Langerhans microabcesses PDF
advertisement
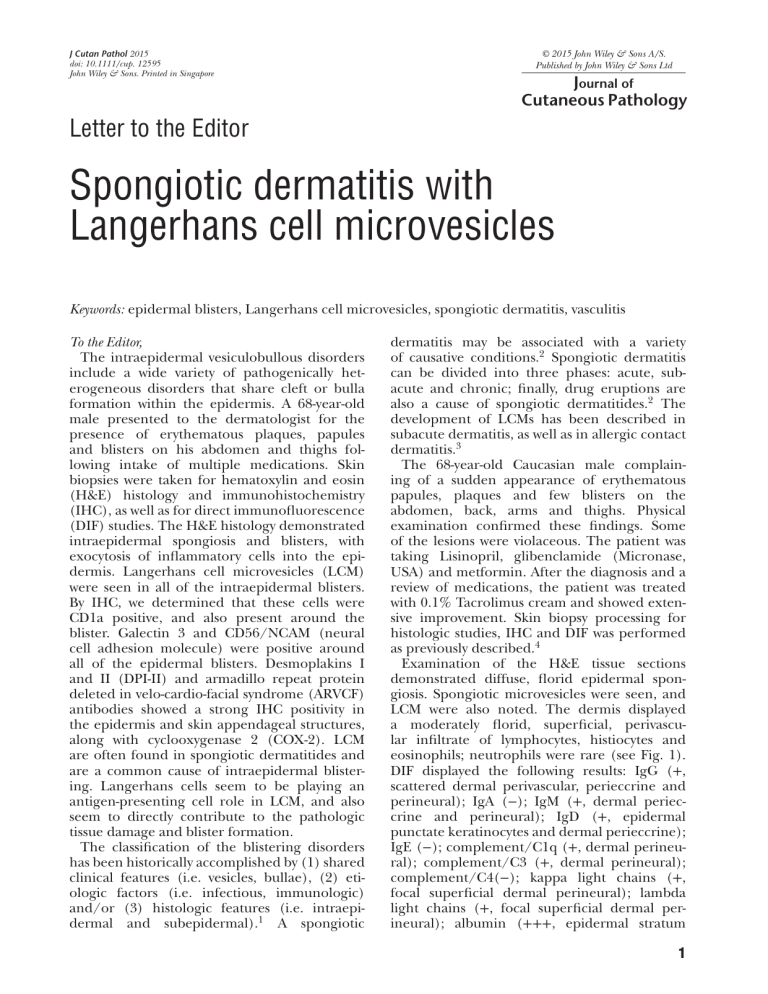
J Cutan Pathol 2015 doi: 10.1111/cup. 12595 John Wiley & Sons. Printed in Singapore © 2015 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd Journal of Cutaneous Pathology Letter to the Editor Spongiotic dermatitis with Langerhans cell microvesicles Keywords: epidermal blisters, Langerhans cell microvesicles, spongiotic dermatitis, vasculitis To the Editor, The intraepidermal vesiculobullous disorders include a wide variety of pathogenically heterogeneous disorders that share cleft or bulla formation within the epidermis. A 68-year-old male presented to the dermatologist for the presence of erythematous plaques, papules and blisters on his abdomen and thighs following intake of multiple medications. Skin biopsies were taken for hematoxylin and eosin (H&E) histology and immunohistochemistry (IHC), as well as for direct immunofluorescence (DIF) studies. The H&E histology demonstrated intraepidermal spongiosis and blisters, with exocytosis of inflammatory cells into the epidermis. Langerhans cell microvesicles (LCM) were seen in all of the intraepidermal blisters. By IHC, we determined that these cells were CD1a positive, and also present around the blister. Galectin 3 and CD56/NCAM (neural cell adhesion molecule) were positive around all of the epidermal blisters. Desmoplakins I and II (DPI-II) and armadillo repeat protein deleted in velo-cardio-facial syndrome (ARVCF) antibodies showed a strong IHC positivity in the epidermis and skin appendageal structures, along with cyclooxygenase 2 (COX-2). LCM are often found in spongiotic dermatitides and are a common cause of intraepidermal blistering. Langerhans cells seem to be playing an antigen-presenting cell role in LCM, and also seem to directly contribute to the pathologic tissue damage and blister formation. The classification of the blistering disorders has been historically accomplished by (1) shared clinical features (i.e. vesicles, bullae), (2) etiologic factors (i.e. infectious, immunologic) and/or (3) histologic features (i.e. intraepidermal and subepidermal).1 A spongiotic dermatitis may be associated with a variety of causative conditions.2 Spongiotic dermatitis can be divided into three phases: acute, subacute and chronic; finally, drug eruptions are also a cause of spongiotic dermatitides.2 The development of LCMs has been described in subacute dermatitis, as well as in allergic contact dermatitis.3 The 68-year-old Caucasian male complaining of a sudden appearance of erythematous papules, plaques and few blisters on the abdomen, back, arms and thighs. Physical examination confirmed these findings. Some of the lesions were violaceous. The patient was taking Lisinopril, glibenclamide (Micronase, USA) and metformin. After the diagnosis and a review of medications, the patient was treated with 0.1% Tacrolimus cream and showed extensive improvement. Skin biopsy processing for histologic studies, IHC and DIF was performed as previously described.4 Examination of the H&E tissue sections demonstrated diffuse, florid epidermal spongiosis. Spongiotic microvesicles were seen, and LCM were also noted. The dermis displayed a moderately florid, superficial, perivascular infiltrate of lymphocytes, histiocytes and eosinophils; neutrophils were rare (see Fig. 1). DIF displayed the following results: IgG (+, scattered dermal perivascular, perieccrine and perineural); IgA (−); IgM (+, dermal perieccrine and perineural); IgD (+, epidermal punctate keratinocytes and dermal perieccrine); IgE (−); complement/C1q (+, dermal perineural); complement/C3 (+, dermal perineural); complement/C4(−); kappa light chains (+, focal superficial dermal perineural); lambda light chains (+, focal superficial dermal perineural); albumin (+++, epidermal stratum 1 Letter to the Editor corneum) and fibrinogen (+++, dermal perivascular and perieccrine). Of interest, we noted the excretion of a material staining positive with fluorescein Isothiocyanate (FITC)-conjugated IgG through the sweat ducts in the epidermal corneal layer (see Figs. 1–3). By DIF, DP I-II and ARVCF were expressed in the epidermis, hair follicles, eccrine sweat glands and on dermal blood vessels and some nerves. IHC results showed mast cell tryptase positive staining around dermal eccrine sweat glands and ducts. Factor XIIIa was positive on dermal dendrocytes, close to dermal neurovascular structures. CD3 was positive under the basement membrane zone (BMZ). CD8 was positive around upper dermal blood vessels, and also around eccrine sweat gland ducts. Bcl-2 was positive at the BMZ, as well as in the upper dermal inflammatory infiltrate and around dermal eccrine sweat glands. COX-2 was positive around dermal eccrine sweat glands. HLA-DP, DQ, DR antigen stained positive on several cells in the epidermis, as well as around blood vessels supplying hair follicular units, the upper dermal vascular plexus and around dermal eccrine gland blood vessels. Several cells of dendritic cell shape in the epidermis were also positive for this marker. CD45 stained positive around some blood vessels in the subcutaneous adipose tissue, around dermal blood vessels and eccrine sweat glands and on several individual cells within the epidermis. CD4 and CD20 were negative. Ki-67 was positive around several dermal blood vessels, around some parts of the dermal eccrine glands, in the hair follicles and at the epidermal BMZ and stratum spinosum of the epidermis. Factor XIIIa was positive in cells around dermal blood vessels. The most dramatically positive staining was seen with CD1a, in selected cells within the epidermis, inside epidermal blisters, at the epidermal BMZ, around upper dermal blood vessels and within all hair follicular units (Fig. 1). Positive staining with Galectin 3, CD56/NCAM and matrix metallopeptidase 9 (MMP9) was seen inside the epidermal blisters and on adjacent epidermis. Tissue inhibitor of metalloproteinases 1 was positive in the hair follicles. The most common cause of spongiotic dermatitis is an eczematous dermatitis; this process often demonstrates the presence of serum scale crust, sometimes psoriasiform epidermal hyperplasia, lymphocytic exocytosis and intraepidermal vesiculation with formation of LCM.1 – 4 We found other dermal dendritic cells within the immunologic response (dermal dendrocytes), highlighted by Factor XIIIa. The dermal 2 dendrocytes were primarily noted surrounding perivascular inflammatory cells in the upper dermal vascular plexus. These findings are indicative of an active antigen processing/presenting process. We also noted that the CD1a-positive cells seemed to be focally ‘damaging the tissue’; indeed, recent studies have shown via zymographic studies the presence of gelatinase in CD1a-positive cells.5 The same authors also showed that tissue inhibitor of metalloproteinase 3 was significantly increased in mature dendritic cells (DCs), and this enzyme may participate in blister formation.5 Increasing evidence indicates an important role of T lymphocytes in drug-induced skin conditions and the drugs may be recognized by alpha/beta T cell receptors, and/or bound covalently to peptides, and also if the drug binds in a labile way to the presenting major histocompatibility complex (MHC)-peptide. In our case, we found colocalization of CD8 as well as HLA-DP, DQ, DR antigen within the dermal perivascular inflammation, but we did not find significant evidence of CD4 involvement as has been previously reported. Bcl-2 was very positive in the majority of the inflammatory cells around the epidermal blisters and the dermal perivascular inflammatory infiltrate. Bcl-2 has a potential role of Bcl-2 gene family members as regulators of cellular antioxidant status via immune modulation have been described. Our DIF and IHC data indicate a complex immune response which includes T lymphocytes, B lymphocytes, MHC molecules, antibodies, antigen-presenting cells and cell junctions. The CD1a-positive cells seem to migrate through the extracellular matrix to sample the local ‘antigenic’ environment; this process requires chemoattractants, cell adhesion and cell junction molecules (in our case, likely including DPI-II and ARVCF). The overall process results in edema and vasodilation; the process also requires proteinases to open the tissue. We noted that fibrinogen, complement/C3c, albumin and to a lesser extent IgG and other immunoglobulins congregated around blood vessels in the upper dermal vascular plexus, as well as around dermal nerves, eccrine glands and hair follicular units. In addition, other inflammatory markers including mast cell tryptase, Bcl-2, COX-2 and Galectin 3 may be involved in increasing edema, and thus allowing increased migration of cytokines and pertinent cells. Our findings suggest that several skin appendageal structures may also play a role in the eczematous process. Letter to the Editor Fig. 1. A) Langerhans cell microvesicles and other markers. A) Hematoxylin and eosin (H&E) (×200) displays a spongiotic epidermis with Langerhans cell microvesicles (LCM) present (black arrows). A lymphohistiocytic infiltrate is also seen around upper dermal blood vessels. B) Immunohistochemistry (IHC) with CD1a shows positive staining for Langerhans cells within a microabscess (brown staining; red arrow). C) IHC staining with metallopeptidase inhibitor 1 (TIMP1), showing positivity on cells within an epidermal blister (red staining; black arrow). D) Direct immunofluorescence (DIF), showing armadillo repeat protein deleted in velo-cardio-facial syndrome (ARVCF) staining a large dermal blood vessel (orange staining; white arrow), and fibrinogen deposits around the blood vessel (green staining; white arrow). E) DIF, showing positive stain with ARVCF to a hair follicle (red staining; white arrow); blood vessels in the vicinity are surrounded by FITC-conjugated fibrinogen deposits (green staining). Of importance, LCs and spongiosis were found in the hair follicles. F) IHC-positive staining with galectin 3 inside an epidermal blister (red staining; black arrow). 3 Letter to the Editor Fig. 2. Direct immunofluorescence (DIF) and immunohistochemistry (IHC) stains. A–D) DIF. A and B) DIF using fluorescein Isothiocyanate (FITC)-conjugated fibrinogen and Texas red-conjugated armadillo repeat protein deleted in velo-cardio-facial syndrome (ARVCF), showing positive staining in (A) on fibroblastoid cells in the intermediate dermis (yellow staining; white arrow) and the same cells in (B) (light red staining; white arrow). C) Positive staining with FITC-conjugated fibrinogen in the epidermal corneal layer (white staining; white arrow), and around upper dermal blood vessels (white staining; red arrow). Additional, adjacent, likely extruded material is noted in light green (which could represent additional fibrinogen, or a different material). D) Positive staining for ARVCF in the upper epidermis (red staining; white arrow). E and F) IHC. E) Positive staining for CD3 on inflammatory cells around upper dermal blood vessels (brown staining; red arrow). F) Positive staining with Bcl-2 at the epidermal basement membrane zone (BMZ) (brown staining; black arrow) and around upper dermal blood vessels (brown staining; red arrow). Moreover, ARVCF stained positive in the epidermis and in several skin appendices along with DP I-II. These molecules represent components of cell junctions, which may be altered in the 4 overall inflammatory process. We do not know the precise significance of these findings; we speculate that these components could be altered as a response to the initial immune Letter to the Editor Fig. 3. A) Direct immunofluorescence (DIF) and double immunohistochemistry (IHC) stains. IHC double staining, with anti-HLA-DP, DQ, DR antigen positive around dermal blood vessels, as well as on several cells in the epidermis (brown staining). In addition, positive staining for Factor XIIIa is focally noted in the dermis (red staining; red arrow). B) IHC, showing positive staining with Factor XIIIa in cells around dermal blood vessels (brown staining; red arrow) and in the same areas with CD68 (red staining; black arrow). C) DIF, showing positive staining with fluorescein Isothiocyanate (FITC)-conjugated anti-human IgG, extruding material from a sweat gland (green staining; white arrow). The nuclei of epidermal keratinocytes were counterstained with 4’,6-diamidino-2-phenylindole (DAPI) (blue). D) DIF, showing positivity around dermal blood vessels using FITC-conjugated fibrinogen (green staining; white arrow), and Texas red-conjugated armadillo repeat protein deleted in velo-cardio-facial syndrome (ARVCF) showing positivity in the vessels (red staining; white arrow). The nuclei of vascular endothelial cells were counterstained with DAPI (blue). E) Same antibodies as in (D), showing positive band-like staining at the epidermal basement membrane zone (BMZ) using FITC-conjugated fibrinogen (light green staining; white arrow). Please note additional punctate positivity in the epidermis with Texas red-conjugated ARVCF (yellow dot-like staining). F) IHC, showing positive staining with CD3 of cells below the epidermal BMZ (brown staining; red arrows), and around upper dermal vessels (brown staining; black arrow). 5 Letter to the Editor process, subsequently altering the respective cell junctions and contributing to surrounding edema. In summary, we noted the involvement and importance of many cells and molecules (including keratinocytes, mast cells, LCs, T lymphocytes and blood vessel endothelial cells) in a complex drug reaction response featuring epidermal spongiosis and LCM. We also suggest that given our data, positive staining markers for cell junction molecules such as DP I-II and ARVCF may indicate a direct role of these structures in edema formation, thus allowing the migration of other pertinent molecules and cells in the overall inflammatory process. Larger studies are needed to address these questions. the histology slides, contributed essential reagents and tools and reviewed the final version. Dr Abreu Velez performed the research, designed the study, correlated the IHC and DIF findings, analyzed the data and wrote the article. Many thanks to Jonathan S. Jones, HT (ASCP) at Georgia Dermatopathology Associates, who provided excellent technical assistance. This work was supported by Georgia Dermatopathology Associates, Atlanta, Georgia, USA. Ana Maria Abreu Velez, MD, PhD1 Michael S. Howard, MD1 Vickie M. Brown, MD2 1 Georgia Dermatopathology Associates, Atlanta, GA, USA 2 Department of Dermatology, Dermatology LLC, Milledgeville, GA, USA e-mail: abreuvelez@yahoo.com Acknowledgements Dr Brown evaluated the patient, took the biopsies, reviewed the draft and approved the final version. Dr Howard read References 1. Tran T, Muelenhoff M, Saeed S, Morgan MB. The miscellaneous blistering disorders. Semin Cutan Med Surg 2004; 23: 19. 2. Gupta K. Deciphering spongiotic dermatitides. Indian J Dermatol Venereol Leprol 2008; 74: 523. 3. Burkert KL, Huhn K, Menezes DW, Murphy GF. Langerhans cell microgranulomas 6 (pseudo-pautrier abscesses): morphologic diversity, diagnostic implications and pathogenetic mechanisms. J Cutan Pathol 2002; 29: 511. 4. Abreu Velez AM, Loebl AM, Howard MS. Spongiotic dermatitis with a mixed inflammatory infiltrate of lymphocytes, antigen presenting cells, immunoglobulins and complement. Our Dermatol Online 2011; 2: 52. 5. Osman M, Tortorella M, Londei M, Quaratino S. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases define the migratory characteristics of human monocyte-derived dendritic cells. Immunology 2002; 105: 73.