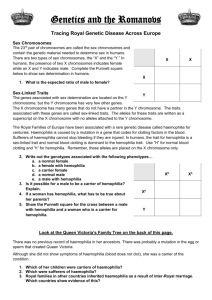
review - Centro Nazionale Sangue
advertisement
Blood Transfus 2014; 12 Suppl 3 Official journal of Blood Transfusion - Trimestrale spedizione in abbonamento postale 70% - Poste Italiane SpA LO/MI Società Italiana di Medicina Trasfusionale e Immunoematologia - SIMTI Associazione Italiana dei Centri Emofilia - AICE Hrvatsko društvo za hematologiju i transfuzijsku medicinu - HDHTM Sociedad Española de Transfusión Sanguínea y Terapia Celular - SETS Haemophilia Centre Accreditation Systems and Networks of Centres of Expertise for Rare Diseases in Europe and North America PROCEEDINGS "Haemophilia Centre certification systems across Europe" Rome (Italy), July 11th 2013 GUEST EDITORS: Gabriele Calizzani, Giuliano Grazzini, Pier Mannuccio Mannucci Blood Transfus 12, Supplement no. 3, April 2014 - ISSN 1723-2007 w w w. b l o o d t r a n s f u s i o n . i t Edizioni SIMTI Blood Transfus DOI 10.2450/2012.00?????? © SIMTI Servizi Srl 1 ISSN 1723-2007 Edizioni SIMTI © SIMTI Servizi Srl Official journal of: Società Italiana di Medicina Trasfusionale e Immunoematologia, SIMTI Associazione Italiana dei Centri Emofilia, AICE Hrvatsko društvo za hematologiju i transfuzijsku medicinu, HDHTM Sociedad Española de Transfusión Sanguinea y Terapia Celular, SETS Affiliated Societies of the journal: Associação Portuguesa de Imuno-Hemoterapia, APIH - Hellenic Society of Blood Transfusion, HSBT Editor-in-Chief Claudio Velati claudio.velati@simti.it Associate Editors Giovanni Di Minno Massimo Franchini Joan Ramon Grifols Irena Jukić Giancarlo M Liumbruno Pier Mannuccio Mannucci Daniele Prati Roberto Reverberi Luisa Romanò Giuseppe Tagariello Tomislav Vuk Alberto Zanella Affiliated Society Editors Maria Helena Gonçalves, APIH Alice Maniatis, HSBT Massimo Morfini, AICE Eduardo Muñiz-Diaz, SETS Ana Planinc Peraica, HDHTM Executive Director Stefano Antoncecchi Founder Lorenzo Lapponi Past Editors-in-Chief Lorenzo Lapponi, 1956-1964 Carlo Alberto Lang, 1965-1966 Roberto Venturelli, 1967-1968 Rosalino Sacchi, 1969-1978 Giorgio Reali, 1979-2006 Editorial Office Luisa Stea and Francesca Fermi Via Desiderio, 21 - 20131 Milano Website www.bloodtransfusion.it Printing Grafica Briantea Srl Via per Vimercate, 25/27 - 20040 Usmate (MI) International Editorial Board Jean-Pierre Allain, United Kingdom Giuseppe Aprili, Italy John Barbara, United Kingdom Lydia Blanco, Spain Ines Bojanić, Croatia Pietro Bonomo, Italy Dialina Brilhante, Portugal Maria Domenica Cappellini, Italy Jean-Pierre Cartron, France Giancarlo Castaman, Italy Francine Décary, Canada Josè António Duran, Portugal Willy A Flegel, United States of America Gilles Folléa, The Netherlands Zulmira Fonseca, Portugal Gabriella Girelli, Italy Giuliano Grazzini, Italy Ana Hećimović, Croatia Giancarlo Icardi, Italy Syria Laperche, France Luis Larrea, Spain Franco Locatelli, Italy Aurelio Maggio, Italy Michael Makris, United Kingdom Ivanka Mihaljević, Croatia Manuel Muñoz, Spain Mario Muon, Portugal Alessandro Nanni Costa, Italy Salvador Oyonarte, Spain Arturo Pereira, Spain Flora Peyvandi, Italy Paolo Rebulla, Italy Angiola Rocino, Italy Elena Santagostino, Italy Dorotea Šarlija, Croatia Erhard Seifried, Germany Paul FW Strengers, The Netherlands Cees L van der Poel, The Netherlands Jonathan H Waters, United States of America Alessandro Zanetti, Italy Tribunale di Milano Authorisation n° 380, 16th June 2003 This number is published in 700 copies. Printed in April 2014 The journal is indexed in PubMed-MEDLINE, Google Scholar, Embase and Scopus and PubMed Central Blood Transfusion articles are indexed in Journal of Citation Reports (JCR) for Impact Factor determination. Impact Factor 2012: 1,858. Associated with USPI Unione Stampa Periodica Italiana CONTENTS PREFACE s491 Claudio Velati EDITORIAL Haemophilia Centre Certification Systems: optional or optimal choice for healthcare systems? Gabriele Calizzani, Michael Makris, Pier Mannuccio Mannucci, Domenica Taruscio, Giuliano Grazzini, Fabrizio Oleari s492 HAEMOPHILIA CENTRES CERTIFICATION SYSTEMS ACROSS EUROPE AND NORTH AMERICA Haemophilia Centre certification system across Europe: the Belgian experience Cedric Hermans Quality of haemophilia care in the Netherlands: new standards for optimal care Frank W.G. Leebeek, Kathelijn Fischer A certification/accreditation model for Haemophilia Centres in Italy Pier Mannuccio Mannucci, Ivana Menichini The Italian institutional accreditation model for Haemophilia Centres Gabriele Calizzani, Fabio Candura, Ivana Menichini, Romano Arcieri, Giancarlo Castaman, Alessandro Lamanna, Maria R. Tamburrini, Antonio Fortino, Monica Lanzoni, Samantha Profili, Simonetta Pupella, Giancarlo M. Liumbruno, Giuliano Grazzini The European Haemophilia Network (EUHANET) Michael Makris, Gabriele Calizzani, Kathelijn Fischer, Alexander Gatt, Estelle Gilman, Robert Hollingsworth, Thierry Lambert, Riitta Lassila, Pier Mannuccio Mannucci, Flora Peyvandi, Jerzy Windyga The methodology for defining the European Standards for the certification of Haemophilia Centres in Europe Fabio Candura, Ivana Menichini, Gabriele Calizzani, Paul Giangrande, Pier Mannuccio Mannucci, Michael Makris The European standards of Haemophilia Centres Paul Giangrande, Gabriele Calizzani, Ivana Menichini, Fabio Candura, Pier Mannuccio Mannucci, Michael Makris The haemophilia certification system in Canada Davide Matino, Jerry Teitel, David Page, Arun Keepanasseril, Alfonso Iorio, Irwin Walker The National Haemophilia Program Standards, Evaluation and Oversight Systems in the United States of America Mark W. Skinner, J. Michael Soucie, Kathryn McLaughlin s497 s501 s505 s510 s515 s519 s525 s531 s542 THE MODEL FOR THE PREVENTION AND REDUCTION OF HEALTH AND SOCIAL IMPACTS OF INHERITED BLEEDING DISORDERS IN ITALY Institutional accreditation of Health Services in Italy: the long road to quality Antonio Fortino, Francesco Di Stanislao Current and evolving features in the clinical management of haemophilia Antonio Coppola, Massimo Morfini, Ernesto Cimino, Antonella Tufano, Anna M. Cerbone, Giovanni Di Minno Uncovered needs in the management of inherited bleeding disorders in Italy Romano Arcieri, Angelo C. Molinari, Stefania Farace, Giuseppe Mazza, Alberto Garnero, Gabriele Calizzani, Paola Giordano, Emily Oliovecchio, Lorenzo Mantovani, Lamberto Manzoli, Paul Giangrande The social burden and quality of life of patients with haemophilia in Italy Yllka Kodra, Marianna Cavazza, Arrigo Schieppati, Marta De Santis, Patrizio Armeni, Romano Arcieri, Gabriele Calizzani, Giovanni Fattore, Lamberto Manzoli, Lorenzo Mantovani, Domenica Taruscio Current status of Italian Registries on inherited bleeding disorders Hamisa Jane Hassan, Massimo Morfini, Domenica Taruscio, Francesca Abbonizio, Adele Giampaolo, Yllka Kodra, Emily Oliovecchio, Luciano Vittozzi Blood Transfus 2014; 12, Suppl 3 © SIMTI Servizi Srl s551 s554 s563 s567 s576 Definition of an organisational model for the prevention and reduction of health and social impacts of inherited bleeding disorders Gabriele Calizzani, Ivana Menichini, Fabio Candura, Monica Lanzoni, Samantha Profili, Maria Rita Tamburrini, Antonio Fortino, Stefania Vaglio, Giuseppe Marano, Giuseppina Facco, Emily Oliovecchio, Massimo Franchini, Antonio Coppola, Romano Arcieri, Cinzia Bon, Marco Saia, Sabina Nuti, Massimo Morfini, Giancarlo M. Liumbruno, Giovanni Di Minno, Giuliano Grazzini s582 REGIONAL, NATIONAL AND EUROPEAN ACTIONS IN THE FIELD OF RARE DISEASES The Italian National Centre for Rare Diseases: where research and public health translate into action Domenica Taruscio, Linda Agresta, Annalisa Amato, Giuseppe Bernardo, Luana Bernardo, Francesca Braguti, Pietro Carbone, Claudio Carta, Marina Ceccarini, Federica Censi, Simona Coppola, Patrizia Crialese, Marta De Santis, Stefano Diemoz, Carlo Donati, Sabina Gainotti, Gianluca Ferrari, Giovanna Floridia, Claudio Frank, Rosa Giuseppa Frazzica, Amalia E. Gentile, Orietta Granata, Yllka Kodra, Manuela Latrofa, Paola Laricchiuta, Armando Magrelli, Cristina Morciano, Agata Polizzi, Stefania Razeto, Marco Salvatore, Antonella Sanseverino, Daniele Savini, Paola Torreri, Fabrizio Tosto, Flavia Villani, Giorgio Vincenti, Luciano Vittozzi The Italian National Rare Diseases Registry Domenica Taruscio, Yllka Kodra, Gianluca Ferrari, Luciano Vittozzi and the National Rare Diseases Registry Collaborating Group The Italian National Plan on rare diseases Maria Elena Congiu Piedmont and Aosta Valley inter-regional network in the context of the Italian National Network for rare diseases Simone Baldovino, Elisa Menegatti, Vittorio Modena, Maria Maspoli, Flavia Avanzi, Dario Roccatello Centres of Expertise and European Reference Networks: key issues in the field of rare diseases. The EUCERD Recommendations Domenica Taruscio, Amalia E. Gentile, Teresinha Evangelista, Rosa G. Frazzica, Kate Bushby, Antoni Moliner Montserrat European Reference Networks for rare diseases: the vision of patients Terkel Andersen, Yann Le Cam, Ariane Weinman s591 ACKNOWLEDGEMEMETS S628 s606 s614 s617 s621 s626 Citation of the manuscripts published in this volume should be as follows Author(s). Title. Journal year; Volume (Suppl 4): page number. E.g.: Taruscio D, Kodra Y, Ferrari G et al. The Italian National Rare Diseases Registry. Blood Transfus 2014; 12 (Suppl 3): s606-13. PREFACE Preface Claudio Velati Editor-in-Chief of Blood Transfusion Haemophilia and other inherited bleeding disorders are life-threatening or chronically debilitating diseases whose prevalence is less than 5 over 10,000 persons in the European Union. Inherited bleeding disorders could be regarded as a case study in the field of health services research on rare disorders (RDs). In the light of the principles contained in the Cross-border Healthcare European Directive, the Italian National Blood Centre, as a part of the Italian National Institute of Health, has recently organised in Rome an international meeting on Haemophilia Centre Certification Systems across Europe. The meeting provided the opportunity for an official presentation of the European Guidelines for the certification of Haemophilia Centres. The meeting stimulated a fruitful discussion among scientific societies, international, national and regional institutions and experts on how to guarantee patients suffering from RDs to benefit of Network of Centres of Expertise and specific clinical pathways. This resulted in a number of manuscripts of remarkable scientific and organisational importance that I consider a valuable contribution to the scientific community as well as to healthcare systems in Europe and North America. Blood Transfusion has the pleasure to publish a Special Issue on this challenging event and on the several related contributions provided by other experts. I would like to give my hearty thanks to Gabriele Calizzani, Giuliano Grazzini and Pier Mannuccio Mannucci for having kindly accepted to be the Guest Editors. Blood Transfus 2014; 12 Suppl 3: s491 DOI 10.2450/2014.0100-14s © SIMTI Servizi Srl s491 EDITORIAL Haemophilia Centre Certification Systems: optional or optimal choice for healthcare systems? Gabriele Calizzani1, Michael Makris2, Pier Mannuccio Mannucci3, Domenica Taruscio4, Giuliano Grazzini1, Fabrizio Oleari5 1 National Blood Centre, National Institute of Health, Rome, Italy; 2Department of Cardiovascular Science, University of Sheffield, United Kingdom; 3Scientific Direction, IRCCS Ca' Granda Maggiore Policlinico Hospital Foundation, Milan, Italy; 4National Centre for Rare Diseases, National Institute of Health, Rome, Italy; 5National Institute of Health, Rome, Italy On July 11th 2013, an international meeting on Haemophilia Centre Certification Systems across Europe was held at the National Institute of Health in Rome1 with the goal of evaluating the possibility of transposing the principles contained in the Directive 2011/24/EU2, usually referred to as the Cross-border Healthcare Directive, into the reality of the current health systems of Member States (MSs). In fact, haemophilia and other inherited bleeding disorders (IBDs) meet the definition of rare diseases (RDs) provided by the European Commission as they are life-threatening or chronically debilitating diseases whose prevalence is less than 5 in 10,000 persons in the EU3. The Cross-border Healthcare Directive aims to ensure access to healthcare meeting defined quality and safety criteria, as well as patient mobility within the European Union (EU) MSs through mutual assistance and cooperation2. Moreover, it encourages the development of Centres of Expertise (CoE) and European Reference Networks in the field of RDs. The provision of an optimal level of healthcare to IBD patients requires the availability of multidisciplinary teams at specialised Haemophilia Centres (HCs)4,5. However, many of the health facilities calling themselves HCs worldwide vary in size, expertise and services provided. In order to assure equitable access and quality of care across their health systems, many Countries are in the process of developing and implementing standards and certification/accreditation systems for HCs. In Belgium, quality and efficiency of haemophilia care are negatively influenced by the lack of an official recognition, certification and an auditing programme and specific funding for HCs by the Belgian Ministry of Health6. In the Netherlands, since 2009, a formal process to draft new quality standards for HCs has been carried out and the text was formally approved by the Central body of Experts on quality standards in clinical care and the Ministry of Health in 20137. HCs have to apply for certification after an audit performed by a team composed of trained haemophilia clinicians, nurses and an officer from a specialised auditing company. The certificate is reviewed annually and audits are scheduled every three years. In Italy, since 2008, a professional accreditation programme proved to be successful in improving good clinical practice and developing benchmark activities among peers 8,9. In parallel, a complementary HCs institutional accreditation system was developed9,10. The defined requirements for HC healthcare delivery are considered necessary and appropriate in order to provide services such as basic levels of healthcare under the aegis of the National Health Service. These experiences, along with those from the United Kingdom11, provided the inspiration for and led to the development and production of the European Guidelines for the certification of HCs in the context of the European Haemophilia Network project (EUHANET, www.euhanet.org)12, in which the National Institute of Health, through the National Blood Centre, participated as collaborating partner. The European Guidelines have been discussed and reviewed by a large number of EU and non-EU stakeholders in different inclusive consultation processes that brought a highly qualified added value to the document13,14. All European HCs will be invited to apply for certification. The implementation of these European Guidelines and the application process on a voluntary basis to the European certification system should be considered as the first stage in order to shape the upcoming European Haemophilia Network, as a part of the wider Network of reference of CoE for RDs envisaged by the Cross-border Healthcare Directive (article 12)2. Similar developments have been taking place in Canada and the United States of America (USA). In Canada, an accountable system of haemophilia care has been developed based on a set of uniform and national standards. It is aimed at being needs-based, data-driven and supported by evidence of effectiveness. A full audit process, modelled on the Irish and UK experience, has been planned and carried out through interviews and patient questionnaires15. At present, there is no formal HCs accreditation system in the USA. Nevertheless, a number of programmes and systems are in place to promote and to assess the level of adherence to best practices, monitor patient outcomes and encourage continuous operational improvement16. Blood Transfus 2014; 12 Suppl 3: s492-4 DOI 10.2450/2014.0076-14s s492 © SIMTI Servizi Srl Haemophilia Centre Certification Systems In Europe, alongside the establishment of a CoE network, the organisation of healthcare pathways through the contribution of relevant experts and the exchange of professional expertise has been identified by the European Union Committee of Experts on Rare Diseases (EUCERD) as a key policy in the management of patients suffering from RDs17. An example is provided by the project, funded in 2010 by the Italian Ministry of Health, on the Definition of a model of disease management of patient with congenital bleeding disorders aimed at the prevention and reduction of both health and social impact of the disease and its complications. Alongside unsolved challenges in clinical management of haemophilia, patients and their treaters are now facing new challenges arising from age-related co-morbidities (e.g. cardiovascular diseases, malignancies)18. As a consequence, in order to define the most appropriate diagnostic and therapeutic strategies for identifying, preventing and treating age-related comorbidities, a closer cooperation among specialists would be required. However, in Italy a wide variation within and between Regions in terms of volume of activity and of organisational models of haemophilia care was observed19. This could at least partially explain the reason why patients must still travel long distances to attend a HC. On the basis of the emerging needs of haemophilia patients5,20, a disease management model for IBDs improving the quality, safety and efficiency in the delivery of basic/essential levels of healthcare by the National Health Service was developed after a highly inclusive process21. With the Agreement between the Government and the Regions of March 13th, 201322, a formal commitment was taken by the Regions to adopt healthcare pathways and an institutional accreditation system for IBDs on the basis of the recommendations established at national level for planning healthcare delivery23, and for identifying organisational requirements and standards for HCs8,10. Notwithstanding this, it is still necessary to improve the process of data collection, in order to support performance of benchmarking and outcome measurement to inform any future strategies19,24. The demand for clotting factor concentrates represents the main driver of total direct costs of haemophilia care25. However, in order to assess the sustainability of the haemophilia model of care, further studies focusing also on the social burden of the disease are required. According to the findings of the project Social and Economic Burden and Health-Related Quality of Life in Patients with RD in Europe (BURQOL RD, www.burqol-rd.com) carried out on a sample of Italian haemophilia patients26, an improved quality of life associated with the current regimen of care has a direct impact on the patient's life as well as on the healthcare and non-healthcare resources consumed and related to the disease (e.g. informal care, productivity loss), and on the patient's capacity to contribute positively to the social-economic system. The improvement of diagnosis, accessible and costefficient quality healthcare assistance is an important objective, especially in the field of RDs in which the Italian National Institute of Health has been engaged for several years27. In RDs, one of the main issues is to collect epidemiological data on the prevalence28. However, where expertise is rare, the need to gather skills, share and disseminate information and knowledge (e.g. international and multicentre clinical trials) is also envisaged with economically efficient use of resources, considering the current economic and financial context. As pointed out by Taruscio et al.29 and Andersen and co-workers30, quality criteria and standards for the delivery of services by CoE, whether considered for groups of RDs or a single RD, are set on the basis of European recommendations shared with patient organisations. All MSs are called on to establish such CoE within their national plans or strategies for RDs. Examples are provided by the inspiring principles driving the development of the Italian national plan for RDs31, as well as by the regional plan of Piedmont and Aosta Valley Regions32. As a common element, in all experiences of certification for HCs, there is a strong participation and involvement of patient organisations in the process, either as a promoter (Italian Institutional model, Canada, EUHANET) or as a component of the inspection team (Canada, UK, Ireland). A difference is the voluntary vs mandatory adherence to the accreditation models that is a characteristic of the Dutch and the Italian institutional models. Whereas the evaluation procedures are based on self-assessment and peer-review procedures in the Italian professional model, the Dutch, Canadian and Italian Institutional models are based on external evaluation carried out by third party and independent auditors. All models aim to achieve a standardisation of haemophilia care and recognition by Health Authorities. Certification/accreditation systems of CoE for groups of RDs or a single RD are an on-going process throughout all Europe. The experience acquired in haemophilia and other IBDs can be regarded as a pilot model in the field of accreditation and designation of CoE for RDs. It is the result of policy development following a vertical scheme/flow (top-down adoption from European, national to regional level and bottom-up pressure from patient organisations to health policy makers) and at the horizontal level through the involvement and consultation of key stakeholders such as health professionals and patient bodies, RD experts, policy and decision makers. In conclusion, the international meeting Haemophilia Centre Certification Systems across Europe contributed to providing a wide-angle snapshot of the on-going HCs certification / accreditation systems which are an addedvalue choice to enhancing national models of public Blood Transfus 2014; 12 Suppl 3: s492-4 DOI 10.2450/2014.0076-14s 493 Calizzani G et al healthcare and can play a key role in promoting the development of international reference networks for RDs. Conflict of interest Pier Mannuccio Mannucci declares that he received honoraria for participating as speaker at educational meetings organised by Biotest, Bayer, Grifols, Kedrion Biopharma and Novo Nordisk. The other Authors declare no conflicts of interest. 17) 18) 19) 20) References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) International Meeting "Haemophilia Centre Certification Systems across Europe". Centro Nazionale Sangue. Available at http://www.centronazionalesangue.it/newsbox/seminariomalattie-emorragiche-congenite-mec. Accessed on 05/03/2014. Official Journal of the European Union L 88/45. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare. Availablt ae http://eur-lex.europa.eu/ LexUriServ/LexUriServ.do?uri=OJ:L:2011:088:0045:0065:e n:PDF. Accessed on 15/01/2014. European Parliament and Council. Regulation (EC) 141/2000 of the European Parliament and of the Council of 16 December 1999 on orphan medicinal products. Official Journal 2000; L 18:1-5. Available at http://eurlex.europa.eu/LexUriServ/LexUriServ.do?uri= OJ:L:2000:018:0001:0005:en:PDF. Accessed on 15/01/2014. Colvin BT, Astermark J, Fischer K, et al. European principles of haemophilia care. Haemophilia 2008; 14: 361-374. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of haemophilia. Haemophilia 2013; 19: e1-47. Hermans C. Haemophilia Centre certification system across Europe: the Belgian experience. Blood Transfus 2014; 12 (Suppl 3): s497-500. Leebeek FWG, Fischer K. Quality of haemophilia care in the Netherlands: new standards for optimal care. Blood Transfus 2014; 12 (Suppl 3): s501-4. Calizzani G, Vaglio S, Arcieri R, et al. Models for institutional and professional accreditation of haemophilia centres in Italy. Haemophilia 2013; 19: e248-55 Mannucci PM, Menichini I. A certification/accreditation model for Haemophilia Centres in Italy. Blood Transfus 2014; 12 (Suppl 3): s505-9. Calizzani G, Candura F, Menichini I, et al. The Italian institutional accreditation model for the Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s510-4. Haemophilia Alliance. A National Service Specification for Haemophilia and other Inherited Bleeding Disorders, 2nd edn. London. The Haemophilia Alliance, 2006. Available at: http:// www.ukhcdo.org/docs/HaemAlliance-NatSvsSpec2006.pdf. Accessed on 15/01/2014. Makris M, Calizzani G, Fischer K, et al. The European Haemophilia Network (EUHANET). Blood Transfus 2014; 12 (Suppl 3): s515-8. Giangrande P, Calizzani G, Menichini I, et al. The European standards of Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s525-30. Candura F, Menichini I, Calizzani G, et al. The methodology for defining the European Standards for the certification of Haemophilia Centres in Europe. Blood Transfus 2014; 12 (Suppl 3): s519-24. Martino D, Teitel J, Page D, et al. The haemophilia certification system in Canada. Blood Transfus 2014; 12 (Suppl 3): s53141. Skinner MW, Soucie JM, McLaughlin K. The National Haemophilia Program Standards, Evaluation and Oversight 21) 22) 23) 24) 25) 26) 27) 28) 29) 30) 31) 32) Systems in the United States of America. Blood Transfus 2014; 12 (Suppl 3): s542-8. EUCERD Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States (24 October 2011). Available at http://www.eucerd.eu/upload/file/EUCERD RecommendationCE.pdf. Accessed on 05/03/2014 Coppola A, Morfini M, Cimino E, et al. Current and evolving features in the clinical management of haemophilia. Blood Transfus 2014; 12 (Suppl 3): s554-62. Nuti S. La sostenibilità del modello di cura. Available at http:// www.centronazionalesangue.it/sites/default/files/nuti_la_ sostenibilita_del_modello_di_cura.pdf. Accessed on 23/02/2014 Arcieri R, Molinari AC, Farace S. Uncovered needs in the management of inherited bleeding disorders in Italy. Blood Transfus 2014; 12 (Suppl 3): s563-6. Calizzani G, Menichini I, Candura F, et al. Definition of an organisational model for the prevention and reduction of health and social impacts of inherited bleeding disorders. Blood Transfus 2014; 12 (Suppl 3): s582-8. Official Journal of Italian Republic no. 107 May 9th, 2013. Accordo, ai sensi dell'articolo 4 del decreto legislativo 28 agosto 1997, n.281, tra il Governo, le Regioni e le Province autonome di Trento e Bolzano sulla definizione dei percorsi regionali o interregionali di assistenza per le persone affette da Malattie Emorragiche Congenite (MEC). Available at http://www.centronazionalesangue.it/sites/ default/files/accordo_csr_13.03.2013_gu_n._107_09.05.2013_ assistenza_mec.pdf. Accessed on 16/02/2014. Fortino A, Di Stanislao F. Institutional accreditation of Health Services in Italy: the long road to quality. Blood Transfus 2014; 12 (Suppl 3): s551-3. Hassan HJ, Morfini M, Taruscio D, et al. Current status of Italian Registries on inherited bleeding disorders. Blood Transfus 2014; 12 (Suppl 3): s576-81. Lanzoni M, Candura F, Calizzani G, et al. Public expenditure for plasma-derived and recombinant medicinal products in Italy. Blood Transfus 2013; 11 (Suppl 4): s110-7. Kodra Y, Cavazza M, Schieppati A, et al. The social burden and quality of life of patients with haemophilia in Italy. Blood Transfus 2014; 12 (Suppl 3): s567-75 Taruscio D, Agresta L, Amato A, et al. The Italian National Centre for Rare Diseases: where research and public health translate into action. Blood Transfus 2014; 12 (Suppl 3): s591-605. Taruscio D, Kodra Y, Ferrari G, et al. The Italian National Rare Diseases Registry. Blood Transfus 2014; 12 (Suppl 3): s606-13. Taruscio D, Gentile AE, Evangelista T, et al. Centres of Expertise and European Reference Networks: key issues in the field of rare diseases. The EUCERD Recommendations. Blood Transfus 2014; 12 (Suppl 3): s621-5. Andersen T, Le Cam Y, Weinman A. European Reference Networks for rare diseases: the vision of patients. Blood Transfus 2014; 12 (Suppl 3): s626-7. Congiu ME. The Italian National Plan for Rare Diseases. Blood Transfus 2014; 12 (Suppl 3): s614-6. Baldovino S. Menegatti E, Modena V, et al. Piedmont and Aosta Valley inter-regional network in the context of the Italian National Network for Rare Diseases. Blood Transfus 2014; 12 (Suppl 3): s617-20. Correspondence: Gabriele Calizzani Italian National Blood Centre Via Giano della Bella 27 00162 Rome, Italy e-mail address: areaplasma.cns@iss.it Blood Transfus 2014; 12 Suppl 3: s492-4 DOI 10.2450/2014.0076-14s s494 HAEMOPHILIA CENTRE CERTIFICATION SYSTEMS ACROSS EUROPE AND NORTH AMERICA Blood Transfus 2014; 12 Suppl 3 © SIMTI Servizi Srl REVIEW Haemophilia Centre certification system across Europe: the Belgian experience Cedric Hermans Haemostasis and Thrombosis Unit, Division of Haematology, Haemophilia Clinic, Saint-Luc University Hospital, Bruxelles, Belgium Introduction Haemophilia is characterised by recurrent bleeding, especially into the joints, which eventually results in chronic crippling arthropathy. Since the early 1960s, replacement therapy using intravenous clotting factors has become available1. Clotting factor concentrates can be administered as on-demand therapy in the event of bleeding episodes, or at regular time intervals, often three times a week, as prophylaxis-therapy to prevent bleeding. Regardless of the strategy chosen, haemophilia care requires intensive life-long treatment. By definition, patient management is multidisciplinary, involving nurses, physiotherapists and social workers, as well as haemophilia physicians or haematologists, surgeons, specialists in rehabilitation and other relevant medical personnel. Delivering high-quality haemophilia care requires skill and experience, from first diagnosis and continuing throughout patients' life. Several initiatives have recently been launched in order to review and assess current trends in haemophilia treatment across Europe, with the ultimate goal of standardising patient care and promoting the best medical practices across the board. This paper outlines the current state of haemophilia care in Belgium and reports on ongoing national and European initiatives aimed at certifying specialised Haemophilia Treatment Centres (HTCs). Haemophilia care in Belgium Approximately 1,150 patients with a deficiency in coagulation factor VIII (FVIII) or factor IX (FIX), including haemophilia carriers with clotting factor deficiency, are currently included in the Belgian patient Haemophilia Association (AHVH) registry. Given the lack of official national independent registry, this represents the most valid demographic estimation currently available. In 2011, the total cost of haemophilia care related to using FVIII and FIX concentrates, as well as by-passing agents, was estimated by the Belgian National Institute of Health (INAMI) at approximately 81 million euro (Table I). As is the case for most countries, in Belgium the cost of replacement therapy has been steadily increasing over the last 10 years. The Belgian paradox and ambiguity of haemophilia care Haemophilia patients, along with the health professionals involved in their care, benefit from excellent access to replacement therapy. Plasma-derived and recombinant FVIII or FIX concentrates are available with no restrictions or limitations of use. This allows for prophylaxis to be given to all ages, invasive procedures to be successfully conducted, and coagulation factor inhibitors to be eradicated using high-dose immune tolerance, where appropriate. Concentrates can easily be obtained from most hospitals, even from private pharmacists, and selfand home-treatment is widely available. The cost of each FVIII unit, excluding subsequent post-procurement taxes and cost-reduction measures implemented by national government, as well as that of service and support costs, is among the highest in Europe, ranging from 0.81-0.98 euro per unit. This renders the Belgian haemophilia market particularly attractive to the pharmaceutical industry. The exceptions to this rule are by-passing agents, such as Factor Eight Inhibitor Bypassing Activity (FEIBA), and FIX concentrates, with the former priced at one of the lowest Table I - Cost of replacement therapy for haemophilia in Belgium (in euros). Factor VIII (plasma-derived and recombinant) Factor IX (plasma-derived) Factor IX (recombinant) FEIBA Novo Seven Total Belgian population 2006 2007 2008 2009 2010 2011 53,901,207 56,035,135 61,902,053 61,662,285 64,127,153 65,624,411 552,223 462,114 510,704 676,431 642,646 662,424 3,666,620 3,994,425 4,863,122 5,207,261 6,357,121 6,597,562 578,834 772,044 1,166,180 729,312 1,545,327 1,525,654 2,039,854 4,241,009 2,563,050 2,584,382 2,849,959 6,692,361 10,511,382 10,584,534 10,666,866 10,753,080 10,839,905 11,000,638 FEIBA: Factor Eight Inhibitor Bypassing Activity Blood Transfus 2014; 12 Suppl 3: s497-500 DOI 10.2450/2014.0061-14s © SIMTI Servizi Srl s497 Hermans C levels in Europe and the latter sold at lower prices compared to other countries. In addition to coagulation factors, other treatment elements, such as specialised consultations, laboratory tests and specific treatments like dental care, orthopaedic surgery and physiotherapy receive full financial support. At present, there are 10 HTCs registered with the World Federation of Haemophilia, spread throughout the country, with five in Flanders, four in Bruxelles and one in Wallonia. Access to high-quality replacement therapy and specialised haemophilia care has been made possible and continuously improved by the sustained initiatives, effort and input of the AHVH, founded over 50 years ago. Yet these positive features are not sufficient to outweigh the numerous weaknesses inherent to haemophilia care in Belgium. Unlike concentrates, which are fully reimbursed, there is currently no financial support for training courses on self- and home-therapy, systematic multidisciplinary consultation or comprehensive care. Furthermore, none of the existing centres are officially recognised or certified by the Belgian Ministry of Health, nor are they audited or specifically funded for haemophilia care. As a result, most centres are highly dependent on external funding provided by the pharmaceutical industry. In addition, there is no independent national registry, rendering it difficult to provide valid data regarding the use of resources, incidence of inhibitor development and patient outcomes at a national level. Given this context, implementing a national tender process for concentrates appears unfeasible. Factor concentrates can also be prescribed by general practitioners, for a significant but undetermined proportion of patients that primarily comprises those with mild or moderate disease. This therefore means there is no incentive to regularly attend specialised clinics. The percentage of Belgian haemophilia patients who are not regularly followed-up in Haemophilia Centres is thus still unknown. For this reason, it may be assumed that the physical health, quality of life and life expectancy of these patients could be markedly improved if they were regularly referred to specialised centres. Current adherence to European haemophilia care principles: the Belgian situation In order to standardise practices, an expert group of haemophilia care providers drew up the Principles of Haemophilia Care in 2008, published by Colvin et al. in Haemophilia2. This document summarises the essential components of a comprehensive national haemophilia care service in the form of 10 recommendations, provided in Table II. They emphasise the need for service coordination, with the first recommendation stating that this could be best achieved by means of a national committee involving all stakeholders, charged with overseeing and planning all national services. The second recommendation, almost as relevant as the first, stresses the need for a confidential national registry of all patients affected by the disease. Knowing the exact number of patients with congenital bleeding disorders, along with their disease severity, makes it possible to better plan the care service, and particularly to precisely calculate what therapeutic resources will be required. The third recommendation advises that comprehensive haemophilia care centres should be established within an appropriate network, with patient distribution and geographic factors likely constituting the basis of its construction. The other recommendations relate to detailed service provision at the centres, such as monitoring adverse therapeutic events, home therapy and prophylaxis implementation. The European principles of haemophilia care are now being considered as a framework for service development over the entire continent, especially in countries with not as well-developed coordinated organisation. When campaigning for improvements in haemophilia care services, the strategy of involving national government health departments has proven useful to advocates. To promote adherence within the European community, the 10 recommendation principles have been presented to members of the European Parliament with positive results. Table II - The European principles of care according to Colvin et al.2. 1. A central haemophilia organisation with supporting local groups. 2. National haemophilia patient registries. 3. Comprehensive Care Centres (CCCs) and Haemophilia Treatment Centres (HTCs). 4. Partnership in delivery of care. 5. Safe and effective concentrates at optimum treatment levels. 6. Home treatment and delivery. 7. Prophylactic (preventive) treatment. 8. Specialist services and emergency care. 9. Management of inhibitors. 10. Education and research. The service provision level within different European countries, in comparison with the principles of haemophilia care recommendations, has recently been audited by two studies, one performed by physicians and the other by patient organisations3,4. The first revealed that the principles of haemophilia care were generally applied throughout Europe, yet with centralised care not being available for all patients (Table III). Moreover, a number of features pertaining to the manner in which national care is organised, such as using registries, physiotherapy coverage, formal paediatric care and laboratory services, warrant improvements. For Blood Transfus 2014; 12 Suppl 3: s497-500 DOI 10.2450/2014.0061-14s s498 Certification of haemophilia centres in Belgium Table III - Summary of adherence to Principles 1, 2, 3 and 7 according to country3. Country N. of centres Principle 1 Central organisation Principle 2 Patient registry Principle 3 All patients treated in CCC/ HTC N. of CCC/ HTC per million inhabitants Principle 7 % of children on prophylaxis Principle 7 % of adults on prophylaxis Belgium 1 No No No 0.83 75-100 50-75 France 1 Yes Yes Yes 0.71 75-100 1-25 Germany 2 Yes Yes No 0.89 75-100 50-75 Greece 1 Yes Yes Yes 0.37 75-100 1-25 Italy 3 Yes Yes Yes 0.81 75-100 1-25 Netherlands 2 Yes No Yes 0.78 75-100 50-75 Norway 1 Yes No Yes 0.40 75-100 50-75 Poland 1 Yes No No 0.84 75-100 1-25 Portugal 1 No No No 3.77 75-100 1-25 Slovakia 1 Yes Yes Yes 7.78 75-100 1-25 Spain 3 No Yes Yes 0.91 75-100 1-25 Sweden 1 Yes No Yes 0.32 75-100 75-100 Switzerland 1 Yes Yes No 1.27 75-100 1-25 United Kingdom 2 Yes Yes Yes 1.06 75-100 50-75 Total 21 79% Yes 57% Yes 64% Yes Median 0.84 IQR0.62-1.11 100% (75-100) 57% (1-25) 36% (50-75) 7% (75-100) Summary CCC: Comprehensive Care Centre; HTC: Haemophilia Treatment Centre; IQR: Interquartile range Belgium, the survey highlighted the absence of both a national registry and designated comprehensive Haemophilia care Centres. National initiative to improve haemophilia care organisation In 2007, a new model for haemophilia organisation in Belgium was proposed, though it has not yet been implemented5. According to this new model, there should be a single national coordinating centre in charge of overseeing over 150 patients with severe FVIII or FIX deficiency. This centre should be characterised by significant scientific production, estimated on the basis of a cumulative impact factor >100 of peer-reviewed publications over the past 5 years, along with recognised expertise in haemophilia care. In addition to this, there should be several smaller HTCs, the exact number of which still needs to be defined. These centres should follow up at least 10 severe haemophilia A or B adults or children, be spread out across the country and provide access to care and concentrates. This recommended number of patients per centre is much lower than that suggested by several established organisations (i.e. the World Federation of Haemophilia and United Kingdom Haemophilia Centre Doctors' Organisation, UKHCDO), and is incompatible with the level of expertise currently required by haemophilia care. The prescription of clotting factor concentrates should be restricted to "haemophilia specialists", the exact qualification and experience of whom still need to be defined for Belgium. Since 2007, applications for hosting a comprehensive Haemophilia care Centre have been submitted by several hospitals. At the beginning of 2014, the Belgian health authorities announced that this new plan for haemophilia care would soon be implemented and granted funding. In addition to this disease's rarity and complexity, there are several obstacles to improving haemophilia care organisation in Belgium. Patient centralisation in a limited number of specialised centres appears, in fact, to be negatively impacted by several factors. These include competition between hospitals, high variability of patient number between centres and political factors, with the latter proving particularly significant in a small but complexly governed country like Belgium. European initiative of Haemophilia Centre certification The European Commission (EC) has asked all member states to support the creation of European Reference Networks for all rare diseases. Given this context, the EC has pledged its support to the European Haemophilia Network (EUHANET) project, one of its aims being to create a certification scheme for European Haemophilia Centres. Following extensive study of the Blood Transfus 2014; 12 Suppl 3: s497-500 DOI 10.2450/2014.0061-14s s499 Hermans C scientific literature and communication with all European countries, a document entitled European Guidelines for the certification of Haemophilia Centres has been produced. After several rounds of extensive consultation, the initial document was modified, and the final version distributed at an international meeting in Rome in July 2013 and at the European Parliament in October 2013. The standard document, consultable at www.euhanet. org, defines two levels of Haemophilia Centre: European Haemophilia Treatment Centre (EHTC) and European Haemophilia Comprehensive Care Centre (EHCCC). EHCCCs will likely be in charge of over 40 severe haemophilia patients and offer round-the-clock care, with high-quality coagulation laboratory back-up and a full range of facilities. Any centre in Europe can apply for certification, with applications reviewed by a committee of medical, nursing and patient representatives. The application form is available on the EUHANET website. By January 2014, 44 centres had applied for certification, including 3 in Belgium. It is worth noting that these Belgian centres will be certified at the European level prior to national recognition and funding. Reference 1) 2) 3) 4) 5) Nilsson IM, Berntorp E, Lofqvist T et al. Twenty-five years' experience of prophylactic treatment in severe haemophilia A and B. J Intern Med. 1992; 232: 25-32. Colvin BT, Astermark J, Fischer K et al. European principles of haemophilia care. Haemophilia. 2008; 14: 361-74. Fischer K, Hermans C. The European Principles of Haemophilia Care: a pilot investigation of adherence to the principles in Europe. Haemophilia. 2013; 19:35-43. O'Mahony B, Noone D, Giangrande PL, Prihodova L. Haemophilia care in Europe - a survey of 35 countries. Haemophilia. 2013; 19: e239-47. Institut National d'Assurance Maladie Invalidité (INAMI). Comprehensive care pour hémophiles - Maladies hémorragiques héréditaires chroniques [in French]. Note CCMC 2007/5. Conclusions Belgian haemophilia patients benefit from unrestricted access to a wide range of plasma-derived or recombinant clotting factor concentrates and by-passing agents. Patient care quality and efficiency is, however, negatively impacted by the absence of a national haemophilia registry and specific funding, as well as by the lack of official recognition and certification for specialised haemophilia centres. In the framework of the Belgian plan for rare diseases, ongoing national and European initiatives should soon contribute to a more efficient organisation of haemophilia care in Belgium. These include the creation of a national funded network and, at the European level, official EUHANET certification of European haemophilia treatment centres. Keywords: haemophilia, comprehensive care, certification. Conflicts of interest Cedric Hermans has received honoraria for his role as consultant for and active participation on advisory boards organised by Baxter, Bayer, Pfizer, CAF-DCF, SOBI, Ipsen, LFB, CSL-Behring, Novo Nordisk and Octapharma. He has received research grants or lecture chair positions from Baxter, Bayer, Pfizer, CAF-DCF, CSL-Behring, Novo Nordisk, Octapharma and Ipsen. Correspondence: Cedric Hermans Haemostasis and Thrombosis Unit Division of Haematology Haemophilia Clinic St-Luc University Hospital Avenue Hippocrate 10 1150 Bruxelles, Belgium e-mail: cedric.hermans@uclouvain.be Blood Transfus 2014; 12 Suppl 3: s497-500 DOI 10.2450/2014.0061-14s s500 ORIGINAL ARTICLE Quality of haemophilia care in the Netherlands: new standards for optimal care Frank W.G. Leebeek1, Kathelijn Fischer2,3 1 Erasmus University Medical Centre, Rotterdam; 2Van Creveldkliniek, University Medical Centre Utrecht, Utrecht, Julius Center for Health Sciences and Primary Care, University Medical Centre Utrecht, Utrecht, the Netherlands 3 Background. In the Netherlands, the first formal haemophilia comprehensive care centre was established in 1964, and Dutch haemophilia doctors have been organised since 1972. Although several steps were taken to centralise haemophilia care and maintain quality of care, treatment was still delivered in many hospitals, and formal criteria for haemophilia treatment centres as well as a national haemophilia registry were lacking. Material and methods. In collaboration with patients and other stakeholders, Dutch haemophilia doctors have undertaken a formal process to draft new quality standards for the haemophilia treatment centres. First a project group including doctors, nurses, patients and the institute for harmonisation of quality standards undertook a literature study on quality standards and performed explorative visits to several haemophilia treatment centres in the Netherlands. Afterwards concept standards were defined and validated in two treatment centres. Next, the concept standards were evaluated by haemophilia doctors, patients, health insurance representatives and regulators. Finally, the final version of the standards of care was approved by Central body of Experts on quality standards in clinical care and the Dutch Ministry of Health. Results. A team of expert auditors have been trained and, together with an independent auditor, will perform audits in haemophilia centres applying for formal certification. Concomitantly, a national registry for haemophilia and allied disorders is being set up. Discussion. It is expected that these processes will lead to further concentration and improved quality of haemophilia care in the Netherlands. Keywords: standards, quality, audit, registry, haemophilia. Introduction Haemophilia in the Netherlands The Netherlands is a densely populated country in Western Europe and has a population of 16.5 million inhabitants, who are living on an area of 33,883 Km2, with a population density of 487 per km2. Although a formal haemophilia registry is still lacking, the estimated number of patients with haemophilia is 1,600 to 1,800, including around 800 with severe haemophilia (< 0.01 U/mL of coagulation factor [F]VIII/IX). Simon van Creveld (1894-1971), professor of paediatrics at the University of Amsterdam since 1938, was the Dutch pioneer regarding the organisation of haemophilia care. Historical organisation of Dutch Haemophilia care 1950-1998 Haemophilia care has always been well organised in our country. Already in 1950, Simon van Creveld founded a specialized clinic for children with chronic diseases, including a specialised centre for children with haemophilia. In 1964, the first haemophilia clinic in the world was officially opened by the Dutch Queen Juliana. This haemophilia clinic was an example for many other clinics in the world, and was recognised by the World Federation of Haemophilia. In 1971, Professor van Creveld died and the clinic was named Van Creveldkliniek. In the late 1960s prophylactic replacement therapy was introduced1, followed by home treatment in 1974 and low dose immune tolerance in 19812. Meanwhile, treatment with cryoprecipitate infusions was applied in many hospitals in the Netherlands. The Dutch Haemophilia Centres Doctors Organisation (NVHB) was established in 1972 and this organisation is still active. The doctors from the NVHB meet every three months. These meetings are also attended by a representative of the manufacturers of coagulation factor concentrates, the Haemophilia Patients Organisation (NVHP) and the haemophilia nurses. Clinical problems Blood Transfus 2014; 12 Suppl 3: s501-4 DOI 10.2450/2014.0041-14s © SIMTI Servizi Srl s501 Leebeek FWG, Fischer K and management issues are discussed, as well as side effects of treatment. In 1981 the Van Creveldkliniek was the national haemophilia treatment centre and eight hospitals were recognised as regional treatment centres, but 21 other hospitals also treated haemophilia patients. This situation remained till 1999, without any quality control. The number of patients treated in these hospitals centre varied from 8 to 600 patients, which resulted in a variability in expertise and quality of care. 1999-2002 In 1999, The Ministry of Health in collaboration with the doctors from the NVHB and the Dutch Haemophilia Patient Society (NVHP), wrote a haemophilia management policy stating that care for patients with haemophilia should be centralised in haemophilia treatment centres to ensure quality of care by concentrating expertise. No distinction was made between national and regional centres, nor between treatment centres and comprehensive care centres at that time. This resulted in 16 haemophilia treatment centres geographically distributed over the country, ensuring treatment in hospitals nearby for all patients, most of these centres treated adults only. 2002-today In 2002 and 2003 the 1999-haemophilia management policy was evaluated and it turned out only 6/16 centres complied with the standards of care. It was advised to further centralise haemophilia care, but this advice was not followed due to opposition of the patient organisation, which was strongly in favour of treatment in hospitals nearby for all. Until 2013 still 13 hospitals were treating haemophilia patients, with patient numbers ranging from under 20 to over 500 per centre. A consensus treatment guideline was drafted by doctors of the NVHB and published in 20093. Complications of haemophilia and of treatment have been registered every three months in a national system (KWARK) since 2002. In addition three treatment centres report their complications to the European Haemophilia Safety Surveillance (EUHASS) database, www.EUHASS.org. Material and methods New quality system for haemophilia in the Netherlands Life-long treatment of haemophilia includes many medical disciplines and requires experience and coordination for optimum results. It has been established that centralised haemophilia care improves patient outcome in different settings4-6. Although the European principles of haemophilia care were formally established in 20087, adherence to these principles is not yet perfect8. In 2009 the NVHB took the initiative to start for a new quality system for haemophilia care in the Netherlands. With financial support of the Ministry of Health a formal development process was undertaken from 2009 to 2011. First, a project group consisting of doctors from larger and smaller haemophilia treatment centres, nurses, and patient representatives in collaboration with the institute for harmonisation of quality standards in clinical care (Stichting HKZ) undertook a study of available literature on quality standards and performed explorative visits to two Dutch haemophilia treatment centres. Secondly, concept standards were defined, which were validated in two treatment centres to test their use in clinical practice. Next, the concept standards were evaluated by haemophilia doctors (NVHB), patients, health insurance representatives and regulators. Finally, the final version of the standards of care was approved by Central body of Experts on quality standards in clinical care (CCvD-Z/W) and submitted to the regulatory body at the Dutch Ministry of Health. Approval was obtained in March 2013. Results Standards for delivery of haemophilia care The most important quality standards for delivery of haemophilia care are shown in Table I. These quality standards are considered mandatory for certification as a haemophilia treatment centre. Each centre should at least treat 40 patients with severe haemophilia, of which at least ten children. This quality norm has been implemented because we felt that in centres with fewer patients expertise cannot be guaranteed, not only by the haemophilia doctors and nurses, but also of other members of the multidisciplinary team involved. One of the new regulations was that a treatment centre should treat both children and adults. This will lead to a better transition of care from the children's hospital to adult care. Also this will result in optimal genetic counselling and care for pregnant carriers of haemophilia and women with other bleeding disorders can be achieved during pregnancy and at delivery. In the team an internist/haematologist, as well as a paediatrician/haematologist should be available. These haemophilia doctors are primarily responsible for the care of these patients with respect to treatment of bleeding and coordinate prophylaxis to prevent bleeding. In addition they coordinate care before and after surgical procedures or other interventions. The team also consists of at least one specialised haemophilia nurse. Nurses are responsible for infusion of coagulation factor concentrates as well as for instructing and teaching patients, both children and adults, how to infuse coagulation factor concentrates and supporting patients on home treatment. They also are involved in teaching other nurses in the hospital. In addition, every Blood Transfus 2014; 12 Suppl 3: s501-4 DOI 10.2450/2014.0041-14s s502 Dutch standards for quality of haemophilia care centre should have a multidisciplinary team including a physical therapist, orthopaedic surgeon, rehabilitation doctor, clinical genetic specialist and social worker or psychologist. There has to be direct collaboration with haepatologists or specialist in infectious diseases and with gynaecologists to take care of pregnant carriers of haemophilia or women with other bleeding disorders, including von Willebrand disease. There is a need for a dedicated dentist or surgeon for dental care in patients with bleeding disorders. The multidisciplinary team meets with minimum intervals (Table I). In addition every haemophilia treatment centre has dedicated laboratory facilities which offers measurements of coagulation factor analysis, including FVIII, FIX, von Willebrand factor and other individual coagulation factors at all hours. Routine molecular diagnostic analysis of mutations in FVIII or FIX is performed and centralised in four treatment centres. All centres have adequate supply of coagulation factor concentrates for all bleeding disorders available at all times. Patients with haemophilia and allied bleeding disorders who are treated with coagulation factor concentrates are seen at least once a year in the haemophilia treatment centre. Patients with severe haemophilia are seen more often, at least 2 to 4 times a year. Surgery should always be performed in one of the haemophilia treatment centres. For every patient an individual treatment plan is made and available in the electronic patient files. In this treatment plan, the diagnosis, treatment in case of acute bleeding or surgery, and co-morbidity are specified. Carriers of haemophilia, especially women with reduced FVIII of FIX (<40%), should be registered in one of the Haemophilia Treatment Centres (HTCs) in order to receive adequate treatment for bleeding, pregnancies and delivery, and obtain genetic counseling. Certification and auditing of Treatment Centres After approval of the regulations in March 2013, candidate treatment centres have to apply for certification as a Haemophilia Treatment Centre (HTC). This includes a 1-2 day audit of each candidate centre. For this purpose a limited number of haemophilia doctors and nurses received training to act as haemophilia experts-auditors. Centres will be visited by a team of a doctor, a nurse and one auditor of an official specialised auditing company (Det Norske Veritas, Barendrecht, the Netherlands). The certificate will be evaluated yearly and audits will be performed every three years. Based on the new standards that have been set up, four HTCs have decided to stop their function as haemophilia treatment centre and two centres have been founded by merging four former HTCs. Other centres who were previously separated into a paediatric and adult centre in the same city are Table I - Most important quality standards for Haemophilia Treatment Centres in the Netherlands. Index Crucial standards Note Number of patients with severe haemophilia Minimum 40 of which at least 10 children Including both children and adults Multidisciplinary haemophilia team Internist-haematologist for adults Paediatrician-haematologist for children Haemophilia nurse/specialised nurse Physical therapist Social worker/psychologist Dedicated protocols for Diagnostics Treatment of bleeding Prophylaxis Peri-operative period Emergency department Treatment in case of inhibitors Treatment of inhibitors Treatment and prevention of viral infections Methods of infusion of coagulation factors Guidance of haemophilia carriers Education for home treatment Registration of patients in national registry NA Complication registration NA Regular meetings of different disciplines Adult and paediatric haemophilia doctors Every month Orthopaedic surgeons/physical therapists and rehabilitation experts Every 2 months Haemophilia expert available for 24 hours a day 7 days a week NA Every patient has an individual treatment plan NA For every bleeding disorder adequate supply of coagulation factor concentrate available NA NA: not applicable. intensifying collaboration to provide more continuity of care and operate as a single centre. Currently, there are in seven candidate HTCs in the Netherlands: Haemophilia Treatment Centre south-west Netherlands (Leiden University Medical Centre, Leiden & HAGA Hospital, The Hague), Haemophilia Treatment Centre south (Maxima Medical Centre Eindhoven & Maastricht University Medical Centre), Academic Medical Centre Amsterdam, University Medical Centre Groningen, Radboud University Medical Centre Nijmegen, University Medical Centre Utrecht (van Creveldkliniek), Blood Transfus 2014; 12 Suppl 3: s501-4 DOI 10.2450/2014.0041-14s s503 Leebeek FWG, Fischer K and Erasmus University Medical Centre Rotterdam. The further centralisation of haemophilia care will lead to larger travel distances for patients, but considering the presumed benefit and the relatively small distances in the Netherlands the patients organisation have decided that quality is more important that proximity. Registration of patients and coagulation factor concentrates Although the Netherlands has a registry of blood products transfused since April 1999 and a registry of mortality, viral infections, and side effects of haemophilia treatment since 2002 (KWARK), there is no formal registry of Dutch haemophilia patients. Despite this, participation in a national haemophilia registry is part of the principles of haemophilia care7 and the Dutch quality regulations. At the same time of starting the certification process, additional funding from The Dutch Organisation for Health Research and Development (ZONMW) was obtained to initiate a registry of Dutch patients with haemophilia and allied bleeding disorders. The registry will use a web-based platform, starting with a database of all patients with their diagnosis, and links to electronic diaries and hospital databases in the second phase of development. The aim of this registry is to provide exact data on the number of patients according to diagnosis, the use of various clotting factor concentrates, safety data and data on outcomes. The registry will serve several purposes. For evaluating treatment and side effects, data across treatment centres can be compared. For decision makers, the registry will provide an overview of the total number of patients according to diagnosis, including data on clotting factor consumption. For research, the registry will serve as a base for the haemophilia in the Netherlands (Haemophilia HIN) projects9. It will identify nationwide sub cohorts (e.g. ex-inhibitor patients, or HIV infected patients) eligible for specific studies. Outcome data can be compared with other full cohorts (e.g. with data collected by United Kingdom Haemophilia Centre Doctors' Organisation in the United Kingdom). Data on side effects can be used for postmarketing surveillance of new clotting factors, which will be registered from 2014 onwards. In addition, data on side effects are entered in EUHASS (European Haemophilia Safety Surveillance System) and used in comparison with those from other countries. Reimbursement In the Netherlands, health insurance is mandatory and up to 2012 all costs for clotting factor concentrates were covered without restriction. Since 2012, hospital budgets, including budget for clotting factor concentrates, are fixed at the level of 2010, with a maximum annual growth of 2.5%. As consumption shows a yearly increase of around 5 %, these budgets are insufficient. Individual centers have negotiated with health insurance companies to increase the budget and at the same time with manufacturers of coagulation factor concentrates to reduce the price of concentrates, e.g. by using only one FVIII product. It is expected that future reimbursement of haemophilia care will be conditional on certification of the HTCs. Conclusion In an effort to improve the quality of haemophilia care in the Netherlands the NVHB, in collaboration with patients and other stakeholders, have undertaken a formal process to draft new quality standards for the HTCs. The quality standards were approved by the regulatory agencies and will be enforced by a formal auditing process initiated in 2014. Concomitantly, a national registry for haemophilia and allied disorders is being set up. It is expected that these processes will lead to further centralisation and improved quality of haemophilia care in the Netherlands. The Authors declare no conflicts of interest. References 1) 2) 3) 4) 5) 6) 7) 8) 9) van Creveld S. Prophylaxis of joint hemorrhages in hemophilia. Acta Haematol 1969; 41: 206-14. Mauser-Bunschoten EP, Nieuwenhuis HK, Roosendaal G, Van den Berg HM. Low-dose immune tolerance induction in hemophilia A patients with inhibitors. Blood 1995; 86: 983-8. Nederlandse Vereniging voor Hemofiliebehandelaars (NVHB). Richtlijn Diagnostiek en behandeling van hemofilie en aanverwante hemostasestoornissen. Leebeek, F.W.G. and Mauser-Bunschoten, E.P. 1. 2009. Utrecht, Van Zuiden Communications BV. Soucie JM, Nuss R, Evatt B et al. Mortality among males with hemophilia: relations with source of medical care. Blood 2000; 96: 437-42. Baker JR, Crudder SO, Riske B, et al. A model for a regional system of care to promote the health and well-being of people with rare chronic genetic disorders. Am J Public Health 2005; 95: 1910-6. Evatt BL, Robillard L. Establishing haemophilia care in developing countries: using data to overcome the barrier of pessimism. Haemophilia 2000; 6: 131-4. Colvin BT, Astermark J, Fischer K et al. European principles of haemophilia care. Haemophilia 2008; 14: 361-74. Fischer K, Hermans C. The European Principles of Haemophilia Care: a pilot investigation of adherence to the principles in Europe. Haemophilia 2013; 19: 35-43. Plug I, Van der Bom JG, Peters M et al. Thirty years of hemophilia treatment in the Netherlands, 1972-2001. Blood 2004; 104: 3494-500. Correspondence: Kathelijn Fischer Van Creveldkliniek Room C 01.425 PO Box 85500 3508 GA Utrecht The Netherlands e-mail: k.fischer@umcutrecht.nl Blood Transfus 2014; 12 Suppl 3: s501-4 DOI 10.2450/2014.0041-14s s504 ORIGINAL ARTICLE A certification/accreditation model for Haemophilia Centres in Italy Pier Mannuccio Mannucci1, Ivana Menichini2 1 Scientific Direction, IRCCS Ca' Granda Maggiore Policlinico Hospital Foundation, Milan; 2Necstep Studio Associato, Modena, Italy Background. The Italian Association of Haemophilia Centres has developed a voluntary programme of professional accreditation of Haemophilia Centres, run by its members. Participation in the programme, which aims to foster staff involvement in clinical governance, includes both medical personnel and nurses. Materials and methods. Accreditation is awarded provided the candidate Haemophilia Centre is able to adhere to a pre-established set of quality standards and meet a number of clinical and organisational requirements, previously defined on the basis of evidence-based medicine. Selfevaluation is the first step in the programme, followed by a site visit by a team of peer professionals experienced in quality auditing. Results. The programme has so far involved 21 Italian Haemophilia Centres. The comparison between self- and peer-evaluation revealed less discrepancies for disease-related than for organisational requirements, the latter being met to a lesser degree by most Haemophilia Centres. Discussion. This programme of professional accreditation developed by the Italian Association of Haemophilia Centres has the potential to describe, monitor and improve clinical and organisational performances in the management of patients with haemophilia and allied inherited coagulation disorders. It should also be seen as a contribution to the implementation of the strategy for improving professional governance in Haemophilia Centres. Keywords: professional accreditation, quality of care, standards. Introduction Improvement in the quality of health care delivery is a primary goal for the medical profession1-5. In the past few years, the attainment of this goal has been attempted by means of several different institutional approaches, local and international, which in general focused on organisational and procedural aspects of health care delivery. These programmes pay relatively little attention to quality aspects of clinical management and, most importantly, do not succeed in involving in the process such key players as the medical and nursing professionals. As a consequence, they often fail to truly promote and implement clinical governance6,7. For instance, the ISO 9000 family of standards, which was devised originally by the industry, is effective as a guideline, but its promotion as a standard "helps to mislead companies into thinking that certification means better quality, … [undermining] the need for each organization to set its own quality standards''8. On the other hand, Joint Commission International (JCI) evaluates organisational processes of hospitals as a whole, being less focused on professional aspects of clinical governance9. Accordingly, the staff involved in clinical management feel that these activities are imposed from above, and sometimes they see them as quite foreign to their medical practice. In order to overcome these limitations, the Italian Association of Haemophilia Centres (AICE) convened a working group with the aim of developing a quality ascertainment programme focused on those clinical and organisational activities that are most appropriate for Haemophilia Centres (HCs), based on the direct involvement of the staff and on site visits by a team of professional peers. The ultimate goal of this programme was to award a certificate of accreditation by a learned professional association to those HCs which had reached a pre-established performance threshold. To attain this goal, the HCs had to demonstrate that they were able first to meet a number of clinical and organisational requirements, and then to focus on deficient aspects and so develop a suitable plan aimed to improve unsatisfactory performance. The early results of the accreditation programme at 21 Italian HCs are presented here, with special emphasis on the comparison between self-evaluation and the subsequent independent evaluation by an external team of professional peers. Blood Transfus 2014; 12 Suppl 3: s505-9 DOI 10.2450/2014.0331-13s © SIMTI Servizi Srl s505 Mannucci PM, Menichini I Materials and methods The process of professional accreditation developed and implemented by AICE followed these steps: self-evaluation was first carried out by each HC, based on adherence to a panel of standards previously defined by the an ad-hoc panel comprising clinicians and patients. Requirements were set on the basis of the best available clinical evidence and management guidelines 10 . After self-evaluation results were obtained, peer-evaluation was carried out by a team of professionals previously trained in the auditing process by external experts in the quality control of health care systems. Peer-evaluation was conducted by means of direct interviews with the staff during site visits conducted at the applicant HC, analysis of a random sample of at least 15 medical records and onsite auditing of the operating procedures. Adherence to each standard was evaluated by means of scores attributed to each requirement. The scores employed to express the degree of adherence to standards were 3 for full compliance (when all aspects of the standards were met); 2, for almost full compliance (when most aspects of the standard were met); 1, for partial compliance (when only some aspects of the standards were met); 0, for non-compliance (when no aspects of the standards were met) and NA for not applicable. This report is based upon an evaluation of 21 Centres (Appendix 1) conducted by a team of 5 professionals (Appendix 2). Evaluation took into account requirements set for awareness, information and education of patients and their families (3 requirements); patient care (119 requirements); laboratory practice (33 requirements) and organisational aspects dealing with the daily activities of the HCs (32 requirements). All these criteria are consultable for Italian HCs on a web site10. Results Figure 1 summarises the overall results for the 21 HCs, obtained by comparing self- with peer-evaluation expressed in percentage of the maximal total score attainable for the whole panel of requirements. On average, self-evaluation gave slightly higher results than peer-evaluation (86 vs 82% of the maximal possible score), self-evaluation being lower in 3 HCs only. Analysis of adherence to each requirement did reveal varied results, of which a few representative examples are reported here. For instance, the requirements related to participation of HCs in national and/or regional registries of inherited and acquired bleeding disorders showed good concordance between self- and peerevaluation (score 3: 86 vs 81%). On the other hand, for the criterion on the regular organisation, in collaboration with patient associations, of events for the education and training of patients and their families (including home therapy/self-infusion), the score assigned by peer-evaluation was higher than that assigned by selfevaluation. Highly relevant requirements for the management of inherited coagulation disorders, such as the prescription of coagulation tests according to professional guidelines, was satisfactorily met by a large percentage of HCs, with a good agreement between self- and peer-evaluation. There was also a good degree of adherence related to the production of a written report on diagnosis within one month of the initial visit. Other requirements were less frequently met. For instance, not all HCs provided 24-hour expert haemophilia medical cover and, for this criterion, there was a clear overestimation of performance in self-evaluation (Figure 2). On the contrary, for some requirements the score assigned by peer-evaluation was even higher than that assigned by self-evaluation: for instance, for the determination of the level of antibody titre in patients who developed inhibitors (score 3: 76 vs 81%) (Figure 3). Figure 1 - Comparison of self-evaluation (closed bars) with peer-evaluation (open bars) for 21 HCs (identified by capital letters). Values are expressed as percentages of the maximal total score that could be obtained for the whole set of standards. Figure 2 - Percent distribution of HCs providing 24-h expert medical cover for hemophilia patients. Blood Transfus 2014; 12 Suppl 3: s505-9 DOI 10.2450/2014.0331-13s s506 A certification/accreditation model for Haemophilia Centres in Italy Discussion Figure 3 - As for Figure 2, according to the capacity to provide the actual titre of the antibody in patients who develop inhibitors. Under the heading of requirements related to periodical clinical and multi-disciplinary check-up, there was a good concordance between self- and peerevaluation for the requirement for the organisation of patient check-ups at least once a year (score 3: 90 vs 81%). For the organisation of specific visits for patients characterised by particularly frequent bleeding episodes or complications such as inhibitors, arthropathy or chronic viral infections (score 3: 76 vs 71%) and for drafting a letter for the patients after each visit, with information about current clinical problems, recommended treatment regimens, results of relevant laboratory data and other tests such as imaging, there was also good concordance (score 3: 76 vs 71%). On the other hand, less concordance was found between self- and peer-evaluation with regard to the network of clinical and specialised services needed to collaborate with the haemophilia team. Only a few HCs have in place specific formal agreements that regulate relationships with structures providing specialist services, and peer-evaluation revealed that standards were much less adhered to than declared on self-evaluation, especially in relation to formal agreements with clinicians expert in hepatology (score 3: 67 vs 29%), infectious diseases (score 3: 67 vs 29%) and physiotherapy/orthopaedics (score 3: 67 vs 24%). For the 11 HCs with an internal laboratory, there was a high degree of adherence to the provision of all coagulation tests recommended by the standards: PT; APTT; thrombin time; search of lupus anticoagulant; factor VIII and factor IX assays; inhibitor screen; VWF antigen and ristocetin cofactor activity; fibrinogen and factor II, V, VII, X, XI, XII, XIII assays; platelet aggregation induced by ADP, collagen, adrenaline and ristocetin: (score 3: 91% both in self- and peer-evaluation). For the 10 HCs centres that have no internal laboratory and that rely on external laboratories to provide them with tests through formal agreements that regulate the relationship, self-evaluation was too optimistic with respect to the satisfaction of standards (score 3: 55% vs 0; score 2: 36% in both self- and peer-evaluation). The first consideration that stems from this programme of accreditation of Italian HCs by peer professionals is that, in comparison with other models of certification or accreditation, the medical teams under evaluation shared with peer evaluators a common language and attitude for tackling clinical problems, which greatly facilitated the auditing process. Peer involvement also helped to make mutually acceptable the final judgement made by the accreditation team concerning the performance of the HCs. Finally, the voluntary nature of this programme emphasises the direct involvement of participating physicians in the resilient affirmation of their role in the professional governance of their own HCs. In general, self-evaluation shows a tendency to overrate the quality of performance in this study, in agreement with previous observations, even if the opposite pattern of results was also observed in some cases. For example, the radiological Pettersson score and the magnetic resonance score were not always performed for all children in the periodic clinical and multi-disciplinary check-ups, at variance with the statement made by some HCs. On the other hand, the prescription of some unusual tests of kidney function rather peculiar for patients with haemophilia B undergoing immune tolerance for FIX inhibitors (serum creatinine, proteinuria) was identified more frequently by the peer-evaluation board than actually declared in self-evaluation. Special attention was paid in the accreditation programme not only to the preparation and updating of patient clinical records but also to the provision of written information addressed to patients' family physicians, pediatricians and other specialists, in order to assure and optimise health care continuity. On these topics, peer-evaluation indicated that adherence to standards was often overestimated by the HCs. The discrepancies between self- and peer-evaluations might reflect some lack of documentation of the activity rather than lack of performing the activity. However, we believe that adequate and accurate documentation of daily professional activities does indeed reflect the best professional knowledge and practice, particularly in the context of team work. The critical aspects documented during on-site visits by peers were incorporated by the HCs, which were encouraged to develop a plan aimed to improve the quality of care, to be monitored regularly at least on a yearly basis. The AICE professional accreditation programme proved to be flexible, so that it could be easily adopted in the different realities of Italian HCs. The programme also proved to be practically feasible, because auditing visits by peers could be concluded and completed within one working day. Like all the models of accreditation Blood Transfus 2014; 12 Suppl 3: s505-9 DOI 10.2450/2014.0331-13s s507 Mannucci PM, Menichini I and certification, this programme is obviously not static and foresees, as mentioned above, updating of the set of requirements at regular intervals, in line with the progress of medical knowledge and corresponding practice guidelines. In conclusion, the professional accreditation programme of AICE is proposing a methodology effective for promoting good clinical practice to identify critical aspects of medical processes and to provide an opportunity for the improvement of professional performance through the effect of peer pressure. Moreover, as an initiative started by professionals and not by external authorities and/or hospital administrators, it fosters the direct and resilient involvement of clinicians in the clinical governance of their HCs. Focusing on the professional aspects peculiar to haemophilia care is not an alternative but rather a complementary strategy to other models and programmes of certification and accreditation widely implemented in Europe, which mainly consider organisational and procedural aspects of health care delivery. Conflict of interest Pier Mannuccio Mannucci declares that he received honoraria for participating as speaker at educational meetings organised by Biotest, Bayer, Grifols, Kedrion Biopharma and Novo Nordisk. Ivana Menichini declares no conflicts of interest. References 1) Donabedian A. Explorations in quality assessment and monitoring: The definition of quality and approaches to its assessment. Ann Arbor, USA; 1980. 2) Berwick DM. Heal thyself or heal thy system: can doctors help to improve medical care? Qual Health Care 1992; 1 (Suppl): S2-8. 3) Moss F. Achieving quality in hospital practice. Qual Health Care 1992; 1 (Suppl): S17-9. 4) Berwick DM. Disseminating innovations in health care. JAMA 2003; 289: 1969-75. 5) Werner RM, Bradlow ET, Asch DA. Does hospital performance on process measures directly measure high quality care or is it a marker of unmeasured care? Health Serv Res 2008; 43: 1464-84. 6) UNI EN ISO 9001:2008. Available at: http://www.iso.org/iso/ iso_9000_essentials. Accessed on 30/11/2013. 7) Werner RM, McNutt R. A new strategy to improve quality. Rewarding actions rather than measures. JAMA 2009; 301: 1375-7. 8) Wade J. Is ISO 9000 really a standard? ISO management systems; May-June, 1-20; 2002. 9) Joint Commission International. Available at: http://www. jointcommissin international.org. Accessed on 30/11/2013. 10) World Federation of Hemophilia. Guidelines for the management of Hemophilia. Available at: http://www.hematologija.org/dl/ uploads/Gudelines%20Hemophilia.pdf. http://eimwebserver01. eim.it/necstep/. Accessed on 30/11/2013. Correspondence: Pier Mannuccio Mannucci Scientific Direction IRCCS Ca' Granda Maggiore Policlinico Hospital Foundation Via Pace 9 20122 Milano, Italy e-mail: piermannuccio.mannucci@policlinico.mi.it Blood Transfus 2014; 12 Suppl 3: s505-9 DOI 10.2450/2014.0331-13s s508 A certification/accreditation model for Haemophilia Centres in Italy Appendix 1 Haemophilia Centres participating in the AICE programme of professional accreditation - Centro Emofilia e Trombosi Angelo Bianchi Bonomi, Fondazione IRCSS Ca' Granda, Ospedale Maggiore Policlinico, Milano, Chief: Pier Mannuccio Mannucci. - Centro per l'Emofilia e Coagulopatie Congenite, IRCCS Fondazione Policlinico San Matteo, Università di Pavia, Chief: Gabriella Gamba. - Centro Malattie Emorragiche e Trombotiche, AOU S. Maria della Misericordia, Udine, Chief: Giovanni Barillari. - Centro Emofilia, U.O. Angiologia e Malattie della Coagulazione "Marino Golinelli", AOU Policlinico S. Orsola-Malpighi Bologna, Chief: Lelia Valdrè. - Centro Emofilia, SSCVD Malattie Trombotiche Emorragiche, Città della Salute e della Scienza, Torino, Chief: Piercarla Schinco. - Centro Emofilia, Emostasi e Trombosi, Ospedale Pugliese Ciaccio, Catanzaro, Chief: Rita Santoro. - Centro di Riferimento Regionale per le Malattie Emorragiche e Trombotiche Ereditarie in età pediatrica, A.O.U Città della Salute e della Scienza, Torino, Chief: Maria Messina. - Centro Regionale Malattie Emorragiche e Trombotiche, Ospedale San Bortolo, ULSS 6 Vicenza, Chief: Giancarlo Castaman. - Centro Regionale per le malattie del sangue - Struttura di riferimento per le malattie rare, ULSS 8 Veneto, Ospedale Civile, Castelfranco Veneto, Chief: Giuseppe Tagariello. - Agenzia per l'Emofilia, AOU Careggi, Firenze, Chief: Massimo Morfini. - Servizio Malattie Emorragiche e Trombotiche, Università Cattolica S. Cuore - Policlinico Universitario A. Gemelli, Roma, Chief: Raimondo De Cristofaro. - Centro Emofilia, U.O. Oncoematologia Pediatrica, Ospedale dei Bambini, Spedali Riuniti di Brescia, Chief: Lucia Dora Notarangelo. - U.O.S. Interdipartimentale di Emostasi, U.O. Ematologia con trapianto, AOU Policlinico P. Giaccone, Palermo, Chief: Sergio Siragusa. - Centro Emofilia e Malattie della Coagulazione, Arcispedale Santa Maria Nuova, Reggio Emilia, Chief: Ido Iori. - Centro Coagulopatie Emorragiche Congenite - Trombofilia, ASUR Area Vasta n° 3, Macerata, Chief: Isabella Cantori. - Centro Emostasi e Trombosi, AO SS. Antonio e Biagio e Cesare Arrigo, Alessandria, Chief: Laura Contino. - U.O.S.D. Centro Emofilia, Malattie Emorragiche e Trombotiche Congenite, ASL Pescara, Chief: Alfredo Dragani. - U.O.S. Gestione e Organizzazione Funzione HUB Emofilia, AOU di Parma, Chief: Anna Rita Tagliaferri. - Centro Emofilia, AOU di Padova, Chief: Ezio Zanon. - Centro Emofilia, ASLTO4, Ivrea, Chief: Grazia Delios. - Centro di Riferimento Regionale per le Malattie Emorragiche, IRCCS G. Gaslini, Genova, Chief: Angelo Claudio Molinari. Appendix 2 Peer professionals involved in the evaluation process of the AICE programme of professional accreditation - Francesco Baudo, physician, expert in bleeding disorders - Elio Boeri, physician, expert in bleeding disorders - Cesare Manotti, physician, expert in bleeding disorders - Vincenzo Trapani Lombardo, physician, expert in bleeding disorders - Ivana Menichini, senior quality systems consultant Blood Transfus 2014; 12 Suppl 3: s505-9 DOI 10.2450/2014.0331-13s s509 ORIGINAL ARTICLE The Italian institutional accreditation model for Haemophilia Centres Gabriele Calizzani1, Fabio Candura1, Ivana Menichini2,3, Romano Arcieri2, Giancarlo Castaman4, Alessandro Lamanna5, Maria R. Tamburrini6, Antonio Fortino7, Monica Lanzoni1,8, Samantha Profili1, Simonetta Pupella1, Giancarlo M. Liumbruno1, Giuliano Grazzini1 1 National Blood Centre, National Institute of Health, Rome; 2Italian Federation of Haemophilia Societies (FedEmo), Rome; 3Necstep Studio Associato, Modena; 4Department of Haematology and Haemophilia and Thrombosis Centre, San Bortolo Hospital, Vicenza; 5National Agency for the Regional Healthcare Systems, Rome; 6Blood and Transplant Unit, Ministry of Health, Rome; 7National Institute for Health, Migration and Poverty, Rome; 8IRCCS Ca' Granda Foundation Maggiore Policlinico Hospital, Milan, Italy Background. In Italy, basic health needs of patients with inherited bleeding disorders are met by a network of 50 haemophilia centres belonging to the Italian Association of Haemophilia Centres. Further emerging needs, due to the increased life expectancy of this patient group, require a multiprofessional clinical management of the disease and provide a challenge to the organisation of centres. In order to achieve harmonised quality standards of haemophilia care across Italian Regions, an institutional accreditation model for haemophilia centres has been developed. Material and methods. To develop an accreditation scheme for haemophilia centres, a panel of experts representing medical and patient bodies, the Ministry of Health and Regional Health Authorities has been appointed by the National Blood Centre. Following a public consultation, a technical proposal in the form of recommendations for Regional Health Authorities has been formally submitted to the Ministry of Health and has formed the basis for a proposal of Agreement between the Government and the Regions. Results. The institutional accreditation model for Haemophilia Centres was approved as an Agreement between the Government and the Regions in March 2013. It identified 23 organisational requirements for haemophilia centres covering different areas and activities. Discussion. The Italian institutional accreditation model aims to achieve harmonised quality standards across Regions and to implement continuous improvement efforts, certified by regional inspection systems. The identified requirements are considered as necessary and appropriate in order to provide haemophilia services as "basic healthcare levels" under the umbrella of the National Health Service. This model provides Regions with a flexible institutional accreditation scheme that can be potentially extended to other rare diseases. Keywords: standards and criteria, accreditation system, haemophilia care. Introduction Among the inherited bleeding disorders (IBDs), haemophilia A and B are the most known forms affecting worldwide around 1 in 6,000 and 1 in 30,000 males, respectively1,2. According to the Italian Association of Haemophilia Centres (AICE), there are 50 Haemophilia Treatment Centres (HCs) across Italy, meeting the basic needs for diagnosis, treatment, emergency management, home treatment and care of patients with haemophilia and other IBDs. In 2008, AICE launched a voluntary professional accreditation project entitled Improve AICE3. According to the results of 21 HC audits, the AICE professional accreditation programme proved to be effective for promoting good clinical practice4. However, as HCs differ widely in term of size, expertise and services provided, the availability and quality of haemophilia care delivery across Italian Regions is not homogeneous; this finding is confirmed by the results of surveys carried out by patient organisations5,6. The emerging needs of patients with IBDs require a multi-professional clinical management of haemophilia patients and provide a challenge to HC organisation7. In order to achieve harmonised quality standards of haemophilia care across Italian Regions, an institutional accreditation model for HCs has been developed, driven by each Regional Authority (RA), through which public and private facilities are authorised to provide services in Blood Transfus 2014; 12 Suppl 3: s510-4 DOI 10.2450/2014.0058-14s s510 © SIMTI Servizi Srl Institutional Accreditation Model for Haemophilia Centres the name, and on behalf of the National Health Service (NHS)8,9. General accreditation criteria specify the structural, technological and organisational requirements of health providers whose compliance is periodically verified by regional inspection systems10. Haemophilia and other IBDs meet the definition of rare disease provided by the European Commission as they are life-threatening or chronically debilitating diseases whose prevalence is less than 5 over 10,000 persons in the European Union11. In Italy, the field of rare diseases (RDs) is regulated by a specific legislative framework and policies. A RDs network was established with the Ministerial Decree (MD) 279/2001, and reasserted by the Agreement between the Government and the Regions of 10th of May 2007, in order to support the prevention, surveillance, diagnosis and treatment of RDs patients 12,13. The RDs network comprises hospital-based Centres of Reference (CoR)14, designed by each RA; this network has not been included in any institutional accreditation process to date. In Italy, haemophilia knowledge and health care has a very long history15 and comprehensive treatment centres as well as home-treatment programmes have been in place since 197016-18. Therefore, a long-standing HC network was already in place when the MD 279/01 (National network of rare diseases) was adopted and many of the 50 HCs now belong to the RDs network. This paper aims to provide a description of the Italian institutional accreditation model for HCs approved with the Agreement between the Government and the Regions no. 66 in March 201319. An outline of the complex process required and the role of multiple actors involved for its development is also provided. Materials and methods With the aim of promoting higher and harmonised standards of haemophilia care across Regions, the Italian Federation of Haemophilia Societies (FedEmo, www. fedemo.it) proposed the development of an institutional accreditation scheme for HCs to the Health Commission of the Permanent Conference for relations among the Government and the Regions (HCCGR). HCCGR appointed the Italian National Blood Centre (NBC, www.centronazionalesangue.it) to investigate the matter and to develop a technical proposal. In order to meet this commitment, the NBC convened a panel of experts belonging to medical (AICE) and patient (FedEmo) bodies, the Ministry of Health (MoH, www.salute.gov. it) and Regional Health Authorities (RHAs). The panel conducted a literature review from institutional sources in order to collect all the available scientific and regulatory references related to requirements, recommendations, as well as general and specific certification/accreditation systems. An analysis was conducted on critical issues specifically related to HC organisation and service management, that were not included in the general accreditation process carried out by Regions for health care centres. Particular concern was given to organisational requirements of HCs, since structural and technological standards were already considered and assessed in the institutional and voluntary/professional accreditation processes, respectively. After a public consultation, held in April 2011, a technical proposal in form of recommendations for RHAs was produced by the NBC and formally submitted to the MoH in February 2012. The MoH launched a further technical consultation process involving internal actors such as the Department of Health Care Planning (RDs Unit), and other institutions such as the National Medicines Agency (AIFA, www.agenziafarmaco.gov.it) and the National Institute of Health (ISS, www.iss.it). The proposal was reviewed after a careful evaluation of the legal nature of the document to be adopted (recommendations or more binding requirements) and of the current legislation and policies on RDs, and taking into account clinical disease-specific pathways to be adopted by RHAs as Basic Levels of Care. The document became the basis for a proposal of an Agreement between the Government and the Regions. The Agreement was approved in March 2013 and the Italian Regions had six months to transpose it into their legislation19. Results The panel of experts convened by the NBC identified two levels of organisational requirements related to different functions assigned to HCs: one level for HCs providing basic haemophilia services and the other for HCs offering a more integrated and specialised multi-professional approach to patients. However, while 23 organisational requirements for basic HCs were substantially confirmed in the final document, 4 additional requirements for the Comprehensive HCs were amended since the Regions decided about the opportunity to recognise only one level of HCs and to adopt an unique accreditation system for it. The organisational requirements for basic HCs cover different areas and activities, such as record-keeping, patient awareness and safety, treatment programme, periodical check-up, home treatment plan, access to laboratories, information, training and quality management. In particular, they include the following activities: 1- preparation and updating of patient records; 2- formalisation of the diagnosis of coagulopathy, detailing a specific set of information; 3- drawing up of the certificate of diagnosis of rare disease, according to the procedures defined by the Regions, valid nationally, in order to release Blood Transfus 2014; 12 Suppl 3: s510-4 DOI 10.2450/2014.0058-14s s511 Calizzani G et al the certificate of exemption from co-payments of healthcare services provision by the Local Health Authority; 4- production of a detailed report in line with specific requirements while formalising the diagnosis of coagulopathy; 5- issuing of a treatment plan containing the personalised prescription of clotting factor concentrate to be used, with dosage and any other prescription the clinician deems appropriate; 6- issuing for each patien, of a sheet containing summary information about the therapeutic product to be used including the recommended dosages and procedures to be considered in the event of minor and major bleeding episodes, and practical references about services, patient rights and how to access them; 7- adoption of specific protocols that define the criteria to be used for research, titration and possible followup of inhibitor; 8- adoption of appropriate protocols in collaboration with the network of genetics laboratories aimed at ensuring the diagnosis of the patient's family members, including genetic counseling and pre-and postnatal genetic diagnosis; 9- for each patient, definition and regular updating of a specific treatment programme (including product, dosage, treatment regimen, the reasons for the choice of treatment and eventual home therapy modality in collaboration with the local health services) with informed consent from the patient; 10-provision of patients with written instructions and instruments for the recording of the infusions of therapeutic products in home therapy; 11- evaluation of the suitability of each patient regarding the self-infusion practice; 12-systematic registration of data regarding the home therapy of each patient infusion of therapeutic products carried out in home therapy, at the HCs or in other health facilities involved in the therapeutic pathway; 13-planning and organisation of periodical check-ups; 14-adoption of protocols for the multidisciplinary assessment of patients with complications associated with IBDs (inhibitor, arthropathy, chronic liver disease, HIV infection); 15-adoption of procedures for the procurement of therapeutic products, in order to ensure continuity of care and timely treatment of bleeding episodes and emergencies, in cooperation with the pharmacies; 16-delivering of multi-disciplinary treatment programmes based on written protocols, planned with specialised services; 17-access to laboratories performing a predetermined set of coagulation tests: Prothrombin time (PT); activated Partial Thromboplastin Time (aPTT); fibrinogen dosage; thrombin time (TT); mixing tests (PT, aPTT, TT; test for the research of lupus anticoagulant; factor VIII/IX dosage; research of FVIII/IX inhibitor; von Willebrand Factor Antigen (VWF:Ag); von Willebrand Factor Ristocetin Cofactor (VWF:RCo); Coagulation factors dosage: II, V, VII, X, XI, XII, XIII; study of platelet function through platelet aggregation induced by ADP, collagen, epinephrine, arachidonic acid, ristocetin; 18-access to laboratories for coagulation tests that guarantee the availability of results and reports in a timeframe compatible with the urgency of the request; 19-availability to patients and their families of appropriate updated information related to the characteristics of haemophilia and other IBDs, as well as issues related to the daily life of patients with haemophilia (PWH); 20-organisation of periodical events for informing and training the patients with IBDs and their families, including courses for home therapy, in collaboration with other HCs and local patient associations; 21-organisation of periodical training addressed to personnel of specialised services (emergency service, general practitioners and paediatricians, pharmaceutical services, etc.); 22-participation in registries related to IBDs, in compliance with current legislation regarding the protection of personal data; 23-conduct of systematic clinical and quality audits aimed at assessing compliance with established policies and procedures, and planning of specific quality improvement objectives related to clinical and organisational processes, also through the involvement of patients and their associations. Therefore, in the first version of the document, 2 levels of haemophilia care delivery were originally developed by the panel of experts convened by NBC and inspired by the Hub and Spoke organisational model of haemophilia care20. In this context, the "Hub" centre performs high resource and competence demanding activities and is linked to a network of "Spoke" centres providing basic services close to where the patient lives. This model would offer the opportunity to balance access to health care and sustainability. In addition, it would allow Hub centres to deal with a minimum number of patients necessary to maintain the multi-disciplinary and specialised expertise required for haemophilia patient management. Thus, four additional requirements/ activities were identified for Comprehensive HCs (Hubs): coordination of a network of hospital facilities providing comprehensive care, 24-hours availability of a physician with experience in the treatment of Blood Transfus 2014; 12 Suppl 3: s510-4 DOI 10.2450/2014.0058-14s s512 Institutional Accreditation Model for Haemophilia Centres coagulation disorders, 24-hours access to a laboratory providing a set of specific tests within agreed turn around times; 24-hours availability of an advisory service to patients and their families, as well as other professionals and caregivers. However, after the consultation process, according to the Agreement between the Government and the Regions, RAs decided, in order to achieve greater autonomy in the organisation of health services, that these functions should be ensured through addressing indications provided in the context of current health planning procedures. Discussion In Italy, a designation process of CoR based on a disease-specific accreditation scheme had not been developed previously. The process that led to the final improvement of the Italian HC accreditation model proved to be complex and time consuming. Different opinions had to be compared and addressed, in particular on the feasibility of developing a specific process of accreditation for RDs. Other challenges are related to the large numbers of actors involved in the process and to the specific features of the relationship between Central State and Regions, influenced by political forces and characterised by a continuous negotiation effort. The experience developed in Italy in the accreditation of HCs -both institutional and professional- provided the inspiration and drove the development of European standards21 in the context of the European Haemophilia Network project (EUHANET, www.euhanet.org)22. The two above-mentioned accreditation models comprised the main reference documents for the production of the European Guidelines for the certification of HCs, supplemented by other European national experiences and models23,24 (e.g. Belgium, the Netherlands, United Kingdom) and the European principles of haemophilia care20. The development of European reference networks in the MS is one of the core provisions of the cross-border health care directive25. In particular, article 12 of this directive describes the general aims and objectives, as well as peculiarities, that reference networks should meet. The European Union Committee of Experts on Rare Diseases (EUCERD)26, which supports the European Commission with the preparation and implementation of Community activities in the field of RDs, has issued, among others, specific recommendations on centres of expertise27 (CoE) and European Reference Networks28. In particular, such centres should be compliant with the EUCERD recommendations for quality criteria for CoE in RDs and Directive 2011/24/EU, mentioned above. Each MS should establish a procedure to define and approve designation criteria along with transparent designation and evaluation processes. The institutional HC accreditation model could be regarded as a "pilot study" in the field of accreditation and designation of CoR for RDs. This experience has shown that an earlier involvement in the process of RD experts and policy makers would have facilitated the process and provided the accreditation model with better flexibility and acceptability. Indeed, it is the opinion of the authors that the specificities linked to haemophilia and other IBDs (number of patients, clinical history of the disease, pre-existing network of HCs, treatments costs, etc.) permit the development of a specific accreditation system for this group of diseases. However, it is necessary to introduce a continuous process of data collection on the model implementation to support decision making processes. It cannot be excluded that in the future, based on the evidence collected, the system of accreditation of HCs might be considered within a broader dedicated system of accreditation for all RDs with consideration of a set of common generic requirements for all CoR for RDs, and a set of specific requirements for each disease or group of RDs. Conclusions The Italian institutional accreditation system aims to achieve harmonised quality standards across Regions and to implement continuous improvement efforts, certified by rigorous and objective regional inspection systems. The identified requirements are considered as necessary and appropriate in order to provide haemophilia services as "basic/essential healthcare levels" under the aegis of the NHS. This system is the outcome of a long and complex consultation process involving experts from RAs and national institutions (NBC, MoH, ISS, AIFA, etc.), with the participation of representatives of patient associations (FedEmo) and learned scientific societies (AICE). All types of facilities providing haemophilia services are eligible to be involved in the accreditation model, regardless of the level, intensity and type of services provided. It is the authors' opinion that this model could provide Regions with a flexible institutional accreditation scheme for HCs which can be potentially extended to other RDs. Regions, in fact, could adapt the requirements to their specific context and develop further more stringent requirements, for instance by taking into account EUHANET recommendations on the minimum number of severe patients followed by HCs. To date, 4 RAs out of 21 (Emilia-Romagna, Liguria, Autonomous Provinces of Trento and Bolzano) have already formally adopted it. A wider implementation will provide useful information in order to adapt and improve the model. The Authors declare no conflicts of interest. Blood Transfus 2014; 12 Suppl 3: s510-4 DOI 10.2450/2014.0058-14s s513 Calizzani G et al References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) Stonebraker JS, Bolton-Maggs PHB, Michael Soucie J et al. A study of variations in the reported haemophilia A prevalence around the world. Haemophilia 2010; 16: 20-32. Stonebraker JS, Bolton-Maggs PHB, Michael Soucie J et al. A study of variations in the reported haemophilia B prevalence around the world. Haemophilia 2012; 18: e91-4. Calizzani G, Vaglio S, Arcieri R et al. Models for institutional and professional accreditation of haemophilia centres in Italy. Haemophilia 2013; 19: e248-55. Mannucci PM, Menichini I. A certification/accreditation model for Haemophilia Centres in Italy. Blood Transfus 2014; 12 (Suppl 3): s505-9. Arcieri R, Molinari AC, Farace S et al. Present and future challenges in the treatment of haemophilia: the patient's perspective. Blood Transfus 2013; 11 Suppl 4: s82-5. Arcieri R, Molinari AC, Farace S. Uncovered needs in the management of inherited bleeding disorders' in Italy. Blood Transfus 2014; 12 (Suppl 3): s553-6. Coppola A, Santoro C, Franchini M et al. Emerging issues on comprehensive hemophilia care: preventing, identifying, and monitoring age-related comorbidities. Semin Thromb Hemost. 2013; 39: 794-802. Decreto del Presidente della Repubblica 14 gennaio 1997: "Approvazione dell'atto di indirizzo e coordinamento alle regioni e alle province autonome di Trento e di Bolzano, in materia di requisiti strutturali, tecnologici ed organizzativi minimi per l'esercizio delle attività 8 sanitarie da parte delle strutture pubbliche e private". Di Stanislao F, Liva C, editors. L'Accreditamento dei Servizi Sanitari in Italia. Turin, Italy: Centro Scientifico Editore; 1998. Fortino A, Di Stanislao F. Institutional accreditation of Health Services in Italy: the long road to quality. Blood Transfus 2014; 12 (Suppl 3): s551-3. European Parliament and Council. Regulation (EC) 141/2000 of the European Parliament and of the Council of 16 December 1999 on orphan medicinal products. Official Journal 2000; L 18:1-5. Available at http:// e u r l e x . e u r o p a . e u / L e x U r i S e r v / L e x U r i S e r v. d o ? u r i = OJ:L:2000:018:0001:0005:en:PDF. Accessed on 15/01/2014. Decreto Ministeriale 18 Maggio 2001, n. 279. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124. Gazzetta Ufficiale n. 160, 12/07/2001. Suppl. Ordinario n.180/L. Accordo, ai sensi dell'articolo 4 del decreto legislativo 28 agosto 1997, n. 281, tra il Governo, le Regioni e le Province autonome di Trento e Bolzano sul riconoscimento di Centri di coordinamento regionali e/o interregionali, di Presidi assistenziali sovraregionali per patologie a bassa prevalenza e sull'attivazione dei registri regionali ed interregionali delle malattie rare. Rep. n. 103/CSR del 10 maggio 2007. Available at: http://www.centronazionalesangue.it/sites/default/files/ accordo_csr_13.03.2013_gu_n._107_09.05.2013_assistenza_ mec.pdf. Accessed on 15/01/2014. Taruscio D, Agresta L, Amato A, et al. The Italian National Centre for Rare Diseases: where research and public health translate into action. Blood Transfus 2014; 12 (Suppl 3): s591-605. Mannucci PM, Ruggeri ZM. Hemophilia care in Italy. Thromb Haemost. 1976; 35: 531-6. 16) Franchini M. The modern treatment of haemophilia: a narrative review. Blood Transfus 2013; 11: 178-82. 17) Franchini M, Mannucci PM. Past, present and future of hemophilia: a narrative review. Orphanet J Rare Dis 2012; 7: 24. 18) Franchini M, Mannucci PM. Present and future challanges in the treatment of haemophilia: a clinician's perspective. Blood Transfus 2013; 11 (Suppl 4): s77-81 19) Official Journal of Italian Republic no. 107 May 9th, 2013. Accordo, ai sensi dell'articolo 4 del decreto legislativo 28 agosto 1997, n.281, tra il Governo, le Regioni e le Province autonome di Trento e Bolzano sulla definizione dei percorsi regionali o interregionali di assistenza per le persone affette da Malattie Emorragiche Congenite (MEC). Rep Atti n 66/CSR del 13 marzo 2013) Available at http:// www.centronazionalesangue.it/sites/default/files/accordo_ csr_13.03.2013_gu_n._107_09.05.2013_assistenza_mec.pdf. Accessed on 16/02/2014. 20) Colvin BT, Astermark J, Fischer K et al. European Principles of Haemophilia Care. Haemophilia 2008; 14, 361-74. 21) Giangrande P, Calizzani G, Menichini I et al. The European standards of Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s525-30. 22) Makris M, Calizzani G, Fischer K et al. The European Haemophilia Network (EUHANET). Blood Transfus 2014; 12 (Suppl 3): s515-8. 23) Hermans C. Haemophilia Centre certification system across Europe: the Belgian experience. Blood Transfus 2014; 12 (Suppl 3): s497-500. 24) Leebeek FWG, Fischer KQuality of haemophilia care in the Netherlands: new standards for optimal care. Blood Transfus 2014; 12 (Suppl 3): s501-4. 25) Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare. Available at: http://eur-lex.europa. eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011:088:0045:006 5:en:PDF. Accessed on 15/01/2014. 26) European Union Committee of Experts on Rare Diseases (EUCERD). Available at: http://www.eucerd.eu/ Accessed on 18/02/2014. Accessed on: 15/01/2014. 27) European Union Committee of Experts on Rare Diseases (EUCERD). Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States (24 October 2011). Available at http://www.eucerd.eu/upload/file/ EUCERDRecommendationCE.pdf Accessed on 18/02/2014. 28) European Union Committee of Experts on Rare Diseases (EUCERD). Recommendations on Rare Disease European Reference Networks (RD-ERNS) (31 January 2013) Available at http://www.eucerd.eu/?post_type=document&p=2207 Accessed on 18/02/2014. Correspondence: Gabriele Calizzani National Blood Centre, National Institute of Health Via Giano della Bella 27 00162, Rome, Italy e-mail: areaplasma.cns@iss.it Blood Transfus 2014; 12 Suppl 3: s510-4 DOI 10.2450/2014.0058-14s s514 REVIEW The European Haemophilia Network (EUHANET) Michael Makris1,2, Gabriele Calizzani3, Kathelijn Fischer4, Alexander Gatt5, Estelle Gilman1, Robert Hollingsworth6, Thierry Lambert7, Riitta Lassila8, Pier Mannuccio Mannucci9, Flora Peyvandi10, Jerzy Windyga11 1 Department of Cardiovascular Science, University of Sheffield, Sheffield, United Kingdom; 2Sheffield Haemophilia and Thrombosis Centre, Sheffield, United Kingdom; 3National Blood Centre, National Institute of Health, Rome, Italy; 4Van Creveldkliniek and Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht, The Netherlands; 5Mater Dei Hospital, Msida, Malta; 6Medical Data Solutions and Services Ltd, Manchester, United Kingdom; 7Treatment Centre of Haemophilia, Bicêtre AP-HP Hospital, Paris, France; 8 Helsinki University Hospital, Helsinki, Finland; 9Scientific Direction, Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Milan, Italy; 10Fondazione IRCCS Ca' Granda, Ospedale Maggiore Policlinico, Angelo Bianchi Bonomi Haemophilia and Thrombosis Centre, Milan, Italy; 11Institute of Haematology and Transfusion Medicine, Warsaw, Poland Introduction Haemophilia A and B are rare inherited bleeding disorders due to reduced factor VIII (FVIII) or factor IX (FIX) activity, occurring in 1 in 10,000 and 1 in 50,000 of the population respectively1,2. Several other bleeding disorders such as deficiencies of factors I, II, V, VII, X, XI and XIII are even rarer. When the deficiency is severe these disorders present with spontaneous bleeding whilst for milder disorders traumatic bleeding is observed3. When bleeding occurs patients are treated with clotting factor concentrates which can be plasma derived or recombinant. Individuals with inherited bleeding disorders are cared for in Haemophilia Centres. There is major disparity in patient access to Haemophilia Centres throughout Europe4, although it must be appreciated that this publication was based on data from the individual country patient organisations and was not based on national registries. There is a need for harmonisation of the data available in care centres, national data sources and patient organisations and these activities are planned to be improved by the European Haemophilia Network (EUHANET) project. There is also variation in the number of Haemophilia Centres within European countries and whilst in some there are over 80 Haemophilia Centres in others there is only a single centre. The use of clotting factor concentrates has been associated with major adverse effects. Patients treated with plasma derived clotting concentrates prior to 1985 had an almost 100% risk of being infected with hepatitis C (HCV) and a 30-60% risk of Human Immunodeficiency Virus (HIV) infection5. Although the HCV/HIV viruses were eliminated following the introduction of viral inactivation, improvements in diagnostic tools used for the biological qualification of blood donations and the use of recombinant concentrates, other adverse events such as alloantibodies to FVIII or FIX remain6. The rarity of these disorders makes it difficult to determine the precise frequency of the adverse events because large numbers of patients are required which are not available in single centres. To overcome this problem, the European Haemophilia Safety Surveillance (EUHASS) system was set up in 2008 7. This was a collaboration of over 70 European Haemophilia Centres in 26 countries which agreed to prospectively report adverse events occurring in their patients. The project was funded by the European Commission with pharmaceutical industry support. The EUHASS project demonstrated the willingness of these Haemophilia Centres to work together so the EUHANET was set up. This is a collaboration in four separate areas, the certification of Haemophilia Centres, the set up of a haemophilia website, the expansion of the EUHASS system and the establishment of a prospective project on afibrinogenemia and FXIII deficiency. Organisation of the project The lead partner of the EUHANET project is the University of Sheffield in the United Kingdom. The other main partners are the European Haemophilia and Allied Disorders organisation, the European Haemophilia Consortium, the University Medical Centre Utrecht, Fondazione IRCCS Ca' Granda in Milan and Medical Data Solutions and Services Ltd in Manchester. In addition there are 84 collaborating partners in 26 European countries. The project has eight work packages and is overseen by a steering committee with a representative from each of the main partners as well as four representatives from the collaborating partners. EUHANET is funded by the European Commission Health Programme through the Executive Agency for Health and Consumers (EAHC) with co-financing from 12 pharmaceutical manufacturers. Blood Transfus 2014; 12 Suppl 3: s515-8 DOI 10.2450/2014.0008-14s © SIMTI Servizi Srl s515 Makris M et al Certification of Haemophilia Centres There is wide variation in the availability of Haemophilia Centres in different countries as well as in the range of services provided by individual centres. Many names are used by centres such as Haemophilia Centre, comprehensive care centre, Haemophilia Treatment Centre, Haemophilia Reference Centre, national haemophilia centre, etc. There is no agreed definition of what constitutes a haemophilia centre and whilst some centres care for more than 350 patients with severe haemophilia, others have less than 5 patients. Furthermore the laboratory support of haemophilia centres varies enormously. Patients with inherited bleeding disorders have no way of knowing how comprehensive the care provided by a particular haemophilia centre is. This knowledge is important both for patients within a geographical region where several haemophilia centres are located, as well as for patients from other countries or areas who are travelling and are looking for emergency care. As a haemophilia community we have been looking at standardising the labelling of European Haemophilia Centres and categorising them. At the same time the European Commission has provided guidance for countries to develop centres for rare diseases8. Therefore a part of the EUHANET project is the standardisation of the labelling of Haemophilia Centres in Europe. The certification work package undertook the development of this work and the process is described in the other manuscripts in this supplement of the Blood Transfusion journal. Briefly, the current regulations and processes within all European countries were reviewed and a document of standards of haemophilia care was prepared. Extensive consultation during several stages of the process led to modification of the document. The final standards document was approved in May 2013 and it was launched at a meeting in Rome in July 20139. Two types of Haemophilia Centres are recognised by the standards document, the European Haemophilia Treatment Centre (EHTC) and the European Haemophilia Comprehensive Care Centre (EHCCC). Because of the length of the standards document, a pro-forma of the key areas was developed for centres to use when applying for certification. This asks for the number of patients registered, the services offered, the emergency care facilities as well as the laboratory backup. Both the standards document and the application pro-forma are available on the EUHANET project website (www.euhanet.org). The application process was launched in December 2013 and any Haemophilia Centre in Europe can apply for certification into EHTC or EHCCC. Although the standards for the two types are different, there are certain minimum requirements that have to be satisfied before one of these two titles are awarded to a centre. Once an application is made, it is reviewed by a five member committee which has representatives from medical and nursing staff as well as patients. The certification process is based on data supplied by the centres and there are no site visits to check the accuracy of the data. Because of this, several parts of the application form will be made publically available. This is a first step and it is anticipated that in future audit visits will be incorporated into the process, although political, geographical and language differences have to be addressed to achieve this. Haemophilia Central website Although there is a lot of information about inherited bleeding disorders on the web, it is spread over many sites and its accuracy is often unclear. In the EUHANET project we set out to develop a website with all the information in a single place. The site is called Haemophilia Central and can be found at www. haemophiliacentral.org. Several components will be developed during the project but those currently publically available are: 1. News - this is produced in collaboration with Dr Uwe Schlenkrich. The site is regularly updated with haemophilia and other bleeding disorder related news; 2. Guidelines - here readers can select guidelines by subject and language. For most guidelines the reader is redirected to the site of the original publication; 3. Clinical trials - this is a search engine for any trials registered on www.clinicaltrials.gov in the field of acquired or inherited bleeding disorders; 4. Concentrate directory - this section contains details of all the available clotting factor concentrates in Europe. Once a concentrate is selected, the details of the manufacturer, production and characteristics of the product as well as publications relating to the products are provided; 5. Database of centres and organisations. A fully functional database assists the user in locating Haemophilia Centres and patient, doctor, nurses and physiotherapy organisations based in Europe; 6. Frequently asked questions section for queries relating to the EUHANET project as well as to bleeding disorders more specifically; 7. Links - contains links to the journals Blood, Haemophilia and Journal of Thrombosis and Haemostasis, and to an information site for very rare coagulation disorders. Haemophilia Centre Locator (www.hclocator.org) The EUHANET project has developed a search engine that can be accessed by all devices including Blood Transfus 2014; 12 Suppl 3: s515-8 DOI 10.2450/2014.0008-14s s516 The European Haemophilia Network personal computers, tablets and mobile phones using any software. Once a user accesses www.hclocator. org they can enter any address or choose their current location. The site generates a map with the nearest five Haemophilia Centres. Clicking on the name of any of these centres will give information on location and phone numbers about how to get emergency care from the centre during normal working hours or in an emergency. Currently the system works only for Europe but it is intended to expand it so it covers Haemophilia Centres worldwide. European Haemophilia Safety Surveillance (EUHASS) The EUHASS project began on 1st October 2008 and currently 84 European Haemophilia Centres from 26 countries are participating. A report on the initial experience has been published7. The original EUHASS project has been extended and incorporated into the EUHANET in 2012. Prior to participation all centres have to obtain clearance from the Ethics Committee (Institutional Review Board) of their organisation. All adverse events are reported anonymously online either when they occur or within a maximum of three months. Every three months all centres have to actively sign off the quarter even if no events have occurred in their centre. The patients included in the surveillance are those with inherited deficiency of factors I, II, V, VII, VIII, IX, X, XI, XIII, von Willebrand disease, Glanzmann thrombasthenia, Bernard Soulier syndrome, platelet storage pool disease, acquired haemophilia and acquired von Willebrand disease. The events reported are: 1. acute or allergic events; 2. transfusion transmitted infections; 3. inhibitors; 4. thromboses; 5. malignancies; 6. deaths; 7. unexpected poor efficacy; 8. any other possible adverse event. For each of the above events limited details regarding the event such as the timing of the last clotting factor exposure and exposure days are also collected. Annually the participating centres report the total number of patients registered at their centre, how many of these have severe disease and how many were treated with concentrate over the previous year. Furthermore the centres report how many patients received each specific concentrate and how many of these patients had severe disease. This information allows the determination of the rates of adverse events per 1,000 treatment years. The rates of inhibitors in previously untreated patients is traditionally calculated by following a cohort of severely affected patients from first treatment to their 50th exposure day, but such studies take a long time to complete. EUHASS determines the inhibitor rate in previously untreated patients using a novel method which is based on number of patients reaching the 50th exposure day during a specific year10. Prospective rare diseases database The evidence base for the bleeding disorders other than the haemophilias is weak due to the rarity of the disorders and the fact that most patients are to be found in countries without a strong background in research. A significant advance has been the collaboration of several Haemophilia Centres in the previously funded EAHC project led by Professor Flora Peyvandi to set up the Rare Bleeding Disorders Database (EN-RBD)11. This database obtained retrospective information on the non-haemophilic RBD. Data was collected on demographics, phenotype, genotype, bleeding manifestations, treatment and their complications. Personal identification data were not entered. A problem with retrospectively collected data is bias and it would be desirable to collect prospective data. As part of the EUHANET project the EN-RBD database, now applied on a global scale (RBDD) has been revised to create the prospective RBDD (Pro-RBDD, http:// eu.rbdd.org), so that prospective information can be collected. Initially this database is collecting data on patients with deficiencies of fibrinogen and factor XIII. Over the three years of the EUHANET project there will be 6 data entry points per patient. Subsequently, prospective data will be collected for all RBD and the data will be used to design clinical trials of treatment modalities. Central laboratory testing for clotting factor levels and genotyping as well as an external laboratory quality control is provided. Acknowledgement This publication arises from the project EUHANET which has received funding from the European Union, in the framework of the Health Programme. Keywords: haemophilia, EUHANET, reference networks, European, certification. Funding and conflict of interest The EUHANET project is funded by the European Commission Health Programme through the Executive Agency for Health and Consumers (EAHC) (Project number 2011207) with co-financing from 12 pharmaceutical manufacturers. The Authors declare that the pharmaceutical companies co-financing this project are Baxter, Bayer, Biotest, BPL, CSL Behring, Grifols, Kedrion, LFB, NovoNordisk, Octapharma, Pfizer, SOBI/Biogen Idec. Blood Transfus 2014; 12 Suppl 3: s515-8 DOI 10.2450/2014.0008-14s s517 Makris M et al 9) References 1) 2) 3) 4) 5) 6) 7) 8) Stonebraker JS, Bolton-Maggs PH, Soucie JM, et al. A study of variation in the reported haemophilia A prevalence around the world. Haemophilia 2010; 16: 20-32. Stonebraker JS, Bolton-Maggs PH, Soucie JM, et al. A study of variations in the reported haemophilia B prevalence around the world. Haemophilia 2012; 18: e91-4. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia 2013; 19: e1-47. O'Mahony B, Noone D, Giangrande PL, Prihodova L. Haemophilia care in Europe - a survey of 35 countries. Haemophilia 2013; 19: e239-47. Makris M, Preston FE, Rosendaal FR, et al. The natural history of chronic hepatitis C in haemophiliacs. British Journal of Haematology 1996; 94: 746-52. Weinstein M, Makris M, Ludlam CA. Biovigilance and pharmacovigilance for haemophilia. Haemophilia 2010; 16 (Suppl 5): 17-21. Makris M, Calizzani G, Fischer K, et al. EUHASS: The European Haemophilia Safety Surveillance system. Thrombosis Research 2011; 127 (Suppl 2): S22-5. EUCERD Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States, 24 October 2011. Available at: http://www.EUCERD.eu/upload/file/ EUCERDRecommenda-tionCE.pdf. Accessed on 09/01/2014. International Meeting "Haemophilia Centre Certification Systems across Europe". Centro Nazionale Sangue. Available at: http://www.centronazionalesangue.it/newsbox/ seminario-malattie-emorragiche-congenite-mec. Accessed on 09/01/2014. 10) Fischer K, Lewandowski D, Van den Berg MH, Janssen MP. Validity of assessing inhibitor development in haemophilia PUPs using registry data. Haemophilia 2012; 18: e241-6. 11) Peyvandi F, Palla R, Menegatti M, et al. Coagulation factor activity and clinical bleeding severity in rare bleeding disorders: results from the European Network of Rare Bleeding Disorders. Journal of Thrombosis and Haemostasis 2012; 10: 615-21. Correspondence: Michael Makris Sheffield Haemophilia and Thrombosis Centre, Royal Hallamshire Hospital Glossop Road Sheffield, S10 2JF, United Kingdom e-mail: m.makris@sheffield.ac.uk Blood Transfus 2014; 12 Suppl 3: s515-8 DOI 10.2450/2014.0008-14s s518 ORIGINAL ARTICLE The methodology for defining the European Standards for the certification of Haemophilia Centres in Europe Fabio Candura1,2, Ivana Menichini1,3, Gabriele Calizzani1,2, Paul Giangrande1,4, Pier Mannuccio Mannucci5, Michael Makris6 1 European Haemophilia Consortium, Brussels, Belgium; 2National Blood Centre, National Institute of Health, Rome, Italy; 3Necstep Studio Associato, Modena, Italy; 4Oxford University Hospitals NHS Trust, United Kingdom; 5 Scientific Direction, IRCCS Ca' Granda Maggiore Policlinico Hospital Foundation, Milan, Italy; 6Department of Cardiovascular Science, University of Sheffield, Sheffield, United Kingdom Introduction. Work Package 4 Development of the standardisation criteria of the European Haemophilia Network project has the main objective of implementing a common and shared European strategy for a certification system for two levels of Haemophilia Centres: European Haemophilia Treatment Centres and European Haemophilia Comprehensive Care Centres in the Member States of the European Union. Materials and methods. An inclusive and participatory process for developing shared standards and criteria for the management of patients with inherited bleeding disorders has been carried out. The process has been implemented through four different consultation events involving the entire European community of stakeholders that significantly contributed in the drafting of the European Guidelines for the certification of Haemophilia Centres. Results. The Guidelines set the standards for the designation of centres that provide specialised and multidisciplinary care (Haemophilia Comprehensive Care Centres) as well as local routine care (Haemophilia Treatment Centres). Standards cover several issues such as: general requirements; patient care; advisory services; laboratory; networking of clinical and specialised services. Conclusions. The drafting of the European Guidelines for the certification of Haemophilia Centres was performed adopting a rigorous methodological approach. In order to build the widest possible consensus to the quality standards, the main institutional and scientific stakeholders have been involved. The resulting document will significantly contribute in promoting standardisation in the quality of diagnosis and treatment in European Haemophilia Centres. Keywords: standards, criteria, certification system, haemophilia care, EUHANET. Introduction One of the work streams of the European Haemophilia Network (EUHANET) project is the promotion of standardisation of the quality of diagnosis and treatment in European Haemophilia Centres. EUHANET is a project funded by the Executive Agency for Health and Consumers (EAHC) of the European Commission1. Within the EUHANET project, Work Package number 4 (WP4) Development of the standardisation criteria has the main objective of implementing a common and shared European strategy for a certification system for two levels of Haemophilia Centres (HCs): European Haemophilia Treatment Centres (EHTCs) and European Haemophilia Comprehensive Care Centres (EHCCCs) in the Member States of the European Union (EU MS). The resulting output was the European Guidelines for the certification of Haemophilia Centres2. The main objective of this article is to describe the methodology adopted for an inclusive and participatory process of developing shared standards and criteria for the management of patients with inherited bleeding disorders as a model to be considered for implementation by other groups of rare diseases. Materials and methods Operational steps for the development of the European Guidelines for the certification of Haemophilia Centres The different drafts of the European Guidelines for the certification of Haemophilia Centres (henceforth referred to as Guidelines) have been widely discussed with different European stakeholders (National Health Authorities, Health Professionals, Patient Organisations, EUHANET Project Partnership) at the time of several events and followed a very inclusive methodology of consultation using a bottom-up approach. Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s © SIMTI Servizi Srl s519 Candura F et al The activities of WP4 have been implemented through five steps: 1) review of literature on certification systems of HCs available in EU MS; 2) definition and sharing of principles and criteria to be considered for the development of requirement standards with EUHANET and other collaborating partners; 3) drawing up of a draft of the guiding document for consultation; 4) finalisation of the guiding document incorporating feedback received from the consultation process; 5) proposal of an evaluation system framework for EU HCs. Review of literature on certification systems of HCs available in EU MS The specific objective of step 1 was to conduct a survey of available standards and certification systems in EU MS. To reach this goal, and in particular to gather and validate information from official sources that may not be available through common search methods (published materials in official languages, grey literature, etc.), the WP4 team disseminated a preliminary questionnaire to 27 EU MS country stakeholders. 7 out of 17 returned questionnaires contained information about certification systems currently in place in the corresponding 7 countries. Definition and sharing of principles and criteria to be considered for the development of requirement standards with EUHANET and other collaborating partners In step 2, a cross-match analysis has been performed using all available materials, such as current national standards and certification systems as well as European key reference documents, including the European Haemophilia Principles of Care 3 and EUCERD recommendations4,5, with the aim of identifying common principles and criteria (i.e. scopes, approaches and rules) to be used as a basis for the draft of the Guidelines. The WP4 team selected 7 criteria such as types of structures involved, types of diseases to be considered, etc. and disseminated a Questionnaire for evaluating the level of agreement on each of them. Table I shows the list of proposed criteria. The Principles and Criteria Questionnaire was launched during the European Haemophilia Consortium Annual Conference held in Prague on the 28 th of October 2012. Thus, WP4 collected 56 questionnaires from 26 EU and non-EU countries. The analysis of free text comments and answers showed a very high Table I - List of criteria proposed. Criteria WP4 proposals 1 Types of structures involved Standards for two levels of HCs, in relation to different functions assigned: Comprehensive Care Centres (CCC - providing specialised and multidisciplinary care and functioning as tertiary referral Centres) and HTC (providing local routine care). 2 Types of diseases Haemophilia and allied inherited bleeding disorders, and acquired bleeding disorders 3 Age groups of patients Adults and paediatric patients. 4 Reference sources Standards developed on the basis of main European and national scientific evidence and recommendations. 5 Types of standards a) Only "organisational" standards. Standards do not aim to take the place of scientific guidelines. HCs are requested to develop clinical protocols in adherence to available national and European scientific references, and to provide evidence of their correct and systematic application and supervision. b) General standards for quality system management (according to EUCERD recommendations). c) Quality indicators to be monitored and evaluated by the HCs to confirm that the clinical outcome reaches the requested standards (according to EUCERD recommendations) and related targets. 6 Assessment Only standards that could objectively be assessed by objective evidence collected during audits. 7 Issues to be analysed and developed a) General organisational requirements - Quality of the facility - Information about the Centre - Organisation and staffing - Policies and procedures - Record-keeping and data collection - Personnel appraisal and continuing education - Equipment - Supply and management of therapeutic products, reagents and medical devices - Quality planning, evaluation and improvement - Participation in institutional registries/databases related to inherited and acquired bleeding disorders - Participation in clinical research b) Patient care - Awareness, information and education of patients and their families - Diagnosis and therapy of haemophilia and allied inherited bleeding disorders, and all the forms of acquired haemophilia - Periodic clinical and multi-disciplinary review - Genetic services c) Laboratory d) Network of clinical and specialised services acting in conjunction with the haemophilia team (physiotherapy, orthopaedic, psychological, dental care, social, infectious diseases, etc.) e) Formal agreements between the CCC and HTC and between the HTC and third parties whose services impact patient management. f) Recommended quality indicators (patient care) that should be routinely measured and evaluated by the HCs. Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s s520 Methodology for European Standards for Haemophilia Centres level of agreement on each of the criteria proposed. This agreement ranged from a minimum of 70% to a maximum of 90% on the total of the questionnaires received (Figure 1). Drawing up of a draft of the guiding document for consultation Once validated, the above-mentioned criteria were used in Step 3 in order to draw up the core draft of the Guidelines document through the following actions: i) definition of standards index and framework, ii) cross reference of EU MS standards, where available, and iii) development of standards. An example of the resulting table of cross reference of EU MS standards is shown in the excerpt below (Table II). From the set of standards developed, 11 key standards were selected for further consultation through the Questionnaire on key points for the production of standards for HCs and for the development of a related evaluation system, that was presented in Warsaw during the Annual Congress of the European Association for Haemophilia and Allied Disorders (EAHAD). In particular, the issues that were brought to the attention of the European community of stakeholders were related to: 1) proposal for the names of the European Haemophilia Centres: European Haemophilia Treatment Centres (EHTCs) and European Haemophilia Comprehensive Care Centres (EHCCCs); 2) criteria for the designation of a HC as an EHCCC or an EHTC - number of patients/severity: i) forty severe haemophilia patients for EHCCCs; ii) exclusion of patients with moderate and mild haemophilia, as well as those with von Willebrand disease and rare disorders, in the number of patients taken into consideration for EHCCC designation; iii) no minimum number of patients required for designation of EHTCs; 3) procedures for the designation of EHCCCs/EHTCs: i) validity of the certification (3 years); ii) designation of EHCCCs/EHTCs based upon selfassessment; 4) requirement standards: i) Provision of 24-h expert haemophilia medical cover for EHCCCs; ii) Provision of 24-h medical cover by formalised arrangements with other departments and/or designated EHCCCs for EHTCs; iii) Establishment of a formal relationship between EHTCs and EHCCCs; Figure 1 - Percentage distribution of answers for each of the seven principles/criteria proposed by the EUropean HAemophilia NETwork project - Work Package 4. Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s s521 Candura F et al Table II - Example of cross-match analysis of some of the relevant documents used as a basis for the drafting of the European guidelines for the certification of Haemophilia Centres6-8. EU principles of haemophilia care EU MS 1 EU MS 2 EU MS 3 EU MS 4 NA The cornerstone of the treatment of haemophilia is comprehensive care delivered by a multi-disciplinary and specialised team on a 24 hour basis. In practice this involves a core team consisting of the following personnel: - Haemophilia centre medical staff, who carry out routine and emergency treatment, … - Haemophilia nursing staff who co-ordinate much of the day to day treatment, … Art. 6 The organisation of treatment centre staff always includes the following functions performed by one or more persons meeting the conditions laid down in Artic. 7: 1) Physician coordinator. 2) Physician specialist in internal medicine. 3) Physician specialist in paediatrics. 4) Physician specialist in clinical biology. 5) …………………………. NA 0.2.1 The Executive Management of the Centre defines and formalises responsibilities, mandates and assigns functions within the organisation… EU MS n Standard WP4 (proposal) The cornerstone of the treatment of haemophilia and other related bleeding disorders is comprehensive care delivered by a multi-disciplinary and specialised team. 1.4.1 The core team members of an EHTC/EHCCC consist of the following personnel: - medical staff, who carry out routine and emergency treatment and follow-up clinical reviews; - nursing staff, who co-ordinate much of the day to day treatment and supplies of coagulation factor concentrates; - laboratory staff, who provide a diagnostic and factor replacement monitoring service. - …………………………………………………………………….. NA: not available iv) Guarantee of an integrated approach to patient multidisciplinary comprehensive care, also through a formal relationship between EHTCs and EHCCCs; v) For both EHCCCs and EHTCs, access to a laboratory that provides a minimum set of coagulation tests (Prothrombin time; activated Partial Thromboplastin Time; Thrombin time and mixing studies; Factor VIII and IX assays; Inhibitor screen; Fibrinogen and factor II, V, VII, X and XI assays; platelet aggregation; von Willebrand Factor multimers) and related monitoring, on the basis of formal agreements between the clinical and laboratory services; 5) availability of information related to EHTCs/EHCCCs on a public website. More than two hundred European stakeholders participated in the survey. Agreement on each key point was shown in the great majority of the questionnaires received, with the exception of key point no. 2 (Figure 2). On this point, although there was agreement in over 50% of the questionnaires received, the comments received pointed out that in small population countries this threshold could represent a discouraging limitation for EHCCC designation. Moreover, the vast majority of respondents agreed to establish a minimum threshold number of patients (10) for the designation of an EHTC. Finalisation of the Guiding document incorporating feedback received from the consultation process In Step 4, the Guidelines document was revised in light of the results of the consultation process taking into account all relevant comments received. A new version of the Guidelines was then made available for further, final consultation. The final release of the document was approved on the 7th of June 2013 and launched in Rome at the Italian National Institute of Health on the 11th of July 2013 during the International Meeting Haemophilia Centre Certification Systems across Europe9 and the round table Haemophilia Centres of Expertise in Europe at the European Parliament on 17th October 201310. Proposal of an evaluation system framework for EU HCs Finally, in Step 5 the WP4 team outlined the proposal of a framework for the evaluation of applications to be received by European HCs during WP5 activities. All the entire methodology about consensus building and consultation processes developed in EUHANET WP4 is represented in Figure 3. Results The European Guidelines for the certification of Haemophilia Centres set the standards for the designation of two levels of European HCs: European Haemophilia Comprehensive Care Centres, that provide specialised and multidisciplinary care and function as tertiary referral Centres, and European Haemophilia Treatment Centres, that provide local routine care. The standards apply to both adults and paediatric patients. Their focus is on organisational issues and covers: 1) general requirements (facility; general policy and objectives; information about the HCs; organisation and staffing; policies and procedures; record-keeping and data collection; personnel appraisal and continuing education; supply and management of therapeutic Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s s522 Methodology for European Standards for Haemophilia Centres Figure 2 - Percentage distribution of answers for each of the key points proposed in the EUropean HAemophilia NETwork project - Work Package 4. 2) 3) 4) 5) products, reagents and medical devices; quality planning, evaluation and improvement; participation in registries; participation in clinical research); patient care (awareness, information and education of patients and their families; diagnosis and therapy of haemophilia and other related bleeding disorders and all forms of acquired haemophilia; periodic clinical and multi-disciplinary review; genetic services; outcome indicators); advisory services; laboratory; networking of clinical and specialised services. Conclusions Figure 3 - Flowchart of the consultation processes developed in the EUropean HAemophilia NETwork project Work Package 4. The drafting of the European guidelines for the certification of haemophilia centres was performed adopting a rigorous methodological approach. The document came into being as a result of a synthesis of the experience accumulated by the EU MS on HC quality management and certification systems and European key reference documents (European Haemophilia Principles of Care, EUCERD recommendations). The drawing up of the Guidelines involved the main institutional and scientific stakeholders (EAHAD, EHC, EUHASS, EUHANET, EU and non-EU countries) in all the key steps of the project, in order to build Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s s523 Candura F et al the widest possible consensus to the quality standards to be implemented in European Haemophilia Centres. Acknowledgements The EUHANET project is funded by the European Commission Health Programme through the Executive Agency for Health and Consumers (EAHC) (Project number 2011207) with co-financing from 12 pharmaceutical manufacturers. Funding and conflict of interest The Authors declare that the pharmaceutical companies co-financing this project are Baxter, Bayer, Biotest, BPL, CSL Behring, Grifols, Kedrion, LFB, NovoNordisk, Octapharma, Pfizer, SOBI/Biogen Idec. Pier Mannuccio Mannucci has received honoraria for participating as speaker at educational meetings organised by Biotest, Bayer, Grifols, Kedrion Biopharma and Novo Nordisk. The other Authors declare no conflicts of interest. References 1) 2) 3) 4) Makris M, Calizzani G, Fischer K, et al. For the EUHANET project Steering Committee. The European Haemophilia Network (EUHANET). Blood Transfus 2014; 12 (Suppl 3): s515-8 . Giangrande P, Calizzani G, Menichini I et al. The European Standards of Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s525-30. Colvin BT, Astermark J, Fischer K, et al. for the Inter Disciplinary Working Group. European principles of haemophilia care. Haemophilia 2008; 14: 361-74. Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States, 24 October 2011. European Committee of Experts on Rare Diseases EUCERD. Available at: http://www.EUCERD.eu/upload/file/ EUCERDRecommendationCE.pdf. Accessed on 15/12/2013. 5) Recommendations to the European Commission and the Member States on European Reference Networks for Rare Diseases, 31 January 2013. European Committee of Experts on Rare Diseases - EUCERD. Available at: http://www.eucerd. eu/?post_type=document&p=2207. Accessed on 15/12/2013. 6) Haemophilia Alliance. A National Service Specification for Haemophilia and other Inherited Bleeding Disorders, 2nd edn. London. The Haemophilia Alliance, 2006. Available at: http:// www.ukhcdo.org/docs/HaemAlliance-NatSvsSpec2006.pdf. Accessed on 15/01/2014. 7) Conseil scientifique des maladie chroniques. «Comprehensive Care» pour Hémophiles. Bruxelles, Belgium: Rijksinstituut voor Ziekte- en Invaliditeitsverzekering (RIZIV) = Institut National Maladie Invalidité (INAMI); 2007. 8) Associazione Italiana Centri Emofilia. Programma di accreditamento professionale AICE, 2nd edn. 2010. Available at: www.aiceonline.it. Accessed on 15/12/2013. 9) I n t e r n a t i o n a l m e e t i n g o n H a e m o p h i l i a C e n t re C e r t i f i c a t i o n S y s t e m s a c ro s s E u ro p e . C e n t r o Nazionale Sangue (Italian National Blood Centre). Available at: http://www.centronazionalesangue.it/ newsbox/seminario-malattie-emorragiche-congenite-mec. Accessed on 15/01/2014. 10) The 20th European Haemophilia Consortium Round Table of Stakeholders on "Haemophilia Centres of Expertise in Europe". Available at http://www.ehc.eu/en/round-table-ofstake-holders/last-round-table/archive-of-round-table/201310-17-round-table.html. Accessed on 15/02/2014. Correspondence: Fabio Candura Italian National Blood Centre National Institute of Health Via Giano della Bella 27 00162 Rome, Italy e-mail: fabio.candura@iss.it Blood Transfus 2014; 12 Suppl 3: s519-24 DOI 10.2450/2014.0046-14s s524 ORIGINAL ARTICLE The European standards of Haemophilia Centres Paul Giangrande1,2, Gabriele Calizzani2,3, Ivana Menichini2,4, Fabio Candura2,3, Pier Mannuccio Mannucci5, Michael Makris6 1 Oxford University Hospitals NHS Trust, Oxford, United Kingdom; 2European Haemophilia Consortium, Bruxelles, Belgium; 3National Blood Centre, National Institute of Health, Rome, Italy; 4Necstep Studio Associato, Modena, Italy; 5Scientific Direction, IRCCS Ca’ Granda Maggiore Policlinico Hospital Foundation, Milan, Italy; 6Department of Cardiovascular Science, University of Sheffield, Sheffield, United Kingdom Introduction. The European haemophilia community of professionals and patients has agreed on the principles of haemophilia care to address comprehensive optimal delivery of care which is nowadays scattered throughout Europe. Many of the health facilities call themselves Haemophilia Centres despite their variation in size, expertise and services provided. Only a small number of countries have Haemophilia Centre accreditation systems in place. Methods. In the framework of the European Haemophilia Network project, following an inclusive process of stakeholder involvement, the European Guidelines for the certification of haemophilia centres have been developed in order to set quality standards for European Haemophilia Centres and criteria for their certification. Results. The Guidelines define the standards and criteria for the designation of two levels of care delivery: European Haemophilia Treatment Centres, providing local routine care, and European Haemophilia Comprehensive Care Centres, providing specialised and multi-disciplinary care and functioning as tertiary referral centres. Additionally, they define standards about general requirements, patient care, provision of an advisory service and establishment of network of clinical and specialised services. Conclusions. The implementation of the European Guidelines for the certification of Haemophilia Centres will contribute to the reduction of health inequalities through the standardisation of quality of care in European Union Member States and could represent a model to be taken into consideration for other rare disease groups. Keywords: standards and criteria, certification system, haemophilia care, EUHANET. Introduction Inherited bleeding disorders (IBDs) are caused by deficiencies of plasma proteins involved in haemostasis. The most common are von Willebrand disease (vWD), haemophilia A and haemophilia B. Inherited coagulation disorders are considered rare diseases, with a prevalence estimated at 1 in 5,000 males for haemophilia A1, 1 in 30,000 for haemophilia B2, and 1-3 in 1,000,000 for the most severe form of vWD (type 3)3. The clinical phenotype of haemophilia is related to the baseline level of the relevant coagulation factor, which may be used to classify the severity. Patients with haemophilia may be classified as severe, moderate or mild. Severe haemophilia is defined by a baseline level of factor VIII (or IX) below 1 IU/dL (%). These patients typically experience repeated and spontaneous bleeding into joints such as the knees, elbows and ankles and require regular treatment. Subjects with a factor VIII (or IX) level between 1 and 5 IU/dL are defined as having moderate haemophilia and experience less frequent bleeding. Patients with levels above 5 IU/dL are classified as having mild disease and usually experience bleeding only after injury or trauma4. In the context of great disparities among (and within) European Union Member States (EU MS) in terms of facilities available for treatment, types of products used, amount of factor VIII and IX concentrates used, number of patients treated in individual centres, conditions of access and quality of care5, 409 facilities in Europe, of widely varying in size and expertise, call themselves "Haemophilia Centres" (HCs)6. Only a small number of countries have accreditation or certification systems in place based on shared standards of care for HCs. In the framework of the Second Health Programme 2008-2013, the European Commission through the Executive Agency for Health and Consumers (EAHC) funded the European Haemophilia Network (EUHANET) project with the main objective of ensuring Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s © SIMTI Servizi Srl s525 Giangrande P et al equity of haemophilia treatment and care throughout Europe7. In order to set quality standards for European HCs and criteria for their certification, a group of experts drafted the European Guidelines for the Certification of Haemophilia Centres (hereinafter called as Guidelines)8, as one of the outputs of EUHANET project. Finally, the main objective of this manuscript is to describe the structure and the contents of the Guidelines. Certification vs accreditation Different meanings could be given to the word "standard". Its origin was used to denote "an emblem or flag of an army, raised on a pole to indicate the rallying point in battle", as a unit of measurement and evaluation for the movement of the armies in the battlefield. From this, as an extension of the meaning, it derived the meaning of "an acknowledged measure of comparison for quantitative or qualitative values" for which it is commonly used nowadays, especially referring to "something, such as a practice or a product that is widely recognised or employed, particularly because of its excellence"9. While the accreditation is a formal procedure that finds its legal framework within the Regulation 765/2008 and it is coordinated at European level by the European co-operation for Accreditation, the certification10, as a process for standardisation, is a voluntary procedure attesting the fulfilment of a set of technical/organisational specifications which are developed on the basis of consensus among all interested parties. It is carried out by independent standards bodies, acting at national, European and international level11. The European Union has, since the mid-1980s, made an increasing use of standards in support of its policies and legislation. Furthermore, European standardisation supports European policies in the areas of competitiveness, information and communication technologies, innovation, interoperability, environment, transport, energy, public health, health care delivery, consumer protection, etc.12. Materials and methods The development of standards and criteria for the certification of HCs is based on the review and analysis of key reference documents including: three recommendations on rare diseases drafted by the European Union Committee of Experts on Rare Diseases (EUCERD)13-15, the European principles of haemophilia care launched at the European Parliament in January 200916, and information on the existing certification systems in use in EU MS. As described elsewhere 17 , the Guidelines are the result of two consultation processes that widely involved European stakeholders. The first consultation process was launched in Prague during the European Haemophilia Consortium (EHC) Conference 18 in October 2012 and aimed to share principles and criteria as preliminary requirements to define the scope, approaches and rules for the production of a common set of EU standards on Haemophilia Centres for European countries. On the basis of the consensus reached and on the literature review, Work Package 4 Team members, in charge of developing the Guidelines, started the production of standards. With the agreement of the EUHANET Steering Committee, these standards were subject to a further round of consultation addressed to EU and non-EU MS stakeholders including clinicians, institutions and patient organisations and the EUHANET project partnership. This second consultation process was launched at the 6th Annual Congress of the European Association for Haemophilia and Allied Disorders held in Warsaw in February 201319. The Guidelines have been modified according to the revisions and comments received and finally launched during the international meeting Haemophilia Centre Certification Systems across Europe held in Rome in July 201320 and at the round table Haemophilia Centres of Expertise in Europe at the European Parliament on 17th October 201321. Results The European Guidelines for the Certification of Haemophilia Centres The Guidelines refer to the management of patients with IBDs, covering haemophilia A and B (including female carriers), the rarer congenital deficiencies of other coagulation factors (such as fibrinogen and factors II, V, VII, X, XI and XIII), vWD and inherited platelet defects and applies to both adult and paediatric patients. All patients should have access to a comprehensive care programme. The document sets the standards for an optimal delivery of haemophilia care and for the designation of two levels of European HCs: i) European Haemophilia Treatment Centres (EHTCs), providing local routine care, and ii) European Haemophilia Comprehensive Care Centres (EHCCCs), providing specialised and multi-disciplinary care and functioning as tertiary referral centres. The delivery of a comprehensive care programme may be provided by a EHCCC or by a EHTC which has established a formal relationship with one or more EHCCCs. Requirements for the two levels of Haemophilia Centres The HCs would be distinguished according to functions and activities they carry out. Functions and activities have been identified and listed for both EHTCs and EHCCCs Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s s526 European standards for Haemophilia Centres and can be summarised in four groups, as follows: 1. minimum number of severe haemophilia patients for the designation as EHTC or EHCCC; 2. expert haemophilia medical cover; 3. coagulation tests and related "turn around time" of the laboratories; 4. integrated approach to patient multidisciplinary comprehensive care. Referring to the first function, the EHTCs should normally care for at least 10 people with severe haemophilia A or B or vWD type 3, while EHCCC should normally care for at least 40 people with severe haemophilia. Another discerning point is the provision of expert haemophilia medical cover in the event of an emergency or in case treatment is needed outside normal working hours. EHTC must provide a 24-hour emergency treatment service, also by formalised arrangements with other departments and/or designated EHCCCs; additionally a EHCCC must provide a 24-hour advisory service for patients, families, hospital doctors, general practitioners and affiliated EHTCs health care professionals as well as a 24-hour laboratory service for clotting factor assays and inhibitors screens. In terms of coagulation tests performed, the EHTCs must provide basic diagnostic and monitoring laboratory support during normal working hours for the more common IBDs and offer specific treatment for patients with inhibitors and immune tolerance in collaboration with a EHCCC which offers a diagnostic and reference laboratory service with a full repertoire of tests for the diagnosis and monitoring of inherited disorders of haemostasis. EHTCs/EHCCCs have both access to a laboratory, which may be either internal or external to the centres, which provides at least an agreed set of coagulation tests in a defined "turn around time" (TAT: completion time from sample collection to result reporting) that could be taken as discerning criterion also. The list of coagulation tests is reported in Table I. The TAT for laboratory tests carried out must be agreed in writing between the clinical and laboratory services and be subject to monitoring. The laboratories that perform the above-mentioned tests must participate in an accredited external quality assurance scheme in haemostasis. The last discernible functions and activities among EHTC and EHCCC are based on the integrated approach to patient multidisciplinary comprehensive care. While EHTC must have access to multidisciplinary support, locally or in conjunction with EHCCCs (i.e. physiotherapy and orthopaedics, surgery, dental care, hepatology, infectious diseases, obstetrics and gynaecology, paediatric facilities if children are treated, genetics, clinical psychology and social worker), EHCCC must carry out and have access to the additional following functions and activities: i) orthopaedic and/ or rheumatology service with provision of surgery, ii) physiotherapy service, iii) specialised obstetric and gynaecological service for the management of haemophilia carriers and women with vWD and other hereditary bleeding disorders, iv) paediatric facilities if children are treated, v) genetic diagnosis service providing also carrier detection and antenatal diagnosis, vi) dental service and vii) hepatology and infectious diseases service for patients with HIV and/or viral hepatitis. The above-mentioned functions and activities are outlined in Table II. Other requirements In the Guidelines, other requirements are grouped in four main areas. General requirements include those activities/functions that a EHTC/EHCCC must attain in Table I - List of coagulation tests provided by both European Haemophilia Treatment Centres and European Haemophilia Comprehensive Care Centres and their related "turn around time". Tests E-HCCC E-HTC 24 hr service 24 hr service PT, APTT, thrombin time and mixing studies Yes TAT: within 3 hours Yes Yes TAT: within 3 hours - Factor VIII and IX assays Yes TAT: within 6 hours Yes Yes - Inhibitor screen Yes TAT: within 12 hours Yes Yes - Fibrinogen, vWF and factor II, V, VII, X, XI activity assays Yes TAT: within 12 hours Yes Yes - Platelet aggregation Yes - - - vWF antigen and multimers Yes - - - Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s s527 Giangrande P et al Table II - Functions and activities for the European Haemophilia Treatment Centres and the European Haemophilia Comprehensive Care Centres. Main functions and activities for the EHTC Main functions and activities for the EHCCC Should normally care for at least 10 people with severe haemophilia A or B or vWD type 3. Should normally care for at least 40 people with severe haemophilia. • Carries out the following additional functions and activities: • Co-ordinates the delivery of haemophilia services - both in hospital and in the community including liaison with affiliated EHTCs. • Provides a 24-hour advisory service for patients, families, hospital doctors, general practitioners and affiliated EHTCs health care professionals. • Provides specialist care for patients with inhibitors, including surgery. • Provides a diagnostic and reference laboratory service with a full repertoire of tests for the diagnosis and monitoring of inherited disorders of haemostasis. • Provides a 24-hour laboratory service for clotting factor assays and inhibitors screens. • Has access to orthopaedic and/or rheumatology. service with provision of surgery. • Has access to physiotherapy service. • Has access to a specialised obstetric and gynaecological service for the management of haemophilia carriers and women with vWD and other hereditary bleeding disorders. • Has access to paediatric facilities if children are treated. • Has access to a genetic diagnosis service providing also carrier detection and antenatal diagnosis. • Has access to dental service. • Has access to hepatology and infectious diseases service for patients with HIV and/or viral hepatitis. • Offers professional psychological support. • Has access to social worker and welfare advice. • Collates data (e.g. product usage, patient demographics). • Participates in research, including clinical trials. • • • • • • • Provides care for patients, including diagnosis, treatment, followup and rehabilitation. Provides patients with safe and effective treatment products. Provides a 24-hour emergency treatment service. Provides basic diagnostic and monitoring laboratory support during normal working hours for the more common inherited bleeding disorders. Has access to multidisciplinary support, locally or in conjunction with EHCCC (physiotherapy and orthopaedics, surgery, dental care, hepatology, infectious diseases, obstetrics and gynaecology, paediatric facilities if children are treated, genetics, clinical psychology and social worker). Offers specific treatment for patients with inhibitors and immune tolerance in collaboration with a EHCCC. Provides advisory service, including genetic counselling, to patients and healthcare professionals. Promotes information and training programs on inherited bleeding disorders to patients and healthcare professionals. order to preserve the role of health care facility for rare diseases. They include among others the record-keeping and data collection (patient register; medical records; data management) and the participation in registers on IBDs at regional/national levels, as well as the supply and management of therapeutic products, reagents and medical devices. Standard requirements describe also the activities addressed to patient care: from the activities of information and education to patients and their families to those pertaining to diagnosis and therapy of haemophilia and other related IBDs (including all forms of acquired haemophilia). Periodic clinical and multi-disciplinary review yearly based as well as genetic services are not excluded within this group of standard requirements. Not last, a core set of outcome indicators should be provided and be subjected of monitoring activities. Indicators should include: units of coagulation factor concentrate used by each patient per year; number of new bleeding episodes (including breakthrough bleeds in the case of patients on prophylaxis); adverse events possibly related to treatment (inhibitors, viral infections, poor efficacy of treatment, etc.); mortality and causes of death. Additionally, a specific call on the social-health impact of IBDs should be also taken into consideration measuring, for example, the quality of life of the patients along with the number of days missed from school or work due to bleeds. Advisory service is provided as a continuous emergency medical cover by the EHCCC but generally both levels provides this service to patients and their families, and to other professionals and caregivers who treat the patients during normal working hours. The last group of standard requirements concerns networking activities of EHTCs/EHCCCs. Many small EHTCs play a critical role in providing effective emergency care at a local level for patients with haemophilia and other IBDs. However, patients may need to attend a EHCCC for more comprehensive elements of care (e.g. elective surgery in patients with inhibitors). The level of collaboration will depend upon the degree of expertise available in the EHTC. In particular, in order to guarantee integrated approach to patient multidisciplinary comprehensive care, the relationships and agreements of a EHTC with one or more EHCCCs must be formally established as well as those with structures providing specialist services and with laboratories (see above). Conclusions The delivery of haemophilia and other related IBDs care is scattered throughout Europe. Many of the health facilities call themselves "Haemophilia Centres" despite considerable variation in size, expertise and services provided . Although a small number of countries have Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s s528 European standards for Haemophilia Centres accreditation systems in place, the majority do not. Delivery of care is challenging because of the rarity and costs of treatment of this group of diseases. As well as other rare disease groups, IBDs are characterised by treatment specificities and peculiarities. In order to deal with the heterogeneity of EU MS health systems as well as to their different regulatory frameworks, the Guidelines have been discussed, evaluated and ameliorated by a sound number of EU and non-EU stakeholders in different inclusive consultation processes that brought a highly qualified added value to the document. Thus, the Guidelines evolved taking into consideration all relevant comments received. Among them it is worthwhile mentioning the concerns for the thresholds applied, as a mandatory standard, to the number of patients treated by the HCs in order to define the level of care provided. These concerns resulted more evident in view of small population countries. While the long-debated threshold for the designation of a EHCCC might be considered as flexible (a EHCCC should normally care for at least 40 people with severe haemophilia) where all other mandatory standards are satisfied, the lower threshold of 10 people with severe haemophilia treated to designate a EHTC has been defined after the proposals received. Relationships and collaborations in patients' health care management between EHTCs and one or more EHCCCs are currently established in some EU MS. It is unusual that these agreements are defined under a formalised framework of protocols. In order to ensure an integrated approach to patient multidisciplinary comprehensive care as recommended within the European principles of haemophilia care16, procedures, rules for collaboration between EHTCs and EHCCCs must be written, shared and made available to the public. The implementation of these Guidelines and the application process on voluntary basis to the European certification system are to be considered as the first stage for shaping the upcoming European haemophilia network. Certification is issued after the examination of the information provided by the HCs (e.g. number of patients registered, facilities offered) to EUHANET. Non confidential information will be available on a public website. Nevertheless, an evaluation framework within a prospective and more structured system of external auditing is wished for and expressively claimed by the national and international patient organisations. Networks of reference of centres of expertise for rare diseases are crucial for EU health policy as stated within the cross-border directive (article 12)22. Thus, all European HCs will be invited to apply for certification (the European Guidelines for the Certification of Haemophilia Centres and the application form for certification are available at the EUHANET project website: http://www.euhanet.org/MappedCentres. aspx). Once implemented across EU MS, the European Guidelines for the certification of Haemophilia Centres will contribute to the reduction of health inequalities through the standardisation of quality of care. The standards are not intended to establish best practices or include all procedures and practices that centres or individuals should implement; on the contrary, are designed to provide minimum Guidelines especially for those EU MS where haemophilia care is not definite deeply affecting equity of access and, more generally, rights of citizenship. Finally, the process of stakeholders engagement, the document itself and the emerging network of treatment centres will represent a model for European networks of reference to be established for other rare diseases groups. Acknowledgements The EUHANET project is funded by the European Commission Health Programme through the Executive Agency for Health and Consumers (EAHC) (Project number 2011207) with co-financing from 12 pharmaceutical manufacturers. Author contributions Paul Giangrande and Gabriele Calizzani are equally first authors of this manuscript. Paul Giangrande contributed to the study implementation and manuscript draft. Gabriele Calizzani contributed to the study design, study implementation and manuscript draft. Ivana Menichini contributed to the study design, study implementation, manuscript revision and manuscript approval. Fabio Candura contributed to the study design, study implementation, manuscript draft, manuscript revision and manuscript approval. Pier Mannuccio Mannucci contributed to the study design, manuscript revision and manuscript approval. Michael Makris contributed to the study design, manuscript revision and manuscript approval. Conflicts of interest The Authors declare that the pharmaceutical companies co-financing this project are Baxter, Bayer, Biotest, BPL, CSL Behring, Grifols, Kedrion, LFB, NovoNordisk, Octapharma, Pfizer, SOBI/Biogen Idec. Pier Mannuccio Mannucci declares that he received honoraria for participating as speaker at educational meetings organised by Biotest, Bayer, Grifols, Kedrion Biopharma and Novo Nordisk. The other Authors declare no conflicts of interest. References 1) Stonebraker JS, Bolton-Maggs PH, Soucie JM, et al. A study of variation in the reported haemophilia A prevalence around the world. Haemophilia 2010; 16: 20-32. Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s s529 Giangrande P et al 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) Stonebraker JS, Bolton-Maggs PH, Soucie JM, et al. A study of variations in the reported haemophilia B prevalence around the world. Haemophilia 2012; 18: e91-94. Mannucci PM. Treatment of von Willebrand's disease. N Engl J Med 2004; 351: 683-94. White GC 2nd, Rosendaal F, Aledort LM, et al. Definition in hemophilia. Recommendation of scientific subcommittee on factor VIII and factor IX of scientific and standardization committee of the International Society of Thrombosis and Haemostasis. Thromb Haemost 2001; 85: 560. O'Mahony B, Noone D, Giangrande PL, Prihodova L. Haemophilia care in Europe - a survey of 35 countries. Haemophilia 2013; 19: e239-247. Geographic distribution of Haemophilia Centres in Europe. http://www.euhanet.org/MappedCentres.aspx. Accessed on 15/01/2014 Makris M, Calizzani G, Fischer K, et al. For the EUHANET project Steering Committee The European Haemophilia Network (EUHANET). Blood Transfus 2014; 12 (Suppl 3): s515-8. European Guidelines for the Certification of Haemophilia Centres. European Haemophilia Network. Available at: http:// www.euhanet.org/docs/Euhanet-European_Guidelines_ for_the_certification_of_Haemophilia_Centres_2013.pdf. Accessed on 09/01/2014. Meaning of the word 'standard' from English Oxford Dictionary. http://www.oxforddictionaries.com/. Accessed on 15/001/2014. L 218/30 Official Journal of the European Union 13.8.2008 Regulation (EC) No765/2008 of the European Parliament and of the Council of 9 July 2008 setting out the requirements for accreditation and market surveillance relating to the marketing of products and repealing Regulation (EEC) No 339/93. Available at: http://eur-lex.europa.eu/LexUriServ/ LexUriServ.do?uri=OJ:L:2008:218:0030:0047:en:PDF. Accessed on 15/01/2014. European standards. Available at: http://ec.europa.eu/ enterprise/policies/european-standards/index_en.htm. Accessed on 15/01/2014. European standardisation policy. Available at: http:// ec.europa.eu/enterprise/policies/european-standards/ standardisation-policy/index_en.htm. Accessed on 12/01/2014. EUCERD Recommendations on rare disease European reference networks (RD ERNS) (31 January 2013). Available at: http://www.eucerd.eu/?post_type=document&p=2207. Accessed on 03/01/2014. EUCERD Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States (24 October 2011). Available at: http://www.eucerd.eu/upload/file/ EUCERDRecommendationCE.pdf. Accessed on 08/01/2014. EUCERD Recommendation to the European Commission 16) 17) 18) 19) 20) 21) 22) and Member States on improving informed decisions based on the Clinical Added Value of Orphan Medicinal Products (COVAMP) information flow (September 2012). Available at: http://www.eucerd.eu/?post_type=document&p=1446. Accessed on 15/01/2014. Colvin BT, Astermark J, Fischer K, Gringeri A, Lassila R, Schramm W, A. Thomas A and Ingerslev J for the inter disciplinary working group. European principles of Haemophilia Care. Haemophilia 2008; 14: 361-74. Candura F, Menichini I, Calizzani G, et al. The methodology for defining the European Standards for the designation of Haemophilia Centres in Europe. Blood Transfus 2014; 12 (Suppl 3): s519-24. European Haemophilia Consortium 2012 Conference. European Haemophilia Consortium. Available at: http:// www.ehc.eu/nc/en/ehc-conference/current-ehc-conference/ former-conferences/ehc-conference2012.html?sword_ list%5B%5D=prague. Accessed on 29/12/2013. European Association for Haemophilia and Allied Disorders 2013 Congress. European Association for Haemophilia and Allied Disorders. Available at: http://www.eahad2013.pl/. Accessed on 29/12/2013. International meeting on Haemophilia Centre Certification Systems across Europe. Centro Nazionale Sangue (Italian National Blood Centre). Available at: http://www. centronazionalesangue.it/newsbox/seminario-malattieemorragiche-congenite-mec. Accessed on 15/01/2014. The 20th European Haemophilia Consortium Round Table of Stakeholders on "Haemophilia Centres of Expertise in Europe". Available at http://www.ehc.eu/en/round-table-ofstake-holders/last-round-table/archive-of-round-table/201310-17-round-table.html. Accessed on 15/02/2014. Official Journal of the European Union L 88/45. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in crossborder healthcare. Correspondence: Gabriele Calizzani National Blood Centre, National Institute of Health Via Giano della Bella 27 00162 Rome, Italy e-mail: areaplasma.cns@iss.it Blood Transfus 2014; 12 Suppl 3: s525-30 DOI 10.2450/2014.0056-14s s530 REVIEW The haemophilia certification system in Canada Davide Matino1, Jerry Teitel2, David Page3, Arun Keepanasseril1, Alfonso Iorio1,4, Irwin Walker4 1 Health Information Research Unit, Department of Clinical Epidemiology and Biostatics, McMaster University, Hamilton; 2St. Michaels Hospital, Toronto; 3Canadian Haemophilia Society, Montreal; 4Division of Hematology, Department of Medicine, Hamilton, Canada Introduction Inherited bleeding disorders are caused by the deficiency or dysfunction of plasma proteins required for the development of a physiological hemostatic process1,2. Von Willebrand disease (vWD), haemophilia A and haemophilia B are the most common inherited disorders of hemostasis. In their severe forms, these disorders are life-threatening. However advanced treatment modalities have enabled even severely affected patients to reach the same life expectancy of the general male population at least in high-income countries3,4 . Indeed, after the dramatic events of widespread blood-borne virus transmission in the 1970s-1980s in haemophilic patients, leading to a 35-to-40-year reduction in life expectancy in Canadian patients5, there has been a strong drive towards continuous improvement, primarily in the safety of replacement therapy6 .There is now a very high degree of safety from risk of blood borne transmission of pathogens as evidenced by the absence of reported transmission of blood-borne viruses in persons with haemophilia since the late 1980s to date7. The safety of current replacement therapies was recently confirmed by a prospective surveillance program ongoing since 2008 and based on regular monitoring of 22,242 European patients (European Haemophilia Safety Surveillance System; www.euhass.org). Regular factor prophylaxis as a therapeutic regimen has been proven effective in preventing haemophilic arthropathy8. Even in the presence of neutralizing antibodies (inhibitors) directed against the deficient clotting factor, particularly in haemophilia A, bleeding can usually be treated successfully using activated variants of coagulation factors9. Moreover, immune tolerance induction (ITI), based on the long-term intravenous infusion of large doses of FVIII, eradicates inhibitors in as many as two-thirds of patients10. Therefore, improving quality of life has become the primary objective of care in developed countries; thus multiple modalities (psychosocial support, physiotherapy, integration into community life, etc), not just the infusion of the deficient factor, are made available to the patient and his family, to allow them to fully experience good health. The haemophilia care in Canada Canada is a very large country geographically. With a total of 9.98 million square kilometres, Canada is the world's second-largest country by total area consisting of 10 provinces and 3 territories. Provinces have a great deal of power relative to the federal government, with jurisdiction over many public goods such as health care (but also education, welfare, and intra-provincial transportation). Current Canada's total population estimate (http://www.statcan.gc.ca/) is 35,295,770. The Canadian Hemophilia Registry identified a total of 2,966 haemophilia A patients, 690 haemophilia B patients, 3,963 patients affected by vWD and 1,740 patients with other bleeding disorders, including rare platelet disorders (http://fhs.mcmaster.ca/chr/data. html). Factors usage from 2007 to 2012 is reported in Table I. In 2012 a total of 190,189,628 FVIII IU were used and the mean per capita FVIII usage was 5.39 IU while a total of 45,772,681 FIX IU consumption was registered with a mean per capita FIX usage of 1.29 IU. Some patients live many hundreds of kilometers from the nearest Haemophilia Treatment Centre (HTC). A number of strategies are used to provide care to them. Home infusion is encouraged where feasible. Specialists in the HTC create links with local practitioners to coordinate care in distant locations. Telemedicine is used to communicate with patients and their caregivers. Nurse coordinators connect extensively with patients by telephone. Some centre teams conduct outreach clinics to smaller centers where a concentration of patients reside. Programs funded by government or the local chapter of the CHS provide financial support for families to travel to the HTC for annual assessments. Electronic infusion reporting systems are used to report product use. Distribution of the 24 Haemophilia Treatment Centers (HTCs) in Canada is shown in Figure 1. The standard of care for haemophilia in Canada A functional, efficient, and accountable system of haemophilia care has been developed in Canada mostly at the initiative of the comprehensive care centers, without acting official mandates. However, several Canadian provinces have since designated provincial haemophilia programs in specific centres (e.g. British Columbia, Saskatchewan, Manitoba and Quebec). The existing system is thus an eloquent testimony to the goodwill and constructive collaboration among patients and their families, health care providers and funders. The idea that Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s © SIMTI Servizi Srl s531 Matino D et al Table I - Reported use of factor concentrates in Canada from 2007 to 2012. Product Factor Eight Inhibitor Bypassing Activity 2012-2013 2011-2012 2010-2011 2009-2010 2008-2009 2007-2008 Unit Quantity Quantity Quantity Quantity Quantity Quantity IU 14.059.865 14.059.865 12.139.931 11.406.109 9.492.307 7.096.409 Compl.prot.total Octaplex IU 3.360.500 3.360.500 9.942.500 920.000 12.600 0 Factor IX IU 42.975.510 42.975.510 43.612.325 39.861.108 37.136.322 33.569.155 Factor VIIa IU 1.463.400 1.463.400 1.248.000 1.107.000 1.227.000 978.600 Factor VIIa rec. NiaStase® mg 25.483 25.483 30.502 30.686 34.124 33.740 Porcine FVIII IU - - 0 0 0 249.340 Recombinant Factor VIII IU 178.234.199 178.234.199 178.792.631 164.791.696 155.487.497 144.129.307 Factor VIII/VWF IU 28.730.716 28.730.716 26.711.363 24.364.514 20.701.440 18.620.052 Factor XI IU 35.890 35.890 51.275 74.455 64.575 85.705 Factor XIII IU 559.000 559.000 533.000 471.750 522.000 444.250 Fibrinogen g 542 542 933 390 1.188 901 Figure 1 - Distribution of Haemophilia Treatment Centers across Canada a national standard of care for haemophilia be developed for Canada was first promulgated in the conference "Comprehensive Care for the Canadian Haemophiliac", Winnipeg, May 1978, organised by the Canadian Haemophilia Society (CHS) in close collaboration with its own multi-disciplinary Medical and Scientific Advisory Committee (MSAC). To analyze the scope of the initiative, we will refer to the definition given in 1998 in the Standards for comprehensive care of haemophilia in Canada, agreed upon during a "second" Winnipeg conference, on April 30 - May 1, 1998. The Association of Haemophilia Clinic Directors of Canada (AHCDC) and the CHS felt that national standards of care for haemophilia should be developed for the following reasons: 1. to preserve the integrity of the network of Haemophilia Comprehensive Care Programs; 2. to assure equal access and equal standards of care; 3. to establish a reference for discussion of future advances and needs; 4. to be a reference point and unifying force for staff of various organizations that are geographically dispersed and serve a small population; 5. to promote discussion and research regarding optimal ways to deliver care; and 6. to provide the basis for the design of clinics, for accreditation, and for audit and evaluation. Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s532 The haemophilia certification system in Canada At its Annual General Meeting in Edmonton, the AHCDC appointed a working group on standards of care with two of us (Irwin Walker and Jerome Teitel) as cochairs. The working group was later expanded to become a multidisciplinary one. With the aim of developing national standards, a national multidisciplinary committee, including members of the CHS, the Canadian Association of Nurses in Haemophilia Care (CANHC), Canadian Association of Physiotherapists in Haemophilia Care (CAPHC), and the Canadian Social Workers in Haemophilia Care (CSWHC) was initiated to further the initiatives of the AHCDC. The National Standards Committee for Haemophilia Treatment Centres conducted a first conference on April 20, 2005. It was attended by the representatives from the CHS and the AHCDC. An important recommendation from the meeting was that Haemophilia Comprehensive Care should be delivered according to a set of uniform national standards and wherever possible these standards should be needs-based, data-driven and supported by evidence of effectiveness. The meeting also held that generic national standards be developed, but as they would be implemented locally the system must be flexible and adaptable, with the emphasis being the delivery of a uniformly high quality of care. The meeting also formalised the constitution of a multidisciplinary standards of care working group to develop comprehensive standards of care for haemophilia, led by the AHCDC. All four health care provider groups and CHS were represented in the working group. Simultaneously, the Ontario clinics were working on provincial standards of care, and they published their document which later became the template for the national standards. This work was spearheaded by the Provincial Haemophilia Coordinator at the time, Julia Sek, and the co-chairs of that group were Jerome Teitel and John Plater. After a series of meetings and deliberations, the first edition of the Canadian Haemophilia Standard of Care was published in 2007 (Canadian Comprehensive Care Standards for Haemophilia and Other Inherited Bleeding Disorders, http://www.haemophilia.ca/en) for use by Haemophilia Treatment Centres, hospital administrations, and provincial Ministries of Health. It has to be acknowledged that this national document was largely based on the Ontario Provincial standards. The premises of the Canadian comprehensive care standards for haemophilia and other inherited bleeding disorders are that: - improved quality of life is the ultimate goal of care, with an emphasis on measurable outcomes and independent living; - inherited bleeding disorders are rare and therefore - - - - collaboration among HTCs and networks needs to be encouraged; bleeding disorders and their treatments are associated with a number of complications - medical, psychological and social-that may affect quality of life of affected individuals and so care needs to be comprehensive; evaluation and documentation of clinical outcomes are essential components of a comprehensive program; standards of care are measures that HTCs can adhere to and which can be used for auditing. Key indicators are signals that demonstrate whether a standard has been attained. They provide a way in which to measure and communicate the impact or result of the standard, as well as the process. accountability for utilization of factor replacement product is necessary due to its potential to cause adverse events and its high cost; this is equally true for products used in centres and at home in supervised home therapy programmes; HTCs have a responsibility to participate in research, education and innovation to the degree that they are capable. Regional differences within the province or region must be acknowledged in the provision of care for people with bleeding disorders. Future perspective and conclusions The vision is to provide comprehensive care to all individuals with inherited bleeding disorders, guided by clear standards, facilitated by engagement with stakeholders, and driven by needs and best practice, resulting in best outcomes. The focus of these standards is on the structural and resource requirements necessary for a HTC to effectively provide care, and on its functions and responsibilities. In 2009 in response to a request from the AHCDC executive, the Standards group initiated a self assessment survey among Canadian Haemophilia Treatment Centers according to the specific standards (Table II, III, IV) and key indicators (see appendix 1) proposed. Standards of care are measures that Haemophilia Treatment Centres can adhere to and which can be used for self-evaluation and auditing. Key indicators are signals that demonstrate whether a standard has been attained. They provide a way in which to measure and communicate the impact or result of the standard, as well as the process. The goal was to validate the Canadian clinic standards by assessing acceptability and adherence. The average adherence by all clinics to all standards was 92% (standards being adhered to by an average of 22 of 24 HTCs). Adherence levels below 83% (20 of 24 HTC) were observed for only 4 standards; for two of these standards the low adherence was due to a lack of core team members, particularly social workers and physiotherapists and possibly administrative staff as well. As indicated by Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s533 Matino D et al Table II - Standards - 1. Scope of care The HTC will: 1. Establish correct diagnoses. 2. Establish and maintain a full complement of core team members 3. Develop visibility in the bleeding disorder and medical community. 4. Strive to enrol all members of the target population in its region. 5. Establish a collaborative relationship among core team members 6. Establish a routine for patient access to regular and emergency care. 7. Establish a process for referring patients to services not provided within the programme. 8. Register patients in CHARMS (Canadian Haemophilia Assessment and Resource Management System) and CHR (Canadian Haemophilia Registry) databases. 9. Provide the patient with documentation that identifies his/her bleeding disorder and recommended treatment. 10. Provide education to affected individuals, family members, health care givers and others as necessary. 11. Have a home infusion program, in which patients and families are instructed in home therapy, including prevention and recognition of bleeds and correct practices. 12. Provide primary and secondary prophylaxis regimens as appropriate (all pediatric patients with severe haemophilia should be considered). 13. Provide early intervention and follow-up care to reduce long-term complications. 14. Network with outside agencies creating formal linkages to provide efficient access to their services. 15. Encourage and facilitate eligible members to participate in activities of AHCDC, CANHC, CPHC, CSWHC and other relevant HTC working groups. Table III - Standards - 2. Quality Measures1 The HTC will: 1. Maintain health records according to legislation, which must include: - history and physical examination; - diagnosis and treatment recommendations; - operative/special procedure notes and records; - interdisciplinary progress notes; - medication records; - consent forms; - adverse events/allergies; - records of home therapy program (teaching, home visit to initiate program, and annual certification); - records of telephone communications. 2. Participate in data collection and submission to CHARMS including: - i. patient demographics; 4. - ii. factor utilization. Submit anonymous data to the Centre Point module of CHARMS and to the CHR, as required by AHCDC. AHCDC will pool and collate factor concentrate utilization data and make it available to the operators of the blood system to plan purchases, flag inconsistencies, outliers and adverse events and to conduct efficient recalls and advisories as necessary. AHCDC will also use data for research planning, and various administrative and political purposes. Adhere to provincial health information privacy protection acts. 5. Be supported by its host hospital and the provincial Ministry of Health. 6. Accept accountability for the appropriate use of all factor concentrates distributed within its catchment area to registered patients with inherited bleeding disorders. This excludes cryoprecipitate and fresh frozen plasma, but includes all plasma derived and recombinant concentrated clotting factors distributed by Canadian Blood Services and Héma-Québec. 7. Participate in a formal accreditation and evaluation process once it is established. 8. Mentor, where possible, students and trainees in the health professions. 9. Establish mechanisms to acknowledge and review compliments, complaints and special requests. These compliments and complaints are documented and reviewed periodically. 3. 1 This section describes expected activities of an HTC that contribute to the quality of both the individual centre and the Canadian HTC network. Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s534 The haemophilia certification system in Canada Table IV - Standards - 3.Therapeutic Services1 The HTC will: 1. Provide the appropriate professional care for their patients, recognizing the need for pediatric and adult medical expertise as appropriate. 2. Provide a comprehensive evaluation (including laboratory testing) at least annually for adult patients and semi-annually for children. This frequency is recommended for those with higher bleeding risk; for those with a lower bleeding risk a less frequent schedule will be appropriate. The evaluation will include updating wallet cards (treatment recommendations). 3. Provide assessments from each core team member at least annually. Patients will have additional access to core team members as required. 4. Provide emergency departments and family physicians with diagnosis and treatment recommendations for registered patients, consistent with the PHIPA and the hospital’s health records policy. The HTC will arrange for qualified 24-hour medical coverage and consultative services for the target population. 5. Educate patients and families on the best way to advocate for and to access emergency care and other services. 6. Utilize, as appropriate, clinical practice guidelines published by AHCDC and other expert bodies for the management of bleeding episodes, inhibitors and special or surgical procedures. 7. Establish formal links to provide access to special hemostasis testing, genetic testing, and treatment for haemophilia and its complications. 8. Work in collaboration with patients and their families to promote health and to enhance ability to cope with a chronic health condition. 9. Provide education and recommendations to other community professionals who provide services to patients with inherited bleeding disorders. 10. Provide prophylaxis (primary and secondary) to patients in accordance with AHCDC recommendations and best practice. 11. Provide a home therapy program to all appropriate patients and monitor its effectiveness for each individual. The home therapy program will include comprehensive training in intravenous technique and procedures for both care givers and patients themselves, as appropriate, safe and responsible handling and storage of factor concentrates and safe disposal of used equipment and supplies. 12. Maintenance of home therapy records will be encouraged and routinely reviewed, to help in making treatment recommendations. 13. Provide injection equipment and other supplies to patients. 14. Provide management for patients with inhibitors with reference to guidelines issued by the AHCDC and other expert bodies. 15. Be located in a facility that should be readily accessible to people with disabilities. 16. Be located within an Ambulatory Clinic area to facilitate prompt assessment and treatment of acute bleeding episodes. 17. Be located in a facility that has or is linked with an Emergency Department where patients can obtain treatment outside of regular hours. 1 This section describes the actions required of an HTC in the direct delivery of therapeutic services. statements from the World Federation of Haemophilia and by the Canadian standards, a lack of any of these team members is particularly serious considering their importance. Lack of complete adherence to other standards was due to a variety of reasons, in most cases either easily explainable or spurious. No correlation was found between the level of adherence to the standards and any one of a variety of HTC descriptors. The general level of acceptability of the standards was high; most clinics (20 of 24, 83%) thought the standards were useful and 22 of 24 clinics (92%) expressed their willingness to participate in evaluation and accreditation processes once these are established. To fulfill the proposed standards of care a full audit process, modeled on the Ireland and UK experience, has been planned by the AHCHC-led Canadian Haemophilia Standards Group, but has been slowed down by unexpected privacy issues encountered early in the process. Complementarily to this process, and in order to gather information that can be used to advocate for adequate resources in clinics, a CHS task force led by PastPresident, Pam Wilton, has developed a Haemophilia/ Bleeding Disorder Clinic evaluation process to be led by CHS to roll out in 2013. The proposed process, which is supported by the Executive Committee of the AHCDC, consists of an assessment of the services and resources in Haemophilia/Bleeding Disorder Clinics through interviews with clinic personnel and a patient questionnaire. This survey is evaluating the adequacy of the physical, material and human resources in Canada's 24 HTC. The overall goal is to identify any gaps in resources that may prevent Haemophilia/Bleeding Disorder Clinics from delivering care and treatment according to the Canadian Comprehensive Care Standards for Haemophilia and Other Inherited Bleeding Disorders and that may lead to sub-optimal patient outcomes (see Table I, II, III). The primary objectives are: - to conduct a thorough assessment of the services and resources in Haemophilia/Bleeding Disorder Clinics in each province; - to prepare a detailed report and recommendations for hospital administrators and/or Ministry of Health officials in each province; - to identify and meet key decision-makers in each province with the goal of maintaining and improving the care for people with inherited bleeding disorders; - to follow up support implementation of recommendations. Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s535 Matino D et al Interviews with clinic personnel and patient questionnaires (see appendix 2, 3) are used in the evaluation. The process is based on a successful initiative by the Quebec Chapter of the CHS. Study interviewers met all 37 clinic personnel across Quebec in half-hour meetings. These face-to-face interviews are preferred to a written survey to allow dialogue and clarification of responses. The resulting report is validated by the clinic directors and recommendations are made to the Ministry of Health. The same approach will be applied to all clinics across Canada. To promote a consistent approach, the interviews are conducted by David Page, CHS National Executive Director, and Michel Long, CHS National Program Manager and, in Ontario, Sarah Crymble, Haemophilia Provincial Coordinator. The patient questionnaire was originally developed for the Irish and U.K. HTC audits, and has been modified by the group preparing the Canadian audit. The observations, based on the clinic interviews and patient questionnaires, will be assembled in a draft report by the CHS National Office for each clinic and then shared first with the clinic director. Once vetted and approved by the clinic director a final report will be shared with the local chapter Board of Directors. Then, if necessary, a strategy will be developed to approach the appropriate health authorities - hospital administration, regional health authority of Ministry of Health - with a proposal to better meet the standards of care. Up to now, most of the Ontario assessments have been concluded and the visits in Western Canada have been scheduled for winter 2014. We expect that by the end of April 2014 the visits will be completed. Patient questionnaires are actively being distributed by Centres and responses are being received. In summary, the process of haemophilia centre accreditation in Canada was born with the cooperation of patients and doctors. It will serve as the model to standardize and, where necessary, to improve the care of Canadian haemophilia patients. There is no "end" to such a process. In our opinion, many important results have been achieved, and several important lessons can be learned. As well, we are sure that interesting and actionable results will stem from the ongoing process. 2) Lillicrap D. vonWillebrand disease: advances in pathogenetic understanding, diagnosis, and therapy. Blood 2013; 122: 3735-40. 3) Darby SC, Kan SW, Spooner RJ et al. Mortality rates, life expectancy, and causes of death in people with haemophilia A or B in the United Kingdom who were not infected with HIV. Blood 2007; 110: 815-25. 4) Tagliaferri A, Rivolta GF, Iorio A et al. Mortality and causes of death in Italian persons with haemophilia, 1990-2007. Haemophilia 2010; 16: 437-46. 5) Walker IR, Julian JA. and Association of Haemophilia Clinic Directors of Canada. Causes of death in Canadians with haemophilia, 1980-1995. Haemophilia 1998; 4: 714-20. 6) Mannucci PM. Treatment of haemophilia: building on strength in the third millennium. Haemophilia 2011; 17 (Suppl 3): 1-24. 7) Blood safety monitoring among persons with bleeding disorders-United States, May 1998-June 2002. MMWR Morb Mortal Wkly Rep. 2003; 51: 1152-4. 8) Iorio A, Marchesini E, Marcucci M, Stobart K, Chan AK. Clotting factor concentrates given to prevent bleeding and bleeding-related complications in people with haemophilia A or B. Cochrane Database Syst Rev. 2011 Sep 7; (9): CD003429. 9) Iorio A, Matino D, D'Amico R, Makris M. Recombinant Factor VIIa concentrate versus plasma derived concentrates for the treatment of acute bleeding episodes in people with haemophilia and inhibitors. Cochrane Database Syst Rev. 2010 Aug 4;(8): CD004449. 10) Hay CR, Di Michele DM. The principal results of the International Immune Tolerance Study: a randomized dose comparison. Blood. 2012; 119: 1335-44. Keywords: haemophilia, comprehensive care, audit, accreditation, certification. The Authors declare no conflicts of interest. References 1) Kumar R, Carcao M. Inherited abnormalities of coagulation: haemophilia, von Willebrand disease, and beyond. Pediatr Clin North Am 2013; 60: 1419-41. Correspondence: Alfonso Iorio HIRU CRL-140 Clinical Epidemiology and Biostatistis McMaster University 1280 Main St. West L8S4L8 Hamilton, Ontario, Canada e-mail: iorioa@mcmaster.ca Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s536 The haemophilia certification system in Canada Appendix 1 Key Indicators - 1. Scope of Care* 1-1 1-2 1-3a 1-3b 1-3c 1-4 1-5a 1-5b 1-6a 1-6b 1-6c 1-7a 1-7b 1-7c 1-8a 1-8b 1-8c 1-9 1-10a 1-10b 1-11a 1-11b 1-11c 1-12a 1-12b 1-13a 1-13b 1-14 1-15a 1-15b Patients’ factor levels are documented in their clinic records. The HTC has a complete complement of core team members as listed in the standards. The HTC has regular communications with the local chapter or region of the Canadian Hemophilia Society. The HTC has a process in which to communicate to outside agencies about current events/workshops and conferences. Outside agencies are able to contact team members for information. The HTC is aware of the pattern of factor concentrate utilization in the region There is evidence of collaboration among all members. Core team members contribute to the development of policies, procedures and standards. Registered patients can access care and follow-up care for acute bleeds. Non life-threatening bleeds in non inhibitor patients are managed in the ambulatory care setting, so that there is a low hospitalization rate for bleeding episodes. Policies & procedures are available for the treatment of non-urgent, urgent and emergency bleeding episodes. The HTC has a referral list for secondary team members and utilizes their services routinely. Secondary team members are extended invitations to team educational workshops and activities. The core team is aware of referral procedures to secondary team members. CHARMS software is available in the HTC. All core team members have access to the CHARMS program. Clerical work for data entry is kept current. Wallet cards or FactorFirst cards are issued to registered patients and updated as needed. Policies and procedures for education of newly diagnosed patients are available. A variety of educational resources are available to distribute to patients, families and community. Policies & procedures are available on how to administer the home therapy program. There are patients registered in the home therapy program and the list of participants is available. There is documentation in the patient health record about participation in home therapy programme (including date of certification) Prophylaxis therapy is made available to the appropriate patients. A current list of patients on prophylaxis is available. The HTC has access to a special hemostasis laboratory, transfusion medicine department, and diagnostic imaging department. The HTC has a procedure for assigning priority for new patient referrals. Contact information for the HTC is current in listings with the Canadian Hemophilia Society, the World Federation of Hemophilia and parent hospital. Core team members are members of relevant organizations and / or working groups within the bleeding disorder community and communicate regularly with these organizations. Core team members, when able, serve on appropriate committees within the organization (AHCDC, CANHC, CPHC, and hospital). Key Indicators - 2. Quality Measures* 2-1a 2-1b 2-2a 2-2b 2-2c 2-3a 2-3b 2-4 2-5a Hospital records contain current HTC documentation that may include assessments by core team members stating patient goals, team recommendations, patient issues, and patient progress. Hospital records and clinic charts include documentation of telephone calls for patient advice and follow-up. Data is routinely exported from CHARMS to Centre Point. Factor utilization reports are available from the local CHARMS program. The HTC has the ability to monitor expiry dates of factor concentrates within its jurisdiction via the CHARMS program. Data is routinely exported from CHARMS to Centre Point. Registered patients are assigned a CHR number. If the HTC has clinic charts, the charts are stored appropriately to maintain privacy and confidentiality, and are accessible to appropriate team members. The HTC participates in hospital or peer evaluation and responds to critical appraisal. 2-5b There is a process to request adjustment in resources and to monitor services available to the patient population. Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s537 Matino D et al 2-6 2-7 2-8 2-9 Data is routinely exported from CHARMS to Centre Point. Centre volunteers to undergo accreditation process or responds to requests to do so. HTCs located in academic healthcare institutions provide professional educational opportunities. Patients and families have a mechanism in which to communicate concerns and compliments. Key Indicators - 3. Therapeutic Services* 3-1 3-2a 3-2b 3-3 3-4a 3-4b 3-5a 3-5b 3-5c 3-6 The members of the HTC have the appropriate training and qualifications to provide care to the patient population. The number of assessment clinics offered is sufficient to meet the standard of annual and semi-annual patient evaluation. The HTC provides a mechanism for team members to share knowledge with each other to promote best patient outcomes. Core team members are available for assessment clinics and urgent care. The HTC has resources available to ER departments regarding treatment and complications. HTC provides treatment recommendations to emergency departments and family physicians. Educational information is offered to patients and family on current issues/events related to bleeding disorders. Each core team member provides education and support to patients and families. Team members ensure that patients have sufficient information to make informed decisions. There are reference materials available to team members and students (i.e. AHCDC Clinical Practice Guidelines, journal articles and texts). 3-7 There are formal links to specialised laboratories and Canadian Blood Services 3-8a When participating in research or clinical trials, team members ensure the safety and well-being of the patient above all other objectives. 3-8b The HTC has contact information available (e.g. business cards). 3-9a When a patient moves to a location served by another HTC, the two centres will ensure that a formal transfer takes place promptly, including the forwarding of all relevant medical records, with patient consent. 3-9b Educational information is offered within the community as requested or needed (i.e. school, daycare). 3-10 There are reference materials available to team members and students (i.e. AHCDC Clinical Practice Guidelines, journal articles and texts). 3-11 The team has a mechanism to evaluate the home therapy program outcomes with participants. 3-12 Patients receive injection equipment and supplies free of charge 3-13 There are reference materials available to team members and students (i.e. AHCDC Clinical Practice Guidelines, journal articles and texts). 3-14 Physical clinic space is appropriate for people with disabilities or mobility aids. 3-15a There is private clinic space available for acute assessments and treatment. 3-15b The HTC ensures an adequate stock of factor concentrates is maintained within its institution. 3-16 The Emergency Department affiliated with the HTC has recommended treatment guidelines for registered patients. *Numbering of Key Indicators refers to the corresponding Standards Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s538 The haemophilia certification system in Canada Appendix 2 Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s539 Matino D et al Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s540 The haemophilia certification system in Canada Appendix 3 Blood Transfus 2014; 12 Suppl 3: s531-41 DOI 10.2450/2014.0032-14s s541 REVIEW The National Haemophilia Program Standards, Evaluation and Oversight Systems in the United States of America Mark W. Skinner1, J. Michael Soucie2, Kathryn McLaughlin3 1 National Hemophilia Foundation, Washington, DC; 2Division of Blood Disorders, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, US Department of Health and Human Services, Atlanta, GA; 3Genetic Services Branch, Division of Children with Special Health Care Needs, Maternal and Child Health Bureau, Health Resources and Services Administration, US Department of Health and Human Services, Washington, DC, United States of America Introduction The US National Hemophilia Program (NHP) is a collaborative relationship between the Maternal and Child Health Bureau (MCHB) of the Health Resources and Services Administration (HRSA), the Centers for Disease Control and Prevention (CDC) and the Medical and Scientific Advisory Council (MASAC) of the National Hemophilia Foundation (NHF). This article is written in three parts outlining the roles, collaborative and integrated working relationships of the three core entities (MCHB, CDC, NHF). We will discuss the birth and evolution of the modern day NHP and haemophilia treatment center (HTC) network, the evolution and role of surveillance programs, treatment guideline and standard setting, the impact of health care reform on access to comprehensive care and on-going initiatives to improve health outcomes for those living with haemophilia and related bleeding disorders. Although there is, at present, no formal HTC accreditation system in the US, we will describe a number of programs and systems that are already in place to promote and measure adherence to best practices, monitor patient outcomes and encourage continual operational and clinical improvement according to established standards. Finally, we will describe various initiatives that are underway to further develop evidencebased guidelines, which may lay the foundation for a future, formalised HTC self-audit evaluation or accreditation system. Discussion History of the evolution of HTCs in the US Legislative Authority Providing federal support to facilitate Federal-State partnerships on public health issues for women and children, specifically those in rural areas and with special health care needs, has been longstanding at HRSA, beginning with the passage of Title V of the Social Security Act in 19351. Title V funding to States helped support the development of an infrastructure to treat patients with haemophilia in the US since 19752. Title V funding has undergone many revisions since its passage in 1935: the most significant change relating to haemophilia occurred in 1981 with passage of the Omnibus Budget Reconciliation Act (OBRA '81), which converted the Title V program into a Maternal and Child Health (MCH) Block Grant program. In addition, with OBRA'81, 15 percent of the Title V appropriation for each fiscal year was set aside to support Special Projects of Regional and National Significance (SPRANS) as part of the MCH Block Grant3. Funding for federal haemophilia diagnostic and treatment centers (now known as the National Hemophilia Program) was included in the fifteen percent of the MCH Block Grant funds set aside for SPRANS programs; this appropriation remains to this day. Evolution of HRSA's National Hemophilia Program (NHP) The MCHB SPRANS funding for the NHP is administered through the Division of Children with Special Health Care Needs (DCSHN) by the Genetic Services Branch (GSB). The NHP has two distinct programmatic parts: the Regional Hemophilia Network (RHN) and the National Hemophilia Program Coordinating Center (NHPCC). The RHN comprises the HTCs that receive the grant funding directly from MCHB. The NHPCC provides technical assistance to the RHN on care delivery and program evaluation to support participating HTCs in complying with NHP roles and responsibilities as discussed below. The main purpose of the RHN is to establish integrated and collaborative regional networks to promote the comprehensive care of individuals with haemophilia and related bleeding disorders or clotting disorders such as thrombophilia. The primary goal of the RHN grant program is to ensure that individuals with haemophilia and other bleeding disorders and their families have access to appropriate, quality care and other medical expertise and information in the context of a medical home model that provides family-centered, comprehensive, and culturally effective care4. Providing Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s542 © SIMTI Servizi Srl US Haemophilia Treatment Center framework and evaluation comprehensive care through a core team of specialists is integral to being considered a federally qualified HTC and all HTCs within the network are required to comply with the NHF MASAC Recommendation 132 - Standards and Criteria for Persons with Congenital Bleeding Disorders, in order to qualify for federal funding as discussed below5,6. Since OBRA '81, MCHB has awarded funding for haemophilia through a regional approach using grants. In 2012, HRSA adjusted the regional structure from 12 historical regions to 8 regions, along with the development and implementation of the NHPCC. This organizational change was made to move from a regional to a national focus in terms of data collection and evaluation, as well as to better align program resources with patient needs. The RHN is currently comprised of 132 HTCs including 8 regional core centers. The regional core centers are funded as grants, however, the NHPCC was awarded as a cooperative agreement which allows the MCHB Program Officer to adjust work plans and timelines to better suit successful completion of goals and objectives. The core centers distribute available funding to their subrecipient HTCs within their regions and the number of HTCs is variable, depending on the geographic size of the region. The core centers are responsible for ensuring that their subrecipient HTCs comply with the roles and responsibilities laid out in the funding opportunity announcement published by HRSA. Advent of the NHPCC and its objectives During the discussions on how to organizationally restructure the NHP in 2011-2012, MCHB looked to other successful regional grant programs. Critical to the success of these other programs was the presence of a national coordinating center to compile and disseminate regional best practices; therefore, the decision was made to develop a similar funding opportunity for a NHPCC. The purpose of the NHPCC is to facilitate, coordinate, and evaluate (in terms of assisting in the development of regional and national evaluation plans) the activities carried out by the RHNs. Working collaboratively with the RHNs to develop a best practices model and establish a standard of care model will also be important activities. The American Thrombosis and Hemostasis Network (ATHN) ATHN was awarded funding as the NHPCC in June 2012. ATHN, as the NHPCC, is not an oversight or punitive organization, but one that provides technical assistance to the RHN on program evaluation, recruitment and retention of staff, as well as incorporation of genetics and public health into the NHP7. The genesis of ATHN dates back to the early 2000s, when specialists and clinicians who provide care to those living with haemophilia and others with rare bleeding disorders within the NHP acknowledged unmet needs within their community regarding collecting data and evaluating care for their patient populations with small numbers in the existing electronic medical record systems. During 2005 and early 2006, a broad range of key haemophilia stakeholders (e.g., haemophilia organizations, institutions, clinical disciplines, and experts in related fıelds of expertise) formed multiple clinical and operational working groups to assess the information needs of the community and develop a consensus approach to address them. The outcome of these deliberations led to the development of ATHN. ATHN's mission is "(…) to provide stewardship of a secure national database infrastructure to support standardised data collection, clinical outcomes analysis, research, advocacy, and public health reporting for the bleeding and clotting disorders community"8. Growth of the surveillance and data collection aspects CDC's Role CDC began its partnership with the US HTCs in the 1980s as part of public health efforts to prevent the spread of HIV infection resulting from use of treatment products made before the virus was identified. In 1991, in response to requests from constituents, Congress authorised CDC to expand its public health prevention activities with the aim of reducing the complications of bleeding disorders. Public health surveillance is the ongoing systematic collection, analysis, and interpretation of health data for purposes of improving health and safety9. In order to assess the public health needs of the haemophilia community, surveillance was conducted in six US states in 1993-1998. Data from this surveillance were used to assess the burden of haemophilia in the country and to identify sources of care and treatment practices. Data were also collected to measure rates and severity not only of infectious disease complications including hepatitis and HIV but also those of chronic joint disease, intracranial hemorrhage and other bleeding complications as well as mortality. Analyses of these population-based surveillance data revealed an estimated US haemophilia population of about 17,000, nearly 70% of which had received care in HTCs10. Although most of those not receiving care in HTCs had mild haemophilia, 34% of those with moderate and 14% of those with severe disease received care outside of the HTC network. When outcomes were compared, males with haemophilia who had received care from HTCs had lower mortality rates 11 and fewer hospitalizations for bleeding complications12. Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s543 Skinner MW et al This population-based surveillance system was replaced in 1998 with the Universal Data Collection (UDC) surveillance system established in the HTC network in order to collect the more detailed data needed to inform and evaluate public health prevention programs13. For example, analyses of UDC data on height and weight and joint range of motion measurements lead to the recognition that increased body mass index (a measure of body adiposity) was associated with decreased joint mobility regardless of haemophilia severity14. Based on these findings it became clear that overweight and obesity, at epidemic levels in the general US population, was not only just as common among boys and men with haemophilia but also was contributing to preventable joint disease. Public health messages about the need to maintain a healthy weight to protect joints are part of the prevention strategies implemented because of these findings. Continued surveillance will be used to evaluate these prevention efforts. The UDC also included annual blood sample collection with infectious disease testing performed at CDC in order to assess the safety of treatment products. Results of this surveillance have provided evidence for the safety of these products as well as the need for continued vigilance15,16. UDC surveillance data have also been used to examine patterns of care within the HTC network. For example, the administration of treatment product on a regular basis to prevent bleeding episodes, called prophylaxis therapy, has been shown to prevent joint disease in young boys with haemophilia17. However, in an analysis of UDC data there was a full spectrum of variation from 0% to 100% of youth in individual HTCs who were receiving prophylaxis therapy18. These kinds of analyses can be useful both to monitor the adoption of standards of care as well as to gain an understanding of facilitators and barriers to the practices by studying the characteristics of HTCs with high and low adoption rates. Another example of using surveillance data is in the identification of an inhibitor, which is currently the most serious complication of haemophilia treatment. An inhibitor is an antibody to treatment product that develops in up to one-third of people with haemophilia and renders it ineffective in preventing or stopping bleeding episodes. People with an inhibitor are more likely to be hospitalised for a bleeding complication and treatment costs are far greater than those without an inhibitor19-21. A blood test is necessary for diagnosing an inhibitor. Earlier identification of inhibitors, accomplished through regular screening, leads to higher inhibitor eradication success22. From 2006-2010, only 46% of patients with severe haemophilia (those at highest risk of an inhibitor) had a screening test performed (unpublished CDC data). Furthermore, similar to the rates of primary prophylaxis, inhibitor testing varied from 0% to 100% among the HTCs. Based on discussions with experts, a substantial barrier to regular inhibitor screening was the lack of capacity of most local laboratories to accurately perform the necessary testing in the presence of infused factor VIII, especially among patients who were receiving prophylactic therapy (unpublished CDC data). To address this barrier, the CDC Division of Blood Disorder's laboratory has developed and validated a modified testing method that can be used to screen for an inhibitor regardless of treatment status23. This method is being disseminated to local laboratories and its use for regular screening for inhibitors should become part of the standard of care for HTCs. The UDC has recently been updated (now called Community Counts) to include national monitoring of inhibitors through the use of both local and CDC testing of blood specimens collected as part of the surveillance. Using data from Community Counts will allow CDC to monitor the adoption of this important testing as a new standard of care. Current Status of the National Hemophilia Program and long term objectives CDC's Public Health Surveillance for the prevention of complications of bleeding and clotting disorders cooperative agreement is the funding mechanism through which its surveillance and prevention programs are funded. In 2011, the RHN applied for the CDC funding through ATHN. As part of the new cooperative agreement, the data elements collected through the new surveillance system were revised based on recommendations from an expert panel through a collaborative process between CDC scientists and a scientific committee comprised of clinicians organised and supported by ATHN. Community Counts, the new surveillance system has three components: 1) the HTC Population Profile; 2) Mortality Reporting; and 3) the Registry for Bleeding Disorders Surveillance. The first component collects a minimum set of demographic and clinical information on all of the patients with bleeding and clotting disorders who are receiving care within the RHN. The second component collects limited data about causes of death. The third component will be a more in-depth data collection project that will collect more complex data elements on health and complications, including collecting biologic samples for infectious disease and inhibitor surveillance. This collaboration marks an exciting new prospect for the haemophilia community as some data elements from the CDC's project will be utilised by the RHN and NHPCC to report as the national data source for several developmental Healthy People 2020 performance measures within the blood disorders and blood safety Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s544 US Haemophilia Treatment Center framework and evaluation topic objective24. Healthy People is a national effort by the US Department of Health and Human Services to develop measures and benchmarks to track national progress, in 10-year cycles, on government efforts to improve the public health of the country25. With the new regional organization and the development of ATHN as the national coordinating center, the NHP is well placed to accomplish goals and activities that have not previously been possible given the lack of focus on working on a national level. Since June 2012, the RHN and the NHPCC has completed the first ever technical assistance needs assessment for HTC Staff, currently under analysis, which will provide insight to HRSA on the help needed by HTC staff both in the management of patient care and in navigating the federal grant process as well as informing HRSA how the NHPCC can begin to provide needed services. The program is also currently analyzing the results of the first national HTC patient needs assessment that was a requirement for both the RHNs and the NHPCC to accomplish, so that the haemophilia community can use the results to set national priorities for the program to help with the development of a national evaluation plan to track the improvement of the care received in the coming years. A third party evaluation consultant has been contracted by both the NHPCC and the regions to analyze the results of the needs assessment, on both a regional and national level. The results of the analysis will be utilised to set national priorities for the NHP through a multistakeholder process involving the regions, the NHPCC, consumer advocacy groups, and our federal partners. The national priorities, once determined, will form the basis of a national evaluation plan to track patient outcomes for those who receive care through the NHP. Results of the patient needs assessment will be widely disseminated within the federal program and haemophilia consumer advocacy groups and other stakeholders within the bleeding community. Finally, these major projects and increased requirements for data collection and evaluation plans will inform the development of standards of care and methods for dissemination of best practices, which will require the assistance and expertise of the National Hemophilia Foundation's MASAC, whose efforts are described below. The role of the NHF MASAC in standard setting Impact of the Affordable Care Act Federal enactment of the Patient Protection and Affordable Care Act26 on March 23, 2010 came with a promise to provide quality affordable health care for all Americans. Since then, the US health care system has been undergoing a major overhaul impacting both insurance availability and the delivery of care. The Affordable Care Act contains many long sought improvements for those living with high cost diseases or having pre-existing conditions such as haemophilia. The substantial growth in managed care plans and the many changes to private and public insurance programs made by the Affordable Care Act are having direct and indirect consequences for the bleeding disorders community. The Affordable Care Act provides for the establishment of essential health benefits that must be offered by new plans available in the insurance market. However, the choice of health care providers available to an insured within a plan is left to the insurance plan provider, subject to rules requiring access to a minimum percentage of the essential community providers in the plan service area27. These rules encourage, but do not require, insurers to include access to a federally funded HTC within their provider networks. To reduce reliance on expensive drugs and incentivize patients to choose lower-cost generic alternatives, if available, some plans are requiring higher cost-sharing (co-payments and coinsurance) for medications such as clotting factor concentrates. While the Affordable Care Act has the potential to increase patient access to needed treatments and services, it is too early to evaluate how this translates into outcomes for people with bleeding disorders. The Affordable Care Act also contained provisions placing a greater emphasis on evidence-based medicine and performance outcomes measures. Thus, establishing and bolstering evidence-based standards and recommendations to support haemophilia care and its delivery through a recognised HTC has taken on an increased importance. Over many years, the NHF and its MASAC have led the development of a range of standards and recommendations addressing clinical management, treatment safety, and care delivery for those living with a bleeding disorder. Issued in the form of recommendations, MASAC guidelines set the standard of care and are frequently referred to by an international array of physicians, medical schools, pharmacists, emergency room personnel, insurance companies, patients and others. MASAC is comprised of scientists, physicians, allied health professionals, patients and government liaisons from the relevant federal agencies within the US Department of Health and Human Services (CDC, Food and Drug Administration, MCHB and the National Institutes of Health). The full list of recommendations are available on the NHF website28. Adherence to MASAC recommendations is widely promoted, however, outside of the specific requirements with the NHP compliance with other MASAC recommendations is voluntary. Two MASAC recommendations are of particular note with regard to the oversight and management of US HTCs: 1) MASAC Recommendation 132 - Standards and Criteria for Persons with Congenital Bleeding Disorders29. Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s545 Skinner MW et al Last revised in 2002, MASAC Recommendation 132 outlines comprehensive standards of care and lists services that should be provided by HTCs. The recommendation includes an extensive discussion of the delivery of integrated, multi-disciplinary, comprehensive care. The recommendation places an emphasis on early diagnosis and intervention to prevent disease complications. The composition, general and specific functions, availability and training of the Comprehensive C a r e Te a m d e p e n d o n p a t i e n t c e n s u s a n d individual circumstance. The staff and services required for proper HIV care for men and women, haepatitis-related services, care for women with bleeding disorders, the need for culturally sensitive outreach programs, and access to clinical research protocols are also addressed. Within the NHP, all HTCs are required and expected to comply with and follow the guidelines for elements and core services of the HTC-based model of care delineated in Recommendation 132. 2) MASAC Recommendation 188 - Standards of Service for Pharmacy Providers of Clotting Factor Concentrates for Home Use to Patients with Bleeding Disorders30. A varied range of pharmacy providers supply clotting factor concentrates to patients for treatment at home. The pharmacy providers are principally specialty pharmacies or factor programs administered through the HTC. When patients do not receive optimal service from these providers, there is potential for adverse health events that lead to poor outcomes and/ or increased costs30. Given challenges in achieving optimal service, MASAC adopted standards of service for pharmacy providers. MASAC acknowledged the necessity of cost efficiency in the provision of health care, yet emphasised that cost efficiency should not occur at the expense of quality patient care. The purpose of the recommendation is to establish minimum standards of service for pharmacy providers to meet the specific needs of individuals with bleeding disorders. The standards address pharmacy provider staff knowledge, availability of clotting factor concentrates and ancillary supplies, processing of prescription orders, hours of operation, access to pharmacy staff, delivery, recordkeeping, billing and product recall. Over 30 national specialty pharmacies and most US HTCs have voluntarily self-reported they have met or exceeded the standards of Recommendation 188. At the state level, various legislative and regulatory initiatives have been implemented to promote optimal access to home care services to further reinforce the importance of pharmacy standards. The most prominent and widely cited examples of best practice of model legislation are New Jersey and more recently Missouri31-33. As this article was written, a number of states are considering adoption of similar statutory or regulatory provisions. The National Association of Boards of Pharmacy recently featured a news article profiling the NHF model standards of service and is working with NHF to achieve uniformity in the regulation of this specialty area34. In 1997, New Jersey included language in state Health Maintenance Organization (HMO) regulations securing access to and reimbursement for care at HTCs. In 2000, legislation was enacted requiring HMO and managed care insurers to comply with standards in the provision of benefits to patients with haemophilia31. Insurance carriers offering managed care health benefit plans in New Jersey must contract with designated health care providers for the delivery of services for the home treatment of bleeding episodes associated with haemophilia, including the purchase of blood products and blood infusion equipment. The State maintains an on-line registry of designated haemophilia home care providers meeting statutory requirements32. Building on the New Jersey precedent, in 2011, Missouri enacted legislation33 creating standards of care for pharmacies dispensing blood-clotting therapies. The Missouri HealthNet Division (which oversees Medicaid) previously covered blood clotting products and services. The law specifically adds blood clotting equipment, supplies, and assessments in the home to the list of Missouri HealthNet benefits. Development of evidence-based clinical practice guidelines for Comprehensive Care NHF is acutely aware of the major ongoing changes in health care occurring in the US. In 2012, the NHF held a strategic summit to develop a plan for haemophilia care within the evolving US health care environment. The Summit report addressed the implications of the Affordable Care Act and provided a series of strategic recommendations35. Among these was a call for NHF to sponsor the production and maintenance of evidence-based clinical practice guidelines (CPGs). Health plans are taking note of the geographic variations in practice and standards of practice (e.g. prophylaxis regimens) and clinical behavior (e.g. use of comprehensive care services). Such variations suggest insufficient evidence to support practice or a lack of clinician concurrence about, or adherence to, evidence-based practice. Recognizing the value of establishing, promoting, and adhering to CPGs and associated standards of practice, the NHF and its MASAC leadership launched an initiative to develop a comprehensive set of evidence-based CPGs to support patient-centered clinical decision-making and optimize care. Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s546 US Haemophilia Treatment Center framework and evaluation The initial phase of the CPG initiative addresses the comprehensive care model for haemophilia. In addition to recognizing the importance of a range of coordinated services to most patients with haemophilia, addressing the comprehensive care model as the first evidence-based CPG will establish a foundation upon which more specific CPGs addressing other aspects of care may be developed. The comprehensive care CPG will: - define comprehensive care as it relates to the haemophilia patient; - specify the coordinated set of diagnostic, therapeutic, and certain auxiliary and supplemental services that are most important for haemophilia patients across the U.S.; - identify the range of clinical and non-clinical members of a haemophilia comprehensive care team (including, e.g., social workers, dentists); - identify best-practices and evidence-based standards of comprehensive/coordinated care for haemophilia treatment centers (HTCs) and individual clinical practices. NHF foresees that the development of the comprehensive care CPG will provide a catalyst to promote harmonization of care delivery and reduce practice variations among the US HTC system. An agreed evidence-based benchmark would allow for both internal and external evaluation of adherence to best practices and benchmark available services with an HTC. Ultimately, it will serve as an important starting point for establishment of a US HTC self-audit or accreditation system. Keywords: Haemophilia Treatment Center, Program evaluation, Child Health Bureau (MCHB), Centers for Disease Control and Prevention (CDC), National Hemophilia Foundation (NHF). Acknowledgments and disclosures Mark Skinner serves as a consultant to the National Hemophilia Foundation. CDC Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) The Authors declare no conflicts of interest. References 1) 2) Katherine B. Oettinger. Title V of the Social Security Act: What it has meant for children. Social Security Bulletin. V23; No8, pgs 39-50, August, 1960. Available at: http://www. ssa.gov/policy/docs/ssb/v23n8/v23n8p39.pdf. Accessed on 19/01/2014. Understanding Title V of the Social Security Act: A Guide to the Provisions of the Federal Maternal and Child Health Block Grant. Maternal and Child Health Bureau, Health Resources and Services Administration. Available at: http://www.amchp. org/AboutTitleV/Documents/UnderstandingTitleV.pdf. Accessed on 18/01/2014. 15) 16) 17) Understanding Title V of the Social Security Act: A Guide to the Provisions of the Federal Maternal and Child Health Block Grant. Maternal and Child Health Bureau, Health Resources and Services Administration., Available at: http://www. amchp.org/AboutTitleV/Documents/UnderstandingTitleV. pdf. Accessed on 18/01/2014. Funding Opportunity Announcement: Regional Hemophilia Network. Announcement No. HRSA-12-133, CFDA# 93.110, FY 2012. Release Date: 11/16/2011; Due Date: 01/10/2012. Available at: https://grants3.hrsa.gov/2010/Web2External/ Platform/Interface/DisplayAttachment.aspx?dm_rtc=16&dm_ attid=89e6028e-37f2-4411-8334-acd06b02d5db&dm_ attinst=0. Accessed on 18/01/2014. NHF MASAC Recommendation 132 - Standards and Criteria for the care of Persons with Congenital Bleeding Disorders. National Hemophilia Foundation. Available at: http://www. hemophilia.org/NHFWeb/Resource/StaticPages/menu0/ menu5/menu57/masac132.pdf. Accessed on 20/01/2014. Funding Opportunity Announcement: Regional Hemophilia Network. Announcement No. HRSA-12-133, CFDA# 93.110, FY 2012. Release Date: 11/16/2011; Due Date: 01/10/2012. Available at: https://grants3.hrsa.gov/2010/Web2External/ Platform/Interface/DisplayAttachment.aspx?dm_rtc=16&dm_ attid=89e6028e-37f2-4411-8334-acd06b02d5db&dm_ attinst=0. Accessed on 18/01/2014. Funding Opportunity Announcement: National Hemophilia Program Coordinating Center. Announcement No. HRSA-12135, CFDA# 93.110, FY 2012. Release Date: 11/16/2011; Due Date: 12/30/2011. Available at: https://grants3.hrsa.gov/2010/ Web2External/Interface/FundingCycle/ExternalView. aspx?&fCycleID=EDA323E3-02AC-483A-ABE6-92474D2 335EF&txtAction=View+Details&submitAction=Go&View Mode=EU. Accessed on 18/01/14. Aschman DJ, Abshire TC, Shapiro AD, et al. A CommunityBased Partnership to Promote Information Infrastructure for Bleeding Disorders. Am J Prev Med 2011; 41 (6S4): S332-7. Available at: http://www.ajpmonline.org/article/S07493797%2811%2900680-5/fulltext. Accessed on 20/01/2014. Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev 1988; 10: 164-90. Soucie JM, Jackson D, Evatt B. The occurrence of hemophilia in the United States. Am J Hematol 1998; 59: 288-94. Soucie JM, Nuss R, Evatt B, et al and the Hemophilia Surveillance System Project Investigators. Mortality among males with hemophilia: relations with source of medical care. Blood 2000; 96: 437-42. Soucie JM, Symons J, Evatt B, et al and the Hemophilia Surveillance System Project Investigators. Home-based factor infusion therapy and hospitalization for bleeding complications among males with hemophilia. Haemophilia 2001; 7:198-206. Soucie JM, McAlister S, McClellan A, et al. The universal data collection surveillance system for rare bleeding disorders. Am J Prev Med 2010; 38 (4 Suppl): S475-81. Soucie JM, Cianfrini C, Janco RL, et al. Joint range of motion limitations among young males with hemophilia: Prevalence and risk factors. Blood 2004; 103: 2467-73. Centers for Disease Control and Prevention. Blood safety monitoring among persons with bleeding disorders - United States, May 1998-June 2002. MMWR Morb Mortal Wkly Rep 2003; 51: 1152-4. Soucie JM, De Staercke C, Monahan PE, et al. Evidence for the Transmission of Parvovirus B19 in Patients with Bleeding Disorders Treated with Plasma-derived Factor Concentrates in the Era of Nucleic Acid Test (NAT) Screening. Transfusion 2013; 53: 1217-25. Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med 2007; 357: 535-44. Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s547 Skinner MW et al 18) Soucie JM, McAlister S, McClellan A, et al. The universal data collection surveillance system for rare bleeding disorders. Am J Prev Med 2010; 38 (4 Suppl): S475-81. 19) Soucie JM, Symons J, Evatt B, et al and the Hemophilia Surveillance System Project Investigators. Home-based factor infusion therapy and hospitalization for bleeding complications among males with hemophilia. Haemophilia 2001; 7: 198-206. 20) Guh S, Grosse SD, McAlister S, et al. Healthcare expenditures for males with haemophilia and employer-sponsored insurance in the United States, 2008. Haemophilia 2012; 18: 268-75. 21) Guh S, Grosse SD, McAlister S, et al. Health care expenditures for Medicaid-covered males with haemophilia in the United States, 2008. Haemophilia. 2012; 18: 276-83. 22) DiMichele DM. Immune tolerance in haemophilia: the long journey to the fork in the road. Brit J Haematol 2012; 159: 123-34. 23) Miller CH, Rice AS, Boylan B, et al, the Hemophilia Inhibitor Research Study Investigators. Comparison of clot-based, chromogenic, and fluorescence assays for measurement of factor VIII inhibitors in the U.S. Hemophilia Inhibitor Research Study (HIRS). J Thromb Haemost 2013: 11; 1300-9. 24) Healthy People 2020. Blood Disorders and Blood Safety Topic Objectives. Available at: http://www.healthypeople.gov/2020/ topicsobjectives2020/overview.aspx?topicid=4. Accessed on 20/01/2014. 25) HHS News Press Release: HHS announces the nation's new health promotion and disease prevention agenda. OASH Press Office. Released December 2, 2010. Available at: http:// www.healthypeople.gov/2020/about/DefaultPressRelease.pdf. Accessed on 20/03/2014. 26) Pub L. 111-148, 111th United States Congress. Washington, DC. March 23, 2010. 27) HHS Centers for Medicare and Medicaid Services. Letter to Issuers in the Federally-facilitated Marketplace. March 14, 2014. Available at: http://www.cms.gov/CCIIO/Resources/ Regulations-and-Guidance/Downloads/2015-final-issuerletter-3-14-2014.pdf. Accessed on 26/03/2014. 28) NHF MASAC Recommendations. National Hemophilia Foundation. Available at: http://www.hemophilia.org/NHFWeb/ MainPgs/MainNHF.aspx?menuid=157&contentid=347. Accessed on 20/03/2014. 29) NHF MASAC Recommendation 132 - Standards and Criteria for the care of Persons with Congenital Bleeding Disorders. National Hemophilia Foundation. Available at: http://www. hemophilia.org/NHFWeb/Resource/StaticPages/menu0/ menu5/menu57/masac132.pdf. Accessed on 20/03/2014. 30) NHF MASAC Recommendation 188 - Standards of Service for Pharmacy Providers of Clotting Factor Concentrates for Home Use to Patients with Bleeding Disorders. National Hemophilia Foundation. Available at: http://www.hemophilia. org/NHFWeb/Resource/StaticPages/menu0/menu5/menu57/ masac188.pdf. Accessed on 20/03/2014. 31) New Jersey Statues Annotated. Section 1 of L. 2001, c. 121, codified at N.J.S.A. 26:2S-10.1, and sections 3 through 10 of L. 2001, c. 121, variously codified throughout Titles 17, 17B and 26. Available at: http://njlaw.rutgers.edu/cgi-bin/njstats/ showsect.cgi?title=26&chapter=2S&section=10.1&actn=get sect. Accessed on 20/03/2014. 32) New Jersey Designated Hemophilia Providers. Available at: http://www.state.nj.us/dobi/division_insurance/managedcare/ mchemoprov.htm. Accessed on 20/03/2014. 33) Missouri Revised Statues. RSMo 338.400. Available at: http:// www.moga.mo.gov/statutes/C300-399/3380000400.HTM. Accessed on 20/03/2014. 34) States Look at Standards of Service for Pharmacies Serving Hemophilia Patients. NABP Newsletter. 2013; June-July: 12830. Available at: http://www.nabp.net/system/redactor_assets/ documents/618/Final_June-July_2013_Newsletter.pdf. Accessed on 20/03/2014. 35) National Hemophilia Foundation: Strategic Summit Report. October 2012. National Hemophilia Foundation. Available at: http://www.hemophilia.org/NHFWeb/MainPgs/MainNHF. aspx?menuid=119&contentid=2120. Accessed on 20/03/2014. Correspondence: Mark W. Skinner National Hemophilia Foundation 1155 23rd Street NW #3A Washington, DC 20037, USA e-mail: mskinnerdc@gmail.com Blood Transfus 2014; 12 Suppl 3: s542-8 DOI 10.2450/2014.0019-14s s548 DEFINITION OF AN ORGANISATIONAL MODEL FOR THE PREVENTION AND REDUCTION OF HEALTH AND SOCIAL IMPACTS OF INHERITED BLEEDING DISORDERS IN ITALY Blood Transfus 2014; 12 Suppl 3 © SIMTI Servizi Srl REVIEW Institutional accreditation of Health Services in Italy: the long road to quality Antonio Fortino¹, Francesco Di Stanislao2 ¹National Institute for Health, Migration and Poverty (INMP), Rome; 2Marche Polytechnic University and National Agency for Regional Health Care Services (Age.Na.S.), Rome, Italy Introduction The term "accreditation" was introduced in Italian health legislation in the early '90s, with the adoption of decrees 502/1992 e 517/19931. The concept added a new element to the authorisation system defined in Law n. 833, that had established the Italian National Health Service (SSN) in 1978. It has developed over time into an institutional recognition, issued by the Public Authority, that is a statutory requirement for any entity providing services as part of the SSN. It aims to achieve a high level of guarantee of service quality and of the selection of service providers, public and private, that work as part of, or on behalf of, the SSN. Specifically, the National Health Plan 1998-2000 identified the accreditation as one of instruments for ensuring quality of healthcare in that it "responds to the need for a process of provider selection that applies healthcare quality criteria", thus clearly identifying their essential aims and characteristics. The implementation of this policy was slow and difficult, not only because of the strength of economic interests associated with healthcare activity and the birth of federalism in healthcare provision, but also because of a widespread culture that tends to give more importance to the work of the individual healthcare professional than to achieving a well-integrated and co-ordinated system as a whole, with attention to, and demonstration of, transparency in terms of inputs (resources) and outputs (processes, results and outcomes). Regulatory development between national and regional level In order to achieve a smooth transition from the previous contracting system to the new accreditation system, Law 724/1994 introduced the concept of "Temporary Accreditation" for those entities already contracted on January 1st 1993, subject to the acceptance of the fixed price system for services provided. Unfortunately that transitional period, that was intended to apply only during 1995 and 1996, was prolonged in most Italian regions and was finally revoked only in 2008. During the same period, in response to legal appeals by some regions, the Constitutional Court was deliberating on the subject of accreditation, providing clarifications on the meaning and specifying that "accreditation" was distinct from "authorisation" and that it constituted a second step in the process. As a consequence, it was impossible for the implementation to proceed without the enactment of the government decree establishing the minimal requirements for authorisation (licensure). This was due for adoption in 1993 but was not, in fact, published until 4 years later, in 19972. No instruction was provided to the regional Authorities regarding the terms "accreditation", or "control and quality improvement"; their definition remained at the level of technical and academic discussion3. In 1999, the so-called "Third Reform of the National Health Service"4 elaborated and defined the entire subject of authorisation and institutional accreditation in the following terms: - authorisation for construction is the administrative measure that permits the construction of new health and social health buildings on the basis of real need with regard to regional planning; - authorisation for practice is the administrative measure (licensure) that permits the practice of health or social health activities by public or private subjects. This authorisation is released on the basis of the demonstration of compliance with minimal structural, technological and organisational requirements; - institutional accreditation is the administrative measure through which a region authorises an entity to provide services in the name and on behalf of the SSN. It is released subject to verification of compliance with a further series of requirements. Through the accreditation process, each regional Authority constructs its own list of service providers, specifically qualified. In the latter case, contractual agreements can be established in which the regional Authorities and local health service organisations define, together with public and private accredited entities, the type and the quantity of services to be provided to the regional health service, the health objectives and the means of integration, as well Blood Transfus 2014; 12 Suppl 3: s551-3 DOI 10.2450/2014.0014-14s © SIMTI Servizi Srl s551 Fortino A, Di Stanislao F as the associated prices to be paid by the public service. Since 1999, there have not been substantial modifications to the legislative framework established by Law 229/99. However, the basis of the institutional relationships between the State and the regions has changed considerably following the reform of Part V of the Italian Constitution (Constitutional Law n. 3 of 2001), which increased the powers of the regional Authorities, enlarging their competence for the organisation of health services. As a result, 21 models for regional accreditation developed in the subsequent decade. These had some characteristics in common but there were significant differences too; the models were summarised in a study by the National Agency for Regional Health Care Services (Agenzia Nazionale per i Servizi Sanitari Regionali - Age.Na.S.) published in 20095. The quality criteria most frequently found in the regional provisions are: patient satisfaction, service access, communication, continuous quality improvement, presence of guidelines and protocols, information and data management, technology assessment, appropriateness and continuity of service provision. Age.Na.S. revisited the topic in 2013, updating and exploring it in more depth, summarising the entire picture of regional planning for authorisation accreditation and focusing on the more recent measures and, in particular, on those adopted to finally overcome temporary accreditation6. In more recent years, there has been a move towards ever greater harmonisation and sharing of approaches between the regional Authorities, a process that has been reinforced by challenges from Europe. Two agreements between the State and the regional Authorities on December 16 th 2010 addressed the quality, safety and appropriateness of the maternity care pathway and blood activities and transfusion medicine7. The agreement prioritised the adoption of uniform health and accreditation policies (including a requirement for a minimum of 1,000 births per year). Two important measures were adopted on July 25th 2012 that promoted national standardisation in a more detailed manner. One was the "Agreement" on guidelines for the accreditation of blood Establishment and blood collection Units and the other was the "Understanding" on standards for the accreditation of hospices and for palliative care and pain therapy units. Lastly, the Agreement of March 13th 2013 on the definition of regional or inter-regional care pathways for patients with congenital haemorrhagic disorders defines general instructions and 23 specific "activities" that organisations accredited for the management of these patients must accomplish8. At the end of this long journey, the destination is also a point of departure: the "Understanding" between the State and the regions of December 20th 2012 defines 8 macro criteria, 28 macro requirements and 123 specific elements of evidence, on the basis of which the regional Authorities are reformulating and updating their own measures for institutional accreditation: operation of a comprehensive management system with identification of roles and responsibilities, description of the range of services provided, suitability of the facilities and equipment, specific competencies of the personnel, communication between professionals and with patients, appropriate clinical practice and risk management, process improvement and innovation and humanisation9. Conclusions Institutional statutory accreditation is in a phase of renewal in the SSN, with a movement toward ever greater convergence between the regional models, in the interest of greater standardisation, uniformity and quality of the health services delivered to citisens10. We look forward to a new phase of intense co-operation between the State and the regional Authorities, the professionals and the Health Service organisations. Keywords: accreditation system, quality, requirements, health service. The Authors declare no conflicts of interest. References 1) 2) 3) 4) 5) 6) Decreto Legislativo 30 dicembre 1992, n. 502: Riordino della disciplina in materia sanitaria, come modificato dal Decreto Legislativo 7 dicembre 1993, n. 517 "Modificazioni al decreto legislativo 30 dicembre 1992, n. 502, recante riordino della disciplina in materia sanitaria, a norma dell'articolo 1 della legge 23 ottobre 1992, n. 421". Decreto del Presidente della Repubblica 14 gennaio 1997: Approvazione dell'atto di indirizzo e coordinamento alle regioni e alle province autonome di Trento e di Bolzano, in materia di requisiti strutturali, tecnologici ed organizzativi minimi per l'esercizio delle attività sanitarie da parte delle strutture pubbliche e private. Di Stanislao F, Liva C. L'Accreditamento dei Servizi Sanitari in Italia. Centro Scientifico Editore, Torino, 1998. Decreto legislativo 19 giugno 1999, n. 229: Norme per la razionalizzazione del Servizio sanitario nazionale, a norma dell'articolo 1 della legge 30 novembre 1998, n. 419 Age.Na.S. - Agenzia Nazionale per i Servizi Sanitari Regionali: Analisi delle dimensioni della qualità presenti nei programmi di accreditamento istituzionale delle regioni italiane. Rapporto agosto 2009. Age.Na.S - Agenzia Nazionale per i Servizi Sanitari Regionali: Ricognizione delle norme regionali sull'accreditamento istituzionale. Available at: www.agenas.it/accreditamento. html. Accessed on 29/11/2013. Blood Transfus 2014; 12 Suppl 3: s551-3 DOI 10.2450/2014.0014-14s s552 Institutional accreditation of health services in Italy 7) 8) 9) Accordo Stato regioni su: Requisiti strutturali, tecnologici e organizzativi minimi per l'esercizio delle attività sanitarie dei servizi trasfusionali e delle unità di raccolta del sangue e degli emocomponenti e sul modello per le visite di verifica. (Rep. Atti n. 242/CSR del 16 dicembre 2010). Accordo Stato Regioni su: Definizione dei percorsi regionali o interregionali di assistenza per le persone affette da Malattie Emorragiche Congenite (MEC). (Rep. Atti n. 66/CSR del 13 marzo 2013). Intesa Stato Regioni su: Disciplinare per la revisione della normativa dell'accreditamento, in attuazione dell'articolo 7, comma 1, del nuovo Patto per la salute per gli anni 20102012. (Rep. Atti n. 259/CSR del 20 dicembre 2012). 10) Di Stanislao F, Bellentani D, Gangale A, et al. L'accreditamento nella legislazione italiana e le sue differenze regionali. Revue Sociologie Santé - Sociologia della Salute 2010; 32: 109-30. Correspondence: Antonio Fortino Istituto Nazionale Malattie Migrazione e Povertà (INMP) Via di San Gallicano, 25 00153 Rome, Italy e-mail: fortino@inmp.it Blood Transfus 2014; 12 Suppl 3: s551-3 DOI 10.2450/2014.0014-14s s553 REVIEW Current and evolving features in the clinical management of haemophilia Antonio Coppola1, Massimo Morfini2,, Ernesto Cimino1, Antonella Tufano1, Anna M. Cerbone1, Giovanni Di Minno1 1 Regional Reference Centre for Bleeding Disorders, Federico II University Hospital, Naples; 2Italian Association of Haemophilia Centres (AICE), Florence, Italy Introduction After the devastating consequences of acquired immunodeficiency syndrome (AIDS) and viral hepatitis epidemics due to the transmission of the human immunodeficiency (HIV) and hepatitis C (HCV) viruses through contaminated coagulation factor concentrates, leading to death of thousands of patients in the 1980s and 1990s, over the past three decades dramatic advances in the treatment and the overall management of haemophilia were achieved1. These improvements of care, at least in high-income countries, presently warrant persons with haemophilia a highly satisfactory quality of life and a progressive increase in life expectancy, now approaching that of the general male population2. Such advances rely upon the continuous improvement of factor concentrate safety and availability, from viral-inactivated plasmaderived products to the different generations of recombinant concentrates1,3,4. Indeed, thanks to the implementation of techniques for inactivating or eliminating possible contaminating viruses from plasmaderived factor concentrates, together with rigorous criteria for selection of donors and the adoption of nucleic acid testing (NAT) of donations and plasma pools, no cases of blood-borne transmission of known virus from plasma products have been reported over the last 25 years1. In parallel, rapid progresses in DNA recombinant technology led to the availability of products removing any trace of human or animal protein from the final formulation, and then from the culture medium and the whole purification process5. The availability of larger amounts of safe products, together with increasing evidence from literature of cost-effectiveness, made possible the diffusion of prophylaxis (i.e. regular infusion regimens of factor concentrates with the aim to prevent bleeding and bleeding-related complications), currently the standard of care in children with severe haemophilia, i.e. those with virtually absent residual factor (F) VIII/IX activity1,6, but increasingly adopted even later in life with favourable clinical outcomes7,8. These advances were significantly promoted thanks to the recognition, implementation and continuous improvement of a multidisciplinary approach in the delivery of care at specialised haemophilia treatment centres (HTCs)9. Indeed, comprehensive haemophilia care is multidisciplinary by nature, in order to face adequately the variable patients' clinical needs from diagnosis onwards throughout life, including treatment of bleeding, education to home treatment, prevention and treatment of haemophilia- and treatment-related complications, as well of other co-morbidities. These clinical and organisational needs are presently even more complex in the light of the evolving scenario of ageing haemophilia patients10. Multi-centre and multi-national efforts in addressing unsolved clinical issues and improving the level of evidence for treatment recommendations have been strongly pursued, together with the development of documents setting basic elements of haemophilia care provision to make available or assisting healthcare providers in implementing care programs and encouraging practice harmonization around the world9,11-16. Although relevant challenges remain, in particular concerning venous access and patients with inhibitors17, and awaiting for further improvements by new factor concentrates with extended half-life on clinical trials18 and by developments in gene therapy overcoming previously disappointing findings19, the comprehensive management of haemophilia, well beyond the treatment of bleeding, may presently focus on warranting the best possible quality of life for patients and their families, tailoring treatment choices and regimens according to specific needs. In the following paragraphs, these aspects and open issues of modern management of haemophilia will be briefly reviewed. Prophylaxis for all: between evidence and personalised treatment In the third millennium two randomised clinical trials ([RCTs] the US Joint Outcome Study12 and the Italian ESPRIT20) unequivocally showed the superiority of prophylaxis over on-demand treatment in the management of children with severe haemophilia, in terms of lower bleeding rates and better joint outcomes and quality of life12,20. These methodologically rigorous trials confirmed what had been long achieved over more than 40 years of clinical experience started in Northern Europe, reported in retrospective cohort studies6,21,22 and in a large prospective international study, the Orthopedic Outcome Study23, and recommended by the World Health Organization Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s554 © SIMTI Servizi Srl Current evolving management of haemophilia (WHO) and the World Federation of Hemophilia (WFH) since 199424. The role of prophylaxis in promoting health and social well-being of haemophiliacs, and reducing the burden of their condition, was stated among the European principles of haemophilia care by the European Association for Haemophilia and Associated Disorders (EAHAD) in 20099. Thanks to the results from the RCTs, a grade 1A recommendation was assigned to the choice of prophylaxis in children with severe hemophilia in the first specific guideline published by the United Kingdom Hemophilia Centre Doctors' Organization (UKHCDO)25. Both RCTs evaluated high-dose regimens, i.e. 25 IU/ Kg e.o.d.12 and 25 IU/Kg thrice weekly20, respectively, started as "primary" or early "secondary prophylaxis", i.e. in children without any clinical evidence of joint damage16. However, benefits of prophylaxis have been shown with a variety of dose regimens and even when started later in life7. Indeed, the lack of formal studies comparing clinical outcomes does not enable to define the optimal prophylaxis regimen6,26. A series of studies report the feasibility and good clinical results with regimens individualised according to the bleeding tendency, including the lower dose in Dutch approach (FVIII 20-40 IU/Kg twice or thrice weekly or FIX 30-40 IU/kg once or twice weekly)22 or the Canadian escalating-dose regimen27, or, more recently, according to the pharmacokinetics (PK)26,28. However, few data concerning long-term outcomes of such personalised approaches, including prevention of arthropathy, and no comparisons with full-dose prophylaxis are presently available26. Individualised regimens may also facilitate the implementation of prophylaxis and adherence of families to treatment in small children, as well as reduce the impact of venous access problems, tailoring the frequency (and the dose) of concentrate infusions6,27. Along this line, lower dose and individualised regimens are enabling the introduction of secondary29 and even primary30 prophylaxis in some developing countries, in which resources for factor concentrates are limited. As regards the age at start of prophylaxis, increasing data are showing that prophylaxis is able to significantly reduce joint bleeding rates, and in parallel, improve health-related quality of life, even when started in adolescent or adult patients15,28,31,32. In this respect, the definition of "tertiary prophylaxis", i.e. started in patients with established joint damage, has been proposed16. Rigorous and long-term data on possible benefits on joint outcomes in such patients are still lacking, however a 5-year prospective study has been recently completed33 and a 3-year randomised study is presently ongoing15. Therefore, data from these studies concerning the possibility of delaying the progression of arthropathy are eagerly awaited, being crucial for clearly assessing cost-effectiveness and cost-utility of such a highly expensive regimen in adolescents and adults and supporting clinical recommendations of prophylaxis "for all"34. Optimal regimens of prophylaxis are even more uncertain in this setting, being extrapolated from those used in children, in whom PK, physical and social needs are largely different7,32. On the other hand, whether generations of patients, presently in the adulthood with absent or minimal joint disease thanks to primary or early secondary prophylaxis, may safely discontinue such regimens or switch to less intensive modalities of treatment is presently unknown35. A recent survey in 6 countries with different attitudes to the use of prophylaxis showed consistently higher quality of life in individuals on long-term prophylaxis when compared with those treated on-demand or on intermittent prophylaxis, with benefits continuing into adulthood36. Available evidence supporting the different types of prophylaxis, according to the start of treatment and the clinical objectives of preventing or limiting the development and progression of hemophilic arthropathy, as recently revised by the WFH guidelines16, is summarised in Table I. Although clinical objectives are clearly different, the choice and the personalization of prophylaxis regimens are crucial for achieving and maintaining the best patient outcomes and, in particular, improvements of quality of life, irrespective of age. In the clinical practice, prophylaxis regimens are implemented and often adjusted by dose and/or frequency based on the observed bleeding pattern and, importantly, on other patient-specific factors, including times of expected physical activity, the status of musculoskeletal system and patient or family needs6,27. On the whole, these clinical choices highly contribute to the effectiveness of prophylaxis, that results from a multi-dimensional assessment of outcomes, particularly in the long-term, including bleeding rates, muscle-skeletal status, laboratory parameters and, not last, health-related quality of life. Larger collection of data are needed for clarifying the clinical impact of less intensive (and less expensive) prophylaxis regimens, useful for overcoming the barrier of costs of treatment in low-income countries. However, only comprehensive evaluations in a lifetime perspective enable to highlight the actual cost-effectiveness and cost-utility of the huge investments for prophylaxis37. Comprehensive care and the evolving scenario of ageing haemophilic patients The WHO and the WFH recommendations, as well the European principles of care, clearly recognize the need for multidisciplinary teams at specialised HTCs, in order to deliver an optimal haemophilia care9,16. According to the available clinical facilities and local organisation, the core group composed of haemophilia physicians, nurses, psychologists, social workers and laboratory specialists, also involves orthopaedic surgeons, physiotherapists and Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s555 Coppola A et al Table I - Prophylaxis in haemophilia, clinical objectives and available evidence. Type of prophylaxis Definition^ Main clinical objective° Evidence Primary prophylaxis Regular continuous* treatment started in the absence of documented osteochondral joint disease, determined by physical examination and/or imaging studies, and started before the second clinically evident large joint** bleed and age 3 years. To prevent or minimize the incidence of hemophilic arthropathy, with its impact on psycho-physical development of children and quality of life RCTs (JOS12, ESPRIT20) Prospective study (Canada27) Retrospective cohorts (Sweden21, Germany , the Netherlands22, US, UK) and comparisons (France vs. the Netherlands and Sweden; Norway vs. Sweden)# Secondary prophylaxis Regular continuous* treatment started after 2 or more bleeds into large joints** and before the onset of joint disease, documented by physical examination and imaging studies. To reduce the frequency of bleeding, the development of target joints and hemophilic arthropathy, maintaining satisfactory levels of quality of life Early: RCT (ESPRIT20) Prospective controlled study (Orthopedic Outcome Study23) Retrospective cohorts (Sweden, the Netherlands, Germany, US, UK) and comparison (France vs. the Netherlands and Sweden)# Tertiary prophylaxis Regular continuous* treatment started after the onset of joint disease documented by physical examination and plain radiographs of the affected joints. To reduce the frequency of bleeding and stop or delay the progression of hemophilic arthropathy, improving quality of life; to prevent bleeding risk due to co-morbidities Retrospective cohorts (UK, Italy31)# Prospective studies, short term28,32 Prospective study, long term (POTTER33) RCT (SPINART15) ^according to the WFH guidelines, 2013 (ref. 16); °In all cases, to prevent life-threatening bleeding episodes; *With the intent of treating for 52 weeks per year and receiving a minimum of an a priori defined frequency of infusions for at least 45 weeks (85%); **Large joints: ankles, knees, hips, elbows and shoulders; #For reviews of these studies see references 6 and 7. specialists in rehabilitation, hepatologists and infectious disease specialists, and other relevant medical personnel, in the frame of highly specialised comprehensive care centres (CCCs). This approach enables to achieve better clinical outcomes, including patients' life expectancy, as shown in the developing world but even in high-income countries38,39. Achieving or maintaining such an optimal standard of care is the main objective of national and international organisations and healthcare programs9,16,40. From a clinical point of view, as a consequence of their increased life expectancy, haemophilic patients and their treaters are now facing the new challenges arising from the age-related co-morbidities41. Indeed, together with joint disease and infectious complications (HIV infection and chronic hepatitis C), routinely managed over the last decades at HTCs and CCCs, ageing haemophilic patients develop the typical diseases of the elderly, previously only rarely seen, such as cardiovascular diseases, malignancies, renal diseases, prostatic hypertrophy, sexual dysfunction and neurologic problems. Few literature data presently support the management of such co-morbidities, that may significantly increase the bleeding risk due to organic lesions or the need for pharmacological interventions or invasive procedures42. The paradigm of these challenges is the management of ischemic heart disease in persons with haemophilia. In these cases, the use of antithrombotic drugs, often in combination in the acute phase, particularly when percutaneous coronary interventions are carried out, or for long-term secondary prevention should be balanced by specific prophylactic regimens to prevent excessive bleeding42,43. Similarly, haemophilic patients with malignancies undergoing diagnostic or therapeutic invasive procedures or chemotherapy should receive adequate replacement treatment in order to minimise the bleeding risk44. In this perspective, the multidisciplinary, comprehensive care for adult and ageing haemophiliacs should be updated and revisited. Haemophilia specialists are now learning to search for the close cooperation of other specialists (i.e., cardiologists, oncologists, neurologists, urologists) to define the most appropriate diagnostic and therapeutic strategies for identifying, preventing and treating agerelated comorbidities10,42. In the lack (and probably unfeasibility) of rigorous studies providing evidencebased approaches, international cooperation is crucial for improving our knowledge and expertise in this setting. Nevertheless, even "typical" haemophilia-related comorbidities or complications should be confronted in the evolving perspective of the prolonged life expectancy of patients10. As regards the management of haemophilic arthropathy, increasing numbers of patients will need orthopedic surgeries, appropriate treatment for chronic pain, and prosthesis revision operations42. Similarly, addressing liver transplantation will be more frequently considered in patients with advanced HCV-related chronic hepatitis45. Late-onset inhibitors represent another poorly investigated issue in elderly haemophilic patients, as recently highlighted by United Kingdom data demonstrating a second peak of incidence in patients aged ≥60 years46. Unsolved challenges in clinical management of haemophilia The need for intravenous, frequent administration of factor concentrates and for an early start of prophylactic regimens in order to optimise clinical outcomes arises the crucial issue of venous access in haemophilic Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s556 Current evolving management of haemophilia children. Indeed, the peripheral vein access is often unfeasible and, although individualization of dose and frequency of infusions enables to reach full-dose regimens later in life when children may have better peripheral accesses6,26, central venous access devices (CVAD) are needed in relevant proportion of children starting prophylaxis12,20,26. The placement of external or fully implantable central venous catheters, providing a stable and long-lasting venous access greatly facilitate home treatment and regular prophylaxis47. However, an accurate specific training for caregivers is needed and CVAD complications (infections, occlusions) remain a major concern in the management of haemophilic children47-48. A newer and possibly safer approach, i.e the arteriovenous fistula (AVF), has been proposed, with encouraging low rate of complications49. However, AVF creation may be difficult in very small children (<2-year-old) and its maturation requires approximately 8 weeks. On the whole, this approach is practiced in few specialised centres and so far only one published relevant clinical experience about it49. Peripherally inserted central venous catheters (PICC) are also being introduced in the management of haemophilic children. These devices, simply inserted (via US guide) and employed in many chronic diseases requiring long-term venous access, are associated with very low rates of complications (infection, occlusion, dislodgement, phlebitis) requiring their removal50. In the era of safe factor concentrates and of the diffusion of prophylaxis to prevent or reduce the impact of arthropathy, the most serious complication of hemophilia treatment remains the development of inhibitory alloantibodies in 25-30% of severe haemophilia A patients and in 3-5% of those with haemophilia B51. Inhibitors render the safe standard replacement therapy ineffective and, particularly, preclude prophylaxis feasibility, exposing children to higher morbidity and poorer quality of life, with a striking increase of economic burden of patient management52. Intensive research has been devoted to unravel mechanisms of such an unfavorable immune response, in which a variety of genetic and environmental factors interplay, only in part presently elucidated (Table II)53. Genetic predisposition relies upon F8/F9 causative mutations, family history, and ethnicity54, but is being revealed more complex than previously thought, an increasing number of genes of immune response and intracellular signalling being identified, potentially relevant and requiring further specific evaluation55. In this genetic background, the presentation of the exogenous, non-self, therapeutic protein may be not sufficient for triggering an immune response but, according to the "danger model", the immune system is activated by alarm signals arising from the injured tissues to a greater extent than by the recognition of non-self56. Consistent with this, an increased inhibitor risk in patients receiving intensive treatments at first exposure days (longer than 5 consecutive exposure days and/or FVIII doses higher than 35 IU/Kg) has been reported57-59. On the other hand, the regular exposure to low doses of the antigen in the absence of danger signals by early prophylaxis might exert protective effects, inducing the tolerance of the foreign protein, as supported by some studies57,60,61. However, the recent large prospective Research Of Determinants of INhibitor development (RODIN) study59 showed that prophylaxis was only associated with decreased inhibitor incidence after 20 exposure days and that this association was more pronounced in patients with low-risk F8 genotypes than in those with high-risk F8 genotypes. Therefore, patients with "genetic" increased risk are likely to be less susceptible to protective effects of prophylaxis59. On the whole, while the risk associated with the source of FVIII product (i.e. plasma-derived vs. recombinant concentrates) remains keenly debated, with conflicting results from cohort studies57,62-64 and meta-analyses65,66 and a randomised trial still ongoing13, the recognition of genetic and non-genetic (thus potentially modifiable) risk factors (Table II) is suggesting prediction models for identifying subjects at higher risk67 and clinical approaches aimed to reduce the risk of inhibitor development68, although presently far to be validated. Even as regards the only available strategy to attempt inhibitor eradication, induction of immune tolerance (ITI), many questions are still unsolved69-71. There is substantial agreement in recommending ITI in all children with persistent inhibitors interfering with standard FVIII replacement, as soon as possible after inhibitor diagnosis, in order to minimize the inhibitor-related morbidity burden, in particular on joint health16,69-72. However, the optimal ITI regimen is still debated, high success rates (60-80%) being reported with heterogeneous protocols, in terms of dose and type of FVIII concentrate, interval of infusions and association of immunomodulating agents. According to the findings from a recent RCT in "good-prognosis" children (i.e. those aged <8 years, with a historical inhibitor peak titer lower than 200 BU/mL and starting ITI when inhibitor titer is lower than 10 BU/mL, within 24 months from inhibitor detection), in spite of similar success rates with a high-dose (the "Bonn" regimen, 200 IU/Kg daily) and a low-dose (50 IU/Kg thrice weekly) FVIII regimen, higher rates of bleeding episodes in patients on the low-dose arm raise concerns for choosing such regimen in this setting73. Therefore, high-dose or intermediatedose (100 IU/Kg) but daily regimens are suggested in "good-prognosis" children72, with the possibility of increasing FVIII dose in the case of intercurrent bleeding or detection of high inhibitor peaks, a putative negative Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s557 Coppola A et al predictor of ITI success73,74. In this respect, in order to reduce the bleeding risk and possible negative effects on joint status in children attempting inhibitor eradication, prophylaxis regimens with bypassing agents, have been proposed while awaiting for ITI start and during ITI, until FVIII recovery is achieved70,71. The administration of activated prothrombin complex concentrate (aPCC, 100 IU/Kg every 12 hours) was included in the original Bonn protocol, however more recently heterogeneous regimens with both aPCC and recombinant activated factor VII (rFVIIa) have been used, with the latter generally preferred in children and before ITI start, due to potential risk of anamnesis from FVIII traces in the aPCC70. Avoiding immunologic "danger signals" from bleeding-related tissue damage through prophylaxis has been hypothesised to affect favorably ITI outcome, however in this respect no evidence is so far available71. Even more debated is the optimal ITI regimen in "poor-risk" patients, in particular in those with long-standing inhibitors, in whom higher success rates are reported with high-dose regimens70,71, as well the choice for the type of FVIII concentrate, in the lack of prospective/controlled studies comparing plasmaderived and recombinant concentrates. Presently, the same product associated with inhibitor development is usually adopted for attempting ITI69-71. Also in the setting of inhibitor eradication, a better knowledge of predictors of ITI outcome (Table II) is becoming useful for optimizing the selection of candidates and regimens of treatment. Also in this case, improving pathophysiologic knowledge and clinical management may result in significant impact on cost-effectiveness of treatment and resource allocation, taking into account the highest costs of care for inhibitor patients75. However, only some patient-related factors, including low inhibitor titer at ITI start - <10 BU/mL - and historical peak inhibitor titer < 200 BU/mL are consistently reported as predictors of ITI success70-72, whereas other immunologic or genetic factors (including F8 mutations)74 have been proposed but currently poorly investigated70,71. Consistent with the search for improving clinical outcomes and quality of life even in patients with inhibitors, growing experience with prophylactic regimens with both bypassing agents even in patients who are not candidate to ITI is extending the excellent results of prophylaxis in non-inhibitor patients in this setting76-79. These clinical outcomes have been documented by rigorous studies, providing evidence of significant reductions in total, joint and target joint bleeding rates and of improved quality of life, although over short-term follow-up (3-12 months)76,77. Due to such a limited observation period, these studies were not able to document effects in preventing or delaying joint deterioration and conflicting data are reported in retrospective case series17,78,79. Therefore, prophylaxis is presently used by many physicians in inhibitor patients, although concerns about cost-effectiveness and the need for longer term assessment of efficacy (in particular with respect to joint outcomes) and safety are clearly highlighted80. Table II - Patient- and treatment-related factors associated with inhibitor development and eradication through immune tolerance induction in haemophilia A^. Inhibitor development Inhibitor eradication (ITI) Patient-related factors F8 mutations Ethnicity Family history F8 polymorphisms HLA-class II and immunogenotype Inhibitor titer at ITI start Historical peak inhibitor titer Inhibitor peak titer during ITI Treatment-related factors Periods of intensive treatment Surgical procedures Dose of FVIII Prophylaxis* Dose of FVIII Unlikely Age at first exposure Type of FVIII product (plasma-derived vs. recombinant) Switching between products Breastfeeding Age at ITI start Time between inhibitor diagnosis and ITI start Need for further data Type of FVIII recombinant product Mode of infusion (bolus vs. continuous infusion) Extravasation of products Vaccinations Infections Amniocentesis, villocentesis F8 mutations Ethnicity Type of FVIII product (plasma-derived vs. recombinant) Interruptions of treatment Infections and other immunologic challenges ^in italics factors not consistently recognised; for reviews of these issues see references 53, 54, 70 and 71; *as a protective factor. Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s558 Current evolving management of haemophilia The search for safety and overcoming current challenges The need for safer and safer factor concentrates was the key for research and development of both plasmaderived and recombinant products over the last three decades1. Current achievements rely upon plasmaderived concentrates, manufactured with rigorous policies for plasma collection, NAT screening and application of viral inactivation and elimination techniques (often in combination), and a variety of recombinant products, including new generation protein-free concentrates, i.e. without any addition of human or animal protein throughout the production process5. In spite of the high-level of safety of plasma-derived concentrates, documented by the lack of transmission of HCV, HIV or other clinically relevant infections over the last 25 years1, many physicians continue to prefer recombinant products (particularly in children), thought to be safer with respect to known and, particularly, emerging or unknown pathogens80,81. This attitude is also consistent with the search for the best possible treatment, although present economic constraints tend to influence therapeutic choices even in high-income countries80,82. On the other hand, the ongoing and future development of replacement products is wholly based on recombinant technology. This search is devoted to overcome current treatment challenges thanks to factor concentrates with improved properties, in particular longer half-life products to obviate frequent administration and venous access problems, and/or reduced antigenicity/immunogenicity products to minimise inhibitor development1,18. As recently reviewed in detail, some modified FVIII and FIX molecules with longer half-life are in advanced phase of clinical trials18,83. The availability of such products will represent a relevant progress for countries that can afford costs of primary prophylaxis, being venous access problems the main barrier to its widespread adoption and adherence. These benefits will be associated ultimately with further improvements of quality of life of persons with hemophilia. A positive impact on the overall factor requirements (and hopefully on costs of treatment) might be obtained through the reduced dosage frequency and truly personalised regimens of prophylaxis with such products, although costs of longer half-life products are presently not predictable83,84. More advanced clinical development and encouraging results with modified FIX than FVIII concentrates18,83 highlight the need for specific studies devoted to patients with haemophilia B. Indeed, due to the lower prevalence of hemophilia B, few patients have been included in clinical studies and the general practice is transferring results obtained in patients with haemophilia A. This is true for prophylaxis regimens but even more scarce information is available concerning inhibitor development and management, which are complicated by the additional morbidity of allergic reactions and unfavorable ITI outcome85. Personalised management in haemophilia B might also be supported by several studies suggesting the different severity of the two forms of haemophilia, with less severe bleeding phenotype in haemophilia B than in haemophilia A86. Conclusions In spite of significant persistent challenges, like the need for intravenous administration of replacement products and inhibitor development in approximately 30% of previously unexposed children, persons with haemophilia presently enjoy a highly effective and safe treatment80, delivered through specialised centres, comprehensively addressing their demanding management. This results, at least in high-income countries, in an excellent quality of life for children born in the era of primary prophylaxis and their families, and in improved clinical outcomes in patients of all ages who predominantly receive long-term prophylaxis as replacement regimen. Thanks to these achievements, haemophilia in the third millennium can remove its historical hallmark of a crippling inherited bleeding disorder1,6. Prophylaxis is the milestone of this pathway of continuous advances in the management of haemophilic patients, driven by the achievement of the best possible long-term quality of life and always requiring shared decisions between physicians, patients and their families80. After the recognition of prophylaxis as the evidence-based treatment of choice in children, studies are being devoted to support its adoption in adolescents and adults and to validate individualised regimens, useful for facilitating long-term adherence and overcoming barriers to its diffusion, in particular venous access and costs. Indeed, in the present era of healthcare budget constraints, these regimens may improve costeffectiveness of treatment and reduce the apparently insurmountable problem of costs. Along this line, in the near future extended half-life concentrates will provide further, possibly cost-effective, strategies for tailored treatment. Improving clinical outcomes and quality of life are key objectives even in the challenging management of inhibitor patients (searching for the optimal ITI or prophylaxis regimens) and of co-morbidities in elderly haemophiliacs. Again, personalised treatments represent the strategy for overcoming the limitations of unsolved issues and lack of evidence. Keywords: bleeding, comprehensive care, haemophilia, prophylaxis, treatment. The Authors declare no conflicts of interest. Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s559 Coppola A et al References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) Franchini M, Mannucci PM. Past, present and future of hemophilia: a narrative review. Orphanet J Rare Dis 2012; 7:24. Tagliaferri A, Rivolta GF, Iorio A, et al. Mortality and causes of death in Italian persons with haemophilia, 1990-2007. Haemophilia 2010; 16: 437-46. Franchini M, Coppola A, Molinari AC, et al. Forum on: the role of recombinant factor VIII in children with severe haemophilia A. Haemophilia 2009; 15: 578-86. Ofosu FA, Freedman J, Semple JW. Plasma-derived biological medicines used to promote haemostasis. Thromb Haemost 2008; 99: 851-62. Franchini M, Lippi G. Recombinant factor VIII concentrates. Semin Thromb Hemost 2010; 36: 493-7. Coppola A, Tagliaferri A, Di Capua M, Franchini M. Prophylaxis in children with hemophilia: evidence-based achievements, old and new challenges. Semin Thromb Hemost 2012; 38: 79-94. Coppola A, Franchini M, Tagliaferri A. Prophylaxis in people with hemophilia. Thromb Haemost 2009; 101: 674-81. Gringeri A, Lambert T, Street A, Aledort L. Adolescent/ Adult Prophylaxis Expert Working Group of the International Prophylaxis Study Group. Tertiary prophylaxis in adults: is there a rationale? Haemophilia 2012; 18: 722-8. Colvin BT, Astermark J, Fischer K, et al. European principles of haemophilia care. Haemophilia 2008, 14: 361-74. Coppola A, Santoro C, Franchini M, et al. Emerging issues on comprehensive hemophilia care: preventing, identifying and monitoring age-related comorbidities. Semin Thromb Hemost 2013; 39: 794-802. Donadel-Claeyssens S. Current co-ordinated activities of the PEDNET (European Paediatric Network for Haemophilia Management). Haemophilia 2006; 12: 124-7. Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis vs episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med 2007; 357: 535-44. Mannucci PM, Gringeri A, Peyvandi F, Santagostino E. Factor VIII products and inhibitor development: the SIPPET study (survey of inhibitors in plasma-product exposed toddlers). Haemophilia 2007; 13 (Suppl 5): 65-8. Hay CR, DiMichele DM; International Immune Tolerance Study. The principal results of the International Immune Tolerance Study: a randomized dose comparison. Blood 2012; 119: 1335-44. Manco-Johnson MJ, Kempton CL, Reding MT, et al. Randomized, controlled, parallel-group trial of routine prophylaxis vs on-demand treatment with rFVIII-FS in adults with severe hemophilia A (SPINART). J Thromb Haemost 2013; 11: 1119-27. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al; Treatment Guidelines Working Group on Behalf of The World Federation Of Hemophilia. Guidelines for the management of haemophilia. HaemophiliaHaemophilia 2013; 19: e1-47. Forsyth AL, Giangrande P, Hay CRM et al. Difficult clinical challenges in haemophilia: international experiential perspective. Haemophilia 2012; 18(Suppl. 5): 39-45. Peyvandi F, Garagiola I, Seregni S. Future of factor replacement treatment. J Thromb Haeamost 2013; 11: 84-98. Chuah MK, Nair N, van den Driessche T. Recent progress in gene therapy for hemophilia. Hum Gene Ther 2012; 23: 557-65. Gringeri A, , Lundin B, Mackensen SV, et al. A randomized clinical trial of prophylaxis in children with hemophilia A (the ESPRIT Study). J Thromb Haemost 2011; 9: 700-10. Nilsson IM, Berntorp E, Löfqvist T, Pettersson H: Twentyfive years experience of prophylactic treatment in severe haemophilia A and B. J Intern Med 1992; 232: 25-32. 22) Fischer K, van der Bom JG, Mauser-Bunschoten EP, et al. The effects of postponing prophylactic treatment on long-term outcome in patients with severe hemophilia. Blood 2002; 99: 2337-41. 23) Aledort L, Haschmeyer RH, Pettersson H. A longitudinal study of orthopaedic outcomes for severe factor-VIII-deficient haemophiliacs. The Orthopaedic Outcome Study Group. J Intern Med 1994; 236: 391-9. 24) Berntorp E, Boulyjenkov V, Brettler D, et al. Modern treatment of haemophilia. Bull World Health Organ 1995; 73: 691-701. 25) Richards M, Williams M, Chalmers E, et al. Paediatric Working Party of the United Kingdom Haemophilia Doctors' Organisation. A United Kingdom Haemophilia Centre Doctors' Organization guideline approved by the British Committee for Standards in Haematology. Guideline on the use of prophylactic factor VIII concentrate in children and adults with severe haemophilia A. Br J Haematol 2010; 149: 498-507. 26) Santoro C, Baldacci E, Mercanti C, Mazzucconi MG. Tailored vs. standard dose prophylaxis in children with haemophilia A. Semin Thromb Hemost 2013; 39: 711-22. 27) Feldman BM, Pai M, Rivard GE, et al. Association of Hemophilia Clinic Directors of Canada Prophylaxis Study Group. Tailored prophylaxis in severe hemophilia A: interim results from the first 5 years of the Canadian Hemophilia Primary Prophylaxis Study. J Thromb Haemost 2006; 4: 1228-36. 28) Valentino LA, Mamonov V, Hellmann A, et al. Prophylaxis Study Group: Prophylaxis Study Group. A randomized comparison of two prophylaxis regimens and a paired comparison of on-demand and prophylaxis treatments in hemophilia A management. J Thromb Haemost 2012; 10: 359-67. 29) Wu R, Luke KH, Poon MC, et al. Low dose secondary prophylaxis reduces joint bleeding in severe and moderate haemophilic children: a pilot study in China. Haemophilia 2011, 17:70-4. 30) Celkan T, Özdemir N. Reduced early prophylaxis of children with haemophilia in a developing country, Turkey. Haemophilia 2011; 17: e840-e841. 31) Tagliaferri A, Franchini M, Coppola A, et al. Effects of secondary prophylaxis started in young-adult hemophiliacs. Haemophilia 2008; 14: 945-51. 32) Collins P, Faradji A, Morfini M, et al. Efficacy and safety of secondary prophylactic vs. on-demand sucrose-formulated recombinant factor VIII treatment in adults with severe hemophilia A: results from a 13-month crossover study. J Thromb Haemost 2010; 8: 83-9. 33) Tagliaferri A, Rivolta GF, Coppola A, et al. Prophylaxis vs on-demand therapy through economic report (POTTER) study: Preliminary data from the final five-year analysis. Haemophilia 2012; 18 (Suppl. 3):160 (abstract). 34) National Hemophilia Foundation. MASAC Recommendations concerning prophylaxis (regular administration of clotting factor concentrate to prevent bleeding). Document 179. Available at: http://www.hemophilia.org/NHFWeb/MainPgs/ MainNHF.aspx?menuid=57&contentid=1007. Accessed on 13/02/2014. 35) van Dijk K, Fischer K, van der Bom JG, et al. Can long term prophylaxis for severe haemophilia be stopped in adulthood? Results from Denmark and the Netherlands. Br J Haematol 2005; 130: 107-12. 36) Noon D, O'Mahony B, van Dijv JP, Prihodova L. A survey of the outcome of prophylaxis, on-demand treatment or combined treatment in 18-35-year old men with severe haemophilia in six countries. Haemophilia 2013; 19: 44-50. 37) Farrugia A, Cassar J, Kimber MC, et al. Treatment for life for severe haemophilia A - A cost-utility model for prophylaxis vs. on-demand treatment. Haemophilia 2013; 19: e228-38. Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s560 Current evolving management of haemophilia 38) Soucie JM, Nuss R, Evatt B, et al. Mortality among males with hemophilia: relations with source of medical care. Blood 2000; 96: 437-42. 39) Baker JR, Crudder So, Riske B, et al. A model for a regional system of care to promote the health and well-being of people with rare chronic genetic disorders. Am J Public Health 2005; 95: 1910-6. 40) Fischer K, Hermans C, on behalf of the European Haemophilia Therapy Standardisation Board (EHTSB). The European Principles of Haemophilia Care: a pilot investigation of adherence to the principles in Europe. Haemophilia 2013; 19: 35-43. 41) Mauser-Bunschoten EP, van de Putte DEF, Schutgens REG. Co-morbidity in the ageing haemophilia patient: the down side of increased life expectancy. Haemophilia 2009; 15: 853-63. 42) Mannucci PM, Schutgens RE, Santagostino E, MauserBunschoten EP. How I treat age-related morbidities in elderly persons with hemophilia. Blood 2009; 114: 5256-63. 43) Coppola A, Tagliaferri A, Franchini M. The management of cardiovascular diseases in patients with hemophilia. Semin Thromb Hemost 2010; 36: 91-102. 44) Tagliaferri A, Di Perna C, Santoro C, et al. Cancers in patients with hemophilia: a retrospective study from the Italian Association of Hemophilia Centres. J Thromb Haemost 2012; 10: 90-5. 45) Lambing A, Kachalsky E, Kuriakose P. Liver transplantation in the haemophilia patient. Haemophilia 2012; 18: 300-3. 46) Hay CR, Palmer B, Chalmers E, et al. Incidence of factor VIII inhibitors throughout life in severe hemophilia A in the United Kingdom. Blood 2011; 117: 6367-70. 47) Valentino LA, Ewenstein B, Navickis RJ, Wilkes MM: Central venous devices in haemophilia. Haemophilia 2004, 10:134-46. 48) Ljung R. The risk associated with indwelling catheters in children with haemophilia. Br J Haematol 2007; 138: 580-6. 49) Mancuso M, Berardinelli L, Beretta C, et al. Improved treatment feasibility in children with hemophilia using arteriovenous fistulae: the results after seven years of followup. Haematologica 2009; 94: 687-92. 50) Bui S, Babre F, Hauchecorne S, et al. Intravenous peripherallyinserted central catheters for antibiotic therapy in children with cystic fibrosis. J Cyst Fibros 2009; 8: 326-31. 51) Franchini M, Mannucci PM. Inhibithors of propagation of coagulation (factors VIII, IX and XI): a review of current therapeutic practice. Br J Clin Pharmacol 2011; 72: 553-62. 52) Gringeri A, Mantovani LG, Scalone L, Mannucci PM. Cost of care and quality of life for patients with hemophilia complicated by inhibitors: the COCIS Study Group. Blood 2003; 102: 2358-63. 53) Coppola A, Santoro C, Franchini M, Tagliaferri A, Di Minno G. Understanding inhibitor development in haemophilia A: towards clinical prediction and prevention strategies. Haemophilia 2010; 16: 13-9. 54) Astermark J. Inhibitor development: patient-determined risk factors. Haemophilia 2010; 16: 66-70. 55) Astermark J, Donfield SM, Gomperts ED, et al. The polygenic nature of inhibitors in hemophilia A: results from the Hemophilia Inhibitor Genetics Study (HIGS) Combined Cohort. Blood 2013; 121: 1446-54. 56) Matzinger P. The danger model: a renewed sense of self. Science 2002; 8: 76-82. 57) Gouw SC, van der Bom JG, van den Berg HM. Treatmentrelated risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood 2007; 109: 4648-54. 58) Maclean PS, Richards M, Williams M, Collins P, Liesner R, Keeling DM, Yee T, Will AM, Young D, Chalmers EA. Treatment related factors and inhibitor development in children with severe haemophilia A. Haemophilia 2011; 17: 282-7. 59) Gouw SC, van den Berg HM, Fischer K, et al. Intensity of factor VIII treatment and inhibitor development in children with severe hemophilia A: the RODIN study. Blood 2013; 121: 4046-55. 60) Santagostino E, Mancuso ME, Rocino A, et al. Environmental risk factors for inhibitor development in children with haemophilia A: a case-control study. Br J Haematol 2005; 130: 422-7. 61) Auerswald G, Bidlingmaier C, Kurnik K. Early prophylaxis/ FVIII tolerization regimen that avoids immunological danger signals is still effective in minimizing FVIII inhibitor developments in previously untreated patients-long-term follow-up and continuing experience. Haemophilia 2012; 18: e18-e20. 62) Goudemand J, Rothschild C, Demiguel V, et al. Influence of the type of factor VIII concentrate on the incidence of factor VIII inhibitors in previously untreated patients with severe hemophilia A. Blood 2006; 107: 46-51. 63) Mancuso ME, Mannucci PM, Rocino A, et al. Source and purity of factor VIII products as risk factors for inhibitor development in patients with hemophilia A. J Thromb Haemost 2012; 10: 781-90. 64) Gouw SC, van der Bom JG, Ljung R, et al; PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med 2013; 368: 231-9. 65) Iorio A, Halimeh S, Holzhauer S, et al. Rate of inhibitor development in previously-untreated hemophilia a patients treated with plasma-derived or recombinant factor VIII concentrates. A systematic review. J Thromb Haemost 2010; 8: 1256-65. 66) Franchini M, Coppola A, Rocino A, et al. Systematic review of the role of FVIII concentrates in inhibitor development in previously untreated patients with severe hemophilia A: a 2013 update. Semin Thromb Hemost 2013; 39: 752-66. 67) Ter Avest P, Fischer K, Mancuso ME, et al. Risk stratification for inhibitor development at first treatment for severe haemophilia A patients: a tool for clinical practice. J Thromb Haemost 2008; 6: 2048-54. 68) Auerswald G, Bidlingmaier C, Kurnik K. Early prophylaxis/ FVIII tolerization regimen that avoids immunological danger signals is still effective in minimizing FVIII inhibitor developments in previously untreated patients--long-term follow-up and continuing experience. Haemophilia 2012; 18: e18-e20. 69) Astermark J, Morado M, Rocino A, et al. Current European practice in immune tolerance induction therapy in patients with haemophilia and inhibitors. Haemophilia 2006;12:363-71. 70) DiMichele D, Hoots WK, Pipe SW, et al. International workshop on immune tolerance induction: consensus recommendations. Haemophilia 2007; 13: 1-22 71) Coppola A, Di Minno MN, Santagostino E. Optimizing management of immune tolerance induction in patients with severe haemophilia A and inhibitors: towards evidence-based approaches. Br J Haematol 2010; 150: 515-28. 72) Collins PW, Chalmers E, Hart DP, et al. Diagnosis and treatment of factor VIII and IX inhibitors in congenital haemophilia: (4th edition). UK Haemophilia Centre Doctors Organization. Br J Haematol 2013; 160: 153-170. 73) Hay CR, DiMichele DM; International Immune Tolerance Study: The principal results of the International Immune Tolerance Study: a randomized dose comparison. Blood 2012; 119: 1335-44. 74) Coppola A, Margaglione M, Santagostino E, et al. Factor VIII gene (F8) mutations as predictors of outcome in immune tolerance induction of hemophilia A patients with highresponding inhibitors. J Thromb Haemost 2009; 7: 1809-15. 75) Di Minno MND, Di Minno G, Di Capua M, et al. Cost of care of haemophilia with inhibitors. Haemophilia 2010, 16: e190-e201. Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s561 Coppola A et al 76) Konkle BA, Ebbesen LS, Erhardtsen E, et al. Randomized, prospective clinical trial of recombinant factor VIIa for secondary prophylaxis in hemophilia patients with inhibitors. J Thromb Haemost 2007; 5: 1904-13. 77) Leissinger C, Gringeri A, Antmen B, et al. Anti-inhibitor coagulant complex prophylaxis in hemophilia with inhibitors. N Engl J Med 2011; 365: 1684-92. 78) Young G, Auerswald G, Jimenez-Yuste V, et al. PRO-PACT: retrospective observational study on the prophylactic use of recombinant factor VIIa in hemophilia patients with inhibitors. Thromb Res 2012; 130: 864-70. 79) Gringeri A, Leissinger C, Cortesi PA, et al. Health-related quality of life in patients with haemophilia and inhibitors on prophylaxis with anti-inhibitor complex concentrate: results from the Pro-FEIBA study. Haemophilia 2013; 19: 736-43. 80) Franchini M, Coppola A, Rocino A, et al. Perceived challenges and attitudes to regimen and product selection from Italian haemophilia treaters. The 2013 AICE survey. Haemophilia 2014; 20: e128-35. 81) Di Minno G, Canaro M, Ironside JW, et al. Pathogen safety of long-term treatments for bleeding disorders: (un)predictable risks and evolving threats. Semin Thromb Hemost 2013; 39: 779-93. 82) Tarantino MD, Ye X, Bergstrom F, Skorija K, Luo MP. The impact of the economic downturn and health care reform on treatment decisions for haemophilia A: patient, caregiver and health care provider perspectives. Haemophilia 2013; 19: 51-8. 83) Kaufman RJ, Powell JS. Molecular approaches for improved clotting factors for hemophilia. Blood 2013; 122: 3568-74. 84) Hart DP. Prophylaxis in the era of long-acting products. Haemophilia 2014; 20(Suppl 2): 7 SP008 (abstract). 85) DiMichele DM. Inhibitors in haemophilia B: An orphan disease in need of attention. Br J Haematol 2007; 138: 305-15. 86) Santagostino E, Fasulo MR. Hemophilia A and hemophilia B: different types of diseases? Semin Thromb Hemost 2013; 39: 697-701. Correspondence: Antonio Coppola Regional Reference Centre for Bleeding Disorders Federico II University Hospital, Via S. Pansini, 5 80131 Naples, Italy e-mail: antocopp@unina.it Blood Transfus 2014; 12 Suppl 3: s554-62 DOI 10.2450/2014.0043-14s s562 REVIEW Uncovered needs in the management of inherited bleeding disorders in Italy Romano Arcieri1, Angelo C. Molinari2,3, Stefania Farace1, Giuseppe Mazza1, Alberto Garnero1, Gabriele Calizzani1,4, Paola Giordano2,5, Emily Oliovecchio6, Lorenzo Mantovani2,7, Lamberto Manzoli2,8, Paul Giangrande2,9 1 Italian Federation of Haemophilia Societies (FedEmo), Rome, Italy; 2FedEmo Scientific Commettee, Rome, Italy; Thrombosis and Hemostasis Unit, Giannina Gaslini Children's Hospital, Genoa, Italy; 4National Blood Centre, National Institute of Health, Rome; 5Department of Biomedical Sciences and Human Oncology, Pediatric Unit, University of Bari, Bari, Italy; 6Department of Internal Medicine, University of Perugia, Perugia, Italy; 7Department of Clinical Medicine and Surgery Federico II University of Naples, Naples, Italy; 8Department of Medicine and Aging Sciences, University of Chieti, Chieti, Italy; 9Oxford Haemophilia and Thrombosis Centre, Oxford, United Kingdom 3 Introduction Haemophilia is an X-linked bleeding disorder1 and is characterised by repeated bleeding, especially in joints. The current management of haemophilia is based on the replacement therapy with intravenous clotting factor and includes plasma-derived and recombinant factor concentrates2. The early treatment in pediatrics age has been recognised as an important determinant of better physical development3, and several studies have demonstrated that primary prophylaxis has a positive and significant impact on the quality of life and the prevention of arthropathy in haemophiliac children4,5. Also, home treatment has shown to improve both life expectancy and quality of life of patients with haemophilia6. The global treatment of haemophilia, however, requires a multidisciplinary team including haematologists, physicians, surgeons, orthopaedics and other specialists in several medical areas7. This level of clinical assistance is or can be guaranteed only in some countries, and this influences the life expectancy of haemophiliacs8. To ensure a high quality of haemophilia care, an appropriate health organisation and economic resources are necessary. The European Principles of Haemophilia Care (EPHC) were published in 20089. These Principles detail the standard of haemophilia care that should be achieved for an appropriate global care of persons with haemophilia (PWH). The aim of this review is to highlight uncovered needs of Italian haemophilia community, relative to the implementation of each of the EPHC. A central haemophilia organisation supporting local groups Patient and medical bodies, represented in Italy by the Italian Federation of Haemophilia Societies (FedEmo, www.fedemo.it) and the Italian Association of Haemophilia Centres (AICE), are national organisations that have addressed the problems of PWH since 1996. Because the Italian National Healthcare Service gives to the 21 Regions political, administrative and financial responsibility regarding the provision of health care, each Region may develop its peculiar healthcare organisational model10. In the majority of the largest Regions (i.e. Emilia-Romagna, Latium, Lombardy, Campania), the network of hospital care is most frequently organised following a "Hub and Spoke" model. For improving the organisation of hemophilia care and the access to services, in 2009 FedEmo asked the Health Commission of the Conference between the Italian State and Regions for the development of an accreditation system for Haemophilia Centres (HCs)11. Following this request, in 2010 the Ministry of Health funded a project aimed at developing a model of disease management to prevent haemophilia complications. Given this background, FedEmo, AICE, the Italian National Blood Center (NBC, www.centronazionalesangue.it), Italian Regional Health Authorities and Ministry of Health proposed an institutional accreditation scheme for HCs, that was approved by a formal State-Regions Agreement in March 201311,12 (hereafter referred as the March 2013 Agreement). This provides an organisational framework for Italian Regional Health Authorities to optimise and standardise haemophilia care on the basis of the latest scientific evidence and international recommendations9,13. National Haemophilia Patient Registries In Italy, the epidemiological data on inherited bleeding disorders derive from the Italian National Registry for Rare Diseases (NRRDs), the National Registry of Congenital Coagulopathies (NRCC) and the Italian Registry of Haemophilia and Allied Disorders of the AICE14. NRRDs is a population-based and multi-diseases register established by law since 2001, that supports national planning of interventions for patients affected by Blood Transfus 2014; 12 Suppl 3: s563-6 DOI 10.2450/2014.0036-14s © SIMTI Servizi Srl s563 Arcieri R et al rare diseases (RDs) and implements the epidemiological national surveillance of RDs. NRCC was activated in 1999 by the AICE and the National Institute of Health (Istituto Superiore di Sanità, ISS, www.iss.it). The main objectives of the National registry of congenital bleeding disorders is to: i) estimate the prevalence of different congenital bleeding disorders, ii) evaluate therapy complications with particular attention to infection diseases (HIV, HCV, prioni), iii) monitor the appearance of inhibitor antibodies, iv) monitor the appropriateness of treatment15. In 2003, AICE also created a new pathology registry: the Italian Registry of Haemophilia and Allied Disorders (www.aiceonline.it). A subset of data is shared between the two registries. The main objective of this registry is to collect data on current clinical practice and provide data for clinical studies16. The registries differ in terms of organisation, purpose and data collection process. They provide epidemiological data on inherited bleeding disorders but at this stage do not fully support benchmarking activities of HC performance. Comprehensive Care Centres (CCCs) and Haemophilia Treatment Centres (HCs) The current management of haemophilia should improve the health and quality of life for PWH. This issue could be achieved with the following two actions. Firstly, establishing a team of specialists in CCCs and HCs, providing a continuous comprehensive care based on three main goals: i) prevention of bleeding, ii) management of joint and muscle damage, iii) management of treatment complications (inhibitor antibodies and viral infections). Secondly, offering an equal access to CCCs and HCs on all the national territory. In Italy, the availability and quality of care vary widely within the country, so that 52% of patients must still travel long distances (101-500 km), 22% of those living in Southern regions and islands travel more than 500 km, and 40% of patients had to change living place to attend a HC with an optimal level of care17. Nowadays, there is a wide difference in the organisation and efficacy of the HCs in Italy. However, commitments endorsed by Regions within the March 2013 Agreement provide the ground for an improvement and standardisation of haemophilia care across the Country. So far, three Regions (Autonomous Province of Trent, Emilia-Romagna and Liguria) over 21 have accepted the March 2013 Agreement into their legislation. Uncertainty remains about the way HCs regional network should be funded. Partnership in delivery of care The 4 th Principle of EPHC declares that the etablishment of an Haemophilia Co-ordination Group is desirable. This group should be represented by physicians, national haemophilia patient organisations and national health authorities. Unfortunately, so far an Italian national haemophilia Co-ordination Group has been missing but a local haemophilia Co-ordination Group is active in a few regions. Some aspects related to the comprehensive care such as pharmacological treatment, organisation and access to specialist services have to be included in the national program. Allocation of economical and structural resources is of primary importance and, to such aim, an effective partnership between different stakeholders has to be defined to draw up the priorities and define national clinical and organisational recommendations. Safe and effective concentrates at optimum treatment levels Actually, the treatment for haemophilia has reached a high degree of effectiveness and safety2. In 2011, even if with a wide variability across Regions, a standardised national consumption of factor VIII and factor IX respectively of 6.5 and 0.9 international units (I.U.) per capita has been achieved18. In Italy, guidelines for diagnosis and treatment of patients affected by coagulation disorders have been produced by AICE in the past years19,20. Very recently, a revised version has been approved and will be shortly published. This document carefully considers all the available products and the different mainstay of the treatment (home treatment, prophylaxis, ITI). A scientific and economical debate on products type, such as recombinant vs plasma-derived, is ongoing21-24 basing on the difference between the two classes of products and mainly on the costs. As we believe that the quality of life of patients represents one of the more desirable outcome of care, we would recommend instead evaluating individual treatment taking into consideration pharmacokinetic response, efficacy, side effects, outcomes, patient's inhibitor history, preference and compliance25,26. Home treatment and delivery Home treatment has shown to improve both life expectancy and quality of life of patients with haemophilia and other inherited coagulation disorders, with a reduction of musculoskeletal damage6,7. In Italy, home treatment is a common practice, but a specific regulation on self infusion has been adopted in only 60% of Italian Regions (Calabria, Campania, Emilia-Romagna, Latium, Liguria, Lombardy, Piedmont, Blood Transfus 2014; 12 Suppl 3: s563-6 DOI 10.2450/2014.0036-14s s564 Global care of bleeding disorders in Italy Apulia, Sardinia, Tuscany, Autonomous Province of Trent and Veneto). No financial constrain is affecting the inhibitors management until now. Prophylactic (preventive) treatment Education and research In Italy, prophylactic treatment is now available in all Regions without financial constrains and regular concentrate availability. The SPINART study (Trial to Evaluate the Effect of Secondary Prophylaxis with Recombinant FVIII Therapy in Severe Hemophilia Adult subjects compared to That of Episodic Treatment)27 and the POTTER study (Prophylaxis vs On-demand Therapy Through Economic Report)28 are eagerly awaited as they could lead to redefine the guidelines on treatment for haemophilia. We believe that the prophylactic treatment should be offered to all PWH -including adults- to maintain a high quality of life. In Italy the number of thrombosis and haemostasis specialist has decreased as in other countries32. It is essential to promote specific actions in the universities, to foster training of healthcare professional in this area and guarantee the continuity of care. Specialist service and emergency care With regard to the management of haemorrhagic emergencies, in 2011 only 36% of the Italian Regions had set up a specific protocol, 68% had emergency units with immediate availability and access to factor concentrates, only 58% of HCs had a physician expert in haemostasis available 24/24 h and 42% had 24 h access to a coagulation laboratory able to perform inhibitor detection and titration29. This picture represents a limitation of access to appropriate care, and therefore the Italian haemophilia community should develop specific plans with the related stakeholders. Indeed, in an emergency care setting accessibility to drugs, appropriateness and competence are critical issues and these are the areas needing to be improved, to avoid severe complications and inequity. In order to improve the awareness about this issue, FedEmo launched in 2011 an educational project called "Safe Factor" involving the key actors involved in emergency care like physicians of HCs, emergency departments, pharmacist, etc. We expect from this campaign and from the implementation of the provisions contained in the March 2013 Agreement a further development of regional networks for the emergency management. Management of inhibitors The difference in HC organisations affects the laboratory facilities, such as performed test and availability of staff during working days as well as in weekends and holidays. In Italy, immune tolerance induction programs are regularly applied in all centers, and bypassing agents such as recombinant activated clotting factor VII (rFVIIa) and activated prothrombin complex concentrate (aPCC) are regularly used 30. However, some children have to move to the largest HCs to receive central venous access device or have AV fistula created31. Conclusions Due to the different organisational models across the Regions, in Italy the pharmacological treatment is accessible in all regions, but wide differences are present for the availability of multidisciplinary services and for the laboratory facilities. The March 2013 Agreement application should improve this situation, as it defines services that should be offered and an essential list of laboratory tests that should be available all day round. To improve accessibility to home treatment and emergency care at the regional level, a Co-ordination Group should be established with the aim of identifying and tackling the actual gaps and define the appropriate organisation. Following the experience of the Institutional Accreditation Model11,12, we believe that the participation of non-governmental organisations, such as national or regional haemophilia patients' organisations, can bring an added value to the policy making process, including the product procurement process. An early involvement of PWH representatives in the discussion of any clinical or organisational guideline, as well as of any associated health care program, should be systematically pursued in line with the fourth principle of the EPHC8, as in Emilia-Romagna Region where the structured involvement of patient organisation for the last 13 years has contributed to produce a well established and effective organisation of care for PWH. Finally, we envisage the establishment of a central organisation, involving all key stakeholders (FedEmo, AICE, Regions and national institutions such as MoH, NBC, National Medicines Agency, etc) with the mission to promote the standardisation of haemophilia care across the Country, by overseeing the implementation of the March 2013 Agreement provisions and by monitoring the replacement therapy supply and costs. We also believe that the Italian national network for HCs, in compliance with European Union Committee of Experts on Rare Diseases (EUCERD) 33 and European Haemophilia Network project (EUHANET)34 recommendations, should benefit of dedicated resources in order to be put in place. Therefore, among the tasks assigned to such central organisation, it would Blood Transfus 2014; 12 Suppl 3: s563-6 DOI 10.2450/2014.0036-14s s565 Arcieri R et al be desirable foreseeing the commitment to advance proposals on funding mechanism for the HCs Network. Keywords: haemophilia, Comprehensive Care Centre, Haemophilia Treatment Centre. 18) 19) Acknowledgements We are indebted to Fabio Candura and Federica Maria Regini for the editorial assistance, and to Francesca Gillespie for reviewing English language. 20) 21) The Authors declare no conflicts of interest. 22) References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) Mannucci PM, Tuddenham EGD. The hemophiliac - form royal genes to gene therapy. N Engl J Med 2001; 344: 1773-9. Mannucci PM. Back to the future: a recent history of hemophilia treatment. Haemophilia 2008; 14 (Suppl 3): 10-8. Fischer K, Van der Bom JG, Mauser-Bunschoten EP, et al. Effects of postponing prophylactic treatment on long-term outcome in patients with severe haemophilia. Blood 2002; 99: 2337-41. Coppola A, Franchini M, Tagliaferri A. Prophylaxis in people with haemophilia. Thromb Haemost 2009; 101: 674-81. Gringeri A, Lundin B, von Mackensen S, et al. A randomized clinical trial of prophylaxis in children with hemophilia A (the ESPRIT Study). J Thromb Haemost 2011; 9: 700-10. Tagliaferri A, Rivolta GF, Iorio A, et al. Mortality and causes of death in Italian persons with haemophilia, 1990-2007. Haemophilia 2010; 16: 437-46. Coppola A, Santoro C, Franchini M, et al. Emerging issues on comprehensive hemophilia care: preventing, identifying, and monitoring age-related comorbidities. Semin Thromb Hemost. 2013; 39: 794-80. Soucie JM, Nuss R, Evatt B, et al. Mortality among males with hemophilia: relations with source of medical care. Blood 2000; 96: 437-42. Colvin BT, Astermak J, Fischer K, et al. European principles of haemophilia care. Haemophilia 2008; 14: 361-74. Maio V, Manzoli L. The Italian Health Care System: W.H.O. ranking versus public perception. P&T, Pharmacy and Therapeutics 2002; 27: 301-8. Calizzani G, Vaglio S, Arcieri R, et al. Models for institutional and professional accreditation of haemophilia centres in Italy. Haemophilia 2013; 19: e248-55. Calizzani G, Candura F, Menichini I, et al. The Italian Institutional Accreditation Model for Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s510-4. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia 2013; 19: e1-47. Hassan HJ, Morfini M, Taruscio D, et al. Current status of Italian Registries on inherited bleeding disorders. Blood Transfus 2014; 12 (Suppl 3): s576-81. National registry of congenital bleeding disorders. Report 2011. Rapporti ISTISAN 12/55 (in Italian). Available at http://www.iss.it/binary/publ/cont/12_55_web.pdf. Accessed on 16/02/2014. Iorio A, Oliovecchio E, Morfini M, et al. Italian Registry of Haemophilia and Allied Disorders. Objectives, methodology and data analysis. Haemophilia. 2008; 14: 444-53. Federazione delle Associazioni Emofilici. Il quadro dell'emofilia in Italia: i bisogni delle persone e le strategie 23) 24) 25) 26) 27) 28) 29) 30) 31) 32) 33) 34) messe in campo. Rapporto ICON. Roma, 25 maggio 2005. Available at: http://fedemo.it/cat/per-il-medico/rapporti/. Accessed on 16/02/2014. Calizzani G, Profili S, Candura F, et al. The demand for factor VIII and for factor IX and the toll fractionation product surplus management. Blood Transfus 2013; 11 (Suppl 4): s64-76. Santagostino E, Mannucci PM, Bianchi Bonomi A. Guidelines on replacement therapy for haemophilia and inherited coagulation disorders. Haemophilia 2000; 6: 1-10. Gringeri A, Mannucci PM, Italian Association of Haemophilia Centres. Italian guidelines for the diagnosis and treatment of patients with haemophilia and inhibitors. Haemophilia 2005; 11: 611-9. Mannucci PM. Plasma-derived versus recombinant factor VIII concentrates for the treatment of haemophilia A: plasmaderived is better. Blood Transfus 2010; 8: 288-91. Franchini M. Plasma-derived versus recombinant factor VIII concentrates for the treatment of haemophilia A: recombinant is better. Blood Transfus 2010; 8: 292-6. Calizzani G, Arcieri R. Clinical and organisational aspects of haemophilia care: the patients' view. Blood Transfus 2012; 10: 110-1. Gringeri A. Factor VIII safety: plasma-derived versus recombinant products. Blood Transfus 2011; 9: 366-70. Mantovani LG, Monzini M, Mannucci PM, et al. Differences between patients', physicians' and pharmacists' preferences for treatment products in haemophilia: a discrete choice experiment. Haemophilia 2005; 11: 589-97. Schramm W, Gringeri A, Ljung R, et al. Haemophilia care in Europe: the ESCHQoL study. Haemophilia 2012; 18: 729-37. Manco-Johnson MJ, Kempton CL, Reding MT, et al. Randomized, controlled, parallel-group trial of routine prophylaxis vs. on-demand treatment with sucrose-formulated recombinant factor VIII in adults with severe hemophilia A (SPINART). J Thromb Haemost 2013; 11: 1119-27. Tagliaferri A. Awaiting evidence-based recommendations on prophylaxis in adult patients. Haemophilia 2010; 16: 955-6. Alioto A, Garnero A, Calizzani G, Arcieri R. Lo sviluppo dei percorsi per la gestione delle emergenze emorragiche nelle regioni italiane. Blood Transfus 2011; 9 (Suppl): 6. Coppola C, Tagliaferri A, Calizzani G, et al. Clinical use and the Italian demand for activated prothrombin complex and activated recombinant factor VII concentrates. Blood Transfus 2013; 11 (Suppl 4): s101-9. Mancuso ME, Berardinelli L, Beretta C, et al. Improved treatment feasibility in children with hemophilia using arteriovenous fistulae: the results after seven years of follow-up. Haematologica 2009; 94: 687-92. Mannucci PM, Roberts HR. Uncertain time for research on hemophilia and allied disorders. J Throm Haemost 2005; 3: 423. EUCERD Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States (24 October 2011). Available at: http://www.eucerd.eu/upload/ file/EUCERDRecommendationCE.pdf. Accessed on 16/02/2014. Makris M, Calizzani G, Fischer K, et al. The European Haemophilia Network (EUHANET). Blood Transfus 2014; 12 (Suppl 3): s515-8. Correspondence: Romano Arcieri Federation of Hemophilia Associations (FedEmo) Via Lorenzo il Magnifico 148 00162 Rome, Italy e-mail: romano.arcieri@fedemo.it Blood Transfus 2014; 12 Suppl 3: s563-6 DOI 10.2450/2014.0036-14s s566 ORIGINAL ARTICLE The social burden and quality of life of patients with haemophilia in Italy Yllka Kodra 1, Marianna Cavazza 2, Arrigo Schieppati 3, Marta De Santis 1, Patrizio Armeni 2, Romano Arcieri4, Gabriele Calizzani5, Giovanni Fattore2, Lamberto Manzoli6, Lorenzo Mantovani6, Domenica Taruscio1 1 Italian National Centre for Rare Diseases, National Institute of Health, Rome; 2Centre for Research on Health and Social Care Management (CERGAS) Bocconi University, Milan; 3Clinical Research Centre for Rare Disease, Mario Negri Institute, Ranica and Department of Medicine, Rare Disease Unit, Papa Giovanni XXIII Hospital, Bergamo; 4Italian Federation of Haemophilia Societies, Rome; 5National Blood Centre, National Institute of Health, Rome; 6Italian Federation of Haemophilia Societies, Medical Council, Rome, Italy Background. In Italy, the project on the social burden and quality of life (QoL) of patients with haemophilia investigates costs from a society perspective and provides an overview of their quality of life. Moreover, as life expectancy increased in recent years along with new treatment strategies implemented in the last decades, it analyses trends of costs other than drugs simulating impacts during patient whole life. Material and methods. We ran a web-based cross-sectional survey supported by the Italian Federation of Haemophilia Societies in recruiting patients with haemophilia and their caregivers. We developed a questionnaire to collect information on demographic characteristics, healthcare and social services consumption, formal and informal care utilisation, productivity loss and quality of life. In particular, quality of life was assessed through the EuroQoL tool. Last, we applied the illness cost method from a society perspective. Results. On average, quality of life is worse in adult patients compared to child and caregivers: more than 75% of adult patients declare physical problems, 43% of adult patients and 54% of their parents have anxiety problems. Assuming a society perspective, the estimated mean annual total cost per patient in 2012 is 117,732 €. Drugs represent 92% of total costs. Focusing on costs other than drugs, each additional point of EuroQoL tool implies a costs' reduction of 279 €. The impact of age varies across age groups: each added year implies a total decrease of costs up to 46.6 years old. Afterwards, every additional year increases costs. Discussion. Quality of life of patients with haemophilia and their caregivers improved and it influences positively on consumed resources and on their contribution to the social-economic system. Costs other than drugs for patients with haemophilia follow the same trends of general population. Keywords: quality of life, cost of illness, haemophilia. Introduction Haemophilias are a group of inherited bleeding disorders caused by an X-chromosome linked deficiency in coagulation factors VIII (FVIII) (in haemophilia A) or IX (FIX) (in haemophilia B). The disorders are rare affecting approximately 1 in 10,000 births1. The prevalence in Italy, according to the most recent report (2012) of the Italian Association of Haemophilia Centres that operates a national registry, consists of 3,690 patients with haemophilia A and 750 with haemophilia B2,3. The use of factor replacements has significantly decreased the mortality and morbidity of patients with haemophilia: life expectancy has increased from 40 years old in the 1960s to 60-70 years today4,5. Quality of life (QoL) has become an important measure of the health improvements in haemophilic patients brought about by therapeutic progress in this field, although it remains significantly poorer as compared with QoL of general population6,7. Specifically, QoL is viewed as a measure of the outcome of care for individuals with haemophilia that can inform disease management and policy decision making8. It is not known, however, whether changes in QoL can have an impact on costs trend in the case of haemophilia9. Last, while there are several studies on QoL in haemophilia10-12, there have been very few on caregivers QoL13-15. On the other hand, the diffusion of new treatment strategies, based not only on factor replacement therapy, but also on a switch from the on demand to prophylaxis treatment, has also an economic impact. Actually, it requires a dramatic increase of economic resources' consumption by a small portion of the population affected by a rare condition and therefore the third-payers interest on this disease is also increased. Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s © SIMTI Servizi Srl s567 Kodra Y et al In particular, it is an example of the socioeconomic impact of biotechnology in rare diseases16. Hence, the scientific literature considering economic aspects has focused mainly on the cost-effectiveness of prophylaxis vs on-demand treatment in patients with a severe haemophilia17,18 or with inhibitors19. A further set of manuscripts implements a cost of illness approach on haemophilia in different countries and in some cases the economic and the social burden of this disease is included20-23. Moreover, amongst the latter ones, only one study21 have addressed in some way the relationship between age and QoL on one side, and costs on the other side. This is, actually, a new perspective arisen from the life expectancy increase in these last years. In the early 2000s, seminal contributions concerning the Italian context provided direct healthcare costs evaluation for patients with haemophilia complicated by inhibitors in the Cost of Care Inhibitors Study16 and the first estimation of the QoL of patients without inhibitors in the Cost of Care of Hemophilia Study24. The Burden and Health-Related Quality of Life in Patients with Rare Diseases - BURQoL-RD Study was a 3 year project under the 2nd Programme of Community Action in the Field of Public Health, that commenced in April 2010 and was promoted by the Directorate General Health and Consumers of European Commission. The main aim of BURQoL-RD was to generate a model to quantify the socio-economic costs and QoL of both patients and caregivers, for up to 10 rare diseases (RD) in different European countries. According to this goal, the evaluation of the economic and social impact of haemophilias has been one of the objects of BURQoL-RD Study. Therefore, the BURQoL-RD Study on haemophilia in Italy investigates costs of this disease from a society perspective (using a cost of illness approach) for the first time and it provides an update of this group of patients' QoL. Moreover, considering the increase of life expectancy occurring in these last years, it analyses the impact of this trend on costs other than drug, simulating the whole life cycle. Last, as the expensive switch of treatment strategies implemented in the last decade has provided an increased QoL, we are going to test this improvement's impact on costs other than drugs. Materials and methods We conducted a web-based cross-sectional study. The target sample were Italian patients diagnosed with haemophilia A and B and their caregivers. Cases were recruited from the Italian Federation of Haemophilia Societies (Federazione delle Associazioni Emofilici,FedEmo, www.fedemo.it). All patients and caregivers were informed about the study objectives and data confidentially, and were asked to indicate their understanding of the study conditions and agreement to participate. The survey was anonymous, as the patients were contacted by their patient organisation and their responses, without any identification data, were sent directly to the researchers. The fieldwork was carried out between March 2012 and October 2012. The questionnaires were administrated by e-mail through patient organisations and patients were asked to provide information on demographic characteristics, consumed healthcare and non healthcare resources related to the disease and QoL information in the six months preceding the enrolment (12 months for hospital admissions). Costs' materials and methods To measure the burden of haemophilia, we have applied the cost of illness approach from a society perspective25. Therefore, both direct and indirect costs were included, and a bottom-up approach was used for their calculation: we valued the average unit cost of each set of resources consumed by enrolled patients. Direct costs include health and non-healthcare resources directly consumed by the surveyed Italian patients with type A and type B haemophilia in 2012. Direct health care costs include drugs, outpatient and inpatient care, and all range of primary care services. As far as their data source, we used services' fees because Italy does not have a national healthcare services' costs data set and we could not run specific costs' survey. However, we applied region Lombardy's fees as this region has updated nearly regularly its tariff set, surveying its providers' costs26. Moreover, as far as drugs, we have considered Italian Medicines Agency 's drugs national formulary, reducing by 30% the price of drugs distributed only by hospitals once they bought them through tenders. Considering the co-payment of drugs and outpatient care, we estimated a national average of regional fees. Last, according to the following strategy, we estimated the healthcare services fees out of Italian National Health Service (INHS), paid out of pocket by patients: we selected a small and a big town in Northern, Centre and Southern Italy and then we ran a pricing market analysis. Direct non healthcare costs comprise socialhealthcare and social services managed at city-council level: the resulting high fragmentation of these services' provision has led us to implement again the above described strategy to collect information on this setting without national or regional standards. This cost's set includes not only the formal care (i.e. provided by contracted professionals), but also the informal care provided by relatives and friends. We have applied the proxy good approach to value these resources, then we have considered if he/she did not provide these services, he/she would need to be replaced by another person who could provide the necessary care, applying the average Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s568 Costs, quality of life of Italian patients with haemophilia hour wage of contracted professionals27. According to evidences provided by literature on different amount of consumed resources by adults and children, we have differentiated costs analysis between these two populations. Indirect costs refer to the output lost by society because of cessation or reduction of productivity (i.e. productivity loss) resulting from morbidity, or disability brought on by the disease. We have collected the following information about patients and caregivers through the questionnaire: i. the working days and the hours per day lost because of disease, and ii. the age of their possible early retirement. Therefore, we have estimated the productivity loss of both patients and caregivers, considering both the sick leaves of both patient and caregiver as well as the economic impact of an early retirement. We have applied the human capital approach28, valuing the amounts of days and hours of sick leaves by the per hour Italian average wage, according to 2012 Eurostat estimation. Moreover, we have estimated the charge of early retirement by valuing the lost gain from retirement contributions of the working years out of the job market according to Eurostat, and the public expenditure because of the early pension's provision based on National Social Insurance Agency (INPS - Istituto Nazionale della Previdenza Sociale) data set. QoL's materials and methods EuroQoL (EQ-5D) was adopted to evaluate the QoL. EQ-5D is applicable to a wide range of medical conditions and treatment and generates a health profile (EQ profile) consisting of 5 domains (mobility, self-care, anxiety/depression, usual activities, and pain/discomfort). For adult and caregivers EQ-5D-5L with 5 levels ("no problem", "some or moderate problems", "extreme problems/impossible to do") was administrated. For children (under 18 years old), the EQ-5D-Y-3L (children version) with 3 level was used ("no problems", "some problems", "extreme problems"). A visual analogue scale (EQ-VAS) scores the overall QoL from 0 (the worst imaginable health status) to 100 (the best imaginable health status). Results from the EQ profile can be converted to utility index, suitable for economic evaluations, by means of an algorithm that uses population-based (social) values. Because specific conversion values for the Italian population are not available yet, we have converted our EQ profile results in EQ utility index, running the algorithm with values from Spain29. Statistical analysis Since it was planned to enrol all patients with haemophilia registered in FedEmo's patients organisations, no sample size calculation was performed. For cost analysis we used means and central tendency parameters, generally expressed as mean cost per patient per year, because this parameter can be easily used for policy maker. We reported the standard deviations as a variability measure. Costs were stratified according to their categories. Descriptive analyses were applied also to define health status measurements variables and QoL separately for adult, children and caregivers. It was convenient to reclassify the EQ-5D-5L and EQ-5D-Y-3L levels into 'no problems' (i.e. level 1) and "problems" (i.e. levels 2 to 5 for EQ-5D-5L and level 2 to 3 for EQ-5D-Y-3L). For categorical measures, statistical significance was determined by using chi-squared test. The one-way analysis of variance (ANOVA) was used to determine whether there were any significant differences between the means of two or more independent (unrelated) groups. Intra class correlation between ranked (ordinal) data, such as EQ-5D, was determined by means of Spearman's correlation coefficients (correlations >r=0.4 were considered relevant). A multiple linear regression was ran in order to assess the relationship between the patients' total costs without drugs (dependent variable) and patients' age and EQ-5D. We tested a possible non-linear (quadratic) relationship for both independent variables and we controlled for drugs costs and age of diagnosis. Moreover, based on estimation results, we ran a two-way simulation analysis to evaluate the joint impact of every pair of age and EQ-5D on costs, all other things being equal. We let both independent variables to range between 0 and 100 in order to capture every possible combination of the two, also including out-of-sample values. Descriptive analyses were performed using SPSS version 21.0 software. Regression analysis and two-way simulation analysis were performed using Stata, release 12. Statistical significance was set up at p<0.05 where sample size permitted. Results Characteristics of the sample A total of 134 questionnaires were collected, 45 of which were excluded because of insufficient or inadequate provided information. The valid sample consisted of 89 patients and 17 caregivers. The mean age was 42.3 (SD±13.0;) years old for adults, 8.0 (SD±4,6) for children and 40.7 (SD±16.0) for careers. Only 3 patients more than 65 years old were enrolled in this study. The main characteristics of patients are shown in Table I. The majority of patients were adults (75.3%) with haemophilia A (79.8%). Ninety-nine per cent of adult patients were married. 82% of patients had a mediumhigh educational level. Sixty percent of adult patients Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s569 Kodra Y et al were employed at the moment of the survey (Table I). Table I - Socio-demographical sample characteristics of patients. Patient sample (n=89) Value Age, n (%) Child (2-17 years old) Adult (≥18 years old) 22 (24.7) 67 (75.3) Frequency, n (%)1 Patients with Haemophilia A Patients with Haemophilia B 71 (79.8) 15 (16.9) Married/with a partner2 60 (90.9) Education level Medium-high (for adult patients) Schooled in an ordinary centre (for children 7-17 years) 55 (82.1) 13 (100) Need for career n (%) 21 (23.3) Employment status (for adult patients) n (%) 1 40 (59.7) Three values were missing; Calculation is made only for adult. 2 QoL results On average, QoL was worse in adult patients compared to child and career according to EQ-VAS (ANOVA; p=0.000) (Table II). Table II - EQ-VAS value and EQ utility index by different study group categories. N. Mean EQ-VAS (DS) EQ utility index (DS) P value Child 13 92.8 (7.5) 0.78 (0.43) 0.0000 Adult 60 68.7 (18.8) 0.69 (0.25) Caregivers 16 83.1 (14.9) 0.95 (0.62) Total 89 74.8 (19.2) 0.70 (0.28) 1 17 values are missing. 1 For adult patients with haemophilia, EQ-VAS score was lower than in general population (Mean=75.8; SD±16.6; Catalonian conversion values29). For children patients non value sets are available for comparison. QOL domains by adult, caregivers and child subjects were examined at a descriptive level (Table III). More than 75% of adult patients had problems in the physical sphere, specifically for mobility (75%) and pain/discomfort (76.7%). 43.3% of adult patients and 53.9% of parents had anxiety problems. For mobility, usual activities and pain/discomfort, the proportions were significantly different between study group. No differences were verified in self-care and anxiety dimension (Table III). Costs results Assuming a society perspective, the estimated average annual total cost per person in 2012 is 117,731.72 € (Table IV). The set of direct healthcare costs is the main driver requiring yearly in average 109,768.70 € per person: specifically, the item drugs is the 98% of this latest and the 92 % of the whole cost in absolute value. The children annual average costs of drugs is higher than adults (130,649.40 € vs 100,649.80 €). Moreover, as we have a very high standard deviation, we have set classes of average annual costs: in this perspective, the 55% of children patients have a drugs cost greater than 200,000 € vs the 38% of adult patients. Excluding haematologic visits, adults (29% is 49 years old over) required an average of 3.89 specialist visits in six months while children needed 2.04 specialist visits in the same period of time. Adults most often required specialist visit by cardiologist, surgeon, orthopedist and dentist. Both adults and children shared a high level of access to physiotherapy sessions (data not shown). Direct non healthcare costs (in average 5,223.08 €) represent the 4.4% of the total costs -in absolute Table III - Proportion of "problem" and "no problem" by EQ dimensions and by adults, children and caregivers. Adult Mobility Self-care Usual activities Pain/discomfort Anxiety/depression Child Caregivers p value n. % n. % n. % No problems 15 25.0 10 76.9 5 38.5 Problems 45 75.0 3 23.1 8 61.5 No problems 36 60.0 12 92.3 7 53.8 Problems 24 40.0 1 7.7 6 46.2 No problems 22 36.7 12 92.3 7 53.8 Problems 38 63.3 1 7.7 6 46.2 No problems 14 23.3 11 84.6 6 46.1 Problems 46 76.7 2 15.4 7 53.9 No problems 34 56.7 11 84.6 6 46.1 Problems 26 43.3 2 15.4 7 53.9 0.000 0.1 0.001 0.000 0.3 Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s570 Total 880.17 € 21.32 0.00% € € € € 114,991.78 Secondary caregivers No healthcare transportation Subtotal Total direct costs (Direct HC Costs and Direct Non HC costs) 991.38 2,739.94 € € € 117,731.72 Loss of labour productivity carers (sick leave and early retirement Subtotal Total costs € 98,013.37 € 7,241.01 100% € 108,750.30 100% 2,320.01 31.46 2,288.55 € € € 2.33% 0.84% 1.49% 36.18% 0.00% 1,748.56 € 3,285.07 132.24 - 2,961.57 2,961.57 191.26 € 106,430.31 € € € € € 4.44% € € 5,904.85 4.59 59.51 587.29 786.15 995.99 61.91 € 103,145.24 € € € € € € € 100,649.80 Mean 97.67% 0.09% 0.36% 3.85% Loss of labour productivity patients (sick leave and early retirement) 63.82% 100% € 20,815.10 € 4,495.55 2.00% 8.14% 86.82% 231.59 € € 2,266.51 € 20,153.44 94.96% Indirect costs 5,223.08 104.43 425.16 4,534.76 € Main caregivers € 22,419.95 4.21% 4,959.92 3.04% € 535.39 Caregiver's time costs (informal care) € 0.13% 93.24% 0.00% 100% 0.00% 0.38% 0.05% 158.72 € 96164.64 0.41% 0.05% 0.75% 0.51% € 3.51 € € 109,768.70 Healthcare transportation Subtotal 137.38 € 1,510.65 € 0.80% 0.55% 0.04% 91.50% % per total costs Social services 54.46 € 1,556.10 € 1,582.75 0.05% 98.14% % cost category Direct non healthcare costs 448.72 € € 600.65 Devices Primary care Acute hospitalization € € Specialistic visits 160.56 € € Tests 52.89 € 95,866.80 € 107,728.30 SD Drugs Direct health care costs Mean 24.34 139.51 1,707.27 1,772.65 1,747.58 182.30 601.42 258.96 5,132.52 259.42 5,028.93 € 96,133.36 € € € € 21,237.26 € € € 21,092.40 € 21,092.40 € € 103,145.24 € € € € € € € 96,513.22 SD Adult 100% 1.36% 98.64% 100% 4.03% 0.00% 90.15% 90.15% 5.82% 100% 0.00% 0.06% 0.57% 0.76% 0.97% 0.06% 97.58% % cost category 100% 2.13% 0.03% 2.10% 0.00% 97.87% 3.02% 0.12% 0.00% 2.72% 2.72% 0.18% 0.00% 94.85% 0.00% 0.05% 0.54% 0.72% 0.92% 0.06% 92.55% % per total costs - 38.10 - - 505.14 23.67 53.33 11,498.54 14.40 1,801.88 9,628.92 4,099.70 4,099.70 - € 146,814.60 € € € € 142,714.84 € € € € € 11,430.80 € € 131,216.30 € € € € € € € 130,649.40 Mean 11,828.46 11,828.46 - 18,475.38 14.52 4,471.95 16,157.54 20,629.49 185.08 92,400.97 - 132.20 - - 479.63 30.45 92,257.03 € 100,733.90 € € € € € € € € € € € € € € € € € SD Children 100% 100% 0.00% 100% 0.13% 15.67% 83.74% 99.41% 0.46% 100% 0.00% 0.03% 0.00% 0.00% 0.38% 0.02% 99.57% % cost category 100% 2.79% 2.79% 0.00% 0.00% 97.21% 7.83% 0.01% 1.23% 6.56% 7.79% 0.04% 0.00% 89.38% 0.00% 0.03% 0.00% 0.00% 0.34% 0.02% 88.99% % per total costs Table IV - Total and percent distribution of direct health care, non health care and indirect costs per patient with haemophilia by adult and paediatric populations, in 2012, in Italy. Costs, quality of life of Italian patients with haemophilia Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s571 Kodra Y et al values- and the most relevant category is the informal care (95%). Specifically, the 23.6% of hemophilic patients surveyed state a need of care and -except oneall of them have an informal care: specifically, the 57% of children require this service vs the 13% of adult patients, moreover these latest do not need a secondary caregiver. As not all caregivers of adult patients provided the required data to value their time, the related results give poor information. Therefore, we focus on children informal care: in this case, the annual average cost of the main caregiver is 9,628.92 € and that one of secondary caregivers is 1,801.88 €. As far as the other items of non healthcare costs, these include social services and non healthcare transport which represent respectively the 3% and the 2% of total costs. In this case, adults are the greater consumer of these services. Lastly, indirect costs include the loss of productivity by patients and caregivers because of sick leave or early retirement. Thirty-four percent of the patients interviewed stated that their labour productivity had decreased in the previous six months because of the disease: specifically, they had an average 38 days of sick leaves a/o they worked in average two hours less per day. Moreover, the 58% of the retired patients did it earlier than the proper retirement age. As far as caregivers, the average number of lost working days was 78 in the previous six months and the average lost working hours were daily 4. Therefore, the annual average value of productivity loss is 2,739.94 € (2% of total costs). This aggregated value requires also to be differentiated between adults and children as the main cost driver of the earliest group is the productivity loss of patients (98%) while the main one of children is of course the productivity loss of caregivers equal to the annual average value of € 4,099.70. The regression of costs without the drugs item on a set of independent variables already described allows us to investigate on the relationship running between the total costs and patients' age and Qol, controlling for drugs' costs and age of diagnosis (Table V). The relationship between EQ-5D and costs without drugs is linear (the quadratic term is not significant) while the quadratic hypothesis is supported for age. In particular, whatever the age, each additional point of EQ-5D implies a reduction in costs of 279 €. A withinsample simulation based on this regression shows that in our sample the 95% confidence interval of EQ-5D is 68.39-77.55, implying a cost-variability of 2,556 €, after controlling for age. Considering the impact of age, whatever the level of EQ-5D, the effect varies across age levels. Starting from an age of 0, an increase by one year implies a cost reduction of 618 €. However this impact is attenuated by 13.27 € every additional year of starting. Therefore the effect of an additional year between an age of 3 and 4 is obtainable from the first order derivative calculated at 3 year and which is −618 € +(3 years×13.27 €)= −578 € (where 13.27 = 2×6.64, the coefficient of the squared term). The minimum point of the parabola is found at the age of 46.6 years old. After that point the impact of age becomes positive, i.e. every additional age makes costs increase. For example, the impact of an additional year between the ages of 55 and 56 is −618 €+(55 years×13.27 €)= +112 € (Figure 1). Discussion The BURQoL-RD study on haemophilia provides an update of patients' QoL, and for the first time in Italy offers an estimation of average total unit cost in the society perspective. This study also shows that there is a significant relationship between both age and QoL, and costs other than drugs. Moreover, our results are consistent with literature on drugs as the main cost driver of haemophilic patients' expenses. These results are relevant because they contribute to further analyse two evidences highlighted by the scientific literature: the treatment strategy's change that occurred in these last years (i.e. the switch from ondemand to prophylaxis based treatment and the factor replacement) and the increase of patients' QoL and life expectancy provided by a greatly improved patient's management. We have used the overall costs other than drugs because of three reasons. Firstly, the BURQoL-RD Table V - Correlation between EQ 5D, total costs, patients' age, age of diagnosis, and total costs other than drugs: multilinear-regression model (n=68)*. Independent variable Coefficient Standard error t P value 95% Confidence Interval EQ 5D −279.4714 64.77232 −4.31 0.000 −408.9916; −149.9511 Drugs costs .0004994 .0093903 0.05 0.958 −.0182777; .0192765 Patients' age −618.0774 208.6071 −2.96 0.004 −1035.213; −200.9416 Squared patients'age 6.636786 2.776952 2.39 0.020 1.083927; 12.18964 Age of diagnosis −154.6141 138.5862 −1.12 0.269 −431.7343; 122.506 *Prob>F=0.0000; Root MSE=6682.3; F(6, 61)=7.56; R-squared=0.3102 Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s572 Costs, quality of life of Italian patients with haemophilia Figure 1 - Trend of costs other than drugs correlated to QoL and age. project provides data on drugs consumption and their valorisation, however information on patients' severity and the related treatment plans are not available, restricting the possible interpretation of drugs' data. Secondly, the core of the treatment strategy's change is the switch from on-demand to prophylaxis based treatment along with new drugs' use: this substitution may imply that the patient's consumption of drugs does not change for long whiles, making drugs' cost no more a fully variable cost over time. Last, even if costs other than drugs represent a small quota of total costs, they have been poorly investigated up to now and their analysis allows to enlighten relevant aspects with respect to the trends we are addressing. The first evidence to consider is the positive impact of new treatment's strategies on patients' QoL: this is a consolidated evidence in both type A and B haemophilia30,31 even if it implies a relevant increase of costs and the debate on the related cost-effectiveness, usually in a third-payer perspective, is still open32. Hence, as we have in hand both direct and indirect costs of this Italian patients' sample, we have tested the impact of a possible QoL improvement on this set of costs, excluding the drug ones: this is a step towards estimating how much the new drugs' greater costs are offset by a decrease of other costs' items33,34. The result is that every EQ-5D point added implies a quota of decreased total costs other than drugs: therefore, an improved QoL has an impact not only on the patient's life, but also on consumed healthcare and non healthcare resources related to the disease by these patients and on their capacity to contribute positively to the socialeconomic system where they live. The second evidence concerns the increased life expectancy that also Italian haemophilic population has experienced2. Specific guidelines and clinical pathways to manage the comorbidities, complications and management aspects are needed now that haemophiliac patients' are getting older35-37. However, it seems that poor attention has been paid to the impact on costs of this aging process. Hence, we have found a significant relationship between age and total costs other than drugs and moreover we have simulated the trend of this set of costs over the patients' whole life cycle. The main finding is that costs other than drugs for haemophilic population follow the same trend of the general population38 or people with diabetes39: costs are at their highest level in the very first years of life and then they decrease up to the age of nearly 46 years old when they start to increase again. Moreover, we have Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s573 Kodra Y et al identified the main driver of costs other than drugs according to the population age: as far as children, the most relevant item of cost is the informal care provided by parents and their related productivity loss that it had never been estimated previously in Italy. In adults, the driver is not only hospitalisation, but also specialist visits including a significant quota of cardiology, dentist and ophthalmologist visits, and these results are consistent with the literature above mentioned. Although this study provides valuable insights into the QoL and the costs of patients with haemophilia and their caregivers, there are some limitations that warrant mention. Both the sample and the recruitment process limit the external validity of the study. A limit of this study is the costs' data source. As far as healthcare services provided by INHS, we have valued them by tariffs which are a costs' proxy, however we have selected the Region Lombardy's ones as they are the most regularly updated according to costs' surveyed at providers. A further problem has been to identify the fees of services provided out of INHS coverage: unfortunately, there are not updated price lists determined by professionals associations and then we resorted to a sort of market survey. A similar difficulty has risen about the social services supplied by the city councils and possibly by Local Healthcare Units when an healthcare expertise is required: the fragmentation level prevents to provide any national or regional average. Therefore, we have implemented a spot survey considering the geographical variability and the size of the city council involved. A further drawback of the study is that the disease severity and treatment were not recorded, limiting our ability for additional stratification by variables of interest. We categorize participants only in terms of disability level. Considering the low level of disability, probably our sample reflects a more motivated and less disabled patient/caregiver population. As BURQoL-RD project comprised other RDs and aimed to possible comparison with general population, to measure the QoL we did not use disease specific instruments for haemophilia. loss of productivity of informal carers that has to be considered. Finally, the ageing of haemophilic population beyond previous life expectancy limits is posing new challenges to the health care systems requiring planning of resources and health care provisions. Funding and resources This deliverable arises from the project "Social Economic Burden and Health Related Quality of Life in Patients with Rare Diseases in Europe" which has received funding under the 2 nd Programme of Community Action in the Field of Public Health. The Authors declare no conflict of interest. References 1) 2) 3) 4) 5) 6) 7) 8) 9) Conclusions The BURQoL study on Italian haemophilic patients provides the first estimation of total costs in the society's perspective that can be of value to policy-makers. The QoL increase in haemophilic patients implies both a life's improvement and a decrease in the overall costs other than drugs: even if we do not have yet evidence that the new drugs' increased costs may be offset by the other costs' reduction, the drugs' costs extent over the total ones suggests that only a partial offset might be possible. A second evidence concerns the charge's level of informal care supplied to haemophilic children and the related 10) 11) 12) 13) Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Treatment Guidelines Working Group on Behalf of The World Federation Of Haemophilia. Guidelines for the management of haemophilia. Haemophilia 2013; 19: e1-47. Abbonizio A, Giampaolo A, Arcieri R, et al. Registro Nazionale delle Coagulopatie Congenite. Rapporto 2011. Rapporti ISTISAN 2012; 55/12: iii, p 63. Italian Association of Haemophilia Centres (AICE). Individuals with Factor VIII Deficiency and Individuals with Factor IX Deficiency. Data Summaries 2012 Dec. Available at: http://www.aiceonline.it/emocard/summaries.htm. Accessed on 20/01/2014. von Mackensen S, Gringeri A, Siboni SM,et al. Health-related quality of life and psychological well-being in elderly patients with haemophilia. Haemophilia 2012; 18: 345-52. Tagliaferri A, Rivolta GF, Iorio A, et al. Mortality and causes of death in Italian persons with haemophilia, 1990-2007. Haemophilia 2010; 16: 437-46. Klamroth R, Pollmann H, Hermans C, et al. The relative burden of haemophilia A and the impact of target joint development on health-related quality of life: results from the ADVATE Post-Authorization Safety Surveillance (PASS) study. Haemophilia 2011; 17: 412. Gringeri A, Mantovani LG, Scalone L, et al. for the COCIS Study Group. Cost of care and quality of life for patients with hemophilia complicated by inhibitors: the COCIS Study Group. Blood 2003; 102: 2358-63. Naraine VS, Risebrough NA, Oh P, et al. Health-related quality-of-life treatments for severe haemophilia: utility measurements using the Standard Gamble technique. Haemophilia 2002; 8: 112-120. Franchini M, Mannucci PM. Co-morbidities and quality of life in elderly persons with haemophilia. Br J Haematol. 2010; 148: 522-33. Gringeri A, von Mackensen S, Auerswald G, et al. Health status and health-related quality of life of children with haemophilia from six West European countries. Haemophilia 2004; 10 (Suppl 1): 26-33. Pollak E, Mühlan H, von Mackensen S, et al. The Haemo-QoL Index: developing a short measure for health-related quality of life assessment in children and adolescents with haemophilia. Haemophilia 2006; 12: 384-92. Szende A, Schramm W, Flood E, et al. Health-related quality of life assessment in adult haemophilia patients: a systematic review and evaluation of instruments. Haemophilia 2003; 9: 678-87. Beeton K, Neal D, Watson T, Lee CA. Parents of children with haemophilia - a transforming experience. Haemophilia 2007; 13: 570-9. Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s574 Costs, quality of life of Italian patients with haemophilia 14) Wiedebusch S, Pollmann H, Siegmund B, Muthny FA. Quality of life, psychosocial strains and coping in parents of children with haemophilia. Haemophilia 2008; 14: 1014-22. 15) Shaw D, Riley GA. The impact on parents of developments in the care of children with bleeding disorders. Haemophilia 2008; 14: 65-7. 16) Gringeri A, Mantovani LG, Scalone L, et al. Cost of care and quality of life for patients with hemophilia complicated by inhibitors: the COCIS Study Group. Blood. 2003; 102: 2358-63. 17) Miners AH, Sabin CA, Tolley KH, et al. Cost-utility analysis of primary prophylaxis versus treatment on-demand for individuals with severe haemophilia. Pharmacoeconomics 2002; 20: 759-74. 18) Steen Carlsson K, Höjgård S, Glomstein A, et al. On-demand vs. prophylactic treatment for severe haemophilia in Norway and Sweden: differences in treatment characteristics and outcome. Haemophilia 2003; 9: 555-66. 19) Odeyemi IAO, Guest JF. Modelling the economic impact of recombinant activated factor VII compared and activated prothrombin-complex concentrate in the home treatment of a mild to moderate bleed in adults with inhibitors to clotting factors VIII and IX at a comprehensive care centre in the UK. Journal of Medical Economics 2002; 5: 119-33. 20) Auerswald G, Von Depka Prondzinski M, Ehlken B, et al. Treatment patterns and cost-of-illness of severe haemophilia in patients with inhibitors in Germany. Haemophilia 2004; 10: 499-508. 21) Globe DR, Curtis RG, Koerper MA, HUGS Steering Committee. Utilization of care in haemophilia: a resourcebased method for cost analysis from the Haemophilia Utilization Group Study (HUGS). Haemophilia 2004; 10 (Suppl 1): 63-70. 22) Nerich V, Tissot E, Faradji A, et al. Cost-of-illness study of severe haemophilia A and B in five French haemophilia treatment centres. Pharm World Sci 2008; 30: 287-92. 23) Johnson K, Zheng Yi K. Costs of Care in Hemophilia and Possible Implications of Health Care Reform. ASH Education Book. December 10, 2011; vol. 2011 no. 1: 413-8. 24) Scalone L, Gringeri A, Von Mackensen S, et al. Quality o of life in haemophilic patients without inhibitors: the COCHE Study. Value in Health 2005; 8: A14. 25) Tarricone R. Cost-of-illness analysis: What room in health economics? Health Policy 2006; 77: 51-63. 26) Bartoli S, Cantù E. Le analisi dei costi per la determinazione delle tariffe: esperienze regionali a confronto. In: Cantù E. editor. Rapporto OASI 2009. L'aziendalizzazione della sanità in Italia. Milan: Egea; 2009; 221-48. 27) Van der Berg B, Brouwe B, Koopmanschap M. Economic valuation of informal care: an overview of methods and application. Eur J Health Ec 2004; 5: 36-45. 28) Drummond M, Sculpher MJ, Torrance GW, et al. Methods for economic Evaluation of Health Care Programmes 3th ed. Oxford University Press, Oxford 2005. 29) Badia X, Roset M, Herdman M, Kind P. A comparison of United Kingdom and Spanish general population time tradeoff values for EQ-5D health states. Med Decis Making. 2001; 21: 7-16. 30) Gringeri A, Leissinger C, Cortesi PA, et al. Health-related quality of life in patients with haemophilia and inhibitors on prophylaxis with anti-inhibitor complex concentrate: results from the Pro-FEIBA study. Haemophilia 2013; 19: 736-43. 31) Windyga J, Indyga VW, Lin J, et al. Improvement in healthrelated quality of life with recombinant factor IX prophylaxis in severe or moderately. Haemophilia 2013; 20: 1-7. 32) Farrugia A, Cassar J, Kimber K et al. Treatment for life for severe haemophilia A. A cost-utility model for prophylaxis vs. on-demand treatment. Haemophilia 2013; 19: e228-38. 33) Lichtenberg FR. Effects of New Drugs on Overall Health Spending: Frank Lichtenberg responds. Health Aff (Millwood). 2007; 26: 887-90. 34) Santerre RE. National and international tests of the new drug cost offset theory. Southern Economic Journal 2011; 77: 1033-43. 35) Mannucci PM, Schutgens REG, Santagostino E, MauserBunschoten EP. How I treat age-related morbidities in elderly persons with hemophilia. Blood 2009; 114: 5256-63. 36) Konkle BA. The aging patient with hemophilia. Am J Hematol. 2012; 87 (Suppl 1): S27-32. 37) Philipp C. The aging patient with hemophilia: complications, comorbidities, and management issues. Hematology Am Soc Hematol Educ Program. 2010; 2010: 191-6. 38) Ministry of Economy and Finance. Tendenze di medio lungo periodo del sistema pensionistico e socio-sanitario 2013. Ragioneria Generale dello Stato 2013 May; Rapporto n. 14. Available at:http://www.rgs.mef.gov.it/VERSIONE-I/Attivit-i/Spesa-soci/Attivita_di_previsione_RGS/2013. Accessed on 30/01/2014. 39) Diabetes American Association. Economic Costs of Diabetes in the U.S. in 2012. Diabetes Care. 2013; 36: 1033-46. Correspondence: Yllka Kodra Italian National Centre for Rare Diseases National Institute of Health Via Giano della Bella 34 00162 Rome, Italy e-mail: yllka.kodra@iss.it Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0042-14s s575 REVIEW Current status of Italian Registries on inherited bleeding disorders Hamisa Jane Hassan1, Massimo Morfini2, Domenica Taruscio3, Francesca Abbonizio1, Adele Giampaolo1, Yllka Kodra3, Emily Oliovecchio2, Luciano Vittozzi3 1 Section of Transfusion Methodologies, Department of Haematology, Oncology and Molecular Medicine, Italian National Institute of Health, Rome; 2Italian Association of Haemophilia Centres (AICE), Florence, 3National Centre for Rare Diseases, Italian National Institute of Health, Rome, Italy Introduction Inherited bleeding disorders are a group of congenital coagulopathies resulting when deficiencies of the proteins responsible for coagulation, platelet function or fibrinolysis occur. Haemophilia A (HA, deficiency of factor VIII), Haemophilia B (HB, deficiency of factor IX) and von Willebrand Disease (vWD) are the most frequent, being >90% of all inherited bleeding disorders with a prevalence of 0.5, 0.1 and 1-5/10,000 respectively1-3. Other rare inherited bleeding disorders are represented by deficiencies of factor I, II, V, VII, X, XI, XII, XIII, combined V+VIII, combined vitamin K-dependent factors, with a general population prevalence between 1/500,000 and 1/2,000,000 4. Inherited bleeding disorders require wide-ranging care and effective management within a multidisciplinary team setting. The modern treatments of inherited bleeding disorders are now remarkably effective, although expensive. In Italy the epidemiological data on inherited bleeding disorders derive from three registries: 1) The Italian National Registry for Rare Diseases (RNMR); 2) The National Registry of Congenital Coagulopathies (RNCC); 3) The Haemophilia Database of the Italian Association of Haemophilia Centres (AICE). These registries differ in terms of organisation, purpose and data collection process. A general description and results for each registry is reported as follow. Italian National Registry for Rare diseases Organisation The Italian National Registry for Rare Diseases has been established by law in 2001 (Ministerial Decree -M.D. n. 279/2001)5, and it is located at the National Centre for Rare Diseases (NCRD) of the Italian National Institute of Health (Istituto Superiore di Sanità - ISS). M.D. n. 279/2001 set up a specific Rare Disease (RD) network dedicated to the prevention, surveillance, diagnosis and treatment of RD patients, set out special rules for the assistance of RD patients and ensured that health services are appropriately delivered to RD patients. The "RD Network" is made of formally designated Centres by each Italian region (FDC), preferably based in hospitals and dedicated to the management, care, training and information of RD patients and research on RD. This network provides data to the RNMR. The mandate of the RNMR is to inform the national and regional planning of RD patient care and to collect demographic, history, clinical, laboratory determinant data of use for medical, biomedical and epidemiological research. The structure of the RNMR is made of three levels, reflecting the Italian Healthcare System: local, regional and national level. The local level is composed by FDC identified in each Region, which are the primary source of data flow. Clinicians of FDC collect demographic and clinical data and transmit them to the regional registries. This is the intermediate level of data flow. Each regional registry has different organisational structure, different objectives or aims, and as a consequence different types of information (variables) to be collected. The use of the RNMR central data repository and the related common data set for the communication of mandatory data from the regional registries to the RNMR was defined with two Agreements among State and Regions in 2002 and in 2007. This set includes socio-demographic as well as disease information of each case: encrypted patient identification code, date of birth, sex, region of residence; vital status (with decease date); diagnosis; RD centre which made the diagnosis; date of disease onset; date of diagnosis; orphan drug treatment. This data set is mainly devoted to monitor RD and RD services at national level. RNMR data are presented and discussed annually in the national meeting of the RNMR and regional RD registries and the production of annual reports has started in 20116. The RNMR monitors 495 conditions, including individual RD and groups of RD, which are listed in the technical annex to M.D. n. 279/2001. In particular, the following specific conditions of inherited bleeding disorders are under surveillance: inherited bleeding disorders, HA, HB, vWD, inherited deficiency of coagulation factors and platelets. Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s576 © SIMTI Servizi Srl Italian Registries on inherited bleeding disorders Results Up to 30 June 2012, a total of 11,135 notifications on inherited bleeding disorders have been collected at RNMR: 7,748 for inherited bleeding disorders; 1,809 for inherited disorders of platelets; 615 for HA; 503 for inherited deficiency of coagulation factors; 367 for vWD and 93 for HB. Cases ≤18 years represent 13%. Considerations The RNMR is a population-based/multi-diseases registry and consequently an important instrument of public health, useful for health planning and epidemiological surveillance. The strong legal base of the RNMR and the compliance with the national legal and ethical requirements ensures stability to the data collection. The future directions of RNMR are also to support the development of further clinical registries on specific RD, in order to better understand the natural history of RD. In fact the NCRD participates actively in a number of collaborative efforts with patient associations and networks of clinicians for the collection and exchange of patient data for specific RD registries; inherited bleeding disorders are the subject of a collaboration with the RNCC. Moreover the RNMR provides important indicators of accessibility of health care and health service utilisation by patients with RD. The RNMR is now implemented in all the Regions but data quality and completeness still need to be improved. Indeed, the collaboration with different registries has shown that case notification is far from being complete, with considerable variation of notification rate across the Italian territory. Moreover, the notification of inherited bleeding disorders in RNMR uses a non specific terminology, which should be updated to allow sounder epidemiological observations. The National Registry of Congenital Coagulopathies Organisation In Italy, haemophilia patients and other persons with inherited bleeding disorders are monitored by the RNCC established at the ISS with the collaboration of AICE. Since 1988 until 1999, at ISS was activated a Registry aimed in particular to the surveillance of infectious diseases in the haemophiliac population, that, at the time, represented the most serious adverse event in the replacement therapy of inherited bleeding disorders7,8. After 1999 and so far, the RNCC has been fed by AICE Database. Since 2005 a section of the Haematology, Oncology and Molecular Medicine Department is in charge of the management of the RNCC: collection, validation, elaboration and dissemination of the data. The RNCC was resumed as a specific pathology registry, in a stringent collaboration with AICE, the Haemophilia Treatment Centres (HTC) and the Patient's Association (FedEmo). The epidemiological surveillance of population with inherited bleeding disorders, treatmentrelated complications and monitoring of needs/ consumption of products utilised in the different regimen therapies are the main aims of the RNCC9-11. Data collected in the RNCC are relative to all the 53 Italian Haemophilia Centres, established by Regional laws, and distributed in the North (49%) Centre (17%) and South and Islands (34%). They assist the Italian patients with bleeding disorders with a coverage of almost 100% of the severe forms. The participation of the HTC to the RNCC data collection is on voluntary basis. Data are provided from the local databases to the national database anonymised and in accordance with the Italian privacy law and standards. Information collected in the RNCC are relative to 9,097 validated patients with HA and HB, vWD, other rare factor deficiencies (fibrinogen and factors II, V, VII, X, XI, XII, XIII inherited deficiencies), inherited platelet disorders and haemophilia carriers. Data are relative to prevalence of inherited bleeding disorders, treatment-related complications (infectious diseases and in particular inhibitor development), needs/consumption of plasma-derived and recombinant products utilised in the haemophilia replacement therapy. These variables are available at national and regional level, by age group and by treatment regimen (prophylaxis/on demand/immune tolerance induction). Haemophilia facilities, addresses, contact numbers and referents of the Centre are indicated and described in the appendix of the RNCC9. Data collection is possible through a software, now substituted by a web-based system, developed and distributed by AICE to the HTC to assist patient management. ISS strongly supported the AICE Database and can access to the information sent by the HTC being identified by AICE as the national organisation responsible for the elaboration and diffusion of the inherited bleeding disorders data. Information collected are analysed and validated through a data quality control system aimed to check the quality of data entry and type of information. In case of data not compliant the referent of the Centre is asked to check the information provided for ensuring the consistency and completeness of patient information housed. Since 2007, ISS has activated a specific questionnaire realised on the basis of the therapeutic treatment plans that represent the most reliable tool for monitoring the consumptions12. In fact therapeutic plans establish the products and doses to be used by patients during the year Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s577 Hassan HJ et al and are necessary to receive therapy free of charge by the national public health service. Regimen and products are defined on a case by case and after informed consent and sharing between the specialist and the patient. This direct data flow on treatment product consumption with the Haemophilia Centres allows to monitor the needs/consumptions of plasma-derived and recombinant products necessary for the haemophilia replacement therapy12. Data analysed and elaborated by ISS are published in an annual technical report (ISTISAN Report) distributed to the National and Regional administrators and to the HTC that contributed to data collection. RNCC is also published on the website of the ISS (www.iss.it). Since 2006, the RNCC has been included in the National Statistic System (SISTAN) that monitors the surveys of public interest and it is regularly published on the SISTAN website (www.sistan.it). Moreover RNCC data are disseminated in the national meetings relative to rare diseases, published on international journals and also provided for the enquires of the Italian Health Ministry and Parliament. Results Patient number/Centre, pathology severity, age, gender, treatment regimen and annual product consumption/patient are the main markers utilised in the data analyses. In 2012 the total number of validated patients included in the RNCC was 9,097, in particular 3,696 with HA (46% with severe HA), 744 with HB (37% with severe HB), 2,212 with vWD (4% with the severe type 3), 1,524 with other rare deficiencies (39% factor VII and 24% factor XI deficiencies). In 2012, the Italian prevalence of HA and HB was 6.1/100,000 inhabitants and 1.2/100,000 inhabitants, respectively. The severe HA patients were 1,698 in total; 18% of these was registered as previously or currently positive to inhibitor. The incidence of inhibitor in severe HA patients was about 30% in 0-2 years. The estimated amount of factor VIII utilised in the HA replacement therapy and factor IX for the HB therapy was 450,000,000 of International Units (IU) and 55,000,000 of IU respectively; in both cases 80% was represented by recombinant products. Considerations The Word Federation of Haemophilia (WFH) recommends the development of national patient registries through the collaboration between national patient organisations, healthcare professionals, treatment Centres and ministries of health13. The availability of a pathology specific Registry at national level improves the knowledge of the disease in terms of epidemiology, correlated diseases, care requirements, resources and new therapeutic strategies. The Italian RNCC corresponds to the requirements of the WFH allowing to provide reliable Italian data to international database. There is the need to have a more efficient registration system in order to eliminate any redundancy in patient records and to make data collection in real time. Data collection, in particular on home therapy, requires the primary collaboration of the Patient's Association. The absence of specific national regulation and funding for the improvement of the RNCC is a limit that should be overcome. The Haemophilia Database of the Italian Association of Haemophilia Centres Organisation The Haemophilia Database was developed within the AICE since 2003, in accordance with the main objectives of AICE to prompt optimal health care delivery through the Italian HTC, basic and clinical research and collection of epidemiological data on inherited bleeding disorders14. It is completely doctorrun and it is characterised by a voluntary nature about the contribution in activities of HTC directors, joined in AICE. Data on patients with haemophilia and allied bleeding disorders are regularly collected twice a year. AICE is the owner of the Haemophilia Database. Furthermore AICE has identified the ISS as the national organisation in charge of the analysis and the diffusion of the epidemiological data. Management software is employed by HC directors for the data collection of Haemophilia AICE Database. In 2009 the software has migrated to the web, becoming web-based (EmoWEB) to improve accessibility, maintenance and security of users and data. EmoWeb was also designed to support all the daily activities of HTC and covers all the relevant fields of haemophilia management, in order to use it as computerised medical record. Every 6 months each HTC director authorises patient data extraction through an automated procedure that anonymizes those records. The Haemophilia AICE Database is regularly updated with information on patient demographics, clinical and laboratory phenotypes; after each update an automatic procedure creates local and national hyper textual reports. The local reports are related to patients treated in each HTC. The national report displays all national data collected and discloses the Italian situation of haemophilia and bleeding disorders. All these reports are published in password-protected pages on the AICE website to allow HTC directors to check and validate the local reports; tables with summary data about Italian patients with Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s578 Italian Registries on inherited bleeding disorders inherited bleeding disorders are also published in a public zone of the AICE website (http://www.aiceonline. it/emocard/homeRN.htm). Moreover Haemophilia Registry data are disseminated during the AICE meeting and used for AICE research projects. Data are also provided by the technical reports published at the ISS. Results Database is filled by 53 HTC, distributed in the country. Since 2003 a total of 11,436 patients were collected, 10,444 after duplicate exclusion. In 2012 9,345 are living patients, 40% with HA, 8% with HB, 24% with vWD and 28% with other bleeding disorders. The percentages of severe, moderate, and mild HCV-infected -HA patients are 45%, 37% and 20% respectively. The percentages of severe, moderate, and mild HCV-infected -HB patients are 38%, 27% and 12% respectively. The percentages of HIV infected patients are: 10% of severe, 4% of moderate, 0.5% of mild HA and 15% of severe, 5% of moderate, 0.6% of mild HB. Considerations The Haemophilia AICE Database, monitoring the data transmission from each HTC on patients with haemophilia and other congenital bleeding disorders, allows to check the HTC participation to the Database and to evaluate the homogeneity of the patient haemophilia management at national level. The same guidelines followed by the Centres allow to collect harmonised data useful to address clinical studies. Therefore, the Haemophilia AICE Database represents a tool aimed to the implementation of important retrospective and prospective clinical and scientific studies on specific topics such as cancer, quality of life and mortality of haemophilia patients15-18. The goal of these studies is to better understand some specific aspects on the haemophilia and bleeding disorders management and to provide more focused recommendations for treatment and follow-up. Conclusions The RNMR, the RNCC and the Haemophilia AICE Database monitor inherited bleeding disorders and are already well established, they have many commonalities but many disparities at the same time (Table I). The primary source of data collection for the RNMR and RNCC is different. The data sources of the RNMR are FDC, established by regional law and dedicated to Table I - Comparative data on the bleeding disorders data flow (2012). National Registry for Rare Diseases (RNMR) Institution National Registry of Congenital Coagulopathies (RNCC) Italian Association of Haemophilia Centres (AICE) Database By law Voluntary Voluntary Governmental National Institute Governmental National Institute Scientific Society Local Centres of Reference Regional Registries- National RNMR Local Haemophilia Centres AICE Database - National RNCC Local Haemophilia Centres - AICE Database Rare diseases surveillance Inherited bleeding disorders surveillance and drug consumption monitoring Clinical and scientific studies on inherited bleeding disorders Severe Haemophilia A No Yes Yes Moderate Haemophilia A No Yes Yes Mild Haemophilia A No Yes Yes Total Haemophilia A Yes Yes Yes Severe Haemophilia B No Yes Yes Organisation Data flow Purpose Data collected Moderate Haemophilia B No Yes Yes Mild Haemophilia B No Yes Yes Total Haemophilia B Yes Yes Yes von Willebrand Disease (type 1) No Yes Yes von Willebrand Disease (type 2) No Yes Yes von Willebrand Disease (type 3) No Yes Yes Total von Willebrand Disease Yes Yes Yes Deficiency of other coagulation factors Yes Yes Yes Inherited thrombophilic disorders Yes No No Platelet disorders No Yes Yes Inherited bleeding disorders Yes Yes Yes Drug consumption monitoring No Yes No 11.135 9.097 9.345 Total inherited bleeding disorders Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s579 Hassan HJ et al the management of RD; data for the Haemophilia AICE Database and the RNCC derive from the Italian HTCs, established by regional law and assisting the Italian patients with bleeding disorders. The completeness of the ISS registries is different; in particular the prevalence of HA and HB, estimated by the RNMR, is much lower than that reported in the RNCC. This underreporting probably depends on the RNMR terminology, in fact the most of patients with HA and HB are notified as patients with inherited bleeding disorders, without specifying which bleeding disorder. Furthermore not all FDC follow patients with bleeding disorders and are active in sending the relative data. The epidemiological data about patients with bleeding disorders, collected in the Haemophilia AICE Database and the RNCC, are more homogenous than that collected in the RNMR because the HTC represent the principal data source for both data collection. The RNMR, the RNCC and the Haemophilia AICE Database are not fully interoperable between them because of different patient identification code and terminology codification. Interoperability procedures should be developed in order to obtain data sharing through standard terminology classification and to exchange agreed and harmonised data. The aim of both the ISS registries is patient care and public health oriented. The RNMR is a multi-diseases registry, containing 495 rare diseases; every class of pathology should be further investigated through the institution of specific disease Registry. The RNCC, investigating the inherited bleeding disorders, allows a specific analysis of this group of pathologies and could represent a model for the institution of other disease Registries. The European Commission Communication: "Rare diseases: Europe's challenge", the subsequent Council Recommendation19,20 and the WFH emphasize the strategic importance of Patient Registries and the development of similar specific registries can be beneficial also for the knowledge of other rare pathologies. The AICE Database is managed by the scientific association of Haemophilia Centres and is a research oriented instrument providing data for prospective clinical studies; epidemiological data are shared with the ISS for the progress of the RNCC to which AICE strongly cooperates. Keywords: registries, rare diseases, inherited bleeding disorders, haemophilia. Authorship contribution Hamisa J. Hassan, Massimo Morfini and Domenica Taruscio contributed equally to the paper. Hamisa J. Hassan, Massimo Morfini and Domenica Taruscio are responsible for i) the National Registry of Congenital Coagulopathies, ii) the Haemophilia Database and iii) the National Registry for Rare Diseases, respectively. Hamisa J. Hassan, Massimo Morfini and Domenica Taruscio conceived the review. Francesca Abbonizio, Adele Giampaolo, Yllka Kodra, Emily Oliovecchio and Luciano Vittozzi analysed the data and were involved in writing. The Authors declare no conflicts of interest. References 1) Franchini M, Mannucci PM. Hemophilia A in the third millennium. Blood Reviews 2013; 27: 179-84. 2) Mannucci PM. Treatment of haemophilia: building on strength in the third millennium. Haemophilia 2011; 17: 1-24. 3) Castaman G, Goodeve A, Eikenboom J on behalf of the European Group on von Willebrand disease (EUvWD). Principles of care for the diagnosis and treatment of von Willebrand disease. Haematologica 2013; 98: 667-74. 4) Mannucci PM, Duga S, Peyvandi F. Recessively inherited coagulation disorders. Blood 2004; 104: 1243-52. 5) Decreto18 maggio 2001, n. 279. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124. (GU n. 160 del 12-7-2001Suppl. Ordinario n.180/L). Available at: http://www.iss.it/ binary/cnmr/cont/DM279-2001.1205943575.pdf. Accessed on 15/11/2013. 6) Taruscio D. Il Registro Nazionale e i Registri Regionali/ interregionali delle Malattie Rare. Rapporto anno 2011. (Rapporti ISTISAN 11/20). Roma: Istituto Superiore di Sanità; 2011. Available at: http://www.iss.it/publ/index. php?lang=1&id=2529&tipo=5. Accessed on 15/11/2013. 7) Ghirardini A, Schinaia N, Chiarotti F, et al. Registro Nazionale delle Coagulopatie Congenite in Italia. Rapporto 1990. (Rapporti ISTISAN 91/33). Roma: Istituto Superiore di Sanità; 1991. Available at: http://www.iss.it/publ/index. php?lang=1&id=780&tipo=5. Accessed on 15/11/2013. 8) Ghirardini A, Puopolo M, Mannucci PM, et al. Registro Nazionale dell'Emofilia del Gruppo Italiano Coagulopatie Congenite (GICC): Rapporto 1993. (Rapporti ISTISAN 94/13). Roma: Istituto Superiore di Sanità; 1994. Available at: http://www.iss.it/publ/index.php?lang=1&id=688&tipo=5. Accessed on 15/11/2013. 9) Abbonizio F, Giampaolo A, Arcieri R, et al. Registro Nazionale delle Coagulopatie Congenite. Rapporto 2011. (Rapporti ISTISAN 12/55). Roma: Istituto Superiore di Sanità; 2012. Available at: http://www.iss.it/publ/index. php?lang=1&id=2681&tipo=5. Accessed on 15/11/2013. 10) Abbonizio F, Giampaolo A, Calizzani G, et al. Registro Nazionale delle Coagulopatie Congenite. Rapporto 2008. (Rapporti ISTISAN 10/31). Roma: Istituto Superiore di Sanità; 2010. Available at: http://www.iss.it/publ/index. php?lang=1&id=2439&tipo=5. Accessed on 15/11/2013. 11) Abbonizio F, Giampaolo A, Palmieri S, et al. Registro Nazionale delle Coagulopatie Congenite. Rapporto 2006-2007. (Rapporti ISTISAN 08/46). Roma: Istituto Superiore di Sanità; 2008. Available at: http://www.iss. it/publ/index.php?lang=1&id=2269&tipo=5. Accessed on 15/11/2013. Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s580 Italian Registries on inherited bleeding disorders 12) Giampaolo A, Abbonizio F, Puopolo M, et al. Consumption of clotting factors in severe haemophilia patients undergoing prophylaxis and on-demand treatment in Italy. Transfus Med 2011; 21: 280-4. 13) Evatt BL, Black C, Batorova A, et al. Comprehensive care for haemophilia around the world. Haemophilia 2004; 10: 9-13. 14) Iorio A, Oliovecchio E, Morfini M, et al. Italian Registry of Haemophilia and Allied Disorders. Objectives, methodology and data analysis. Haemophilia 2008, 14: 444–53. 15) Tagliaferri A, Di Perna C, Santoro C, et al. Cancers in patients with hemophilia: a retrospective study from the Italian Association of Hemophilia Centers. J Thromb Haemost 2012; 10: 90-5. 16) Tagliaferri A, Rivolta GF, Iorio A, et al. Mortality and causes of death in Italian persons with haemophilia 1990-2007. Haemophilia 2010; 16: 437-46. 17) Tagariello G, Iorio A, Santagostino E, et al. Comparison of the rates of joint arthroplasty in patients with severe factor VIII and IX deficiency: an index of different clinical severity of the 2 coagulation disorders. Blood 2009; 114: 779-84. 18) Rocca A, Pizzinelli S, Oliovecchio E, et al. Replacement therapy with recombinant factor IX. A multicentre evaluation of current dosing practices in Italy. Blood Transfusion 2010; 9: 60-9. 19) Communication from the Commission to the European Parliament, the Council, the European economic and social committee and the committee of the regions on rare diseases: Europe challenges. Commission of the European Communities. Available at http://ec.europa.eu/health/ph_threats/non_com/ docs/rare_com_en.pdf. Accessed on 15/04/2013. 20) Council Recommendation of 8 June 2009 on an action in the field of rare diseases. The Council of the European Union. Available on line at: http://eur-lex.europa.eu/LexUriServ/ LexUriServ.do?uri=OJ:C:2009:151:0007:0010:EN:PDF. Accessed on 23/08/2013. Correspondence: Hamisa J. Hassan Department of Haematology, Oncology and Molecular Medicine Italian National Institute of Health Viale Regina Elena 299 00161 Rome, Italy e-mail: jane.hassan@iss.it Blood Transfus 2014; 12 Suppl 3: s567-75 DOI 10.2450/2014.0017-14s s581 ORIGINAL ARTICLE Definition of an organisational model for the prevention and reduction of health and social impacts of inherited bleeding disorders Gabriele Calizzani1, Ivana Menichini2,3, Fabio Candura1, Monica Lanzoni1,4, Samantha Profili1, Maria Rita Tamburrini5, Antonio Fortino6, Stefania Vaglio1,7, Giuseppe Marano1, Giuseppina Facco1, Emily Oliovecchio8,9, Massimo Franchini9,10, Antonio Coppola9,11, Romano Arcieri2, Cinzia Bon12, Marco Saia13, Sabina Nuti14, Massimo Morfini9, Giancarlo M. Liumbruno1, Giovanni Di Minno9,11, Giuliano Grazzini1 1 National Blood Centre, National Institute of Health, Rome; 2Italian Federation of Haemophilia Societies (FedEmo), Rome; 3Necstep Studio Associato, Modena; 4IRCCS Ca' Granda Foundation Maggiore Policlinico Hospital, Milan; 5 Blood and Transplant Unit, Ministry of Health, Rome; 6National Institute for Health, Migration and Poverty, Rome; 7 Faculty of Medicine and Psychology, Sapienza University of Rome, Rome; 8Department of Internal Medicine, University of Perugia, Perugia; 9Italian Association of Haemophilia Centres (AICE), Florence; 10Department of Transfusion Medicine and Hematology, Carlo Poma Hospital, Mantua; 11Regional Reference Centre for Coagulation Disorders, Federico II University Hospital, Naples; 12Veneto Region Health Authority, Venice; 13Veneto Region Health Directorate, Venice; 14 Laboratorio Management e Sanità, Istituto di Management, Scuola Superiore Sant'Anna, Pisa, Italy Introduction. Due to the increase in life expectancy, patients with haemophilia and other inherited bleeding disorders are experiencing age-related comorbidities that present new challenges. In order to meet current and emerging needs, a model for healthcare pathways was developed through a project funded by the Italian Ministry of Health. The project aimed to prevent or reduce the social-health burden of the disease and its complications. Material and methods. The National Blood Centre appointed a panel of experts comprising clinicians, patients, National and Regional Health Authority representatives. Following an analysis of the scientific and regulatory references, the panel drafted a technical proposal containing recommendations for Regional Health Authorities, which has been formally submitted to the Ministry of Health. Finally, a set of indicators to monitor haemophilia care provision has been defined. Results. In the technical document, the panel of experts proposed the adoption of health policy recommendations summarised in areas, such as: multidisciplinary integrated approach for optimal healthcare provision; networking and protocols for emergency care; home therapy; registries/databases; replacement therapy supply and distribution; recruitment and training of experts in bleeding disorders. The recommendations became the content of proposal of agreement between the Government and the Regions. Monitoring and evaluation of haemophilia care through the set of established indicators was partially performed due to limited available data. Conclusions. The project provided recommendations for the clinical and organisational management of patient with haemophilia. A particular concern was given to those areas that play a critical role in the comorbidities and complications prevention. Recommendations are expected to harmonise healthcare care delivery across regional networks and building the foundation for the national haemophilia network. Keywords: haemophilia care, clinical pathway, performance indicators. Introduction Inherited bleeding disorders (IBDs) are rare diseases characterised by hereditary abnormalities of proteins necessary for blood clotting. Among IBDs, the best known are haemophilia A, caused by a deficiency of coagulation factor VIII (FVIII), haemophilia B, also known as Christmas disease, caused by a deficiency of factor IX (FIX), and von Willebrand disease (vWD), caused by a defect or deficiency of von Willebrand factor1. In persons with haemophilia, although the bleeding phenotype is recognised to be heterogeneous and affected by many genetic and environmental factors, the severity of clinical symptoms is correlated to the residual endogenous FVIII/FIX concentrations: on the basis of plasma factor levels below 1 IU/dL, or between 1-5 IU/dL, or between 5-40 IU/dL haemophilia patients are classified respectively as severe, moderate, and mild2. Thus, patients with severe haemophilia bleed spontaneously or after trivial trauma. The most frequently reported bleeding is haemarthrosis, particularly into joints such as ankle, knee and elbow. Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s582 © SIMTI Servizi Srl Model for prevention and reduction of impacts of haemophilia Recurrent episodes may lead to progressive joint morbidity (haemophilic arthropathy) associated with chronic pain and disability and often requiring orthopaedic surgery and joint replacement. Muscles may be also affected. Other less common symptoms are bleedings involving soft tissues, mucosae and parenchyma including lifethreatening intracranial, neck-throat and gastro-intestinal haemorrhages. Patients with moderate haemophilia experience excessive bleeding after relatively minor trauma while those with mild haemophilia experience excessive bleeding in the large majority of cases only in response to surgery, other invasive procedures or major injuries3. Bleeding phenotype is more heterogeneous and not easily predictable by laboratory data in vWD and, particularly, in rarer IBDs. Among the clinical complications of haemophilia, the most dramatic is presently the appearance of inhibitors against the therapeutically administered factors, which render the replacement therapy less effective. As a consequence, an increased bleeding-related morbidity and a drastic reduction in the quality of life due to the physical disability caused by hemophilic arthropathy is reported in inhibitor patients4. According to the Haemophilia Registry of the Italian Association of Haemophilia Centres (AICE, Associazione Italiana Centri Emofilia)5, the total number of patients suffering from IBDs in Italy was 9,345 in the first semester of 2013. Of these, 1,746 had severe haemophilia A, 293 had severe haemophilia B, and the remainder had less severe or rarer defects. The number of patients suffering from a severe form of haemophilia A or B, who have an inhibitor history, are 345 and 8, respectively. Of these, 181 and 6, respectively (10.4 and 2% of the population with a severe form of haemophilia) have currently detectable inhibitors. During the 1980s a number of patients were infected with human immunodeficiency virus (HIV) and hepatitis C virus (HCV), as a complication of treatment using non-viral inactivated plasma derived medicinal products. These infections and the related complications represented the main cause of death in persons with haemophilia (PWH) over the last three decades 6. Currently, 278 (3.1%) HIV-positive, 1,647 (17.9%) HCV-positive, and 239 HIV-HCV co-infected (2.6%) living patients suffering from IBDs are registered in Italy. Nonetheless, life expectancy for PWH has considerably increased in recent decades as a direct result of greater and more widespread factor availability of efficacious and safe both plasma-derived and recombinant factor products6. This is confirmed through regular monitoring of more than 30,000 patients with IBDs via the European Haemophilia Safety Surveillance (EUHASS) system7. In Italy, the analysis of death rate trends in the haemophilic population in the period 1980-2007 showed a significant reduction in mortality over time. In 2007, life expectancy was comparable to that of the general male population, excluding the effects on mortality related to infection with HIV/HCV. Currently, the main cause of death is bleeding, thanks to the reduction of the impact of HIV/HCV-related mortality8. Thus, as a consequence of the increased lifeexpectancy, the emerging population of middle-aged and older PWH is experiencing age-related comorbidities such as cardiovascular diseases, metabolic syndrome, renal diseases, sexuality issues, malignancies, and neurologic problems, which have rarely been seen in this group of patients in the past. These issues represent new challenges for physicians working in haemophilia centres (HCs), that are adding to the clinical complications (arthropathy, chronic infections, psychosocial problems) routinely managed in the comprehensive care of these patients9. In order to satisfy emerging needs, HCs must rely on specific, specialised clinical skills and resource planning in order to address important organisational challenges effectively and efficiently. Timely and effective interventions for prevention and clinical management of the disease can result from the definition and implementation of disease-specific clinical pathways for patients with IBDs. Moreover, improvements in the efficiency and sustainability of healthcare services provision are demanded by the progressive reduction of the health budget witnessed in recent years. The objective of this paper is to describe a model for healthcare pathways for the management of patients with IBDs; this model was developed by a group of experts through a three-year project funded by the National Centre for Disease Prevention and Control (CCM) of the Italian Ministry of Health in 2010. The project aimed at the prevention and reduction of the social-health burden of the disease and its complications. Materials and methods The project, coordinated by the Italian National Blood Centre (NBC, www.centronazionalesangue. it), involved the Italian Association of Haemophilia Centres (AICE, www.aiceonline.it), the Federation of Haemophilia Patient Associations (FedEmo, www. fedemo.it), the Veneto Region (Regional Agency of Health - ARSS, http://www2.arssveneto.it/) representing the Conference of the Italian Regions, and the Laboratorio Management e Sanità, Istituto di Management, Scuola Superiore Sant'Anna, Pisa (SSSUP, http://www. meslab.sssup.it/en/) as partners. Available scientific evidence was reviewed to identify best practice in the clinical and organisational management of haemophilia patients, including clinical pathways. Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s583 Calizzani G et al In addition, an analysis of the current service provision by haemophilia services was carried out. The analysis used the results of qualitative and quantitative surveys carried out by FedEmo10, the pilot study conducted by SSSUP11 and interviews of experts from the Project Research Units and to a delegation of Regional Health Authorities (RHA). Regulatory frameworks in place in Italy and policies adopted for the management of rare and chronic diseases were also taken in consideration. In this way, all the available scientific and regulatory references were identified, focusing, in particular, on organisational requirements included in the Professional Accreditation Model developed by AICE and described in detail by Calizzani et al. and by Mannucci and co-workers12,13. Finally, a set of indicators to monitor HC activities was identified. These indicators were used for performing regional comparisons, in terms of numbers of patients given access and treated, complexity of diseases treated, appropriateness of clinical practices, and timely access of patients with IBDs to the services of a centre11. The analysis carried out through the application of these indicators is not the main objective of this manuscript. Results In order to tackle the most critical issues that have a negative effect on patient healthcare management and to foster the provision of optimal healthcare to PWH, the panel of experts, through the technical document produced, proposed the adoption of the following policies. a) Multidisciplinary integrated approach for optimal healthcare provision According to a patient survey carried out by FedEmo10, the availability and quality of care vary widely across Italian Regions, so that 52% of patients must still travel long distances (101-500 km) for access to services. In particular, among patients living in Southern regions and islands (22%) travel more than 500 km, and 40% had to change their residence in order to attend a HC with an optimal level of care. These data are partially confirmed by a recent study conducted within the framework of the CCM project by the Research Unit SSSUP11. According to the results of the survey, more than 15% of patients affected by a severe form of haemophilia are treated by a HC outside the Region in which the patient lives. At this stage, it is unclear how much of this phenomenon can be explained by the lack or poor quality of haemophilia services, by referrals to more specialised centres that play a tertiary role, or simply by the patient's choice. However, the study shows a wide variation within and among Regions in terms of volumes of activity and organisational models of care11. In order to address the differences in haemophilia services provision, an integrated approach to the healthcare pathway of patients with IBDs should be developed. The Regions should define an organisational model of haemophilia healthcare capable to ensuring integrated services and networking between HCs, both adult and paediatric ones, and specialised units (e.g. orthopaedics, physical and rehabilitation therapies, emergency department, laboratory diagnostics, dentistry, hepatology-infectious diseases, medical genetics). In some cases, this organisation will require specific interregional agreements. In particular, Regions should adopt the following policies. Regions and Autonomous Provinces should ensure different levels of complexity of healthcare functions through IBD accredited HCs 14- 16, which provide services directly and / or indirectly through facilities / units functionally related to them. Standards for HCs have been described in detail elsewhere15. Healthcare pathways should include pre- and post-natal genetic diagnosis and genetic counselling, in accordance with the current legislative framework on rare diseases (RD) management. Finally, Regions should identify laboratories that can ensure the provision of coagulation tests for the diagnosis, treatment, and follow-up of PWH, as well as for 24-hour emergency services. 15 b) Networking and protocols for emergency care Although many PWH and their families are trained in self-administered replacement coagulation factors therapies, they could, however, need to attend emergency departments in cases of unexpected bleeding due to trauma, physical effort, or even following spontaneous bleeding, regardless of the distance to the emergency department. Appropriate and timely triage of patients, as well as the interaction between the emergency staff and the expert of the HC to ensure the most appropriate management and timely administration of coagulation factors has been proven to be crucial in order to prevent immediate, sometimes life-threatening, and long-term complications17. In order to deal with these issues, the panel of experts proposed to the Regions to define, with the support of inter-regional agreements, the organisation of the HC network to ensure a 24-hour management of haemorrhagic emergencies and the availability of phone consultations with experts in IBDs. In addition, Regions are prompted to share protocols between their emergency units and their HC networks to achieve an effective and proper emergency management of patients within the regional territory. These protocols should contain guidelines on the assignment of proper triage codes and emergency treatment procedures. Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s584 Model for prevention and reduction of impacts of haemophilia c) Home therapy The benefits of home therapy have been widely proven18. Home therapy allows the administration of clotting factor concentrates as soon as bleeding occurs, thus decreasing the morbidity because of more rapid recovery from bleeding episodes, and avoiding longterm complications. Home treatment also allows patients to benefit from prophylactic treatment. Early treatment results in the use of less factor, reduces the frequency of accesses to HCs and provide patients and their families with better quality of life8. In Italy, home treatment is a common practice, but specific regulations on self-infusion have been developed and adopted in only 60% of Italian Regions10. Regions should be invited to adopt policies, including legislative provisions, based on the most recent scientific and technological evidence and patients' needs, in order to provide PWH with the benefits of home treatment. These policies should include the organisation of training and re-training of patients and their caregivers, including nurses. d) Registries/databases As part of significant measures addressed to prevention of RD, disease-specific registries or registries for groups of rare diseases are an effective way to assess health care needs as well as to develop research in several areas, including epidemiology and pharmacovigilance. In many cases, registries are the only existing source of scientific/clinical and epidemiological information on RD19. In particular, in Italy, three well established registries monitoring IBDs are operating: the Italian National Registry for RD (NRRD)20,21, the National Registry of Congenital Coagulopathies (NRCC) at the National Institute of Health (ISS, Istituto Superiore di Sanità)22 and the Hemophilia Registry run by AICE23. Although they share many features, they significantly differ in terms of objectives, data collection methods, data sets and last, but not least, resulting epidemiological data24. Therefore, interoperability among the three registries should be promoted. Regions should strengthen IBD data collection and surveillance activities at the regional and inter-regional levels. e) Replacement therapy supply and distribution The importance of making factor concentrates available to meet health needs is recognised by international organisations and their strategic relevance is confirmed by their inclusion in the WHO Essential Medicines List25. According to the data analysed by NBC26, in 2011 and 2012, a standardised national demand for FVIII of 6.5 and 7.4 international units (I.U.) per capita, respectively, was met. The comparison with European and extra-European Countries with similar standards for the treatment of haemophilia patients showed a per capita national utilisation which seems to be adequate in term of supply and in line with those internationally described27. However, there is wide variability among Italian Regions in the demand for clotting factors concentrates (ranging from 2.1 in Aosta Valley to 11.5 I.U. per capita in Calabria and Latium Regions), and consequently in the costs sustained by the NHS. Such differences need to be explained and addressed. A variety of plasma-derived and recombinant concentrates are licensed in Italy for the treatment of haemophilia and other IBDs25. As far as FVIII is concerned, toll fractionation products account for around 60% of the total demand for plasma-derived concentrates. The observed regional per capita expenditure differs among Regions showing the influence of both purchase volumes and mean purchase prices per unit. Consequently, forms of centralised purchases should be envisaged28. The evolution of the Italian regulatory framework related in particular to the opening of the toll fractionation market29 will certainly introduce new elements to the Regions that could presumably benefit from stronger competition in terms of qualitative and quantitative supply of plasma-derived products. These strategies are strongly needed even in the supply of recombinant products, that are currently used by the majority of Italian patients. In order to ensure the continuity of care in any treatment regimen and to ensure constant monitoring of data related to product demand, consumption and appropriateness, Regions should plan the supply of medicinal products for the treatment of IBDs together with the Regional Blood Centres. f) Recruitment and training of experts in bleeding disorders The training of professionals and the development and exchange of best practices and education are high priority issues and are the main determinants for developing and maintaining adequate diagnostic and therapeutic facilities and a high quality of care. Concern has been expressed by several authors in the past regarding the risk of a dramatic fall off in the number of young physicians interested in a clinical and research career in bleeding disorders30,31. In order to address this risk, the European Association for Haemophilia and Allied Disorders was established32, and the European Curriculum for Thrombosis and Haemostasis produced33. According to the European recommendation in the field of RD34, the need for training does not refer only to clinical expertise, but also to the ability to communicate with patients and their families. Despite the efforts made by professional bodies, including AICE, the difficulties for many Italian young Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s585 Calizzani G et al professionals to be permanently recruited by HCs emerged, so that some of them were forced to opt out such career. The formal recognition of the role of HCs in training of professionals, through an institutional accreditation system to be implemented by Italian Regions, should ensure actions taken to prevent such occurrences16. Regions should adopt any further possible measure to ensure the availability of expertise appropriate to the clinical management of PWH. HCs should identify, on the other hand, and formalise the skills and professional qualifications required for personnel performing activities critical to quality of patient care, also implementing plans in order to guarantee their adequate training before they start working35. g) Monitoring and evaluation A set of performance indicators was defined using data from the AICE Registry. They include: number and case-mix of patients treated per HC, patients inflow/outflow, number of accesses to HCs for the following possible reasons: check-up, on demand or prophylactic treatment, emergency, volumes of surgeries (especially orthopaedic and prosthetic operations), monitoring timing (follow-up, emergency accesses), variation in the clinical and pharmaceutical treatment of haemorrhagic events (haematoma, haemarthrosis) by patients case-mix, outcome indicators (quality of life, adverse events related to treatment, adjusted mortality per cause)11. However, an adequate measurement of HCs and Regional Network outcomes and related benchmarking activities was not carried out because of the limited data availability. Discussion For the model of haemophilia care delivered by the project, a number of strengths and weaknesses can be identified. A key strength was the fact that the model was the result of an inclusive process involving all key stakeholders: patients, physicians and regional as well as national decision makers. Therefore different expectations were met, facilitating the implementation of the model. The development of the model was influenced by principles and guidance from international and national organisations12,13,35,36 but it was also informed by an accurate knowledge of the context, provided by the stakeholders involved. The project partners focused their attention on the most critical areas of the current provision of haemophilia care, in terms of the quality of services with ultimate impact on patient outcomes. Some of the recommendations emerging from the project have a direct impact, in the short term, on the prevention and management of complications and include the Multidisciplinary integrated approach for optimal healthcare provision, Networking and protocols for emergency care, and Home therapy. Others, such as Registries/databases, Replacement therapy supply and distribution, Recruitment and training of experts in bleeding disorders - have an indirect impact on the quality of healthcare delivery. However, the latter could play a critical role in disease management, guiding service provision in the medium to-long-term period or providing essential information for disease surveillance. Some weaknesses were also identified. The project supported the development of recommendations that still have to be implemented in many of the Italian Regions, before being adequately assessed. In addition, some may be considered to be too generic and might be seen more as principles of care than organisational provisions. In fact, the project partners were limited in their recommendations by the current nature of relationships between central State and Regions.The Regions have, following the devolution process, a complete organisational autonomy in the field of healthcare. The authors envisage that the outputs and outcomes of the project could have significant impacts and consequences in terms of local health and social care and in terms of management of PWH and other IBDs. It is expected that a national network for HCs will be put in place through the harmonisation of healthcare delivery of different haemophilia regional networks. The model of care aims to adequately meet some basic needs, such as: - diagnosis and early treatment; - organisational and therapeutic appropriateness; - assistance in emergency; - social and health care for PWH and other IBDs, also in the context of serious co-morbidities, such as cancer and multifactorial diseases (cardiovascular diseases, diabetes, osteoporosis, etc.); - prevention and reduction of the social health burden of the disease and its complications (inhibitors, joint damage, co-morbidity); - provision of information and training of patients and their families, to promote social inclusion and home treatment, namely the model of care that is most effective for improving the quality of life and extending the life expectancy of PWH and other IBDs. Despite significant limitations posed by the available data, further studies are required in order to assess if the observed variability can be correlated with the degree of specialisation of network centres. The difficulty of applying methodologies of analysis traditionally used to measure common health interventions or procedures to low prevalence diseases such as IBDs are evident. However, regarding patient flows, there are still significant margins to redefine the network in a more integrated and homogeneous way and to improve the efficiency and efficacy of the model of care. In this context, it is worthwhile to underline the need to Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s586 Model for prevention and reduction of impacts of haemophilia strengthen the quality of data collection by existing registers. In fact, at this time the registers and information flows do not support reliable and consistent application of the majority of the performance indicators identified by the panel of experts, including outcome measures. Moreover, these limitations hinder benchmarking activities and comparisons between Regions and HCs. In designing a sustainable and efficacious network for rare disorders, such as IBDs, a continuous trade-off between the need to provide services close to the home of the patient and the need to provide services with a high level of expertise and experience present an inevitable conflict. If on the one hand, low volumes do not justify the presence of a comprehensive HC on the territory, on the other hand basic services are necessary to guarantee timeliness of intervention. 5) 6) 7) 8) 9) 10) 11) Conclusion The CCM project defines a model for healthcare pathways for the management of patient with IBDs aimed at the prevention and reduction of the socialhealth burden of the disease and its complications. Such a model provides Italian Regions with recommendations for the arrangement of care for PWH based on the most recent scientific evidence and current best practice. However, the project monitoring and evaluation require an improvement in data collected by haemophilia registries and information matching with other health information flows. Further evidence coming from a wider implementation of the recommendations across Italian Regions will show if the model is successful in achieving the expected outcome. 12) 13) 14) 15) 16) 17) Acknowledgements The project Model of Disease Management of Patient with Congenital Bleeding Disorders Aimed at the Prevention and Reduction of both Health and Social Impact of the Disease and its Complications is a three-year project funded by the national Centre for Disease Prevention and Control of the Italian Ministry of Health. The Authors declare no conflicts of interest. 18) 19) 20) 21) References 1) 2) 3) 4) Mannucci PM, Tuddenham E. The Hemophilias - From Royal Genes to Gene Therapy. N Engl J Med 2001; 344: 1773-9. White GC, Rosendaal F, Aledort LM, et al. Definitions in hemophilia. Recommendation of the scientific subcommittee on factor VIII and factor IX of the scientific and standardization committee of the International Society on Thrombosis and Haemostasis. Thromb Haemost 2001; 85: 560. Morfini M, Coppola A, Franchini M, Di Minno G. Clinical use of factor VIII and factor IX concentrates. Blood Transfus 2013; 11 (Suppl 4): s55-63. Morfini M, Haya S, Tagariello G, et al. European study on orthopaedic status of haemophilia patients with inhibitors. Haemophilia 2007; 13: 606-12. 22) 23) 24) The Hemophilia Registry of the Italian Association of Hemophilia Centres. Available at: http://www.aiceonline.it/ emocard/homeRN.htm. Accessed on 15/01/2013. Mannucci PM, Franchini M. Present and future challenges in the treatment of haemophilia: a clinician's perspective, Blood Transfus 2013; 11 (Suppl 4): s77-81. Makris M, Calizzani G, Fischer K, et al. EUHASS: The European Haemophilia Safety Surveillance system. Thrombosis Research 2011; 127 (Suppl 2): S22-5. Tagliaferri A, Rivolta GF, Iorio A, et al. Mortality and causes of death in Italian persons with haemophilia, 1990-2007. Haemophilia. 2010 May; 16: 437-46. Coppola A, Santoro C, Franchini M et al, Emerging issues on comprehensive hemophilia care: preventing, identifying, and monitoring age-related comorbidities. Semin Thromb Hemost. 2013; 39: 794-802. Arcieri R, Molinari AC, Farace S, et al. Uncovered needs in the management of inherited bleeding disorders'. Blood Transfus 2014; 12 (Suppl 3): s563-6. Nuti S. La sostenibilità del modello di cura. Available at http://www.centronazionalesangue.it/sites/default/files/ nuti_la_sostenibilita_del_modello_di_cura.pdf. Accessed on 23/02/2014. Calizzani G, Vaglio S, Arcieri R, et al. Models for institutional and professional accreditation of haemophilia centres in Italy. Haemophilia 2013; 19: e248-55. Mannucci PM, Menichini I. A certification/accreditation model for hemophilia centers in Italy. Blood Transf Decreto Ministeriale 18 Maggio 2001, n. 279. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124. Gazzetta Ufficiale - Serie Generale n. 160, 12 luglio 2001. Suppl. Ord. n. 180/L. Calizzani G, Candura F, Menichini I, et al. The Italian Institutional Accreditation Model for Haemophilia Centres. Blood Transfus 2014; 12 (Suppl 3): s510-4. Fortino A, Di Stanislao F. Institutional accreditation of healthcare services in Italy: the long road to quality. Blood Transfus 2014; 12 (Suppl 3): 551-3. Fowler H, Lacey R, Keaney J, et al. Emergency and out of hours care of patients with inherited bleeding disorders. Haemophilia 2012; 18: e126-31. Colvin BT, Astermak J, Fischer K, et al. European principles of haemophilia care. Haemophilia 2008; 14: 361-74. Recommendations for the Development of National Plans for Rare Diseases - Guidance Document. Available at: http:// www.europlanproject.eu/_newsite_986989/Resources/ docs/2008-2011_2.EuroplanRecommendations.pdf. Accessed on 15/01/2014 Taruscio D, Kodra Y, Ferrari G, et al. The Italian National Rare Diseases Registry. Blood Transfus 2014; 12 (Suppl 3): 606-13. Taruscio D (Ed.). Il Registro Nazionale e i Registri Regionali/ interregionali delle malattie rare. Rapporto anno 2011. Roma: Istituto Superiore di Sanità; 2011 (Rapporti ISTISAN 11/20). Available at: http://www.iss.it/binary/cnmr/cont/ISTISAN_ RNMR_2011.pdf. Accessed on 15/01/2014. Abbonizio F, Gianpaolo A, Arcieri R, Hassan HJ on behalf of the Italian Association of Haemophilia Centres. Registro Nazionale Coagulopatie Congenite. Rapporto 2011. Rapporti ISTISAN 12/55. Iorio A, Oliovecchio E, Morfini M, Mannucci PM on behalf of the Association of Italian Hemophilia Centres Directors. Italian Registry of Haemophilia and Allied Disorders. Objectives, methodology and data analysis. Haemophilia 2008; 14: 444-53. Hassan HJ, Morfini M, Taruscio D, et al. Current Status of Italian Registries on inherited bleeding disorders. Blood Transfus 2014; 12 (Suppl 3): s576-75. Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s587 Calizzani G et al 25) WHO Model List of Essential Medicines. 18th list (April 2013). World Health Organization. Available at: http://www. who.int/medicines/publications/essentialmedicines/18th_ EML_Final_web_8Jul13.pdf. Accessed on 15/01/2014 26) Lanzoni M, Biffoli C, Candura F, et al. Plasma-derived medicinal products in Italy: information sources and flows. Blood Transfus 2013; 11 (Suppl 4): s13-7 27) Calizzani G, Profili S, Candura F, et al. The demand for factor VIII and for factor IX in Italy and the toll fractionation product surplus management. Blood Transfus 2013; 11 (Suppl 4): s64-76. 28) Lanzoni M, Candura F, Calizzani G, et al. Public expenditure for plasma-derived and recombinant medicinal products in Italy. Blood Transfus 2013; 11 (Suppl 4): s110-7. 29) Decreto del Ministro della Salute 12 aprile 2012 "Modalità per la presentazione e valutazione delle istanze volte ad ottenere l'inserimento tra i centri e le aziende di produzione di medicinali emoderivati autorizzati alla stipula delle convenzioni con le Regioni e le Province Autonome per la lavorazione del plasma raccolto sul territorio nazionale". Available at: http://www.centronazionalesangue.it/sites/ default/files/dd.mm_._12.04.2012_plasma_gu_n._147_ del_26.06.2012_.pdf. Accessed on 15/01/2014. 30) Mannucci PM, Roberts HR. Uncertain times for research on hemophilia and allied disorders .J Thromb Haemost 2005; 3: 423. 31) Vermylen J. More on: uncertain times for research on hemophilia and allied disorders. J Thromb Haemost 2005; 3: 1547. 32) Ludlam CA, Mannucci PM on behalf of the Interdisciplinary Working Group. Proposal to establish a European Association for Hemophilia and Allied Disorders. J Thromb Haemost 2006; 4: 2270-1. 33) Astermark, J, Negrier C, Hermans C, et al. European curriculum for thrombosis and haemostasis. Haemophilia 2009; 15: 337-44. 34) European Council. Recommendation of 8 June 2009 on European action in the field of rare diseases. Official Journal C151: 7-10. Available at: http://eur-lex.europa.eu/LexUriServ/ LexUriServ.do?uri=OJ:C:2009:151:0007:0010:EN:PDF. Accessed on 21/01/2014 35) European Haemophilia Network - EUHANET. European guidelines for the certification of Haemophilia Centres. Available at http://www.euhanet.org/docs/Euhanet-European_guidelines _for_the_certification_of_Haemophilia_Centres_2013.pdf. Accessed on 15/01/2014. 36) European Union Committee of Experts on Rare Diseases (EUCERD). Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States (24 October 2011). Available at: http://www.eucerd.eu/upload/file/ EUCERDRecommendationCE.pdf. Accessed on 18/02/2014. Correspondence: Gabriele Calizzani Italian National Blood Centre Via Giano della Bella 27 00162 Rome, Italy e-mail: areaplasma.cns@iss.it Blood Transfus 2014; 12 Suppl 3: s582-8 DOI 10.2450/2014.0087-14s s588 REGIONAL, NATIONAL AND EUROPEAN ACTIONS IN THE FIELD OF RARE DISEASES Blood Transfus 2014; 12 Suppl 3 © SIMTI Servizi Srl REVIEW The Italian National Centre for Rare Diseases: where research and public health translate into action Domenica Taruscio, Linda Agresta, Annalisa Amato, Giuseppe Bernardo, Luana Bernardo, Francesca Braguti, Pietro Carbone, Claudio Carta, Marina Ceccarini, Federica Censi, Simona Coppola, Patrizia Crialese, Marta De Santis, Stefano Diemoz, Carlo Donati, Sabina Gainotti, Gianluca Ferrari, Giovanna Floridia, Claudio Frank, Rosa Giuseppa Frazzica, Amalia E. Gentile, Orietta Granata, Yllka Kodra, Manuela Latrofa, Paola Laricchiuta, Armando Magrelli, Cristina Morciano, Agata Polizzi, Stefania Razeto, Marco Salvatore, Antonella Sanseverino, Daniele Savini, Paola Torreri, Fabrizio Tosto, Flavia Villani, Giorgio Vincenti, Luciano Vittozzi Italian National Centre for Rare Diseases, National Institute of Health, Rome, Italy Introduction The Italian National Centre for Rare Diseases (CNMR) is the result of a strategic approach, which the National Institute of Health (ISS) has been developing for more than 10 years, to deal with the public health challenges associated with rare diseases (RDs). The CNMR was formally established within the ISS in 20081. Its mission is to promote and develop experimental research and public health actions, as well as to provide technical expertise and information on RDs and orphan drugs, for the prevention, treatment and surveillance of these diseases. It is also the national focal point for information and communication for patients suffering from one of several thousand RDs, and for their families, collaborating with the national organisations of patients suffering from RDs. The Centre employs a wide range of scientific and technical expertise from various fields (medicine, genetics, molecular biology, epidemiology, public health, psychology, sociology etc.) and holds a network of national and international collaborations, which allow the development of a sound and integrated approach to RDs. The CNMR provides expert advice to the Italian Ministry of Health (MOH), to the National Health Council, to the National Health Service (NHS), and collaborates with the Regions, which are responsible for the provision of health services in the Italian devolved health system. Expert advice on RDs is also provided at EU and at international level. Since its establishment, the Centre has developed into a lively and propulsive hub for experimental research, public health, information, communication and training on RDs in Italy, and for patient empowerment. In addition, it has contributed to networks and scientific boards at national, European and international level and has implemented a number of strategic projects on RDs. The Centre is in continuous evolution in order to follow closely the pace of science and research, the emerging needs of patients, the solicitations of policy makers, and the demands of the health system. The Italian National Centre for Rare Diseases European and national frame of reference Before introducing the Centre's present configuration and its activities in detail, it is worthwhile to clarify some general issues concerning RDs and the institutions responsible for RD policy, programmes and actions at the European and at the National level, which provide the foundations for the CNMR work. The Centre maintains relations with them as well as with other qualified national, European and international institutions for the realisation of its activities in the field of RDs. General considerations on rare diseases RDs are characterised by low prevalence (by European Union (EU) definition less than 5/10,000 in the general population) but represent a considerable public health burden due to their high number and to their complex management. According to the European Commission2, the number of existing RDs is estimated at between 7,000 and 8,000, affecting, altogether, 6-8% of the general population. RDs are distinguished by specific clinical and etiopathogenetic characteristics, but their social and health burden share a number of common features. Most of them set out at birth or during infancy, while the rest appear in adulthood. RDs are chronic, multisystem conditions often associated with reduced life expectancy and a relevant mortality rate in childhood, a severe disabling course, high medical expenses and poor quality of life. Their low prevalence rate is the main cause of a poor awareness among health care professionals and often of inadequate levels of care expertise. These can result in delayed diagnosis, misdiagnosis or even un-diagnosis, difficulties in assessing and adopting the appropriate disease management, and in problems related to Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s © SIMTI Servizi Srl s591 Taruscio D et al the psychological and economic impact on patients and their families. In addition, the limited market represented by the single conditions does not make the development of new drugs and treatments attractive to the pharmaceutical industry. As a consequence, orphan drugs are expensive and seldom available; furthermore, their efficacy and safety usually cannot be thoroughly assessed, due to the lack of a large patient population. The Italian legislative support for rare diseases Since 1998, RDs have been recognised as a health priority in each of the 3-year Italian national health plans, though a national plan/strategy for RDs has not yet been formalised by the MOH. Meanwhile, a coordinated and comprehensive framework of actions was defined by Ministerial Decree (D.M.) n. 279/20013, which established a national network of selected clinical centres for prevention, surveillance, diagnosis and treatment of RDs, a National Registry for RDs (RNMR), and defined the exemptions for the costs of medical care for a number of RDs. Accordingly, disease related services are free for citizens affected by a RD in the list (see Annex 1 D.M. n. 279/2001). A major shortcoming is that not all RDs and groups of diseases are included in the inventory and that it is not regularly updated, although a revision is expected in the near future. Since 2001, Regions have established regional registries, centres for the diagnosis and treatment of RD patients and regional coordination centres, in order to manage the activities, including the exchange of information among centres and to provide expertise and data to the regional RD registries. Regional registries send the epidemiological data to the RNMR, established at the CNMR in 2001, in accordance with Article 3 of the D.M. n. 279/2001. The RNMR is supported by public funds; it is web-based, in compliance with the legal and ethical requirements, and it is a populationbased registry, although the regional coverage is still heterogeneous. The RNMR collects the data ("common data set") coming from the regional registries and it is the tool for epidemiological surveillance of RDs and for the national and regional planning of RD measures. The European framework for the Italian National Centre for Rare Diseases activities The European Union and the Council of the European Union The RDs gained political concern at the EU level in the early 1990s. In fact, in November 1993, the European Commission (EC) published the "Commission communication on the framework for action in the field of public health" (1993)4, defining the framework for action by the Community and describing the role of the Community Institutions and the Member States (MS). After this publication, the Commission opened a wide consultation in the Union on public health issues. In December 1993 the Commission invited experts to submit a proposal describing how they would seek to formulate draft policy proposals in some of the areas indicated in the framework document. In consultation with the Commission, five priority areas were identified, among them also "An EU programme for management of rare diseases". Subsequently, four key policy documents have been emanated by the EU and these have paved the way to current RDs developments in Europe; the CNMR has aligned to it. Following are the cited documents. a. The Orphan Medicinal Product Regulation5 This text defines the criteria for orphan designation in the EU and described the incentives to encourage the research, development and marketing of medicines to treat, prevent or diagnose RDs. b. The Commission Communication on Rare Diseases: Europe's challenge2 This document, which was adopted on 11 November 2008, proposes an overall strategy to support MS in diagnosing, treating and caring for RD patients in Europe. This Communication focuses on three main areas: i) improving recognition and visibility of RDs, ii) supporting policies on RDs in MS for a coherent overall strategy, and iii) developing cooperation, coordination and regulation for RDs at EU level. c. The Council Recommendation on an action in the field of RDs6 This document was adopted on 8 June 2009 and comprises twenty recommendations gathered into seven main areas. The seven themes are: plans and strategies in the field of RDs; adequate definition, codification and inventorying of RDs; research on RDs; centres of expertise and European reference networks; gathering the expertise on RDs at European level; empowerment of patient organisations; sustainability. d. Directive 2011/24/EU on the application of patients' rights in cross-border healthcare7 This Directive was approved on 28 February 2011 and is particularly important for RD patients, because of scarce and scattered resources for diagnosis and care of these disorders. The Directive is meant to facilitate the access of EU citizens to cross-border health care and to encourage the cooperation between EU Member States in the field of health. The European Union Committee of Experts on Rare Diseases The European Union Committee of Experts on Rare Diseases (EUCERD) was formally established by Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s592 Italian National Centre Rare Diseases: research and public health the European Commission Decision8 on 30 November 2009, replacing the European Commission's Rare Diseases Task Force (RDTF). Its mission is to assist the EC in the cooperation and consultation efforts with the specialised bodies in the MS, the relevant European authorities dealing with research and public health action and other relevant stakeholders operating in the field of RDs. Recently, the EUCERD has been replaced by the Commission Expert Group on Rare Diseases9. The CNMR participated regularly to the RDTF and EUCERD meetings, and will continue to take part to the activities of the newly established Commission Expert Group on Rare Diseases. The role of patient organisations in the Italian National Centre for Rare Diseases work National, European and international patient organisations, representing the voice of the RDs community, play a key role in the activities carried out by the CNMR as highlighted in the following sections. The Italian organisations of patients with rare diseases The role of patient organisations in the field of RDs is crucial. Driven by the need to share difficulties and problems, and by a desire to see their rights recognised, they encourage targeted policies, research and specific interventions for health and social care. In recent years, much of the progress in inter-institutional relations and between institutions and patients are attributable to the efforts of these organisations. Their work comprises a body of knowledge complementary to that of the doctor. For this reason, it becomes increasingly important to have a constructive and cooperative relationship between patients and social and health professionals. This collaboration allows the former to reach such a level of empowerment that enables them to take an active part in the decision making processes that affect them, and the latter to make strides in research and take effective charge of the patients, improving their quality of life. Of the several patient organisations present in Italy, some have chosen to carry on their battle individually, others have opted to join umbrella organisations at national and international level. In Italy there are currently three major leagues: - the Italian Federation for Rare Diseases - UNIAMO10, connected to the European Organisation for Rare Diseases - EURORDIS11; - the National Council for RDs12; - the Italian Movement for Rare Patients (MIR)13. The European Rare Diseases Organisation The European Rare Diseases Organisation (EURORDIS) is a non-governmental patient-driven alliance of patient organisations and individuals active in the field of RDs. It was founded in 1997 for the promotion of research on RDs and the commercial development of orphan drugs. EURORDIS is dedicated to improving the quality of life of all people living with RDs in Europe. It represents more than 606 RDs organisations in 56 different countries (of which 25 are EU MS), covering more than 4,000 RDs11. The CNMR works closely with EURORDIS, particularly with regard to the implementation of the European Project for Rare Diseases National Plans Development (EUROPLAN) and European Platform for Rare Disease Registries (EPIRARE) projects and for other patient centred activities. The International Rare Diseases Research Consortium The International Rare Diseases Research Consortium (IRDiRC)14 was launched in 2011 by the European Commission and by the US National Institutes for Health Research to foster international collaboration in the RDs field. The Consortium's goal is to team up researchers and organisations investing in research to deliver 200 new therapies for RDs and to diagnose most RDs by the year 2020. These are some the ambitious challenges on IRDiRC agenda to be addressed through collaborative actions: - establish and provide access to harmonised data and samples; - perform the molecular and clinical characterisation of RDs; - boost translational, preclinical and clinical research. The collaboration will also be required to harmonise the policies related to research utilisation, standardisation and dissemination. Each organisation will use its own funding mechanism to support RDs research. The CNMR participates in some IRDiRC research projects and research, including the Interdisciplinary Committee, and chairs the Working Group on Registries and Natural History of RDs. The frame of action of the National Centre for Rare Diseases The history of the CNMR dates back to the institution of the National Registry3 for Rare Diseases in 2001, which was the first nucleus of the Centre. In fact, when the National Registry was instituted, the first building stone of the CNMR was also laid. On it, through the years, the CNMR has steadily evolved into a dynamic and vital centre for research and action, for prevention, diagnosis and treatment of RDs, for patient's empowerment and public awareness, through information and communication tools. In order to meet old and new challenges posed by RDs, the Centre has Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s593 Taruscio D et al developed its institutional activities along six main pillars: 1) experimental research; 2) public health; 3) projects; 4) information and communication; 5) training and empowerment; 6) networks and collaborations. 1. Experimental research on Rare Diseases The CNMR plays an important role in the coordination and promotion of experimental research on RDs in Italy, has participated in the Advisory Committee for European Research and is an active Work package (WP) leader of E-Rare project (see later). In 2003, a bilateral Italian and US agreement between the ISS and the US National Institutes of Health (NIH) was undersigned with the purpose of developing and increasing research in a number of fields, including RDs. In this respect, the CNMR has assured the implementation of a national programme of scientific research projects mainly based on the study of pathogenetic mechanisms, diagnosis, treatment and clinical management of RDs. On 16 December 2013, the agreement with the NIH was renewed until 2016. Within this international context, the CNMR carries out scientific research projects on selected RDs using advanced technologies (e.g. bioinformatic methodologies, high resolution melting, micro-RNA platform and CGH array). These studies are focused on a better comprehension of the molecular mechanisms underlying the pathogenesis of RDs, as well as the identification of specific biological markers involved in both RDs and rare cancers. The Centre is involved in collaborative studies on pathological conditions related to RDs15-24. In order to overcome the problems of the low number of patients with RD, a transnational collaboration with multidisciplinary approaches is highly desirable. In this respect, the CNMR has taken part in the activities of E-Rare, a EU funded project described in the Projects section. 2. Public Health actions on Rare Diseases The CNMR develops a number of public health activities in the field of RDs, from public health research on matters of relevance to its mission (e.g. epidemiology, service accessibility, identification of patients' needs) to policy. Through the coordination of the EU co-funded EUROPLAN project, it assists European States in defining needs and developing national plans for RDs, in accordance with the EU Recommendations. Following is a description of the main Public Health activities undertaken by the Centre to deal with the RDs emerging needs and interests. Primary and secondary prevention Since 2004, the Centre has coordinated the Italian Network for folic acid promotion in the primary prevention of congenital anomalies, which comprises more than 200 public and private organisations, such as local health authorities, patients organisations, scientific societies, research institutes and communication experts. In 2004, it developed and delivered the "Official Recommendation for the peri-conceptional supplementation of folic acid"25 and is currently working for the widest application of this Recommendation26. Subsequently, the Italian Medicines Agency (AIFA) decided to offer 0.4 mg folic acid supplements free of charge to all women planning a pregnancy. In 2008, the CNMR was part of the Scientific Cooperation Working Group (ESCO WG), established by the European Food Safety Authority (EFSA) for the study on the "Analysis of risks and benefits of fortification of food with folic acid", and was co-author of the final report published in November 200927. The CNMR participates to the European surveillance of congenital anomalies (EUROCAT) Joint Action 2011-2013 (see later) as coordinator of the WP on "Primary prevention of Congenital Anomalies". This WP has joined efforts with EUROPLAN in order to provide the "EUROCAT-EUROPLAN Recommendations on policies to be considered for the primary prevention of congenital anomalies in National Plans and Strategies on Rare Diseases"28. The document represents the first comprehensive set of recommendations for the primary prevention of congenital anomalies in the EU. The Centre played an important role in the coordination of the EU Tender on EU New-born Screening (NBS) Practices. The tender delivered a report on the practices of neonatal screening for RDs implemented in all the MS and established by the European Network of Experts on New-born Screening (EUNENBS). After consultation of EUNENBS members, 70 expert opinions were finalised into an Expert Opinion Document, to actively support the discussion for the development of European policies in the field of NBS of RDs29-31. Currently, the CNMR is working on a national project to expanded new-born screening, funded by the National Centre for Disease Prevention and Control (CCM) of the MOH, under their 2011 programme. Its aim is to overcome different implementation strategies at regional level, regarding the expanded new-born screening, through a national model based on principles of uniformity, coherence, effectiveness and portability32. The Registries Following is the presentation of the National Registry for Rare Diseases (RNMR) and the Disease-specific Registries conducted by the CNMR. Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s594 Italian National Centre Rare Diseases: research and public health The National Registry for Rare Diseases The RNMR was established in 2001 by Ministerial Decree (M.D.) 279/20013 and is run by the CNMR in collaboration with the regional registries. It collects epidemiological information useful to determine the dimension of the issue and the potential risk factors, to support clinical research and to foster the definition of diagnostic criteria. The general objectives of the RNMR are indicated in the Article 3 of the M.D. 279/2001; they were reasserted in two Agreements between the State and the Regions, in 200233 and 200734: 1 - planning and evaluating health care programmes (services utilization, patients' mobility…); 2 - diseases surveillance (estimation of prevalence and incidence, geographical and temporal distribution of RDs). The RNMR is structured into three levels, reflecting the Italian Healthcare System: local, regional and national level. The local level refers to clinical centres identified in each Region, which are the primary source of data flow. From here, patients' demographic and clinical data are collected and transmitted to the regional level. This is the intermediate level of data flow and is composed by regional registries. Each regional registry has a different organisational structure, different objectives, and, as a consequence, different types of information (variables) collected. Meanwhile, a common data set to be communicated from the regional registries to the RNMR was defined in line with the CNMR's mandate. This set includes socio-demographic as well as disease data for each patient: patient's identification code, birth date and place of birth, gender, place of residence; live-dead condition (with death date); diagnosis; RDs clinical centre where the diagnosis has been made; date of disease onset; date of diagnosis; orphan drug treatment used. The RNMR collects data on the conditions afferent to the list of RDs (see Annex 1 M.D. n. 279/2001). In 2012, the RNMR, in collaboration with Regional Registries, prepared it first annual report35. The RNMR future strategies include supporting the development of new clinical registries on specific RDs in order to better understand their natural history. Furthermore, the RNMR plans to strengthen the collaboration and networking among existing disease specific registries at national, as well as, at International level. For example, the RNMR is currently collaborating with the National Registry of Congenital Coagulopathies, established at the ISS, on Inherited Bleeding Disorders36,37. Meanwhile, the RNMR is working towards the improvement of quality of data collection at national and regional level. Accordingly, the Centre has collaborated with the EU Task Force on RDs of the EC Health and Consumers Protection Directorate General, whose goal is to revise the classification and codification of RDs in the ICD system. Its objective is to ensure that RDs are traceable in all health information systems, including national and international registries. Disease specific Registries The following Disease specific registries are maintained by the CNMR. Cystic Fibrosis Registry The Italian Cystic Fibrosis Registry (ICFR) collects demographic and epidemiological data on Cystic Fibrosis (CF) patients from the Italian CF Regional Centres. Anonymous data are collected using a specific common set of variables and definitions; these data are also forwarded to the European CF Patients Registry. Each participating centre is identified through a specific code. Use of data for scientific purposes is possible only after application and approval by a scientific committee and a representative of each regional centre. An Annual Report is elaborated by the scientific committee and a detailed description of CF patients (demography, diagnosis, genetics, etc.) is published. The ICFR sends the core data to the European Registry. T h e I t a l i a n D a t a b a s e f o r P a ro x y s m a l N o c t u r n a l Haemoglobinuria The Italian Database for Paroxysmal Nocturnal Haemoglobinuria (IDPNH) was set up in 2010 through the cooperation of the CNMR staff, haematologists and representatives of the patient organisation. The database, which interfaces with the RNMR, includes all patients with a diagnosis of PNH established according to international criteria. The IDPNH main objective is to enhance the knowledge of the natural history of the disease and to obtain information on short and longterm follow-up, particularly on how patients respond to available treatments. A set of variables are collected: personal data, clinical data, diagnostic tests, other laboratory data, blood transfusion treatment, drug treatment, pregnancies and quality of life. The IDPNH is web based and personal data are encrypted according to national regulations on the protection of personal data. A national expert on PNH validates the complete data set for each individual patient. The experience gained in the management of an institutional/epidemiological registry that collects data on all RDs - the RNMR - and in the management of research oriented registries, collecting data on single diseases (CF and PNH), has provided the CNMR with the track record that facilitated its selection for the coordination of the EPIRARE project and, as Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s595 Taruscio D et al well, for the WP on RD registries of the RD-Connect project. The two projects are aimed at building research infrastructures for exchange of data, with a focus, respectively, on epidemiology (EPIRARE), "omics" and translational research (RD-Connect). Both projects are presented in the specific Projects section. Quality Assurance on genetic tests and external quality assessment programmes The CNMR participated in the Organisation for Economic Cooperation and Development (OECD) Panel of experts for the preparation of Guidelines for quality assurance in molecular genetics tests and in the EU funded project "Multi-National External Quality Assay (EQA) programmes in Clinical Molecular Diagnostics" 38,39. The CNMR is a member of the European Molecular Genetics Quality Network and takes part in the EU funded EuroGentest excellence network, which aims at the standardisation and harmonisation of the quality of genetic testing in the EU MS. Since 2001, the CNMR has coordinated the National External Quality Assessment programme for genetic testing that covers molecular genetics (Fragile-X syndrome, Beta-Thalassemia, FAP (APC gene) and Cystic Fibrosis) and cytogenetics (prenatal, postnatal and oncological diagnosis) tests40,41. Since 2009, this activity is institutional and laboratories pay a fee to participate in each scheme42. Participation is voluntary and is open both to public and private laboratories. All submissions are assessed and reviewed by assessors, using previously agreed marking criteria. In molecular genetics, assessment takes into account genotyping, interpretation and reporting. In cytogenetics, assessment reviews banding quality, karyotype reconstructions, completeness/accuracy of the analysis, International System for Human Cytogenetic Nomenclature (ISCN), written description of the result, interpretation, completeness/accuracy of the report and reporting times. At the end of each round, participant laboratories receive a report with marks and comments; a web-utility has been developed to share documents and information among ISS/CNMR, the assessors and the laboratories. Up to now, nine rounds have been completed and, for the 9th round, a category of poor performance has been defined. In 2013, the number of participating medical genetics centres was 94; the number of participating cytogenetics and molecular genetics laboratories was 69 and 77 respectively. Each year the CNMR organises the annual Meeting on "Quality assessment of genetic testing", inviting relevant speakers, laboratories and assessors for a joint discussion on the aggregated results obtained. A specific external quality control scheme for the sweat test, a "gold standard" for the diagnosis of CF43, has been set up and the first Italian pilot experience, to be carried out by the CNMR, is under way. In fact, it is of critical importance that sweat testing is carried out accurately, with precise measurement of relevant analytes, in order to have the most accurate discrimination of results. Guidelines The CNMR is involved in developing guidelines for the management of RDs. Guidelines are produced in collaboration with the Italian National Guideline System (SNLG) and with relevant stakeholders - research organisations, governmental bodies and institutions of the Italian National Health System. In order to disseminate and promote the adoption of guidelines on RDs, the CNMR selects and makes available on its website guidelines prepared by national and international organisations. Moreover, an International Summer School on the development of guidelines on RDs is organised by the CNMR yearly. The CNMR actively participates in the international debate on the quality of existing guidelines, on their development and on the role of guidelines for RDs. In 2012, an international workshop with worldwide experts was organised to stimulate the debate on these themes. The FP7 project "RARE-Bestpractices", led by CNMR, was conceived in the mainstream of such debate and it is detailed in the Projects section. Narrative Medicine Narrative Medicine (NM) is considered a complementary approach to classic medicine, practiced with narrative skills of recognizing, absorbing, interpreting and being moved by the stories of illness. Treating by the narrative competencies, it is conducted through the doctor's and patient's understanding of the origin of the illness following the background of the problems, the reason of the illness and the whole body approach43-46. Since 2005, NM has emerged among the activities of the CNMR with the objective to disseminate its application on RDs, among social and health professionals, patients with RDs and their families, and patient organisations. In order to achieve its objective, a number of national and international activities were organised by the "national laboratory of narrative medicine" of the CNMR: - Documentation: research, analysis, monitoring of national and international literature in Open Source publishing; - Research: study of narratives relating to patients with RDs, relatives, health professionals, patient Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s596 Italian National Centre Rare Diseases: research and public health organisations. Following are some examples: the pilot study "General practitioners and rare diseases: knowledge, skills and needs" at national level; the first funded project "Rare diseases and Narrative Medicine: integrations and contributions in Public Health projects, quality of life, accessibility to social and health services and training" (in the NEPHIRD context), at European level and, recently, the European project "Story Telling on Record" (S.T.o.Re.). - Communication and training: activities addressing NHS workers, RD patients and their familiars. The CNMR organised the National Congress on "Narrative medicine and rare diseases" (2009, 2010, 2011) and the First International Congress "Narrative medicine and rare diseases" (2012). There are several approaches and methods in NM. In order to clarify its definition, methodology and practical utility (experiences and examples of application), the CNMR promoted the Italian Consensus Conference (CC) aimed at (a) developing recommendations (addressed to professionals working in the medical, social and health care sectors) for the implementation of NM at the clinical level, with regard to rare and chronic degenerative diseases and (b) identifying indicators useful to evaluate their implementation. The CC celebration day will be held in June 2014 together with the Second International Congress on "Narrative medicine and RDs". The CC document will be ready in Autumn 2014 and will be addressed to health professionals working in the Italian social and health care sectors. A number of activities have their roots in the NM Laboratory, such as the communication project "Controvento - Upwind", which includes a theatre piece, a book based on RD patients' stories and the National Competition "The Flight of Pegasus". The National competition "The Flight of Pegasus" "The Flight of Pegasus" is a literary art contest, sponsored by the CNMR. All participants are invited to tell their own experiences through writings, poems, drawings, photos and paintings. The main objectives are: (a) to provide a space for expression and visibility for people with RDs, as well as for all citizens, through various artistic and literary channels, and (2) to promote and disseminate the knowledge of RDs in all its aspects, by means of targeted communication and awareness campaigns. The results show the diverse viewpoints with which the disease is faced: isolation and neglect, indifference and difficulty of diagnosis and treatment, but also strong willpower and courage, sharing and tolerance. After years of activity, the most important outcome is the creation of a national network with all the participants, providing a real exchange of ideas, knowledge sharing and updating. The sixth award ceremony has taken place at the ISS on 25 February 2014, close to the Rare Disease Day. Orphan drugs CNMR has instituted the National Register of Orphan Drugs to collect, for a limited time period after their marketing, data of selected drugs newly authorised for the treatment of RDs, for the assessment of their appropriateness and safety. From 2001 to 2009 and from 2012-up to now, the CNMR has been the Italian member of the Committee of Orphan Medicinal Products (COMP) at the European Medicines Agency (EMA). Rare Diseases and organ transplantations: a new frontier Organ transplantation in RDs patients represents a new area of research for the CNMR, both for its clinical aspects, and for potential public health implications. Since the literature has very few data on this topic, the CNMR is carrying out a statistical survey, in collaboration with the Italian National Transplant Centre, with the aim of assessing the number of cases of RDs patients receiving organ transplantation, defining the type of RD and the transplantation carried out, together with the evaluation of the outcome. According to the preliminary data, 1,306 patients with RDs have undergone an organ transplantation over the period 2008-2012. This figure represented 8.9% of the total of the patients undergoing a transplant surgery in the same period (14,821 patients). The organs transplanted were mainly kidneys, livers, hearts, or lungs (71% of all the latter cases had RDs, mostly CF). The data on organ survival in RDs recipients show that, 5-6 years after the surgery, the cumulative survival is better for the RD patients compared with patients with other diagnoses. The reasons for this result are currently under study. However, some hypotheses are already being explored: are the results due to a better selection of the cases, when the patient is not yet in a severe condition, or to the fact that the transplantation represents a cure for some diseases? 3. Projects A number of national, European and international projects on RDs are undertaken yearly by the Centre. Following are some of the projects still under way or recently closed. European Platform for Rare Disease Registries European Platform for Rare Disease Registries (EPIRARE, www.epirare.eu)47, is a project co-funded by the EU Commission, DG-SANCO (2011-2014). It Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s597 Taruscio D et al is a feasibility study addressing regulatory, ethical and technical issues, associated with the registration of RD patients. The feasibility of a minimum data set common to all RDs designed to inform policy-makers is also being assessed by the project. The project carried out two surveys among registry and database holders and one among patients. The first was meant to explore the conditions and needs of existing RDs registries and to define the services and the contents that they would expect from a European platform. The second survey among registry holders was dedicated to assess the feasibility of a set of Common Data Elements (CDEs) from the existing RDs registries, by exploring the data elements that are currently collected by these registries. The survey among patients was dedicated to understand their needs and expectations from registries and from the implementation of a common EU framework for the registration of RD patients. In the framework of EPIRARE, particular interest and concrete actions have been devoted to monitor and influence the debate in the EU Parliament on the draft of the Regulation on General Personal Data Protection and an on-line petition was launched on this matter48. The work of the EPIRARE project resulted in two publications until now49,50. ERA-Net for Research Programmes on Rare Diseases ERA-Net for Research Programmes on Rare Diseases (E-RARE: 2006-2010, 2010-2014)51 is a project funded by FP7, dedicated to transnational coordination of research programmes on RDs (www.e-rare.eu). E-Rare 2, which follows the successful implementation of E-Rare-1 (2006-2010), aims at deepening and extending the cooperation among partners interested in the funding mechanisms for research on RDs. It works through the systematic exchange of information, the yearly launching of joint calls, the assessment of the funding strategies and the strategic activities for the sustainable development and the extension of the network. In order to reach this goal, the E-Rare Consortium has gathered 17 funding agencies/ministries from 14 European and Associated countries. Since 2007, E-Rare has launched and completed five joint transnational calls for research projects on RDs whereby 249 research groups belonging to 53 research consortia have been supported for an investment of € 37,5 million. In particular, the CNMR coordinates the WP dedicated to update and expand the analysis on the state of the art of RD research funding in Europe and in selected countries outside Europe, in order to map the current situation in these countries. The map will reveal the existing opportunities and the unmet needs throughout Europe. E-Rare-2 activities contribute to reducing the fragmentation of research and of resources through the coordination and the transnational funding of excellent research projects on RDs. This project has now become a key reference point in the landscape of European Transnational research funding on RDs. European Network for Surveillance of Congenital Anomalies Joint Action The European Network for Surveillance of Congenital Anomalies (EUROCAT) Joint Action (JA), was funded by the Public Health Programme 2008-2013 of the European Commission, to take place on the period January 2011-December 2013 (www.eurocat-network.eu)52. This JA combines funding of the EU and MS in order to secure a sustainable, high quality and easily accessible information system on Congenital Anomalies (CA). Its main objectives were the improvement of surveillance and the identification of strategies for primary prevention of CA, involving 36 Associate and 9 Collaborating Partners, and was structured into 9 WPs. The CNMR has coordinated the WP7, which focused on the effectiveness of CA primary prevention. The central aspect was the role of folic acid in the incidence of CA but other potential risk factors have been investigated. Risk factors studied were: use of drugs in pregnancy, effects of maternal infection and vaccination, chronic diseases, environmental factors, alcohol and smoking, and other maternal lifestyle issues. These issues were translated into the "EUROCAT-EUROPLAN Recommendations on policies to be considered for the primary prevention of congenital anomalies in National Plans and Strategies on Rare Diseases" as specified in the section on Primary and Secondary Prevention28. European Project for Rare Diseases National Plans Development The European Project for Rare Diseases National Plans Development (EUROPLAN, www. europlanproject.eu)53-57, which comprises two phases: EUROPLAN I (2008-2011) and EUROPLAN II (2012-2015), is co-funded by the EU Commission (DG-SANCO) and is coordinated by the CNMR. Its goal is to promote and implement National Plans or Strategies (NP/S) for RDs, and to share relevant experiences within Countries, linking national efforts with a common strategy at European level. This "double-level" approach ensures that progress is globally coherent and follows common orientations throughout Europe. Its main objective is to establish an international and interactive network of stakeholders (mainly policy makers) to speed up the elaboration and Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s598 Italian National Centre Rare Diseases: research and public health the implementation of NP/S for RDs, through scientific and technical assistance, workshops and the active participation of patient organisations (EURORDIS and National Alliances). EUROPLAN II builds on the achievements of the first project, whose goals was to elaborate tools and carry out activities to help EU Countries establish and implement NP/S in the field of RDs, coherent with the European Council Recommendations6. One of the tools developed during the first phase was the development of a set of 59 Indicators, as specified in the "Report on indicators for monitoring the implementation and evaluating the impact of National Plans or Strategies for rare diseases"54. In EUROPLAN II, WP 4 of the EUCERD Joint Action, foresees the participation of EURORDIS and Associated e Collaborating Partners from 33 Countries. EUROPLAN II, means to provide technical and scientific support to Countries with various geographical/economic concerns for the elaboration of their NP/S for RDs. This is meant to be achieved mainly through capacity building actions, which include training and continuing technical and scientific support for the sustainable development of the NP/S for RDs. In order to achieve the project's objectives, a process has been undertaken that comprises a number of steps: 1. a survey was carried out to identify strengths and weaknesses in the definition of NP/S in each Country context. 2. A set of 21 Core Indicators was defined, out of the original list, and was selected on the bases of their usefulness and feasibility to monitor health and social planning. The selection was the result of a Delphi Method organised by the ISS, then easily integrated with those selected according to the participatory process established by EURORDIS. This work has contributed to the elaboration of the EUCERD "Recommendations on Core Indicators for Rare Disease National Plans/Strategies"58. 3. Debrief sessions have been organised at the end of each national conference on RDs, to help local governments to focus on weak areas that need strengthening in order to develop effective NP/S. This is the first effective action for defining the collaboration and the other capacity building activities. 4. The next steps foresee the CNMR and its partners, along with the EU, providing the necessary support for the development of NP/S for RDs and furnishing all that is needed to guarantee its effective and timely sustainability. EU Tender on EU Newborn Screening EU Tender on EU Newborn Screening (NBS)59 was launched by the European Commission in July 2009 in order to (1) report on the practices of neonatal screening for RDs implemented in all MS, including number of centres, to estimate the number of infants screened and the number of disorders included in the NBS, as well as the criteria adopted for the selection of the diseases to be screened; (2) identify the types of clinical pathways implemented in MS; (3) establish a network of experts to analyse the results and formulate final recommendation on the best practices, as well as on the core panel of NBS conditions that could be included in all MS practices, and (4) develop a decision-making matrix that could be used by member states' programmes to systematically expand (or contract) screening mandates. The project, coordinated by the CNMR, was concluded in June 2011 with a consensus conference where the deliverables produced were approved by the members of the EU Network of Experts in NBS (EUNENBS), nominated by the RD competent authorities. The documents produced by the tender are available at: http://ec.europa.eu/health/rare_diseases/ screening/index_en.htm and have given rise to a number of publications on scientific journals. A platform for sharing best practices for the management of rare diseases A platform for sharing best practices for the management of rare diseases (RARE-Bestpractices)60 is is a four-year project (January 2013-December 2016), funded by the Seventh Framework Programme of the European Union (FP7/2007-2013) (www. rarebestpractices.eu). The overall aim of the project is to improve the care of patients by disseminating globally best practices for the management of persons with RDs. The CNMR acts as coordinator of 14 partners across Europe, all with a strong commitment in research on RDs, public health and evidence based medicine. The project main objectives are: Regarding guidelines - to provide reliable informative resources for the RD community by creating a collection of methodologically trustworthy and up-to-date guidelines for the management of RDs; - to develop a standard methodology suitable for the development of RD guidelines; - to set up training activities and educational tools targeted at key stakeholders for the production of high quality RD guidelines. Regarding Health Technology Assessment of orphan drugs - to ascertain cost-effectiveness assessment methods as well as criteria for funding decision making process of orphan drugs across European countries. Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s599 Taruscio D et al Other key elements of the platform will be the identification of mechanisms to address the limitations of the evidence, set priorities for RD research and propose improvements in pre-approval and post-marketing studies. Moreover, RARE-Bestpractices is supporting the creation of a new international open access, online, peer-reviewed journal: "RARE DISEASES AND ORPHAN DRUGS. An International journal of public health" (RARE Journal). RARE Journal is a science journal, published three times per year with no publishing fees for readers and authors and focuses on important aspects of public health, health policy and clinical research on RDs. More details are provided at the website: http://rarejournal.org/rarejournal. An integrated platform connecting databases, registries, biobanks and clinical bioinformatics for rare disease research An integrated platform connecting databases, registries, biobanks and clinical bioinformatics for rare disease research (RD-Connect)61 is a six-year project funded by the EC (7FP, 2012-2016) and the CNMR coordinates the WP on RD registries. RD-Connect is building a global infrastructure connecting data from RD research into a central resource for researchers across the world. RD-Connect is developing an integrated platform in which "omics" data will be combined with registries, clinical phenotype information and biomaterial availability. As therapeutic interventions are increasingly tailored towards the underlying genetic defects, patient registries need to include the genetic information of individual patients in a standardised way. Several clinical research networks, such as the one on CF, the one on Huntington disease and neuromuscular diseases, have concentrated efforts on a "new generation" of gene-specific patient databases. These include genotype data and detailed quality-controlled phenotype data and maintain the link with the patient within a secure ethical framework and in close collaboration with patient organisations. These initiatives have a much broader range of clinical utility than either locus-specific genetic databases (which are often anonymous and thus have no link to the patient for trial recruitment) or registries that do not collect genetic information and thus cannot facilitate cohort selection for trials. These next-generation registries have facilitated numerous studies including clinical trials, generated investments by commercial partners, and resulted in better treatments. The WP2 coordinated by the CNMR directly answers the need to harmonise and standardise global databases and patient registries for RDs in order to maximise their utility for "omics" and other research. Social Economic Burden and Health-related Quality of Life in Patients with Rare Diseases in Europe Social Economic Burden and Health-related Quality of Life in Patients with Rare Diseases in Europe (BURQOL-RD;www.burqol-rd.com)62 was a 3-year project under the 2nd Programme of Community Action in the Field of Public Health, commenced in April 2010 and ended in October 2013. It was funded by DG SANCO to generate a model to quantify the socio-economic costs and Health Related Quality of Life (HRQOL), of both patients and caregivers, for up to 10 RDs in different European countries. The general objective of this project was to develop a disease based model capable of quantifying the socioeconomic burden and the HRQOL of RD patients in Europe and of their caregivers. The model has to be adaptable and sufficiently sensitive to capture the differences in the distinct Health and Social Care Systems in the EU MS. BURQOL-RD represents the most complete and realistic costing of the burden of RDs performed in European countries to date. The results of the project show that the healthcare costs of RDs are very substantial. However, other social costs are even higher, such as loss of labour productivity and that of formal or informal care, representing significant hidden costs that should be made apparent to society. The information generated by the BURQOL-RD consortium will help: - policy makers design future policies in the area of RDs, which will ultimately have positive benefits for EU citizens' health, both of patients and of their caregivers; - patient organisations and RD Federations to give more weight to their requirements when addressing health policy makers; - scientific community to stimulate future research in the field of RDs transferring the protocols established to other RDs and to other countries. Story Telling on Record Story Telling on Record (S.T.o.Re. - www. storeproject.eu) is a 2-year European partnership funded in the Lifelong Learning Programme (Leonardo da Vinci Multilateral Partnerships August 2013 - July 2015). The project is coordinated by the CNMR, involves 7 partners from 6 Countries and foresees 4 partners' meetings and a final conference in Italy. The objective is to design an action-research that includes: (a) training participants, giving them the knowledge and the skills necessary to design, test and train people in the use of Integrated Medical Records (IMRs), and (b) organise courses on the use of IMRs for health care system personnel. Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s600 Italian National Centre Rare Diseases: research and public health The results of the project will be disseminated through a dedicated website, scientific reports and 2 booklets (toolkits in English and in the Partners' languages, tailored to patient organisations and to Health institutions and professionals). 4. Information and communication The CNMR uses different channels for information and communication purposes. The Institutional site The CNMR holds a portal on RDs63 which provides topics of interest to RD patients, to the scientific community and to anyone interested in RDs and includes a user friendly tool for searching disease-specific information. National helpline for Rare Diseases In order to provide quality information on RDs, a national telephone helpline for RDs (TVMR)64 was established at the CNMR in February 2008. It is a public, toll-free service that can be reached by composing the phone number 800.89.69.49 or via e-mail at: tvmr@ iss.it. The service is active 5 days per week, from 9 am to 1 pm. A team of psychologists and medical doctors trained and experienced in telephone counselling, public health policies and management of RDs are involved. The main aim of the service is to gather and provide information, through an active and personalised listening, on several issues regarding RDs, such as exemptions from the costs of medical cares, clinical centres, national and international centres of expertise, coordination of care, clinical trials for specific conditions running in Italy and abroad, patient organisations, how to get in contact with other patients, access to drugs and special services. Medical information regards rare, ultra-rare and relatively "common" rare conditions and refers, as a source of data, to the international scientific literature and to the main European and international databases on RDs. The service is addressed to any individual with an interest in RDs: patients and their relatives, health care professionals, clinicians, researchers, and patient organisations. Information is accurate and up-to-date and is meant to support and encourage patients and family members to face and solve specific problems and needs related to RDs. To date, more than 17,000 enquires (most of them phone calls) have been received and worked on. Calls are rather equally distributed over the different geographic areas of the country. Notably, one of the commonest purposes of calls and complaints is about undiagnosed diseases and/or on how to find the most appropriate specialist for a given suspected disease. Since 2012, TVMR is part of a European network of email and telephone help lines for RDs coordinated by EURORDIS. Publications The CNMR produces every year a number of publications, including articles for national, European and international journals on the activities of the Centre, brochures, posters and other relevant material. In order to expand its information strategy and highlight the broad range of national and international activities in the field of scientific research and public health, in 2007, the CNMR has initiated the publication of the Supplement of the ISS Bulletin on "Rare diseases and orphan drugs". The journal provides an overview of the CNMR activities and, more generally, of all matters related to RDs, from research to patient organisations. Divided into several sections, the Bulletin is addressed to general practitioners, to the personnel responsible for public health at regional and national level, to patients, family members or patient groups and to all those interested in RDs. The publication is distributed both in paper form, especially during scientific-informative events, and in a digital format, published in the website of the ISS and of the CNMR. The journal is also sent by e-mail to the CNMR mailing list. 5. Education, training and empowerment Every year, the CNMR organises a number of education and training activities on RDs65,66 directed to various stakeholders (patients and their families, patient organisations, physicians, nurse practitioners, paediatricians, residents of professional schools, etc.). Training of patients and families The CNMR is developing a programme of continuing education in RD patient identification, referral and management, addressed to GPs and other health professionals. The Centre has also carried out a number of courses, addressed to patient organisations, aiming at empowering RD patients, as well as their families, in the daily management of their disease. Courses for the members of patient organisations The CNMR has organised several training courses dedicated to the members of patient organisations. Among these it is worth mentioning: 1. "Implementation and evaluation of a training programme on orphan drugs targeting patient associations and families of patients with rare diseases" (2008-2010), a participatory training of trainers course on one of the major needs expressed by patients: orphan drugs (including Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s601 Taruscio D et al steps and challenges related to their development and commercialisation) and issues related to the accessibility of treatment for RDs. The course used Problem Based Learning (PBL) and the production of a Project work on the elaboration of a training and information programme on orphan drugs to be realised in the associations to which participants belonged. 2. The course on "Parent Training on Prader-Willi syndrome" was to engage the parents of children with PWS in order to improve their relationship with the children and children's behaviour, to increase the knowledge on PWS and to empower parents in managing their children. The intervention was offered to 32 parents coming from different Italian regions. The Parent Training programme consisted of twelve sessions of 2,3hours (from September 2008 to February 2009), and was conducted by two moderators: a psychologist and a parent with experience in parent training methods. Several questionnaires have been elaborated for the evaluation of the programme. Results from this study have suggested that parent training is a promising intervention for parents of children with behaviour problems. Thus, the next steps are to disseminate this intervention model to other RDs. Training activities for the NHS personnel In order to contribute to improving the quality of health care offered to patients with RDs, the CNMR - in collaboration with other institutions and organisations has organised, for many years, educational interventions for health and social personnel of the NHS. One of the most interesting training activity at the national level was the course "Rare diseases: diagnostic suspicion and effective communication", intended for General Practitioners and Paediatricians. Designed originally for the personnel of a local health organisation in the province of Rome, the course was then replicated in other Italian regions. It used PBL and a "one day/one problem" approach, to make the training model flexible and usable in a variety of contexts. Similar initiatives, targeted at clinicians and health professionals, also arise from the collaboration with organisations: an example is a course on congenital vascular malformations within the project "Promoting the network for general practitioners and paediatricians" (October 2013). In addition to courses on RDs, training programmes on specific topics such as guidelines, narrative medicine, disease registries, helpline on RDs, have also been carried out. Furthermore, the CNMR's researchers offer numerous lectures on national and international projects, oral presentations and posters, in collaboration with institutions, scientific societies and/or patient organisations. Advanced national and international courses and e-learning experience Followig are some of the Centre's most significant experiences regarding advanced of training. - Summer School on Guidelines In order to improve knowledge and adoption of RDs guidelines, the CNMR has organised since 2012 the International Summer School on "Clinical practices guidelines on rare diseases". The one-week intense course means to provide participants with the methodological basis for the development of RD guidelines. It also gives an introduction of the commonly used standards for the assessment of existing guidelines. The international team of trainers facilitates an informal and interactive learning environment, offering useful insights for discussion and stimulating the exchange of experiences between colleagues coming from different countries. The official language is English. - Summer School on Registries The first edition of the Summer School on RDs and orphan drug registries was in October 2013 and the second edition is planned to take place on 15-19 September 2014. The course takes the participants through the main concepts and practical steps that must be undertaken in the establishment and management of a RD registry to ensure its usefulness, soundness and sustainability. It provides basic notions on the methodology of observational studies, on the selection of data elements, on quality assurance and on the technical and legal tools that must be adopted to protect patients' data confidentiality. The course consists of frontal presentations followed by small group exercises. The official language is English. - Distance learning The CNMR has organised, in collaboration with the Distance Learning (FAD)67-69 working group of the External Relation Office/ISS, a 5 modules training course on "The prevention of congenital defects in the peri-conceptional and peri-natal: risk factors and protective factors for pregnancy" supported by a specific project funded by the Italian MOH. The training used an interactive and experiential methodology - PBL - which is normally used in classroom training. Therefore, using PBL in FAD, presented aspects of training innovation70. More than 1,000 health professionals attended this e-learning course. One year after the training, a "Follow-up skills questionnaire" was administered to course participants to assess their perceived impact of the course on learning, on their professional practice, Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s602 Italian National Centre Rare Diseases: research and public health on opinions and attitudes towards the improvement of the promotion of folic acid supplementation. The data collected from the questionnaire shows an increased awareness and an improved quality of the participants professional practice, with more attention paid to health promotion and primary prevention. According to the data analysis, knowledge increased of about 30% and about 80% of the participants thought that the course provided a positive contribution to change their professional activities. Overall, the participants evaluated positively the learning experience, appreciating the opportunity to attend an e-learning programme with such an innovative methodology71. - Capacity building activities Recently, the CNMR has initiated activities of capacity building in the framework of the EUROPLAN project, on request of the EU. Capacity Building is a conceptual approach to development that focuses on understanding the obstacles that inhibit governments from realizing their developmental goals, while enhancing their abilities that will allow them to achieve measurable and sustainable results. Capacity building is a process and starts with the definition of needs and the obstacles that hinder progress in achieving the results. It includes all those actions that allow the Government to accomplish specific objectives and maintain the results over the time. Activities, tailored to each situation, include the training of human resources but are not limited to it. It comprises technical support and other strengthening efforts. The experience in capacity building that will be gained in the EUROPLAN II project will be useful for other active sectors of the Centre's areas of interest. 6. Networks and collaborations The CNMR base most its work on networking and on effective collaboration at national, European and international level. Evidence of this effort is found in the description of the research activities, of the projects and of the many actions related to RDs. Furthermore, the CNMR participates, through its staff, in different national and international committees. Among these, it is worth mentioning the CNMR participation in: - the Italian Clinical Trial Phase I Committee, which is the national committee that authorises Phase I clinical studies of new drugs; - the Committee for Orphan Medicinal Products (COMP), at the European Medicines Agency (EMA); - the EU Commission Expert Group on Rare Diseases. Discussion and final considerations RDs have undoubtedly been on the European agenda since the early 1990s. While a disease might be defined as "rare", the number of persons in Europe suffering from a RD is estimated to be between 27 and 36 million, or 6 to 8% of the European population. Insufficient resources are dedicated to research for RDs and these, as well as expertise in these conditions, is fragmented across individual EU countries. Likewise, limited resources are devoted to improve ability and competencies in diagnosis, treatment and care of RDs patients throughout Europe. For this purpose, a number of documents and recommendations have been issued by the EU advising MS to take action in addressing RDs in their National context. In particular, a recommendation called on all EU MS to develop plans or strategies for RDs by 2013, in order to ensure universal access of RD patients to high quality care. The Italian Government has taken factual steps in recognising the importance of RDs and has complied with some of the main Council Recommendations. Nevertheless, Italy has no National Plan for Rare Diseases yet72, and this remains an open issue for this country. Likewise, the exclusion of some/most RDs from the list that would exempt individuals with RDs from paying for disease-related services creates inequities among the patients population. The low level of investments in scientific research, the insufficient number of specialised infrastructures and their uneven geographical distribution, along with the lack of knowledge of many RDs, make diagnosis and treatment difficult, delayed and costly. Often, RD patients have to migrate from one region to another, or even travel abroad, in search of a diagnosis or appropriate treatment. Without any doubt, it can be stated that RD patients, in addition to the heavy burden of the disease, face heavy inequalities in the access to care and services. RDs do not only affect diagnosed people, but also their families, friends, caregivers and society as a whole. It is not uncommon for families of RD patients to end up impoverishing themselves in the effort to obtain a proper and timely diagnosis or an appropriate treatment for their diseased relatives. These open challenges require the utmost attention by the Government and by all stakeholders, both at Italian and at European level. Particularly relevant is the action of patient organisations which, by voicing the real instances of RD patients, can be catalyst of more positive and rapid societal changes. Their consistent call for policies and programmes that aim at improving the quality of life of all people living with RDs should produce effective results. The Italian patient organisations are proactive and it is hopeful that their positive and determinate action can bring about a better future for Italian RD patients and for their families. Since its establishment in 2008, the CNMR has developed and carried out a wide range of activities tackling old and new RD challenges in a comprehensive Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s603 Taruscio D et al and integrated manner. Innovation, enthusiasm, scientific rigour, quality, vision and hard work are the basic values on which the dynamic group of professionals, that constitute the CNMR, base their daily work. Their strategy is to gather essential elements of experimental research, acquire the newest and most relevant public health findings and translate both into effective and efficient actions for the prevention, surveillance, diagnosis and treatment of RDs in Italy. They also participate in the on-going research and action on RDs in Europe and at international level and thus contribute to improving the quality of life and the care of RD patients in Italy and elsewhere. Keywords: rare diseases, orphan drugs, experimental research, public health, registries. The Authors declare no conflict of interest. References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) Italia. Decreto Ministeriale 26 giugno 2008. Norme per l'organizzazione strutturale e la disciplina del rapporto di lavoro dei dipendenti dell'Istituto Superiore di Sanità. Centro Nazionale delle Malattie Rare, missione: ricerca, consulenza e documentazione sulle malattie rare e farmaci orfani finalizzata a prevenzione, trattamento e sorveglianza. Gazzetta Ufficiale Serie Generale n. 157, 7 luglio 2008. Commission of the European Communities. Proposal for a Council Recommendation on a European action in the field of rare diseases. COM(2008); 726 final. Italia. Decreto Ministeriale 18 Maggio 2001, n. 279. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124. Gazzetta Ufficiale - Serie Generale n. 160, 12 luglio 2001. Suppl. Ord. n. 180/L. Commission of the European Communities. Communication on the framework for action in the field of public health. COM(1993); 559. European Parliament and Council. Regulation (EC) 141/2000 of the European Parliament and of the Council of 16 December 1999 on orphan medicinal products. Official Journal 2000; L 18:1-5. European Council. Recommendation of 8 June 2009 on European action in the field of rare diseases. Official Journal C151:7-10. European Parliament and Council. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare. Official Journal of the European Union 2011; L 88/45 Commission of the European Communities. Decision of 30 November 2009 establishing a European Union Committee of Experts on Rare Diseases 2009; 872. Commission of the European Communities. Decision of 30 July 2013 setting up a Commission expert group on rare diseases and repealing Decision 2009/872/EC (2013/C 219/04) The Italian Federation for Rare Diseases - UNIAMO. Available at: http://www.uniamo.org. Accessed on 15/01/2014. European Organisation for Rare Diseases - EURORDIS. Available at: https://www.eurordis.org. Accessed on 15/01/2014. The National Council for RDs. Available at: http://www. cndmr-insieme.it/. Accessed on 15/01/2014 The Italian Movement for Rare Patients - MIR. Available at: http://www.movimentorari.it/mir/. Accessed on 15/01/2014 14) International Rare Diseases Research Consortium - IRDiRC. Available at: http://www.irdirc.org/. Accessed on 15/01/2014. 15) Taruscio D, Salvatore M, Magrelli A, Tomanin R. Predictive medicine and biomarkers: the case of rare diseases. Personalized Medicine 2012; 9: 143-6. 16) Taruscio D, Salvatore M, Magrelli A. The Role of microRNAs in the Biology of Rare Diseases. Int J Mol Sci. 2011; 12 (10): 6733-42. 17) Magrelli A, Azzalin G, Salvatore M, et al. Altered microRNA Expression Patterns in Hepatoblastoma Patients. Transl Oncol. 2009, 2: 157-63. 18) Matteucci A, Gaddini L, Macchia G, et al. Developmental expression of dysbindin in Muller cells of rat retina. Experimental eye research 2013; 116C: 1-8. 19) Fratini F, Macchia G, Torreri P, et al. Phosphorylation on threonine 11 of ß-dystrobrevin alters its interaction with kinesin heavy chain. FEBS journal 2012; 279: 4131-4. 20) Saulle E, Guerriero R, Petronelli A, et al. Autocrine role of angiopoietins during megakaryocytic differentiation. PLoS One. 2012; 7: e39796. 21) D'Arcangelo G, Grossi D, De Chiara G, et al. Glutamatergic neurotransmission in a mouse model of Niemann-Pick Type C Disease. Brain Res. 2011; 1396: 11-9. 22) Petrini S, Minnone G, Coccetti M, et al. Monocytes and macrophages as biomarkers for the diagnosis of megalencephalic leukoencephalopathy with subcortical cysts. Molecular and Cellular Neuroscience 2013; 56: 307-21. 23) Villa L, Carattoli A, Nordmann P, et al. Complete sequence of the IncT-type plasmid pT-OXA-181 carrying the blaOXA-181 carbapenemase gene from Citrobacter freundii. Antimicrob Agents Chemother. 2013; 57: 1965-7. 24) Sassera D, Leardini I, Villa L, et al. Draft Genome Sequence of Stenotrophomonas maltophilia Strain EPM1, Found in Association with a Culture of the Human Parasite Giardia duodenalis. Genome Announc. 2013; 1: e0018213. 25) Salerno P, Bianchi F, Pierini A, et al. Folic acid and congenital malformation: scientific evidence and public health strategies. Ann Ig. 2008; 20: 519-30. 26) Taruscio D, Carbone P, Granata O, et al. Folic acid and primary prevention of birth defects. Biofactors. 2011, 37: 280-4. 27) ESCO Report on Analysis of Risks and Benefits of Fortification of Food with Folic Acid. EFSA 2009. 28) EUROCAT (European Surveillance of Congenital Anomalies) and EUROPLAN (European Project for Rare Diseases National Plans Development) Primary prevention of congenital anomalies. Recommendations on policies to be considered for the primary prevention of congenital anomalies in National Plans and Strategies on Rare Diseases. Available at: http://www.eucerd.eu/wp-content/uploads/2013/03/ Eurocat_Reco_PrimaryPrevention.pdf. Accessed on 15/01/2014. 29) Cornel MC, Rigter T, Weinreich SS, et al. A framework to start the debate on neonatal screening policies in the EU: an Expert Opinion Document. Eur J Hum Genet. 2014; 22: 12-7. 30) Loeber JG, Burgard P, Cornel MC, et al. Newborn screening programmes in Europe; arguments and efforts regarding harmonization. Part 1. From blood spot to screening result. J Inherit Metab Dis. 2012; 35: 603-11. 31) Burgard P, Rupp K, Lindner M, et al. Newborn screening programmes in Europe; arguments and efforts regarding harmonization. Part 2. From screening laboratory results to treatment, follow-up and quality assurance. J Inherit Metab Dis. 2012; 35: 613-25. 32) Carbone P, Sanseverino A, Granata O, et al. Expanded newborn screening: an operative model for prevention of inborn errors of metabolism. Not Ist Super Sanità 2013; 26 (Suppl. 1): 6-9. 33) Italia. Accordo Stato - regioni dell'11 luglio 2002 (repertorio 1485/CSR). 34) Italia. Accordo Stato - regioni del 10 maggio 2007 (repertorio 103/CSR). 35) Taruscio D (Ed). Il Registro Nazionale e i Registri Regionali/ interregionali delle malattie rare. Rapporto anno 2011. Roma: Istituto Superiore di Sanità; 2011 (Rapporti ISTISAN 11/20). Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s604 Italian National Centre Rare Diseases: research and public health 36) Abbonizio F, Giampaolo A, Arcieri R, Hassan HJ, AICE. Registro Nazionale delle Coagulopatie Congenite. Rapporto 2011. Roma: Istituto Superiore di Sanità; 2012. (Rapporti ISTISAN 12/55). 37) Hassan HJ, Morfini M, Taruscio D, et al. Current Status of Italian Registries on inherited bleeding disorders. Blood Transfus 2014; 12 (Suppl 3): s576-81. 38) Genetic Testing: A Survey of Quality Assurance and Proficiency Standards. Available at: http://www.oecd.org/sti/ biotech/genetictestingasurveyofqualityassuranceandproficie ncystandards.htm; Accessed on 15/01/2014. 39) Orlando C, Verderio P, Maatman R, et al. EQUAL-qual: a European program for external quality assessment of genomic DNA extraction and PCR amplification. Clin Chem. 2007; 53:1349-57. 40) Floridia G, Falbo V, Censi F, et al. The Italian external quality assessment scheme in classical cytogenetics: four years of activity. Community Genet. 2008; 11: 295-303. 41) Censi F, Tosto F, Floridia G, et al. The Italian National External Quality Assessment programme in molecular genetic testing: results of the VII round (2010-2011). Biomed Res Int. 2013, doi: 10.1155/2013/739010. 42) Italia. Decreto Presidenziale. Tariffario dei servizi resi a pagamento dall'Istituto Superiore di Sanità Gazzetta Ufficiale Serie Generale n. 199 del7/7/2008 43) Taylor CJ, Hardcastle J, Southern KW. Physiological measurements confirming the diagnosis of cystic fibrosis: the sweat test and measurements of transepithelial potential difference. Paediatr Respir Rev. 2009; 10: 220-6. 44) Charon R. Narrative medicine. A Model for Empathy, Reflection, Profession and Trust. JAMA. 2001; 286: 1897-902. 45) Gentile AE, Taruscio D. Conclusioni. Le parole nel tempio. In "Narrazione e disabilità intellettiva. Valorizzare le esperienze individuali nei percorsi educativi e di cura" a cura di Ruggerini C, Manzotti, S, Griffo G, Veglia F, in "Le Guide Erickson. Metodologie e percorsi per la didattica, l'educazione, la riabilitazione, il recupero e il sostegno" Collana diretta da Dario Ianes. 2013, Edizioni Erickson, Trento. 46) Luzi I, Gentile AE, Taruscio D (Ed.). First International Congress Narrative Medicine and Rare Diseases. Istituto Superiore di Sanità. Rome, June 4, 2012. Proceedings. Roma: Istituto Superiore di Sanità; 2013. (Rapporti ISTISAN 13/13). 47) European Platform for Rare Disease Registries. Available at: http://www.epirare.eu/. Accessed on 15/01/2014 48) Vittozzi L. Don't Stop Research on Rare Diseases! Available at: http://www.change.org/en-GB/petitions/don-t-stop-researchon-rare-diseases-2. Accessed on 15/01/2014. 49) Taruscio D, Gainotti S, Mollo E, et al. The current situation and needs of rare disease registries in Europe. Pub. Health Genomics 2013; 16: 288-98. 50) Vittozzi L, Gainotti S, Mollo E, et al. A Model for the European Platform for Rare Disease Registries. Pub. Health Genomics 2013; 16: 299-304. 51) ERA-Net for Research Programmes on Rare Diseases. Available at: http://www.e-rare.eu/. Accessed on 15/01/2014. 52) European Network for surveillance of Congenital Anomalies. Available at: http://www.eurocat-network.eu/aboutus/ jointactioneurocat. Accessed on 15/01/2014. 53) The European Project for Rare Diseases National Plans Development (EUROPLAN). Available at: http://www. europlanproject.eu/. Accessed on 15/01/2014. 54) Report on EU Member States initiatives, with previous and current experiences on rare diseases. Available at http://www. europlanproject.eu/_newsite_986989/Resources/docs/20082011_1.EUCERDReport.pdf. Accessed on 15/01/2014. 55) Taruscio D, Gentile AE, De Santis M, et al. National Plans on rare diseases. In Meral Özgüç (Editor) «Rare Diseases: Integrative PPPM Approach as the Medicine of the Future», Series: Advances in Predictive, Preventive and Personalised Medicine, Springer (in press). 56) Taruscio D, Gentile AE, De Santis M, et al. EUROPLAN: A Project to Support the Development of National Plans on Rare Diseases in Europe. Public Health Genomics 2013; 16: 278-87. 57) Taruscio D, Vittozzi L, Stefanov R. National plans and strategies on rare diseases in Europe. Adv Exp Med Biol 2010; 686: 475-91. 58) EUCERD Recommendations on Core Indicators for RD National Plans/Strategies (June 2013b). Available at http:// www.eucerd.eu/wp-content/uploads/2013/06/EUCERD_ Recommendations_Indicators_adopted.pdf. Accessed on 15/01/2014. 59) EU Tenders: Evaluation of population newborn screening practices for rare disorders in Member States of the European Union Rare diseases - New born screening. Available at: http:// ec.europa.eu/eahc/health/tenders_H09C2.html. Accessed on 15/01/2014. 60) RARE-Bestpractices A platform for sharing best practices for the management of rare diseases. Available at: http://www. rarebestpractices.eu/home. Accessed on 15/01/2014. 61) An integrated platform connecting databases, registries, biobanks and clinical bioinformatics for rare disease research -RD-Connect. Available at: http://rd-connect.eu/. Accessed on 15/01/2014. 62) Social economic burden and health-related quality of life in patients with rare diseases in Europe. Available at: http:// burqol-rd.com/index.html Accessed on 15/01/2014. 63) Italian National Center for Rare Diseases. Available at: http:// www.iss.it/cnmr. Accessed on 15/01/2014. 64) Taruscio D, Gentile AE. Approfondimento. Il Telefono Verde Malattie Rare (TVMR - 800 89 69 49) dell'Istituto Superiore di Sanità. In: Cognetti G, Il grano e il loglio: viaggio nell'informazione sulla salute in internet per i cittadini. 2012; 8: 107. 65) Ferrelli RM, Gentile AE, De Virgilio G, Taruscio D. Training general practitioners and paediatricians on rare disease diagnostic suspect and effective communication [abstract]. European Conference on Rare Diseases and Orphan Products 2012 Brussels. 66) Ferrelli RM, Gentile AE, Coclite D, et al. Integrazione di competenze tecniche e metodologiche in ISS: l'esempio della formazione dei medici di medicina generale sulle malattie rare. Notiziario dell'Istituto Superiore di Sanità 2011; 24: 3-6. 67) Carbone P, Granata O, Barbina D, et al. Stato delle conoscenze degli operatori sanitari sulla prevenzione di difetti congeniti con acido folico: le evidenze scaturite da un corso E-learning. Network Italiano Promozione Acido Folico per la Prevenzione Primaria di Difetti Congeniti e Coordinamento Nazionale dei Registri delle Malformazioni Congenite, ISTISAN Congressi. 2010; 10 (C6): 15-6. 68) Granata O, Carbone P, Barbina D, et al. Il contributo della formazione a distanza nella promozione attiva dell'acido folico per la prevenzione di difetti congeniti: risultati di un followup sulle attitudini e i comportamenti degli operatori sanitari. ISTISAN Congressi 2010; 10 (C6): 18-9. 69) Carbone P, Baldi F, Barbina D, et al. Realizzazione di un percorso di formazione e-learning: La prevenzione dei difetti congeniti nel periodo peri-concezionale e peri-natale - Fattori di rischio e fattori protettivi per la gravidanza. ISTISAN Congressi. 2009; 09 (C8): 32-3. 70) De Vita L, Barbina D, Bonciani M, et al. Il metodo dell'apprendimento per problemi in un corso di formazione a distanza sulla prevenzione delle malformazioni congenite. ISTISAN Congressi. 2009; 09 (C8): 36-7. 71) Granata O, Carbone P, Taruscio D. Attività di formazione e informazione per la prevenzione primaria di difetti congeniti. Rapporti ISTISAN 2013; 13/28, 85-98. 72) Congiu ME. Italian National Plan for rare diseases. Blood Transfus 2014; 12 (Suppl 3): s614-6. Correspondence: Domenica Taruscio Italian National Centre for Rare Diseases - Istituto Superiore di Sanità Viale Regina Elena 299 00161 Rome, Italy e-mail: domenica.taruscio@iss.it Blood Transfus 2014; 12 Suppl 3: s591-605 DOI 10.2450/2014.0040-14s s605 ORIGINAL ARTICLE The Italian National Rare Diseases Registry Domenica Taruscio, Yllka Kodra, Gianluca Ferrari, Luciano Vittozzi and the National Rare Diseases Registry Collaborating Group National Centre for Rare Diseases, Istituto Superiore di Sanità, Rome, Italy Introduction. Rare disease registries are a priority at European level and specific actions are being implemented by the European Commission to support their development. In Italy, a National Registry of rare diseases has been established in 2001 as a network of regional registries. The latter have gradually been established and the full coverage of the Italian territory was attained during 2011. Methods. Here we describe the basic features of the National Registry of rare diseases; the activities carried out to promote consistent operations in the regional registries; and the overall quality and composition of the records collected. Results. After a validation process, including removal of duplicate records, 110,841 records of patients with rare diseases, single and with group denominations, are stored in the National Registry of rare diseases. They correspond to the overall diagnoses communicated to national registry by regional registries up to 30 June 2012. The quality of the data collected by the the National Registry of rare diseases has been assessed with respect to completeness and consistency of procedures. Variables characterising case and diagnosis showed a very limited number of missing values. Records reported at least one case of 485 rare conditions. Discussion. To date, the National Registry of rare diseases is a surveillance system with the main objective of producing epidemiologic evidence on rare diseases in Italy, and of supporting policy making and health services planning. Data quality still represents a limitation for any sound epidemiological estimate of rare diseases in Italy. However, improvements of the quality of collected data and the completeness of case notifications should be strengthened. Keywords: Italy, rare diseases, registry, public health. Introduction Rare Diseases (RD) are a special challenge for the healthcare systems, because of their limited knowledge about their natural history, chronicity, need for long-term follow-up and potential high demand for assistance. Sound data on their prevalence and incidence are scantly available1 but, since they are as many as 7-8,000, it is estimated that, in the European Union only they affect about 29 million people2. Thus, the term "Registry" in the field of RD means more than a common epidemiologic tool for collection of secondary data related to patients with a specific RD diagnosis. Indeed, RD registries represent an effective way to achieve a sufficient sample size for epidemiological and clinical research3-5. Therefore, RD registries are key instruments for the surveillance of these diseases, with the aim of improving patient care and health care planning6. For these reasons registries are a priority at European level in the field of rare diseases2,7 and specific actions are being implemented to support the development of RD registries8. A national institutional registry of rare disease patients, the Registro Nazionale Malattie Rare (RNMR), has been established in Italy in 2001 and is run by the National Centre for Rare Diseases (Centro Nazionale Malattie Rare, CNMR) of the Istituto Superiore di Sanità (National Institute of Health). Since then, the national and regional health authorities have cooperated for its implementation and after some years necessary for the development of the local communication networks and of the gradual establishment of the regional registries (RRs), the system achieved the full coverage of the national territory during 2011. In consideration of the expected developments resulting from the European Union initiatives, this paper presents the main steps of the implementation of the RNMR and its main achievements, with the aim of sharing the RNMR experience with scientists and policy makers in the field of RD. Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s606 © SIMTI Servizi Srl The Italian RD Registry Methods Legal basis, integration in the health system and scope of the RNMR The RNMR has been established at the National Institute of Health by Ministerial Decree (MD) in 2001 as part of the measures devoted to improve health care for RD patients9. Indeed, it also envisaged the establishment, at regional or interregional level, of a network of formally designated centres (FDCs) with recognised expertise on RD, which could carry out the confirmatory investigations free of charge for the suspect patient, ensure a better and more effective patient management and ascertain the right of the patient to RD clinical assistance and treatments. This decree made reference to a list of 314 individual RD identified with own codes and 52 groups and subgroups of RD with group codes. Within these groups, 160 example pathologies were mentioned. The RNMR mandate was to monitor RD and inform the national and regional planning of measures for the protection of RD patients. The decree also explicitly mentioned the faculty for RNMR to liaise with international registries and to collect demographic, anamnesis, clinical, laboratory, determinant data of use for medical, biomedical and epidemiological research. Patient pseudonymization and the possibility of patient tracing in case of need were allowed in compliance with data protection legislation. Due to the devolved organisation of the Italian health system, which gives the Regions the responsibility for the delivery of health services, the MD provided that the RNMR was functionally linked to RRs, which were to be established by regional authorities. Two agreements between the Central Government and the Regional Authorities, in 2002 and 2007, ensured the coordinated implementation of the RRs, defining the set of variables and the procedures for the data communication between the RRs and the RNMR10,11. Establishment of regional registries Following the MD, to ensure the delivery of RD special assistance, the regional authorities proceeded to the designation of their FDCs on the basis of criteria related to competence in the diagnosis, care and treatment of RD and to the availability of appropriate complementary services. Subsequently, the regional authorities established the RRs with regional decrees and other regulations, which ensured the necessary infrastructures as well as the legitimacy and security of the data flow from the FDCs to the corresponding RRs in compliance with the personal data protection legislation. In many cases, specific information systems have been developed at regional level with the aim of supporting the data collection and in some cases, the delivery of health care services to RD patients. The RRs may differ in aims and internal organisation: some have mainly epidemiological and public health purposes, in support of regional planning, while others also aim at evaluating health services and diagnostic procedures, or are integrated in the regional health care delivery system. Data set and data communication A common data set for the communication of data from the RRs to the RNMR was defined to fulfil the mandate of RNMR. This set is detailed in Table I. The diagnosis was expressed according to the exemption code attributed by the MD. The RRs sent RNMR the data batches regarding confirmed diagnoses made by their FDCs in each semester of the calendar year. Data communication took place normally during January and July. This practice is changing to an annual transfer based on whole calendar years. Table I - The common data set of the RNMR. Variables Reason ID (encrypted code based on given name, family name, birth date and place, sex) Avoid multiple registrations of the same patient; conduct any type of record linkage Sex Epidemiologic analysis Date of birth Age at disease onset, diagnosis, death Place of residence Prevalence, geographical distribution, patient mobility Live - dead condition Prevalence Date of death Prevalence; age at death Diagnosis of rare disease Epidemiologic analysis Date of diagnosis Incidence; diagnosis delay Centre of RD diagnosis Patient mobility; health service utilization Date of disease onset Incidence; diagnosis delay Orphan drug used Treatment monitoring Training of the operators Statisticians and computer technicians of the RNMR have held training courses from 2002 to 2009 to the Regions without a proprietary rare diseases registry to introduce the operators of the RRs to the proprietary software developed by CNMR and to standardize the methods used to collect the data throughout the country. Quality control procedures Experts in each RRs were responsible for the validation of the data of the corresponding FDCs. Some information systems supporting registries allow quality data control at the moment of the data entry by users. Furthermore, quality control processes are regularly carried out by RRs staff. In addition, at national level, the quality control of the common data set was carried out on the whole database in two steps by the RNMR operators. Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s607 Taruscio D et al The first step consisted of a control of duplicate records, logical inconsistencies and range errors on individual data batches sent by the RRs. In case that range errors or logical inconsistencies were found, the records were sent back to the RRs for a check with the regional data sources. Inconsistencies and range errors which were not resolved after this control were considered as missing data. The second step was carried out on the database resulting from the merging of the regional data batches. In particular, this procedure checked for possible duplicates coming from different RRs and a specific protocol for the management of duplicate records was followed as shown in Table II. As shown in this table, the record management was dependent on the type of duplication and different record extractions were carried out depending on the scope of the analyses. Periodic meetings and reporting The experts responsible for the RRs convened yearly to report on achievements and experience in the management of their registries and to discuss common issues. In 2012, the RNMR, in collaboration with the RRs, prepared its first annual report12, where the main features of the RRs and of the data quality were described. Compliance with personal data protection Regulations Each regional registry collects information on patients according to the national data protection law. When part of the data collected by RRs are communicated to the RNMR, an algorithm is used for the secure transfer of information. The data transmission took place by means of a temporary channel opened temporarily for this purpose and the personal data were transmitted separately from sensitive data. Personal and sensitive data were stored in separate servers of the informatics service of the National Institute of Health, protected with advanced firewall and technological systems. Results The geographic coverage of RNMR When the MD was put into effect, a RR of RD patients was in operation in the Veneto region only. Since then, RRs were progressively established and connected to the RNMR (Figure 1). The 2007 Agreement between Central Government and the Regions11, triggered a significant acceleration of the process (Figure 2) and the full coverage of the Italian territory connected with the RNMR was achieved during 2011. The establishment of the RRs resulted in a significant increase of the cases communicated to the RNMR, which approximately paralleled the increase in the nominal population coverage calculated from the official resident population of the regions. Quality of the common data set Up to 30 June 2012, 112,766 records of RD patients were communicated to the RNMR. During the subsequent validation process, 25 records showed missing values for diagnosis or ID code or missing date of birth or sex. After check with the RRs, 17 records were discarded and 8 records were retained for subsequent processing. The remaining set of 112,749 records were checked for the presence of duplicate records, i.e., multiple records of a same patient received from different RRs and managed depending on the type of duplication as reported in Table II, which also shows the Table II - Description and process management of duplicate records. Duplicate type 1 Duplicate type 2 Duplicate type 3 Description Records with same ID, diagnosis and diagnostic centre. Records with same ID and diagnosis and different diagnostic centre for RDs. Records with same ID and different rare disease diagnosis. Presumed cause Additional notifications are made of a case already notified. The case was diagnosed in two or more different centres, which notified the case. The case is affected by more RDs. Record management Aim of analysis Analysis of the activity of diagnosis centres Only the record with less recent diagnosis is considered. The other records are discarded. All records are considered. No records are discarded. All records are considered. No records are discarded. Analysis of cases recorded in the RNMR Only the record with less recent diagnosis is considered. The other records are discarded. Only the record with less recent diagnosis is considered. No records are discarded. Only the record with less recent diagnosis is considered. No records are discarded. Analysis of RDs recorded in the RNMR Only the record with less recent diagnosis is considered. The other records are discarded. Only the record with less recent diagnosis is considered. No records are discarded. All records are considered. No records are discarded. Number of duplicate records 3,322 3,393 2,483 Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s608 The Italian RD Registry results of this analysis. Discarded Type 1 records, which represent true duplicates, were 1 908, corresponding to 1.7% of the total valid records. Therefore the cleaned database was made of 110,841 records. The quality of the data collected by the RNMR has been assessed with respect to completeness and consistency of procedures. Table III summarizes the results of this control for each variable of the common data set. While completeness analysis was based on the observation of the database records, the assessment of consistency of procedures summarizes the discrepancies emerged during the preparation of the first RNMR report. The variables characterizing case and diagnosis showed a very limited number of missing values and a remarkable improvement could be observed, during time, in the completeness of recording of the centre making diagnosis. It is often the case with registries, that the date of death of patients is not collected systematically and timely by registry data providers. Although some records reported live cases with unrealistic age, there was no criterion that the RNMR could use to spot all records that did not update this information regularly. The date of disease onset is largely and persistently incomplete. An analysis of the records showed that missing data were mostly associated with some RRs. Indeed, while it is difficult to define the date of the symptoms onset in the case of patients affected by a rare diseases since a long time, or when the first signs or symptoms of a rare diseases are unspecific, some RRs do not collect this data. The completeness of data regarding the use of orphan drugs was assessed as follows. At first, the diseases were identified, for which an indication of use of orphan drugs was given; then, making reference to all the records of each of the diseases so identified, the fraction of records with missing values was calculated. This analysis indicated that, in the whole database, treatments were indicated for 56 conditions and that incomplete records (i.e. records which do not show the indication of a drug nor the explicit indication of no drug use) represented 14.9%. The lack of this data showed a marked decrease with time, indicating the steady improvement in its collection. Table 3 also summarizes the observations regarding the accuracy of the minimum set of data collected by RNMR. Figure 1 - Establishment of regional RD registries in Italy. The year indicated refers to the year of institution of the registry. Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s609 Taruscio D et al Figure 2 - Nominal population coverage of the RNMR and notification flow. The year indicated refers to the institution of the regional registry. Notifications reported for the year 2012 refer to the first half of the year. Table III - Completeness and accuracy of the common dataset. Completeness (% missing)a Common data set Whole database Calendar years 2010-2011 Accuracy (110,841 records) (27,114 records) Calendar year 2012 (6 months) (9,913 records) Gender 0.0 0.0 0.0 Data is collected consistently among data sources according to usual identification procedures Date of birth 0.0 0.0 0.0 Data is collected consistently among data sources according to usual identification procedures Region of residence 0.1 0.1 0.0 Data is collected consistently among data sources according to usual identification procedures Diagnosis 0.0 0.0 0.0 Diagnoses are controlled and validated by the RRsb and their accuracy rely on the selection criteria for the centres to become FDC of the RD network Date of diagnosis 1.0 -- -- Inconsistencies among regions on the identification of the relevant diagnostic event and diagnostic centre. Centre of RD diagnosis 11.9 1.2 0.4 Inconsistencies among regions on the identification of the relevant diagnostic event and diagnostic centre. A centre may change name following reorganisation. Vital status ND ND ND c Uncertainties in this variable depend on the fact that the data sources of RRsb may not be fully aware of the reason why patients are lost to follow up. In the future, date of decease will be collected from death registries: this will result in a systematic and precise, although delayed, appraisal of this condition. Date of decease ND ND ND Expectedly good (when reported). In the future, date of decease will be collected from death registries: this will result in a systematic and precise, although delayed, appraisal of this condition. Date of disease onset 46.4 57.1 81.4 Uncertainties in this variable depend on i) lack of patient's recollection; ii) gradual appearance of unspecific symptoms over a long period. Symptoms could also not set on due to effective treatment following early diagnosis (e.g. following neonatal screening) Orphan drug used 14.9 10.7 4.6 The name of the active substance is communicated, but no standard catalogue or coding is used. Data completeness is measured as the proportion (%) of records without the indication of the value of the variable; calendar years refer to the date of diagnosis; b Regional registry; c ND = not determined a Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s610 The Italian RD Registry Preliminary results after the start of activity with full nominal coverage of the national territory Altogether, the valid records which are stored at present into RNMR are 110.841. This number corresponds to the overall diagnoses communicated to RNMR up to 30 June 2012 by RRs which have started their collection at different dates between 2000 and the end of 2011. The records referred to diagnoses made in the first 6 months of 2012, with RRs covering all the national territory, were 9,913. Although these features prevent, at present, any sound epidemiological estimate of rare diseases in Italy, some observations on the composition of the rare diseases notifications communicated to RNMR, may be of interest. Table IV shows the distribution, across the ICD 9-CM Chapters, of the diagnoses notified to the RNMR. The RDs under this surveillance system include conditions named individually and with group denominations. Altogether, the records reported at least one case of 485 conditions. All groups and subgroups mentioned in the MD were represented, making up 58,942 records, including 7,328 records of 137 pathologies mentioned as examples. Besides these, 296 individual RDs were represented with 51,899 records. Of these records, about 50% were made up by 15 most frequent diseases: achalasia, amyotrophic lateral sclerosis, behçet disease, bullous pemphigoid, chronic inflammatory demyelinating polyneuropathy, down syndrome, hereditary hemorrhagic telangiectasia, idiopathic central precocious puberty, keratoconus, Klinefelter syndrome, Lambert-Eaton syndrome, Marfan syndrome, mixed cryoglobulinemia, pemphigus, Turner syndrome. Twenty-nine diseases were represented with one record only. Discussion The European Commission Communication: "Rare diseases: Europe's challenge"2 and the subsequent Council Recommendation7 emphasize the strategic importance of Patient Registries in the field of RD. The national network of Centres, identified at regional and interregional level, and of Regional/Interregional Registries dedicated to RD, was successfully implemented in Italy following the MD and the agreements between the Government and the Italian regions. To date, the Italian RNMR is a surveillance system, with the the main objective of producing epidemiologic evidence on RD in Italy, and of supporting policy making and HS planning. This role of the RNMR has been confirmed by the draft National Plan on RD, recently proposed for public consultation by the Ministry of Health13. Considering the complexity of building such registries in a devolved system of responsibility for healthcare delivery, substantial efforts were necessary in various steps of RNMR development, especially at regional level where the supporting infrastructures had to be established. Table IV - Distribution, across the ICD 9-CM Chapters, of diseases notified to RNMR up to 30 June 2012. ICD 9-CM Chapters Percent records 1. Infectious and parasitic diseases 0.1 2. Neoplasms 5.0 3. Endocrine, nutritional, and metabolic diseases, and immunity disorders 17.4 4. Diseases of the blood and blood-forming organs 16.6 6. Diseases of the central nervous system and sense organs 26.0 7. Diseases of the circulatory system 4.3 9. Diseases of the digestive system 1.3 10. Diseases of the genitourinary system 0.6 12. Diseases of the skin and subcutaneous tissue 3.3 13. Diseases of the musculoskeletal system and connective tissue 5.5 14. Congenital anomalies 19.7 15. Certain conditions originating in the perinatal period 0.1 16. Symptoms, signs, and ill-defined conditions 0.0 Total 100 The strong legal base, its integration in the public health service and its connection with the dedicated national RD patient protection policy ensures the registry stability, comprehensiveness and population coverage. However, the need to cope with different levels of local resources, the slow responsiveness and limited flexibility typical of institutional processes as well as the need to rely on quality and comparable data made the implementation of the RNMR a slow and stepwise process, which is far from being concluded. The common data set agreed among the central and regional health authorities, is indeed the result of a selection of data, the collection of which could be sustainable, made comparable and be used to provide information coherent with the national scope of the RNMR, as distinct from the regional level responsibilities. During the gradual establishment of the Regional RD registries, which achieved nominal completion during 2011, a steadily increasing flow of data on RD patients was established from the RRs to the RNMR. Moreover, we could observe also a continuously increasing involvement of the operators of the RD registry system. To achieve this result, an important role was played by the dedicated training courses in the regions which do not have a proprietary Rare Diseases Registry, conducted in a systematic way by the experts of the RNMR. The preparation of the first Report on the RNMR activity9, in collaboration with the RRs, turned to be a powerful tool to review the operation of this complex system and to highlight the need for a number of critical improvements. The collection of the vital status and death date should be undertaken systematically. To this aim, the Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s611 Taruscio D et al RNMR is seeking access to the national database of death records. Moreover, the inconsistencies in the collection of the disease onset date and the adoption of improved definitions of the diagnostic event relevant to determine the date of diagnosis and the centre making diagnosis are being discussed. Finally a more accurate list of active substances is to be adopted. The procedures used to validate records and to control data completeness also should be better distributed between the RNMR and the RRs to make the data flow a smooth process. The actual coverage of the population depends on the quality and functions of the information systems developed at regional or interregional level. The different lengths of periods of operation of the RRs (ranging from about 1 to more than 10 years) result in different effectiveness of the registration process and only some regions collect data on RD patients using multiple data sources. Therefore, with the progressive improvement of RRs operations, the heterogeneity of the case reporting completeness will become less and less relevant. However, this issue has to be assessed and addressed appropriately. At present, therefore, the data currently stored in the RNMR represents the baseline for a continuous improvement of the national and RRs and to start a validation process through the comparison of the RNMR results with studies in other population groups. For an overall improvement of the Italian RD surveillance system, CNMR is promoting collaborations with National statistical services, clinicians, patient associations and other data sources. Moreover, additional opportunities for improvement will come from the participation of CNMR and other experts of the Italian RD network in other European and global initiatives, such as the European Platform for rare disease registries (EPIRARE: www. epirare.eu), the International Rare Disease Research Consortium, (IRDiRC: www.irdirc.org) and the Integrated Platform connecting databases, registries, biobanks and clinical bioinformatics for Rare Disease research (RDConnect:www.rd-connect.eu. G. Monasterio, Pisa, Tuscany Region) and Cecilia Berni (Regional Coordination of Rare Diseases, Tuscany Region), Lucia Borsellino and Salvatore Scondotto (Department of Health and Epidemiological Observatory, Sicily Region), Francesco Benedicenti (Provincial Coordination Centre for Rare Diseases, Bolzano Autonomous Province) and Paola Zuech (Provincial Epidemiological Observatory, Bolzano Autonomous Province), Paola Casucci and Maria Concetta Patisso (Regional Directorate of Health and Social Cohesion, Umbria Region), Domenico di Lallo (Public Health Agency, Latium Region), Maria Lucia Di Nunzio (Directorate General V, Molise Region), Annunziata Di Palma (Provincial Coordination Centre for Rare Diseases, Trento Autonomous Province), Matteo Volta and Maria Vizioli (Directorate General of Health and Social Policy, Emilia Romagna Region), Paola Facchin and Monica Mazzucato (Coordination Rare Diseases, Rare Diseases Registry, Veneto Region), Orazio Gabrielli (Salesi Hospital, Clinical pediatric, Marche Region), Roberto Della Casa ed Iris Scala (Coordination Centre for Rare Diseases, Campania Region), Gedeone Baraldo (Directorate General for Health, Lombardy Region) ed Erica Daina (Coordination Centre for Rare Diseases, Institute for Pharmacological Research "Mario Negri", Lombardy Region), Giandomenico Palka (Department of Biomedical Sciences, University Hospital of Chieti, Abruzzo Region), Dario Roccatello and Vittorio Modena (CMID, Centre of Research of Immunopathology and Rare Diseases; ASL TO2, S. Giovanni Bosco Hospital, Piedmont Region), Mirella Rossi (Regional Health Agency, Liguria Region), Domenico Tripaldi and Antonella Angione (Department of Health, Safety and Social Solidarity, Personal Services and the Community, Basilicata Region). References 1) 2) The Authors declare no conflicts of interest. National Rare Disease Registry collaborating group Giuseppina Annicchiarico and Ettore Attolini (Regional Coordination of Rare Diseases, Apulia Region), Antonello Antonelli (Department for Hygiene and Health and for Social Assistance of the Autonomous Region, Directorate General of Health, Sardinia Region), Rosalba Barone (Department of Health Protection and Health Policies, Calabria Region), Bruno Bembi and Laura Deroma (Regional Coordination Centre for Rare Diseases, Friuli-Venezia Giulia Region), Fabrizio Bianchi (Institute of Clinical Physiology CNR/Fondativo 3) 4) 5) 6) Posada de la Paz M, Villaverde-Hueso A, Alonso V, János S, et al. Rare Diseases Epidemiology Research Adv Exp Med Biol 2010; 686: 17-39. Communication from the Commission to the European Parliament, the Council, the European economic and social committee and the committee of the regions on rare diseases: Europe challenges. Commision of the European Communities. Available on line at http://ec.europa.eu/health/ph_threats/ non_com/docs/rare_com_en.pdf. Accessed on 15/01/2014. Griggs RC, Batshaw M, Dunkle M, Gopal-Srivastava R, et al. Rare Diseases Clinical Research Network: Clinical research for rare disease: opportunities, challenges, and solutions. Mol Genet Metab 2009; 96: 20-6. Cole JA, Taylor JS, Hangartner TN, Weinreb NJ, et al. Reducing selection bias in case-control studies from rare disease registries. Orphanet J Rare Dis 2011; 12: 6: 61. Luisetti M, Campo I, Scabini R, Zorzetto M, et al. The problems of clinical trials and registries in rare diseases. Respir Med. 2010; 104 (Suppl 1): S42-4. Webb SM, Santos A, Valassi E. The value of a European Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s612 The Italian RD Registry registry for pituitary adenomas: the example of Cushing's syndrome registry. Ann Endocrinol (Paris). 2012; 73: 83-9. 7) Council Recommendation of 8 June 2009 on an action in the field of rare diseases. The Council of the European Union. Available on line at: http://eur-lex.europa.eu/LexUriServ/ LexUriServ.do?uri=OJ:C:2009:151:0007:0010:EN:PDF. Accessed on 23/08/2013. 8) European Commission. Supporting rare diseases registries and providing a European Platform for rare diseases registration. Available on line at: http://ec.europa.eu/health/rare_diseases/ policy/registries/index_en.htm. Accessed on 28/08/2013. 9) Italian Ministry of Health. Decreto 18 maggio 2001, n. 279. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124. (GU n. 160 del 12-7-2001- Suppl. Ordinario n.180/L) (in Italian). Available at: http://www.iss.it/binary/cnmr/cont/DM2792001.1205943575.pdf. Accessed on 25/03/2014. 10) Conferenza Stato Regioni. Accordo tra il Ministro della Salute, le Regioni e le Province Autonome di Trento e Bolzano sui criteri di individuazione e di aggiornamento dei Centri Interregionali di riferimento delle malattie rare. (Repertorio Atti n 1485 dell'11 luglio 2002) (in Italian). Available at: http://www.iss. it/binary/cnmr/cont/STATOREGIONI2002.1205943700.pdf. Accessed on 25/03/2014. 11) Conferenza Stato Regioni. Accordo, ai sensi dell'articolo 4 del Decreto Legislativo 28 Agosto 1997, n. 281, tra il Governo, le Regioni e le Province Autonome di Trento e Bolzano sul riconoscimento dei Centri di coordinamento regionali e/o interregionali, di Presidi assistenziali sovraregionali per patologie a bassa prevalenza e sull'attivazione dei registri regionali ed interregionali delle malattie rare. (Repertorio 103/ CSR del 10 maggio 2007) (in Italian). Available at: http://www. iss.it/binary/cnmr/cont/STATOREGIONI2007.1205943700. pdf . Accessed on 25/03/2014. 12) Taruscio D. Il Registro Nazionale e i Registri Regionali/ interregionali delle Malattie Rare. Rapporto anno 2011. (Rapporti ISTISAN 11/20). Roma: Istituto Superiore di Sanità; 2011 (in Italian). Available on line at: http://www. iss.it/publ/index.php?lang=1&id=2529&tipo=5. Accessed on 15/11/2013. 13) Italian Ministry of Health. Piano Nazionale Malattie Rare 2013-2016. Available on line at: http://www.salute.gov.it/ imgs/C_17_pagineAree_3296_listaFile_itemName_0_file. pdf. Accessed on 15/01/2014. Correspondence: Domenica Taruscio Italian National Centre for Rare Diseases Istituto Superiore di Sanità Viale Regina Elena, 299 00161, Rome, Italy e-mail: domenica.taruscio@iss.it Blood Transfus 2014; 12 Suppl 3: s606-13 DOI 10.2450/2014.0064-14s s613 REVIEW The Italian National Plan for Rare Diseases Maria Elena Congiu Italian Ministry of Health, Rome, Italy Introduction Italy was one of the first Member States (MS) in the European Union (EU) to regulate the field of rare diseases (RD). Since 2001, many initiatives were carried out at central and regional level. The development of a national plan or strategy for RD stems from the necessity to fulfill the EU Commission Recommendation to MS to adopt national plans or strategies for RD by the end of 20131. However, the adoption of a systematic measure, logical and coherent with planned strategies and actions at all levels, was demanded by national stakeholders in the field of RD. The first version of the document was drafted by the General Directorate of Planning at the Ministry of Health (MoH) in collaboration with small groups of experts. It was submitted to all the stakeholders (patient and family organisations, healthcare professionals and professional bodies) during a brief consultation process. The document considered also previous requests from the National Board of Patients with RD (http://www.cndmrinsieme.it/) and patient organisations (Federation of the Organisations of the Italian Patients with RDs - UNIAMO and Italian Movement of Rare Patients - MIR). These requests had been previously presented at the final national conference of the EUROPLAN project in 20122. The Italian legal framework on rare diseases Coming into force just before the approval of the Regulation (EC) n. 141/2000 of the European Parliament and the Council on orphan medicinal products3, the Italian legislation in the field of RD derives from the willingness to combine the organisation of healthcare assistance with all aspects related to the rights of citizens affected by RD. Specifically, the Legislative Decree n. 124/19984 introduced the new discipline on exemption from co-payment for health services nationwide and led to the adoption of the Ministerial Decree (MD) n. 279/20015, which is the first regulatory act in the field of RD. The decree identified a list of life-threatening or chronically debilitating diseases with both a high level of complexity of care and a prevalence of not more than 5 in 10,000 inhabitants, in accordance with the EU definition. The diseases included in the above-mentioned list are formally called as "rare" and totally exempted from the co-payment for outpatients benefits provided by the National Health Service (NHS) for diagnosis and treatment. When necessary for patient's diagnosis, also genetic testing to blood relatives is delivered without any charge. Medicinal products are not the subject of the decree and are provided in accordance with Italian Medicines Agency (Agenzia Italiana del Farmaco, AIFA) classification. Moreover, the MD 279/2001 establishes a specific network for RD consisting in both accredited health facilities identified by Regions, which are responsible for the diagnosis and treatment of RD and the systematic collection of data concerning RD resulting in the National Registry of Rare Diseases (NRRD) at the Italian National Institute of Health (Istituto Superiore di Sanità, ISS)6. The effectiveness of MD 279/2001 was confirmed after the approval of the Constitutional Law n. 3/2001 that conferred to the Regions the entire responsibility for the organisation of the healthcare assistance, the planning and management of their own healthcare activities, as well as the provision of healthcare services to the population through Local Health Units. The central State (namely the MoH) has the responsibility to define the general principles and priorities and to establish the national healthcare entitlements (Essential/ Basic Levels of Healthcare Assistance, LEA), which are financed by general taxation. Moreover, the MoH is required to ensure that LEA are provided to all citizens and that the Regions have the appropriate financial resources. Finally, the main guiding principles of the NHS are those of universality, equity and solidarity and the LEA provided to people with RD are the same, but free, national healthcare entitlements which are guaranteed to all citizens according to criteria of effectiveness, appropriateness and quality, as well as quantitative and qualitative standards and appropriate way of delivery. On the other side, Regions are allowed to provide further services, as far as they can cover the costs with their own economic means. In recent years, many Regions decided to supply "extra-LEA services" to their population. Among the "extra-LEA services", some Regions include free access to specific further benefits for people suffering from a RD, such as some medicinal products currently delivered with fee but also healthcare assistance to further diseases not currently included in the national list of RD. Blood Transfus 2014; 12 Suppl 3: s614-6 DOI 10.2450/2014.0337-13s s614 © SIMTI Servizi Srl Italian Plan on rare diseases: role of Ministry of Health The contents of the draft of the National Plan for Rare Diseases The first part of the National Plan for Rare Diseases (NPRD) recalls the European and national legislation and a description of the main areas of intervention: LEA; the organisation of the system and its components (the National network for RD, the NRRD, the Congenital Malformations Registers (CMR), and Disease-specific registers, the National Board of Regional Health Authorities on RD, biobanks, coding and classification of RDs); the healthcare and pharmaceutical pathways for RD patients; the cross border healthcare; the role of the patient alliances; research; training and education of professionals, and information; prevention activities. It is important to highlight that any social intervention is not included in the current NPRD. The second part of the NPRD "Objectives and monitoring" links each of the above areas of interventions with specific actions for the 3-year period. The network organisation, set up with the MD 279/2001, deserves special consideration. Despite the exclusive competence of the Regions established by the aforementioned Constitutional Law, a supra-regional level is recommended for very RD ensuring follow-up activities to be performed near the patient residence. An inter-regional organisation may allow different but appropriate treatment of patient needs according to the level of know-how of each health professional. The model aims at guaranteeing both high specialised functions and assistance to general needs, available at the healthcare district level. Identified units (preferably hospital units) are the national network hubs, specifically detected among those who can provide documentary evidence of expertise in diagnosis and care of a specific rare disease or groups of RD, as well as suitable equipment and complementary services to assist in emergencies and to perform molecular, genetic and biochemical diagnoses. These facilities can be guaranteed also by means of functional relations with external services, such as genetics centres and become integral part of the RD network. Furthermore, the identified units are required to comply with the clinical protocols set up in accordance with the clinical guidelines issued by the scientific societies. In addition, all units must also cooperate with general practitioners and local services to provide personal, comprehensive and continuing care to patients. Finally, the national network must fulfill the EU requirements in order to comply with the Council Recommendation on an action in the field of rare diseases (2009/C 151/02)7 adopted on June 8th, 2009 along with both the EUCERD Recommendation8 concerning the quality criteria for Centers of Expertise (CEs) in Member States and the implementation of European Reference Networks (ERNs)9. All its identified units, firmly included within the regional networks of care, must be able to perform the duties expected from European CEs. In the assessment process of these units, Regions can use multi-stakeholder opinions, including patient organizations; benchmarks and indicators should cover processes, outcomes and impacts, such as patient reported outcomes. An appropriate governance is ensured through the establishment of a National committee, involving the competent Ministries, the Regions and AIFA, as well as the National Agency for Regional Health Services (Agenzia Nazionale per i Servizi sanitari regionali, Age.Na.S.) and patient alliances. The Committee has the task to both define the main strategies for diagnosis and care, research and social promotion, adapting them to the specific economic resources and to optimise the most appropriate monitoring actions. All services and national healthcare entitlements, including those regarding RD, are currently funded by general taxation and the NHS financial budget is yearly distributed by the central Government to the Regions. The specific expenditure for RDs is difficult to quantify. However, since medicinal products are among the major invoices of expenditure, an accurate medicinal products' accountability may help to predict a great part of the real expense for the NHS. In recent years, the situation has become more complex and more heterogeneous among Italian Regions, due to the dramatic differences of Regional Health Services budgets. In order to address this scenario, the Central Government has enforced a series of so-called Budgetary Balance Plans aimed at solving the problems of insufficient financial coverage for services provided in some "very critical Regions". The Plans introduced substantial budgetary limits and measures to contain their healthcare cost levels and trends. As a consequence, many Regions undergoing a Budgetary Balance Plan have been forced to cancel the extra-LEAs services they were previously providing, including services for people suffering from RD. Conclusions The MoH is aware that expectations of the main stakeholders, in particular of patient associations, might be excessive compared to the actions proposed in the NPRD draft, mainly because of the limitation of financial resources. The possibility to further allocate dedicated funds for RD depends on the overall evaluation of the central Government. Indeed, the draft of the NPRD suggests to include RD among the performances that are being verified by the national committee for the evaluation of the provision of LEA. Blood Transfus 2014; 12 Suppl 3: s614-6 DOI 10.2450/2014.0337-13s s615 Congiu ME However, the draft of the NPRD specifically considers the efficiency and the effectiveness of the general organisation and the national network to minimize the consequences of budgetary limits. Moreover, it emphasises the importance of a strict cooperation and exchange of experiences and best practices among all the identified regional expert units coordinated at a supra-regional level. 5) 6) 7) 8) Keywords: Essential Levels of Assistance (LEA), extra LEA services, national network, budgetary balance plans. The Author declares no conflicts of interest. 9) Decreto ministeriale 18 maggio, n. 279 "Regolamento di istituzione della rete nazionale delle Malattie are e di esenzioni dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124" [in Italian]. SO alla GU n. 160 del 12 luglio 2001, N. 180/L. Taruscio D, Kodra Y, Ferrari G, et al. The Italian Registry on Rare Diseases. Blood Transfus 2014; 12 (Suppl 3): s606-13. Council Recommendation on an action in the field of rare diseases. 2009/C 151/02. Recommendations on Quality Criteria for Centres of Expertise for Rare Diseases in Member States. European Union Committee of Experts on Rare Diseases (EUCERD) http:// www.eucerd.eu. Accessed on 24/10/2011. Recommendations on Rare Diseases European Reference Networks (RD ERNS). European Union Committee of Experts on Rare Diseases (EUCERD), 31 January 2013. Available at: http://www.eucerd.eu/. Accessed on 18/12/2013. References 1) 2) 3) 4) Communication from the Commission to the European Parliament, the Council, the European economic and social Committee of the Regions on Rare Diseases: Europe's challenge. Bruxelles, 11.11.2008. COM (2008), 679 final. Conferenza Nazionale EUROPLAN in ITALIA - REPORT FINALE [in Italian]. Available at: http://www.europlanproject. eu/_newsite_986989/Resources/docs/EUROPLAN2010_ FINALReport_Italy.pdf. Accessed on 15/02/2014. Regolamento del Parlamento europeo e del Consiglio concernente i medicinali orfani [in Italian].(CE N. 141/2000) . Decreto Legislativo 29 aprile 1998, n. 124 "Ridefinizione del sistema di partecipazione al costo delle prestazioni sanitarie e del regime delle esenzioni, a norma dell'articolo 59, comma 50, della L. 27 dicembre 1997, n. 449" [in Italian]. Pubblicato nella G.U. 30 aprile 1998, n. 99 Correspondence: Maria Elena Congiu Ministry of Health Via Giorgio Ribotta n. 5 00144 Roma, Italy e-mail: me.congiu@sanita.it Blood Transfus 2014; 12 Suppl 3: s614-6 DOI 10.2450/2014.0337-13s s616 REVIEW Piedmont and Aosta Valley inter-regional network in the context of the Italian National Network for rare diseases Simone Baldovino 1,2, Elisa Menegatti 2, Vittorio Modena 1, Maria Maspoli 3, Flavia Avanzi 3, Dario Roccatello1,2 1 CMID - Centre of Research of Immunopathology and Rare Diseases, Coordinating Centre of Piedmont and Aosta Valley Network for Rare Diseases, St. G. Bosco Hospital and University of Turin, Turin; 2Department of Clinical and Biological Sciences, University of Turin, Turin; 3Piedmont Regional Health Department, Turin, Italy Introduction The Italian regulatory framework on RD In Europe rare diseases (RDs) are defined as "diseases with a prevalence in the European Union (EU) population of less than 5 per 10,000". This definition includes a large group of more than 6,000 diseases, 90% of which are genetically determined and which potentially involve all organs1. RDs are therefore a very heterogeneous group as far as both clinical and epidemiological aspects are concerned. There are in fact RDs with less severe clinical manifestations and others with important ones which can compromise the quality of life and the life expectancy. Furthermore, some RDs have a prevalence approaching to the 5 per 10,000 limit and therefore affect a significant number of patients. Indeed, from the June 2005 to the December 2013 the Piedmont and Aosta Valley interregional register for RDs collected 21,062, with an estimated overall prevalence of RD of 45 patients on 10,000 inhabitants. Moreover half of the patients registered are affected by less than 20 diseases or groups of diseases (Table I) that represent the most important burden of care for the regional healthcare systems. On the other hand there are several with a much lower prevalence affecting a very small number of patients2. These latter often lack of timely and correct diagnosis and adequate treatment. Moreover, the world-wide orphan drug policies are associated with unacceptably high costs of newly developed drugs and inaccessibility of previously available drugs which become unavailable over time because of limited production by pharmaceutical industries3. Finally, despite the low prevalence of each disorder, the number of rare disease is fairly high. The European Commission reports that RDs affect a total of 6-8% of the population. Due to all these problems, and to the fact that RDs are often chronic and invalidating or cause early mortality, they represent a significant public health matter of concern in many countries. In Europe the problem of RDs was addressed for the first time by The Program of Community Action on rare diseases 1999-20034. Italy was one of the first European countries to develop specific regulations regarding RDs5. Since 1998, the three year National Health Plans has been issued, intended as national-wide instructions. This document indicated RD as a priority for National Health Service (NHS). Moreover, in 2001, the Ministry of Health Table I - Distribution of diseases covering 50% of reported diseases in the Piedmont and Aosta Valley Rare Diseases Registry. Rare disease or group n. of patients % Cumulative % Hereditary coagulation disorders 1,245 5.9% 5.9% Lateral amyotrophic sclerosis 997 4.7% 10.6% Hereditary anaemias 981 4.7% 15.3% Progressive systemic sclerosis 888 4.2% 19.5% Congenital metabolic iron disorders 745 3.5% 23.1% Neurofibromatosis 607 2.9% 25.9% Undifferentiated connective tissue disease 548 2.6% 28.5% Sarcoidosis 487 2.3% 30.9% Chronic idiopathic thrombocytopenic purpura 474 2.3% 33.1% Antiphospolipids syndrome 451 2.1% 35.2% Keratoconus 419 2.0% 37.2% Idiopathic pulmonary fibrosis 399 1.9% 39.1% Genetic arrhytmias 359 1.7% 40.8% Down syndrome 358 1.7% 42.5% Disorders of aminoacids metabolism and transport 356 1.7% 44.2% Arnold-Chiari syndrome 337 1.6% 45.8% Muscular dystrophies 332 1.6% 47.4% Lichen sclerosus et atrophicus 289 1.4% 48.8% Bullous pemhigoid 271 1.3% 50.1% Blood Transfus 2014; 12 Suppl 3: s617-20 DOI 10.2450/2014.0055-14s © SIMTI Servizi Srl s617 Baldovino S et al comprehensively addressed the issue of RDs with a specific Decree (DM 279/2001)6. DM 279/2001 established the national network for RDs and cost exemptions for related health service provisions for a consistent cohort of RDs5. DM 279/2001 also established a National Registry of RDs to be kept at the National Institute of Health7. A few months after the publication of DM 279/2001, a Constitutional Law (Constitutional Law 3/2001) reformed Title V of the Italian Constitution. Several decisions on health, including RDs, were consequently delegated to the regional administrations. As a result the development of networks for RDs was quite different among the various Italian Regions. Prior to DM 279/2001, other national laws had dealt with specific RDs, such as cystic fibrosis and hereditary haemorrhagic diseases. For instance, as addressed in other papers in this issue, a network of reference centres for haemophilia and related disorders was already operating before 2001. The inclusion of these previously existing network for specific RDs was one of the problem faced by regional administrations in implementing DM 279/2001. and the scientific relevance of each centre. In some regions, such as in Lombardy, the reference centres are subject to periodic re-evaluation by a local coordinating Centre which evaluate all the above mentioned parameters. Some regions have made inter-regional agreements. Therefore there are two formally recognized interregional areas. The first one is made up of Piedmont and Aosta Valley. The second includes Veneto, the Autonomous Provinces of Trento and Bolzano, FriuliVenezia Giulia, Emilia-Romagna, Liguria, Puglia and Campania13,14. The regions involved in the two inter-regional networks share the same policy for the accreditation of reference centres, the information system for the management of the Registry of RDs, treatment protocols, and standards of care. Finally, in 2006, all the Italian Regions and Autonomous Provinces joined in an inter-regional network for RDs with the purpose of a joined approach to common issues such as home administration of drugs for metabolic diseases and telemedicine. The regional RD networks: examples from the current experiences The Piedmont and Aosta Valley Inter-regional Network for RDs was developed in 2008. It is the result of the union between two previously separate systems, i.e., the Piedmont regional network for RDs, founded in 2004, and the system for RDs in the Aosta Valley region14,15. It is a decentralised organisational model based on the active involvement of all the professionals operating in the public health system of the two regions. The Piedmont Network for RDs was created to guarantee equal opportunities of assistance throughout the Region, develop diagnostic and treatment protocols to be shared among physicians, provide information on regional health organization and legislation to caregivers and patients' associations. It has also be created to collect data for epidemiological studies through the Regional Registry, allowing to identify both critical problems (including delays in diagnosis and care) and areas of possible investment of resources. The Inter-Regional network for RDs was designed to develop a model of healthcare assistance that would guarantee the quality of diagnosis (including genetic analysis) in centres with proven expertise. More importantly, it aims to offer appropriate healthcare to patients as close as possible to their place of living. Thus, the Piedmont and Aosta Valley model of decentralised network for RDs is unique among the Italian experiences. Unlike most networks in other Italian regions, the Piedmont and Aosta Valley network involves all the healthcare facilities within the regions, thus giving all the specialists the opportunity to be The network of RDs was implemented following different organisation systems in various Italian regions. In some of the smaller regions with a small population, such as Marche region, one or two reference centres paediatric and adult patients were established8. In other regions, such as Veneto, reference centres for homogeneous nosological groups of diseases were set up. Moreover, these regions have created a network for local care in order to provide a day to day patients take in charge9. A similar model was applied by the Tuscany region where a diagnostic network made up of reference centres and a care network interact with each other to manage the patient's healthcare needs10. Contrarily, the Lombardy Region applied a model based on establishing reference centres on which insist all the aspects of the diagnosis and care of the patient11. A final model is the "hub and spoke model" which is implemented, for example, by Emilia Romagna. This model bases on concentrating the more complex cases in a limited number of centres (hubs). The clinical activity of the hub is highly integrated through functional connections with that of the peripheral health centres (spokes)12. All the above models are based on establishing reference centres which are entrusted for the diagnosis of the disease and to supply the appropriate therapeutic prescription. In most cases the reference centres were established considering the number of treated patients The Piedmont and Aosta Valley network for RDs decentralised model Blood Transfus 2014; 12 Suppl 3: s617-20 DOI 10.2450/2014.0055-14s s618 Piedmont and Aosta Valley network of rare diseases involved in treating patients with RDs. A network as widespread as that of Piedmont and Aosta Valley requires a Coordinating Centre and a monitoring system to evaluate the appropriateness of diagnoses and therapy. The Coordinating Centre was established in 2004 and, since 2005, it has been supported by a regional technical board15,16. The coordination of clinical activities for RDs throughout the two regions is guaranteed by Working Groups for RDs operating in all heath institutions of the public regional systems that act in collaboration with the Coordinating Centre. The supply of drugs for treatment of patients suffering from RDs is ensured by a wide network of hospital pharmacies. These provide all the needed medicinal products including drugs not currently available nationwide or still under investigation in selected cases, and off-label agents. In addition, they also produce galenic preparations which are essential for the treatment of specific RD. The network of collaboration for the productions of galenics among hospital pharmacies is, to date, unique in Italy17. Another peculiarity of the network of RDs in Piedmont and Aosta Valley is the presence of multidisciplinary working groups, called Consortia, dedicated to specific RDs or to RDs with similar therapeutic or diagnostic problems. They operate throughout the two Regions and are composed of volunteer clinicians, other health professionals, and patient's associations. Consortia main goal is the development of shared protocols and clinical pathways18,19. The Consortia deal with the most prevalent RDs, or with the ones that are characterised by specific issues such as the cost of treatment or the lack of reliable data regarding treatment effectiveness and efficacy. Twenty two Consortia were active at the end of 2013. Fourteen disease-specific or disease groupspecific clinical pathways have been implemented to date (Table II). In addition to developing the clinical pathways, the Consortia also identify, if needed, Centres of Expertise. A Centre of Expertise must have proven diagnostic and therapeutic experience as well as availability of appropriate support structures and complementary services, such as laboratory and imaging facilities, emergency department availability, etc. The main aims of the centres of expertise are supporting the local health authorities in the care of patients, and providing specialised training to the health professionals. To date, Centres of Expertise have been established for amyotrophic lateral sclerosis, for syringomyelia, and Arnold-Chiari syndrome. Lastly, an important activity of the Consortia is the production of clinical and epidemiological studies on RDs19-24. The Piedmont and Aosta Valley network for rare Table II - Multidisciplinary working groups (so-called Consortia) at December 31, 2013. In bold are indicated the implemented clinical pathways. Adrenogenital Syndromes Amyloidosis Anti-phospholipid Syndrome Arnold Chiari Syndrome, Syringomyelia Autoimmune peripheral neuropathies Autoimmune Polyendocrinopathies Bladder Pain Syndrome Congenital Osteodystrophy Hereditary coagulation Disorders Hereditary retinal dystrophy Klinefelter Syndrome Neurofibromatosis Lysosomal Storage Diseases Porphyrias Prader-Willi Syndrome Precocious Puberty Primary Lymphedema Primary Pulmonary Hypertension Systemic Sclerosis Transition from childhood to adulthood Undifferentiated Connective Tissue Disease Uveitis diseases is also involved in international collaborations, such as the network International Conference for Rare Diseases and Orphan Drugs, Europlan initiatives promoted by the National Institute of Health, by the European Community, and by Eurordis, and in the rare diseases coding promoted by World Health Organization and by Orphanet. Conclusion The network of RDs in Piedmont and Aosta Valley is a unique experience in the Italian scenario. An analysis of 10 years of activity allows us to give a largely positive assessment. This widespread network has improved the clinicians' knowledge of the specific RD. Moreover, the clinical activities of the Consortia and of the Network of Hospital Pharmacies allowed to provide appropriate cares to patients and to limit both the costs and the therapeutic healthcare mobility toward other regions. Authorship contributions Simone Baldovino and Elisa Menegatti participated equally to the first draft of the paper. Keywords: rare diseases, regional policies, Public Health, healthcare. The Authors declare no conflict of interest. Blood Transfus 2014; 12 Suppl 3: s617-20 DOI 10.2450/2014.0055-14s s619 Baldovino S et al References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) Taruscio D, Cerbo M. Rare diseases: general principles, specific problems, and health interventions. Ann Ist Super Sanita. 1999; 35: 237-44. Prevalence of rare diseases: Reference data listed in order of decreasing prevalence or number of published cases. Available at: http://www.orpha.net/orphacom/cahiers/docs/GB/ Prevalence_of_rare_diseases_by_decreasing_prevalence_or_cases. pdf. Accessed on 27/02/2014. Murphy SM, Puwanant A, Griggs RC et al. Unintended effects of orphan product designation for rare neurological diseases. Ann Neurol 2012; 72: 481-90. Programme of Community Action on Rare Diseases (19992003) Decision No 1295/99/EC of the European Parliament and of the Council of 29 April 1999 (O.J. n° L 155 of 22.06.1999, p. 1) Available at: http://ec.europa.eu/health/ archive/ph_overview/previous_programme/rare_diseases/ raredis_wpgm99_en.pdf (accessed on 07/04/2014) Taruscio D, Capozzoli F, Frank C. Rare diseases and orphan drugs. Ann Ist Super Sanita; 2011; 47: 83-93. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'articolo 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124). Decreto No. 279 (18/05/2001). Available at: http://www.iss.it/binary/cnmr/ cont/DM279-2001.1234897572.pdf. Accessed on 07/04/2014. Taruscio D, Kodra Y, Ferrari G, et al. The Italian National Rare Disease Registry. Blood Transfus. 2014; 12 (Suppl 3): s606-13. Individuazione del Centro regionale di riferimento per le malattie genetiche e/o rare. Deliberazione della G.R. No. 2236 ME/SAN (25/09/2001). Available at: http://www.iss.it/binary/ ccmr/cont/20010925_DGR2236.pdf. Accessed on 07/04/2014. Individuazione dei presidi regionali di riferimento per le malattie rare. DGR No.204 (08/02/2002). Available at: http:// www.iss.it/binary/ccmr/cont/20020802_DGR204.pdf. Accessed on 07/04/2014. "Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'art. 5, comma 1, lettera b del D.Lgs. 124/98" - Individuazione presidi regionali. DGR No. 570 (14/06/2004) - D.M. 279/2001. Available at: http:// www.iss.it/binary/ccmr/cont/20040614_DGR570.pdf Accessed on 07/04/2014. DGR n. 7/7328. Individuazione della Rete per la prevenzione, la sorveglianza, la diagnosi, la terapia delle malattie rare. Available at: http://www.iss.it/binary/ccmr/cont/20011202_ DGR7_7328.pdf. Accessed on 07/04/2014. Hub & Spoke Emofilia Deliberazione della Giunta Regionale No.1267 (22/07/2002). Available at: http://www.iss.it/cnmr/ ccmr/regi/cont.php?id=113&lang=1&tipo=17&regi=5. Accessed on 07/04/2014. Approvazione dello schema di convenzione tra la Regione autonoma Valle d'Aosta e la Regione Piemonte per la realizzazione di un Centro interregionale di coordinamento per le malattie rare nonché di un Registro interregionale delle malattie rare, nell'ambito della rete sanitaria interaziendale ed interregionale prevista dall'accordo approvato con deliberazione della Giunta regionale n. 1692/2002 e di modificazione alla deliberazione della Giunta regionale n. 4054/2006. DGR No. 234 (01/02/2008). Available at: http:// www.iss.it/binary/ccmr/cont/20080201_DGR234.pdf. Accessed on 07/04/2014. Accordo tra Regione del Veneto, Regione Friuli Venezia Giulia, Provincia Autonoma di Bolzano e Provincia Autonoma di Trento per la realizzazione dell'area vasta nel campo delle 15) 16) 17) 18) 19) 20) 21) 22) 23) 24) malattie rare. Individuazione dei Centri Interregionali di Riferimento dell'area vasta per le Malattie Rare. DGR No. 2046 (03/07/2007). Available at: http://www.iss.it/binary/ccmr/ cont/20070703_DGR2046.pdf. Accessed on 07/04/2014. Individuazione della rete regionale per la prevenzione, la sorveglianza, la diagnosi, la terapia delle malattie rare e costituzione c/o l'ASL 4 di Torino del Centro regionale di coordinamento. DGR Deliberazione della Giunta Regionale No. 22-11870 (02/03/2004) Available at: http://www.iss.it/ binary/ccmr/cont/20040302_DGR22_11870.pdf. Accessed on 07/04/2014. Regolamento di istituzione della rete nazionale delle malattie rare e di esenzione dalla partecipazione al costo delle relative prestazioni sanitarie, ai sensi dell'art. 5, comma 1, lettera b), del decreto legislativo 29 aprile 1998, n. 124". Integrazione disposizioni. DGR No. 38-15326 (12/04/2005). Available at: http://www.malattierarepiemonte.it/15326.php. Accessed on 07/04/2014. Crosasso P, Mosso B, Peila E et al. Percorso gestionale standardizzato dalla prescrizione all'erogazione di galenici magistrali per pazienti affetti da malattie rare ed allestiti presso le farmacie ospedaliere di Piemonte e Valle d'Aosta. Giornale Italiano Farmaci a Clinica 2012; 26: 389-397. Ciaramitaro P, Baldovino S, Roccatello D, et al. Chiari and Syringomyelia Consortium: a model of multidisciplinary and sharing path for rare diseases. Neurol. Sci. 2011; 32 (Suppl 3): S271-3. Rete regionale delle malattie rare: Linee guida per la definizione dei Gruppi Tecnici e dei Centri Esperti. DGR No. 36-5284 (29/01/2013). Available at: http://www.regione. piemonte.it/governo/bollettino/abbonati/2013/08/siste/00000201. htm. Accessed on 07/04/2014. Bertero MT, Bazzan M, Carignola R et al. Antiphospholipid syndrome in northwest Italy (APS Piedmont Cohort): demographic features, risk factors, clinical and laboratory profile. Lupus. 2012; 21: 806-9. Sciascia S, Roccatello D, Bertero MT et al. 8-isoprostane, prostaglandin E2, C-reactive protein and serum amyloid A as markers of inflammation and oxidative stress in antiphospholipid syndrome: a pilot study. Inflamm. Res. 2012; 61: 809-16. Bazzan M, Vaccarino A, Stella S et al. Thrombotic recurrences and bleeding events in APS vascular patients: a review from the literature and a comparison with the APS Piedmont Cohort. Autoimmun Rev. 2013; 12: 826-31. Rossi D, Mansouri M, Baldovino S, et al. Nail fold videocapillaroscopy in mixed cryoglobulinaemia. Nephrol. Dial. Transplant. 2004; 19: 2245-9. Mereuta OM, Baldovino S, Errichiello E, et al. Systemic AA amyloidosis as a unique manifestation of a combined mutation of TNFRSF1A and MEFV genes. Amyloid. 2013; 20:122-6. 10). Correspondence: Dario Roccatello CMID - University Centre of Immunology and Documentation on Rare Diseases, Coordinating Centre of Piedmont and Aosta Valley Network for Rare Diseases P.zza del Donatore di Sangue 3 10154 Torino, Italy e-mail: dario.roccatello@unito.it Blood Transfus 2014; 12 Suppl 3: s617-20 DOI 10.2450/2014.0055-14s s620 ORIGINAL ARTICLE Centres of Expertise and European Reference Networks: key issues in the field of rare diseases. The EUCERD Recommendations. Domenica Taruscio1, Amalia E. Gentile1, Teresinha Evangelista2, Rosa G. Frazzica1, Kate Bushby2, Antoni Moliner Montserrat4 1 Italian National Centre for Rare Diseases, Istituto Superiore di Sanità, Rome, Italy; 2Institute of Genetic Medicine, International Centre for Life, Newcastle upon Tyne, United Kingdom; 3Directorate of Public Health and Risk Assessment, European Commission, Luxembourg, Luxembourg Background. Rare diseases, because of their intrinsic characteristics - large number of disorders and syndromes, low individual prevalence, severity, often limited information, lack of therapies - can benefit from collaboration and sharing of expertise while maximising the limited resources available for these conditions. Therefore, the development of Centres of Expertise (CEs) and European Reference Networks (ERNs) in this field is crucial. The European Union Committee of Experts on Rare Diseases (EUCERD) has been charged to assist the European Commission with the preparation and implementation of activities in the field of rare diseases in Europe. In particular, EUCERD has assisted the EC in drawing up the recommendations issued in the Commission Communication and in the Council Recommendation. In this paper the authors focus on the EUCERD Recommendations on CEs and one on ERNs. Materials and Methods. Recommendations on CEs and ERNs are the result of two different processes, developed through iterative reviews and discussions at workshops and EUCERD meetings, and according to the European Union documents. Results. EUCERD has issued two complementary Recommendations, one on CEs (2011) and a second on ERNs (2013). Both address multiple targets (from Member States to Centres, and patient organisations), with the objective of helping them define and organise CEs and ERNs. Conclusions. The establishment, designation, financial support, and evaluation of CEs throughout Europe allow RD patients and local health care providers to identify high-quality specialised services that can simplify disease management and improve patients' care. The EUCERD Recommendations are useful instruments to help and guide stakeholders in the development of CEs and ERNs and thus ensure equity of access to services and care for rare diseases patients across Europe. Keywords: rare diseases, Centres of Expertise, reference networks, public health, policy. Introduction Rare Diseases (RDs) are defined in Europe as those that affect fewer than 5 in 10,000 people. They have specific characteristics as a low prevalence in the population, a multitude of different diseases and syndromes, the lack of general awareness, the difficulty in diagnosing and, for most of them, the lack of effective therapies. These conditions make them an exceptional field for collaboration and sharing of expertise. RDs represent one of the best examples where European cooperation can be a strong added value. Furthermore, only through the strengthening of international collaboration, it will be possible to maximise the scarce resources devoted to RDs and, at the same time, deliver the best quality of care to the RD patients. Therefore, the development of Centres of Expertise (CEs) and European reference networks (ERNs) in RDs is fundamental. In November 1993, the European Commission (EC) published a Communication1, defining the framework for action in the field of public health and describing the role of Community Institutions and of Member States (MSs). After this publication, the EC opened a wide consultation in the European Union (EU) on public health issues. In December 1993, experts were invited by the EC to submit proposals describing how they would seek to formulate draft policy proposals in some of the areas indicated in the framework document. In consultation with the Commission, five priority areas were identified, among them there was also "an EU programme for management of rare diseases". It is worth noting that, even at that early time, the experts recommended "a system whereby the Commission might seek to encourage identification of centres of expertise on RDs and support the establishment Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0026-14s © SIMTI Servizi Srl s621 Taruscio D et al of networks for the development of research in appropriate fields". They underlined that RD "focal points (CEs on RD and networks with a central secretariat), should be identified, and the existing structures concerned with RDs within the MSs should form the backbone of the focal points2". More recently, the need for the development of CEs and ERNs in the field of RDs has been highlighted in several EU documents3-5, as a means of organising effective care for the thousands of heterogeneous RDs affecting patients scattered across Europe. Moreover, the Recommendations6 of the European Project for Rare Diseases National Plans Development (EUROPLAN www.europlanproject.eu) has reinforced the Council Recommendations4 and has underscored the importance of MSs to identify national or regional CEs, to define good practices for their designation and evaluation, and to encourage their participation in ERNs. Between 2004 and 2013, the European Union Committee of Experts on Rare Diseases (EUCERD7 www.eucerd.eu) - formerly the European Commission's Rare Diseases Task Force (RDTF) - was mandated to assist the EC with the preparation and implementation of community activities in the RDs field. In particular, EUCERD has assisted the EC in drawing up Recommendations, including those concerning CEs and ERNs for RDs, deriving them from the Commission Communication3 and the Council Recommendation4. EUCERD was composed of 51 members: experts from MSs, current and former RD research project leaders, representatives from relevant international organisations (DG SANCO, DG Research, DG Enterprise, EuroStat, EMA, WHO, OECD), pharmaceutical industries, and representatives of patient organisations. EUCERD has issued five Recommendations on the following areas: - Quality Criteria for CEs for RDs in MSs (October 2011)8; - Informed decisions based on the Clinical Added Value of Orphan Medicinal Products (CAVOMP) (September 2012)9; - ERNs for RDs (January 2013)10; - RD Patient Registration and Data Collection (June 2013a)11; - Core Indicators for RD National Plans/Strategies (NP/S) (June 2013b)12. Materials and methods The elaboration of the EUCERD Recommendations on CEs and ERNs was based upon the results of concepts defined by the High Level Group on health care and medical services (HLG)13, EU projects documents6, meetings with experts and other stakeholders, several reports investigating the state-of-the-art in the field of RDs, and on the previous work of the RDTF/EUCERD group14-19. In particular, the legal aspects associated with the Recommendations, as well as the political background, were established by the Commission Communication3, by the Council Recommendation4 and by the "Directive on the application of patients' rights in cross-border healthcare" (CBHCD)5. All draft Recommendations were elaborated by the EUCERD Scientific Secretariat, were sent to EUCERD members for comments, and the wording of the recommendations was discussed in dedicated workshops. The revised draft of the Recommendations was then submitted to EUCERD members for final approval prior to their meeting, where the Recommendations were unanimously adopted by the Committee. Results The main results concern the publication of the EUCERD Recommendations on CEs and ERNs, which are complementary, as they are elucidated below. They address numerous targets: MSs, the EC, other EC initiatives (e.g. projects and joint actions, Cross-Border Healthcare Expert Group, EUnetHTA, EPAAC), CEs in the field of RDs healthcare providers, RD experts and existing RD network co-ordinators and partners, patient organisations. EUCERD Recommendations on CEs The aim of these Recommendations is to help MSs in their reflections/policy developments concerning NP/S for RDs. Specifically, they are useful in addressing the organisation of healthcare pathways at national and at European level. Potentially, they are helpful for the CBHCD application in the context of ERNs development. This document includes 45 Recommendations, concerning 4 main areas: - mission and scope of CEs: definition, coverage, patient focus, core competencies, role in disseminating information and education, role in research; - criteria for designation: leadership and credibility, multidisciplinarity and inclusiveness, capacity, links and collaborations, mechanisms for measuring performance/evaluation; - process for designation: core principles of designation, designation criteria, duration of designation; - European dimension: sharing experience and indicators at EU level, networking. According to the EUCERD Recommendations, CEs are defined as physical highly specialised structures for the management and care of RD patients, with the mission of providing them with the highest standards of care and delivering timely diagnosis, appropriate treatment and follow up, on a regional, national, European or international level. Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0026-14s s622 CEs and ERNs: key issues in RD field. EUCERD Recommendations Each CE specialises in a single RD or in a group of RDs. It gathers or coordinates - within the specialised healthcare sector - multidisciplinary competences/skills, including paramedical skills and social services, in order to serve the specific medical, rehabilitative, palliative and social needs of RD patients. Multidisciplinarity and inclusiveness were defined as the capacity to deliver a multidisciplinary approach, integrating medical, paramedical, psychological and social needs and to ensure the continuity of care, from childhood through adolescence and adulthood, as well as in all stages of the disease. CEs should offer a wide range of specialised services: consultations, medical examinations, using specialised equipment, genetic testing, counselling and social care. They should also participate in building healthcare pathways, starting from primary care. Furthermore, they should contribute to research efforts through their participation in both data collection for clinical research and in clinical trials. They should collaborate with different stakeholders, including RD patient organisations. The focus of these Recommendations on CEs is on patients, so that all their needs may be effectively met. The criteria for the designation of CEs should be based on leadership and credibility, multidisciplinarity and inclusiveness, as well as on their capacity to create links and collaborations and on the existence of an evaluation mechanism. Moreover, MSs are responsible for their designation and this should be done through the adoption of transparent designation criteria, the assurance of an on-going evaluation process and the facilitation of access to the patients. The designation process at MS level should ensure that the designated CEs have the capacity and the resources to fulfil their obligations according to the criteria and that they have a strategy in place to meet all the criteria during a set period of time. The CEs designation is an important step as it provides the base for its connection to the next level of collaboration, the ERNs level. EUCERD Recommendations on ERNs The general concept and the method of implementing ERNs are defined in Article 12 of the CBHCD. The aim of these Recommendations on ERNs is to inform (a) the Commission's services and expert groups, working on the criteria for the creation and designation of ERNs on RDs specificities, in the context of the CBHCD; (b) MSs that are developing their healthcare pathways at, both, the national and the EU levels in the field of RDs, particularly in the context of NP/S for RDs. This document includes 21 Recommendations, concerning 5 main areas: - mission, vision and scope: providing a framework for healthcare pathways, covering core tools and activities; - governance: robust and clearly defined governance, strong leadership; - composition of RD ERNs: different forms of affiliation to allow inclusivity, linking CEs and stakeholders involved in the care management of patients; - funding and evaluation: long-term sustainable funding mechanisms (MS competence); - designation of RD ERNs: development of shared platforms across RDs, clear designation process, stepwise-strategy, defining and implementing a formal system for networking across all RD ERNs and sharing expertise. According to the EUCERD Recommendations, an RD ERN is the physical or virtual networking of knowledge and expertise of national CEs in more than one European Country. The goal of an ERN is the improvement of the overall quality and management of care of a single RD or a group of RDs with similar health care needs, by complementing, supporting and providing added-value to the existing services and expertise at the national level. In these Recommendations, it is stated that designated CEs are the core participants, so RD ERNs should be flexible enough to be able to work with different national structures. This networking activity among national CEs promotes the sharing and mobility of expertise rather than the movement of patients, and facilitates the travelling of patients to cross-border CEs when necessary. In order to improve the delivery of care in an effective way, while reducing its costs, the ERNs need to facilitate the sharing of information and tools amongst CEs and other care providers. For instance, information on disease registries, communication of guidelines/best standards of diagnosis and care, training and education tools, quality assurance schemes, telemedicine, cross-border referral mechanisms should be shared among CEs and other interested parties. The co-ordinating site(s) should be selected on the basis of proven leadership and capability to coordinate a network; it is not necessarily to be the best centre of expertise or the one with the largest number of patients. In the composition of RD ERNs different forms of affiliation (association, collaboration) can be foreseen. In small countries, where there may be a small number of CEs or no CEs at all, other healthcare providers can become affiliated members of an RD ERN. This allows an RD ERN to reach out of as many MSs as possible. RD ERNs should have clearly defined mechanisms of governance and evaluation, and patient organisations should play an important role in the process. Patients in every European country can benefit from an RD ERN, even if in their country there may not be a CE Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0026-14s s623 Taruscio D et al that is member of an RD ERN. The objective, in the next decade, is that RD ERNs cover all RDs grouped by diagnostic and systemic areas, using a step-wise approach. of RDs offers enormous and practical potentials for European cooperation. The specificities of these diseases the limited number of patients and the scarcity of relevant knowledge and expertise - single them out as a prime area for cooperation, with a very high European added-value26. Conclusions There are currently more than 6,000 identified RDs20, each of which affects fewer than 5 in 10,000 people, according to the EU definition. These diseases are thought to affect around 30 million people in the EU countries. For the last 10 years, RDs have become one of the priorities of the EU health policies and the development of CEs and ERNs in the field of RDs was encouraged in several EC documents, as well as in EU projects, such as EUROPLAN21. The establishment, designation, financial support, and evaluation of CEs throughout Europe allow RD patients and local health care providers to identify high-quality specialised services thus simplifying disease management and improving patients' care. The MSs should promote and support CEs in order to guarantee equity of access to good quality of services and care to their citizens affected by RDs. CEs should reduce costs in healthcare systems by contributing to shorter delays in diagnosis, less adverse consequences, a reduction in misdiagnoses and subsequent unnecessary treatments and more adequately adapted care, as pointed out also by EURORDIS22. The political commitment of MSs to identify and financially support CEs is a prerequisite for the creation of ERNs. Moreover, the establishment of ERNs also allows health authorities to identify the best allocation of financial resources to support the activities linked to the effective management of RD patients. Due to the differing health care structures, different definitions of a CEs and differences in the diseases they treat, each ERN, which consists of individual CEs, will also reflect this variability. CEs should be flexible to accommodate different stakeholders and healthcare providers with particular emphasis being placed on patients representatives. Nevertheless, the establishment and the sustainability of ERNs, as indicated in the CBHCD, is a major opportunity for the RD community23, especially for ultra RDs (by definition prevalence <1:2,000,00024Table I) in which expertise may be available only in a very small number of European countries. Therefore, ultra RD patients may need to receive care across borders. The added-value25 of ERNs is given by the existence of several multilateral cross border health care agreements, by many EC funded projects, documented by the EC HLG and by the currently funded EC pilot projects. CEs and ERNs are a good example of how the field Table I - Comparison of the major characteristics of rare and ultra-rare disorders25. Rare Disorders Ultra-rare disorders Prevalence <1:2,000 <1:2,000,000 Number of affected newborns/disorder in Europe 5,000 or less 5 or less Diagnosis Centers of expertise (national); E-mail consulting. Electronic database (international); E-mail consulting. Follow-up Centers of expertise Local healthcare professionals; Virtual centres of expertise. Provision of information Text books; literature; sites (OMIM, Orphanet, etc.) Wiki sites Support groups National International Research Grants difficult Grants extremely difficult Acknowledgements This paper was made possible thanks to the help of the EUCERD Joint Action: Working for Rare Diseases, which was funded by the EU in the framework of the Health Programme (grant 20112201). The Authors declare no conflicts of interest. References 1) 2) 3) 4) 5) 6) Commission of the European Communities, Commission communication on the framework for action in the field of public health.COM(93) 559. Brussels: CEC, 1993. Available at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=C OM:1997:0266:FIN:EN:PDF. Accessed on 03/01/2014. Birt CA, Gunning-Schepers L, Hayes A, Joyce L. How should public health policy be developed? A case study in European public health. J Public Health Med. 1997; 19: 262-7. Communication of the European Commission "Rare Diseases: Europe's challenge" (COM[2008] 679 final)" (11 November 2008). Available at: http://ec.europa.eu/health/ph_threats/ non_com/docs/rare_com_en.pdf. Accessed on 03/01/2014. Council Recommendation on an Action in the Field of Rare Diseases (2009/C 151/02) (8 June 2009). Available at: http:// eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:C:2009: 151:0007:0010:EN:PDF. Accessed on 03/01/2014. Directive on the application of patients' rights in cross-border healthcare (2011/24/EU) (9 March 2011). Available at: http:// eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2011: 088:0045:0065:EN:PDF. Accessed on 03/01/2014. EUROPLAN Recommendations for the Development of National Plans for Rare Diseases. Guidance Document. Available at: www.europlanproject.eu. Accessed on 03/01/2014. Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0026-14s s624 CEs and ERNs: key issues in RD field. EUCERD Recommendations 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) European Commission Decision of 30 November 2009 (2009/872/EC). Available at: http://eur-lex.europa.eu/ LexUriServ/LexUriServ.do?uri=OJ:L:2009:315:0018:0021: EN:PDF. Accessed on 03/01/2014. EUCERD Recommendations on Quality Criteria for Centres of Expertise for RD in MS (October 2011). Available at: www. eucerd.eu. Accessed on 03/01/2014. EUCERD Recommendations on Informed decisions based on the Clinical Added Value of Orphan Medicinal Products (September 2012). Available at: www.eucerd.eu. Accessed on 03/01/2014. EUCERD Recommendations on European reference networks for RD (January 2013). Available at: www.eucerd.eu. Accessed on 03/01/2014. EUCERD Recommendations on Rare Disease Patient Registration and Data Collection (June 2013a). Available at: www.eucerd.eu. Accessed on 03/01/2014. EUCERD Recommendations on Core Indicators for RD National Plans/Strategies (June 2013b). Available at: www. eucerd.eu. Accessed on 03/01/2014. Work of the High Level Group on Health Services and Medical Care during 2005. Available at: http://ec.europa. eu/health/archive/ph_overview/co_operation/mobility/docs/ highlevel_2005_013_en.pdf. Accessed on 03/01/2014. RDTF Report: Overview of Current Centres of Reference on rare diseases in the EU (September 2005). Available at: http:// www.eucerd.eu/upload/file/Publication/RDTFECR2005.pdf. Accessed on 03/01/2014. RDTF Report: Centres of Reference for Rare Diseases in Europe – State-of-the-art in 2006 and Recommendations of the Rare Diseases Task Force (September 2006). Available at: http://www.eucerd.eu/upload/file/Publication/ RDTFECR2006.pdf. Accessed on 03/01/2014. RDTF Report: European reference networks in the field of Rare Diseases: State of the art and Future Directions (July 2008). Available at: http://www.eucerd.eu/upload/file/ Publication/RDTFERN2008.pdf. Accessed on 03/01/2014. EUCERD Workshop Report: Centres of expertise and European reference networks for rare diseases (8-9 December 2010). Available at: http://www.eucerd.eu/upload/file/ WorkshopReport/EUCERDWorkshopReportCECERN.pdf. Accessed on 03/01/2014. EUCERD Workshop Report: National centres of expertise for rare diseases and networking between centres of expertise for rare diseases (21-22 March 2011). Available at: http://www. eucerd.eu/upload/file/EUCERDReport220311.pdf. Accessed on 03/01/2014. 19) EUCERD Report: Preliminary analysis of the experiences and outcomes of ERNs for rare diseases (May 2011). Avalaible at: http://www.eucerd.eu/upload/file/Reports/ERN2011Analysis. pdf. Accessed on 03/01/2014. 20) European Parliament and Council. Regulation (EC) 141/2000 of the European Parliament and of the Council of 16 December 1999 on orphan medicinal products. Official Journal 2000; L18: 1-5. 21) Taruscio D, Gentile AE, De Santis M, et al. EUROPLAN: A Project to Support the Development of National Plans on Rare Diseases in Europe. Public Health Genomics 2013; 16: 278-87. 22) 2013 EURORDIS Policy Fact Sheet - Centres of Expertise. Available at: www.eurordis.org. Accessed on 03/01/2014. 23) 2013 EURORDIS Policy Fact Sheet - European reference networks of Centres of Expertise. Available at: www.eurordis. org. Accessed on 03/01/2014. 24) Bushby K. European reference networks: developing a EUCERD opinion. Orphanet J Rare Dis 2012; 7 (Suppl 2): A6. 25) Hennekam RCM. Care for patients with ultra-rare disorders. European Journal of Medical Genetics. Eur J Med Genet 2011; 54: 220-4. 26) Moliner Montserrat A. Creating a European Union framework for actions in the field of rare diseases. Adv Exp Med Biol 2010; 686: 457-73. Correspondence: Domenica Taruscio Italian National Centre for Rare Diseases – Istituto Superiore di Sanità Viale Regina Elena, 299 00161 Rome, Italy e-mail: domenica.taruscio@iss.it Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0026-14s s625 LETTER TO THE EDITOR European Reference Networks for rare diseases: the vision of patients Terkel Andersen, Yann Le Cam, Ariane Weinman European Organisation for Rare Diseases (EURORDIS), Paris, France Dear Sir, The European Organisation for Rare Diseases -EURORDIS- is a non-governmental patient-driven alliance of patient organisations and individuals active in the field of rare diseases. EURORDIS represents over 600 rare disease organisations in 58 countries (including 26 EU Member States) covering more than 4,000 rare diseases. More information is available on www.eurordis.org1. Since 2004, EURORDIS has been involved in different discussions at European and national levels on shaping Centres of Expertise and European Reference Networks (ERNs) for rare diseases with a view to improve timely access to appropriate diagnosis and care for people living with a rare disease. Over almost a decade, EURORDIS has gathered the opinions of its members on these topics through its Annual Membership Meetings as well as through surveys and workshops organised within the European co-funded projects RAPSODY and POLKA2. The opinions of our members have informed relevant EURORDIS position papers, which thus reflect the expectations of patients and their families regarding the organisation of care and delivery of treatments for their diseases. Why are ERNs important for patients with rare diseases? Due to the low prevalence of each rare disease, expertise is by essence scarce and scattered throughout Europe. The best way to accelerate access to a proper, timely diagnosis, as well as appropriate care, is to share expertise by linking at European level the national Centres of Expertise, healthcare providers, diagnostic laboratories, other relevant services and patients' organisations. ERNs are also intended to gather a critical mass of patients and data to support rare disease registries and clinical research. The national Centres of Expertise are seen to constitute the nodes of ERNs for rare diseases. EURORDIS, through its representatives, contributed to the Recommendation of the European Committee of Experts on Rare Diseases (EUCERD) on the "quality criteria for Centres of Expertise for Rare Diseases in Member States", which was adopted on 24 October 2011. To date, the EU Member States are developing criteria based on this Recommendation for designated Centres of Expertise for RDs in their territory within their national plans/strategies for rare diseases. The European Directive 2011/24/EU 3 on the "application of patients' rights in cross-border healthcare" has delineated for the first time the legal framework for European reference networks. This has been a success in translating a concept into a real healthcare framework with an added value for patients. In addition, Article 13 of this Directive is specifically dedicated to rare diseases: "The Commission shall support Member States in cooperating in the development of diagnosis and treatment capacity in particular by aiming to make health professionals aware of the tools available to them at Union level to assist them in the correct diagnosis of rare diseases, in particular the Orphanet database, and the European Reference Networks". In this evolving context, EURORDIS adopted in May 2012 a position to outline its vision and strategy for ERNs for rare diseases; what they should comprise and how they should function based on the patient's real life experience. EURORDIS rejects the logic of selecting priorities amongst rare diseases; all patients affected with a rare disease should be covered by at least one ERN in the long run. As it will not be possible to fund numerous ERNs, EURORDIS recommends that a limited number of ERNs for RDs (20 to 30) should be created by diagnostic and therapeutic areas in order to cover a wide range of rare diseases. EURORDIS also emphasises that a high-level of multi-disciplinarity and inter-operability among ERNs are absolutely necessary. The successful development of ERNs for RDs will rely on a step-wise approach aimed at establishing progressively the various activities of the ERN, such as experts' opinions, good practice guidelines on medical care as well as social care, training, patient registries, e-health. The ERNS should remain flexible in order to evolve over time. The EURORDIS representatives in the EUCERD voiced the patients' perspectives during the consultations on the elaboration of the Recommendation on European Reference Networks for Rare Diseases. This EUCERD Recommendation4 was adopted on 31 January 2013 and integrates many elements of the rare disease patients' position. The new Health for Growth Programme of the European Commission, adopted in March, shall cover a period of seven years, from 2014 to 2020. We are aware that there will not be enough funding for European Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0039-14s s626 © SIMTI Servizi Srl European reference networks: the vision of patients reference networks. Therefore, we need to be creative and seek other sources of funding, for instance from the Horizon 2020 programme and possibly structural funds for health. Tonio Borg, European Commissioner for Health, has recently emphasised that research on rare diseases is a priority for the European Commission and where there is an opportunity to offer a better service to citizens, the principle of subsidiarity applies; hence this principle applies to Cross-Border Healthcare for Rare Diseases. 4) European Union Committee of Experts on Rare Diseases EUCERD. Recommendations on Rare Disease European Reference Networks (RD ERNS). 31 January 2013. Available at: http://www.eucerd.eu/?post_type=document&p=2207. Accessed on 21/02/2014. The Authors declare no conflicts of interest. References 1) 2) 3) Eurordis.org [Internet]. Brussels. EURORDIS Rare Diseases Europe. Available at: www.eurordis.org. Eurordis.org [Internet]. Brussels. POLKA: Patients' Consensus on Preferred Policy Scenarii for Rare Disease. EURORDIS Rare Diseases Europe. September 2008 [Page last updated: 20/07/2011]. Available at: http://www.eurordis.org/content/ polka-patients-consensus-preferred-policy-scenarii-raredisease. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare. Available at: http://ec.europa.eu/ health/cross_border_care/policy/index_en.htm. Accessed on 21/02/2014. Correspondence: Ariane Weinman European Organisation for Rare Diseases 96, rue Didot 75014 Paris, France e-mail: ariane.weinman@eurordis.org Blood Transfus 2014; 12 Suppl 3: s621-5 DOI 10.2450/2014.0039-14s s627 ACKNOWLEDGEMENTS Our thanks to those who have helped with this special issue of Blood Transfusion and who have kindly given their time, effort and expertise; their generosity has helped establish this publication. Abbonizio F. Agresta L. Amato A. Andersen T. Arcieri R. Armeni P. Avanzi F. Baldovino S. Bernardo G. Bernardo L. Berntorp E. Bon C. Braguti F. Calizzani G. Candura F. Carbone P. Carta C. Castaman G. Cavazza M. Ceccarini M. Censi F. Cerbone A.M. Cimino E. Congiu M.E. Coppola A. Coppola S. Crialese P. De Santis M. Di Minno G. Di Stanislao F. Diemoz S. Donati C. Evangelista T. Facco G. Farace S. Fattore G. Ferrari G. Fischer K. Floridia G. Fortino A. Franchini M. Frank C. Frazzica R.G. Gainotti S. Garnero A. Gatt A. Gentile A.E. Giampaolo A. Giangrande P. Gilman E. Giordano P. Granata O. Grazzini G. Hassan, H.J. Hermans C. Hollingsworth R. Iorio A. Kate Bushby K. Keepanasseril A. Kodra Y. Lamanna A. Lambert T. Lanzoni M. Laricchiuta P. Lassila R. Latrofa M. Le Cam Y. Leebeek, F.W.G. Liumbruno G.M. Magrelli A. Makris M. Mannucci P.M. Mantovani L. Manzoli L. Marano G. Maspoli M. Matino D. Mazza G. McLaughlin K. Menegatti E. Menichini I. Modena V. Molinari A.C. Moliner Montserrat A. Morciano C. Morfini M. Nuti S. Oleari F. Oliovecchio E. Page D. Peyvandi F. Polizzi A. Profili S. Pupella S. Razeto S. Roccatello D. Saia M. Salvatore M. Sanseverino A. Santoro C. Savini D. Schieppati A. Skinner, M.W. Soucie J.M. Tamburrini M.R. Taruscio D. Teitel, J. Torreri P. Tosto F. Tufano A. Vaglio S. Velati C. Villani F. Vincenti G. Vittozzi L. Walker I. Weinman A. Windyga J. Zanon E. Special thanks to Cannata L., Fehily D. and Gillespie F. who kindly provided the linguistic review of the manuscripts. Blood Transfus 2014; 12 Suppl 3 s628 © SIMTI Servizi Srl www.fedemo.it Associazione Italiana Centri Emofilia www.aiceonline.org Italian Association of Haemophilia Centres (AICE) Federation of Haemophilic Patient Associations (FEDEMO) and the World Federation of Hemophilia (WHF) TOGETHER to improve the quality of life of patients with haemophilia www.smc-media.com FedEmoeAICEaWFH.indd 2 18/04/14 13.02