Heart failure review Pharmacy
advertisement

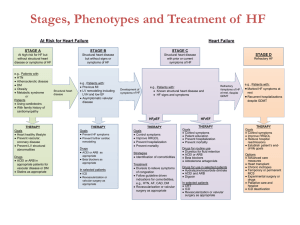
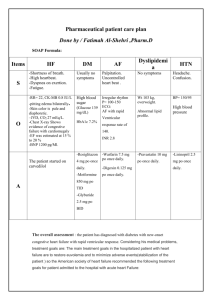
Heart Failure Progressive Disease: any structural or functional impairment of: o Ventricular filling (diastolic dysfunction) – small pool o Ejection of blood (systolic dysfunction) – no strength to pump out HF= Chronic HF (CHF), but NOT: cardiomyopathy or left ventricular dysfunction o Black males – highest risk HF o Mortality rate: 50% w/in 5 years of diagnosis Normal Heart Anatomy o Left: Left atriumMitral valveLeft VentricleAortic valveBody Back into heart via lungs to push out to the body. Systolic HF: weak LV, blood pools and wont pump out. Diastolic HF: thick stiff muscle, wont fill up. o Right: Right atriumTricuspidRight VentriclePulmonary valveLungs Preparing blood to leave heart. Risk Factors Modifiable: Smoking, Diet/Obesity, Immobility, Alcohol Common Causes Dilated Cardiomyopathies (ineffective pumping) Ventricular dilation and depressed myocardial contractility HTN or valvular diseases Drugs Compensatory Mechanisms (impaired LV) Non-Modifiable: Age, Heredity, Race (AA male), Comorbidities -#1 HTN, DM, Arrhythmia, Virus, Cardiomyopathies, Myocarditis, IHD, Vascular/valvular disease, CKD, Dyslipidemia, Cardiotoxic drugs, Systemic toxins, Metabolic Syndrome -Others: Thyroid disease, Growth Hormone deficiency, Iron overload, Stress, Tachycardia. CAD & Ischemic Damage Non-Ischemic -1/3 of patients. -2/3 of pts. -Intrinsic myocardial disease: valvular disease, myocarditis, -LV/systolic dysfunction autoimmune. of heart. -Excess work load: resistance to ejection (HTN, aortic -Ischemic damage has stenosis). affected pumping. SV (valvular disease) (aortic, mitral, tricuspid insuff.) -CHD/MI present. demand (thyrotoxicosis, anemia, pregnancy etc.) -Iatrogenic: drugs and radiation Na/H2O retention (NSAIDS, steroids) contractility (BB, CCB) BV (IV fluids, albumin) Activate RAAS: Na & fluid retention, SNS (A1-A2 conversion) SNS: (+) feedback, RAAS stimulated, heart tries pumping fast Remodeling and other cellular changes: damage electrical conduction (arrhythmia), function of myocytes & amount of vasodilators (b/c +feedback), enlarged ventricles (increase O2 demand & decrease O2 supply) Cardinal Manifestations: dyspnea, fatigue, fluid retention Left Heart Dysfunction Right Heart Dysfunction Symptoms: DOE or @rest, fatigue, orthopnea, Symptoms: swelling, anorexia, abdominal PND, cough, mental, cool extremities. (Lungs, bloating & pain. Caused by Left Dysf. (worse, fluid built up) body SE’s) Signs: cardiomegaly, tachycardia, HTN, pulm Signs: cardiomegaly, edema, JVD, HJR, edema & HTN, rales & crackles, RF, Cheynes ascites, hepatomegaly, splenomegaly, loss of Stokes (b/c fluid in lungs). appetite. SV: amount of blood ejected after contraction (Preload-Afterload=SV) EF: SV + Preload(EDV), fraction ejected each heartbeat, pump efficiency. ECHO: live view of heart motion, estimate EF (TTE’s & TEE’s) Chest X-ray: show shape of heart, pulmonary congestion. BNP: formed by cardiomyocytes with myocardial stretch. Over 400, can be falsely elevated. CBC &CMP: look for anemia/infection, renal/liver function & electrolytes (dilutional Na due to fluid overload). Presentation Diagnosis Based on symptoms, no true diagnostic test HFrEF Systolic HF: EF 40%. Ejection problem (no strength) Structural ventricular hypokinetic abnormalities Lifestyle Mod. Interventional Tx. HFpEF Diastolic HF: EF 50%. Filling problem (small pool) Diagnosis of exclusion Borderline HFpEF: EF 41-49% Exercise: symptoms, improve exercise capacity, slows progression (decondition) Na Restrict: target - 1.5-2g daily, fluid accumulation Fluid Restrict: target - 1.5-2L daily Record home BP, pulse & weight (sign of fluid). Operation: CAD (CABG, PCI/stent), Valve repair. Options for stages B & C. Implant Cardioverter Defibrillator (ICD): Stages B or C, deactivated in D. Cardiac Resynch Therapy (CRT): Stage C Mechanical Circulatory Support (MCS): VAD’s (help ventricles), Stage D, Class 2a recommendation, bridge to recovery, prolong survival. Cardiac Transplant: Stage D, Class 1 recommendation. Classifications ACCF/AHA Stages of HF NYHA Functional Classification (development & progression of disease) (CANNOT move back in stage!) A: high risk HF, no structural heart disease or symptoms. o (ACE/ARB) (can statins) B: Structural heart disease, no signs or symptoms. o Operation, ICD (ACE/ARB, Entresto) (can BB’s) C: Structural heart disease, prior or current symptoms. o Operation, ICD, CRT (all meds) D: Refractory HF, require specialized interventions. o Deactivate ICD, MCS, Transplant (iontropes) (exercise capacity & symptom status) (CAN move back in classification!) 1: no activity limits, ordinary activity – no symptoms. o A, B & C (same as 2) “exercise induced” 2: slight limit, comfy @rest, ordinary activity – symptoms. o (all pt’s try to be on BB’s) 3: marked limit, comfy @rest, ordinary – symptoms. o C 4: no physical activity, symptoms @ rest. o C&D Goals of Therapy Stage A Stage C Heart healthy lifestyle Prevent vascular/coronary disease & LV structural abnormalities. Stage B Prevent HF symptoms from starting & further cardiac remodeling (already started) Control symptoms Improve Quality of Life Prevent hospitalization & mortality Stage D Control symptoms, Improve Quality of Life Reduce hospitalizations, establish “end of life” goals Pharmacological Treatment: HFrEF Stage A ACEI/ARB: vascular disease, CKD, or diabetes Statins as appropriate Stage B ACEI or Entresto + BB + Ald Antag If tolerated, do all. Stage D (“all”): ACEI/ARB, BB, Entresto, Ald. Antag, BiDil, Digoxin, Ivabradine, Diuretics. 2nd Line/Select Pop. First Line Stage C ACEI/ARB or Entresto BB’s as appropriate Add immediately once symptoms are seen. ARB, BiDil, Digoxin or Ivabradine ARB only if ACEI not tolerated Chronic Inotropes Palliative care & hospice Transplant Last Line – Stage D Chronic Inotropes Pharmacological Treatment: HFpEF (no drugs to help mortality!) Diuretics: relieve symptoms of congestion Spironolactone & ARB: to decrease hosplitalizations Follow guidelines for comorbidities: HTN, AFib, CAD, DM etc. Pharmacologic Treatment 9 Major Classes: ACEI, BB, Sacubitril/Valsartan, Aldosterone Antag, ARB, Vasodilators, Sinus node Inhibitor (Ivabradine), Digoxin, Diuretics. Advanced HF Tx: Inotropes Monitoring (All agents) o Weight, BP, HR, Salt, Fluid, Electrolytes, Kidney, Liver, BNP, SE’s of meds. HFrEF: Benefits of HF Agents Mortality Benefits (1st line) ACEI/ARB’s Beta Blockers Aldosterone Antagonists Sacubitril/Valsartan Hydralazine/Isosorbide Dinitrate (black ppl) (dilators) Hospitalizations (2nd line) All w/ mortality benefits Digoxin, Ivabradine Hydralazine/Isosorbide Dinitrate (black ppl) (dilators) Symptom Relief All agents listed Diuretics (loop & thiazide) ACE Inhibitors (1st Line Agent) MOA Benefit Monitor Adverse Dosing Interactions Inhibit AT1AT2, competitively bind to ACE Prevent breakdown of bradykinin Deters SNS activation: vasoconstriction, PL & AL Relieve symptoms (slower than diuretics) Improve NYHA class and functional status. Hospitalizations, Mortality & Side Effects K, SCr and BUN w/ initiation or dose change Paradoxical effect on kidneys: can renal function Hypotension, Hyperkalemia, Dry cough, Angioedema CI: prev. anaphylaxis or angioedema w/ ACEI o Bilateral renal artery stenosis (unilateral ok) Start low and as tolerated, dose w/ renal disease. Hypotension problem w/ hyponatremia Benefit may not appear for several weeks No tolerance w/ chronic use Diuretics may act synergistically with ACEI’s K supplements or agents that K NSAIDS Hypotension w/ other anti-hypertensive agents. Drugs (target dose for survival benefit) Captopril: 50mg TID Quinapril: 20mg BID Enalapril: 10-20mg BID Fosinapril: 40mg daily Lisinopril: 20-40mg daily Ramipril: 10mg daily Trandolapril: 4mg daily ARB’s (1st Line Agent – somewhat) MOA Benefits Adverse competitively bind and block AT2-R prevent vasoconstriction and aldosterone activation pt intolerant to ACEI, just as effective less evidence to support as 1st line agent NOT a drug effect: Candesartan, Valsartan & Losartan (studied) pumping, mortality. Hospitalizations, Mortality & Side Effects. similar to ACEI profile equal: Hypotension, renal function & Hyperkalemia lower rate: Angioedema Drugs (target dose for survival benefit) Valsartan: 160mg BID Losartan: 50-150mg daily Candesartan: 32mg daily ACEI/ARBs: K (w/ Ald. Antagonists even higher), avoid NSAIDs, hypotension o Can worsen renal function Beta Blockers (1st Line Agent) MOA Benefit Use Dosing Adverse Antag B adrenergic-R’s in heart & vasculature (restore variability, prevent arrhythmia & remodeling) Inhibit NE release & Renin secretion Carvedilol: block beta1, beta2 & alpha-adrenergic receptors Bisoprolol & Metoprolol: block beta1 adrenergic receptors Symptom relief, exercise tolerance & improve NYHA class. More effective at maintaining ventricular response especially during exercise (help HF patients with A Fib) Hospitalizations, Mortality & Side Effects Consider for NYHA class 1 patients Used in ALL pt’s in class 2 and 3 (unless specified) If tolerated: class 4 patients Shown to improve HF: Bisoprolol, Metoprolol Succinate & Carvedilol. Start low, as tolerated every 2 weeks. Taper off to avoid rebound Not a rescue medication: benefit may take weeks Added only once pt is hemodynamically stable Initiate only if patient is euvolemic Fluid retention & worsening HF @ 1st Watch for weight increase and worsening signs of HF Fatigue (try reducing dose or switching agent) Bradycardia & Heart Block (decrease dose, look for drug interactions) Hypotension (Carvedilol) (dizzy, lightheaded, blurry) Drugs (target dose for survival benefit) (1) Metoprolol Succ: 200mg daily ( & ) Carvedilol: 50mg BID ( & ) Carvedilol CR: 80mg daily (1) Bisoprolol: 10mg daily Aldosterone Antagonists (1st Line Agent) MOA Benefit Dosing Adverse Competitively bind aldosterone-R’s in distal tubule & collecting duct of the nephron Na & water reabsorption, as well as cardiac & vascular fibrosis Symptom relief Hospitalizations, Mortality & Side Effects start w/ 25mg daily, 50mg if symptoms persist 12.5mg if hyperkalemia develops Eplerenone: $, reserved for gynecomastia patients Hyperkalemia: risk w/ ACEI or K supplements & renal impaired Gynecomastia: anti-androgen properties of Spironolactone ACEI/ARBs: K (w/ Ald. Antagonists even higher) Drugs (target dose for survival benefit) Eplerenone: 50mg daily Spironolactone: 25mg daily/BID Hydralazine/Isosorbide Dinitrate (BiDil) (1st Line Agent – Vasodilator Class) MOA Benefit Dosing Adverse Unknown, synergistic effects Isosorbide dilate by releasing nitric oxide. Hydralazine mitigate tolerance to nitrates. If ACEI/ARB not tolerated. Possibly more effective than ACEI in black patients. Hospitalizations, Mortality & Side Effects. Most decrease in mortality of agents so far. Effects only with short acting dinitrate (not mononitrate) 1-2 Tablets TID 1 Tablet: 37.5mg hydralazine/20mg isosorbide dinitrate BiDil Resolved by d/c medication (headeache, dizzy, hypotension) CI: phosphodiesterase-5-inhibitors (sildenafil, vardenafil etc) could result in severe hypotension. Sacubitril/Valsartan (Entresto) (New 1st Line Agent) MOA Benefit Dosing Adverse Sacubitril: neprilysin inhibitor (neutral endopeptidase: NEP) Valsartan: ARB Together NP’s & Inhibit RAAS (ARNI) Neprilysin also clears: Sub P, Bradykinin, AT1 & AT2 Add ARB to inactivate RAAS b/c of clearing AT2 & to angioedema. Hospitalizations, Mortality & Side Effects For CHF (NYHA classes 2-4) & EF: In place of ACEI/ARB 24/26mg, 49/51mg, 97/103mg (target dose) If previously on ACEI/ARB start at 49/51mg If naïve, start on 24/26mg BID Do not administer with an ACEI or within 36hrs of last dose of ACEI. CI: history of angioedema. Healthy Heart ANP/BNP: vasodilate, excrete water and Na, fibrosis & cardiac hypertrophy Heart Failure BNP & neprilysin: NP’s, vasoconstrict, water and Na retention, fibrosis & cardiac hypertrophy Ivabradine (2 Line Agent) nd MOA Benefit Dosing Sinus node inhibitor Selectively inhibit hyperpolarization of Na channel - SA & I current: regulates HR. Hospitalizations & Side Effects For stable, symptomatic CHF with left ventricular EF 35% who are in sinus rhythm with resting HR 70. Used if on max tolerated BB’s or have CI for BB use. 5mg, 7.5mg (target dose) Start on 5mg BID. High risk for bradycardia: start on 2.5mg BID Digoxin (2nd Line Agent) MOA Benefit Dosage Adverse Monitor Interactions Positive inotrope (mild), enhanced parasympathetic tone (calm down SNS) Normal plasma ½ life: 36hrs with normal renal function. Excreted primarily renally. If anuric: plasma ½ life – 5days! Remain symptomatic even on ACEI/ARB, BB & diuretics For HF patients with A Fib. (BB’s better w/ ventricular response during exercise) Hospitalization & Side Effects Therapeutic Range: 0.5-2.0ng/mL Goal in HF: 0.5-0.9ng/mL. Goal in A Fib: 1-2ng/mL Monotherapy NOT appropriate! Do NOT abruptly d/c. 0.125-0.25mg daily. 0.125 in renal impaired/elderly. No loading dose needed. Narrow TPW. Many Side Effects! Elderly more sensitive, data showing negative effects in women ( mortality). CI: Heart Block Obtain serum digoxin levels, changing renal function, interacting drugs added to regimen. Assessment of HF symptoms Assessment of Digitalis toxicity: GI most common, neurological/neuromuscular, cardiac symptoms. o Hypokalemia, hypomagnesemia, hypercalcemia. Diuretics: can induce K and Mg loss. Spironolactone: changes elimination, digoxin concentrations. Diuretics (3 Line Agents) rd MOA Benefit Dosage Adverse Inhibit reabsorption of electrolytes in the nephron. o In loop Henle (loops) o In distal tubule (thiazides) Remove peripheral edema, pulm congestion cardiac performance by circulatory overload Most rapid symptoms of all agents. (hrs/days) Won’t delay progression. All patients with Stage C. Monotherapy NOT appropriate! Loops Thiazides Hyponatremia, Hypokalemia, Hypomagnesia, uric acid, renal dysfunction. HYPOcalcemia Hyponatremia, Hypokalemia, Hypomagnesia, uric acid, renal dysfunction. HYPERcalcemia Drugs Thiazides: chlorthalidone & HCTZ less effective in advanced disease. Loops Ferosemide, Torsemide, Bumetanide 40: 20-10: 1 Potent & effective in all stages HF Linear dose/response relationship Remain effective in renal failure Thiazide-Like Metolazone (PO) Chlorothiazide (IV) Useful combo with Loops. Inotropes (Advanced HF Treatment Only) MOA Benefit Ventricular Filling Stroke Volume Palliation in end stage HF Used as a bridge to cardiac transplant Can Mortality!! Mirinone Dopamine Phosphodiesterase-3 Inhibitor Strengthen HB & relax BV’s Doesn’t O2 demand (prefer: ischemia) Better for severe HF w/ BB’s Adverse: tachyarrhythmia, hypotension & LFT’s Dose: 0.125-0.75mcg/kg/min IV heart function, may BP, help edema Help w/ renal perfusion & ionotrophy Tolerance may develop Adverse: irregular heart rhythm, tachyphylaxis, headache, nausea, tissue necrosis. Dose: 5-15mcg/kg/min IV o Low: 2 “renal dose” o Interm: 2-10 “beta dose” o High: 10 “alpha dose” Dobutamine heart function, may BP Tolerance faster than dopamine Adverse: irregular heart rhythm (less), tachyphylaxis, nausea, fever, hypersensitivity CI: sulfite allergy Dose: 2.5-20 mcg/kg/min IV Acute Decompensated Heart Failure Sudden worsening (exacerbation) of HF symptoms leading to hospitalization #1 cause hospitalizations in patients 65. Patho Causes (either med or disease related) “always want to control HTN” Characteristics Cardiac output and/or cardiogenic pulmonary edema Activation of sympathetic nervous system and RAAS Compensatory mechanisms Common: Nonadherence to chronic meds & Nonadherence to Na or fluid restrictions. Uncontrolled BP, Acute MI, AFib/arrhythmias, drugs/alcohol/pulmonary embolus, infections (-) Inotropic drugs: verapamil, nifedipine, diltiazem, BB’s Drugs Na retention: steroids, thiazolidinediones, NSAIDs Endocrine disorders: DM, hyperthyroidism, hypothyroidism Other acute vascular disorders: valvular disease, endocarditis, myopericarditis, aortic dissection Cardinal Symptoms: SOB, Edema, Fatigue Elderly or near, equally male/female Equally HFrEF/HFpEF: pEF (more female, uncontrolled HTN, older, but less CAD) History of HTN + one of the following o CKD, hyponatremia, hematological abnormalities, COPD Congestion at Rest Low Perfusion at Rest Orthopnea ( 2 pillows), 12 JVP (can see it) Narrow Pulse Pressure Pulmonary rates, S3 gallop, Edema Tachycardia with pulsus alternans Pulm Capillary Wedge Pressure (PCWP): fluid Cool extremities, Hypotension status, 30 mmHg Cardiac Index (CI): degree of perfusion, proportional pulse pressure. 2.2 (cold) Improve symptoms, restore normal oxygenation, optimize vol status, identify etiology Address precipitating factors, optimize chronic oral therapy (discharge), minimize adverse effects Identify patients who benefit from revascularization or a device Identify risk of thromboembolism and need for anticoagulant therapy Educate patients, consider initiating a disease management program BB’s initiated AFTER volume status is optimal o PO diuretics, vasodilators & inotropic agents should be d/c as well. ACEI, ARB, Ald Antag, Entresto: held or reduced in pt with significant renal decline Make sure standard therapy agents are restarted before discharge o Follow up 7-14 days & telephone follow up after 3 days Diagnosis Goals of Therapy Chronic Therapy Recommendations Symptomatic Classifications Forrester Hemodynamic Classifications Congestion at Rest Pulm Capillary Wedge Pressure (PCWP) -fluid status (mid 18) Warm & Dry - 1 Low Perfusion at Rest Cardiac Index (CI) (mid 2.2) No additional therapy Not a lot of edema or SE’s IV Vasodilators (or Inotropes) (+ IV fluids if too dry) Not perfusing to organs well Warm & Wet - 2 IV Diuretics (+/- Vasodilators) Tons of fluid IV Diuretics + IV Vasodilators (or Inotropes) Not perfusing and accumulating fluid Cold & Dry - 3 Cold & Wet - 4 Diuretic Therapy Mainstay Therapy Dosage IV Loop’s: no difference b/w cont. inf. vs IV bolus (possibly cause hypokalemia) 2-2.5 times oral dose given IV intermittently Double the dose if no response in 1st 6-8 hours Switch to IV infusion if no response o Monitor: urine output/renal function, electrolytes, symptoms, vitals, weight closely o Furosemide (Lasix) 20mg IV = Furosemide 40mg PO (1 IV: 2 PO) o Bumetanide & Torsemide (1 IV: 2 PO) Adjuncts to Diuretic Therapy If Symptoms Persist 1. Trial higher doses of IV loop if pt can tolerate 2. Add thiazide-like or thiazide diuretic a. Metolazone-PO (common before loop), Chlorothiazide-IV (allergic to sulfa etc) or HCTZ 3. Add Ald. Antag.: Spironolactone or Eplerenone (watch for hyperkalemia) 4. Add Vasopressin Antagonists: Conivalptan or Tolvaptan (not given often) 5. Low-Dose (“renal dose”) Dopamine IV Infusion 6. Ultrafiltration if diuretics fail (dialysis) Vasopressin Antagonists May consider short term: vol overloaded pts w/ persistent severe hyponatremia & at risk for symptoms despite water restriction and optimal management. Improves serum Na concentrations in hypervolemic, hyponatremia states, but NO benefits long term. Vasodilator Therapy Uses Absence of symptomatic hypotension. Only as adjuvant to Loop’s. Benefit: symptomatic relief ONLY! Caution w/ HFpEF bc more volume sensitive IV Nitroglycerin (go to) IV Na Nitroprusside (last line) MOA: venodilate, preload & pulm congestion Best for HF & HTN, coronary ischemia, or significant mitral regurgitation Adverse: tachyphylaxis 24hr/resistance Dose: 5-10mcg/min IV infusion Can increment 5-10mcg Q 3-5min Usual Range: 10-200mcg/min Max Dose: 400mcg/min MOA: veno & arteriodilator, preload & afterload Awaiting transplant (limited use) Adverse: hypotension & cyanide toxicity (especially in renal failure) Na thiosulfate – antidote Dose: 5-10mcg/min IV infusion Can increment 5-10mcg Q 5min Usual Range: 5-300mcg/min Dose 400 not recommended IV Nesiritide (human BNP) MOA: LV filling pressure, variable CO, urinary output & Na excretion. Adverse: hypotension (bc long t ½) Dose: 2mcg/kg IV bolus (optional) followed by 0.01mcg/kg/min