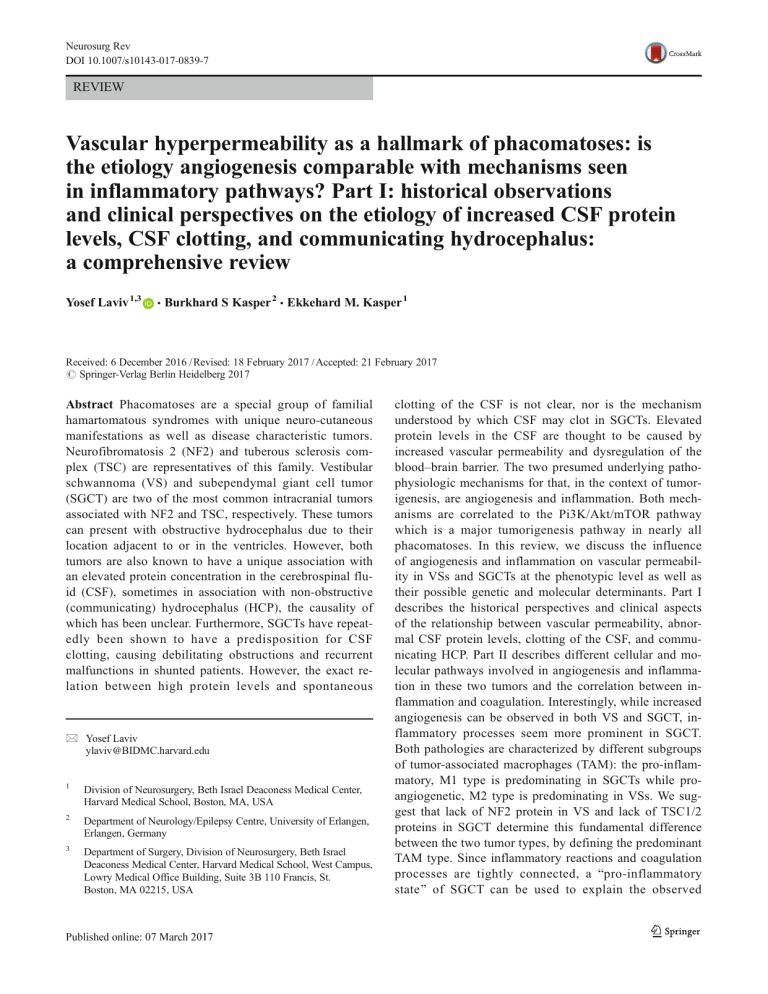
Neurosurg Rev DOI 10.1007/s10143-017-0839-7 REVIEW Vascular hyperpermeability as a hallmark of phacomatoses: is the etiology angiogenesis comparable with mechanisms seen in inflammatory pathways? Part I: historical observations and clinical perspectives on the etiology of increased CSF protein levels, CSF clotting, and communicating hydrocephalus: a comprehensive review Yosef Laviv 1,3 & Burkhard S Kasper 2 & Ekkehard M. Kasper 1 Received: 6 December 2016 / Revised: 18 February 2017 / Accepted: 21 February 2017 # Springer-Verlag Berlin Heidelberg 2017 Abstract Phacomatoses are a special group of familial hamartomatous syndromes with unique neuro-cutaneous manifestations as well as disease characteristic tumors. Neurofibromatosis 2 (NF2) and tuberous sclerosis complex (TSC) are representatives of this family. Vestibular schwannoma (VS) and subependymal giant cell tumor (SGCT) are two of the most common intracranial tumors associated with NF2 and TSC, respectively. These tumors can present with obstructive hydrocephalus due to their location adjacent to or in the ventricles. However, both tumors are also known to have a unique association with an elevated protein concentration in the cerebrospinal fluid (CSF), sometimes in association with non-obstructive (communicating) hydrocephalus (HCP), the causality of which has been unclear. Furthermore, SGCTs have repeatedly been shown to have a predisposition for CSF clotting, causing debilitating obstructions and recurrent malfunctions in shunted patients. However, the exact relation between high protein levels and spontaneous * Yosef Laviv ylaviv@BIDMC.harvard.edu 1 Division of Neurosurgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA 2 Department of Neurology/Epilepsy Centre, University of Erlangen, Erlangen, Germany 3 Department of Surgery, Division of Neurosurgery, Beth Israel Deaconess Medical Center, Harvard Medical School, West Campus, Lowry Medical Office Building, Suite 3B 110 Francis, St. Boston, MA 02215, USA clotting of the CSF is not clear, nor is the mechanism understood by which CSF may clot in SGCTs. Elevated protein levels in the CSF are thought to be caused by increased vascular permeability and dysregulation of the blood–brain barrier. The two presumed underlying pathophysiologic mechanisms for that, in the context of tumorigenesis, are angiogenesis and inflammation. Both mechanisms are correlated to the Pi3K/Akt/mTOR pathway which is a major tumorigenesis pathway in nearly all phacomatoses. In this review, we discuss the influence of angiogenesis and inflammation on vascular permeability in VSs and SGCTs at the phenotypic level as well as their possible genetic and molecular determinants. Part I describes the historical perspectives and clinical aspects of the relationship between vascular permeability, abnormal CSF protein levels, clotting of the CSF, and communicating HCP. Part II describes different cellular and molecular pathways involved in angiogenesis and inflammation in these two tumors and the correlation between inflammation and coagulation. Interestingly, while increased angiogenesis can be observed in both VS and SGCT, inflammatory processes seem more prominent in SGCT. Both pathologies are characterized by different subgroups of tumor-associated macrophages (TAM): the pro-inflammatory, M1 type is predominating in SGCTs while proangiogenetic, M2 type is predominating in VSs. We suggest that lack of NF2 protein in VS and lack of TSC1/2 proteins in SGCT determine this fundamental difference between the two tumor types, by defining the predominant TAM type. Since inflammatory reactions and coagulation processes are tightly connected, a Bpro-inflammatory state^ of SGCT can be used to explain the observed Neurosurg Rev associated enhanced CSF clotting process. These distinct cellular and molecular differences may have direct therapeutic implications on tumors that are unique to certain phacomatoses or those with similar genetics. Keywords Phacomatoses . Neurofibromatosis . Tuberous sclerosis . Cerebrospinal fluid . Vascular permeability . Angiogenesis . Inflammation . Protein . Giant cell tumor . Schwannoma Abbreviations BBB Blood–brain barrier (c)HCP (Communicating) hydrocephalus CNS Central nervous system CSF Cerebrospinal fluid EC Endothelial cell eNOS Endothelial nitric oxide synthase HGB Hemangioblastoma ICP Intracranial pressure mTOR Mammalian target of rapamycin NF Neurofibromatosis NO Nitric oxide Pi3K Phosphatidylinositol-3-kinase SGCT Subependymal giant cell tumor TSC Tuberous sclerosis complex VEGF Vascular endothelial growth factor vHL von Hippel–Lindau VPS Ventriculoperitoneal shunt VS Vestibular schwannoma Introduction In 1923, the European ophthalmologist Van der Hoeve introduced the term Bphacomatoses^ into the literature to describe a hereditary group of diseases characterized by the presence of disseminated hamartomas in neuro-ectodermal-derived tissues [99]. The technical term is derived from the Greek word BPhakos,^ meaning Blentil,^ which was used to describe the lens of the eye, an organ that is characteristically involved in all phacomatoses. It also carries the meaning of Bspot^ or Bbirth mark,^ emphasizing both the patchy (or Bspotty^) involvement of the skin and various other organs as well as the hereditary nature of these syndromes. Although each original description of any of the classic phacomatoses was based on careful clinical and pathologic observations, we know now that phacomatoses are bound together by complex genetics and molecular pathways. These autosomal dominantly inherited disorders include neurofibromatoses 1 and 2 (NF1/2); tuberous sclerosis complexes 1 and 2 (TSC-1/2) and von Hippel–Lindau disease (vHL); and the less known Sturge– Weber syndrome, ataxia telangiectasia, nevoid basal cell carcinoma syndrome, Cowden disease, Peutz–Jeghers syndrome, familial adenomatous polyposis, and juvenile polyposis [98]. Each of the genetic mutations underlying a phacomatosis encodes a tumor suppressor protein that functions in signal transduction [98]. Some tumors may occur sporadically, without the associated manifestations of the respective syndromes [29], yet their molecular signature alterations and phenotype presentation are similar to tumors encountered in the setting of syndromic phacomatoses [29]. Subependymal giant cell tumors (SGCTs; characteristic of TSC) and vestibular schwannomas (VSs; characteristic of neurofibromatosis 2 (NF2)) are two benign, intracranial tumors related to phacomatoses. Both locate to distinct CSF spaces, namely the lateral ventricle and the cerebellopontine angle cistern, respectively. Interestingly, these two unique tumors are the only intracranial benign neoplasms repeatedly associated with elevated CSF protein levels (= proteinorhachia), sometimes in the context of symptomatic non-obstructive hydrocephalus. However, of the two, only SGCT is associated with a true clotting tendency of the CSF, which frequently leads to refractory shunt obstructions [66]. Increased cerebrospinal fluid (CSF) protein level results as a consequence of interrupted blood–brain barrier (BBB). The BBB is a complex, highly selective anatomical and physiological barrier, which regulates the entry and egress of metabolites such as cerebral nutrients and other biological substances essential for cerebral metabolism and neuronal activity [20]. The BBB is formed primarily by the layer of endothelial cells lining the microvessels within the brain parenchyma along with their closely associated astrocytic processes. Neighboring endothelial cells are joined via tight junctions that effectively block free passage of molecules and ions via the paracellular route across this layer. Any substance exchange with the brain across the barrier must hence be processed through the cells and must either pass through the lipid portions of the plasma membranes (if hydrophilic) or be transferred via specific transporters localized in the apical or basilar membranes of the cells [54]. Central nervous system (CNS) pathologies, such as trauma, ischemia, inflammation, malignancy, and degenerative and demyelinating diseases, can cause interruption and breakdown of the BBB [2], leading to spillage of intravascular plasma proteins into the brain parenchyma and CSF. This pathological Bopening^ of the BBB can also be referred to as vascular hyperpermeability. Traditionally, the term vascular permeability plays a paramount role in basal vascular sieving of solutes and small molecules in an unstimulated setting [24] and is essential for normal tissue homoeostasis. When dysregulated though, hyperpermeability becomes an important feature of many pathological processes, including cancer [25]. Molecular regulators of vascular permeability include angiogenesis- Neurosurg Rev associated growth factors (such as vascular endothelial growth factor (VEGF)), activating factors (such as platelet-activating factor (PAF)), and inflammatory cytokines (such as histamine, bradykinin, and nitric oxide) [24, 37]. In this first part of our manuscript, we will describe the seminal historic observations made on the topic. We shall review clinical aspects regarding changes in CSF protein levels seen in association with CNS tumors, and we will correlate these parameters to the occurrence of communicating hydrocephalus and clotting of the CSF that is characteristic for SGCT and VS. Communicating hydrocephalus and elevated CSF protein levels Hydrocephalus (HCP) is characterized by abnormal CSF dynamics that leads to CSF accumulation with dilatation of the ventricles. HCP can be classified as either obstructive with mechanical blockage of CSF circulation or communicating (= non-obstructive) from presumed impaired CSF absorption. This absorption is thought to occur via arachnoid granulations into the venous sinuses [62]. Common etiologies of communicating hydrocephalus (cHCP) are idiopathic, post subarachnoidal hemorrhage, and post meningitis. cHCP may also be associated with conditions causing increased CSF protein levels, such as in, e.g., Guillain-Barré syndrome [7]. Other scenarios include cHCP secondary to intraspinal tumors, which occurs in about 1% of patients with benign spinal cord tumors [7] and in as many as 65% of malignant spinal tumor cases [23]. In patients with intracranial tumor, cHCP is most frequently observed in the setting of leptomeningeal metastasis [78, 83], with an incidence of about 25% [58]. It can also be associated with supratentorial gliomas in ca. 2.5% of cases [31]. Interestingly, in the largest series published on this topic for supratentorial gliomas, 95% of hydrocephalic cases occurred in high-grade gliomas after at least one surgical resection [31]. The etiology of cHCP in this setting may be multifactorial and related to post surgical changes, post radiation changes, and leptomeningeal spread leading to high protein content of the CSF [31, 55, 74]. Most of these factors, however, cannot explain the occurrence of cHCP in association with benign, single, small, previously untreated intracranial tumor. The most likely explanation for this rare scenario is some form of de novo increase in CSF protein concentration. Almost all CSF protein is derived from serum [44]. There is a 200-fold difference in the steady-state concentration between these two compartments (about 35 and 7000 mg/dl in CSF and serum, respectively), and this difference is maintained because of the BBB [44]. Several aspects are of interest here. Serum contains three main protein constituents: albumin, globulins, and fibrinogen [3]. If the BBB is intact and undisturbed, all serum proteins with a molecular weight greater than 160 kDa are largely excluded from the CSF [42]. For example, fibrinogen (whose molecular weight is 340 kDa) has a normal CSF concentration of 0.6 mg/dl with a plasma-to-CSF ratio of 4940. However, when the BBB is dysfunctional, certain macromolecules from the serum may be readily detected in the CSF [44]. In fact, five mechanisms for pathological changes in distribution of proteins in the CSF have been described [44]: (a) increased entry of plasma proteins due to disruption in BBB, (b) defective reabsorption of CSF proteins via the arachnoid villi, (c) primary changes in plasma protein (rare, example, elevated Bence–Jones protein in CSF in multiple myeloma patients), (d) local immunoglobulin production due to various chronic and subacute inflammatory diseases of the CNS, and (e) degenerative patterns. In their classic monograph (1937), Merritt and FremontSmith provided the most detailed description regarding CSF findings in patients with brain tumors [71]. In their series of 106 patients, the second most common finding (after elevated opening pressure) was an elevated total protein content. Total CSF protein was >100 mg/dl (normal 15–45 mg/dl) in 29% of glioma patients and was 45–100 mg/dl in another 37% of cases. Furthermore, higher protein levels were associated with higher pathological tumor grades. It was suggested that such changes are due to increased passage of plasma proteins into the CSF across an abnormal BBB or due to local inflammatory response and necrosis generated by the tumor itself [56, 75]. Importantly, Merrit and Fermont-Smith found VS to be an exception of this rule; these lesions were commonly associated with a total CSF protein contents of 100–500 mg/dl in the absence of any significant necrosis or inflammation [71]. In 1954, Gardner et al. described two cases in which small, benign intracranial and intraspinal tumors were associated with high CSF protein content, increased intracranial pressure, and papilledema [46]. The first case was that of a cauda equina ependymoma with a CSF protein level of 425 mg/dl, yellow fluid, and no cells. In the second case, a 2-cm VS was associated with a CSF protein level of 400 mg/dl. After resection of the tumor, protein levels dropped to 31 mg/dl and the associated HCP resolved. It was noted that high protein levels in the CSF caused Bclotting of the CSF, with obstruction of the Pacchionian bodies^ [46]. Interestingly, the authors have suggested that the chronicity of the case is more important than the actual level of the protein (i.e., the cause of the malabsorption is the gradual blocking of CSF egress and not the increased osmotic tension of the protein-enriched fluid). In a related experiment, the authors injected a dog with high levels of albumin and gamma-globulin (two components of CSF’s proteins) into its subarachnoid cisterns. This maneuver failed to produce papilledema, and protein levels declined rapidly from 1000 mg/dl immediately post injection to 100–200 mg/ dl at 5 h and back to normal levels at 24 h. Accordingly, the authors concluded that in order to achieve and maintain high protein levels in the CSF, the entry of proteins into it must be Neurosurg Rev constant and at high rate [46]. Their final conclusion was that Ba small tumor located anywhere along the cerebrospinal axis can cause increased intracranial pressure, papilledema and communicating hydrocephalus^ through constantly elevated levels of protein in the CSF and that these sequelae are reversible once the tumor is resected [46]. In a separate experiment, an elevation of CSF total protein level by injection of serum itself resulted in a decreased rate of absorption of CSF albumin. Thus, a vicious cycle exists, whereby a gradual increase in protein further slows protein absorption [88]. It should be noted that it is still unclear whether high protein concentrations in the CSF contribute to cHCP formation through a malabsorptive or a hyperosmotic mechanism. Proteins are large macromolecules that are not diffusible through the BBB and therefore contribute to larger osmotic content in any fluid compartment. Higher protein content in a fluid compartment will change the osmotic gradient in favor of water transport into the respective compartment vs. the level present at that time in blood [61]. Indeed, recent studies suggest that chronically increased CSF osmolality is sufficient to produce HCP by creating an osmotic gradient which draws water into the ventricles (presumably through aquaporins) [62, 63]. Regardless of what pathophysiological mechanism is correct or dominant, the association between high levels of protein in the CSF and the subsequent development of cHCP has been repeatedly demonstrated. For over half a century, cHCP is being treated successfully by way of ventricular shunting [35]. On the other hand, high CSF protein levels are considered a relative contraindication for shunt placement [82]. This conflict will be discussed in the following section. CSF viscosity, CSF clotting, and fibrin Bsignature^ of tumors BAmong the many changes which the cerebrospinal fluid may undergo, certainly the most striking to the clinical observer is a yellow coloration associated with the formation in the fluid, soon after it is received into a test-tube, of a coagulum, which may be so firm as to allow of the tube being turned upside down without a drop of fluid escaping^ [Sir JC Greenfield, 1921]. The main objection for shunting hyperproteinorhachic patients has been that a high protein content in the CSF would increase its viscosity and would thus impair its flow through the catheter [82]. However, it has been shown that the mean viscosity of CSF with a normal protein content is only 1.4% greater than water at the same temperature, and there is little increase in the mean viscosity of CSF specimens with increased protein content [22]. It means that in order to have high protein levels resulting in blocking of a shunt catheter, it probably will not be due to changes in viscosity. It therefore must be due to specific proteins that promote coagulation and adhesion and/or a strong inflammatory response. Recurrent shunt obstructions can occur in the presence of a highly viscous fluid or a coagulable fluid. However, these are two different pathophysiological properties. Viscosity is the one property of a fluid that will affect its flow through any given length of tubing. Viscous CSF refers to CSF that flows very slowly, dripping like glycerine from a tube. Truly viscous CSF is extremely rare and, as mentioned, unrelated to absolute levels of CSF protein. Fishman described two cases with truly high CSF viscosity [44]: one case associated with large amounts of mucin secreted by a metastatic mucinous adenocarcinoma originating from colon which presented with diffuse leptomeningeal carcinomatosis and a second case of cryptococcal meningitis (in this case, high viscosity was attributed to the polysaccharide capsules of the yeasts). Viscous CSF can also occur secondary to puncturing the annulus fibrosus of a lumbar disc and the release of its liquid nucleus pulposus [36]. However, these are all extremely rare scenarios. On the other hand, the observation of a CSF sample that clots easily occurs more frequently. It occurs when sufficient serum protein, including fibrinogen, is present in the CSF. The conversion of fibrinogen to fibrin in the subarachnoid space may induce arachnoiditis, fibrous adhesions, and eventually obliteration of the subarachnoid spaces [96]. The same process will lead to obliteration of a ventricular catheter or any other indwelling catheter located in a CSF compartment. In healthy conditions, fibrinogen circulates through the brain and the spinal cord vasculature without entering the CNS parenchyma due to the elaborate architecture of the BBB [30]. Several pathological conditions that involve either acute hemorrhage, especially in the subarachnoid space (such as brain or spinal cord injury, aneurysmal bleeding, and hemorrhagic stroke), or chronic disruption of the BBB (such as multiple sclerosis, Alzheimer’s disease, brain glioblastoma, HIV encephalitis, and bacterial meningitis) result in the deposition of fibrin/fibrinogen in the CNS [30, 44]. In regard to tumors, acute or chronic subarachnoid hemorrhage or seeping from tumor vessels is known as Fincher’s syndrome [43] and has been described in various settings including in cases of VS [10, 47, 50]. However, for the purpose of this review, we will focus on non-hemorrhagic causes for increased CSF protein levels and CSF clotting. Of note, although non-hemorrhagic clotting of CSF is very rare in the context of benign, intracranial neoplasms, deposition of fibrin in the stroma of tumor masses has long been demonstrated. The Irish pathologist, R.A.Q. O’Meara, was the first to propose in the late 1950s that fibrin was deposited in solid tumors [81]. Further studies have shown that fibrin provides a characteristic and reproducible signature for certain types of tumors in much the same way as seen with other histologic features [40]. Fibrin deposits must result from the Neurosurg Rev extravasation and extravascular clotting of plasma fibrinogen because only a very few well-differentiated hepatocellular carcinomas can actually synthesize and secrete fibrinogen [40]. In tumors, as well as in other non-neoplastic pathologies, extravascular fibrin serves as a provisional matrix that favors and supports the ingrowth of new blood vessels and other mesenchymal cells that generate mature, vascularized stroma [38]. The most important among these changes is the wellcoordinated inward migration of macrophages, fibroblasts, and new blood vessels, followed by local synthesis and deposition of interstitial collagens and proteoglycans [40]. The extent of fibrin deposition and its persistence over time vary extensively between different tumors. Apparently, these differences depend on quantitative balances among vascular hyperpermeability, clotting, and fibrinolysis that are unique to individual tumors [39]. Indeed, accumulation of fibrinogen and fibrin in the CSF can be associated with increased level of protein in this media in the absence of hemorrhage. Usually, this is the result of hyperpermeability of the respective tumor vasculature and was associated with CSF protein levels in excess of 1500 mg/dl [44]. Classically, this was observed in the presence of an intradural tumor in the lumbar region, a condition known as Froin’s syndrome [13, 17, 79]. The association between Froin’s syndrome, high levels of CSF proteins, and CSF clotting in relation to VS and SGCT is further discussed in the following section. Elevated CSF protein levels and hypercoagulable CSF in VS and SGCT Vestibular schwannomas (VSs or acoustic neuromas) are benign, Schwann cell-derived tumors that commonly arise from the vestibular portion of the eighth cranial nerve. They are the most common intracranial schwannomas and are also associated with NF2 [94]. The overall incidence of VS is about 1/100,000 person-years [89] whereas the incidence of NF2 is between 1/33,000 and 1/87,410 live births [94]. Stunningly, a correlation between VS, elevated levels of CSF protein, and Froin’s syndrome can be dated back nearly a century. In 1921, Sir Joseph Godwin Greenfield, Bthe father of neuropathology,^ published his landmark review on Froin’s syndrome [52]. Froin’s syndrome was also known as Bsyndrome de coagulation massive et de xanthochromie^ and was originally (1903) described as hypercoagulable, xantochromic CSF in the presence of chronic CNS infections [45]. A few years later (1909), Blanchetiere and Lejonne were the firsts to describe the full syndrome of Froin in association with a spinal tumor (here Bsarcoma^) [52]. Over the years and mainly due to the markedly decreased prevalence of chronic spine infections such as leprosy and tuberculosis, Froin’s syndrome was mostly associated with the presence of a spinal tumor blocking distal CSF flow [64, 67, 73]. Importantly, in the same review, Greenfield mentioned that others have found yellow and highly albuminous fluid in several cases of tumors of the pontocerebellar angle [52]. Greenfield acknowledged this observation by commenting that Bit is not impossible that these changes might be present in the fluid of cases of solitary eighth-nerve tumor, though I have not personally encountered this^ [52]. Almost 100 years later, the association between high CSF protein levels, cHCP, and VS has become a welldocumented phenomenon. HCP occurs in 1.2 to 42% of VS patients [6, 11, 14, 19, 87, 91, 97, 101]. Due to its relative proximity to the fourth ventricle, large VS can cause obstructive HCP. Nevertheless, in large published series, the majority (60–80%) of observed HCP cases were of the communicating type [48, 91]. In other series, the exact pathophysiology remained unclear and was considered to be a combination of both types. For example, in a study on 400 resected VSs, persistent HCP was found in up to 22% of Bobstructive^ cases even after resection (compared to 12.5% of Bcommunicating^ cases) suggesting a dual pathophysiology [48]. The presenting symptoms of HCP can either be increased intracranial pressure (ICP), which usually indicates an obstructive pathology, or the persistence of a clinical triad typical of normal pressure hydrocephalus (NPH), which may indicate a communicating pathology. In the series by Pirouzmand et al., 90% (30/33) of patients with VS and HCP clinically presented with NPH [87]. This observation further supports the relatively high incidence of cHCP in VS patients [18]. In our own series on 30 VSs treated by stereotactic radiosurgery, 4 were associated with cHCP (unpublished data). All four patients had signs and symptoms of NPH, and two were treated with shunt placement. None of these patients needed shunt revision over >5-year follow-up. Figures 1 and 2 illustrate two of the cases. In our two shunted patients, pretreatment CSF protein levels were 114 and 193 mg/dl, respectively. In a number of series describing an association between cHCP and VS, varying levels of CSF protein have been reported with an increase in concentration ranging from 1.5- to 15-fold [6, 14, 91]. Other etiological factors considered relevant for the development of cHCP in VS patients are recurrent tumor bleeding, seeding of tumor cells through the CSF, and an age-related decrease in CSF reabsorption capacity [6]. Of note, the incidence of HCP in patients with small VSs (<3 cm) was 12-fold higher in older patients than in younger ones (25 vs. 2.1%, respectively) [97], which again may reflect a more complex pathophysiology. As mentioned earlier, in order to eliminate potential selection bias secondary to post surgical or post radiation changes, we shall focus on the prevalence of elevated liquor protein levels and cHCP in untreated patients. In a review by Edwards et al., 73/75 (97%) of patients with untreated VSs were found to have high CSF protein levels (>70 mg/dl) [41]. On the other hand, none of the larger series in which shunt Neurosurg Rev Fig. 1 A 63-year-old male presents with mild hearing loss on the left side, found to have a 13 mm × 16 mm, homogenously enhancing lesion in the left cerebellopontine angle (CPA), extending into the internal auditory canal, consisting with vestibular schwannoma (a MRI; post-contrast T1wi, coronal cuts). Patient had no signs or symptoms compatible with increased intracranial pressure or NPH. Ventricles’ sizes were only mildly enlarged (b MRI, fluid attenuation inversion recovery (FLAIR) sequence). Patient underwent SRS treatment (hypofractionated, 2500 cGy) 1 year after diagnosis due to gradual tumor’s enlargement. Approximately 8 months later, he started having NPH-related symptoms (NPH triad). Repeat MRI showed very mild change in tumor’s size since the time of diagnosis (c MRI; post-contrast T1-wi, coronal cuts); however, the ventricles were significantly larger (d MRI, FLAIR sequence), with signs of transependymal flow (black arrows). The fourth ventricle was not compressed (not shown), and images were compatible with communicating hydrocephalus. Unfortunately, patient was lost to follow-up before placement of ventricular shunt could be discussed placement was the primary surgical intervention for VS have reported complications of recurrent shunt malfunction secondary to elevated CSF protein levels or CSF clotting [48, 87, 97]. In the study by Al Hinai et al., VS patients presenting with symptomatic cHCP were treated with ventriculoperitoneal shunt (VPS) placement despite CSF protein concentrations as high as 900 mg/dl and no subsequent shunt obstruction was reported [6]. In fact, although an association between VS, high CSF protein levels, and HCP has been inferred for nearly a century, we did not come across a single description of recurrent shunt malfunctions secondary to increased CSF protein levels or due to hypercoagulable CSF in this setting. This is in sharp contradiction to the reports on managing SGCT under similar circumstances. Tuberous sclerosis complex (TSC) affects approximately one million individuals worldwide, with a birth incidence of approximately 1 in 6000 [66]. Subependymal giant cell astrocytoma (SGCT) is a benign (WHO grade I) and slow-growing intraventricular tumor. It is almost always encountered in the setting of TSC. Up to 20% of individuals with TSC will develop SGCT, usually during the first two decades of life [4], making it the most frequent intracranial tumor type in TSC. SGCTs are known to present with signs and symptoms of increased ICP secondary to obstructive HCP due to its most common location at the foramen of Monroi [32]. In addition and similar to VS, most symptomatic cases are treated by surgical resection of the tumor [32]. In a review on 84 pediatric patients, 22 (26%) shunt surgeries were reported [53]. Neurosurg Rev Fig. 2 A 69-year-old female patient presented with tinnitus and gait instability. She was found to have a wide-based, shuffling gait. Brain MRI demonstrated a 20 mm × 27 mm, homogenously enhancing lesion in the left CPA, extending into the internal auditory canal, consisting with vestibular schwannoma (a MRI, post-contrast T1-wi, axial cuts). All four ventricles were enlarged substantially, consisting with communicating hydrocephalus (b MRI, FLAIR sequence; arrows indicate transependymal flow). Patient’s gait was improved after a lumbar puncture trial, and a permanent ventriculoperitoneal shunt was placed. Three months later, she was treated with hypofractionated SRS (2500 cGy) to the lesion. On a 5-year followup, both the tumor and the ventricles are smaller and well controlled (c MRI, post-contrast T1wi, axial cuts. d MRI, T2-wi, axial cuts; arrow points at the ventricular catheter) Comparable to VS, 86 % (19/22) of these shunts were inserted after tumor resection [53]. Nevertheless, reports on presurgical elevated protein content in the CSF in this setting and an association with cHCP exist. In a case series by Di Rocco and colleagues, all ten pediatric patients with tuberous sclerosis and SGCT were found to have high CSF protein levels (mean 600 mg/dl, range 270–1500 mg/dl) [33]. Three out of those ten patients were treated with upfront VPS placement, and two out of those three suffered repeat episodes of obstruction of the shunt system. Of note, the third patient who has not had VPS malfunction also had the lowest CSF protein level of the entire cohort (270 mg/dl) [33]. Since this report was published, others have encountered similar problems of recurrent shunt malfunctioning in the presence of protein-rich, highly clotting CSF [66, 85] (Fig. 3). Reported CSF protein levels were between 945 and 2250 mg/dl [66], and in all of these cases, all four ventricles were enlarged, consistent with cHCP. This phenomenon of increased CSF coagulability is a unique feature of SGCT, making it an Bintracranial variant^ of the classic observation made in Froin’s syndrome. One of the pathophysiological prerequisites for Froin’s syndrome to occur is that spinal CSF must be contained in the lumbar Bculde-sac,^ which was shut off from communicating with fluid around the upper part of the cord (the mechanism being due to meningitis, tumor, or disease of the bones of the spine) [52]. Similarly, the predilection of SGCT to occur near the foramen of Monroi can cause the frontal horn of the lateral ventricle to become an isolated Bintracranial cul-de-sac,^ mimicking the pathological conditions of Froin’s syndrome. It is hard to decide whether or not this is part of the pathogenesis of CSF clotting observed in SGCT. However, it needs to be pointed out that (a) no other known obstructing intraventricular lesions are associated with this phenomena and (b) this was also reported in association with SGCTs not located at the foramen of Monroi [66]. It is noteworthy that this phenomenon has never been described in association with VS or other benign intraventricular neoplasms. Both angiogenesis and inflammation are characterized by increased vascular permeability, leading to extravasation of proteins from the serum [72, 77]. The presence of these two pathophysiologic mechanisms in VS and SGCT may contribute to the mentioned phenomena in these tumors. Neurosurg Rev Fig. 3 Hypercoagulable CSF as was observed at the time of ventriculoperitoneal shunt revision in TSC patient with SGCT Angiogenesis, inflammation, and vascular hyperpermeability in phacomatoses BAs a rule the tumors are sparsely vascularized but in some cases the vessels in certain areas are sufficiently numerous to give to the tumor an angiomatous appearance.^ [H. Cushing, Tumors of the nervus acusticus and the syndrome of the cerebellopontine angle, 1917]. Most solid tumors, regardless of their type and origin, cannot grow beyond a certain size (~11 mm3) unless they establish a blood supply by inducing new vessels sprouting from existing host capillaries in a process known as angiogenesis [65]. In tumors, the process of angiogenesis is strongly correlated with increased vascular permeability [77]. Fluid leakage in tumors takes place in such newly formed, highly abnormal blood vessels post angiogenesis [76]. These neovessels usually display greatly enlarged sinusoids that arise from preexisting normal venules by a process that involves pericyte detachment, vascular basal lamina degradation, and a 4–5-fold increase in lumen size that is accompanied by extensive endothelial cell thinning [76]. Microvascular extravasation has several clinical consequences, such as the formation of vasogenic brain edema and the formation of tumor-related cysts [12]. It is also a major determinant of radiographic appearance such as prominent and diffuse contrast enhancement of the tumor [27]. Interestingly, significant angiogenesis is a unifying feature of most familial hamartoma syndromes [9, 21]. In this regard, von Hippel–Lindau disease (vHL) is perhaps the most representative phacomatosis of all. The most common CNS tumor associated with vHL is hemangioblastoma (HGB), benign vascular tumors composed of tightly packed capillaries and neoplastic stromal cells. Besides the obvious, highly angiogenetic radiological and histological properties of these tumors, they are characterized by a very high rate (ca. 80%) of observed peritumoral edema and cysts, which are two characteristic features of increased vascular permeability [12, 49, 69]. Of note, nearly 30% of intracranial HGBs are also associated with HCP [57] though this is usually of the obstructive type, secondary to their most frequent location in the cerebellum with resulting compression of the fourth ventricle. These cases of HCP are usually resolved by surgical resection of the tumor, and shunt placement in vHL patients occurs rarely. In a large (n = 164) series on the management of cerebellar HGB in vHL patients, Jagannathan et al. described only two patients requiring VP shunt placement (one with craniospinal hemangioblastomatosis and one who developed renal cell carcinoma with metastases to the cerebellum and leptomeningeal carcinomatosis) [57]. In a pertinent review of the literature, we have found that VPS placement for patients with HGB is usually associated with the rare scenario of disseminated cases [5]. As expected from disseminated neoplasms, some of these cases were reported to have increased CSF protein levels [90, 102]. However, we could not find a single reported case describing an association between solitary HGB and high levels of protein in the CSF, clotting of the CSF, recurrent shunt malfunctions, or communicating HCP. We think that the reason for that is the intraaxial (i.e., intraparenchymal) location of HGB, as opposed to the intracisternal and intraventricular location of VS and SGCT, respectively. Therefore, despite being exemplary as a phacomatosis tumor with increased angiogenesis and hyperpermeability, we shall focus in this review on VS and SGCT only. The increased vascular permeability of schwannomas has been known for decades. Studies from the early 1970s have demonstrated that in human VS, numerous vessels are open to the extracellular space by gaps between capillary endothelial cells, lack of junctional substructure, and fenestrated membranes [68]. In addition, cyst formation as an expression of vascular hyperpermeability is frequently observed in VS [86]. Histologically, VSs are often characterized by cystic or fatty degeneration (aka degenerative changes or Antoni B morphology), focal accumulations of hyaline material around vessels, infiltration of histiocytes and siderophages, and hypercellularity (= Antoni A morphology) [8]. Although the occurrence of BAntoni B^ patterns was initially thought to be related to slow growth of schwannomas [28], such changes were not observed in slow-growing meningiomas or neurofibromas [84]. Vilanova et al. pointed out that the degree of degenerative changes correlates with tumor size and vascular abnormalities in the tumor [100]. Papiez et al. have shown that these degenerative changes are indeed related to the proliferation of vessels observed in schwannomas, along with functional deficits in the wall integrity causing increased permeability to proteins and blood. Interestingly, these vascular Neurosurg Rev changes were significantly more prominent in Antoni B areas and areas with such degeneration were not demonstrated in benign meningiomas or neurofibromas [84]. Most VSs contain numerous scattered vessels, often with thin walls. These vessels may cause bleeds within the tumor, and the resulting pigment deposit of hemosiderin in both macrophages and parenchyma is a characteristic feature of schwannoma [60]. Due to their unique vascular texture, schwannomas have been conceptualized as structurally analogous to benign mixed mesenchymal tumors such as angiomyoma, angiolipoma, and angiomatous fibrohistiocytoma [60]. Strikingly, these are also tumors of the TSC [9]. Many, if not all, solid tumors contain inflammatory features [26]. The effects of inflammation on vascular permeability have been known for decades [103]. Under normal physiological conditions, the peripheral vasculature is not permeable to macromolecules. However, in the presence of inflammation, potent mediators (such as histamine, bradykinins, serotonin, and prostaglandins) cause a significant increase in microvascular permeability of the peripheral vasculature [92]. The normal cerebral blood vessels appear mostly unable to respond to these potent mediators of microvascular extravasation [27], although it has been shown that brain endothelium permeability increases in response to as little as nanomolar concentrations of these agents [1]. Brain tumor vasculature loses BBB properties during angiogenesis, causing their vessels to function similarly to peripheral vasculature. Therefore, in certain cases, brain tumor vasculature can become responsive to mediators of vascular permeability associated with inflammation [80]. The interplay of angiogenesis, increased vascular permeability, and inflammatory responses is of special importance in TSC. Its associated tumors are highly vascularized [34] and inflammatory markers, such as cytokines and chemokines, have been found in specimen from patients with TSC [15, 16, 70, 93]. The characteristic histopathological feature of SGCT is a rich vascular stroma [51] with a substantial component of inflammatory cells, including mast cells and T lymphocytes [93]. In part II of this review, we discuss the close resemblance between pathways of inflammation and coagulation. We suggest that the predominance of the former in SGCT might explain the unique association between SGCT and the propensity of clotting of CSF in afflicted patients. Both NF2 and TSC phacomatoses demonstrate abnormal activation of the Pi3K/Akt/mTOR pathway (see part II, BNF2, TSC, and the Pi3K/Akt/mTOR pathway^ section). This pathway is involved in angiogenesis [59] as well as in inflammation [95]. In the second part of this review, we describe both aspects of this pathway in detail and emphasize their involvement in SGCT and VS at the cellular and molecular levels. Correlation between these two mechanisms and two types of tumor-associated macrophages is given as an explanation for the phenotypical differences between the two tumors. Finally, therapeutic implications of these differences are discussed. Summary VSs and SGCTs represent two of the most common intracranial tumors related to phacomatoses, recognized as NF2 and TSC syndromes, respectively. Both VS and SGCT are known to cause obstructive HCP due to their critical anatomical locations next to or inside the ventricles. Remarkably, both tumors are also uniquely known to be associated with elevated concentrations of protein levels in the CSF, sometimes in association with communicating HCP. Furthermore, SGCTs have been reported to be associated with CSF clotting, causing debilitating clinical courses due to recurrent shunt obstructions. This phenomenon of CSF clotting in the presence of small, benign tumor had been reported under the label of BFroin’s syndrome^ in the past when observed in association with spinal tumors. Thus, SGCT can be seen as representing a unique, intracranial variant of Froin’s syndrome. Elevated levels of CSF proteins and CSF clotting are caused by increased vascular permeability and dysfunction of the BBB. The two main pathophysiologic mechanisms responsible for that in association with tumorigenesis are angiogenesis and inflammation. In this review, we were able to demonstrate that these two mechanisms are actively present in VSs and SGCTs at the phenotypic level. In part II of the review, we describe these two pathological processes at the cellular and molecular levels and discuss their therapeutic implications. Compliance with ethical standards Conflict of interest The authors declare that they have no conflict of interest. Funding This work was not funded or financially supported. Informed consent Informed consent was obtained from all individual participants included in the study. Ethical approval For this type of study, formal consent is not required. References 1. 2. 3. 4. Abbott NJ (2000) Inflammatory mediators and modulation of blood-brain barrier permeability. Cell Mol Neurobiol 20:131–147 Adams RA, Passino M, Sachs BD, Nuriel T, Akassoglou K (2004) Fibrin mechanisms and functions in nervous system pathology. Mol Interv 4:163–176 Adkins JN, Varnum SM, Auberry KJ, Moore RJ, Angell NH, Smith RD, Springer DL, Pounds JG (2002) Toward a human blood serum proteome: analysis by multidimensional separation coupled with mass spectrometry. Mol Cell Proteomics 1:947–955 Adriaensen ME, Schaefer-Prokop CM, Stijnen T, Duyndam DA, Zonnenberg BA, Prokop M (2009) Prevalence of subependymal giant cell tumors in patients with tuberous sclerosis and a review of the literature. Eur J Neurol 16:691–696. doi:10.1111/j.14681331.2009.02567.x Neurosurg Rev 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. Akimoto J, Fukuhara H, Suda T, Nagai K, Hashimoto R, Michihiro K (2014) Disseminated cerebellar hemangioblastoma in two patients without von Hippel-Lindau disease. Surg Neurol Int 5:2152–7806 Al Hinai Q, Zeitouni A, Sirhan D, Sinclair D, Melancon D, Richardson J, Leblanc R (2013) Communicating hydrocephalus and vestibular schwannomas: etiology, treatment, and long-term follow-up. J Neurol Surg B Skull Base 74:68–74. doi:10.1055/s0033-1333621 Amlashi SF, Riffaud L, Morandi X (2006) Communicating hydrocephalus and papilloedema associated with intraspinal tumours: report of four cases and review of the mechanisms. Acta Neurol Belg 106:31–36 Antonescu CR SB, Woodruff JM (2013) Schwannoma. Tumors of the peripheral nervous system, AFIP atlas of tumor pathology series 4. American Registry of Pathology, City, pp 129–210 Arbiser JL, Brat D, Hunter S, D’Armiento J, Henske EP, Arbiser ZK, Bai X, Goldberg G, Cohen C, Weiss SW (2002) Tuberous sclerosis-associated lesions of the kidney, brain, and skin are angiogenic neoplasms. J Am Acad Dermatol 46:376–380 Arienta C, Caroli M, Crotti FM (1988) Subarachnoid haemorrhage due to acoustic neurinoma. Case report and review of the literature. Neurochirurgia (Stuttg) 31:162–165 Atlas MD, Perez de Tagle JR, Cook JA, Sheehy JP, Fagan PA (1996) Evolution of the management of hydrocephalus associated with acoustic neuroma. Laryngoscope 106:204–206 Baggenstos MA, Butman JA, Oldfield EH, Lonser RR (2007) Role of edema in peritumoral cyst formation. Neurosurg Focus 22:E9 Bergquist BJ (1988) Intraspinal tumor with hydrocephalus. Neurosurgery 22:969–970 Bloch J, Vernet O, Aube M, Villemure JG (2003) Non-obstructive hydrocephalus associated with intracranial schwannomas: hyperproteinorrhachia as an etiopathological factor? Acta Neurochir 145:73–78 Boer K, Crino PB, Gorter JA, Nellist M, Jansen FE, Spliet WG, van Rijen PC, Wittink FR, Breit TM, Troost D et al (2010) Gene expression analysis of tuberous sclerosis complex cortical tubers reveals increased expression of adhesion and inflammatory factors. Brain Pathol 20:704–719. doi:10.1111/j.1750-3639.2009. 00341.x Boer K, Jansen F, Nellist M, Redeker S, van den Ouweland AM, Spliet WG, van Nieuwenhuizen O, Troost D, Crino PB, Aronica E (2008) Inflammatory processes in cortical tubers and subependymal giant cell tumors of tuberous sclerosis complex. Epilepsy Res 78:7–21. Borgesen SE, Sorensen SC, Olesen J, Gjerris F (1977) Spinal tumours associated with increased intracranial pressure. Report of two cases and a discussion on the pathophysiology. Acta Neurol Scand 56:263–268 Bradley WG (2000) Normal pressure hydrocephalus: new concepts on etiology and diagnosis. AJNR Am J Neuroradiol 21: 1586–1590 Briggs RJ, Shelton C, Kwartler JA, Hitselberger W (1993) Management of hydrocephalus resulting from acoustic neuromas. Otolaryngol Head Neck Surg 109:1020–1024 Brightman MW, Klatzo I, Olsson Y, Reese TS (1970) The bloodbrain barrier to proteins under normal and pathological conditions. J Neurol Sci 10:215–239 Brugarolas J, Kaelin WG Jr (2004) Dysregulation of HIF and VEGF is a unifying feature of the familial hamartoma syndromes. Cancer Cell 6:7–10 Brydon HL, Hayward R, Harkness W, Bayston R (1995) Physical properties of cerebrospinal fluid of relevance to shunt function. 1: the effect of protein upon CSF viscosity. Br J Neurosurg 9:639– 644 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. Celli P, Cervoni L, Morselli E, Ferrante L (1993) Spinal ependymomas and papilledema: report of 4 cases and review of the literature. J Neurosurg Sci 37:97–102 Claesson-Welsh L (2015) Vascular permeability—the essentials. Ups J Med Sci 120:135–143. doi:10.3109/03009734.2015. 1064501 Claesson-Welsh L, Welsh M (2013) VEGFA and tumour angiogenesis. J Intern Med 273:114–127. doi:10.1111/joim.12019 Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30:1073–1081. doi:10.1093/ carcin/bgp127 Criscuolo GR (1993) The genesis of peritumoral vasogenic brain edema and tumor cysts: a hypothetical role for tumor-derived vascular permeability factor. Yale J Biol Med 66:277–314 Dahl I (1977) Ancient neurilemmoma (schwannoma). Acta Pathol Microbiol Scand A 85:812–818 Daras M, Kaley TJ (2015) Benign brain tumors and tumors associated with phakomatoses. Continuum (Minneap Minn) 21:397– 414. doi:10.1212/01.CON.0000464177.73440.44 Davalos D, Akassoglou K (2012) Fibrinogen as a key regulator of inflammation in disease. Semin Immunopathol 34:43–62. doi:10. 1007/s00281-00011-00290-00288 de la Fuente MI, DeAngelis LM (2014) The role of ventriculoperitoneal shunting in patients with supratentorial glioma. Ann Clin Transl Neurol 1:45–48. doi:10.1002/acn1003.1017 de Ribaupierre S, Dorfmuller G, Bulteau C, Fohlen M, Pinard JM, Chiron C, Delalande O (2007) Subependymal giant-cell astrocytomas in pediatric tuberous sclerosis disease: when should we operate? Neurosurgery 60:83–89 discussion 89-90 Di Rocco C, Iannelli A, Marchese E (1995) On the treatment of subependymal giant cell astrocytomas and associated hydrocephalus in tuberous sclerosis. Pediatr Neurosurg 23:115–121 Dodd KM, Yang J, Shen MH, Sampson JR, Tee AR (2015) mTORC1 drives HIF-1alpha and VEGF-A signalling via multiple mechanisms involving 4E-BP1, S6K1 and STAT3. Oncogene 34: 2239–2250. doi:10.1038/onc.2014.164 Drake JM, Kestle JR, Tuli S (2000) CSF shunts 50 years on—past, present and future. Childs Nerv Syst 16:800–804 Dripps RD, Vandam LD (1951) Hazards of lumbar puncture. J Am Med Assoc 147:1118–1121 Duran WN, Breslin JW, Sanchez FA (2010) The NO cascade, eNOS location, and microvascular permeability. Cardiovasc Res 87:254–261. doi:10.1093/cvr/cvq139 Dvorak HF, Brown LF, Detmar M, Dvorak AM (1995) Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol 146: 1029–1039 Dvorak HF, Harvey VS, McDonagh J (1984) Quantitation of fibrinogen influx and fibrin deposition and turnover in line 1 and line 10 guinea pig carcinomas. Cancer Res 44:3348–3354 Dvorak HF, Nagy JA, Berse B, Brown LF, Yeo KT, Yeo TK, Dvorak AM, van de Water L, Sioussat TM, Senger DR (1992) Vascular permeability factor, fibrin, and the pathogenesis of tumor stroma formation. Ann N Y Acad Sci 667:101–111 Edwards CH, Paterson JH (1951) A review of the symptoms and signs of acoustic neurofibromata. Brain 74:144–190 Felgenhauer K (1974) Protein size and cerebrospinal fluid composition. Klin Wochenschr 52:1158–1164 Fincher EF (1951) Spontaneous subarachnoid hemorrhage in intradural tumors of the lumbar sac; a clinical syndrome. J Neurosurg 8:576–584 Fishman RA (1980) Cerebrospinal fluid in disease of the nervous system. W.B Saunders City Neurosurg Rev F G (1903) Inflammations me ‘ninge’es avec chromatique, fibrineuse et cytologique du liquide ce’phalo-rachidien. Gazette des hoˆpitaux 76:1005–1006 46. Gardner WJ, Spitler DK, Whitten C (1954) Increased intracranial pressure caused by increased protein content in the cerebrospinal fluid; an explanation of papilledema in certain cases of small intracranial and intraspinal tumors, and in the Guillain-Barre syndrome. N Engl J Med 250:932–936 47. Gavra M, Thanos L, Pomoni M, Batakis N (2010) Spontaneous subarachnoid haemorrhage due to acoustic neurinoma. Case report and review of the literature. Br J Neurosurg 24:82–83. doi:10. 3109/02688690903506085 48. Gerganov VM, Pirayesh A, Nouri M, Hore N, Luedemann WO, Oi S, Samii A, Samii M (2011) Hydrocephalus associated with vestibular schwannomas: management options and factors predicting the outcome. J Neurosurg 114:1209–1215. doi:10. 3171/2010.10.JNS1029 49. Glasker S, Vortmeyer AO, Lonser RR, Lubensky IA, Okamoto H, Xia JB, Li J, Milne E, Kowalak JA, Oldfield EH et al (2006) Proteomic analysis of hemangioblastoma cyst fluid. Cancer Biol Ther 5:549–553 50. Gleeson RK, Butzer JF, Grin OD Jr (1978) Acoustic neurinoma presenting as subarachnoid hemorrhage. Case report. J Neurosurg 49:602–604 51. Grajkowska W, Kotulska K, Jurkiewicz E, Matyja E (2010) Brain lesions in tuberous sclerosis complex. Review. Folia Neuropathol 48:139–149 52. Greenfield JG (1921) Original papers: on Froin’s syndrome, and its relation to allied conditions in the cerebrospinal fluid. J Neurol Psychopathol 2:105–141 53. Harter DH, Bassani L, Rodgers SD, Roth J, Devinsky O, Carlson C, Wisoff JH, Weiner HL (2014) A management strategy for intraventricular subependymal giant cell astrocytomas in tuberous sclerosis complex. J Neurosurg Pediatr 13:21–28. doi:10.3171/ 2013.3179.PEDS13193 54. Hladky SB, Barrand MA (2014) Mechanisms of fluid movement into, through and out of the brain: evaluation of the evidence. Fluids Barriers CNS 11:26. doi:10.1186/2045-8118-1111-1126 eCollection 2014 55. Inamasu J, Nakamura Y, Saito R, Kuroshima Y, Mayanagi K, Orii M, Ichikizaki K (2003) Postoperative communicating hydrocephalus in patients with supratentorial malignant glioma. Clin Neurol Neurosurg 106:9–15 56. Irani DN (2008) Cerebrospinal fluid in clinical practice. Saunders, Elsevier Health Sciences, City 57. Jagannathan J, Lonser RR, Smith R, DeVroom HL, Oldfield EH (2008) Surgical management of cerebellar hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg 108:210– 222. doi:10.3171/JNS/2008/108/2/0210 58. Jung TY, Chung WK, Oh IJ (2014) The prognostic significance of surgically treated hydrocephalus in leptomeningeal metastases. Clin Neurol Neurosurg 119:80–83 59. Karar J, Maity A (2011) PI3K/AKT/mTOR pathway in angiogenesis. Front Mol Neurosci 4 60. Kasantikul V, Netsky MG (1979) Combined neurilemmoma and angioma. Tumor of ectomesenchyme and a source of bleeding. J Neurosurg 50:81–87 61. Krishnamurthy S, Li J (2014) New concepts in the pathogenesis of hydrocephalus. Transl Pediatr 3:185–194. doi:10.3978/j.issn. 2224-4336.2014.07.02 62. Krishnamurthy S, Li J, Schultz L, Jenrow KA (2012) Increased CSF osmolarity reversibly induces hydrocephalus in the normal rat brain. Fluids Barriers CNS 9:13. doi:10.1186/2045-8118-11891113 63. Krishnamurthy S, Li J, Schultz L, McAllister JP 2nd (2009) Intraventricular infusion of hyperosmolar dextran induces 45. 64. 65. 66. 67. 68. 69. 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. hydrocephalus: a novel animal model of hydrocephalus. Cerebrospinal Fluid Res 6:1743–8454 Kwon SK, Kim MW (2014) Pseudo-Froin’s syndrome, xanthochromia with high protein level of cerebrospinal fluid. Korean J Anesthesiol 67:S58–S59. doi:10.4097/kjae.2014.4067. S.S4058 Lane HA, Wood JM, McSheehy PM, Allegrini PR, Boulay A, Brueggen J, Littlewood-Evans A, Maira SM, Martiny-Baron G, Schnell CR et al (2009) mTOR inhibitor RAD001 (everolimus) has antiangiogenic/vascular properties distinct from a VEGFR tyrosine kinase inhibitor. Clin Cancer Res 15:1612–1622. doi:10. 1158/1078-0432.CCR-08-2057 Laviv Y, Jackson S, Rappaport ZH (2015) Persistent communicating hydrocephalus in adult tuberous sclerosis patients: a possible therapeutic role for everolimus. Acta Neurochir 157:241–245. doi: 10.1007/s00701-014-2309-0 Ljevak J, Poljakovic Z, Adamec I, Habek M (2014) Glioblastoma multiforme presenting as Froin’s syndrome: a new face of an old foe. Acta Neurol Belg 114:319–320. doi:10.1007/s13760-0140289-8 Long DM (1973) Vascular ultrastructure in human meningiomas and schwannomas. J Neurosurg 38:409–419 Lonser RR, Vortmeyer AO, Butman JA, Glasker S, Finn MA, Ammerman JM, Merrill MJ, Edwards NA, Zhuang Z, Oldfield EH (2005) Edema is a precursor to central nervous system peritumoral cyst formation. Ann Neurol 58:392–399 Maldonado M, Baybis M, Newman D, Kolson DL, Chen W, McKhann G 2nd, Gutmann DH, Crino PB (2003) Expression of ICAM-1, TNF-alpha, NF kappa B, and MAP kinase in tubers of the tuberous sclerosis complex. Neurobiol Dis 14:279–290 Merritt H.H. F-SF (1937) The cerebrospinal fluid. W. B. Saunders Co., City Michel CC, Curry FE (1999) Microvascular permeability. Physiol Rev 79:703–761 Mirza S, Adams WM, Corkhill RA (2008) Froin’s syndrome revisited, 100 years on. Pseudo-Froin’s syndrome on MRI. Clin Radiol 63:600–604. doi:10.1016/j.crad.2007.07.027 Montano N, D’Alessandris QG, Bianchi F, Lauretti L, Doglietto F, Fernandez E, Maira G, Pallini R (2011) Communicating hydrocephalus following surgery and adjuvant radiochemotherapy for glioblastoma. J Neurosurg 115:1126–1130. doi:10.3171/2011.8. JNS11738 Murray KJ, Ausman JI, Chou SN, Douglas SD (1977) Immunoproteins in human brain tumor cyst fluids. J Neurosurg 46:314–319 Nagy JA, Benjamin L, Zeng H, Dvorak AM, Dvorak HF (2008) Vascular permeability, vascular hyperpermeability and angiogenesis. Angiogenesis 11:109–119. doi:10.1007/s10456-10008-19099-z Nagy JA, Dvorak AM, Dvorak HF (2012) Vascular hyperpermeability, angiogenesis, and stroma generation. Cold Spring Harb Perspect Med 2:a006544. doi:10.1101/cshperspect. a006544 Nigim F, Critchlow JF, Kasper EM (2015) Role of ventriculoperitoneal shunting in patients with neoplasms of the central nervous system: an analysis of 59 cases. Mol Clin Oncol 3:1381–1386 Nishida K, Ueda S, Matsumoto K, Kusaka K, Takeuchi R (1990) Cauda equina neurinoma associated with normal pressure hydrocephalus—case report. Neurol Med Chir (Tokyo) 30:258–262 Nomura T, Ikezaki K, Natori Y, Fukui M (1993) Altered response to histamine in brain tumor vessels: the selective increase of regional cerebral blood flow in transplanted rat brain tumor. J Neurosurg 79:722–728 O’Meara RA (1958) Coagulative properties of cancers. Ir J Med Sci 394:474–479 Neurosurg Rev 82. 83. 84. 85. 86. 87. 88. 89. 90. 91. 92. Occhipinti ECC (1982) Shunt failure in hydrocephalus with high protein fluid. Monog Neural Sci 8:220–222 Omuro AM, Lallana EC, Bilsky MH, DeAngelis LM (2005) Ventriculoperitoneal shunt in patients with leptomeningeal metastasis. Neurology 64:1625–1627 Papiez J, Rojiani MV, Rojiani AM (2014) Vascular alterations in schwannoma. Int J Clin Exp Pathol 7:4032–4038 eCollection 2014 Perek-Polnik M, Jozwiak S, Jurkiewicz E, Perek D, Kotulska K (2012) Effective everolimus treatment of inoperable, lifethreatening subependymal giant cell astrocytoma and intractable epilepsy in a patient with tuberous sclerosis complex. Eur J Paediatr Neurol 16:83–85. doi:10.1016/j.ejpn.2011.1009.1006 Piccirillo E, Wiet MR, Flanagan S, Dispenza F, Giannuzzi A, Mancini F, Sanna M (2009) Cystic vestibular schwannoma: classification, management, and facial nerve outcomes. Otol Neurotol 30:826–834. doi:10.1097/MAO.0b013e3181b04e18 Pirouzmand F, Tator CH, Rutka J (2001) Management of hydrocephalus associated with vestibular schwannoma and other cerebellopontine angle tumors. Neurosurgery 48:1246–1253 discussion 1253-1244 Prockop LD, Fishman RA (1968) Experimental pneumococcal meningitis. Permeability changes influencing the concentration of sugars and macromolecules in cerebrospinal fluid. Arch Neurol 19:449–463 Propp JM, McCarthy BJ, Davis FG, Preston-Martin S (2006) Descriptive epidemiology of vestibular schwannomas. NeuroOncology 8:1–11 Rogers LR, LoRusso P, Nadler P, Malik G, Shields A, Kaelin W (2011) Erlotinib therapy for central nervous system hemangioblastomatosis associated with von Hippel-Lindau disease: a case report. J Neuro-Oncol 101:307–310. doi:10.1007/ s11060-010-0244-3 Rogg JM, Ahn SH, Tung GA, Reinert SE, Noren G (2005) Prevalence of hydrocephalus in 157 patients with vestibular schwannoma. Neuroradiology 47:344–351 Scallan J HV, Korthuis RJ. (2010) Capillary fluid exchange: regulation, functions, and pathology. Morgan & Claypool Life Sciences, City 93. Sharma M, Ralte A, Arora R, Santosh V, Shankar SK, Sarkar C (2004) Subependymal giant cell astrocytoma: a clinicopathological study of 23 cases with special emphasis on proliferative markers and expression of p53 and retinoblastoma gene proteins. Pathology 36:139–144 94. Slattery WH (2015) Neurofibromatosis type 2. Otolaryngol Clin N Am 48:443–460. doi:10.1016/j.otc.2015.02.005 95. Stark AK, Sriskantharajah S, Hessel EM, Okkenhaug K (2015) PI3K inhibitors in inflammation, autoimmunity and cancer. Curr Opin Pharmacol 23:82–91 96. Sullivan RL Jr, Reeves AG (1977) Normal cerebrospinal fluid protein, increased intracranial pressure, and the Guillain-Barre syndrome. Ann Neurol 1:108–109 97. Tanaka Y, Kobayashi S, Hongo K, Tada T, Sato A, Takasuna H (2003) Clinical and neuroimaging characteristics of hydrocephalus associated with vestibular schwannoma. J Neurosurg 98:1188– 1193 98. Tucker M, Goldstein A, Dean M, Knudson A (2000) National Cancer Institute Workshop Report: the phakomatoses revisited. J Natl Cancer Inst 92:530–533 99. Van der Hoeve J (1923) Eye diseases in tuberous sclerosis of the brain and in Recklinghausen’s disease Tran Ophthalmol Soc UK 43: 534–541 100. Vilanova JR, Burgos-Bretones JJ, Alvarez JA, Rivera-Pomar JM (1982) Benign schwannomas: a histopathological and morphometric study. J Pathol 137:281–286 101. Wada K, Nawashiro H, Shimizu A, Shima K (2003) MRI analysis of hydrocephalus associated with acoustic neurinoma. Acta Neurochir Suppl 86:549–551 102. Weil RJ, Vortmeyer AO, Zhuang Z, Pack SD, Theodore N, Erickson RK, Oldfield EH (2002) Clinical and molecular analysis of disseminated hemangioblastomatosis of the central nervous system in patients without von Hippel-Lindau disease. Report of four cases J Neurosurg 96:775–787 103. Wilhelm DL (1973) Mechanisms responsible for increased vascular permeability in acute inflammation. Agents Actions 3:297–306



