Alcohol & Alcoholism Vol. 39, No. 4, pp. 340–345, 2004
doi:10.1093/alcalc/agh064, available online at www.alcalc.oupjournals.org
BLOOD ALCOHOL IS THE BEST INDICATOR OF HAZARDOUS ALCOHOL
DRINKING IN YOUNG ADULTS AND WORKING-AGE PATIENTS WITH TRAUMA
OLLI SAVOLA1*, ONNI NIEMELÄ2 and MATTI HILLBOM1
1
Department of Neurology, Oulu University Hospital, Oulu and 2Department of Laboratory Medicine, Tampere University,
Tampere and Seinäjoki Central Hospital, Seinäjoki, Finland
(Received 19 September 2003; first review notified 1 December 2003; in revised form 18 March 2004; accepted 20 March 2004)
frequent binge drinking is a growing problem in most Western
countries and often precedes the sequence of events leading to
chronic alcoholism (Chikritzhs et al., 2001; Goldberg, 2002;
Naimi et al., 2003).
The present study set out to compare the usefulness of
various diagnostic tools for identifying hazardous drinking
among trauma patients.
INTRODUCTION
Alcohol drinking and its consequences are currently one of the
major health hazards worldwide (Kristenson et al., 1982; Hasin
et al., 1990; Anderson et al., 1993; Lieber, 1995; Chikritzhs
et al., 2001), creating significant financial burdens for societies
(Rice et al., 1991; Goldberg, 2002). Excessive alcohol
consumption is closely linked with trauma-related hospital
admissions, especially in young adults and working-age
individuals (Peppiatt et al., 1978; Baker et al., 1992; Jurkovich
et al., 1992; Rivara et al., 1993; Nilssen et al., 1994; Corrigan,
1995). Alcohol potentiates vulnerability to injury (Waller et al.,
1986), causes diagnostic and therapeutic difficulties in the
management of trauma patients (Jurkovich et al., 1992), and
has an exacerbating effect on the outcome of injury (Waller
et al., 1986; Rönty et al., 1993; Corrigan, 1995).
There is a high incidence of hazardous drinkers among the
patients admitted to accident and emergency departments
(Soderstrom and Cowley, 1987; Charalambous, 2002). Their
early identification is needed for the initiation of a brief
alcohol intervention. However, alcohol-related health
problems continue to escape detection by clinicians. Despite
accumulating evidence showing that brief alcohol
interventions are effective in reducing alcohol drinking (AnttiPoika et al., 1988; Walsh et al., 1991; Maheswaran et al.,
1992; Fleming et al., 1997) and the risk of injury recurrence
(Dinh-Zarr et al., 1999; Gentilello et al., 1999), there
continues to be a lack of attention to alcohol problems
(Soderstrom and Cowley, 1987). It would be particularly
important to detect not only dependent drinkers but also the
patients who are binge drinkers as early as possible, because
SUBJECTS AND METHODS
Patients
The study was conducted at a hospital that treats all trauma
patients, with or without referral from primary health care,
in a city of 120 000 inhabitants. We logged 385 consecutive
admissions in the age range 16–49 years showing evidence of
physical trauma needing assessment and treatment by the
emergency room physician. We could not include in the
analysis 36 patients in whom completed interview material
(see below) was not obtained (this included three fatal cases).
Thus our series comprised 349 patients (252 men, 97 women).
After immediate critical care, all clinical data, including the
cause, type and extent of the injury, and the patient’s health
status, which also included history of infections (HIV/AIDS,
hepatitis B and C), liver status, use of alcohol, medications,
illicit drugs and smoking, were recorded by trained emergency
department physicians based on a structured questionnaire
designed for this purpose. The Injury Severity Score (ISS)
(Baker et al., 1974; Copes et al., 1988) was used as an index
of trauma severity. The study was approved by the ethics
committee of the hospital, and informed consent was obtained
from all patients or their close relatives.
Alcohol data
Venous blood samples were obtained from all the patients for
determinations of the mean corpuscular volume (MCV) of
*Author to whom correspondence should be addressed at: Department
of Neurology, Oulu University Hospital, Box 25, Oulu, FIN-90029, Finland.
Tel.: +358 8 315 4137; Fax: +358 8 315 4544; E-mail: osavola@paju.oulu.fi
340
Alcohol & Alcoholism Vol. 39, No. 4 © Medical Council on Alcohol 2004; all rights reserved
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
Abstract — Aims: To determine the most effective marker of hazardous alcohol drinking in trauma patients. Methods: A prospective
study of 349 trauma patients aged 16–49 years admitted into a general hospital trauma centre. Information on the amount and pattern
of alcohol drinking was obtained by interview. Blood or breath alcohol concentration (BAC), serum gammaglutamyl transferase
(GGT), aspartate aminotransferase (AST), carbohydrate-deficient transferrin (CDT) and the mean corpuscular volume (MCV) of
erythrocytes were measured as markers of alcohol consumption. Results: In this series, 8% of all trauma patients were found to be
dependent drinkers, while 61% were frequent binge drinkers, 17% infrequent binge drinkers, 8% light-to-moderate drinkers and 6%
nondrinkers. On admission, the BAC test was positive in 68% of the hazardous drinkers (i.e. dependent drinkers or frequent binge
drinkers). Using a cut-off level of >0 mg/dl, the sensitivity and specificity of the BAC test for identifying hazardous drinking were 68%
(95% confidence intervals [CI], 61–73%) and 94% (95% CI, 87–97%), respectively, and the positive predictive value was 96% (95%
CI, 92–98%). GGT, MCV, CDT and AST were less accurate indicators of hazardous drinking. BAC was the least expensive marker.
Conclusions: Two-thirds of trauma patients were hazardous drinkers, and blood alcohol on admission was an accurate indicator of this.
BAC should be systematically used in trauma centres if patients are to be selected for an alcohol intervention.
ALCOHOL MARKERS AND INJURY
Laboratory procedures
Venous blood samples were obtained immediately after
admission and not later than 6 h after the trauma event,
centrifuged and stored at –20C until analysed for the various
markers in an accredited (SFS-EN 45001, ISO/IEC Guide 25)
clinical chemistry laboratory. MCV, GGT, AST and CDT
were measured from every patient, with the exception of MCV,
which was determined from 288 patients (83%). Blood alcohol
concentrations were measured using a Vitros 250 clinical
chemistry analyser (Johnson and Johnson, Rochester, NY).
ALCO-SENSOR III (Intoximeters, St Louis, MO) was
used for the breath analyses. Serum CDT was measured
with a competitive radioimmunoassay after microcolumn
separation (CDTect; AxisShield, Oslo, Norway). MCV,
GGT and AST were measured using standard laboratory
methods.
In the analyses for the diagnostic characteristics of the
markers, the following cut-off’s were used: MCV (>96 fl for
women and men), GGT (>50 U/l for women, >80 U/l for
men), AST (>35 U/l for women, >50 U/l for men) and CDT
(>26 U/l for women, >20 U/l for men).
The costs of the different markers of alcohol consumption
were also calculated. The costs of obtaining a blood sample,
the assay procedure, labour work and overheads were
included. Costs were expressed as US dollars.
Statistical methods
Sensitivities, specificities, positive and negative predictive
values, and 95% confidence intervals (CI) of the different
markers of alcohol consumption for detecting hazardous
drinking were calculated by the exact method using the CIA
statistical software for Windows. Odds ratios and 95% CI,
Student’s t-test, Mann–Whitney U-test, and univariate associations of continuous variables were tested with Spearman’s
rank correlation coefficients (rs) when appropriate and by
using SPSS version 10.0 for Windows.
RESULTS
Clinical characteristics and causes of injury are shown in
Table 1. Men and women were of the same age (31.3 ± 10 vs
30.8 ± 11 years, Student’s t-test: P = 0.726). Eight per cent of
the patients were classified as dependent drinkers, while 61%
were frequent binge drinkers and 17% infrequent binge
drinkers (Table 2). The group of light-to-moderate drinkers
and nondrinkers represented 8 and 6% of the study population,
respectively. Smoking was common among the dependent
drinkers (81%) and the frequent binge drinkers (64%). Use of
illicit drugs at the time of injury was verified in five patients,
all of whom were frequent binge drinkers.
Sex
Men were frequent binge drinkers or dependent drinkers more
often than women (OR 2.7, 95% CI 1.7–4.4). In addition, men
(72/252, 27%) were clinically strongly intoxicated more often
than women (15/97, 15%) (OR 2.2, 95% CI 1.2–4.0). In those
patients who had alcohol in blood, men had higher
concentrations than women (2.0 ± 1.0 vs 1.7 ± 0.8, Student’s
t-test: P < 0.05).
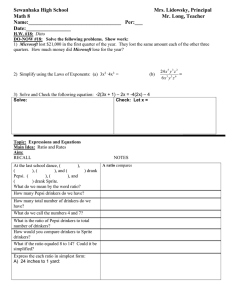
Table 1. Clinical characteristics of the trauma patients
Variable
No. patients
Age, mean ± SD (years)
Causes of injury:
Traffic accident
Fall
Assault
Sport
Others
Total
Men
Women
349
31 ± 10
252 (72%)
31 ± 10
97 (28%)
30 ± 11
79 (23%)
83 (24%)
54 (15%)
22 (6%)
111 (32%)
53 (21%)
56 (22%)
46 (18%)
16 (7%)
81 (32%)
26 (27%)
27 (28%)
8 (8%)
6 (6%)
30 (31%)
4±4
3±3
35 (14%)
9 (9%)
57 (23%)
17 (18%)
113 ± 137
51 ± 73
317 ± 462
106 ± 154
33 ± 43
10 ± 13
Injury Severity Score,
4 ± 4 (1–25)
mean ± SD (range)
Operation room
44 (13%)
surgery, n (%)
Hospital stay >2 days,
74 (21%)
n (%)
Alcohol consumption, mean ± SD:
During 24 h prior
96 ± 126
to injury (g)
During 1 week prior
258 ± 412
to injury (g)
During 1 year prior
27 ± 38
to injury (g/day)
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
erythrocytes, serum gammaglutamyl transferase (GGT),
aspartate aminotransferase (AST), and carbohydrate-deficient
transferrin (CDT). Alcohol concentration (BAC) was
determined either from breath air (BrAC) (n = 184) or from
serum samples (BlAC) (n = 165). The amount and pattern of
alcohol consumption was recorded by one of us (O.S.),
blinded to the data on the biochemical markers of alcohol
consumption and BAC. Interviews were carried out using a
structured interview protocol during a follow-up visit within
6 weeks of injury. The history of alcohol consumption
included the following information: how many drinks of
alcohol (standard drink = 12 g ethyl alcohol corresponding to
one beer, one glass of table wine or 4 cl 40% proof spirit)
the patient had consumed during (1) 24 h, and (2) 1 week
preceding injury. Daily alcohol consumption during the period
1 year prior to the trauma was assessed using ‘time-line follow
back’ (Sobell and Sobell, 1995). Based on the data, the
patients were classified into groups as follows: dependent
drinkers (‘alcoholics’), binge drinkers, light-to-moderate
drinkers and nondrinkers. The dependent drinkers were those
who showed clinical evidence of pathological alcohol use,
social impairment and tolerance/withdrawal. In these
individuals, the daily alcohol consumption had exceeded a
mean of 80 g. Binge drinking was defined as an ethanol intake
of six or more (men) or four or more (women) standard drinks
of alcohol in one session. Binge drinkers were further divided
into two groups: frequent binge drinkers reported binge-type
drinking more than once monthly. Infrequent binge drinkers
reported binging 1–11 times per year. Light-to-moderate
drinkers consumed one to two standard drinks per day either
daily or less frequently. Nondrinkers had not drunk any
alcohol during the year preceding the injury. They included
both life-long abstainers and ex-drinkers. Dependent drinkers
and frequent binge drinkers together made up the group
referred to as hazardous drinkers.
341
342
O. SAVOLA et al.
Table 2. Characteristics of the patients classified according to the history of alcohol consumption (n = 349)
Dependent drinkers
Frequent binge drinkers
Infrequent binge drinkers
Light-to-moderate drinkers
Nondrinkers
Patients
n (%)
Women
n (%)
Age (years)
mean ± SD
BAC (mg/dl) on
admission
mean ± SD
26 (8)
214 (61)
59 (17)
28 (8)
22 (6)
0
51 (24)
25 (42)
14 (50)
7 (32)
38 ± 9
30 ± 10
33 ± 10
31 ± 12
30 ± 12
210 ± 160
120 ± 110
20 ± 70
0 ± 10
0
Clinically
intoxicated
on admission
n (%)†
Consumption of alcohol
during the preceding
year (g/day) mean ±
SD, women/men
Smoking
n (%)
20 (77)
124 (58)
5 (8)
1 (4)
0
137 ± 45‡
16 ± 15/27 ± 20
6 ± 3/6 ± 6
2 ± 1/4 ± 4
0/0
21 (81)
138 (64)
15 (25)
5 (18)
6 (27)
BAC, blood alcohol concentration (100 mg/dl = 22 mmol/l). †Data from hospital record; ‡men only.
Table 3. Spearman’s rank correlation coefficients between reported consumption of alcohol and laboratory markers (n = 349)
BAC
GGT
MCV
CDT
AST
Preceding 24 h
Preceding week
Preceding year
0.866
0.655
0.530
0.336
0.412
0.459
0.233
0.338
0.368
0.328
0.339
0.273
0.234
0.346
0.352
P < 0.001.
Table 4. Percentages of trauma patients showing alcohol in blood and positiveness of biochemical markers suggesting alcohol use (n = 349)
Sensitivity
mg/dL
Dependent drinkers
Frequent binge drinkers
Infrequent binge drinkers
Light-to-moderate drinkers
Non-drinkers
BAC >0 mg/dl
BAC 100 mg/dl
BAC 150 mg/dl
BAC 200
+ve GGT
+ve MCV
+ve CDT
+ve AST
81
66
10
4
0
69
56
10
0
0
65
46
7
0
0
58
29
5
0
0
42
16
3
0
5
22
18
8
0
5
46
32
9
18
14
42
14
5
0
14
Cut-off values: AST (50/35 U/l, men/women); CDT (20/26 U/l, men/women); GGT (80/50 U/l, men/women); MCV (96 fl, men and women). MCV
was measured from 288 (83%) of the interviewed patients (n = 349). BAC, blood alcohol concentration (100 mg/dl = 22 mmol/l).
Table 3 summarizes Spearman’s rank correlation coefficients
between self-reported alcohol consumption at different time
periods prior to sampling and laboratory marker values. BAC,
as measured either from breath air (BrAC) or serum (BlAC) at
admission, correlated with reported alcohol intake at each of the
three time periods more strongly than any of the other markers.
BAC correlated strongly not only with acute drinking as would
be expected, but also with both recent drinking (preceding
week) and chronic drinking (past year).
The relationships between markers and pattern of drinking
are shown in Table 4. BAC, even at several different cut-off
points, appeared to be the most sensitive indicator of hazardous
drinking. Altogether 81% of dependent drinkers, 66% of
frequent binge drinkers, and 10% of infrequent binge drinkers
were BAC-positive on admission. Among the binge drinkers,
the proportion of BAC-positive patients decreased sharply with
increasing BAC cut-offs, whereas 58% of the dependent
drinkers were at or above the cut-off level of 200 mg/dl.
GGT, MCV, CDT and AST showed sensitivities of 42, 22,
46 and 42% among the dependent drinkers, respectively. The
sensitivities for the frequent binge drinkers were 16, 18,
32 and 14%, respectively. These markers were also
positive for some of the light-to-moderate drinkers and even
abstainers.
The sensitivities, specificities and positive and negative
predictive values of the different alcohol markers for detecting
hazardous alcohol drinking (including dependent drinkers and
frequent binge drinkers) are shown in Table 5. Taken together,
240 (69%) of the consecutive trauma patients reported hazardous
alcohol drinking. Of these, 137 (57%) had BAC (blood/breath
alcohol) above 100 mg/dl. When a cut-off of >0 mg/dl was used,
the sensitivity of identifying hazardous alcohol drinkers
increased to 68% (95% CI, 61–73%) with a positive predictive
value of 96% (95% CI, 92–98%). Thus, 96% of the
BAC-positive trauma patients proved to be hazardous alcohol
drinkers.
We also studied the correlation between markers and
alcohol intake separately for men and women. MCV, CDT and
BAC correlated statistically significantly to the amount of
alcohol consumed during the preceding year (Mann–Whitney
U-test: P < 0.01) both in men and women, but AST and GGT
correlated more strongly with alcohol intake in men than in
women.
In the cost analyses of the various markers, measurement of
alcohol from breath air was found to be the least expensive
method for assessing hazardous drinking (Table 5). We further
analysed the usefulness of various combinations of biochemical markers. BAC (>0 mg/dl) together with CDT was
the most sensitive combination, which correctly identified
73% of the target population. However, even though both CDT
and GGT slightly improved sensitivity when combined with
BAC, the additional effect did not reach significance.
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
Reported alcohol consumption
ALCOHOL MARKERS AND INJURY
343
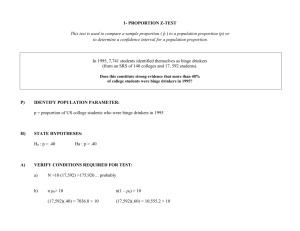
Table 5. Sensitivities, specificities, positive predictive values (PPV), negative predictive values (NPV), and costs of the different markers of alcohol
consumption for detecting hazardous alcohol drinking (including dependent drinkers and frequent binge drinkers) in trauma patients (n = 349)
Screening test
BAC >0 mg/dL, (95% CI)
BAC >100 mg/dL
GGT
MCV
CDT
AST
Sensitivity
Specificity
PPV
NPV
68% (61 to 73%)
57% (51 to 63%)
11% (8 to 16%)
18% (13 to 24%)
33% (28 to 40%)
17% (13 to 22%)
94% (87 to 97%)
94% (89 to 98%)
97% (92 to 99%)
94% (88 to 98%)
88% (81 to 93%)
94% (89 to 98%)
96% (92 to 98%)
96% (91 to 98%)
90% (74 to 97%)
88% (75 to 95%)
86% (78 to 92%)
87% (74 to 94%)
57% (49 to 64%)
50% (43 to 57%)
33% (28 to 39%)
34% (28 to 40%)
38% (32 to 44%)
34% (29 to 40%)
Cost
0.56†/11.7 ‡
2.3
3.0
11.5
2.3
The calculations were performed between hazardous and non-hazardous drinkers: hazardous alcohol drinkers, frequent binge drinkers or alcohol dependent
drinkers; non-hazardous alcohol drinkers, infrequent binge drinkers, light-to-moderate drinkers and non-drinkers. Cut-off values: AST (50/35 U/l,
men/women); CDT (CDTect method) (20/26 U/l, men/women); GGT (80/50 U/l, men/women); MCV (96 fl, men and women). BAC, blood alcohol
concentration (100 mg/dl = 22 mmol/l). Cost per one measurement as US dollars (USD): ‡cost per one measurement from breath air; ‡cost per one
measurement from blood sample. MCV was measured from 288 (83) of the interviewed patients (n = 349).
BAC was the most accurate marker of hazardous alcohol
drinking in trauma patients. Ninety-six per cent of the BACpositive trauma patients reported hazardous alcohol drinking.
BAC was more sensitive and specific than the conventional
biochemical markers of alcohol misuse. Therefore, BAC
measurements should be systematically included in the
assessment of trauma patients and used as a basis to guide
patients to alcohol interventions at trauma centre.
Binge-type drinking was the most common pattern of
hazardous drinking (61%) among trauma patients, whereas
chronic heavy drinking appeared to be less frequent (8%).
These findings are consistent with the view that the harm
caused by alcohol is not restricted to those who are dependent
drinkers (Lieber, 1995; Niemelä, 2002; Naimi et al., 2003).
Growing evidence is currently available to indicate that
adverse social, health and economic consequences of periodic
heavy drinking exceed those of the chronic effects (Chikritzhs
et al., 2001; Goldberg, 2002). Although the latter may be
responsible for most deaths, acute alcohol-related accidents
may account for the greatest proportion of years of life lost
(Chikritzhs et al., 2001). Early detection of binge-type
drinking should therefore be emphasized, since possible
interventions are expected to benefit especially those who are
not yet dependent drinkers, but at the beginning of a path
towards alcoholism.
However, there continues to be a lack of attention in trauma
centres to the patients who are hazardous drinkers (Soderstrom
and Cowley, 1987; Charalambous, 2002). Patients with alcohol
problems tend to remain without specific treatment, although a
positive effect of brief alcohol intervention in reducing alcohol
intake and its adverse consequences, such as readmissions due to
trauma, has been found in several studies (Antti-Poika et al.,
1988; Walsh et al., 1991; Maheswaran et al., 1992; Fleming et al.,
1997; Dinh-Zarr et al., 1999; Gentilello et al., 1999;
Longabaugh et al., 2001). This might be due to the lack of
practical tools for identifying the target groups. Thus, a simple
and inexpensive method for detecting hazardous drinkers
would be of utmost importance.
The occurrence of different drinking patterns in trauma
patients has so far been poorly investigated. The methods used
to detect alcohol misuse previously have varied greatly, and
the incidences of hazardous drinking have therefore also
varied from 10 to 66% (Peppiatt et al., 1978; Brismar et al.,
1983; Rivara et al., 1993; Corrigan, 1995; Dikmen et al.,
1995; McLeod et al., 1999; Ryb et al., 1999). The identification
of alcohol misuse can be based on clinical history, specific
questionnaires, and laboratory markers (Ewing, 1984; Skinner
et al., 1986; Davis et al., 1987; Ross et al., 1990; Nilssen et al.,
1994). Questionnaires may be fairly sensitive and specific
(Bernadt et al., 1982), but their realistic use among trauma
patients is limited because they require time and full
cooperation by the patient. Previous studies on various
laboratory markers have concentrated primarily on dependent
drinkers (Bernadt et al., 1982; Mihas and Tavassoli, 1992;
Hartz et al., 1997). However, laboratory markers could be
helpful compared to questionnaires, because many of the
trauma patients are having blood taken anyway, and no extra
procedure needs to be carried out (Huntley et al., 2001). The
reported sensitivities have varied within 30–62% for GGT and
AST, 30–40% for MCV and 83–90% for CDT (Bernadt et al.,
1982; Mihas and Tavassoli, 1992; Niemelä, 2002). Nilssen et al.
(1994) found elevated GGT in 21% of men and 15% of women
with trauma, but elevated MCV in only 5%. Rivara et al. (1993)
found increased GGT in 28% of intoxicated trauma patients
and in 11% of nonintoxicated patients. Ryb et al. (1999)
concluded that BAC is the best detector of alcohol dependence
in trauma patients and that GGT, AST and MCV have little
value as screening tests.
Yates et al. (1987) reported that questionnaires were better
than conventional biochemical markers to identify problem
drinkers in the emergency department. In our study, the
conventional biochemical markers (GGT, MCV, CDT and
AST) were all found to lack sensitivity and specificity,
especially for detecting binge drinkers. Interestingly, the
specificity of CDT in this study was also markedly lower than
that found in previous studies. It should be noted, however, that
previous studies have usually contrasted teetotalers and
alcoholics with severe dependence. The specificity of CDT
(when analysed with the CDTect method) may also be poor in
patients showing elevations in serum total transferrin levels,
which may occur, for example, in patients with iron deficiency.
However, it should be noted that, at this time, underreporting of
alcohol consumption cannot be ruled out in individual patients.
Combinations of various laboratory tests did not offer any
additional benefit for this purpose, possibly due to a variety of
sources causing unspecificity in these assays (Niemelä, 2002).
Instead, BAC on admission was found to be a sensitive (68%)
and specific (94%) marker of all types of hazardous alcohol use,
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
DISCUSSION
344
O. SAVOLA et al.
Acknowledgements — The studies were supported in part by The Oulu
Medical Foundation (OS) and the Finnish Foundation for Alcohol Studies
(ON). We thank Risto Bloigu MSc for his statistical help.
REFERENCES
Anderson, P., Cremona, A., Paton, A., Turner, C. and Wallace, P. (1993)
The risk of alcohol. Addiction 88, 1493–1508.
Anton, R. F. and Moak, D. H. (1998) Carbohydrate-deficient transferrin
and gammaglutamyltransferase as markers of heavy alcohol
consumption: gender differences. Alcoholism: Clinical and
Experimental Research 18, 747–754.
Antti-Poika, I., Karaharju, E., Roine, R. and Salaspuro, M. (1988)
Intervention of heavy drinking—a prospective and controlled study
of 438 consecutive injured male patients. Alcohol and Alcoholism
23, 115–121.
Baker, S. P., O’Neil, B., Ginsburg, M. J. and Li, G. (1992) The Injury
Fact Book. Oxford University Press, New York.
Baker, S. P., O’Neil, B., Haddon, W. and Long, W. B. (1974) The injury
severity score: a method for describing patients injuries and
evaluating emergency care. Journal of Trauma 14, 187–196.
Bernadt, M. W., Mumford, J., Taylor, C., Smith, B and Murray, R. M.
(1982) Comparison of questionnaire and laboratory tests in the
detection of excessive drinking and alcoholism. Lancet 1, 325–328.
Brismar, B., Engström, A. and Rydberg, U. (1983) Head injury and
intoxication: a diagnostic and therapeutic dilemma. Acta Chirurgica
Scandinavica 149, 11–14.
Charalambous, M. P. (2002) Alcohol and the accident and emergency
department: a current review. Alcohol and Alcoholism 37, 307–312.
Chikritzhs, T. N., Jonas, H. A., Stockwell, T. R., Heale, P. F. and
Dietze, P. M. (2001) Mortality and life-years lost due to alcohol: a
comparison of acute and chronic causes. Medical Journal Australia
174, 281–284.
Conigrave, K. M., Degenhardt, L. J., Whitfield, J. B., Saunders, J. B.,
Helander, A. and Tabakoff, B. and the WHO/ISBRA Study Group
(2002) CDT, GGT, and AST as markers of alcohol use: the WHO/
ISBRA collaborative project. Alcoholism: Clinical and Experimental
Research 26, 332–339.
Copes, W. S., Champion, H. R., Sacco, W. J., Lawnick, M. M.,
Keast, S. L. and Bain, L. W. (1988) The injury severity score
revisited. Journal of Trauma 28, 69–77.
Corrigan, J. D. (1995) Substance abuse as a mediating factor in
outcome from traumatic brain injury. Archives Physical Medicine
and Rehabilitation 76, 302–309.
Davis, L. J. Jr, Hurt, R. D., Morse, R. M. and O’Brien, P. C. (1987)
Discriminant Analysis of the Self-Administered Alcoholism Screening
Test. Alcoholism: Clinical and Experimental Research 11, 269–273.
Dikmen, S. S., Machamer, J. E., Donovan, D. M., Winn, H. R. and
Temkin, N. R. (1995) Alcohol use before and after traumatic head
injury. Annals of Emergency Medicine 26, 167–176.
Dinh-Zarr, T., DiGuiseppi, C., Heitman, E. and Roberts, I. (1999)
Preventing injuries through interventions for problem drinking: a
systematic review of randomized controlled trials. Alcohol and
Alcoholism 34, 609–621.
Ewing, J. A. (1984) Detecting alcoholism. The CAGE questionnaire.
Journal of the American Medical Association 252, 1905–1907.
Fleming, M. F., Barry, K. L., Manwell, L. B., Johnson, K. and London, R.
(1997) Brief physician advice for problem alcohol drinkers. A
randomized controlled trial in community-based primary care
practices. Journal of the American Medical Association 277,
1039–1045.
Gentilello, L. M., Rivara, F. P., Donovan, D. M., Jurkovich, G. J.,
Daranciang, E., Dunn, C. W., Villaveces, A., Copass, M. and Ries, R. R.
(1999) Alcohol interventions in a trauma center as a means of
reducing the risk of injury recurrence. Annals of Surgery 230,
473–480.
Goldberg, J. (2002) Economic impact of motor vehicle crashes. Annals
of Emergency Medicine 40, 429–430.
Hartz, A. J., Guse, C. and Kajdacsy-Balla, A. (1997) Identification of
heavy drinkers using a combination of laboratory tests. Journal of
Clinical Epidemiology 50, 1357–1368.
Hasin, D., Grant, B., Harford, T., Hilton, M. and Endicott, J. (1990)
Multiple alcohol-related problems in the United States: on the rise?
Journal Studies of Alcohol 51, 485–493.
Huntley, J. S., Blain, C., Hood, S. and Touquet, R. (2001) Improving
detection of alcohol misuse in patients presenting to an Accident
and Emergency Department. Emergency Medicine Journal 18,
99–104.
Jurkovich, G. J., Rivara, F. P., Gurney, J. G., Seguin, D., Fligner, C. L.
and Copass, M. (1992) Effects of alcohol intoxication on the initial
assessment of trauma patients. Annals of Emergency Medicine 21,
704–708.
Kraus, J. F. (1993) Epidemiology of head injury. In Head Injury,
Cooper, P. R., ed., pp. 1–25. Williams and Wilkins, Baltimore.
Kristenson, H., Peterson, B., Trell, E. and Hood, B. (1982)
Hospitalization and alcohol-related morbidity within three years after
screening in middle-aged men. Drug and Alcohol Dependence 9,
325–333.
Levin, H. S. (1993) Neurobehavioral sequelae of head injury. In
Head Injury, Cooper, P. R., ed., pp. 525–551. Williams and Wilkins,
Baltimore.
Lieber, C. S. (1995) Medical disorders of alcoholism. New England
Journal of Medicine 333, 1058–1065.
Longabaugh R., Woolard, R. E., Nirenberg, T. D., Minugh, A. P.,
Becker, B., Clifford, P. R., Carty, K., Licsw, Sparadeo, F. and
Gogineni, A. (2001) Evaluating the effects of a brief motivational
intervention for injured drinkers in the emergency department.
Journal Studies of Alcohol 62, 806–816.
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
including binge drinking and chronic alcoholism. Ninety-six
per cent of all BAC-positive trauma patients turned out to be
hazardous alcohol drinkers. Although false-positive findings
may occur, our data suggest that they are rare. Therefore, those
who guide all BAC-positive trauma patients towards an alcohol
intervention will seldom be subjecting people to an unacceptable
degree of stigma as problem drinkers. Indeed, due to the high
sensitivity, specificity and positive predictive value and the
relatively low costs of analysis, BAC can be recommended as a
primary screening tool to guide patients towards an alcohol
intervention before severe dependency develops.
Here we focused on young adults and working-age
individuals because the highest rates of morbidity, mortality
and persistent functional and psychological impairment due
to trauma are known to occur in this group (Soderstrom and
Cowley, 1987; Kraus, 1993; Levin, 1993). Therefore, our
findings cannot be generalized to all age groups. The drinking
habits of adolescents and elderly people may differ from those
observed here.
An obvious limitation of the BAC test is that it does not
detect hazardous drinkers who are not drinking prior to
admission. Although false-positive findings may also be
expected to occur, our data suggest that such findings are rare in
trauma clinics. It should also be noted that this was a mixed-sex
study and that there may be differences in the characteristics
of biochemical markers of alcohol intake between men and
women (Anton and Moak, 1998; Sillanaukee, et al., 1998;
Wetterling et al., 1998; Tønnesen et al., 1999; Conigrave et al.,
2002). However, we believe this does not change our main
result, because BAC was found to be the best indicator of
alcohol intake also when men and women were analyzed
separately. Despite these possible limitations, our finding that
BAC is the best detector of hazardous alcohol drinking in
trauma patients is encouraging, and further studies on the effects
of brief alcohol interventions in all BAC-positive trauma
patients appear to be warranted (Longabaugh et al., 2001).
ALCOHOL MARKERS AND INJURY
Ryb, G. E., Soderstrom, C. A., Kufera, J. A., Dischinger, P. C. and
Ho, S. M. (1999) Use of blood alcohol concentration and laboratory
tests to detect current alcohol dependence in trauma center patients.
Journal of Trauma 47, 874–879.
Sillanaukee, P., Aalto, M. and Seppä, K. (1998) Carbohydrate-deficient
transferrin and conventional alcohol markers as indicators for brief
intervention among heavy drinkers in primary health care.
Alcoholism: Clinical and Experimental Research 22, 892–896.
Skinner, H. A., Holt, S., Sheu, W. J. and Israel, Y. (1986) Clinical versus
laboratory detection of alcohol abuse: the alcohol clinical index.
British Medical Journal (Clinical Research Edition) 292, 1703–1708.
Sobell, L. and Sobell, M. (1995) Alcohol consumption measures.
In Assessing Alcohol Problems: A Guide for Clinicians and
Researchers, Allen, J. P. and Columbus, M., eds, pp. 55–73. NIAAA
Treatment Handbook Series No. 4, Department of Health and
Human Services, Washington DC.
Soderstrom, C. A. and Cowley, R. A. (1987) A national alcohol and
trauma center survey. Missed opportunities, failures of responsibility.
Archives of Surgery 122, 1067–1071.
Tønnesen, H., Carstensen, M. and Maina, P. (1999) Is carbohydrate
deficient transferrin a useful marker of harmful alcohol intake among
surgical patients? European Journal of Surgery 165, 522–527.
Waller, P. F., Stewart, J. R., Hansen, A. R., Stutts, J. C., Popkin, C. L. and
Rodgman, E. A. (1986) The potentiating effects of alcohol on driver
injury. Journal of the American Medical Association 256, 1461–1466.
Walsh, D. C., Hingson, R. W., Merrigan, D. M., Levenson, S. M.,
Cupples, L. A., Heeren, T., Coffman, G. A., Becker, C. A., Barker, T. A.
and Hamilton, S. K. (1991) A randomized trial of treatment options
for alcohol-abusing workers. New England Journal of Medicine 325,
775–782.
Wetterling, T., Kanitz, R. D., Rumpf, H. J., Hapke, U. and Fischer, D.
(1998) Comparison of cage and mast with the alcohol markers CDT,
gamma-GT, ALAT, ASAT and MCV. Alcohol and Alcoholism 33,
424–430.
Yates, D. W., Hadfield, J. M. and Peters, K. (1987) The detection of
problem drinkers in the Accident and Emergency Department.
British Journal of Addiction 82, 163–167.
Downloaded from http://alcalc.oxfordjournals.org/ at Pennsylvania State University on February 28, 2014
Maheswaran, R., Beevers, M. and Beevers, D. G. (1992) Effectiveness
of advice to reduce alcohol consumption in hypertensive patients.
Hypertension 19, 79–84.
McLeod, R., Stockwell, T., Stevens, M. and Phillips, M. (1999) The
relationship between alcohol consumption patterns and injury.
Addiction 94, 1719–1734.
Mihas, A. A. and Tavassoli, M. (1992) Laboratory markers of ethanol
intake and abuse: a critical appraisal. American Journal of the
Medical Sciences 303, 415–428.
Naimi, T. S., Brewer, R. D., Mokdad, A., Denny, C., Serdula, M. K. and
Marks, J. S. (2003) Binge drinking among US adults. Journal of the
American Medical Association 289, 70–75.
Niemelä, O. (2002) Serum Diagnosis of Alcoholic Liver Disease and
Markers of Ethanol Intake. In Ethanol and the Liver, Sherman, D. I. N.,
Preedy, V. and Watson, R. R., eds, pp. 411–449. Taylor and Francis,
New York and London.
Nilssen, O., Ries, R. K., Rivara, F. P., Gurney, J. G. and Jurkovich, G. J.
(1994) The CAGE questionnaire and the Short Michigan Alcohol
Screening Test in trauma patients: comparison of their correlations
with biological alcohol markers. Journal of Trauma 36, 784–788.
Peppiatt, R., Evans, R. and Jordan, P. (1978) Blood alcohol
concentration of patients attending an accident and emergency
department. Resuscitation 6, 37–43.
Rice, D. P., Kelman, S. and Miller, L. S. (1991) Estimates of economic
costs of alcohol and drug abuse and mental illness, 1985 and 1988.
Public Health Reports 106, 280–292.
Rivara, F. P., Jurkovich, G. J., Gurney, J. G., Seguin, D., Fligner, C. L.
Ries, R., Raisys, V. A. and Copass, M. (1993) The magnitude of
acute and chronic alcohol abuse in trauma patients. Archives of
Surgery 128, 907–912.
Ross, H. E., Gavin, D. R. and Skinner, H. A. (1990) Diagnostic validity
of the MAST and the alcohol dependence scale in the assessment of
DSM-III alcohol disorders. Journal of Studies of Alcohol 51,
506–513.
Rönty, H., Ahonen, A., Tolonen, U., Heikkilä, J. and Niemelä, O.
(1993) Cerebral trauma and alcohol abuse. European Journal of
Clinical Investigation 23, 182–187.
345