SABCS 2014 -‐ ANCO REVIEW SABCS 2014 – Surgery Review
advertisement
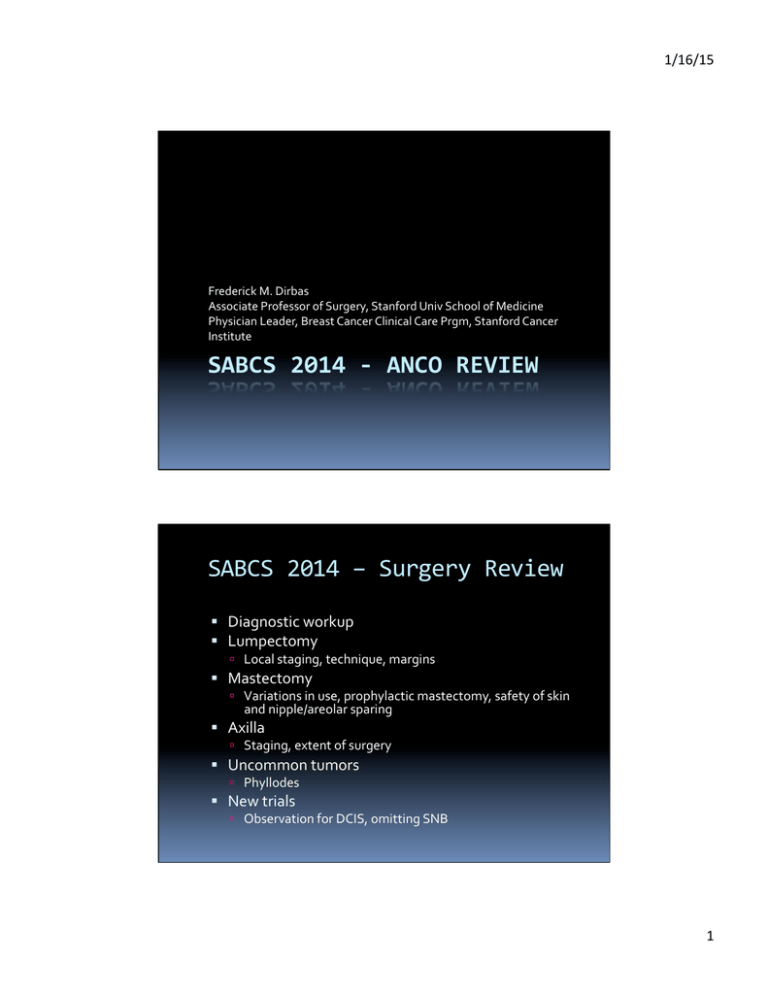
1/16/15 Frederick M. Dirbas Associate Professor of Surgery, Stanford Univ School of Medicine Physician Leader, Breast Cancer Clinical Care Prgm, Stanford Cancer Institute SABCS 2014 -­‐ ANCO REVIEW SABCS 2014 – Surgery Review ! Diagnostic workup ! Lumpectomy " Local staging, technique, margins ! Mastectomy " Variations in use, prophylactic mastectomy, safety of skin and nipple/areolar sparing ! Axilla " Staging, extent of surgery ! Uncommon tumors " Phyllodes ! New trials " Observation for DCIS, omitting SNB 1 1/16/15 Surgical Mgmt ! Diagnostic workup Workup-­‐Core Bx: Papillary Lesions ! Common finding ! Excision “unpopular” but routinely performed ! Metanalysis 15 studies 2010-­‐2014 ! Recommendation remains surgical excision P2-­‐13-­‐19 2 1/16/15 Workup-­‐Core Bx: Flat Epithelial Atypia ! FEA is a relatively new ! ! ! ! entity Atypia on core biopsy usually approached with surgical excision Does FEA also require excision? Metanalysis,n= 1420 cases, covering 2003-­‐2014 Recommendation is surgical excision P2-­‐13-­‐06 Work-­‐up – Presurgical Imaging FDG-­‐PET/CT for DCIS? ! Can FDG-­‐PET/CT help identify invasive cancer if core biopsy demonstrates DCIS? " FDG-­‐PET/CT is not normally recommended for DCIS alone " 83 patients with core biopsy showing DCIS alone, studied between 2010-­‐2013, Hiroshima University " 29/83 (34.9%) were found to have invasive cancer on excision " On multivariate analysis only high SUVmax predictive ! If SUVmax ≤ 1.6 only 11.4% had invasive cancer " Is FDG-­‐PET/CT reasonable for core biospy showing DCIS? ! This group upstaged 34.9% with excision: normal rate of upstaging is typically 10-­‐15% ! Preop imaging, biopsy technique, pathology review needed ! Digital tomosynthesis, MRI incorporated are used more frequently and could be part of analysis ! False positive findings of FDG-­‐PET/CT and consequences not reviewed P1-­‐02-­‐11 3 1/16/15 Surgical Mgmt ! Lumpectomy Work-­‐up – Presurgical Imaging MRI ! Does MRI Predict Ipsilateral or Contralateral Recurrence? “Enterprise Data Warehouse”, Northwestern University, queried for DCIS or invasive breast cancer, 2004-­‐2010 " 1097 pts: 526 w/ MRI and 571 no MRI " ! Event defined as diagnosis > 6mos after intervention ! Adjusted for age, T, N, triple negative, RT, systemic tx ! 49 events in MRI group, 68 in no MRI group " Authors did not find statistically significant difference in reduced hazard rate for ipsilateral events (HR 0.93, 95% CI .59-­‐1.36) or contralateral events (HR 1.22, 95% CI .57-­‐2.62) ! “However, the MRI group had a more adverse tumor and patient profiles…” ! MRI associated with younger age, premenopausal, palpable, ILC, less commonly DCIS, more nodal involvement, more triple negative " Assessment: ! Customary limitations of retrospective reviews (eg reason for MRI not provided, eg dense mammogram, BRCA status, use of neoadjuvant therapy) ! Absolute risk of recurrence 9.3% in MRI group and 11.9% in no MRI group ! Is 10% recurrence risk typical for median f/u < 10 years? P1-­‐01-­‐05 4 1/16/15 Work-­‐up – Presurgical Imaging MRI ! “A Critical Look… at Preoperative Use of MRI..” " " Notes “routine” use for all breast cancer at Ottowa Hospital, Ontario,Canada Retrospective review, 2010-­‐2012, newly dx breast cancer, n=1159 ! 540 pts (47%) underwent additional imaging ! 415 pts (35%) underwent additional biopsy (481 if counted over 2 years) ! 93% breast (446) " 46% true positive " " ! " " 162 invasive cancer 50 DCIS 7% axilla (35) 38% true positive for regional metastasis New guidelines established ! Neoadjuvant therapy for locally advanced or inflammatory breast cancer ! Unknown primary ! Extent of disease potentially unclear (dense mammogram, lobular, extent unclear) " Post-­‐guidelines ! 52% MRI, 48% no MRI: 83% ordered by radiologist, 17% by surgeon ! Indication ! ! ! ! " 70% assess extent 24% no obvious indication 5% locally advanced .3% unknown primary With 24% w/o obvious reason, ordering of MRI now done by surgeon rather than radiologist P1-­‐01-­‐11 Assessment of Preop MRI ! Alliance Clinical Trials Group A011104 " " " " Stage I/II ER/PR/Her2 negative, Her2 positive Randomized to MRI/no MRI Primary Endpoint: Re-­‐operation rate Secondary endpoints: ! Rate of multifocal disease ! Conversion to mastectomy ! Time to contralat breast cancer ! DFS/CSS/OS " Enrollment 536 5 1/16/15 Lumpectomy -­‐ Technique ! Intraoperative ultrasound (1) " Bulent Ecevit University, Turkey ! Compared intraop US for palp/non-­‐palp tumors ! Single surgeon, 208 pts, 2011-­‐2=2014, frozen section of 6 margins, cavity shaved margins ! 70.6% of pts with + shaved margins had DCIS ! Reoperation needed in 2.4% P1-­‐16-­‐04 Lumpectomy -­‐ Technique ! Intraoperative ultrasound (2) " Regional Breast Care, Fort Myers, Florida ! Intraop US plus guidewire placement ! Retrospective, planned on 118 patients, Jan 2013 to Aug 2014, seen by US on 110 (93%): lesion or hematoma bracketed in 93 pts, clip bracketed in 17 patient. ! 2 pts had + margins (tumor on ink) (1 ILC, 1 DCIS) " Limitations of both US studies ! Detailed comments on pt selection, eg T, calc’s, volume, cosmesis would be useful P2-­‐13-­‐16 6 1/16/15 Lumpectomy -­‐ Margins ! Residual Disease to Excise or not to Excise? " Mt. Sinai, NY ! 1998-­‐2013, 828 pts: close = < 2 mm, = tumor @ ink ! 230 pts (28%) residual disease, 103 (12.4%) re-­‐ excision P1-­‐16-­‐03 Lumpectomy – Margins ILC ! Margin width needed for ILC " Dana Farber/Brigham, retrospective, 1997-­‐2007, 803 pts (335 pure ILC/468 mixed ILC) ! BCS 398 pts (49%), mastectomy 403 pts 51% ! 101 pts (25%) re-­‐excision, + in 33 (33%) ! Predictive fx for + marg: yr of surg, T, MF/Not: ILC ! Preop MRI in 22%: no impact on margin +/-­‐ (p=.59) P1-­‐16-­‐01 7 1/16/15 SSO/ASCO Margin Guidelines ! Meta-­‐analysis 33 studies, 28, 162 patients ! Invasive breast cancer ! Positive margins associated with 2-­‐fold risk increase in IBTR ! Risk not associated with biology, endocrine therapy, boost. ! Wider margins not beneficial Moran MS1, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-­‐American Society for Radiation Oncology consensus guideline on margins for breast-­‐conserving surgery with whole-­‐breast irradiation in stages I and II invasive breast cancer. ; Society of Surgical Oncology; American Society for Radiation Oncology. J Clin Oncol. 2014 May 10;32(14):1507-­‐15. doi: 10.1200/JCO.2013.53.3935. Epub 2014 Feb 10. Lumpectomy – Impact of Subtype ! Should subtype impact choice of BCS? No " Yonsei Univ College of Medicine, Seoul, Korea, 2000-­‐2010, 3608 pts with T1/T2 breast cancer ! Focus on TNBC, neoadjuvant and DM omitted ! Multivariate analysis: histology, receptors, N, systemic therapy, hormonal therapy. p=NS ! TNBC is acceptable for BCT. N = .03 for OS, not IBTR P2-­‐15-­‐09 8 1/16/15 Lumpectomy – IORT ! Short Term Toxicity of IORT " 396 patients, tx 2006-­‐2012, median age 70, median clinical tumor size 1.2 cm, Intrabeam©, 20 Gy, Haifa, Israel ! Infection 10% (50% prophylactic abx) ! Wound dehiscence 8% " Authors’ conclusions ! Infection can be confused with radiation dermatitis ! Seromas (10%) common source of secondary complic. ! DM (dehis) and anti-­‐coagulant use (bleeding) are risk fx P1-­‐15-­‐13 Surgical Mgmt ! Mastectomy 9 1/16/15 BCT vs M – Variations in Care ! Analysis of NCCN database " 24,931 cases, of which 10,868 were T1N0M0. ! 7,888 (77%) chose BCT ! 2,361 (23%) chose mastectomy " Among 8 institutions, M rate varied from 14 – 30% ! Time from dx to surgery longer for M ( 4 vs 6 weeks) ! Time from surgery to chemotherapy similar (11 wks) P2-­‐13-­‐03 Contralateral Prophylactic Mastectomy ! Jatoi: Clinical Implications of Prophylactic Mastectomy ! Partridge: Contralateral Prophylactic Mastectomy ! Pusic: Prophylactic Mastectomy and Reconstruction Clinical Science Forum 10 1/16/15 Contralateral Prophylactic Mastectomy ! Jatoi " Does not believe in CPM. " Rates of mastectomy decreasing: rate of concurrent CPM increasing. " No definitive improvement in survival; decreasing rates of contralateral BC (was .5%/yr now .2%/yr " rate of CPM related to breast reconstruction ! Partridge: " “I don’t think I have the right answer.” ! Pusic " Impact of availability of plastic surgery " Long term cosmetic results of reconstruction Clinical Science Forum Kurian AW, Lichtensztajn DY, Keegan TH et al. Use of and mortality after bilateral mastectomy compared with other surgical treatments for breast cancer in California, 1998-­‐2011. 2014 Sep 3;312(9):902-­‐14. Contralateral Prophylactic Mastectomy ! Pusic Clinical Science Forum 11 1/16/15 Contralateral Prophylactic Mastectomy ! Pusic Clinical Science Forum Contralateral Prophylactic Mastectomy ! Pusic Clinical Science Forum 12 1/16/15 Prophylactic M – Decision Making ! 55 item survey administered to 136 women before surgery Univ of Chicago/Northshore Univ HealthSystem Women asked what influenced decision making regarding keeping their healthy breast " 58.6% BCS, 32%M, 9.4% CPM " " ! Sources of influence ! ! ! ! ! ! ! ! " 44% used sources rec by MD 41.7% sought info aside from MD 6.7% relied heavily on social media 62.6% stated given no information re CPM by medical team 36% stated no information regarding contralateral risk 59% stated no discussion regarding MD if pt had bilat M Source of influence: 81% surgeon; 59.1% med onc; 29.8% recon Outside of medicine 58.7% influence by survivors Summary ! One third of women stated websites identified on their own strongly influenced decision making regarding CPM P2-­‐12-­‐06 Nipple Sparing Mastectomy in BRCA 1 and 2 Mutation Carriers ! Retrospective review, MSKCC, 2005-­‐2013 ! 177 nipple sparing mastectomies (88 bilateral) documented BRCA mutation and/or variant of uncertain significance in 89 patients ! Of 88, 26 had therapeutic NSM (T 1.46 cm, N0) ! 5 patients required N/A excision due to close margins, necrosis, or discharge " At median f/u 2.3 year, no local recurrences ! 1 patient developed DM ! 1 patient developed metastatic ovarian cancer ! Of 88, 63 had proph NSM, no newly dx breast cancer P2-­‐13-­‐02 No. of Breasts; n (%) No. of Patients; n (%) Skin desquamation 68 (38.4) 40 (44.9) Necrosis requiring debridement 18 (10.2) 13 (14.6) Infection 7 (4.0) 7 (7.9) Hematoma 3 (1.69) 3 (3.4) Complication requiring implant or tissue expander removal 6 (3.4) 6 (6.7) 13 1/16/15 Safety of Skin Sparing and Nipple Sparing Mastectomy ! Retrospective review, Yeungnam University, Daegu, Korea, 1996-­‐2008, median f/u 94.9 months ! 272 patients with primary breast cancer " 94 pts SSM/178 pts NASSM ! Findings " " " " 81 NAC margins (29.8%) had tumor, often DCIS SSM: 8 (8.5%) IBTR NASSM: 25 (14%) IBTR – 7 skin, 18 NAC No difference in OS P2-­‐13-­‐23 Breast Cancer After Prophylactic Mastectomy ! Mayo Clinic experience with breast cancer recurrence, 1960 to 1993, included SC mastectomy or bilat SM, 1065 patients w/ total 1,6423 women ! Median f/ul 22 years, 25 patients w/ path confirmed breast cancer ! 5 year DF survival when treated with curative intent 69% P5-­‐12-­‐05 14 1/16/15 Breast Cancer After Prophylactic Mastectomy P5-­‐12-­‐05 Prediction of Local Recurrence After Mastectomy ! Retrospective analysis, T1-­‐T3 tumors, 2000-­‐2005, focus on local, regional, DM. Mean f/u 6.6 years ! 198 screen detected, 379 symptomatic ! 577 women, 462 simple mastectomies, 115 SSM " Recurrence rates 5.6% and 6.9%, respectively at 5 years " Recurrence rates 5.7% and 9.0% respectively at 8 years " Predictors were N+ (HR 7.97) and + margins (HR 3.28) P2-­‐14-­‐06 15 1/16/15 Surgical Mgmt ! Axilla Do We Overtreat Patients with Preop Dx of Axillary Node Mets? ! Univ Hosp Leicester, Glenfield Hospital, UK " 2007-­‐2013, 441 pts with + FNA of axilla and 324 pts with + SNB bx. 161/324 had cALND " 410 of 441 had cALND " 147 of 410 had NEO (36%), 34 (23%) had pCR " 101 of 263 (38%) w/o NEO had 1 or 2 nodes involved " Few pts have ≥ 3 involved nodes, cALND value ? P2-­‐01-­‐21 16 1/16/15 Can US Identify Patients Who May Omit Axillary Dissection? ! Aichi Cancer Center Hospital, Aichi, Japan " 2008-­‐2011 390 pts with + ALN by retrospec chart review classified into 4 groups based on US of axilla ! ! ! ! Group A (41) – suspicious nodes w/ + FNA Group B (47) – only 1 suspicious node +/-­‐ FNA Group C (53) – mult suspicious nodes +/-­‐ FNA Group D ((249) – negative nodes by US but SNB positive ! Pts dx preop with mult susp N should have ALND P2-­‐01-­‐18 Can MRI Identify Extent of Axillary Node Involvement? Pathologic Node Positive All Cases (n=763) Sensitivity (95% CI) 234 (31%) Specificity (95% CI) 52.6 (46-59.1) Approximate biologic subtype missing (= 24) ER+/HER2(n=609) 194 (32%) 51.0 (43.8-58.2) HER2+ (n=69) 20 (29%) 65.0 (40.9-83.7) ER-/HER2(n=61) 17 (28%) 58.8 (33.5-80.6) p value 0.74 0.43 58 (22%) 32.8 (21.4-46.5) 2 (n=351) 124 (35%) 55.6 (46.5-64.5) 3 (n=148) 51 (34%) 66.7 (52.0-79.0) p value 0.001 pts identified retrospectively with + nodes, MRI in 763 pts, most T1-­‐T2. " MRI identified suspicious nodes Tumor Grade (missing=5) 1 (n=259) ! Mayo Clinic, 2010-­‐2013, 1510 0.0003 in 240 (31%), of which 123 (51%) positive ! Sensitivity 48% for 1 abnormal node, 54% for > 1 abnormal node. Multiple suspicious nodes correlated with ≥ 3 involved nodes ! Tumor grade influenced sensitivity and PPV of MRI P1-­‐01-­‐03 17 1/16/15 Methods Impacting FN Rate of SNB after NEO in Z1071 ! ACOSOG Z1071 " 756 women, 136 institutions, 687 had SNB and ALND. Primary analysis 525 pts with cN1 with ≥ 2 SN removed ! ! ! ! Clip placement at node biopsy in 170 In 107 cases with clip found in SN, FN rate was 6.8% In 34 cases with clip found in ALND, FN rate was 19% Nodal involvement if micromet (< .2 mm) ! Recommend clip placement and removal after NEO ! Rec use of IHC after NEO P2-­‐01-­‐02 Methods of Assessing RT alone after Neoadjuvant Therapy in Node + patients ! Alliance A011202: ! Comparison of Axillary Lymph Node Dissection with Axillary Radiation ! ! ! ! for Patients with Node-­‐Positive Breast Cancer Treated with Chemotherapy Stage II, IIIA Proven involved node prior to NEO, then cCR in axilla patients randomized to SN bx + RT or RT alone. Primary endpoint is invasive breast cancer recurrence-­‐free interval Secondary endoints OS, invasive breast cancer recurrence, lymphedema P2-­‐01-­‐02 18 1/16/15 Breast Surgery in Stage IV Dz ! GEICAM Alamo I-­‐III breast cancer registry " 1990-­‐2001, 1331 patients ! 51.8% single organ mets ! Skin/soft tissue 16.2%, bone 33.7%, visceral 48.4% " Pts in S group younger, oligometast vs single site (61.9% svs 43.9%), different sites 40.2% vs 54.3% visceral P2-­‐13-­‐17 Breast Surgery in Stage IV Dz ! SEER Database Analysis " 1988-­‐2011, 41,601 patients ! Trend towards less surgery ! Pts in S group younger, oligometast vs single site (61.9% svs 43.9%), different sites 40.2% vs 54.3% visceral ! No data regarding site of met P2-­‐13-­‐26 19 1/16/15 Breast Surgery in Stage IV Dz ! SABCS 2013 " Soran et al, no benefit to resection of the primary tumor " Trend to improved survival, esp solitary bone metastasis, but overall p=NS ! ECOG 2108 " Ongoing " Randomization to surgical treatment of the primary tumor P2-­‐13-­‐26 or not in patients with stage IV breast cancer at presentation Surgical Mgmt ! Special tumors ! New studies 20 1/16/15 Phyllodes Tumors ! UT MD Anderson " 1964-­‐2011, 229 patients, median f/u 76 months " RT improved local control for BCS and M, no benefit to DM or CSS. Consider systemic tx. P2-­‐13-­‐26 Studies In Process ! LORD trial: A randomized, non-­‐inferiority trial, between active surveillance versus standard treatment in patients with low risk ductal carcinoma in situ (EORTC) OT3-­‐6-­‐01 21 1/16/15 Studies In Process ! Prospective, randomized trial of SNB vs no additional staging with T1-­‐T2 N0 M0 IDC and negative axillary US (Wash. Univ, St. Louis) OT3-­‐6-­‐01 22