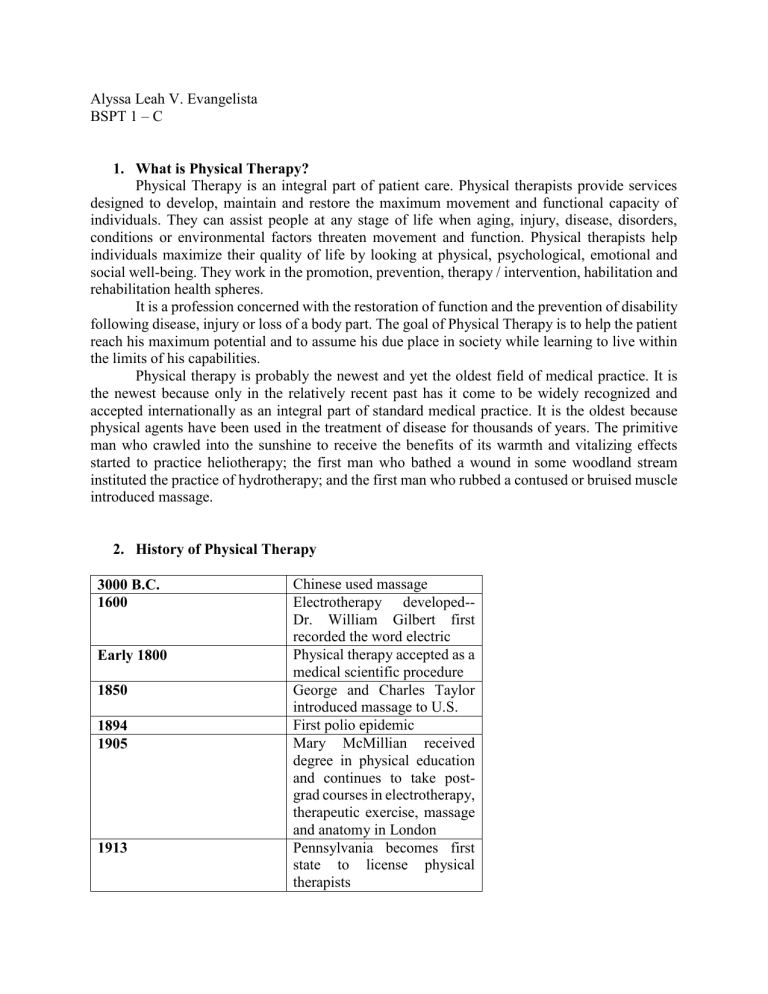
Alyssa Leah V. Evangelista BSPT 1 – C 1. What is Physical Therapy? Physical Therapy is an integral part of patient care. Physical therapists provide services designed to develop, maintain and restore the maximum movement and functional capacity of individuals. They can assist people at any stage of life when aging, injury, disease, disorders, conditions or environmental factors threaten movement and function. Physical therapists help individuals maximize their quality of life by looking at physical, psychological, emotional and social well-being. They work in the promotion, prevention, therapy / intervention, habilitation and rehabilitation health spheres. It is a profession concerned with the restoration of function and the prevention of disability following disease, injury or loss of a body part. The goal of Physical Therapy is to help the patient reach his maximum potential and to assume his due place in society while learning to live within the limits of his capabilities. Physical therapy is probably the newest and yet the oldest field of medical practice. It is the newest because only in the relatively recent past has it come to be widely recognized and accepted internationally as an integral part of standard medical practice. It is the oldest because physical agents have been used in the treatment of disease for thousands of years. The primitive man who crawled into the sunshine to receive the benefits of its warmth and vitalizing effects started to practice heliotherapy; the first man who bathed a wound in some woodland stream instituted the practice of hydrotherapy; and the first man who rubbed a contused or bruised muscle introduced massage. 2. History of Physical Therapy 3000 B.C. 1600 Early 1800 1850 1894 1905 1913 Chinese used massage Electrotherapy developed-Dr. William Gilbert first recorded the word electric Physical therapy accepted as a medical scientific procedure George and Charles Taylor introduced massage to U.S. First polio epidemic Mary McMillian received degree in physical education and continues to take postgrad courses in electrotherapy, therapeutic exercise, massage and anatomy in London Pennsylvania becomes first state to license physical therapists 1914 1917 1918 1921 192 1922 1923 1933 1936 1938 1940 1941 WWI Started and polio epidemic Margaret Sanderson and Mary McMillan work together in the reconstruction aid program at Walter Reed Hospital Mary McMillan was appointed head reconstruction aid at Walter Reed Hospital in Washington, D.C. The American Physical Therapeutic Association was formed Mary McMillan was elected first President of American Women's Physical Therapeutic Association Name of American Women's Physical Therapeutic Association was changed to American Physiotherapy Association (APA) First man (men) admitted into American Physiotherapy Association APA asked for assistance from the AMA to help set standards and education requirements American Medical Association adopted the Essentials of an Acceptable School for Physical Therapy Technicians-13 schools were approved American Physiotherapy Association gets first permanent address when offices are established in Chicago Catherine Worthingham becomes wartime president of American Physiotherapy Association WW II Starts 1944 1946 1954 1960 1967 1969 1971 1975 1978 1979 1980 1983 1988 WWII ends and American Physiotherapy Association moves into first national office in New York American Physiotherapy Association changes its name to the American Physical Therapy Association (APTA) APTA develops 7 hour long competency exam for state licensing boards APTA decides the bachelor's degree is the minimum standard for physical therapists Standards for physical therapist assistant programs were created First set of PTA's graduated Headquarters of the APTA was relocated from New York to Washington D.C. to increase political involvement Individuals with Disabilities Act (IDEA) is passed The APTA created a board of specialties to provide a mechanism for physical therapists to become certified and recognized as clinical specialists in certain areas Master's degree required by December 31, 1990 Bylaws amended to limit size of House of Delegates to 400 delegates The Commission on Accreditation in Education (CAPTE) became the sole agency for accrediting education programs for physical therapists and physical therapists assistant Direct access to physical therapy services became legal in 20 states 1990 1992 1996 1998 1999 2000 2002 2006 2013 Americans with Disabilities Act signed into law House of Delegates membership revised upward to 432 American Physical Therapy Association celebrates 75th anniversary of Association and profession A separate deliberative body for physical therapist assistants, the National Assembly was approved Ratio of women:men is 70:30 in the APTA Vision 2020 created a rapid transition to the doctor of physical therapy (DPT) Baccalaureate degree finally phased out for PT's First meeting of the Physical Therapy Assistant Caucus Indiana was the last state to accept Direct Access 3000 B.C. The Chinese employed rubbing as a therapeutic measure. 641 B.C. Thales of Militis found that amber (in Greek, electron) acquired, by being rubbed, certain properties such as the power of attracting to itself light objects. 460 B.C. Hippocrates wrote concerning it. 1600 A.D. The foundation of modern scientific electrotherapy was laid down by Dr. Gilbert Colchester of England. On that date, he published his treatise, “De Magnete”. 1791 Galvani discovered the current which bears his name. 1812 Peter Henry Ling first placed it on a scientific basis. Metzger, Dr.Weir Mitchel and Dr. Douglas Graham (who published the first American work on massage) all added to its scientific rationale. 1831 Faraday likewise was responsible for faradism. 1890 D’Arsonval evolved the high frequency current. 1895 The X-ray and a little later Tesla modified the D’Arsonval current. Dr. Kellog of the United States first introduced the use of incandescent lights for radiant heat. 19th Century There were three principal divisions of Physical treatments: electrotherapy, hydrobalneology, and massage / exercise. 1931 Physical Therapy evolved into Physical Medicine in the medical field in England. 1946 Physical Therapy evolved into Physical Medicine in the medical field in United States. 1947 The House of Delegates of the American Physiotherapy Association voted to adopt physical therapy as the official nomenclature. Physical therapists formed their first professional association in 1921, called the American Women's Physical Therapeutic Association. Led by President Mary McMillan, an executive committee of elected officers governed the association, which included 274 charter members. In 1922, the association changed its name to the American Physiotherapy Association (APA) and men were admitted. In the 1930s, APA introduced its first "Code of Ethics" and membership grew to just under 1,000. With the advent of World War II and a nationwide polio epidemic during the 1940s and 1950s, physical therapists were in greater demand than ever before. The association's membership swelled to 8,000 and the number of physical therapy education programs across the US increased from 16 to 39. By the late 1940s, the association had changed its name to the American Physical Therapy Association, hired a full-time staff, and opened its first office in New York City. A House of Delegates representing chapter members was established to set APTA policies. The House elected a Board of Directors, previously the Executive Committee, to manage the association. In addition, sections were created to promote and develop specific objectives of the profession. The first two sections were the School and Private Practice sections. In the 1960s, APTA membership reached almost 15,000, and the number of education programs nationwide grew to 52. Archival Photos History: McMillan Headshot Mary McMillan, shown wearing her Reconstruction Aide uniform. History: Reconstruction Aides in NY Reconstruction Aides, who typically learned military drills prior to being transported to overseas US Army hospitals, on July 4, 1918, in New York. History: Aides Treating Solders in TX Reconstruction Aides treat soldiers at Fort Sam Houston, Texas, in 1919. History: PT Using Aquatic Therapy on Child Patient A physical therapist uses pool therapy to treat a child with poliomyelitis. History: Two PTs Using Pool Therapy on Child Director Janet Merrill (right) and her assistant, Eleanor Gillespie (left), use early pool therapy to treat a youngster with polio at Boston Children's Hospital. History: Aides With Two Patients in France Reconstruction Aides and two recovering patients enjoy a bit of sunshine at Base Hospital #8 in Savenay, France, shortly after Armistice. History: PTs and Physicians Treating Children in New England Physical therapists and physicians work together to treat children at a New England poliomyelitis clinic in 1916. Now headquartered in Alexandria, Virginia, APTA represents more than 95,000 members throughout the United States. A national professional organization, APTA's goal is to foster advancements in physical therapy practice, research, and education. Currently 213 institutions offer physical therapy education programs and 309 institutions offer physical therapist assistant education programs in the United States. 3. What were the educational requirements in the past vs now? Physical therapists must have graduated from an accredited academic program in physical therapy before being permitted to exercise. Typically, these programs culminate in a PhD and take at least three years to finish. Students typically need to obtain a bachelor's degree, complete prerequisite scientific classes, obtain volunteer or observation experience in physical treatment, submit graduate record scores (GRE) and retain an acceptable grade point average for admission to a physical therapy program. Themes such as human anatomy, biomechanics, musculoskeletal system, pathology, and neurological dysfunction management are typically studied by students in physical therapy programs. They may also take part in clinical internships and take hands-on clinical classes that provide patient care, screening, evaluation, therapy, and intervention training. Physical Therapist (PT) Education Overview Physical therapist (PT) professional education refers to the didactic and clinical education that prepares graduates for entry into practice of physical therapy. Education for the advancement of practicing physical therapists is termed post-professional. Mission of Physical Therapist Professional Education The mission of PT professional education is to graduate knowledgeable, service-oriented, selfassured, adaptable, reflective practitioners who, by virtue of critical and integrative thinking, lifelong learning, and ethical values, render independent judgments concerning patient/client needs that are supported by evidence; promote the health of the patient or client; and enhance the professional, contextual, and collaborative foundations for practice. These practitioners contribute to society and the profession through practice, teaching, administration, and the discovery and application of new knowledge about physical therapy experiences of sufficient excellence and breadth to allow the acquisition and application of essential knowledge, skills, and behaviors as applied to the practice of physical therapy. Learning experiences are provided under the guidance and supervision of competent faculty, in both the classroom and the clinic. Physical Therapist Degree Professional (entry-level) physical therapist education programs in the United States only offer the Doctor of Physical Therapy (DPT) degree to all new students who enroll. The Master of Physical Therapy (MPT) and Master of Science in Physical Therapy (MSPT) degrees are no longer offered to any new students in the United States. To practice as a physical therapist in the US, you must earn a physical therapist degree from a CAPTE- accredited physical therapist education program and pass a state licensure exam. Curriculum The length of professional DPT programs is typically 3 years. Primary content areas in the curriculum may include, but are not limited to, biology/anatomy, cellular histology, physiology, exercise physiology, biomechanics, kinesiology, neuroscience, pharmacology, pathology, behavioral sciences, communication, ethics/values, management sciences, finance, sociology, clinical reasoning, evidence-based practice, cardiovascular and pulmonary, endocrine and metabolic, and musculoskeletal. Eighty percent (80%) of the DPT curriculum comprises classroom (didactic) and lab study and the remaining 20 percent (20%) is dedicated to clinical education. PT students spend on average 27.5 weeks in their final clinical experience. Bachelor's Degree Required? Most physical therapist education programs require applicants to earn a bachelor's degree prior to admission into the professional DPT program. Other programs offer a 3+3 curricular format in which 3 years of specific pre-professional (undergraduate/pre-PT) courses must be taken before the student can advance into a 3-year professional DPT program. Freshmen Entry - A few programs recruit all or a portion of students directly from high school into a guaranteed admissions program. High school students accepted into these programs can automatically advance into the professional phase of the PT program pending the completion of specific undergraduate courses and any other stated contingencies (eg, minimum GPA). Degree Requirements Most master’s and doctoral physical therapy programs require students to first earn a bachelor’s degree in physical therapy, or a very closely related healthcare field. However, some schools offer a combined undergraduate/doctoral degree program that allows students to graduate with both a bachelor’s and doctoral degree. Undergraduate students who volunteer at hospitals or clinics gain valuable experience while observing licensed professionals. Volunteering is also typically required for admission into doctoral programs. All individuals must earn a doctoral degree in physical therapy (DPT) in order to practice as a physical therapist. To illustrate how fast this field is growing, there were more than 200 physical therapy programs accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE) in 2015 alone. DPT programs typically last at least three years. Alongside seven months of supervised experience in a clinical setting, coursework at the doctoral level usually includes lab and classroom instruction in medical diagnostics, patient examination, patient evaluation, orthotics, prosthetics, and medical screening. Clinical experience is unmatched in preparing therapists for careers in which they interact with clients every day, as well as providing valuable time in the trenches that can lead to full time employment upon graduation. Therapists who wish to specialize in a particular area can apply to and complete a residency program, which usually lasts about one year and provides additional on-the-job training. Certification The American Board of Physical Therapy Specialties (ABPTS) offers eight designations for physical therapists seeking advancement in the field. The eight specialties include: Sports - both amateur and professional athletics Orthopedics Geriatrics Neurology Clinical electrophysiology Cardiovascular & pulmonary Pulmonary Women’s health Therapists applying for ABPTS certification must have at least 2,000 hours of practice, must be licensed, and must pass a certification exam that measures the skills and knowledge in their specialty. Licensing Physical therapists must be licensed in the state where they wish to practice. After completing an accredited physical therapy program, individuals must pass the National Physical Therapy Examination by the Federation of State Boards of Physical Therapy to become licensed. The examination assesses an applicant's knowledge in practice, physical therapy theory, and consultation. Residency Many physical therapists complete their residency after graduating from a DPT program. The American Physical Therapy Association (APTA), programs include 1,500 hours of clinical physical therapy practice to be completed within nine to 36 months. Residencies allow individuals to diagnose and examine patients under the direct supervision of a licensed physical therapist(s). Individuals will often also contribute to medical research and supervise other healthcare professionals while in residency. References: https://www.apta.org/PTCareers/RoleofaPT/ https://www.apta.org/PTEducation/Overview/ https://careersinpsychology.org/physical-therapist-careers/