ocular motor deficits in parkinson`s disease
advertisement

Brain (19&3), 106, 571-587
OCULAR MOTOR DEFICITS IN
PARKINSON'S DISEASE
II. CONTROL OF THE SACCADIC AND SMOOTH
PURSUIT SYSTEMS
by OWEN B. WHITE, JEAN A. SAINT-CYR, R. DAVID TOMLINSON
and JAMES A. SHARPE
(From the Neuro-ophthalmology Unit, Division of Neurology, the Play fair Neuroscience Unit, Toronto
Western Hospital, and the Departments of Medicine, Ophthalmology and Anatomy, University of
Toronto, Canada)
SUMMARY
We quantified the horizontal pursuit and saccadic function of 14 parkinsonian patients and 10 normal
subjects matched for age. Eight patients had mild, and 6 advanced disease. Ocular motor deficits were
more marked in patients with advanced disease. Saccadic reaction times and postsaccadic refractory
periods were prolonged. Peak saccadic velocities were significantly reduced. Slow saccades may be
caused by inappropriate coactivation of opposing ocular muscles. Multiple step, hypometric saccades
were abnormally frequent. Correctfinaleye position towards a brief targetflashwas attained without
visual feedback. Brief corrective intervals occurred after hypometric saccades. They are attributed to
internal (nonvisual) efference copy feedback of eye position errors. Frequent square wave jerks were
also a feature of Parkinson's disease.
Smooth pursuit gain was lowered in all patients while tracking sinusoidal targets at frequencies from
0.25 to 1 Hz. Pursuit gain was uniformly reduced at all target velocities at each frequency. This decrease
in gain indicates that dysfunction of the gain element, rather than abnormal drop acceleration
saturation is responsible for impaired smooth pursuit.
The results indicate that Parkinson's disease damages structures involved in the regulation of the
saccadic and pursuit systems. We infer that nigrostriatal pathways, known to be damaged in
Parkinson's disease, control the latency, velocity and amplitude of saccades, and the gain element of
smooth pursuit.
INTRODUCTION
Parkinson's disease is a syndrome of disordered motor performance attributed to
abnormal dopaminergic systems in the basal ganglia. Studies of limb motor function
have demonstrated prolonged latencies and bradykinesia (Evarts et al., 1981),
inappropriate coactivation of agonist-antagonist muscle pairs and abnormalities of
stretch and shortening responses, impaired predictive capacity and abnormalities of
long-loop reflexes (Evarts et al., 1979). These deficits are translated into the clinical
features by which we recognize parkinsonism of any aetiology: tremor, rigidity,
akinesia and bradykinesia.
Reprint requests to Dr J. A. Sharpe, Toronto Western Hospital, 399 Bathurst St., Toronto, Ontario M5T 2S8,
Canada.
572
OWEN B. WHITE AND OTHERS
Ocular motor functions lend themselves to quantification of motor performance,
relative to limb movement, because of the accessibility of eye movements for
recording and the ease with which single movements can be accurately repeated. The
balanced agonist-antagonist muscle pairings, low inertia of the globe and the
relatively constant viscoelastic properties of the orbit permit analysis of neural
control mechanisms. Despite these attributes, few studies have quantified the
function of the saccadic or smooth pursuit systems in parkinsonism. In a qualitative
oculographic study Corin et al. (1972) observed 'cog-wheel' pursuit, hypometric
saccades, gaze impersistence, subnormal optokinetic reflexes, impaired vergence
and defective vertical eye movements. Shibasaki et al. (1979) and Teravainen and
Calne (1980) recorded an increased frequency of saccades during pursuit but they
did not measure smooth pursuit. Shibasaki et al. (1979) described reduced saccadic
velocities but did not correlate velocity with amplitude. Quantitative study of
saccades has found increased latency of self-placed refixations and hypometric
saccades (DeJong and Melvill Jones, 1971; Melvill Jones and DeJong, 1971;
Teravainen and Calne, 1980). The relationship between saccadic velocity and
amplitude was reported to be normal.
We report a quantitative study of the saccadic and pursuit systems. We
examined horizontal saccadic latency, accuracy and velocity to predictable and
unpredictable target motion. Smooth pursuit gain, the ratio of smooth eye
movement velocity to target velocity, was measured during horizontal tracking of
sinusoidal and constant velocity targets.
METHODS AND SUBJECTS
Descriptions of the subjects and equipment used were detailed in the companion paper (White
et al., 1983). Briefly, we examined 14 parkinsonian patients and 10 control subjects matched for age
and sex. Eye movements were recorded by photoelectric infrared oculography and data were
stored on magnetic tape. After data were digitized off-line at 200 samples/s for computer analysis,
the full system bandwidth was 0 to 100 Hz. Calibrations were performed before and after each
paradigm. Subjects were seated with the head stabilized by chin, frontal, parietal and occipital
supports.
Saccadic System
Targets for saccadic eye movements were light-emitting diodes (LED) arrayed on a stimulus arc,
radius 114 cm, with the subject seated at the origin in order to eliminate changes in vergence (Sharpe et
al., 1979). Target position was controlled by a microprocessor. All paradigms were performed in
darkness. Frequent verbal encouragement ensured alertness while saccades were made under each of
four conditions. (1) Predictable target steps. The target was stepped from 10 deg left to 10 deg right at
predictable intervals greater than 2 s. All saccadic responses to at least 50 target steps were analysed in
each subject. (2) Unpredictable amplitude target steps. The target was stepped 5, 10, 15, 20 or 40 deg left
or right at predictable intervals (3 s), in pseudorandom directions and amplitudes. Large target steps
always crossed the centre so that angular displacement never exceeded 20 deg from midposition, the
limits of the linear range of the infrared system. Saccadic responses to target steps (n > 150) were
quantified for each subject. (3) Unpredictable amplitude target flash. The target was stepped in
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
573
unpredictable directions and amplitudes as in condition 2, except that when the original target was
extinguished, the new target was illuminated for only 40 ms and then extinguished for 2 s (fig. 1E). The
LED was then reilluminated and became the fixation target. Since normal saccadic latency is
approximately 200 ms, the brief target flash ensured that subjects made saccades without visual
feedback. As in condition 2, saccadic data from at least 150 target steps were analysed for each subject.
A
Target
B
r
]20°
] 20°
1 20°
I206
Eye
"
;
Velocity
^
] 200°/s
^
J 200°/s
C
] 20°
Target
1 20°
I 20°
E
y
Velocity
e
"
~
,
1 20°
- -
] 2 00°/s
~"
. , w _
]200°/s
40 ms target flash
•
Darkness
•
1 20°
Target
Eye
500 ms
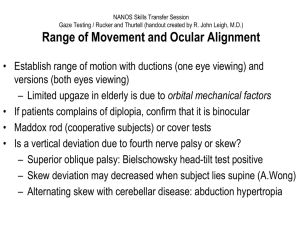
FIG. 1. Examples of digitized saccadic eye movements in response to stepped targets, A, normal subject, B, patient:
note slow onset and reduced peak velocity, c, patient: multiple, hypometric saccades. D, patient: slow saccade. E,
patient: response to flashed target.
574
OWEN B. WHITE AND OTHERS
(4) Unpredictable time target steps. The target stepped from 10 deg left to 10 deg right at pseudorandom
intervals ranging from 300 to 2000 ms. This paradigm made the time of target shift unpredictable, but
amplitude and direction remained predictable. We recorded for 4 min in each subject. Fixation time
was designated as the period from the instant of fixation of the target until the target stepped again.
Fixation time was measured to differentiate between prolonged latencies to target steps and a
prolonged refractory period after refixation, before another saccade could be generated. Refractory
delay and initiation delay could both be construed as saccadic akinesia, but quite separate mechanisms
may be responsible.
Fixation stability was observed in all patients and quantified in 8 patients while fixating a stationary
LED target for 3 min. The frequency of square wave jerks was recorded.
Smooth Pursuit System
Subjects were instructed to follow a laser target (0.25 deg at the retina) projected from the rear on to
a screen 170 cm from their nasion. Target movement was achieved by reflecting the laser beam on to
a galvanometer mounted mirror and was controlled by a microprocessor. Target motion was 20 deg
peak-to-peak. Ambient lighting was maintained at a low level.
1. Predictable ramps. The target moved in predictable directions and velocities. Fixed intervals
between each ramp also made timing predictable. Ramp velocities were 10, 20 and 40 deg/s. We
analysed responses to 80 ramps at each velocity for each subject.
2. Predictable sinusoids. The target moved sinusoidally at constant frequencies of 0.25, 0.5 or 1.0 Hz.
Peak-to-peak amplitude was 20 deg. Peak velocity was 16, 31 and 63 deg/s, yielding peak target
accelerations of 25, 99 and 395 deg/s/s, respectively. The sinusoidal motion elicited a large range of
target velocities with low acceleration demands relative to ramp targets. We analysed all responses to
25 target cycles at each frequency for each subject.
Data Analysis
Digitized eye position data were displayed on a graphics terminal simultaneously with a
differentiated velocity trace. For target steps, cursors placed on the target channel defined the
time, direction and amplitude of target motion. Cursors on the eye position channel delineated the
onset and termination of each saccade. The peak velocity was measured from the eye position
trace between 2 cursors, 10 ms apart, at the segment corresponding to the peak of the differentiated
signal.
For pursuit paradigms, the target movement was marked and the cursors were placed on the eye
position channel at the onset and completion of all smooth eye movement segments. A computer
program divided sinusoidal target motion into segments of approximately uniform velocity, and
selected time-locked smooth eye movement segments; pursuit gain was then computed for a range of
velocities at each target frequency.
Statistical analyses of all data were performed using the nonparametric Mann-Whitney U test.
RESULTS
Patients were divided into two groups, mild and advanced, on the basis of severity
of rigidity and bradykinesia, and the duration of disease, as described in the
companion article (White et al., 1983).
Saccadic System
1. Predictable target steps and 2, unpredictable amplitude target steps. Protocols
1 and 2, in which target timing was always predictable, are considered together since
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
575
latencies and saccade metrics did not differ significantly for any individual subject
between the two conditions. Normal subjects and patients often made eye
movements before target steps, whether or not the amplitude and direction of target
step were predictable. These anticipatory movements towards the expected goal
were of two types: either saccades, or smooth eye movements which had velocities
less than 1 deg/s. When the direction and amplitude of target step were
unpredictable (condition 2), subjects frequently made errors in the direction of their
anticipatory movements but persisted in attempts to predict. Anticipatory movements, having negative latencies, were excluded from latency data. Patients with
advanced disease had significantly longer mean saccadic latencies than normals
(P < 0.001; Table 1; fig. 2A). There was a wide intrasubject range of saccadic
latencies even for mildly affected patients (SD + 80 ms) compared to normal subjects
(SD±40ms).
B
^ 600
A
S> 500
5*15
$• 400
'o
<a
"S 10
I
•§ 300
>
8
V3
I
511. I
| 200
o
-rajj EJ,n n
70
140
210 280 350 420
Saccade latency (ms)
490 560
100
-20
0Left
5 5
-10
9
10
Saccade amplitude (deg)
20
Right
c
25 r
10
o
0
-30 -20 -10
6
10 20
Saccade amplitude (deg)
30
0
-40 -30 -20 -10
0
10 20
Saccade amplitude (deg)
30
FIG. 2. A, histogram of saccade latencies for patients with advanced disease (crosshatched columns) and normal
subjects (open columns), B, graph of saccade mean peak velocity vs amplitude for advanced patients (A) and normal
subjects (o). Error bars indicate 1 SD. c, histogram of frequency of saccades of varying amplitudes in response to
predictably timed target steps of 20 deg; mild patients (crosshatched columns); normal subjects (open columns), D,
histogram of saccadic amplitude for patients having advanced disease (crosshatched columns) shows more frequent
saccadic hypometria. Negative amplitude indicates leftward saccades, positive rightward.
40
576
OWEN B. WHITE AND OTHERS
The peak velocity-amplitude relationship of 4, 10 and 18 deg saccades, made by
patients and normals, were compared. We obtained these velocities from conditions
1 and 2, using over 15 saccades at each amplitude for each subject (Table 1). Patients
demonstrated far more variability than normals. Mean saccadic velocities were
significantly slowed at all amplitudes for advanced patients (P < 0.01; Table 1;
fig. 2B), but velocities were within the normal range (normal mean + 2 SD). Patients
also generated many more saccades terminated by slow glissadic movements than
did normal subjects. In patients, initial responses, after target steps, were frequently
slow movements, continuous with the saccade, which were not by their timing
anticipatory (fig. 1B). Such slow acceleration was not a feature of saccades in normal
subjects.
TABLE 1. SACCADIC LATENCIES AND VELOCITIES FOR PREDICTABLY TIMED
TARGET STEPS
Patients
Latency (ms)
Normals
Mild
220 ±40
270 + 80
Advanced
360 ±90**
Mean peak velocity (degls)
Saccade amplitude
4 deg
10 deg
18 deg
176+15
314±43
396 + 54
157 + 36*
288 + 49***
387 + 66
130±34***
246±56**
296 + 55***
* P < 0.05, ** P < 0.01, *** P < 0.001.
Saccadic inaccuracy was frequent in patients. They made multiple hypometric
steps to refixate the target (fig. lc). Hypometria was measured by computer
histogram plots of the frequency of saccades of all amplitudes in response to a target
step of constant amplitude (fig. 2c, D). Normal subjects made primary saccades
close to or equal to the amplitude of the target step of 20 deg. Patients made initial
hypometric saccades unrelated in amplitude to the size of the target step. They were
followed by a corrective saccade, beginning at a mean interval of 150 ms (range 10 to
1000 ms) after the completion of the primary saccade (fig. 1 c). Mean correction time
was not significantly different from normal subjects but the range was greater.
Hypometric saccadic segments had the same reduced peak velocity-amplitude
relationship as the patients' normometric saccades.
3. Unpredictable amplitude target flash. This paradigm examined saccadic
accuracy without visual feedback. Nine patients, 4 with advanced disease and 3
normal subjects, were examined. Accuracy of saccades to a flashed target did not
differ from accuracy to a continuous target in patients or normals. Patients
generated multiple hypometric saccades but attained the position of the target flash
prior to its reillumination like normal subjects (fig. 1E). Latencies, saccadic velocities
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
577
and corrective times were comparable to those obtained with constantly lighted
targets.
4. Unpredictable time target steps. Variation of the timing of target steps
prolonged the latency for saccades {see Tables 1 and 2). Fixation times were grouped
in bins and correlated with latency (Table 2). Normal subjects demonstrated only
TABLE 2. SACCADIC LATENCY VS DURATION OF TARGET FIXATION TIME FOR
UNPREDICTABLY TIMED TARGET STEPS
Fixation time (ms)
Subjects
Normals
L
<200
<300
< 400
<500
<800
>800
390
370
320
270
240
210
440
340
350
250
220
210
670*
630*
400*
380
330**
260*
A
T
Mild patients
E
XI
IN
Advanced patients
c
Y
* P < 0.05, ** P < 0.01. Latencies are the mean of the mean values for each subject.
mild lengthening of latency for refixations performed after periods of fixation less
than 300 ms. Although mildly affected patients had prolonged latencies, these did
not differ significantly from normal. Advanced patients showed significantly
prolonged latencies (Table 2). After brief fixation periods the increase in saccadic
delay was twice that of normal subjects. In other words, the time required to initiate
a saccade increased as the time available for target sampling (fixation time)
decreased.
Square wave jerks, consisting of horizontal saccades followed after an interval by
saccadic return to the fixation position, occurred far more frequently in patients
with Parkinson's disease (mean frequency 52/min + 29, range 5-82) than in normal
subjects (Herishanu and Sharpe, 1981). Abnormally frequent square wave jerks
were observed both during fixation and low velocity pursuit.
Smooth Pursuit System
1. Predictable ramps. All but one patient (Case 14, White et al., 1983) showed
significant reduction in smooth eye velocities while pursuing ramps at both 10 and
20 deg/s (Table 3). Neither patients nor normals pursued the repeated single ramps
successfully at 40 deg/s. Patients, like normals, generated anticipatory smooth eye
movements before target movement (fig. 3). These anticipatory movements
frequently attained velocities up to 10 deg/s. Saccadic intrusions, in both directions,
were frequent, but patients with advanced disease adopted a stratagem of saccadic
pursuit, even at the lowest target velocities (fig. 3). This smooth pursuit eye
movement deficit is illustrated by histograms of cumulative time spent in smooth
OWEN B. WHITE AND OTHERS
578
TABLE 3. SMOOTH PURSUIT OF PREDICTABLE SINGLE RAMPS
Mean eye velocity (degjs)
Patients
Target velocity
lOdeg/s
2Odeg/s
Normals
8.99±0.72
15.82 + 2.02
Mild
8.49 + 0.59*
13.22 + 1.89***
Advanced
7.29+1.97*
10.33±3.49***
* P < 0.05, ** P < 0.01, *** P < 0.001.
pursuit expressed as a percentage of the total time that the target moved across the
screen at each velocity (fig. 4). Patients demonstrated greater variability and spent
more time at lower pursuit gain than normals, a deficit more evident in advanced
disease (fig. 4; Table 3).
10°
Normal
Eye
10°
Patient
Eye
10°
500 ms
10°
10°
Normal
Eye
10°
500 ms
FIG. 3. Examples of digitized smooth pursuit movements made by patients with advanced disease and normal
subjects, A, single repeated ramps, B, sinusoidal target. Right is upward, left downward.
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
579
: duration
30 r
1
o.
Noi •mal:
1
20
10
0
-40
Left
-20
0
20
Pursuit velocity (deg/s)
40
Right
FIG. 4. Histogram of normalized pursuit duration (cumulative duration of smooth pursuit eye
movements expressed as a percentage of cumulative ramp duration) for advanced patients (crosshatched columns) and normal subjects (open
columns), while tracking 20 deg/s ramps.
2. Predictable sinusoids. Normal subjects pursued targets at 0.25 and 0.5 Hz with
gain close to unity; at 1.0 Hz, gain declined to 0.55 (Table 4; fig. 5). Pursuit gain, the
ratio of smooth eye movement velocity to target velocity, was independent of target
velocity at each target frequency (for example, 0 to 63 deg/s at 1.0 Hz;fig.6). The
relationship between target velocity and smooth eye movement velocity indicated
that pursuit gain decreased with increasing target frequency not with increasing
target velocity. Patients had significantly lower pursuit gains at each frequency than
controls (Table 4;fig.5). All but Case 14 substituted saccadic tracking for defective
smooth pursuit at even the lowest frequency.
Smooth pursuit depends on visual feedback; it is a closed-loop negative feedback
system (fig. 7). Closed-loop pursuit gain was measured as the ratio of eye velocity to
target velocity for each target segment, then averaged to obtain mean pursuit gains
for each target frequency over the range of target velocities. We estimated pursuit
TABLE 4. SMOOTH PURSUIT OF SINUSOIDAL TARGETS
Closed-loop pursuit gain
Patients
Frequency
{Hz)
Normals
Mild
0.25
0.5
1.0
0.92 ±0.07
0.90 ±0.10
0.55 + 0.12
0.84 + 0.09*
0.74+0.12**
0.49 ±0.12
Advanced
0.70 + 0.14**
0.54±0.23***
0.35±0.13*
Open-loop pursuit gain
0.25
0.5
1.0
11.5
9.0
1.2
5.25
2.8
0.95
2.33
1.2
0.54
No significance was obtained at 1.0 Hz for mildly impaired patients but 2 patients from this group
and 3 more severely impaired patients were unable to follow at this frequency. * P < 0.05,
** P < 0.01, *** P < 0.001.
580
OWEN B. WHITE AND OTHERS
1.0
r
0.9
0.8
0.7
5 0.6
0.5
0.4
0.3
0.21-
0.25
0.50
1.0
0.75
Target frequency (Hz)
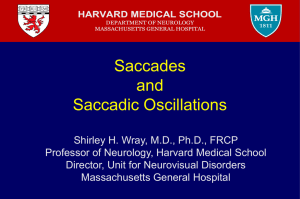
FIG. 5. Graph of smooth pursuit gain vs target frequency for sinusoidal targets. Patients with advanced disease
(A). Patients with mild disease (A). Normal subjects (o). Error bars indicate + 1 SD.
I
1.0 r0.9
0.8
.1
3. 0.7
I
I
I i
1 1
0.5
0.4
0.3 L
10
20
Target velocity (deg/s)
30
FIG. 6. Graph of smooth pursuit gain vs target velocity for a sinusoidal target at 0.5 Hz. Patients with advanced
disease (A). Patients with mild disease (A). Normal subjects (o).
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
581
system performance by calculating the open-loop gain (k) from the closed-loop gain
(G) where k = G/l-G. Although closed-loop gain was decreased by less than 30 per
cent for target velocities under 30 deg/s (at 0.25 and 0.5 Hz in the sinusoidal
protocols), calculated open-loop gain was decreased by about 70 per cent (Table 4).
G = E/T =
1 +k
FIG. 7. Simplified model of smooth pursuit system. Proceeding from the left, eye velocity (E) is subtracted from
target velocity (T) to yield retinal slip velocity (e). This signal is passed through a saturating nonlinearity, depicted
by the box containing a sigmoid curve, and then multiplied by a gain factor, k, before being fed to the orbital plant
(eye muscles and orbital mechanical properties) resulting in an eye velocity (E) which is the output of the system. The
negative feedback loop causes the overall system gain (G) to be k/1 + k.
DISCUSSION
This study documents abnormalities of saccadic initiation and trajectory, and
smooth pursuit gain, not previously quantified in Parkinson's disease. We examined
patients taking L-DOPA and anticholinergic medications, in combination or alone,
as well as untreated patients. Ocular motor dysfunction occurred regardless of
medication. We did not study the effects of medications longitudinally. Highstein et
al. (1969) recorded improvement in saccadic speed and accuracy after L-DOPA in 2
patients. In our 14 patients the severity of ocular motor impairment correlated with
the duration of the disease and the severity of bradykinesia and rigidity.
Saccadic System
Saccadic delay. The mean latency of saccades to target steps was markedly
increased in advanced disease (Table 1). Both patients and normal subjects
frequently initiated saccades at short latency when target timing was predictable
(fig. 2A). Patients, like normal subjects, made anticipatory movements before the
target moved. Most were saccades, but a few were smooth eye movements that did
not exceed 1 deg/s. Both our patients and normals generated anticipatory smooth
eye movements at velocities up to 10 deg/s before ramp targets. Short latency
saccades and anticipatory eye movements to regular target motion signified
preserved ocular motor prediction in parkinsonism. This relative integrity of ocular
motor prediction contrasts with impairment of anticipatory limb movements
(Flowers and Downing, 1978).
The prolonged reaction time for limb movement (akinesia) is disproportionately
increased for visually triggered responses when compared with kinaesthetic
582
OWEN B. WHITE AND OTHERS
responses (Evarts et al., 1981). In our patients, saccadic delay to unpredictably
timed targets was disproportionately increased after brief periods of target fixation
(Table 2). The large increment in patients' reaction time (approximately 340 ms)
compared with that of normals (approximately 150 ms), greatly exceeds the increase
in delay of visual evoked potentials in Parkinson's disease (approximately 15 ms)
(Bodis-Wollner and Yahr, 1978). This saccadic akinesia cannot be explained by
visual afferent delay alone. Since saccadic delay after prolonged fixation was
relatively brief (330 ms), the increment in delay after brief fixation (latency 670 ms)
cannot be explained by absolute delay in motor efferent pathways.
Normal saccadic responses to visual stimuli usually occur at discrete intervals of
approximately 200 ms. A sampled-data system model was proposed to explain this
behaviour (Young and Stark, 1962). However, observation of shorter latency
responses and visual modification of saccades in flight prompts revision of the
sampled-data concept (Hallett and Lightstone, 1976). Robinson (1973) proposed
parallel processing for saccades of specific amplitude and direction. According to
this hypothesis, each parallel process can initiate a saccade and cancel others. In our
patients, saccadic delay increased as sampling time decreased (fixation time; Table
2). The increased time required for sampling could indicate increased refractoriness
in sampled-data behaviour. This refractory delay implies that defective selection of
channels that trigger saccades might be responsible for saccadic akinesia in
Parkinson's disease. This explanation is highly speculative, and other mechanisms
might account for refractory delay.
Dementia and cerebral cortical damage also cause prolonged saccadic latency
(Pirozzolo and Hansch, 1981; Sharped al., 1979). Dementia occurs more frequently
in Parkinson's disease than in an age-matched population (Lieberman et al., 1979)
and cerebral cortical degeneration can occur without dementia in Parkinson's
disease (Boiler et al., 1980). Our patients who had advanced motor deficits and
normal intellectual function (White et al., 1983) had saccadic delay. The delay may
be an otherwise undetected disorder of vigilance that results from cerebral cortical
or basal ganglia dysfunction in Parkinson's disease.
Frequent square wave jerks signifiedfixationalinstability. Although prominent in
cerebellar system disease, they are also common in patients with focal cerebral
hemisphere damage (Sharpe et al., 1982). Our recordings indicated that square wave
jerks are a feature of Parkinson's disease.
Slow saccades. Peak velocities for saccades of defined amplitudes, although within
the normal range, were significantly reduced and more variable in patients (fig. 2B;
Table 1). Slowing was more marked in patients with advanced disease (Table 1).
Saccades are probably initiated by supranuclear trigger signals that inhibit pause
cells in the midline pontine tegmentum (Robinson, 1975): Pause cells, in turn, are
thought to inhibit presaccadic burst units in the pons. In the monkey, van Gisbergen
et al. (1981) recorded from motor neurons in the abducens nuclei, and from
medium-lead burst neurons in the pontomedullary reticular formation, which
discharge before saccades. Burst cells fire for saccades in all directions. Motor
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
583
neurons discharge for saccades in both horizontal directions but their firing
sequence varies with the direction of saccades, thereby defining on and off
directions. The on-direction burst drives the saccade, and subsequent off-direction
firing of burst cells on the opposite side of the pons may be responsible for dynamic
braking of the eye at the end of saccades.
The difference between on-direction burst rate and off-direction burst rate
correlates with instantaneous eye velocity. Inhibitory burst neurons in the
medullary reticular formation are thought to inhibit motor neurons reciprocally
during saccades in off-directions (Hikosaka et al., 1978). The reciprocal agonistantagonist discharge of motor neurons is determined by synchronized activity of ondirection burst neurons, off-direction burst neurons and inhibitory burst neurons.
The slowed saccades recorded in our patients indicate disordered regulation of
motor neuron innervation. The pontine tegmentum is the only supranuclear site
where damage is proven, by pathological correlation, to cause marked slowing
of saccades (Sanders, 1975). Progressive supranuclear palsy is a parkinsonian
syndrome in which slow hypometric horizontal saccades accompany vertical
ophthalmoplegia (Troost and Daroff, 1977). Degeneration of the pontine reticular
formation (Steele et al., 1964) is a feature of the disorder that can explain slowed
saccades. However, the pontine reticular formation is considered to be structurally
intact in idiopathic Parkinson's disease (Alvord et al., 1974). The occurrence of
many saccades with normal peak velocities in our patients implies a normal
complement of burst cells in the pons.
Slatt et al. (1966) and Chaco (1971) recorded slowed development of the
electromyographic (EMG) interference pattern is agonist ocular muscles, in
association with inappropriate coactivation of antagonist muscles during saccades.
We suggest that the slowed saccades of our patients are caused by impaired
reciprocal activation of agonist on-direction burst cells, antagonist off-direction
burst cells and inhibitory burst cells.
Cofiring of muscles can cause ocular retraction. For example, patients with
paralysis of upward saccades from dorsal midbrain damage exhibit retraction of the
eyes when they attempt to make upward saccades (Gay et al., 1963). We did not
observe ocular retraction during saccades in our patients. The amount of
coactivation required simply to slow saccades would not be expected to cause visible
retraction.
Hypometric saccades. Patients, unlike normal subjects, frequently require multiple
saccadic steps to attain desired eye position. Inappropriate coactivation of agonist
and antagonist ocular muscle pairs may explain slow saccades but not hypometric
saccades. After a brief (40 ms) targetflash,patients achievefinaldesired eye position
in complete darkness, without the benefit of continuous visual feedback, indicating
that desired eye position is correctly coded by the retinal error in Parkinson's
disease. Robinson (1975) proposed a model in which desired eye position signals
the duration of burst cell discharge while a trigger signal inhibits the pause cells, thus
releasing the burst cell discharge. According to this hypothesis, collaterals of burst
584
OWEN B. WHITE AND OTHERS
cells maintain inhibition of the pause cell and an internal copy of eye position signal
(efference copy) is fed back to inhibit the burst cell. When the efference copy of eye
position is equal to desired eye position, burst cells cease firing, pause cells resume
activity and the saccade stops.
Stimulation of pause cells in the medial pontine reticular formation of monkeys
stops saccades while in progress, and if the stimulus is sufficiently brief, saccades
subsequently resume their course to near correct final eye position (Keller, 1977).
The hypometric saccades of parkinsonism could be explained by inappropriate
pause cell activation while a saccade is in progress. Pause cell activity might explain
the irregular development of the EMG interference pattern in agonist ocular
muscles (Slatt et al., 1966; Chaco, 1971), thereby causing the slow saccadic
acceleration recorded in our patients.
Following an initial hypometric step, further saccades were generated at intervals
ranging from 10 to 1000 ms. These corrective saccades might be preprogrammed,
but a strategy of multiple saccades would delay refoveation. After pathologically
hypometric steps, corrective saccades could be mediated by visual feedback, orbital
proprioceptive feedback or by an internal (nonretinal) efference copy of eye
position. The occurrence of corrective saccades in the target flash condition
indicated that visual feedback was not required to generate corrective saccades.
Known latencies of orbital proprioceptive responses via the cerebellum or superior
colliculi, proposed relays for orbital proprioception, are too long to explain
corrective intervals less than about 30 ms (Kimura and Maekawa, 1981; Ron and
Robinson, 1973; Rose and Abrahams, 1978; Wurtz and Albano, 1980). Corrective
saccades after shorter intervals must be determined by mismatch of desired eye
position with an internal efference copy of eye position. The short latency corrective
saccades indicate that pathways transmitting internal feedback of eye position are
intact in Parkinson's disease.
Smooth Pursuit System
Smooth pursuit gain, the ratio of eye velocity to target velocity, is lowered in
Parkinson's disease. By holding target acceleration constant while changing target
velocity, amplitude and frequency, Lisberger et al. (1981) demonstrated that normal
pursuit system gain is insensitive to changes in target velocity or frequency. Then
while holding target velocity constant by changing target amplitude and frequency
inversely, they showed that pursuit gain decreases at high target accelerations. This
acceleration limitation on normal pursuit gain is called a saturating nonlinearity in
engineering terms; it is depicted by the box containing a sigmoid curve infig.7.
One of the advantages of negative feedback systems such as smooth pursuit (fig.
7) is that the closed-loop gain (k/1 + k) is relatively insensitive to changes in openloop gain (k). However, the open-loop gain is determined by neural circuits; it is the
pursuit parameter that assesses neurological dysfunction. Direct measures of openloop gain require artificial stabilization of a retinal image (Pola and Wyatt, 1981) or
monocular ophthalmoplegia. We calculated open-loop gain from the measured
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
585
closed-loop gain (G). At frequencies of 0.25 and 0.5 Hz, gain was reduced uniformly
at all target velocities, whether target acceleration was large or small. Changes in the
saturating nonlinear element that limits acceleration would reduce eye acceleration
and thereby reduce the frequency at which saturation (gain decrease) occurred.
However, changes in the saturating nonlinear element would not affect the low
frequency performance where target acceleration is minimal. The uniform reduction
in gain at low frequencies (fig. 5) indicates that the pursuit defect in Parkinson's
disease is a disorder of the gain element, not the saturating nonlinearity alone.
Reduction in pursuit gain at all target frequencies in Parkinson's disease is similar
to that recorded in cerebellar system degeneration in man (Zee et al., 1976), and after
flocculectomy in monkeys (Zee et al., 1981). It differs from impaired pursuit after
cerebral cortical damage, when low frequency pursuit gain approaches unity but
decreases (saturates) as frequency increases (Sharpe et al., 1979). The difference in
the pursuit performance suggests that cerebral cortical lesions damage the nonlinear
saturating element of the pursuit loop, whereas Parkinson's disease, like cerebellar
degeneration, involves the gain element. Little is known about the anatomical
substrates for smooth pursuit. We infer that dopaminergic nigrostriatal pathways
affect the gain element of the pursuit system.
Several sites of potential dysfunction could disrupt saccadic performance. Schiller
et al. (1980) demonstrated that combined lesions of frontal eyefieldsand superior
colliculus produce slowed small saccades. The frontal eyefieldsproject to the corpus
stria turn (Kiinzle and Akert, 1977), which in turn has a major outflow via the
substantia nigra pars reticulata to the superior colliculus (Nauta, 1979). Wurtz and
Hikosaka (1981) recorded from cells in the substantia nigra pars reticulata which
modulate with saccades and project to the superior colliculus. Microstimulation in
the superior colliculus activates pause cells in the pontine reticular formation
(Raybourn and Keller, 1977) and elicits retinotopically coded saccades (Stryker
and Schiller, 1975). Lesions of the superior colliculus produce delayed, slowed and
hypometric saccades (Schiller et al., 1980) similar to those in Parkinson's disease.
We suggest that involvement of this nigrocolliculoreticular circuit may explain the
saccadic deficits that we have described in Parkinson's disease.
ACKNOWLEDGEMENTS
This work was supported by MRC of Canada Grants ME 5509 and MT 5404 and by the Physicians
Services Incorporated Foundation of Ontario (Dr Sharpe). Dr White was a Fellow in Neuroophthalmology, supported by the PSI grant and by the Department of Medicine Fund, Toronto
Western Hospital.
We thank Drs R. D. G. Blair, G. Sawa and R. Yufe for referring patients for study, Dr W. G. Tatton
for invaluable technical assistance and C. D. Sherret for computer programming. We thank Mrs R.
Armstrong for editorial assistance.
586
OWEN B. WHITE AND OTHERS
REFERENCES
ALVORD E C, FORNO L S, KUSSKE J A, KAUFFMAN R J, RHODES J S, GOETOWSKI C R (1974) The
pathology of Parkinsonism: a comparison of degenerations in cerebral cortex and brainstem.
Advances in Neurology, 5, 175-193.
BODIS-WOLLNER I, YAHR M D (1978) Measurements of visual evoked potentials in Parkinson's disease.
Brain, 101, 661-671.
BOLLER F, MIZUTANI T, ROESSMANN U, GAMBETTI P (1980) Parkinson disease, dementia and
Alzheimer disease: clinicopathological correlations. Annals of Neurology, 7, 329-335.
CHACO J (1971) Impairment of function of the extraocular muscles in Parkinson's disease.
Ophthalmologica, 162, 343-347.
CORIN M S, ELIZAN T S, BENDER M B (1972) Oculomotor function in patients with Parkinson's disease.
Journal of the Neurological Sciences, 15, 251-265.
DEJONG J D, MELVILL JONES G (1971) Akinesia, hypokinesia, and bradykinesia in the oculomotor
system of patients with Parkinson's disease. Experimental Neurology, 32, 58-68.
EVARTS E V, TERAVAINEN H, BEUCHERT D E, CALNE D B (1979) Pathophysiology of motor
performance in Parkinson's disease. In: Dopaminergic Ergot Derivitives and Motor Function.
Edited by K. Fuxe and D. B. Calne. Oxford: Pergamon Press, pp. 45-59.
EVARTS E V, TERAVAINEN H, CALNE D B (1981) Reaction time in Parkinson's disease. Brain, 104,
167-186.
FLOWERS K A, DOWNING A C (1978) Predictive control of eye movements in Parkinson's disease.
Annals of Neurology, 4, 63-66.
GAY A J, BRODKEY J, MILLER J E (1963) Convergence retraction nystagmus. An electromyographic
study. Archives of Ophthalmology, Chicago, 70, 456-461.
GISBERGEN J A M van, ROBINSON D A, GIELEN S (1981) A quantitative analysis of generation of
saccadic eye movements by burst neurons. Journal of Neurophysiology, 45, 417-442.
HALLETT P E, LIGHTSTONE A D (1976) Saccadic eye movements to flashed targets. Vision Research 16,
107-114.
HERISHANU Y O, SHARPE J A (1981) Normal square wave jerks. Investigative Ophthalmology and Visual
Science, 20, 269-272.
HIGHSTEIN S, COHEN B, MONES R (1969) Changes in saccadic eye movements of patients with
Parkinson's disease before and after L-DOPA. Transactions of the American Neurological
Association, 94, 277-279.
HIKOSAKA O, IGUSA Y, NAKAO S, SHIMAZU H (1978) Direct inhibitory synaptic linkage of ponto-
medullary reticular burst neurons with abducens motoneurons in the cat. Experimental Brain
Research, 33, 337-352.
KELLER E L (1977) Control of saccadic eye movements by mid-line brainstem neurons. In: Control of
Gaze by Brainstem Neurons Edited by R. Baker and A. Berthoz. Amsterdam: Elsevier, pp. 327-336.
KIMURA M, MAEKAWA K (1981) Modulation of purkinje cell afferents in the flocculus by extraocular
muscle afferents. In: Progress in Oculomotor Research. Edited by A. F. Fuchs and W. Becker:
Amsterdam: Elsevier, pp. 291-296.
KUNZLE H, AKERT K (1977) Efferent connections of cortical, area 8 (frontal eye field) in Macaca
fascicularis. A reinvestigation using the autoradiographic technique. Journal of Comparative
Neurology, 173, 147-163.
LlEBERMAN A , DZIATOLOWSKI M , KUPERSMITH M , SERBY M , GOODGOLD A , KOREIN J, GOLDSTEIN M
(1979) Dementia in Parkinson disease. Annals of Neurology, 6, 355-359.
LISBERGER S G, EVINGER C, JOHANSON G W, FUCHS A F (1981) Relationship between eye acceleration
and retinal image velocity during foveal smooth pursuit in man and monkey. Journal of
Neurophysiology, 46, 229-249.
MELVILL JONES G, DEJONG J D (1971) Dynamic characteristics of saccadic eye movements in
Parkinson's disease. Experimental Neurology, 31, 17-31.
SACCADES AND PURSUIT IN PARKINSON'S DISEASE
587
NAUTA H J W (1979) A proposed conceptual reorganization of the basal ganglia and telencephalon.
Neuroscience, 4, 1875-1881.
PIROZZOLO F J, HANSCH E C (1981) Ocular motor reaction time in dementia reflects degree of cerebral
dysfunction. Science, 214, 349-350.
POLA J, WYATT H J (1981) Smooth pursuit eye movement in open and closed loop: a linear system,
roughly speaking. Society for Neuroscience Abstracts, 7, 133.
RAYBOURN M S, KELLER E L (1977) Colliculoreticular organization in primate oculomotor system.
Journal of Neurophysiology, 40, 861-878.
ROBINSON D A (1973) Models of the saccadic eye movement control system. Kybernetik, 14, 71-83.
ROBINSON D A (1975) Oculomotor control signals. In: Basic Mechanisms of Ocular Motility and their
Clinical Implications. Edited by G. Lennerstrand and P. Bach-y-Rita. Oxford: Pergamon Press,
pp. 337-374.
RON S, ROBINSON D A (1973) Eye movements evoked by cerebellar stimulation in the alert monkey.
Journal of Neurophysiology, 36, 1004-1022.
ROSE P K, ABRAHAMS V C (1978) Tectospinal and tectoreticular cells: their distribution and afferent
connections. Canadian Journal of Physiology and Pharmacology, 56, 650-658.
SANDERS M D (1975) Discussion remarks. In: Basic Mechanisms of Ocular Motility and their Clinical
Implications. Edited by G. Lennerstrand and P. Bach-y-Rita. Oxford: Pergamon Press,
pp. 393-394.
SCHILLER P H, TRUE S D, CONWAY J L (1980) Deficits in eye movements following frontal eye-field and
superior colliculus ablations. Journal of Neurophysiology, 44, 1175-1189.
SHARPE J A, HERISHANU Y O, WHITE O B (1982) Cerebral square wave jerks. Neurology, New York, 32,
57-62.
SHARPE J A, Lo A W, RABINOVITCH H E (1979) Control of the saccadic and smooth pursuit systems
after cerebral hemidecortication. Brain, 102, 387-403.
SHIBASAKI H, TSUJI S, KUROIWA Y (1979) Oculomotor abnormalities in Parkinson's disease. Archives
of Neurology, Chicago, 36, 360-364.
SLATT B, LOEFFLER J D, HOYT W F (1966) Ocular motor disturbances in Parkinson's disease.
Electromyographic observations. Canadian Journal of Ophthalmology, 1, 267-273.
STEELE J C, RICHARDSON J C, OLSZEWSKI J (1964) Progressive supranuclear palsy. A heterogeneous
degeneration involving the brainstem, basal ganglia and cerebellum with vertical gaze and
pseudobulbar palsy, nuchal dystonia and dementia. Archives of Neurology, Chicago, 10, 333-359.
STRYKER M P, SCHILLER P H (1975) Eye and head movements evoked by electrical stimulation of
monkey superior colliculus. Experimental Brain Research, 23, 103-112.
TERAVAINEN H, CALNE D B (1980) Studies of parkinsonian movement: I. Programming and execution
of eye movements. Ada Neurologica Scandinavica, 62, 137-148.
TROOST B T, DAROFF R B (1977) The ocular motor defects in progressive supranuclear palsy. Annals of
Neurology, 2, 397-403.
WHITE O B, SAINT-CYR J A, SHARPE J A (1983) Ocular motor deficits in Parkinson's disease. I. The
horizontal vestibular ocular reflex and its regulation. Brain, 106, 555-570.
WURTZ R H, ALBANO J E (1980) Visual-motor function of the primate superior colliculus. Annual
Review of Neuroscience, 3, 189-226.
WURTZ R H, HIKOSAKA O (1981) Axonal projection of visual-oculomotor cells in the substantia nigra
to the superior colliculus. Society for Neuroscience Abstracts, 7, 132.
YOUNG L R, STARK L (1962) A sampled-data model for eye movement tracking movements. In:
Quarterly Progress Report Research Laboratory for Electronics, 66, 370-384.
370-384.
ZEE D S, YEE R D, COGAN D G, ROBINSON D A, KING ENGEL W (1976) Ocular motor abnormalities in
hereditary cerebellar ataxia. Brain, 99, 207-234.
ZEE D S, YAMAZAKJ A, BUTLER P H, GUCER G (1981) Effects of ablation of flocculus and paraflocculus
on eye movements in primate. Journal of Neurophysiology, 46, 878-899.
(Received July 7,1982. Revised November 23,1982)