birth should be gentle and slow to avoid rapid compression and decompression of the head Episiotomy may be done to minimize head compression if there is perineal resistance The cord is to be clamped immediately at birth to prevent hypervolemia and hyperbilirubinemia To shift the baby to neonatal intensive care unit under the care of a neonatologist STEP 6: Complications of Preterm Labour (5 minutes) Maternal. Fetal Maternal side effects of tocolytics e.g. nausea, vomiting, tachycardia etc Sepsis Preterm labor and delivery of a low birth weight baby results in high perinatal mortality and morbidity Birth asyphxia and development of respiratory distress syndrome Fetal side effects of tocolytics e.g. tachycardia, hypoglacemia STEP 7: Key points (5 minutes) Preterm labor is defined as cervical changes and uterine contractionsoccurring between 20 and 37 weeks of pregnancy. Preterm birth is any birth that occurs before the completion of 37 weeks of pregnancy, regardless of birth weight. Complications related to preterm birth account for more newborn and infant deaths than anyother cause. Although preterm birth often is not preventable, early recognition of preterm labor is still essential to implement interventions that have been demonstrated to reduce neonatal and infant morbidity and mortality. STEP 8: Session Evaluation (5 minutes) What is preterm labour? What are the causes of preterm labour? What are the signs and symptoms of preterm labour? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 134 Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. Dutta, D. C. (2013). Text Book of Obstetrics: Including Perinatology and Contraception 7th Edition. New central book agency. Jaypee Brothers Medical Publishers (P) Ltd. India. SESSION 23: CARE OF A WOMAN WITH PREMATURE RUPTURE OF MEMBRANE (PROM) Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define premature rupture of membrane(PROM) Explain causes of PROM Explain the diagnosis of PROM Explain the conservative management of a woman with PROM Explain complications of PROM Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 135 Session Overview Box Step Time (min) Activity/ Method Presentation Content Definition of PROM 1 05 Presentation of session title and learning objectives 2 05 3 05 Brainstorming Presentation Lecture/discussion 4 05 Lecture/discussion Diagnosis of PROM 5 25 Buzzing Lecture/discussion Conservative management of a woman with PROM 6 05 Presentation Complications of PROM 7 05 Presentation Key Points 8 05 Presentation Session Evaluation Causes of PROM SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Premature Rupture of Membranes (PROM) (5 minutes) Activity: Brainstorming (2 minutes) ASK students to brainstorm on the definition of premature rupture of membranes (PROM) ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 136 Definition of premature rupture of membranes (PROM) It is defined as rupture of membranes before onset of labour. o Spontaneous rupture of the membranes any time beyond 28th week of pregnancy but before the onset of labor is called premature rupture of the membranes (PROM). STEP 3: Causes of PROM (5 minutes) The causes are mostly unknown. o PROM can be brought about iatrogenically either during induction of labour or accidentally during membranes sweeping. o A weak point in the amniotic membranes could rupture before labour starts. o It is common in multiple pregnancy, polyhydramious and if the presenting part of fetus is poorly fitted into the pelvis. o After PROM, labour may set in within 6 hours or the leaking of liquor may continue for days or weeks or the rupture may close spontaneously. The following factors are incriminated: o Cervical incompetence. o Polyhydramious. o Multiple pregnancy. o Malpresentations as the presenting part is not fitting against the loweruterine segment. o Chorioamnionitis o Low tensile strength of the membranes. STEP 4: Diagnosis of PROM (5 minutes) The only subjective symptom is escape of watery discharge per vagina either in the form of a gush or slowleak. This is often confused with:(a) Hydrorrheagravidarum—a state where periodic watery discharge occurs probably dueto excessive decidual glandular secretion; (b) Incontinence of urine especially in the later months. Confirmation of diagnosis: o Speculum examination is done taking aseptic precautions to inspect the liquor escaping outthrough the cervix; o To examine the collected fluid from the posterior fornix (vaginal pool) for: (a) Detection of pH bylitmus or Nitrazine paper. The pH becomes 6–6.2 (Normal vaginal pH during pregnancy is 4.5–5.5 whereas that of liquoramnii is 7–7.5). Nitrazine paper turns from yellow to blue at pH > 6; (b) To note the characteristic ferning pattern when asmeared slide is examined under microscope; (c) Centrifuged cells stained with 0.1% Nile blue sulfate showing orange bluecoloration of the cells (exfoliated fat containing cells from sebaceous glands of the fetus) o Ultrasonography is to be donenot only to support the diagnosis but also to assess the fetal wellbeing. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 137 STEP 5: Conservative Management of a Woman with PROM (25 minutes) Activity: Buzzing (10 minutes) TELL the students to pair up and discuss on the conservative management of a woman with PROM (5 minutes) ALLOW few students to respond and let other pairs provide unmentioned responses CLARIFY and summarize by using the information below All women with PROM should be reffered to hospital. Before reffering such a patient to hospital ascertain that what is coming out per vaginum is liquor and not urine or pus by: o History. The patient will complain of sudden watery vaginal discharge. o Observations of; Odour of the discharge. Urine has ammonical smell, while liquor smells like seminal fluid. Alkalinity. Liquor is alkaline so it will change litmus paper blue. Liquor contains lanugo hair from the fetus. Fern test. In liquor fern test is positive. If the discharge is smeared on a microscope slide and examined under microscope it will form a fern-like structure. Conservative management of PROM Bed-rest. Prophylactic antibiotics. Corticosteroids can be given to the mother so as to mature the baby’s lungs. Dexamethasone 12 mg, intramuscularly, 12 hourly for 24 hours. Frequent monitoring of maternal pulse, temperature and the fetal heart rate. Monitoring vital signs especially temperature and pulse rate for monitoring infections In hospitals where culture can be done, frequent culturing of the liquor should be done. During conservative management avoid unnecessary vaginal examinations. The management of PROM depends on the gestational period. Cord prolapse should be ruled out. If the cord is prolapsed then woman should be delivered regardless of the gestational age. If there is no cord prolapse then: o If the gestational period is 34 weeks or above, the dangers of the fetus staying in utero are more than if delivered. Thus at this gestation period the woman should be delivered and care of the baby is done accordingly. o If the gestation period is less than 34 weeks then conservative management can be tried. o If gestation age is less than 24 weeks salvaging the pregnancy is not easy. o If there is a lot of liquor draining out salvaging the pregnancy is not easy. o If there is none of the above conservative management can be tried. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 138 STEP 6: Complications of PROM (5 minutes) Dry labour. If most of the liquor drains out the fetus will be in close contact with the uterine walls, thus labour will be dry. Ascending infection is common after 24 hours. The ascending infection can cause amnionitis, neonatal pneumonia and even peritonitis if the infection spreads. o Signs of infection will include smelly liquor, high temperature and pulse rate of the woman and the fetal heart bear will be raised (tachycardia). Cord prolapse. Abruptio placenta. Choriomnitis STEP 7: Key Points (5 minutes) When rupture of membranes occur beyond 37th week but before the onset of labor it is called term PROM and when it occurs before 37 completed weeks, it is called preterm PROM. Rupture of membranes for > 24 hours before delivery is called prolonged rupture of membranes. It is common in multiple pregnancy, polyhydramious and if the presenting part of fetus is poorly fitted into the pelvis. After PROM, labour may set in within 6 hours or the leaking of liquor may continue for days or weeks or the rupture may close spontaneously. STEP 8: Session Evaluation (5 minutes) What is PROM? What are the complications of PROM? References Bennett, V. R., & Brown, L. K. (1993). Myles textbook for midwives (12th ed.). London: Churchill Livingstone. Fraser, D. M., & Cooper, M. A. (2009). Myles textbook for midwives (15th ed.). London: Churchill Livingstone. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers and midwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MoHSW. (2010). Focused antenatal care: Learner’s guide for ANC service providers and supervisors. Dar es Salaam. MOHSW. (2006). National guidelines for diagnosis and treatment of malaria. Dar es Salaam. Dutta, D. C. (2013). Text Book of Obstetrics: Including Perinatology and Contraception 7th Edition. New central book agency. Jaypee Brothers Medical Publishers (P) Ltd. India. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 139 SESSION 24: CARE OF A WOMAN WITH BREECH PRESENTATION Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define breech presentation Explain the types of breech presentation Describe causes and diagnosis of breech presentation Explain mechanism of breech delivery Give care to the woman with breech presentation Outline complications of breech delivery Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Models Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Brainstorming/presentation 3 10 Lecture discussion Definition breech presentation Types of breech presentation 4 10 Lecture discussion Causes and Diagnosis of breech presentation 5 20 Lecture discussion Mechanism of breech delivery 6 55 Lecture discussion/demonstration Care to the woman with breech presentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 140 8 05 9 05 10 05 Lecture discussion Complication of breech presentation Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Breech Presentation (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to define breech presentation ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below It is a longitudinal lie in which the buttocks is the presenting part with or without the lower limbs while the head occupies upper pole of uterus. o In the breech presentation the baby enters the birth canal with the buttocks or feet first as opposed to the normal head first presentation. o Compared with a fetus with cephalic presentation, a breech fetus faces increased risk during labor and delivery of asphyxia from cord compression and of traumatic injury during delivery of the shoulders and head STEP 3: Types of Breech presentation (10 Minutes) There are two types of breech presentation which are Complete breech presentation o Is this type the normal attitude of full flexion is maintained. o The thighs are flexed at the hips and the legs at the knees Incomplete breech presentation o This is due to varying degrees of extension of thighs or legs at the podalic pole. o Three varieties are possible: Breech with extended legs (Frank breech): In this condition, the thighs are flexed on the trunk and the legs are extended at the knee joints. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 141 The presenting part consists of the two buttocks and external genitalia only. It is commonly present in primigravidae, about 70%. The increased prevalence in primigravida is due to a tight abdominal wall, good uterine tone and early engagement of breech o Footling presentation (25%) Both the thighs and the legs are partially extended bringing the legs to present at the brim. o Knee presentation: Thighs are extended but the knees are flexed, bringing the knees down to present at the brim. This is very rare Figure: Showing varieties of breech presentation STEP 4: Cause and Diagnosis of Breech Presentation (15 Minutes) Causes of breech presentation Prematurity which is due to o relatively small foetal size, o relatively excess amniotic fluid, and o more globular shape of the uterus Multiple pregnancy o One or both will present by the breech to adapt with the relatively small room. Poly-and oligohydramnios Hydrocephalus Intrauterine foetal death. Bicornuate and septate uterus. Uterine and pelvic tumours. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 142 Placenta praevia Anencephaly Contracted pelvis Diagnosis of breech presentation The diagnosis of breech presentation is mainly by physical examination and investigation though sometimes the mother may admit that she feels the baby kicking in her lower abdomen but this is unreliable ,the diagnosis includes o Abdominal examination Lie is longitudinal with a soft presentation which is more easily felt using pawlik’s grip On palpation of the uterus the fundus will be found to be occupied by a firm, smooth, round and ballottable mass which indicates the head. A woman may complain of discomfort under the ribs due to the pressure of the head on the diaphragm o Auscultation The foetal heart rate may be heard clearly above the umbilicus. If already descended in to the pelvis, the fetal heart sounds tend to be heard at a lower level. o Vagina examination On vaginal examination done at proper time will reveal soft and irregular mass instead of smooth and round mass with palpable sutures indicating the head. Anus may be felt and fresh meconium on the examining finger is usually diagnostic If the legs extended, external genitalia (vulva/scrotum) are very evident though it may become edematous o Ultrasound It is used to confirm the diagnosis STEP 5: Mechanism and of breech presentation(20 Minutes) Positions in breech presentation o Left Sacro Anterior o Right Sacro Anterior o Left Sacro Posterior o Right Sacro Posterior o Left Sacro Transverse o Right Sacro Transverse Mechanism of breech presentation Example in Left sacro- anterior position o The lie is longitudinal o The attitude is one of complete flexion o The presentation is breech o The position is left sacroanterior o The denominator is the sacrum NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 143 o The presenting part is the anterior (left) buttock o The bitrochanteric diameter, 10cm, enters the pelvis in the left oblique diameter of the brim. o The sacrum points to the left iliopectineal eminence. Compaction o Descent takes place with increasing compaction due to increased flexion of the limbs Internal rotation of the buttocks o The anterior buttock reaches the pelvic floor first and rotates forwards 1/8 of a circle along the right side of the pelvis to lie underneath the symphysis pubis. o The bitrochanteric diameter is now in the anteroposterior diameter of the outlet. Lateral flexion of the body o The anterior buttock escapes under the symphysis pubis, the posterior buttock sweeps the perineum and the buttocks are born by a movement of lateral flexion. Restitution of the buttocks o The anterior buttock turns slightly to the mother’s right side Internal rotation of the shoulders o The shoulders enter the pelvis in the same oblique diameter as the buttocks, the left oblique. o The exterior shoulder rotates forwards 1/8 of a circle along the right side of the pelvis and escapes under the symphysis pubis, the posterior shoulder sweeps the perineum and the shoulders are born. Internal rotation of the head o The head enters the pelvis with the sagittal suture in the transverse diameter of the brim. o The occiput rotates forwards along the left side and the sub occipital region (the nape of the neck) impinges on the undersurface of the symphysis pubis. External rotation of the body o At the same time the body turns so that the back is uppermost. Birth of the head o The chin, face and sinciput sweep the perineum and the head is born in a flexed attitude STEP 6: Care of a Woman with breech presentation (55 minutes): The care of a woman with breech presentation according to the stages of labour includes Care during first stage of labour Basic care during this stage is the same as in normal labour. It is usual to monitor the fetal heart and uterine contractions continuously once labour is established. Although the breech with extended legs fits the cervix quite well, the complete breech is a less well-fitting presenting part and the membranes tend to rupture early. There is an increased risk of cord prolapse and a vaginal examination is performed to exclude this as soon as the membranes rupture NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 144 If not ruptured spontaneously at early stage, it is safer to leave them until labor established and the breech is in the level of ischial spines Care during the second stage of labour Full dilation of cervix should be always confirmed by vagina examination before the woman commences active pushing because o in footling presentation, a foot may appear at the vulva when the cervix is only partially dilated o Also when legs are extended, particularly if the fetus is small, the breech may slip through an incompletely dilated cervix o Hence, head may be trapped by the cervix when the fetus is partially delivered Types of breech delivery includes o In spontaneous breech delivery Birth occurs with little assistance from the midwife. Assisted breech delivery o The buttocks are born spontaneously, but some assistance is necessary for delivery of extended legs or arms and the head. Breech extraction. o This is a manipulative delivery carried out by an obstetrician and is performed to hasten birth in an emergency situation such as fetal compromise (Distress) Conducting delivery Delivery of the buttocks and legs o Once the buttocks has entered the vagina and cervix is full dilated tell the woman that she can bear down with contractions and the buttocks are delivered spontaneously o If the perineum is very tight perform an episiotomy o If the legs are flexed, the feet disengage at the vulva, and the baby is born If the legs do not deliver spontaneously, o Deliver one leg at a time through Pinard maneuver Leg abducted and flexed at knee by pressing popliteal fossa Foot and leg are brought down and delivered Procedure repeated for other leg and foot Do not pull the baby while the legs are being delivered Do not hold the baby by the flanks or abdomen as this may cause kidney or liver damage If there is a loop of cord it should be gently pulled down to avoid traction on the umbilicus Delivery of the Shoulder/Arms o Wrap the baby’s with small towel around the hips to preserve warmth and improves the grip on the slippery skin NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 145 o The uterine contractions and weight of the body will bring the shoulders down in to the pelvic floor where they will rotate in to anterior posterior diameter of the outlet o Let the descent continue until the shoulder blades are seen o If the arms are felt on the chest, allow them to disengage spontaneously o After spontaneous delivery of the first arm, lift the buttocks toward the mother’s abdomen to enable the posterior shoulder and arm to deliver spontaneously. o If the arm does not deliver spontaneously, place one or two fingers in the elbow and bend the arm, bringing the hand down over the baby’s face. o If the arms are stretched above the head or folded around the neck (extended arms) o Use the lovset’s manouvure Hold the baby by the hips and turn half a circle keeping the back uppermost and applying downward traction at the same time so that the arm that was posterior become anterior and can be delivered under the pubic arch Assist delivery of the arm by placing one or two fingers on the upper part of the arm draw the arm down over the chest as the elbow is flexed, with the hands sweeping over the face. To deliver the second arm turn the baby half circle keeping the back uppermost and applying downward traction and deliver the second arm in the same way under the pubic arch NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 146 Figure; Showing the illustration of Lovset maneover Delivery of the head o When the back has been turned the infant is allowed to hang from the vulva without support. o His weight brings the head onto the pelvic floor on which the occiput rotates forwards. o The sagittal suture is now in the anteroposterior diameter of the outlet. o If rotation of the head fails to take place, two fingers should be placed on the molar bones and the head rotated. o The baby can be allowed to hang for 1 to 2 minutes. o Gradually the neck elongates the hairline appears and the suboccipital region can be felt. o Control delivery of the head to avoid any sudden change in intracranial pressure and subsequent cerebral haemorrhage. o Delay in delivery of the head (Extended head) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 147 When the body has been allowed to hang, the neck and hairline are not visible, it is probable that the head is extended. This may be dealt with by the use of forceps or the Mauriceau Smellie veit If the head is trapped in an incompletely dilated cervix, an air channel can be created to enable the baby to breathe pending intervention. This is done by inserting two fingers or a Sim’s speculum in front the baby’s face and holding the vaginal wall away from the nose Complete steps as normal delivery after delivering the baby, including active management of third stage of labour and immediate newborn care. Figure; Showing mauriceau smellie veit maneuver Activity: Demonstration (30 minutes) DIVIDE students depending on the size of the class. Demonstrate: On how to conduct breech extraction delivery ALLOW One student from each group to do return demonstration and let others comment on it CLARIFY and summarize. . NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 148 STEP 7: Complications of Breech presentation (5 minutes) Perinatal mortality is increased 2- to 4-fold with breech presentation, regardless of the mode of delivery. Deaths most often are associated with difficult delivery, malformations, prematurity and intrauterine fetal demise Premature separation of the placenta Fetal hypoxia/Birth asphyxia Incidence of prolapsed umbilical cord: Footling 17%, Complete 5%, Frank 0.5 Superficial tissue damage Fracture of the humerus, clavicle or femur or dislocation of the shoulder or hip Spinal cord damage or fracture of the spine Birth trauma ; intra-cranial haemorrhage, trauma of internal organs Lower Apgar scores Impacted breech/An entrapped head Cervical spine injury STEP 8: Key Points (5 minutes) Breech presentation is a longitudinal lie in which the buttocks is the presenting part with or without the lower limbs while the head occupies upper pole of uterus. There are two types of breech complete and incomplete Pinard maneuver is used to deliver the extended legs Lovset maneuver is used to deliver the extended arms Encourage the woman to push with contractions and the buttocks are delivered spontaneously. Excessive delay in delivery of the head may cause severe hypoxia in the fetus STEP 9: Session Evaluation (5 minutes) What is breech presentation? What are the causes of breech presentation? What are the the complications of breech presentation? References . Advanced life saving skills (2005) volume 2 reproductive child health section Dar-es -Salaam: Tanzania Bennett V.R., & Brown L, K. (1996) Myles text book for midwives (14th ed) Callahan, T., & Caughey, A. B. (2013). Blueprints obstetrics and gynecology (Vol. 6). Lippincott Williams & Wilkins. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 149 . Dutta, D. C. (2004). Text Book of Obstetrics: Including Perinatology and Contraception. New central book agency. Diane, M.F., & Margaret, A.C. (2003). Myles Textbook for Midwives (14th ed). London: Churchill Livingston. El Mowafi, D. M.(2002) .Obstetric Simplified Fraser, D.M., & Cooper, M.A. (2009). Myles text book for midwives (15th ed).London Churchill Livingston MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667 SESSION 25: CARE OF A WOMAN WITH BROW PRESENTATION Total Session Time: 120 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define brow presentation Explain causes of brow presentations Explain the diagnosis of brow presentation Give care to a woman with brow presentation Complication of brow presentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 150 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 5 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 5 Brainstorming/presentation 3 10 Lecture discussion Definition of brow presentation Causes of brow presentation 4 10 Lecture discussion Diagnosis of brow presentation 5 20 Lecture discussion Care of a woman with brow presentation 6 15 Lecture discussion Complications of abortion 7 5 Presentation Key Points 8 5 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Objectives (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 151 STEP 2: Definition of Brow presentation (5 Minutes) Activity: Brainstorming (3 minutes) ASK the leaner to define brow presentation ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below It is a cephalic presentation in which the head is midway between flexion and extension. o In Brow the fetal head is partially extended with frontal bone, which is bounded by the anterior fontanel and orbital ridges lying in the pelvic brim o The presenting diameter is mentovertical (13.5cm). This diameter exceeds all the diameters in an average pelvis. Figure: showing brow presentation STEP 3: Causes of Brow presentation(10 Minutes) During the process of extension from vertex to face presentation, the brow will present temporarily and in a few cases it will persist. Anterior obliquity of the uterus o Multiparous women with slack muscles and a pendulous abdomen will have a uterus that leans forward and alters the direction of the uterine axis. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 152 o This causes the fetal buttocks to lean forward and the force of the uterine contractions are directed towards the chin rather than the occiput resulting in the extension of the head Contracted pelvis o The parietal eminences are held in the obstetrical conjugate, the head then becomes extended. o Alternatively, in an android pelvis, the occipital posterior head does not descend. The head is extended and the brow may present Polyhydramnious. o Sudden rupture of the membranes results in the extension of the head as it descends. Congenital abnormalities o Tumour of the fetal neck and anencephaly STEP 4: Diagnosis of Brow presentation (10 Minutes) Not diagnosed before the onset of labour. Abdominal exam o Head is high, appears unduly large and does not descend into the pelvis despite good contractions On vaginal examination o Presenting part is high and may be to reach o Anterior fontanelle may be felt on one side of the pelvis and the orbital ridges and the root of the nose may be felt on the other side. o A large caput may mask these landmarks if the woman has been in labour for a while STEP 6: Care of a Woman Brow presentation (20minutes) Inform the doctor immediately if this presentation is suspected Vaginal delivery is very rare and obstructed labour usually results. When the brow reaches the pelvic floor, the maxilla rotates forwards and the head is born by a mechanism similar to that of the occiput posterior Although this is the exception from the rule The mother should be warned about the possible course of labour and that a vaginal birth is unlikely If there is no evidence of foetal compromise, the doctor may allow labour to continue for a short while in case further extension of the head converts the brow presentation to a face presentation Occasionally spontaneous flexion may occur, resulting in a vertex presentation. If the head fails to descend and the brow presentation persists, a caesarean section is performed, with maternal consent. The mother will be given the normal pre operative care before caesarean section and then taken to the operating theatre. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 153 Preoperative care o Inform the mother about the procedure and reassure to allay anxiety o Check vital signs such as Blood pressure, pulse and respiration o Intravenous infusion should be in situ o Give IV ceftriaxone 1 g and IV metronidazole 500 mls. o Insert an indwelling catheter to empty the bladder. o Any valuables items are placed in safe keeping according to hospital policy o Laboratory investigation such as hemoglobin, Grouping and cross matching o Check urea and electrolyte levels and clotting factors Postoperative care o Blood pressure and pulse every ¼ hour o Temperature every 2 hours o Inspect the wound every ½ an hour o Inspect lochia (normally it should be small in amounts) o Nurse the woman in the left lateral or recovery position until fully conscious since the risk of regurgitation and silent aspiration of stomach contents is still present. o Give analgesics as prescribed. o If the mother opts to breastfeed, put the baby to the breast as soon as she recovers. Breast feeding can be achieved with minimal disturbance to the mother STEP 7: Complications of Abortion (15 minutes) Maternal complications o Obstructed labour o Maternal trauma Extensive perineal laceration may occur during delivery due to large submental and biparietal diameters There is increased incidence of operative delivery either forceps or caesarean delivery Foetal complications o Facial bruising o Cord prolapse o Cerebral hemorrhage STEP 8: Key Points (5 minutes) Brow presentation is a cephalic presentation in which the head is midway between flexion and extension The presenting diameter is mentovertical (13.5cm). This diameter exceeds all the diameters in an average pelvis. It cannot be diagnosed before the onset of labour NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 154 STEP 9: Session Evaluation (5 minutes) What is brow presentation? What are the causes of brow presentation? What are the complications of brow presentation? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 155 SESSION 26: CARE OF A WOMAN WITH FACE PRESENTATION Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define face presentation Describe causes of face presentation Explain mechanism of face presentation Explain the course and outcome of labour in face presentation Give care to the woman with face presentation Describe complications of face presentation Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content Definition of face presentation 1 05 Presentation of session title and learning tasks 2 05 3 05 Brainstorming Presentation Presentation 4 10 Lecture discussion Mechanism of face presentation 5 10 Lecture discussion Course and outcome of labour in face presentation 6 10 Lecture discussion Care of the woman with face presentation Causes of face presentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 156 7 05 8 05 9 05 Presentation Complicationsof face presentation Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Face Presentation (5 minutes) Activity: Brainstorming (3 minutes) ASK students to define face presentation ALLOW time for them to respond CLARIFY and provide summary using the content below: Face presentation Face is a rare variety of cephalic presentation where the presenting part is the face. Face presentation is when the attitude of the head is one of the complete extensions, the occiput of the foetus will be in contact with its spine and the face will present. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 157 STEP 3: Causes of Face Presentation (5 minutes) The actual cause is unknown. It can either be primary (occurs during pregnancy) or secondary (occurs during labour). Primary face is less common and it is usually due to foetal causes which may be: o Anencephaly: due to absence of the bony vault of the skull and the scalp while the facial portion is normal. o Loops of the cord around the neck. o Dolichocephalic head with long anteroposterior diameter o Tumours of the foetal neck e.g. congenital goiter o Increased tone of the extensor group of neck muscles o Dead or premature foetus. Secondary face is more common and it may be due to: o Contracted pelvis particularly flat pelvis which allows descent of the bitemporal but not the biparietal diameterleads to extension of the head. o Pendulous abdomen or marked lateral obliquity of the uterus. o Further deflexion of brow or occipito - posterior positions. o Other causes of malpresentations as polyhydramious and placenta praevia. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 158 STEP 4: Mechanism of face presentation (10 minutes) The principal movements are like those of corresponding occipitoanterior position. The exceptions are increasing extension instead of flexion and delivery by flexion instead of extension of the head. Engagement: The diameter of engagement is the oblique diameter, with the mentum related to one ilio-pubic eminence to the opposite sacroiliac joint. The engaging diameter of the head is submento-bregmatic 9.5 cm in fully extended head or submento-vertical 11.5 cm in partially extended head. Engagement is delayed because of long distance between the mentum and biparietal plane (7 cm). Descent with increasing extension occurs till the chin touches the pelvic floor. Internal rotation—Internal rotation of the chin occurs through 1/8th of a circle anteriorly, placing the mentum behind the symphysis pubis. Further descent occurs till the submentum hinges under the pubic arch. Delivery of the head—The head is born by flexion delivering the chin, face, brow, vertex and lastly the occiput. The diameter distending the vulval outlet is submentovertical 11.5 cm. Restitution occurs through 1/8th of a circle opposite to the direction of internal rotation. External rotation occurs further 1/8th of circle to the same side of restitution so that ultimately the face looks directly to the left thigh in LMA and right thigh in RMA. This follows delivery of the anterior shoulder followed by the posterior shoulder and the rest of the trunk by lateral flexion. STEP 5: Course And Outcome Of Labour In Face Presentation. (10 Minutes) Antenatal diagnosis o Antennal diagnosis is rare since face presentation develop during labour in majority of cases. Intrapatrum diagnosis o On abdominal palpation Face presentation may not be detected especially if mentum is anterior. The occiput feels prominent, with a groove between head and the back, but it may be mistaken for the sinciput. The limbs may be palpated on the side opposite to the occiput and the foetal heart is best heard through the foetal chest on the same side as the limbs. In ment- posterior position the foetal heart is difficult to hear because the foetal chest is in contact with the maternal spine o On vaginal examination The presenting part is high, soft and irregular. When the cervix is sufficiently dilated, orbital ridges, eyes, nose and mouth may be felt. Confusion between mouth and anus could arise, but the moth will be open, and the hard gums. The foetus may suck the examining fingers. As the labour progresses the face becomes oedematous, making it more difficult to distinguish from breech presentation. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 159 To determine position the mentum must be located and if it is posterior, the midwife should decide whether it is lower than the sinciput, if so, it will rotate forwards if it can advance. In left mento anterior position, the orbital ridges will be in the left oblique diameter of the pelvis. Care must be taken not to injure or infect the eyes with the examining finger. STEP 5: Care to the woman with face presentation (10 minutes) Overall assessment of the case is to be done o Counseling and reassuring of the woman on the condition o Should be kept on iv fluids and blood investigation be done o Pelvic adequacy (clinical), o size of the baby, o associated complicating factors, if any, like elderly primigravidae, severe preeclampsia, postcesarean pregnancy and postmaturity, o congenital fetal malformation o position of the mentum. Indications of elective or early cesarean section: o Contracted pelvis, o Big baby, o Associated complicating factors. Vaginal delivery o MENTOANTERIOR First stage: In uncomplicated cases, a wait and watch policy is adopted. Labor is conducted in the usual procedure and the special instructions, as laid down in occipitoposterior positions, are to be followed. Second stage: One should wait for spontaneous delivery to occur. Perineum should be protected with liberal mediolateral episiotomy. o MENTOPOSTERIOR First stage: In uncomplicated cases, vaginal delivery is allowed with strict vigilance hoping for spontaneous anterior rotation of the chin. Second stage: If anterior rotation of the chin occurs, spontaneous delivery with episiotomy is needed. In incomplete or malrotation: Early decision for the method of delivery is to be taken soon after full dilatation of the cervix. The following methods may be employed to expedite the delivery. Cesarean section is the preferred method and is commonly done these days. Delay of labor, in all the stages, is common. The causes ar o weak uterine contractions, o Absence of moulding of the facial bones o delayed engagement—the distance between the biparietal plane to chin is 7 cm and to occiput is only 3 cm o late internal rotation Birth of the head o When the face appears at the vulva, extension must be maintained by holding back the sinciput and permiting the mentum to escape under the symphyisis pubis before the occiput allowed sweeping perineum. Because the perineum is distended by the the NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 160 parietal diameter an elective episiotomy may be performed to avoid extensiveperial lacerations. o If the head does not descend in the second stage the doctor should be informed for further management. STEP 6: Complications of Face Presentation (5 minutes) Maternal—In mentoanterior, the maternal risk is not much increased. However, o there is increased morbidity due to operative delivery and o vaginal manipulation. o In neglected cases, the risks of impacted ment-oposterior leading to obstructed labor and ruptured uterus o Chance of perineal damage is more because of a wide biparietal diameter—9.5 cm (3 3/4”) stretches the perineum and submento-vertical diameter o Postpartum hemorrhage is more likely due to atonic uterus and trauma following operative delivery. o Obstructed labour Fetal complications o cord prolapse, o increased operative delivery, o cerebral congestion due to poor venous return from the head and neck and o Neonatal infection due to bacterial contamination within the vagina. STEP 7: Key Points (5 minutes) Face is a rare variety of cephalic presentation where the presenting part is the face It can either be primary (occurs during pregnancy) or secondary (occurs during labour). The exceptions are increasing extension instead of flexion and delivery by flexion instead of extension of the head. In mento-anterior, the maternal risk is not much increased. However, there is increased morbidity due to operative delivery STEP 8: Session evaluation (5 minutes) What are the causes of face presentation? What are common complications of face presentation? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Konar, H. (Ed.). (2011). DC Dutta's Textbook of Obstetrics Including Perinatology and Contraception. New Central Book Agency. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers andmidwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 161 SESSION 27: CARE OF A WOMAN WITH SHOULDER PRESENTATION Total Session Time: 60minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define shoulder presentation Explain causes of shoulder presentation Assess for shoulder presentation Give pre and post-operative care to the woman Outline complications of shoulder presentation Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content Presentation of session title and learning tasks 2 05 Brainstorming/presentation Definition of shoulder presentation 3 05 Lecture discussion Causes of shoulder presentation 4 10 Lecture discussion Diagnosis of shoulder presentation 5 20 Lecture discussion Pre and post-operative care to the woman with shoulder presentation 6 05 Lecture discussion Complications of shoulder presentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 162 7 05 8 05 Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Shoulder presentation (5 Minutes) Activity: Brainstorming (2 minutes) ASK students to define shoulder presentation ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below Is when the fetus lies with its long axis across the long axis of the uterus (transverse lie) and the shoulder is likely to present. Or when the long axis of the fetus is approximately perpendicular (90°) to the long axis of the mother o Occasionally the lie is oblique but this does not persist as the uterus contractions during labour make it longitudinal or transverse o Shoulder of the fetus come in to lower uterine segment and lie over the pelvic inlet o Head-in one iliac fossa/on one side of the abdomen o Breech-in the other iliac fossa/with the breech at a slightly higher on the other side o The feta back may be anterior or posterior STEP 3: Causes of Shoulder presentation (5 Minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 163 Maternal factors o Contracted pelvis as may prevent the head from entering the pelvic brim o Lax abdominal and uterine muscles especially in multigravidae. o Uterine causes as bicornuate, subseptate and fibroid uterus. o Pelvic masses as ovarian tumours. Foetal factors o Multiple pregnancy o Polyhydramious o Placenta praevia o Prematurity o Intrauterine foetal death due to lack of muscle tones STEP 4: Diagnosis of Shoulder Presentation ( 10 Minutes) On abdominal examination o The uterus appears broad/wide abdomen and the fundal height is less than expected for the period of gestation. o Fundus extends to only slightly above umbilicus o On pelvic and fundal palpation neither head nor breech is felt. o The mobile head is found on one side of the abdomen and the breech at a slightly higher level on the other. o But when the membranes have ruptured the irregular outline of the uterus is more marked o If the uterus is contracting strongly and becomes moulded around the foetus, palpation is very difficult. o The pelvis is no longer empty, the shoulder being wedged into it On vaginal examination o This should not be performed without first excluding placenta praevia o In early labour the presenting part may be may not be felt as the lower uterine segment is imperfectly filled o Late in labor, the membranes usually ruptured early because of the ill-fitting presenting part with a high risk of cord prolapse o Then if the cervix is sufficiently dilated, scapula, acromion, clavical, axilla and ribs can be felt. o If possible to palpate the ribs, their characteristics grid-iron pattern being diagnostic STEP 5: Pre and Post Operative care of a Woman with Shoulder Presentation (10 Minutes) There is no mechanism for delivery of shoulder presentation NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 164 Spontaneous delivery is impossible with a persistent transverse lie If this persists in labour delivery must be by caesarean section to avoid obstructed labour and subsequent uterine rupture Preoperative care o Inform the mother about the procedure and reassure to allay anxiety o Check vital signs such as Blood pressure, pulse and respiration o Intravenous infusion should be in situ o Give IV ceftriaxone 1 g and IV metronidazole 500 mls. o Insert an indwelling catheter to empty the bladder. o Any valuables items are placed in safe keeping according to hospital policy o Laboratory investigation such as hemoglobin, Grouping and cross matching o Check urea and electrolyte levels and clotting factors Postoperative care o Blood pressure and pulse every ¼ hour o Temperature every 2 hours o Inspect the wound every ½ an hour o Inspect lochia (normally it should be small in amounts) o Nurse the woman in the left lateral or recovery position until fully conscious since the risk of regurgitation and silent aspiration of stomach contents is still present. o Give analgesics as prescribed. o Monitor the condition of the baby as well o If the mother opts to breastfeed, put the baby to the breast as soon as she recovers.Breast feeding can be achieved with minimal disturbance to the mother STEP 6: Complications of Shoulder Presentation (5minutes) Neglected Shoulder presentation (Impacted shoulder) o After rupture of membrane, labor continue o Fetal shoulder is forced into the pelvis, the corresponding arm frequently prolapse o After some descent, shoulder is arrested in pelvis, with the head is in the one iliac fossa and breech in the other o As labor continues, the shoulder is impacted firmly in the upper part of the pelvis o Contracts vigorously o After a time, a retraction ring rises increasingly higher o If not promptly managed, uterine rupture, mother & fetus dies. o So once diagnosed emergency caesarean section should be done Cord prolapse Prolapsed arm o Occurs when the membrane have ruptured and e emergency caesarean section should be done STEP 8: Key Points (5 minutes) NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 165 Shoulder presentation occurs when the fetus lies with its long axis across the long axis of the uterus (transverse lie) and the shoulder is likely to present. The lie is transverse ,though sometimes can appear oblique The complication of shoulder presentation includes o Neglected Shoulder presentation (Impacted shoulder o Cord prolapse o Prolapsed arm STEP 9: Session Evaluation (5 minutes) What is shoulder presentation? What are the causes of shoulder presentation? What is the diagnosis of shoulder presentation? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.). London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. SESSION 28: CARE OF A WOMAN WITH UNSTABLE LIE AND COMPOUND PRESENTATION Total Session Time: 120 minutes Prerequisite: None NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 166 Learning Tasks At the end of this session a learner is expected to be able: Define unstable lie and compound presentation Explain the causes of unstable lie and compound presentation Explain complication unstable lie and compound presentation Explain how to diagnose unstable lie and compound presentation Give pre and post operative care to woman with unstable lie and compound presentation Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content 2 05 Brainstorming/presentation Definitions of unstable lie and compound presentation 3 05 Lecture discussion The causes of unstable lie and compound presentation 4 10 Lecture discussion Complication unstable lie and compound presentation 5 10 Lecture discussion Diagnose unstable lie and compound presentation 6 15 Lecture discussion Pre and post operative care to woman with unstable lie and compound presentation 7 05 Presentation Key Points 8 05 Presentation Session Evaluation Presentation of session title and learning tasks SESSION CONTENTS NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 167 STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definitions of Unstable Lie And Compound Presentation (5Minutes) Activity: Brainstorming (3 minutes) ASK students to brainstorm on the definitions of unstable lie and compound presentation of the feotus. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below. Unstable lie is a condition where the presentation of the fetus is constantly changed even beyond 36th week of pregnancy when it should have been stabilized. o Lie refers to the relationship between the longitudinal axis of the feotus and that of its mother, which may be longitudinal, transverse or oblique. Compound presentation is when a cephalic presentation is complicated by the presence of a hand or a foot or both alongside the head or presence of one or both hands by the side of the breech. o The commonest one being the head with hand and the rarest one being the presence of head, hand and a foot. The incidence is about 1 in 600. As in figure NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 168 Figure showing Compound presentation STEP 3: The Causes of Unstable Lie and Compound Presentation (10 Minutes) Causes of unstable lie: The causes are those which prevent the presenting part to remain fixed in the lower pole of the uterus. Such conditions are: o Grand multipara with lack of uterine tone and pendulous abdomen—commonest cause, o Hydramnios o Contracted pelvis o Placenta previa o Pelvic tumor. Causes of compound: Conditions preventing engagement of the head can result in slipping of either upper or lower limbs by the side of the head. o Prematurity (commonest), o contracted pelvis, pelvic tumours, o multiple pregnancy, o macerated fetus, o high head with premature or early rupture of the membranes and hydramnios are the known etiological factors. STEP 4: Complication Unstable Lie and Compound Presentation (10 Minutes) Complications unstable lie: Cord entanglement is a possible risk. o Risk of cord prolapse is there once the membranes rupture. o Birth asyphyxia o Operative delivery o Perinatal death is high. Compound presentation o Foetal compilcations; NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 169 Premature delivery Fresh still birth Sepsis Birth injuries Cord prolapse o Maternal complication o Operative deliveries o Haemorrhage(PPH) o Shoulder dystocia and shoulder presentation o Chorioamnitis STEP 5: Diagnose Unstable Lie and Compound Presentation (110 Minutes) Diagnosis of unstable lie Unstable lie can be diagnosed after 32 weeks’ gestation and not before, because before that period foetus can assume any position without being abnormal. However, diagnosis can be made during labour, as the lie change from time to time.Unstable lie is commonly found in multigravida of high parity (grand maltigravida) and polyhydramnious. Diagnosis in compound presentation: The diagnosis is not difficult when the cervical os is sufficiently dilated to feel the limb by the side of the presenting part, especially after rupture of the membranes. Premature or early rupture of the membranes occurs in about one-third of the cases. Cord prolapse is to be excluded because of its frequent association—10–15%. STEP 6: Pre and Post Operative Care of Woman with Unstable Lie And Compound Presentation (15 Minutes) Unstable lie the woman is to be admitted at 37th week. Premature or early rupture of the membranes with cord prolapsed is the real danger with the lie remaining oblique. The mode delivery is preferable cesarean section, so if the woman not in labour elective cesarean section is done in majority of the cases or emergency caesarean is planned. Pre-operative care o Counsell the woman on the condition and tell the mode of delivery o Inserting canular for IV fluids and taking blood for haemoglobin and blood grouping and cross-matching o Catheterization of the patient o Labeling the patient (name ward from, operation and site) o Consent signing for the patient o Check and record vital signs the morning before the patient is sent to theatre o Escort the patient to theatre and hand her to the theatre nurse Post-operative care o Receive the patient and make sure she is safe o Check and record the vital signs o Observe the wound and note its safety o Administer prescribed medications like strong analgesics to reduce pain, antibiotics, blood transfusion if ordered o Taking part in nursing process by charting vitals, intake and output NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 170 o Turning the patient accordingly o Considering early ambulation to the woman Compound presentation o Caring a woman with compound presentation the factors to be considered are: stage of labor, maturity of the fetus, singleton or twins, pelvic adequacy Associated cord prolapse. o The indication of cesarean section in compound presentation Mature singleton fetus associated with contracted pelvis or cord prolapse with the fetus alive o During second stage of labour if midwife sees a hand out she should try to hold the back towards the chest. STEP 7: Key Points (5 minutes) Unstable lie is a condition where the presentation of the fetus is constantly changed even beyond 36th week of pregnancy when it should have been stabilized. Compound presentation is when a cephalic presentation is complicated by the presence of a hand or a foot or both alongside the head or presence of one or both hands by the side of the breech. Grand multipara with lack of uterine tone and pendulous abdomen is the commonest cause of unstable lie. In compound presentation conditions preventing engagement of the head can result in slipping of either upper or lower limbs by the side of the head. STEP 8: Session Evaluation (5 minutes) What is unstable lie? What are predisposing factors for unstable lie? What are the complications of compound presentation? References Callahan, T., & Caughey, A. B. (2013). Blueprints obstetrics and gynecology (Vol. 6). Lippincott Williams & Wilkins. Konar, H. (Ed.). (2011). DC Dutta's Textbook of Obstetrics Including Perinatology and Contraception. New Central Book Agency. Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 171 SESSION 29: CARE OF A WOMAN WITH OCCIPITAL POSTERIOR PRESENTATION Total Session Time: 120 minutes Prerequisite: None Learning Tasks At the end of this session a learner is expected to be able: Define Occipital Posterior Position Explain the cause of Occipital Posterior Position Explain the mechanism of labour in Occipital Posterior Position Explain the course and outcome of labour in Occipital Posterior Position Explain how to diagnose Occipital Posterior Position Give general care and delivery to a woman with Occipital Posterior Position Give care to a woman with deep transverse arrest. Give management of 3rd and 4th stage of labour Explain the complications of Occipital Posterior Position Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content 2 10 Brainstorming/presentation Definitions of Occipital Posterior Position 3 10 Lecture discussion Presentation of session title and learning tasks The causes of Occipital Posterior Position NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 172 4 30 Lecture discussion The mechanism of labour in Occipital Posterior Position 5 25 Lecture discussion The course and outcome of labour in Occipital Posterior Position 6 25 Lecture discussion Diagnosis of Occipital Posterior Position 7 30 Lecture discussion General care and delivery of a woman with Occipital Posterior Position 8 10 Lecture discussion Care of a woman with deep transverse arrest. 9 10 Lecture discussion Give management of 3rd and 4th stage of labour 10 10 Lecture discussion The complications of Occipital Posterior Position 11 05 Presentation Key Points 12 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of the Occipital Posterior Position (10 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the definitions of Occipital posterior position. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below. Occipito-posterior position is a vertex presentation where the occiput is placed posteriorly over the sacroiliac joint or directly over the sacrum. NB: When the occiput is placed over the right sacroiliac joint, the position is called right occipito-posterior (ROP), traditionally called 3rd position of the vertex and when placed over the left sacroiliac joint, is called left occipito-posterior (LOP), traditionally called 4th position of the vertex (Fig. below) and when it points towards the sacrum, is called direct occipito-posterior. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 173 (Occipito-posterior is an abnormal position of the vertex rather than an abnormal presentation) Figs (A) Right occipito-posterior position (B) Left occipito-posterior position STEP 3: The Cause of Occipital Posterior Position (10 Minutes) In majority, the cause of the abnormal position is not clear. The following are the responsible factors: o Shape of the pelvic inlet: The shape of the inlet significantly determines the position of the head at the onset of labor. In more than 50%, the occipito-posterior position is associated with either an anthropoid or android pelvis. o Fetal factors: Marked deflection of the fetal head, too often favors posterior position of the vertex. The causes of deflexion are: High pelvic inclination. Attachment of the placenta on the anterior wall of the uterus—This favors the well flexed fetus ovoid looking towards the anterior wall of the uterus, i.e. remains in dorso-posterior position. Primary brachycephaly—This shortens the length of the lever from the frontal to atlanto-occipital joint, and thereby diminishes the effective movement of flexion. Uterine factor: Abnormal uterine contraction which may be the cause or effect, leads to persistent deflexion and occipito-posterior position. STEP 4: The Mechanism of Labour in Occipital Posterior Position (30 Minutes) The head engages through the right oblique diameter in ROP and left oblique diameter in LOP. The engaging transverse diameter of the head is biparietal (9.5 cm) and that of anteroposterior diameter is either suboccipitofrontal (10 cm) or occipitofrontal (11.5 cm). Because of deflexion, engagement is delayed. In Favorable Circumstances (90%) Flexion: Good uterine contractions result in good flexion of the head. Descent occurs until the head reaches the pelvic floor. o Internal rotation of the head: As the occiput is the leading part, it rotates 3/8 th of a circle (135°) anteriorly to lie behind the symphysis pubis. As the neck cannot sustain such amount of torsion, the shoulders rotate about 2/8th of a o NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 174 circle to occupy the right oblique diameter in ROP and the left oblique in LOP with 1/8th of a circle torsion of the neck still left behind. Thus, the rest of the mechanism is like that of right occipito-anterior in ROP and that of left occipitoanterior in LOP. o Further descent and delivery of the head occurs like that of occipito-anterior position o Restitution: There is movement of restitution to the extent of 1/8th of a circle in the opposite direction of internal rotation of the head. o External rotation: The external rotation of the head occurs through 1/8th of a circle in the same direction of restitution as the shoulders rotate from the oblique to antero-posterior diameter of the pelvis o Birth of the shoulders and trunk: The process of expulsion is the same as that of occipit-oanterior. In unfavorable circumstances: (Non-rotation or mal-rotation)—10%. o In certain circumstances, the occiput fails to rotate as described previously. o The causes are deflexion of the head, weak uterine contraction, faulty shape of the pelvis such as flat sacrum, prominent ischial spines or convergent side walls and weak pelvic floor muscles. Big baby and immobility of the fetal trunk consequent to the drainage of liquor amnii also contribute to faulty rotation. o Incomplete forward rotation: In this condition, the occiput rotates through 1/8th of a circle anteriorly and the sagittal suture comes to lie in the bispinous diameter. Thereafter, further anterior rotation is unlikely and arrest in this position is called deep transverse arrest. o Non-rotation: Both the sinciput and the occiput touch the pelvic floor simultaneously due to moderate deflexion of the head resulting in non-rotation of the occiput. The sagittal suture lies in the oblique diameter. Further mechanism is unlikely and the condition is called oblique posterior arrest. o Malrotation: In extreme deflexion, the sinciput touches the pelvic floor first resulting in anterior rotation of the sinciput to 1/8th of a circle and putting the occiput to the sacral hollow. This position is termed as occipitosacral position. This is, in the true sense, “Persistent Occipito-Posterior Position” (POP) of the vertex. STEP 5: The Course and Outcome of Labour in Occipital Posterior Position (25 Minutes) Unlike the occipitoanterior, the course of events in labour is likely to be modified in occipitoposterior position. The average duration of both the first and second stage of labor is increased. First stage: There is tendency to delay. o Engagement: Engagement is delayed due to: Persistence of deflexion of the head thereby increasing the diameter of engagement The driving force transmitted through the fetal axis is not in alignment with the axis of the inlet. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 175 o Membrane status: Deflexed head becomes ovoid and this cannot fit well the spherical lower segment loss of ball valve action during uterine contraction Early rupture of the membranes and drainage of liquor. o Uterine contraction: Because of ill fitting of the deflexed head to the lower uterine segment, there is lack of stimulus for uterine contraction. This results in abnormal uterine contraction with slow dilatation of the cervix. Pressure on the rectum by the wide occiput results in premature desire of bearing down effort even in the first stage. The patient, as a result, becomes exhausted. ( There is prolongation of the first stage). Second stage: the second stage is often delayed due to long internal rotation or malrotation, with at times, arrest of the head. This may happen in android pelvis or in mid pelvic contraction. If felt uncared for, arrest of the head may lead to obstructed labor. Third stage: There is increased incidence of postpartum hemorrhage and trauma of the genital tract. Step 6: Diagnose Occipital Posterior Position (20 Minutes) Abdominal Examination Inspection: The abdomen looks flat, below the umbilicus. Palpation o Fundal soft mass palpable o Lateral palpation the findings are: The fetal limbs are more easily felt near the midline on either side. The fetal back is felt far away from the midline on the flank and often difficult to outline clearly. The anterior shoulder lies far away from the midline. o Pelvic palpation the findings are: The head is not engaged. The cephalic prominence (sinciput) is not felt so prominent as found in well flexed occipito-anterior. In direct occipitoposterior; the small sinciput is confused with breech. Auscultation: The maximum intensity of the fetal heart sounds is heard on the flank and often difficult to locate especially in LOP. However, in direct occipito-posterior, the FHS is distinctly felt in the midline. Vaginal Examination The findings in early labor are: o Elongated bag of membranes which is likely to rupture during examination. o The sagittal suture occupies any of the oblique diameters of the pelvis. o Posterior fontanelle is felt near the sacroiliac joint o The anterior fontanelle is felt more easily because of deflexion of the head and at times, is felt at a lower level than the posterior one In late labor, the diagnosis is often difficult because of caput formation which obliterates the sutures and fontanelles. In such cases, the ear is to be located and the unfolded pinna points towards the occiput. Simultaneous assessment of the pelvis should be done. NB:Imaging: Ultrasonography is rarely done. It is helpful to know the descent, attitude of the head and its relation to the pelvic walls (position). A NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 176 STEP 7: General Care and Delivery of A Woman With Occipital Posterior Position (30 Minutes) The underlying principles in the management of the occipitoposterior position are— o early diagnosis, o strict vigilance with watchful expectancy hoping for descent and anterior rotation of the occiput and o judicious and timely interference, if necessary. Diagnosis and evaluation: After diagnosed OPP (mentioned earlier). o The overall assessment of the woman should be done, the pelvic assessment is mandatory. Pelvic adequacy is assessed clinically. Inclination of the pelvis, configuration of the inlet, sacrum, ischial spines and the side walls are to be noted. First stage: In otherwise uncomplicated cases, the labor is allowed to proceed in a manner similar to normal labor. The following are the special instructions: o In anticipating prolonged labor, intravenous infusion line is sited and Ringer’s solution drip is started. o Progress of labor is judged by— progressive descent of the head rotation of the back and the anterior shoulder towards the midline increasing flexion of the head, position of the sagittal suture on vaginal examination and cervical dilatation. o Weak pain, persistence of deflexion and non-rotation of the occiput are the triad too often coexistent. In such a situation, oxytocin infusion is started for augmentation of labor. Indication of cesarean section: o Arrest of labor (failure of rotation), o incoordinate uterine action and o fetal distress. Second stage: In majority, anterior rotation of the occiput is completed and the delivery is either spontaneous or can be accomplished by low forceps or ventouse. In minority (unrotated and malrotated): Provided the fetal and maternal conditions permit, one should take a watchful expectancy for the anterior rotation of the occiput and descent of the head. In occipitosacral position, spontaneous delivery as face-to-pubis may occur. In such cases, proper conduction of delivery and liberal episiotomy should be done to prevent complete perineal tear. Third stage: Because of prolongation of labor, tendency of postpartum hemorrhage can be prevented by prophylactic intravenous oxycitocin 20 IU in 500mils of Ringers Lactate with the delivery of anterior shoulder. Following vaginal operative delivery, meticulous inspection of the cervix and lower genital tract should be made to detect any injury and the woman should be counseled for hygiene including sitz bath with dettol. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 177 STEP8:Care of A Woman With Deep Transverse Arrest(DTA). (15 Minutes) The head is deep into the cavity; the sagittal suture is placed in the transverse bispinous diameter and there is no progress in descent of the head even after 1/2–1 hour following full dilatation of the cervix. The arrest in occipito-transverse position may be the end result of incomplete anterior rotation (1/8th of circle) of oblique occipitoposterior position, or it may be due to non-rotation of the commonly primary occipito-transverse position of normal mechanism of labor. Causes: o Faulty pelvic architecture such as prominent ischial spines, flat sacrum and convergent side walls, o Deflexion of the head o Weak uterine contraction, o Laxity of the pelvic floor muscles. Diagnosis: o The head is engaged, o The sagittal suture lies in the transverse bispinous diameter, o Anterior fontanelle is palpable o Faulty pelvic architecture may be detected. Management: The fetal condition and pelvic assessment give the guide as to the line of management (mentioned earlier). o Vaginal delivery is found not safe (big baby and or inadequate pelvis): Cesarean section. o Vaginal delivery is found safe (any of the methods may be employed): Ventouse—Excessive traction force should not be used Manual rotation and application of forceps Operative vaginal delivery for DTA should only be performed by a skilled obstetrician. Otherwise cesarean delivery is always preferred. STEP 9: Care Of 3rd And 4th Stage Od Labour(15 Minutes) Third stage: It begins after expulsion of the fetus and ends with expulsion of the placenta and membranes (after-births). Following delivering a difficult labour of an OPP there is risk of: Uterine atony Cervical tear Perineal tear During managing third stage of labour Im oxytocin 10IU is given, massaging the uterus, controlled cord traction the placenta is delivered while IV fluids ringers lactate in situ. Then asses the placenta and the perineum while helping the woman to massage the uterus. Fourth stage: It is the stage of observation for at least 1 hour after expulsion of the after-births. During this period, general condition of the patient and the behavior of the uterus are to be carefully monitored. Including checking vital signs( Pulse rate,blood pressure, temperature, respiratory rate) Assess the perineum if any tear and cervical then repair bedside a 1st and 2nd degree perineum tear ,in case there was an episiotomy should be repaired . If woman had significant bleeding blood for Haemoglobin and grouping and cross-matching should be done NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 178 Analgesics and prophylactics antibiotics should be given. Counseling and reassurance to the woman should be done. Counseling the woman to continue breastfeeding if the baby was alive, in case of FSB give reassurance for future delivery and family planning The woman to use sitz barth for perinal hygiene STEP 10: The complications of Occipital Posterior Position (10 Minutes) Maternal complication o Operative deliveries o Uterine rupture o Haemorrhage(PPH) o Perineum injury o Cervical tear and uterine perforation o Sepsis o May lead to cervical incompetence to future pregnancies Foetal compilcations; o Increase operative delivery (Ventouse delivery) o Superficial scalp abrasion o Sloughing of the scalp o Fresh still birth o Birth asyphyxia o Sepsis ( Neonatal infection due bacteria contamination during delivering ) o Birth injuries STEP 11: Key Points (5 minutes) Occipito-posterior position is a vertex presentation where the occiput is placed posteriorly over the sacroiliac joint or directly over the sacrum The shape of the pelvic inlet, fetal factors and uterine factors are main factors responsible for the Occipital posterior position. Ocipito-posterior per se is not an indication of cesarean section however pelvic inadequacy or its unfavorable configuration, along with obstetric complications such as, pre-eclampsia, postcesarean pregnancy, big baby usually need cesarean section. STEP 12: Session Evaluation (5 minutes) What are the causes of occipital posterior position? What is the course of labour in OPP? What are the complications of OPP? NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 179 References Callahan, T., & Caughey, A. B. (2013). Blueprints obstetrics and gynecology (Vol. 6). Lippincott Williams & Wilkins. Konar, H. (Ed.). (2011). DC Dutta's Textbook of Obstetrics Including Perinatology and Contraception. New Central Book Agency. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers andmidwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. SESSION 30:CARE OF A WOMAN WITH MULTIPLE PREGNANCY Total Session Time: 120 minutes Prerequisite Note Learning Tasks At the end of this session a learner is expected to be able: Define the term multiple pregnancy Explain types of multiple pregnancy Describe the method of delivery of a woman with multiple pregnancy Explain complications associated with multiple pregnancy Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 180 Session Overview Box Step Time (min) 1 2 05 10 Activity/ Method Presentation Brainstorming Content 3 20 Presentation Explanation on types of multiple pregnancy 4 40 Lecture discussion Method of delivering a woman with multiple pregnancy 5 35 Lecture discussion complications associated with multiple pregnancy 7 05 Presentation Key Points 8 05 Presentation Session Evaluation Presentation of session title and learning tasks Define the term multiple pregnancy SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Define the Term Multiple Pregnancy (10 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm on the defition of multiple pregnancy and twins pregnancy ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers if necessary: When more than one fetus simultaneously develops in the uterus, it is called multiple pregnancy. o Simultaneous development of two fetuses (twins) is the commonest; although rare, development of three foetuses (triplets), four fetuses (quadruplets), five fetuses (quintuplets) or six fetuses (sextuplets) may also occur. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 181 o Simultaneous development of two fetuses in the uterus is the commonest variety of multiple pregnancies. VARIETIES: Dizygotic twins—It is the most common (80%) and results from the fertilization of two ova. Monozygotic twins (20%) results from the fertilization of a single ovum. STEP 3: Explain Types of Twin Pregnancy (20 Minutes) o This is to help identify whether the babies share a placenta and it is important because babies who share a placenta have a higher risk of complications. o Twins can be: Dichorionic diamniotic (DCDA) – if two eggs are fertilised or if one egg splits soon after fertilisation, each baby has its own placenta with its own outer membrane called a ‘chorion’ and its own amniotic sac (Dizygotic) Monochorionic diamniotic (MCDA) – if the fertilised egg splits a little later, the babies share a placenta and chorion but they each have their own amniotic sac; these babies are always identical(monozygotic) Monochorionic monoamniotic (MCMA) – much less commonly, the fertilised egg splits later still and the babies share the placenta and chorion and are inside the same amniotic sac; these babies are always identical; this is rare and carries additional risks STEP 4: Management of a Woman with Multiple Pregnancy ( 40 Minutes) Antenatal Review: o The successful outcome of a twin pregnancy is to make an early diagnosis. o High index of clinical suspicion and thorough ultrasound examination are the keys to the diagnosis. o It is useful to make early diagnosis and to detect chorionicity, amniocity, fetal growth pattern and congenital malformations. o Antenatal services:o Diet: Increased dietary supplement is needed for increased energy supply than that needed in a singleton pregnancy. o Increased rest at home and early cessation of work is advised to prevent preterm labor and other complications. o Supplement therapy: (i) Iron therapy is to be increased (ii) Additional vitamins, calcium and folic acid above those prescribed for a singleton pregnancy o Interval of antenatal visit should be more frequent to detect at the earliest, the evidences of anemia, preterm labor or preeclampsia. o Fetal surveillance Assessment of fetal growth, amniotic fluid volume and AFI o The woman may be admitted to hospital from 30th – 36th weeks to avoid pre-term labour by providing rest During labour: The twin pregnancy is considered a ‘high risk’; the patient should be confined in an equipped hospital preferably having an intensive neonatal care unit. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 182 Vaginal delivery is allowed when either the twins are or at least the first twin is with vertex presentation. First stage of Labour o The 1st stage tends to be longer than in single fetus due to the large size of the uterus o Carry out routine observation and care of 1st stage o The fetal heart rate sound should be auscultated by two midwives at the same time o Lie and presentation of 1st twin should be found out o Prepare to conduct delivery if 1st twin should be found out o Inform the doctor when the 1st twin present by breech. o After rupture of membranes perform per vaginal examination in order to: Exclude cord prolapse Detect presentation and presenting part of 2nd twin o Prepare equipment at the end of 1st stage of labour. Second stage of labour o Additional swabs, gauzes, cord tie and forceps, scissors, mucous extractor episiotomy scissors plus the rest to be added to the delivery trolley o Extra cots, identification bands, labeled number 1 and 2, extra clothes o Equipment for resuscitation of the babies should be at hand to combat asphyxia neonatorum if it should occur o Syntocinon or Syntometrine 1ml should be drawn up in redness to be given after the delivery of last baby or soon after delivery of the placenta o Fetal Heart Rate should be checked continuously until delivery o As soon as the first twin has been delivered, clamp the cord and cut, note the time, clear the baby’s airway and identify the baby as twin one, handle the baby to the assistant to continue with other management e.g. putting the baby in a warm towel o Another assistant should perform abdominal palpation to diagnose lie, presentation and position of 2nd twin o If longitudinal confirm lie, presentation and position by vaginal examination o Check fetal heart rate o Rupture the 2nd bag of waters at the highest point of contraction o Exclude cord prolapse. o Deliver the baby, note the time and identify by no. 2 o Give oxytocino IV/IM within one minute of delivery of the second Twin Delivery of delayed 2nd Twin o Re-assessment by abdominal examination,vaginal examination o Oxytocin drip is administered if delay was due to hypotonic uterine action and aid delivery of baby by vacuum extraction if the presentation is vertex. Management of the third stage: o The risk of postpartum hemorrhage can be minimized by routine administration of oxytocin 10 IU IM with the delivery of the anterior shoulder of the second baby. o The placenta is to be delivered by controlled cord traction. It is a sound practice to continue the oxytocin drip for at least one hour, following the delivery of the second baby. o A blood loss of more than average should be immediately replaced by blood transfusion, already kept at hand. o The patient is to be carefully watched for about 2 hours after delivery,multiple birth puts an additional stress and strain on the mother as well as on the family members. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 183 o Mother should be given additional support at home to look after both the babies. STEP 5: Complications Associated With Multiple Pregnancy (30 Minutes) MATERNAL During pregnancy: o Nausea and vomiting occurs with increased frequency and severity. o Anemia is more due to increased iron and folate requirement by the two fetuses Deficiency of folic acidleads to increased incidence of megaloblastic anemia. o Preeclampsia (25%) is increased three times over singleton pregnancy. Exposure to superabundance of chorionic villi is the possible explanation. o Hydramnios (10%) is more common in monozygotic twins and usually involves the second sac. It is perhaps due to increased renal perfusion with consequent increased urinary output which may accompany the hypervolaemia in the larger twin. o Antepartum hemorrhage may occur with slight increased frequency. The increased incidence of placenta previa is due to the bigger size of the placenta encroaching on to the lower segment. The separation of normally situated placenta may be due to increased incidence of preeclampsia sudden escape of liquor following rupture of the membranes of the hydramniotic sac deficiency of folic acid and following delivery of the first baby due to sudden shrinkage of the uterine wall adjacent to the placental attachment. o Malpresentation is quite common in twins compared to singleton pregnancies. o Preterm labor (50%) frequently occurs and the mean gestational period for twins is 37 weeks. (Over distension of the uterus, hydramnios and premature rupture of the membranes are responsible for preterm labor). o Mechanical distress such as palpitation, dyspnoea, varicosities and hemorrhoids may be increased compared to a singleton pregnancy. During Labor o Early rupture of the membranes and cord prolapse are likely to be increased due to increased prevalence of malpresentation. Cord prolapse is five times more common than in singleton pregnancy and is more common in relation to the second baby. o Prolonged labor though theoretically expected, is practically not met with. This is because of parous women with smaller babies. o Increased operative interference is due to high prevalence of malpresentation with its associated complications. o Bleeding (intrapartum) following the birth of the first baby, may at times be alarming and is due to separation of the placenta following reduction of placental site. o Postpartum hemorrhage is the real danger in twins. It is due to: Atony of the uterine muscle due to overdistension of the uterus A longer time taken by the big placenta to separate Bigger surface area of the placenta exposing more uterine sinuses Implantation of a part of the placenta in the lower segment which is less retractile. During puerperium: o There is increased incidence of: Subinvolution—because of bigger size of the uterus NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 184 Infection because of increased operative interference, pre-existing anaemia and blood loss during delivery Lactation failure—this is minimized by reassurance and giving her additional support. FOETAL Abortion Vanishing twin Preterm birth Fetal anomalies Discordant growth Intrauterine death of one fetus Twin transfusion syndrome Cord prolapsed Locked twins Increased perinatal mortality STEP 6: Key Points (5 minutes) Multiple pregnancy refers to the development of more than one foetus in utero. The 1st stage tends to be longer than in single fetus due to the large size of the uterus. Multiple pregnancies are at risk and should preferably be managed at facilities that have ultrasound, theatres and facilities for the care of premature babies Mother should be given additional support at home to look after both the babies STEP 7: Session Evaluation (5 minutes) What is multiple pregnancy? What are the types of multiple pregnancies? What is the differences between monozygotic and dyzagotic pregnancy. What are the complications associated with multiple pregnancy? References Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.). London: Churchill Livingston Duttas .D.C,Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contarceptives( 7th ed). New Delh: India MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 185 SESSION 31: CARE OF A WOMAN WITH PUERPERAL SEPSIS Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define puerperal sepsis Outline predisposing factors of puerperal sepsis Identify causative organisms of puerperal sepsis Explain signs and symptoms of puerperal sepsis Describe the nursing care to a woman with puerperal sepsis Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content Definition of puerperal sepsis Causative organisms of puerperal sepsis 1 05 2 05 3 05 Brainstorming Presentation Presentation 4 10 Buzzing Presentation of session title and learning objectives Predisposingfactors of puerperal sepsis NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 186 Presentation 5 10 Presentation Signs and symptoms of puerperal sepsis 6 15 Presentation Nursingcare to a woman with puerperal sepsis 7 05 Presentation Key Points 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Puerperal Sepsis (5 minutes) Activity: Brainstorming (3 minutes) ASK students to define puerperal sepsis ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Puerperal sepsis Puerperal sepsis is defined as a genital tract infection resulted from bacterial invasion during or after labour. o This is still a major cause of maternal death if undetected or untreated. STEP 3: Predisposing Factors of Puerperal Sepsis (5 minutes) The predisposing factors for puerperal sepsis includes; Antepartum factors: o Malnutrition and anemia o Preterm labor o Premature rupture of the membranes NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 187 o Chronic debilitating illness o Prolonged rupture of membrane > 18 hours. Intrapartum factors: o Repeated vaginal examinations o Prolonged rupture of membranes (> 18 hours) o Dehydration and keto-acidosis during labor o Traumatic operative delivery o Hemorrhage during antepartum or postpartum o Retained bits of placental tissue or membranes o Placenta praevia - placental site lying close to the vagina o Cesarean delivery STEP 4: Causative Organisms of Puerperal Sepsis (10 minutes) Activity: Buzzing (5 minutes) TELL the students to pair up and discuss on the causative organisms of puerperal sepsis ALLOW few students to respond and let other pairs to provide unmentioned responses CLARIFY and summarize by using the information below Causative Organisms Haemolytic streptococcus group A o Are the most dangerous organism for the postpartum woman as they are able to invade the blood stream o However if treated promptly the infection can usually be brought under control o Are very sensitive to certain antibiotics otherwise the spread of infection can be controlled through infection prevention and control including; Scrupulous domestic cleanliness, ventilation and dust control and proper application of aseptic and antiseptic techniques Staphylococcal Infection o This tends to be localized, and abscess formation is common, but fatal as septicemia may occur Clostridium Welchii o Occasionally found in the vagina and in the presence of bruised or necrosed tissue. o May become aggressive and cause septicaemia o Other features includes, haemolysis of red cells resulting to anaemia, anuria and death Escherichia Coli o Genital urinary tract infection by this organism is usually confined to the uterus and treatment and management give rise to foul smelling lochia o Septicemia sometimes occurs NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 188 STEP 5: Signs and Symptoms of Puerperal Sepsis (10 minutes) The signs and symptoms of puerperal sepsis depends on the site of infection. The sites can be: Local infection (Wound infection) Uterine infection Extra uterine spread infection Local infection (wound infection): There is slight rise of temperature, generalized malaise or headache, The local wound becomes red and swollen, Pus may form which leads to disruption of the wound. Whensevere (acute), there is high rise of temperature with chills and rigor. Uterine infection: Mild uterine infection o There is rise in temperature and pulse rate. o Lochial discharge becomes offensive and copious. o The uterus is sub-involuted and tender. Severe uterine infection o The onset is acute with high rise of temperature, often with chills and rigor o Pulserate is rapid, out of proportion to temperature o Lochia may be scanty and odorless o Uterus maybe sub-involuted, tender and softer. There may be associated wound infection (perineum, vagina or thecervix). Extra uterine spread: o Is evident by presence of pelvic tenderness (pelvicperitonitis), tenderness on the fornix (parametritis), bulging fluctuant mass in the pouch of Douglas (pelvicabscess). o Parametritis - The onset is usually about 7–10th day of puerperium. Constant pelvic pain Tenderness on eithersides on the hypogastrium Vaginal examination reveals an unilateral tender indurated mass pushing the uterus tothe contralateral side Rectal examination confirms the induration specially extending along the uterosacral ligament. Steady rise of spikytemperature with chills and rigor Intense pain Gradual deterioration of the general condition o Pelvic peritonitis – The signs and symptoms include Pyrexia with increase in pulse rate Lower abdominal pain and tenderness. Vaginal examination reveals tenderness on the fornix and with the movement of the cervix Collection ofpus in the pouch of Douglas is evidenced by swinging temperature, diarrhea and a bulging fluctuant mass felt through theposterior fornix. o General peritonitis – the signs and symptoms include High fever with a rapid pulse NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 189 Vomiting Generalised abdominal pain Patient looksvery ill and dehydrated Abdomen is tender and distended. Rebound tenderness is often present. o Septicemia- the signs and symptoms include There is high rise of temperature usually associated with rigor. Pulse rate is usually rapid even afterthe temperature settles down to normal Blood culture is positive Symptoms and signs of metastatic infection in thelungs, meninges or joints may appear. STEP 6: Nursing Care to a Woman with Puerperal Sepsis (15 minutes) The nursing care to a woman with puerperal sepsis includes the following: Set up an IV infusion and start Iv fluids Keep the woman in a semi sitting position to help drain of discharge from the uterus and vagina Start antibiotics such penicillin/ampicillin 2 grams every 6 hours and gentamycin 5 mg/kg body weight every 24hours. Drug therapy may change depending on the progress of the patient and response to initial treatment Administer analgesics In case of perineal or abdominal wound, the wound will be dressed with a damp dressing which should be changed every 24 hours Monitor for vital signs including hydration and urinary output Regardless of the location of care, postpartum women and health care professionals should be aware of how infection can be acquired and should pay particular attention to Effective hand washing techniques Adhere to accepted practices for aseptic techniques when in contact with wound care Use of gloves appropriately STEP 7: Key Points (5 minutes) Puerperal sepsis is an infection of the genital tract by organisms that is occurring within 14 days after child birth. Aseptic techniques are very important to prevent cross infection. Untreated puerperal sepsis can progress to septic shock resulting to death. STEP 8: Session Evaluation (5 minutes) What is puerperal sepsis? What are the predisposing factors of puerperal sepsis? NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 190 References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. SESSION 32: CARE OF A WOMAN WITH PUERPERAL PSYCHOSIS Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define puerperal psychosis Explain the etiological factors of puerperal psychosis Outline clinical features of a woman with puerperal psychosis Describe the nursing care to a woman with puerperal psychosis Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 191 Session Overview Box Step Time (min) Activity/ Method Presentation Content Brainstorming Presentation Presentation Definition of puerperal psychosis 1 05 Presentation of session title and learning objectives 2 05 3 05 4 10 Buzzing Presentation Clinicalfeatures of a woman with puerperal psychosis 5 25 Presentation Nursingcare to a woman with puerperal psychosis 6 05 Presentation Key Points 7 05 Presentation Session Evaluation Etiological factors of puerperal psychosis SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Puerperal Psychosis (5 minutes) Activity: Brainstorming (3 minutes) ASK students to define puerperal psychosis ALLOW time for them to respond WRITE their answers on a flip chart/board. CLARIFY and provide summary using the content below: Puerperal psychosis is a severe mental illness characterized by extreme difficulty in responding emotionally to a newborn baby; it can even include thoughts of harming the child. o Puerperal psychosis is the most severe form of postpartum affective disorder that tend to show onset within two weeks postpartum. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 192 STEP 3: Etiological Factors of Puerperal Psychosis (5 minutes) The causes of postpartum psychosis are not well understood. The most important etiological factors for this condition are biological factors (neuroendocrine and genetic) It's possible that the abrupt shift in hormones after delivery could trigger the condition. Some women will have suffered from a similar illness following the birth of a previous child. Some women may have suffered from a non-postpartum bipolar affective disorder from which they have long recovered. Family history of bipolar illness. Marked psychosocial adversity. STEP 4: Clinical Features Activity: Buzzing (5 minutes)of Puerperal Psychosis (10 minutes) TELL the students to pair up and discuss on the clinical features of puerperal psychosis ALLOW few students to respond and let other pairs provide unmentioned responses CLARIFY and summarize by using the information below Puerperal psychosis is an acute, early onset condition. Characteristically, the woman begins to complain of fatigue, insomnia, and restlessness and can have episodesof tearfulness and emotional lability. Sudden thoughts of throwing the baby or harming it in some way Delusions (beliefs that have no basis in reality) Hallucinations (seeing or hearing things that aren't there) "Flat affect," or a lack of emotional response or blank facial expression Difficulty responding emotionally to the baby Difficulty sleeping beyond the normal interrupted sleep of new motherhood Changes in appetite or eating Irritability Confusion Agitation An inability to bond with baby Thoughts of suicide, or the belief that the baby or the family would be better off without the mother In extreme situations, a woman with postpartum psychosis may exhibit behaviors such as staring off into space, muttering to herself, refusing to eat, or making seemingly irrational statements. The woman may be unable to attend to her own personal hygiene and nutrition and unable to care for her baby. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 193 STEP 5: Care to a Woman with Puerperal Psychosis (20 minutes) Care of a woman with puerperal psychosis involves the following: A woman with puerperal psychosis will almost always need to be admitted to a psychiatric hospital setting. Hospital admission facilitates stabilisation of symptoms and initiation of medications with ongoing monitoring by health professionals. Admission to a psychiatric setting with a mother and baby unit is preferable to enable continued contact between mother and baby. Because mothers with puerperal psychosis can harm their infants,extra precaution is needed in assessment and intervention. The nurseneeds to ask specifically if the mother has had thoughts about harmingher baby. Due to the high risk of suicide or infanticide, management of puerperal psychosis needs to be ongoing, often for many weeks or months. Assessment and monitoring of the mother–infant interactionis a key part of care of both mother and infant. Treatment with medication is essential. Antipsychotics and mood stabilizers such as lithium are the treatments of choice. Antidepressants should be used verycautiously in treating postpartum psychosis, even when depressivesymptoms are present, because of the risk for precipitating rapidcycling. Because of potential risks to the breastfeeding infant,informed consent regarding the risks and benefits of exposing thenewborn to a psychotropic agent and maternal mental illness mustbe discussed and documented. It is usuallyadvantageous for the mother to have contact with her baby if she sodesires, but visits must be closely supervised. Psychotherapy is indicatedafter the period of acute psychosis has passed. Mood stabilisers are used to treat manic episodes and psychotic symptoms and help reduce relapse. Antipsychotics and antidepressants may also be of benefit, depending on the range of symptoms. A psychiatrist should be consulted when medications are prescribed, changed or ceased, and the potential risks and benefits to the woman and baby should be considered. Medication should not be ceased suddenly. Given the need for medication and maximising sleep in women with puerperal psychosis, the advantages and disadvantages of breastfeeding for mother and baby need to be discussed with the woman and her partner. Sodium valproate and clozapine should not be used without consultation with a psychiatrist. Lithium should be used cautiously. Advice should be sought from a psychiatrist if breastfeeding, and it is important to ensure close monitoring of the baby by a specialist (e.g. neonatologist/paediatrician). A woman’s physical activity levels and diet need to be considered if she is taking antipsychotics (due to their association with weight gain). Electroconvulsive therapy (ECT) may be used or even essential to treat acute mania, psychosis and severe depression. This treatment is only used in major hospital settings, with close monitoring of the woman. Psychological therapiescan assist women to develop effective coping strategies as they recover. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 194 Mother-infant therapy can be useful in promoting mother-infant bonding. Counselling/support is also recommended for the partner and key support people. STEP 6: Key Points (5 minutes) It is rare, affecting approximately 0.1% to 0.2% of postpartum women. Once a woman has had one episode of postpartum psychosis, she has a 30% to 50% likelihood of recurrence with each subsequent birth. The overwhelming majority of cases present in the first 14 days postpartum. They rarely arise within 48 hours following birth and most commonly develop suddenly between day 3 and day 7. Because mothers with puerperal psychosis can harm their infants, extra precaution is needed in assessment and intervention. The nurse needs to ask specifically if the mother has had thoughts about harming her baby. STEP 7: Session Evaluation (5 minutes) What is puerperal psychosis? What are the clinical features of puerperal psychosis? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13thed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15thed.). London: Churchill Livingston. Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones &BarteltPg 666-667. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 195 SESSION 33: CARE OF A WOMAN WITH BREAST INFECTION AND MASTITIS Total Session Time: 60 minutes Prerequisites: None Learning Tasks At the end of this session a learner is expected to be able to: Define breast infection and mastitis Identify causes of breast infections Explain two types of mastitis Explain preventive measures of mastitis Explain complications of breast infections Explain the management of breast infection and mastitis Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content Definition of breast infection and mastitis 1 05 Presentation of session title and learning objectives 2 05 3 05 Brainstorming Presentation Presentation 4 10 Presentation Types of mastitis 5 05 Presentation Preventive measures of mastitis Causes of breast infection NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 196 6 05 Presentation Complicationsof breast infections 7 15 Buzzing Presentation Managementof breast infection and mastitis 8 05 Presentation Key Points 9 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Breast Infection and Mastitis (5 minutes) Activity: Brainstorming (3 minutes) ASK students to define breast infection and mastitis ALLOW time for them to respond CLARIFY and provide summary using the content below: Breast infection Breast infections are usually caused by bacteria and the infection takes place in the fatty tissue of the breast and causes swelling. Mastitis Is painful inflammation of the breast, usually accompanied by an infection. Mastitis most commonly affects women who are breast-feeding (lactation mastitis). STEP 3: Causesof Breast Infection (5 minutes) Bacterial infection o The cause of most breast infections is Staphylococcus aureus bacteria. o The second most common cause is Streptococcus agalactiae. o Bacteria from the baby’s mouth can enter and cause an infection. Obstruction of a milk duct o For breastfeeding mothers, a plugged milk duct can cause milk to back up and an infection to begin. Cracked nipples also increase the risk of breast infection. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 197 STEP 4: Types of Mastitis (10 minutes) There are two types of mastitis namely Non-infective and Infective mastitis. Non infective (acute intramammary) mastitis This condition results from milk stasis. It may occur during the early days as the result of unresolved engorgement. It occurs as a result of a poor feeding technique whereby the milk from one or moresegment of the breast is not sufficiently emptied after breast feeding. It most frequently occurs in the breast that is opposite the mothers preferred side forholding the baby. Infective mastitis This is an infection of the breast caused by damage to the epithelium, which allowsbacteria to enter the underlying tissues. The damage results from incorrect attachment of the baby to the breast which hascaused trauma to the nipple. Infective mastitis if left untreated may lead to abscess (Breast Abscess). A cracked nipple will also let micro-organisms to into the breast. STEP 5: Preventive measures of Mastitis (5 minutes) The following measures may help prevent mastitis: Avoid sudden changes in feeding schedules. Avoid using soap and intense cleaning of the nipple. The areola has self-cleaning and lubricating ability. Taking care to prevent irritation and cracking of the nipple Frequent breast-feeding and emptying at least one breast very well every feeding, and alternate breasts. Avoiding tight-fitting bras that can dig in and impede natural milk flow. Massaging the breasts, especially if you feel a thickening or lump. Using a proper breast-feeding technique that allows for good latching by the infant Weaning the baby over several weeks, instead of suddenly stopping breast-feeding STEP 6: Complications of Breast Infection (5 minutes) The complications of breast infection includes: If the blocked milk ducts that occur in milk stasis become infected with bacteria, a woman is at risk of forming a breast abscess. Chronic infection can result if an abscess is not completely drained. Women with abscesses may be told to temporarily stop breastfeeding. Undergoing surgical procedure to drain abscess that may result into scarring of the breast. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 198 STEP 7: Management of Breast Infection and Mastitis (15 minutes) Activity: Buzzing (5 minutes) TELL the students to pair up and discuss on management ALLOW few students to respond and let other pairs to provide unmentioned responses CLARIFY and summarize by using the information below Management of breast infection and mastitis It is extremely important that breast feeding from the affected breast continues, toprevent milk stasis which is ideal condition for pathogenic bacteria to replicate. Educate the mother to improve her feeding technique by allowing her baby to finish thefirst breast first. A sample of breast milk is sent for bacteriological examination. A broad spectrum antibiotic is given until the causative organism is known. Breast feeding should be suspended if pus is found in the milk, and the breast is emptiedby the gentle use of breast pump or hand expression. The breast must be gently and firmly supported by large pad of cotton wool to protect thepainful infected area. Apply a warm, moist cloth to the affected area several times a day If the infection is mild, breast feeding may be continued. For babies who are difficult to attach: o If the breast is engorged, gently manipulate the tissue that lies under the areola toreduce oedema. o Hand expression or the use of breast pump, may relieve fullness to the point where thebaby can draw in the inner tissue to create necessary teat from the breast. o If attachment is still difficult, ask the mother to lie on her side with a short edge of apillow under her ribs to raise the breast off the bed. o If attachment is still difficult despite of the measures above, teach the mother how tohand express and how to give colostrum to her baby. STEP 8: Key Points (5 minutes) Breast infections are usually caused by bacteria and the infection takes place in the fatty tissue of the breast and causes swelling. Mastitis is is painful inflammation of the breast, usually accompanied by an infection. There are two types of mastitis namely Non-infective and Infective mastitis. In the majority of women, mastitis is the result of milk stasis, not infection although infection maysupervene. STEP 8: Session Evaluation (5 minutes) What is mastitis? What are the preventive measures of mastitis? NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 199 References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London:Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives (14th ed.).London: Churchill Livingston. Fraser, D. M., & Cooper, M. A. (2009). Myles’ textbook for midwives (15th ed.).London: Churchill Livingston. Mbilu, J. N. K. (2010). Essentials of obstetrics and gynaecology for clinical officers andmidwives: Obstetrics (2nd ed., Vol. 1). Dar es Salaam: Matai & Company Limited. MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric andnewborn care. Dar es Salaam. SESSION 34: CARE OF A WOMAN WITH UTERINE SUB-INVOLUTION Total Session Time: 60 minutes Prerequisites None Learning Tasks At the end of this session, a learner is expected to be able to: Define sub-involution of the uterus Outline causes of sub-involution of uterus Outline signs and symptoms of a woman with uterine sub-involution Describe the care to a woman with uterine sub-involution State complications of uterine sub-involution NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 200 Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Content 1 05 Presentation Presentation of session title and learning tasks 2 05 Presentation Definition of uterine sub-involution 3 05 Lecture discussion Causes of uterine sub-involution 4 05 Lecture discussion Signs and symptoms of uterine sub-involution 5 25 Small group discussion/Lecture discussion Care of a woman with uterine sub-involution 6 10 Lecture discussion Complications of uterine sub-involution 7 05 Presentation Key Points 8 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definition of Uterine Sub-involution (5 Minutes) Uterine sub-involution is a condition after child birth in which the uterus does not return to its normal pre-pregnant size. o It occurs when the process of uterine contraction does not take place as it should and is either prolonged or stops NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 201 STEP 3: Causes of Uterine Sub-involution (5 Minutes) Retained products of conception Uterine sepsis (endometriosis) Retroversion causing congestion Uterine myomas. Antepartum over distension e.g. multiple pregnancy Prolapse of the uterus, Maternal ill health Caesarean section Urine stasis STEP 4: Sign and symptoms of uterine sub-involution (5 Minutes) Symptoms o Abnormal lochial o Discharge either excessive or prolonged o Irregular or at times excessive uterine bleeding, o Irregular cramp like pain in cases of retained products o Rise of temperature in sepsis Signs o The uterus feels boggy and softer. o Uterus does not decrease in size o Fundal height remains stationary rather than descending. STEP 5: Care Of A Woman With Uterine Sub Involution (25Minutes) Activity: Small Group Activity (15 minutes) DIVIDE students depending on the size of the class. ASK students to explain how to care for a woman uterine sub-involution ALLOW the groups to work together to come up with answers to the question above. GIVE students an example, if necessary. For example, say “Give the woman antibiotics.” ALLOW groups 10 minutes for this exercise. ASK students to report back the care plan per group. The following part of the presentation has more details about the care. APPRAISE the students NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium PROVIDE feedback by summarizing the students’ answers 202 Care of a woman with uterine sub-involution Give broad spectrum antibiotics treat any underlying infection Catheterize the patient in order to rule out full bladder or urine stasis Exploration of the uterus in retained products followed by the evacuation of the retained products a Give fluid infusions to replace fluid loss Give uterotonics to help in uterine contraction after o Emptying the bladder o Evacuation of the retained products Take blood for grouping and cross matching Encourage the mother to maintain hygiene by sitz bath Encourage the mother to take proper nutrition. Encourage the woman to empty the bladder frequently STEP 6: Complications of Uterine Sub-involution (5minutes) Severe bleeding Sepsis-septicaemiaAnaemia Infertility Can lead to hysterectomy STEP 8: Key Points (5 minutes) Uterine sub-involution is a condition after child birth in which the uterus does not return to its normal pre-pregnant size. Sub-involution occurs when the process of uterine contraction does not take place as it should and is either prolonged or stops. The process of involution may be hampered by retained placental fragments, myomata, or infection Giving the woman antibiotics is important to treat infection or as a prophylaxis STEP 9: Session Evaluation (5 minutes) What is uterine sub-involution What are the sign and symptoms of uterine sub-involution What are the complications of uterine sub -involution NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 203 References Advanced life saving skills (2005) volume 2 reproductive child health section Dar-es -Salaam: Tanzania Bennett V.R., & Brown L, K. (1996) Myles text book for midwives (14th ed) Callahan, T., & Caughey, A. B. (2013). Blueprints obstetrics and gynecology (Vol. 6). Lippincott Williams & Wilkins. Dutta, D. C. (2004). Text Book of Obstetrics: Including Perinatology and Contraception. New central book agency. Diane, M.F., & Margaret, A.C. (2003). Myles Textbook for Midwives (14th ed). London: Churchill Livingston. El Mowafi, D. M.(2002) .Obstetric Simplified Fraser, D.M., & Cooper, M.A. (2009). Myles text book for midwives (15th ed).London Churchill Livingston MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. Tanzania Nurses and Midwives Council. (2009). Nursing ethics: A manual for nurses. Dar es Salaam Varney H., (2004). Varney’s Midwifery text book 4th edition massarchusets, Tones & Bartelt Pg 666667 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 204 SESSION 35:CARE OF A WOMAN WITH VENOUS THROMBOSIS IN PREGNANCY Total Session Time: Prerequisite : 120 minutes None Learning Tasks At the end of this session a learner is expected to be able: Define venous thrombosis, thrombophlebitis, phlebothrombosis and pulmonary embolism Outline predisposing factors for venous thrombosis Identify signs and symptoms of venous thrombosis Explain the management of a woman with venous thrombosis Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) Activity/ Method Presentation Content 1 05 Presentation of session title and learning tasks 2 20 Brainstorming/presentation Definitions of venous thrombosis, thrombophlebitis, phlebothrombosis and pulmonary embolism 3 20 Lecture discussion Predisposing factors for venous thrombosis 4 15 Presentation signs and symptoms of venous thrombosis 5 40 Lecture discussion Care of a pregnant woman with venous thrombosis 6 05 Presentation Key Points NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 205 7 05 Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Definitions of Venous Thrombosis, Thrombophlebitis, Phlebothrombosis and Pulmonary Embolism ( 20 Minutes) Activity: Brainstorming (10 minutes) ASK students to brainstorm on the definitions of venous thrombosis, thrombophlebitis, phlebothrombosis and pulmonary embolism. ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as indicated in the notes below. Pregnancy is generally considered a ‘hypercoagulable’ state with its pathogenesis not been described but several mechanisms have been proposed including increased coagulation factors, endothelia damage, and venous stasis. Definitions; o A venous thrombus (thrombi) is a blood clot (thrombus) that forms within a vein. Thrombosis is a term for a blood clot occurring inside a blood vessel. A common type of venous thrombosis is a deep vein thrombosis (DVT), which is a blood clot in the deep veins of the leg. o Thrombophlebitis is inflammation of a vein caused by a blood clot. It typically occurs in the legs. A blood clot is a solid formation of blood cells that clump together. o Phlebothrombosis occurs when a blood clot (thrombosis) in a vein (phlebo) forms independently from the presence of inflammation of the vein (phlebitis) or thrombosis of a vein without prior inflammation of the vein; associated with sluggish blood flow (as in prolonged bed rest or pregnancy or surgery) or with rapid coagulation of the blood. o Pulmonary embolism (PE) occurs when a pulmonary artery becomes blocked— usually by a blood clot that has broken free from its site of origin and embolized or migrated to the lungs. If misdiagnosed, unrecognized, or untreated, PE can cause death quickly. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 206 STEP 3: Predisposing Factors for Venous Thrombosis (20 Minutes) Risk factors for venous thrombosis are o Vascular stasis, o Hyper coagulability of blood, o Vascular endothelial trauma (Virchow’s triad 1856). NB: Virchow's triad or the triad of Virchow describes the three broad categories of factors that are thought to contribute to thrombosis. Other pregnancy specific risk factors are as mentioned below: o Venous thrombo-embolic diseases include: Deep vein thrombosis (ileofemoral). Thrombophlebitis (superficial and deep veins) Pulmonary embolus. Pathophysiology of venous thrombosis can explain the risk factors: o In a normal pregnancy there is rise in concentration of coagulation factors I, II, VII, VIII, IX, X,XII and plasma fibrinolytic inhibitors are produced by the placenta and the level of protein S is markedly (40%) decreased can increase the chance of thrombosis o (Alteration in blood constituents—increased number of young platelets and their adhesiveness. o Venous stasis is increased due to compression of gravid uterus to the inferior vena cava and iliac veins. This stasis causes damage to endothelial cells and may caus thrombosis. o Thrombophilias are hypercoagulable states in pregnancy that increase the risk of venous thrombosis. It may be inherited or acquired: Inherited thrombophilias are the genetic conditions associated with the deficiencies of antithrombin III, protein C, and protein S. Others are factor V Leiden mutation and hyperhomocysteinemia. Acquired thrombophilias are due to the presence lupus anticoagulant and antiphospholipid antibodies. Other acquired risk factor for thrombosis are; o Advanced age and parity o Operative delivery o Obesity o Anemia o Heart disease o Infection-pelvic cellulitis o Trauma to the venous wall o Cancer: Some forms of cancer increase substances in blood that cause blood to clot. Some forms of cancer treatment also increase the risk of blood clots. o Inflammatory bowel disease: Bowel diseases, such as Crohn's disease or ulcerative colitis, increase the risk of DVT o Immobility o Smoking, o Prior DVT or PE. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 207 STEP 4: Signs and Symptoms of Venous Thrombosis (15 Minutes) Deep vein thrombosis signs and symptoms can include: Swelling in the affected leg. Rarely, there's swelling in both legs. Painful in affected leg. (The pain often starts in calf and can feel like cramping or soreness) Red or discolored skin on the leg. A feeling of warmth in the affected leg. NB: Deep vein thrombosis can occur without noticeable symptoms. The warning signs and symptoms of a pulmonary embolism include: Sudden shortness of breath Chest pain or discomfort that worsens when you take a deep breath or when you cough Feeling lightheaded or dizzy, or fainting Rapid pulse Coughing up blood STEP 5: Care of A Pregnant Woman With Venous Thrombosis (40 Minutes) Care of the pregnant woman with venous thrombosis should start from diagnosis of the condition. Clinical diagnosis is unreliable. In majority it remains asymptomatic. However pain in the calf muscles, swelling of legs and rise in skin temperature, difference in circumference between the affected and the normal leg more than 2 cm may be significant. These investigations may help a proper care: Doppler ultrasound to detect the changes in the velocity of blood flow in the femoral vein by noting the alteration of the characteristic ‘whoosh’ sound which is audible from a patent vein Venography by injecting nonionic water soluble radiopaque dye to note the filling defect in the venous lumen is a reliable method, if carefully interpreted. Venogram is restricted in pregnancy; due to the risk of radiation and contrast allergy Magnetic resonance imaging (MRI) is found superior to VUS and equivalent to contrast venography in the diagnosis of DVT. The sensitivity and specificity of MRI in the diagnosis of DVT is 100 percent and the accuracy is 96 percent. Full Blood count shows polymorphonuclear leucocytosis. Preventive measures for venous thrombosis: Women at risk of venous thromboembolism during pregnancy have been grouped into different categories depending on the presence of risk factors. Thrombo prophylaxis to such a woman depends on the specific risk factor and the category. A low risk woman has no personal or family history of VTE. Such a woman need no thromboprophylaxis will need the following preventive measures; o Prevention of trauma, sepsis, anemia in pregnancy and labour. Dehydration during delivery should be avoided. o Use of elastic compression stocking and intermittent pneumatic compression devices during surgery. o Leg exercises, early ambulation are encouraged following operative delivery. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 208 A high risk woman is one who has previous VTE or VTE in present pregnancy, or antithrombin–III deficiency. o Such a woman needs low molecular weight heparin prophylaxis throughout pregnancy and postpartum 6 weeks. o Women with antithrombin-III deficiency can be treated with antithrombin-III concentrate prophylactically. Imminent care to a woman with venous thromboembolism The patient is put to bed rest with the foot end raised above the heart level. Pain on the affected area may be relieved with analgesics. Appropriate antibiotics are to be administered. Anticoagulants— o Heparin 15,000 units are administered intravenously followed by 10,000 units, 4–6 hourly for four to six injections when the blood coagulation is likely to be depressed to the therapeutic level. Heparin is continued for at least 7–10 days or even longer if thrombosis is severe. Prolongation of activated partial thromboplastin time (APTT) to 1.5–2.5 times indicate effective and safe anticoagulation. Low molecular weight heparin (LMWH), can be used safely in pregnancy. Enoxaparin 40 mg daily is given. It does not cross the placenta. A drug of coumarin series—warfarin is commonly used orally with an overlap of at least three days with heparin. The initial daily single dose of 7 mg for 2 days is adequate for induction. Subsequent maintenance dose depends upon international normalised ratio (INR) which should be within the range of 2.0–3.0. The daily maintenance dose of warfarin is usually 5–9 mg to be taken at the same time each day. The anticoagulant therapy should be continued till all evidences of the disease have disappeared which generally take 3–6 months. The anticoagulant should not prevent the mother from breast-feeding. As soon as the pain subsides, gentle movement is allowed on bed by the end of first week. High quality elastic stockings are fitted on the affected leg before mobilization.. Fibrinolytic agents like streptokinase produce rapid resolution of pulmonary emboli. Venous thrombectomy is needed for massive illiofemoral vein thrombosis or for massive pulmonary embolus. Nursing care for a woman with pulmonary embolism includes: Prevent venous stasis by encourage ambulation and active and passive leg exercises to prevent venous stasis. Monitor thrombolytic therapy and anticoagulant therapy through INR or PTT. Manage pain Manage oxygen therapy Relieve anxiety. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 209 STEP 6: Key Points (5 minutes) Pregnancy is generally considered a ‘hypercoagulable’ state which increase coagulation factors, and venous stasis. Thrombosis is a term for a blood clot occurring inside a blood vessel. A common type of venous thrombosis is a deep vein thrombosis (DVT), which is a blood clot in the deep veins of the leg. Risk factors for venous thrombosis are Vascular stasis, Hyper coagulability of blood and Vascular endothelial trauma Encouraging ambulation and active and passive leg exercises will prevent venous stasis. STEP 7: Session Evaluation (5 minutes) What are the predisposing factors for venous thrombosis? What are prevent measures to a low risk pregnant woman with suspected venous thrombosis? Can you list the warning signs of pulmonary embolism? References Kozek-Langenecker, S. A. (2011). New anticoagulants: perioperative considerations. Wiener Medizinische Wochenschrift, 161(3-4), 63-67. Chiu, J. J., & Chien, S. (2011). Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiological reviews, 91(1), 327-387. Callahan, T., & Caughey, A. B. (2013). Blueprints obstetrics and gynecology (Vol. 6). Lippincott Williams & Wilkins. Konar, H. (Ed.). (2011). DC Dutta's Textbook of Obstetrics Including Perinatology and Contraception. New Central Book Agency. Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2013). Maternal child nursing care. Elsevier Health Sciences. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 210 SESSION 36: CARE OF A WOMAN WITH URINE INCONTINENCE Total Session Time: 120 minutes Prerequisite Note Learning Tasks At the end of this session participants are expected to be able: Define urine incontinence, stress incontinence and vesico-vagina fistula Classification of urine incontinence Identify predisposing factors of stress urine incontinence and Vesico-vagina fsitula Outline signs and symptoms of stress urine incontinence and vesico-vagina fistula Explain the management of a woman with incontinence and vesico-vagina fistula Resources Needed: Flip charts, marker pens, and masking tape Black/white board and chalk/whiteboard markers LCD Projector and computer Note Book and Pen Session Overview Box Step Time (min) 1 05 Activity/ Method Presentation Content 2 10 Brainstorming Define the term Urine incontinence, stress incontinence, vesico-vagina fistula 3 15 Presentation Classification of urinary incontinence 4 25 Lecture discussion Identification of predisposing factors for stress urinary incontinence vesco-vagina fistula 5 20 Lecture discussion signs and symptoms of stress urine incontinence and vesico-vagina fistula Presentation of session title and learning tasks NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 211 6 30 7 10 8 05 Lecture discussion Management of a woman with stress urinary incontinence and vesico-vagina fistula Presentation Key Points Presentation Session Evaluation SESSION CONTENTS STEP 1: Presentation of Session Title and Learning Tasks (5 minutes) READ or ASK participants to read the learning tasks ASK participants if they have any questions before continuing STEP 2: Define the term Urine incontinence (10 Minutes) Activity: Brainstorming (5 minutes) ASK students to brainstorm definitions of Urine incontinence Stress urine incontinence Vesco-vagina fistula ALLOW time for them to respond WRITE their answers on a flip chart/board. PROVIDE possible answers as below. Urinary incontinence is the involuntary leakage of urine or person cannot prevent urine from leaking out. Urinary incontinence is more common among women than men. An estimated 30 percent of females aged 30-60 are thought to suffer from it. Stress urine incontinence, also known as effort incontinence, is due essentially to insufficient strength of the pelvic floor muscles to prevent the passage of urine, especially during activities that increase intra-abdominal pressure, such as coughing, sneezing, or bearing down. Vesico-vaginal fistula or VVF, is an abnormal opening tract extending between the bladder (or vesico) and the vagina that allows the continuous involuntary discharge of urine into the vaginal vault. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 212 STEP 3: Classification of Urine Incontinence (15 Minutes) Urinary incontinence is defined as objectively demonstrable involuntary loss of urine so as to cause hygienic and/or social inconvenience for day to day activity. Urinary insentience can be classified as urethral or extra-urethral. Urethral classification; o Urge incontinence is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person's life. o Stress incontinence due to poor closure of the bladder (also known as stress urinary incontinence (SUI) or effort incontinence. It is due to insufficient strength of the closure of the bladder. o Overflow incontinence due to either poor bladder contraction or blockage of the urethra (characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. o Functional incontinence due to medications or health problems making it difficult to reach the bathroom (is a form of urinary incontinence in which a person is usually aware of the need to urinate, but for one or more physical or mental reasons they are unable to get to a bathroom. Extra-urethral classification; o Acquired urinary incontinence e.g vesco-vagina fistula and other fistulas. o Congenital like ectopic ureter. STEP 4: Predisposing Factors for Stress Urinary Incontinence Vesco-Vagina Fistula (25 Minutes) Stress urinary incontinence its pathogenesis is strictly an anatomic problem. o In the normal continent woman, the bladder neck and the proximal urethra are intraabdominal and above the pelvic floor in standing position. o Normally the urethral pressure exceeds that of intravesical pressure. So when there is a descent of the bladder neck and proximal urethra which normally lies above the urogenital diaphragm, hinders rise of intraurethral pressure during straining leading to incontinence. The following are the predisposing factors of stress urinary incontinence: o Developmental weakness of the supporting structures maintaining the bladder neck and proximal urethra in position. There may be genetic variations in collagen and other connective tissues which normally maintain anatomic and physiologic aspect of the vesicourethral unit. o Childbirth trauma causing damage of the pelvic floor and pubocervical fascia. The injury is more common in gynecoid and least in android pelvis. o Pregnancy—It is probably functional in nature and related to high level of progesterone o Postmenopausal—Estrogen deficiency leads to atrophy of the supporting structures along with diminished periurethral vascular resistance. o Trauma—Injury to symphysis pubis due to fracture or following symphysiotomy. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 213 o Following surgery like anterior colporrhaphy, local repair of VVF or bladder neck surgery, there may be fibrosis of the urethra and urethral musculature. o Age: Although stress incontinence isn't a normal part of aging, physical changes associated with aging, such as the weakening of muscles, may make you more susceptible to stress incontinence o Body weight: People who are overweight or obese have a much higher risk of stress incontinence. Excess weight increases pressure on the abdominal and pelvic organs. Vesco-vagina fistula: There is communication between the urinary bladder and the vagina and the urine escapes into the vagina causing true incontinence .This is the commonest type of genitourinary fistula.The following are the predisposing factor for VVF: o Obstetrical factors; Obstructed labour this is the commonest one, about 80-90% causes obstetric fistula. Instrumental vagina delivery such as destructive delivery and forceps delivery Abdominal operations such as hysterectomy following ruptured uterus or caesarean section from a previous caesarean section o Gynaecological factors; though are very rare in developing countries. Operative injury likely to produce fistula includes operations like anterior colporrhaphy, abdominal hysterectomy for benign or malignant lesion Traumatic—the anterior vaginal wall and the bladder may be injured following fall on a pointed object, by a stick used for criminal abortion, following fracture of pelvic bones or due to retained and forgotten pessary. Malignancy—Advanced carcinoma of the cervix, vagina or bladder may produce fistula by direct spread. Radiation—Following malignancy treatment, apart from overdose or malapplication, it may occur even with accurate therapy. It takes usually long time (1–2 years to produce such fistula. Infective—Chronic granulomatous lesions such as vaginal tuberculosis, lymphogranuloma venereum, schistosomiasis or actinomycosis may produce fistula. STEP 5: Signs and Symptoms of Stress Urine Incontinence and Vesico-Vagina Fistula (20 Minutes) Stress Urinary Incontinence; o Symptoms: The only symptom is escape of urine with coughing, sneezing or laughing. The loss of urine has got the following features Brief and coincides precisely to the period of raised intra-abdominal pressure. Un-associated with a desire to pass urine. Rarely, occurs in supine position or during sleep. Patients are fully aware of it. The amount of loss is small o A woman with stress urinary incontinence she may experience urine leakage when: Cough, sneeze, laugh, stand up, get out of a car, lift something heavy, exercise, have sex. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 214 Vesco-vagina Fistula(VVF); o Symptoms Continuous escape of urine per vaginum (true-incontinence) is the classic symptom. The patient has got no urge to pass urine. There is associated pruritus vulvae/ vagina itching. o Signs Escape of watery discharge per vaginum of ammoniacal smell is characteristic. Evidences of sodden and excoriation of the vulval skin. Varying degrees of perineal tear may be present STEP 6: The Management Of A Woman With Stress Urinary Incontinence And Vesico-Vagina Fistula (30Minutes) Stress urinary incontinence Management of stress urinary incontinence is divided into preventive and definitive Preventive management: Avoiding repeated childbirth trauma and delaying second stage of labour Proper monitoring of labour and proper assessment of the mother in labour to avoid neglected obstructed and prolonged labour Counselling the mother to avoid overweight and obesity Definitive management: It is also divided into conservative and surgical management and the principles for definitive are, restoration of the function of the muscles of urethrovesical junction and strengthening the support of the urethra. Conservative management; o To improve the pelvic floor muscles by counselling and training the mother to do a pelvic muscle exercises this will strengthen the muscular part of pelvic floor muscles.(The pelvic floor muscles training are in the form of drawing up the anus and tightening the vagina for stopping micturition) This should be done about 100 times a day for several months. o Use of vaginal devices ; pessaries ring for bladder neck support o Use of vagina cone o Electrical stimulation activation of the pelvic floor muscles by stimulation of pudendal nerves. o Diet control in obese o Use of drugs; Estrogen use in postmenoposal woman may be useful and improve pelvic muscle strength Impramine (10-25)mg or Ephedrine (15-30)mg twice daily may be of effective Surgery—The principles of surgery are: o Restoration of normal anatomy to maintain bladder neck and proximal urethra as intraabdominal structures. So that it lies within the abdominal pressure zone o Strengthening the support of bladder neck and proximal urethra. This prevents the funneling of vesicourethral junction in response to raised intravesical pressure. o To increase the functional urethral length. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 215 Surgery for Stress urinary incontinence may be vaginal (anterior colporrhaphy) or abdominal (elevation of the bladder neck) or combined. Vesical-vagina fistula ; Management a woman with VVF is of preventive and operative. Preventive: Obstetric fistula in the developing world can be prevented with safe motherhood initiative (WHO-1987). Women with obstetric VVF is considered as a ‘near-miss’ maternal death. Gynecological fistula—can be prevented with better anticipation and improved surgical skill. The following preventive measures: o Adequate antenatal care is to be extended to screen out ‘at risk’ mothers likely to develop obstructed labor. o Anticipation, early detection (partograph) and ideal approach in the method of delivery in relieving the obstruction. o Continuous bladder drainage for a variable period of about 5–7 days following delivery either vaginally or abdominally in a case of longstanding obstructed labor. o Care to be taken to avoid injury to the bladder during pelvic surgery—obstetrical or gynecological. o Immediate management: Once the diagnosis is made, continuous catheterization for 6–8 weeks is maintained. This may help spontaneous closure of the fistula tract. Unobstructed outflow tract helps epithelialization, provided the tissue damage is minimum. o The management of genitourinary fistula needs a team approach both by the gynecologists, nursing staff and the urologists. These socially neglected women need realistic counseling. Other-wise treatment failure may cause further devastation. Operative: local repair of the fistula is the surgery of choice. So preoperative assessment, preoperative preparations and definitive surgery should be considered. o Preoperative Assessment Fistula status—Assessment is done as regards the site, size, number, mobility and status of the margins of the fistula. Urethral involvement is assessed by introducing a metal catheter through external urethral meatus into the bladder. To ascertain the position of the ureteric openings in relation to a big fistula, cystoscopy is indicated. Some blood investigations like FBC, urea and creatinine (renal function) estimation are done. o Preoperative Preparations As the patients are usually from poor socioeconomic status, and socially neglect the improvement of the general condition is essential prior to surgery. Local infection in the vulva should be treated by application of silicone barrier cream or glycerine and general vulva bathing is important. Urinary infection, if any, should be corrected beforehand. It is difficult to collect urine for culture and sensitivity. It is preferable to collect It is advised to start urinary antiseptics at least 3–5 days prior to surgery. Definitive surgery Time; o The ideal time of surgery is after 3 months following delivery. By this time, the general condition improves and local tissues are likely to be free from infection. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 216 o Further delay is likely to produce more fibrosis and unnecessary prolongs the misery of the patient. o Early repair may compromise the success. o Surgical fistula if recognized within 24 hours, immediate repair may be done provided it is small. Otherwise it should be repaired after 10–12 weeks. o Radiation fistulae should be repaired after 12 months. STEP 7: Key Points (5 minutes) Stress urine incontinence, also known as effort incontinence, is due essentially to insufficient strength of the pelvic floor muscles to prevent the passage of urine, especially during activities that increase intra-abdominal pressure, such as coughing, sneezing, or bearing down. Vesico-vaginal fistula or VVF, is an abnormal opening tract extending between the bladder (or vesico) and the vagina that allows the continuous involuntary discharge of urine into the vaginal vault. Stress Urinary Incontinence; o Symptoms: The only symptom is escape of urine with coughing, sneezing or laughing. The loss of urine has got the following features Vesco-vagina Fistula(VVF); o Symptoms Continuous escape of urine per vaginum (true-incontinence) is the classic symptom. The patient has got no urge to pass urine. Stress urinary incontinence o Management of stress urinary incontinence is divided into preventive and definitive Vesical-vagina fistula ; Management a woman with VVF is of preventive and operative STEP 8: Session Evaluation (5 minutes) What is urine incontinence? What is the similarity between stress urinary incontinence and vesico-vagina fistula? Give the classification of urine incontinence. What are the predisposing factors of stress urine incontinence? What are preventive measures of vesico-vagina fistula? References Bennett, V. R., & Brown, L. K. (1999). Myles’ textbook for midwives (13th ed.). London: Churchill Livingston. Fraser, D. M., Cooper, M. A., & Fletcher, G. (2003). Myles’ textbook for midwives 14thed.).London: Churchill Livingston. Duttas .D.C, Konar Hiralal.(Nov. 2013). Textbook of Obstetrics including Perinatology and Contraceptives ( 7th ed). New Delh: India MOHSW. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam MOHSW. (2005). Advanced life saving skills (Vol. 2). Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 217 MOHSW-RCHS. (2010). Learning resource package for basic emergency obstetric and newborn care. Dar es Salaam. NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 218 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 219 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 220 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 221 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 222 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 223 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 224 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 225 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 226 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 227 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 228 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 229 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 230 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 231 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 232 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 233 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 234 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 235 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 236 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 237 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 238 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 239 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 240 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 241 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 242 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 243 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 244 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 245 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 246 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 247 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 248 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 249 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 250 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 251 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 252 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 253 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 254 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 255 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 256 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 257 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 258 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 259 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 260 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 261 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 262 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 263 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 264 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 265 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 266 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 267 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 268 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 269 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 270 NMT 06101: Care of a Woman with Abnormal Pregnancy, Labour and Puerperium 271