cardio cases
advertisement
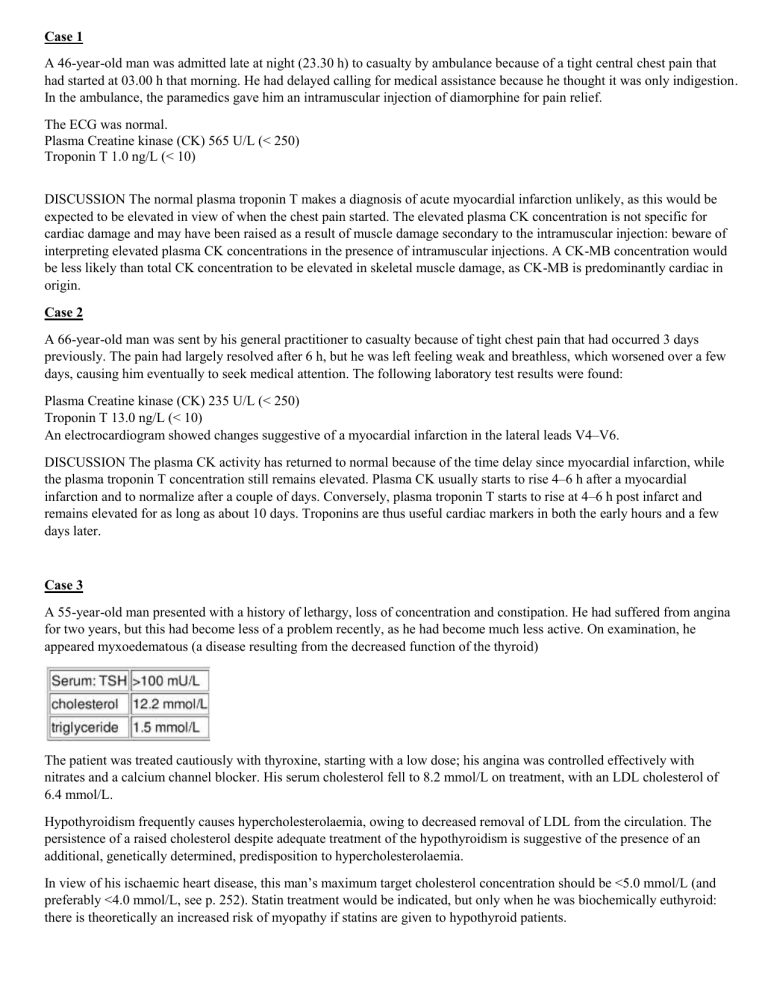
Case 1 A 46-year-old man was admitted late at night (23.30 h) to casualty by ambulance because of a tight central chest pain that had started at 03.00 h that morning. He had delayed calling for medical assistance because he thought it was only indigestion. In the ambulance, the paramedics gave him an intramuscular injection of diamorphine for pain relief. The ECG was normal. Plasma Creatine kinase (CK) 565 U/L (< 250) Troponin T 1.0 ng/L (< 10) DISCUSSION The normal plasma troponin T makes a diagnosis of acute myocardial infarction unlikely, as this would be expected to be elevated in view of when the chest pain started. The elevated plasma CK concentration is not specific for cardiac damage and may have been raised as a result of muscle damage secondary to the intramuscular injection: beware of interpreting elevated plasma CK concentrations in the presence of intramuscular injections. A CK-MB concentration would be less likely than total CK concentration to be elevated in skeletal muscle damage, as CK-MB is predominantly cardiac in origin. Case 2 A 66-year-old man was sent by his general practitioner to casualty because of tight chest pain that had occurred 3 days previously. The pain had largely resolved after 6 h, but he was left feeling weak and breathless, which worsened over a few days, causing him eventually to seek medical attention. The following laboratory test results were found: Plasma Creatine kinase (CK) 235 U/L (< 250) Troponin T 13.0 ng/L (< 10) An electrocardiogram showed changes suggestive of a myocardial infarction in the lateral leads V4–V6. DISCUSSION The plasma CK activity has returned to normal because of the time delay since myocardial infarction, while the plasma troponin T concentration still remains elevated. Plasma CK usually starts to rise 4–6 h after a myocardial infarction and to normalize after a couple of days. Conversely, plasma troponin T starts to rise at 4–6 h post infarct and remains elevated for as long as about 10 days. Troponins are thus useful cardiac markers in both the early hours and a few days later. Case 3 A 55-year-old man presented with a history of lethargy, loss of concentration and constipation. He had suffered from angina for two years, but this had become less of a problem recently, as he had become much less active. On examination, he appeared myxoedematous (a disease resulting from the decreased function of the thyroid) The patient was treated cautiously with thyroxine, starting with a low dose; his angina was controlled effectively with nitrates and a calcium channel blocker. His serum cholesterol fell to 8.2 mmol/L on treatment, with an LDL cholesterol of 6.4 mmol/L. Hypothyroidism frequently causes hypercholesterolaemia, owing to decreased removal of LDL from the circulation. The persistence of a raised cholesterol despite adequate treatment of the hypothyroidism is suggestive of the presence of an additional, genetically determined, predisposition to hypercholesterolaemia. In view of his ischaemic heart disease, this man’s maximum target cholesterol concentration should be <5.0 mmol/L (and preferably <4.0 mmol/L, see p. 252). Statin treatment would be indicated, but only when he was biochemically euthyroid: there is theoretically an increased risk of myopathy if statins are given to hypothyroid patients. Note that hypothyroidism should be treated under close medical supervision in patients with ischaemic heart disease. The increase in metabolic rate increases the body’s oxygen requirements and can exacerbate angina or precipitate myocardial infarction Case 4:A 66-year-old man had experienced central chest pain on exertion for some months, but in the afternoon of the day prior to admission he had had a particularly severe episode of the pain, which came on without any exertion and lasted for about an hour. On admission there were no abnormalities on examination and the ECG was normal. The troponin was clearly detectable. Comment on these results. Has he suffered a myocardial infarction? Comments: He has an elevated troponin plus a typical history. This is sufficient to diagnose a myocardial infarction by the most recent definition, even in the absence of ECG changes. Case 5 A well-trained marathon runner collapsed as he was approaching the fi nishing line. An ECG was normal, but CK was elevated at 9500 U/L (reference range 30–200 U/L), and the CK-MB was 14% of the total CK (normally <6%). Troponin was undetectable. Comment on these results. Comments: The total CK is substantially elevated, and CK-MB >6% can usually be taken to mean that it is of myocardial origin. However, the normal ECG and troponin are both reassuring. In trained endurance athletes, the proportion of CK-MB in muscle increases from the normal low levels and may be as high as 10–15%. An elevated CK-MB in such individuals can no longer be taken to imply a cardiac origin for the raised CK. Extreme exercise, especially in unfit individuals, causes an elevated CK, potentially to very high levels. Case 6 A 33-year-old man was referred to the lipid clinic with a cholesterol of 10.2 mmol/L. He had a vague memory of having his cholesterol checked at a medical examination at work in his early twenties, and thought it had been normal at that time. He had been dieting for the last few months and had succeeded in losing ∼3 kg, but his cholesterol had not changed. Over the preceding 2 years he had felt tired, and stressed by his work. His GP felt that he was depressed, and had been treating him with anti-depressants with little benefi t. He had stopped playing football, and his muscles ached on exertion. He had put on 20 kg over this period Comments: He has an extremely high [cholesterol] which has not improved with diet, and if his recollections were accurate had previously had a normal [cholesterol]. This raises the question of a secondary hypercholesterolaemia. He has certainly put on weight, which may increase lipids, but not usually to this extent. His symptoms of weight gain, tiredness and depression raised the possibility of hypothyroidism, and this was confi rmed by his profoundly hypothyroid thyroid function tests. Hypothyroidism can also cause a myopathy, with aching muscles and very high CK, and a dilutional hyponatraemia. He thus had a full range of the biochemical abnormalities that may be seen in hypothyroidism! Treatment with thyroxine resulted in a dramatic improvement in all his symptoms apart from the muscle aching, which still persisted 6 months later. [Cholesterol] came down to a satisfactory 4.6 mmol/L without the need for any lipid-lowering medication. CK and sodium returned to normal.