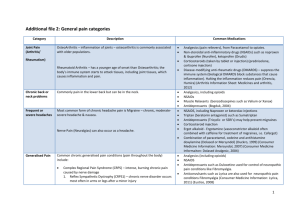
CHRONIC PAIN AGNES CARUNGCONG MD DEPARTMENT OF ANESTHESIOLOGY OSPITAL NG MAYNILA MEDICAL CENTER CHRONIC PAIN • Pain that continues a month or more beyond the usual recovery period the usual recovery period for an injury or illness or goes for months or years due to a chronic condition • may not be constant but disrupts daily life • interfere with sleep, keeping the patient awake at night ACUTE VS CHRONIC PAIN Characteristic Acute Pain Chronic Pain Cause Generally known Often unknown Duration of pain Short, well-characterized Persists after healing, 3 months Treatment approach Resolution of underlying cause, usually self-limited Underlying cause and pain disorder; outcome is often pain control, not cure DOMAINS OF CHRONIC PAIN Quality of Life Physical functioning Ability to perform activities of daily living Work Recreation Psychological Morbidity Depression Anxiety, anger Sleep disturbances Loss of self-esteem Social Consequences Socioeconomic • Marital/family relations Consequences • Intimacy/sexual activity • Disability • Social isolation • Lost workdays • Healthcare costs NOCICEPTIVE VS NEUROPATHIC PAIN Nociceptive Pain Mixed Type Caused by activity in neural pathways in response to potentially tissue-damaging stimuli Caused by a combination of both primary injury and secondary effects Neuropathic Pain Initiated or caused by primary lesion or dysfunction in the nervous system CRPS* Postoperative pain Arthritis Mechanical low back pain Sickle cell crisis Sports/exercise injuries *Complex regional pain syndrome Postherpetic neuralgia Trigeminal neuralgia Neuropathic low back pain Central poststroke pain Distal polyneuropathy (eg, diabetic, HIV) DEFINITION OF TERMS • Neuropathic pain: Paroxysmal and lancinating, has a burning quality and is associated with hyperpathia • Deafferentation pain: neuropathic pain associated with loss of sensory input into the CNS • Sympathetically mediated pain: sympathetic system plays a major role DEFINITION OF TERMS • Neuralgia – an extreme painful condition consisting of recurrent episodes of intense shooting or stabbing pain along the course of the nerve • Causalgia – recurrent episodes of severe burning pain • Phantom limb pain – feelings of pain in a limb that is no longer there and has no functioning nerves CHRONIC PAIN SYNDROMES • Somatic – low back pain, degenerative and inflammatory arthritis, lumbosacral radiculopathy, failed back surgery, vertebral compression fractures, bony metastases, Myofascial pain syndrome • Visceral – abdominal cancers, chronic pancreatitis • Neuropathic – CRPS, Post herpetic neuralgia, Trigeminal neuralgia, diabetic neuropathy, phantom limb pain, spinal stenosis/sciatica, spinal metastasis EVALUATION EVALUATION OF CHRONIC PAIN • Medical evaluation (History, PE etc) • Onset, Provokes/Palliates, Quality, Radiation, Severity, Time, Response to previous treatments (OPQRSTRx) • Plain radiographs (X-ray) • CT-Scan • MRI • Bone Scans • Electromyography and Nerve Conduction Studies EVALUATION OF CHRONIC PAIN • Pain Scales: Numerical rating scale, Faces rating scale, Visual analog scale, McGill pain questionnaire EVALUATION OF CHRONIC PAIN MANAGEMENT PAIN TREATMENT CONTINUUM Least invasive Most invasive Psychological/physical approaches Topical medications Systemic medications* Interventional techniques* Continuum not related to efficacy *Consider referral if previous treatments were unsuccessful. MANAGEMENT NON PHARMACOLOGIC TREATMENT NONPHARMACOLOGIC OPTIONS • Biofeedback • Relaxation therapy • Physical and occupational therapy • Cognitive/behavioral strategies • meditation; guided imagery • Acupuncture • Transcutaneous electrical nerve stimulation MANAGEMENT PHARMACOLOGIC TREATMENT PHARMACOLOGIC TREATMENT OPTIONS • Classes of agents with efficacy demonstrated in multiple, randomized, controlled trials for neuropathic pain • topical analgesics (capsaicin, lidocaine patch 5%) • anticonvulsants (gabapentin, lamotrigine, pregabalin) • antidepressants (nortriptyline, desipramine) • opioids (oxycodone, tramadol) • Consider safety and tolerability when initiating treatment NONSTEROIDAL ANTI-INFLAMMATORY DRUGS • Traditional NSAIDs are effective in the treatment of mild to moderate pain, but their use is limited by potentially serious adverse effects • Ketorolac: indicated only in the management of moderately severe acute pain that requires opioid level analgesics; no more than 5 days • COX-2 selective inhibitors (celecoxib, rofecoxib etc) OPIOIDS: MORPHINE • Morphine is the standard for opioid therapy for cancer pain. • Metabolites: Morphine-6-glucuronide and Morphine-3glucuronide • Dosing: 0.01-0.2mg/kg IV OPIOIDS: MORPHINE • Oral equinalgesic doses of morphine 10mg IV or 30mg per orem: • 200mg codeine • 30mg hydrocodone • 20-30mg oxycodone • 130mg propoxyphene • 120mg tramadol OPIOIDS: HYDROMORPHONE • μ- receptor agonist • 3-5x more potent > morphine (orally) • 5-7x more potent (parenterally) • Side effects are less frequent compared with morphine • Metabolite: hydromorphone-3-glucoronide OPIOIDS: METHADONE • Has high potency and longer duration of action • Has no metabolites • Has additional salutary effects: NMDA receptor antagonist and Serotonin reuptake inhibitor. • Potency compared with morphine – 1:1 to 1:4, may be as low as 1:10 with chronic usage OPIOIDS: METHADONE • Has unpredictable half-life – increasing risk of accumulation • Causes cardiac rhythm abnormalities: QT prolongation and Torsade de pointes OPIOIDS: OXYCODONE • More potent than morphine when given intravenously (10x) • Has low histamine release • Has extensive first-pass hepatic metabolism = ↓ bioavailability (10%) • Has greater lipid solubility • Should not be taken with alcohol: ↑ plasma concentration as much as 300% OPIOIDS: BUPRENORPHINE • Partial agonist at μ-receptor, a κ-antagonist, and a weak ϩagonist. • Has rapid onset when given orally (30 minutes) • Long duration of action (6-9 hours) • (+) abuse of drug OPIOIDS: TRAMADOL • Opioid agonist • Bioavailability of 80-90% • Low abuse potential • Low incidence of constipation and minimal risk for fatal respiratory depression • Maximum dose is: 400-500mg/day CO-ANALGESICS • Agents which enhance analgesic efficacy, have independent analgesic activity for specific types of pain, and/or relieve concurrent symptoms which exacerbate pain CO-ANALGESICS • Antidepressants • Anticonvulsants • Corticosteroids • Neuroleptics • Antihistamines • Benzodiazepines • Antispasmodics • Muscle relaxants • Systemic local anesthetics ANTIDEPRESSANTS • Effective agents in the treatment of neuropathic pain • MOA: blockade of presynaptic reuptake of serotonin, norepinephrine or both • Side effects: anticholinergic effects (dry mouth, confusion, urinary retention) • E.g. Amitryptiline, Clomipramine, Doxepine, Fluoxetine, Imipramine ANTIDEPRESSANTS ANTICONVULSANTS • Blocks voltage-gated sodium channels and can suppress spontaneous neuronal discharges • Phenytoin, carbamazepine and valproic acid • Gabapentin appears to be the most effective and well tolerated at present. LOCAL ANESTHETICS • Lidocaine Infusion • More effective in neuropathic pain but can be used for all pain syndromes. Starting dose 0.5mg – 2mg/kg per hour IV or SC. Some studies demonstrate long-lasting pain relief even after drugs has been stopped. No need to decrease opioids when starting • Lidocaine Patch (700mg/adhesive) • Maximum of 3 patches for 12/hr/day PHARMACOLOGIC AGENTS AFFECT PAIN DIFFERENTLY BRAIN CNS PNS Peripheral Sensitization Descending Modulation Spinal Cord Dorsal Horn Local Anesthetics Topical Analgesics Anticonvulsants Tricyclic Antidepressants Opioids Anticonvulsants Opioids Tricyclic/SNRI Antidepressants Central Sensitization Anticonvulsants Opioids NMDA-Receptor Antagonists Tricyclic/SNRI Antidepressants MECHANISTIC APPROACH TO PAIN THERAPY Increase Inhibition TCA’s, SSRI’s, Clonidine Modify Expression Anxiolytics Decrease Inflammatory Response NSAIDs, Local Anesthetics, Steroids Decrease Conduction Gabapentin, Carbamazepine, Local Anesthetics, Opioids Prevent Centralization COX 2, Opioids, Ketamine, -2 Agonists. WORLD HEALTH ORGANIZATION (WHO) ANALGESIC LADDER. DISTINGUISHING DEPENDENCE, TOLERANCE, AND ADDICTION • Physical dependence: withdrawal syndrome arises if drug discontinued, dose substantially reduced, or antagonist administered • Tolerance: greater amount of drug needed to maintain therapeutic effect, or loss of effect over time • Pseudoaddiction: behavior suggestive of addiction; caused by undertreatment of pain • Addiction (psychological dependence): psychiatric disorder characterized by continued compulsive use of substance despite harm MANAGEMENT INVASIVE PAIN TREATMENT INTERVENTIONAL PAIN MANAGEMENT • Epidural or Perineural injections of local anesthetics or cortico steroids. • Implantations of epidural and intrathecal drug delivery systems. • Neural ablative procedures. • Insertion of spinal cord stimulators. • Sympathetic nerve blocks. ROLE OF INVASIVE PROCEDURES • Intractable pain • Intractable side effects • Symptoms that persists despite carefully individualized patient management SELECTION OF BLOCK • Depends on: • Location of pain • Presumed mechanism • Skills of treating physician • Local anesthetics can be applied locally, at peripheral nerve, somatic plexus, sympathetic ganglia or nerve root, centrally in neuraxis SOMATIC NERVE BLOCKS • Trigeminal nerve blocks • Cervical, Thoracic, Lumbar paravertebral blocks • Facet blocks • Trans sacral nerve blocks etc. LOW BACK PAIN: FACET SYNDROME LOW BACK PAIN: FACET SYNDROME SYMPATHETIC BLOCKS • Stellate ganglion block • Celiac plexus block • Thoracic, lumbar sympathetic chain block etc. EPIDURAL INJECTIONS • Lumbar interlaminar epidural injections • Fluoroscopic Injections • Transforaminal injections • Radiofrequency rhizotomy LOW BACK PAIN AND RADICULAR PAIN SECONDARY TO A HERNIATED DISC LOW BACK PAIN AND RADICULAR PAIN SECONDARY TO A HERNIATED DISC • Steroids recommended for ESI: • Methylprednisolone (largest) • Betamethasone • Triamcinolone (smallest) • Dexamethasone (no identifiable particles) PAIN TREATMENT CONTINUUM Diagnosis Oral Medications PT, Exercise, Rehabilitation Behavioral Medicine Corrective Surgery Therapeutic Nerve Blocks Oral Opiates Implantable Pain Management Devices Neurostimulation Intrathecal Pumps Neuroablation PRINCIPLES OF MANAGEMENT OF CHRONIC PAIN • By the Mouth - Simple, effective, convenient • By the Clock - Prevent pain after treating it Do not use PRN. Do not wait for pain to return • By the Ladder - move on to stronger analgesics if pain is not controlled. • Individualize PAIN CONSULTATION TEAM • Multidisciplinary group • Provides consultation services only • not ongoing treatment Consultation Team Anesthesiology Neurology Psychology Pharmacy Nursing Referral Recommendation CHRONIC PAIN DISCIPLINES AND ROLES (CORE) Anesthesiology – nerve blocks, pharmacologic Kinesiotherapy – pool therapy; activity Neurology – eval. treatment Nursing – patient care Physical Medicine/ Physical Therapy – exercise; modalities Psychology – eval. and treatment Occupational Therapy – UE eval and treatment Vocational Rehab – job eval and training SUMMARY • Chronic neuropathic pain is a disease, not a symptom • “Rational” polypharmacy is often necessary • combining peripheral and central nervous system agents enhances pain relief • Treatment goals include: • balancing efficacy, safety, and tolerability • reducing baseline pain and pain exacerbations • improving function and QOL • New agents and new uses for existing agents offer additional treatment options REFERENCES • Review Neuropathic pain: a practical guide for the clinician ; Ian Gilron, C. Peter N. Watson, Catherine M. Cahill and Dwight E. Moulin • Dworkin RH, Backonja M, Rowbotham MC, et al. Advances in neuropathic pain. Arch Neurol 2003;60:1524-34. • Gilron I, Bailey JM, Tu D, et al. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med 2005;352:1324-34. • Stephen Macres, Understanding Neuropathic Pain • Eisenberg E, McNicol ED, Carr DB. Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin. JAMA 2005;293:304352. Thank You! DISTINGUISHING DEPENDENCE, TOLERANCE, AND ADDICTION • Physical dependence: withdrawal syndrome arises if drug discontinued, dose substantially reduced, or antagonist administered • Tolerance: greater amount of drug needed to maintain therapeutic effect, or loss of effect over time • Pseudoaddiction: behavior suggestive of addiction; caused by undertreatment of pain • Addiction (psychological dependence): psychiatric disorder characterized by continued compulsive use of substance despite harm