(+)-N-3-Benzyl-Nirvanol and
advertisement

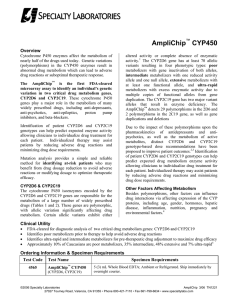
0090-9556/02/3003-235–239$3.00 DRUG METABOLISM AND DISPOSITION Copyright © 2002 by The American Society for Pharmacology and Experimental Therapeutics DMD 30:235–239, 2002 Vol. 30, No. 3 578/964303 Printed in U.S.A. (ⴙ)-N-3-BENZYL-NIRVANOL AND (ⴚ)-N-3-BENZYL-PHENOBARBITAL: NEW POTENT AND SELECTIVE IN VITRO INHIBITORS OF CYP2C19 HISASHI SUZUKI, M. BYRON KNELLER, ROBERT L. HAINING,1 WILLIAM F. TRAGER, AND ALLAN E. RETTIE Department of Medicinal Chemistry, School of Pharmacy, University of Washington, Seattle, Washington (Received September 13, 2001; accepted November 28, 2001) This article is available online at http://dmd.aspetjournals.org ABSTRACT: mal CYP2C19, with Ki values ranging from 71 to 94 nM and 210 to 280 nM, respectively. At single substrate concentrations of 0.3 M [(ⴚ)-N-3-benzyl-phenobarbital] and 1 M [(ⴙ)-N-3-benzyl-nirvanol] that were used to examine inhibition of a panel of cDNA-expressed P450 isoforms, neither CYP1A2, 2A6, 2C8, 2C9, 2D6, 2E1, nor 3A4 activities were decreased by greater than 16%. In contrast, CYP2C19 activity was inhibited ⬃80% under these conditions. Therefore, (ⴙ)-N-3-benzyl-nirvanol and (ⴚ)-N-3-benzyl-phenobarbital represent new, highly potent and selective inhibitors of CYP2C19 that are likely to prove generally useful for screening purposes during early phases of drug metabolism studies with new chemical entities. The cytochrome P450 (P4502) proteins represent a superfamily of oxidative enzymes responsible for the metabolism of a structurally diverse range of drugs (Nelson et al., 1996). Many adverse drug-drug interactions of clinical interest are attributable to pharmacokinetic changes that can be understood in terms of alterations of the drug’s metabolic clearance by these enzymes (Bertz and Granneman, 1997; Lin and Lu, 1998). In particular, inhibition of cytochrome P450mediated metabolism is a well understood mechanism, and potential clinical problems can often be predicted from knowledge of the substrate and inhibitor specificity of the major human liver P450s (Thummel et al., 2000). Therefore, high-throughput screening approaches for identification of P450 isoforms relating to drug metabolism and for assessment of P450 inhibition are performed in early drug development (White, 2000). These efforts can often lead to drug candidates that have a lower potential for drug-drug interactions. The identification of human P450 isoforms involved in a given reaction is routinely assessed by performing in vitro studies using human liver microsomes or cDNA-expressed enzymes. Such microsomal studies generally rely on the availability of potent, selective “diagnostic” inhibitors of the individual P450 isoforms, which are available for most P450s with the notable exception of CYP2C19 (Pelkonen et al., 1998). Therefore, when it is necessary to evaluate the participation of CYP2C19 in human liver microsomal metabolism, the prototypic substrate (S)-mephenytoin is generally used at high concentrations (⬎100 M) because its affinity for the enzyme is low. CYP2C19 is one of the polymorphically regulated P450 isoforms, absent in about 5% of the Caucasian population and up to 20% of the Asian population (Wrighton and Stevens, 1992). As reviewed recently by Wedlund (2000), consideration of data from in vivo studies with CYP2C19-null subjects shows that CYP2C19 is the major isoform (⬎80% involvement) responsible for the oxidation of only a small number of drugs, such as the (S)-enantiomer of mephenytoin, the proton pump inhibitors omeprazole, lansoprazole, and pantoprazole, and carisoprodol. More commonly, CYP2C19 is a secondary contributor to metabolic clearance of drugs, such as phenytoin, diazepam, clomipramine, and citalopram (Bajpai et al., 1996; Jung et al., 1997; Wu et al., 1998; von Moltke et al., 2001). In these latter instances in particular, the availability of a potent and selective inhibitor for CYP2C19 would be expected to be a highly beneficial aid to rapidly assess the extent of the contribution of this isoform to the metabolic clearance of an investigational agent in vitro. Recently, we synthesized new hydantoin and barbiturate inhibitors of the human CYP2C enzymes for use in the development of comparative molecular field analysis models for these enzymes (Suzuki et al., 2000). This article describes characteristics of two of the most This work was supported in part by National Institutes of Health Grant GM 32165. Portions of this research were presented previously at the 10th North American Meeting of the International Society for the Study of Xenobiotics in Indianapolis, IN, October 24–28, 2000. 1 Present address: Department of Basic Pharmaceutical Sciences, West Virginia University, Box 9530, Morgantown, WV 26505. 2 Abbreviations used are: P450, cytochrome P450; MFL, 3-O-methylfluorescein; CEC, 3-cyano-7-ethoxycoumarin; DBF, dibenzylfluorescein; MAMC, 7-methoxy-4-(aminomethyl)coumarin; MFC, 7-methoxy-4-(trifluoromethyl)coumarin; HPLC, high-performance liquid chromatography; TLC, thin-layer chromatography; DMSO, dimethyl sulfoxide. Address correspondence to: Dr. Allan E. Rettie, Department of Medicinal Chemistry, Box 357610, School of Pharmacy, University of Washington, Seattle, WA 98195-7610. E-mail: rettie@u.washington.edu 235 Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2016 Highly potent and selective CYP2C19 inhibitors are not currently available. In the present study, N-3-benzyl derivatives of nirvanol and phenobarbital were synthesized, their respective (ⴙ)- and (ⴚ)enantiomers resolved chromatographically, and inhibitor potencies determined for these compounds toward CYP2C19 and other human liver cytochromes P450 (P450s). (ⴚ)-N-3-Benzyl-phenobarbital and (ⴙ)-N-3-benzyl-nirvanol were found to be highly potent, competitive inhibitors of recombinant CYP2C19, exhibiting Ki values of 79 and 250 nM, respectively, whereas their antipodes were 20- to 60-fold less potent. In human liver preparations, (ⴚ)-N-3benzyl-phenobarbital and (ⴙ)-N-3-benzyl-nirvanol inhibited (S)mephenytoin 4ⴕ-hydroxylase activity, a marker for native microso- 236 SUZUKI ET AL. FIG. 1. Chemical structures of N-3-benzyl-nirvanol and N-3-benzylphenobarbital. potent and selective CYP2C19 inhibitors, (⫹)-N-3-benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital, that emerged from these efforts. The structures of N-3-benzyl-nirvanol and N-3-benzyl-phenobarbital are shown in Fig. 1. Materials and Methods Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2016 Chemicals. MFL, fluorescein, 2,7-dichlorofluorescein, coumarin, 7-hydroxy-4-methylcoumarin, and 4-hydroxymephenytoin were purchased from Sigma Chemical Co. (St. Louis, MO). CEC and 3-cyano-7-hydroxycoumarin were obtained from Molecular Probes, Inc. (Eugene, OR). 7-Hydroxycoumarin and 7-hydroxy-4-(trifluoromethyl)coumarin were from Aldrich (Milwaukee, WI). DBF, MAMC, 7-hydroxy-4-(aminomethyl)coumarin, and MFC were purchased from GENTEST (Woburn, MA). Nirvanol and (S)-mephenytoin were synthesized as reported previously (Wienkers et al., 1996). Phenobarbital sodium was obtained from Spectrum Chemical Mfg. Corp. (Gardena, CA). Racemic N-3-benzyl-nirvanol and N-3-benzyl-phenobarbital were synthesized and then resolved into their (⫹)- and (⫺)-enantiomers by HPLC according to methods that follow. (S)-Flurbiprofen, 4⬘-hydroxyflurbiprofen, and 2-fluoro4-biphenylacetic acid were gifts from Dr. Tim Tracy (West Virginia University, Morgantown, WV). All other chemicals and reagents were of the highest quality commercially available. Synthesis of Racemic N-3-Benzyl-Nirvanol and N-3-Benzyl-Phenobarbital. N-3-Benzyl-nirvanol. Nirvanol (0.5 g, 2.45 mmol) was dissolved in 15 ml of N,N-dimethylformamide. Potassium carbonate (4.4 Eq) and benzyl bromide (1.1 Eq) were added, and the reaction was stirred at room temperature until TLC indicated that the starting material had been consumed. TLC plates were POLYGRAM SIL G/UV254 from Macherey-Nagel (Düren, Germany), developed with hexane/ethyl acetate (1:1, v/v). The reaction mixture was then added to 3 volumes of water and extracted with ethyl acetate. The ethyl acetate extracts were washed with 5% NaOH, water, and brine and then dried over MgSO4. The solvent was removed under reduced pressure. The product, N-3-benzyl-nirvanol, was recrystallized from hexane, and its identity confirmed by 1H NMR. Yield: 0.650 g, 90%. TLC: Rf 0.46. 1H NMR (DMSO-d6): ␦ 0.7 (t, 3H, -CH2-CH3), 2.0 (m, 2H, -CH2-CH3), 4.5 (s, 2H, -CH2-Ph), 7.3 (m, 9H, Ph), 9.1 (s, 1H, NH). N-3-Benzyl-phenobarbital. Phenobarbital sodium (0.5 g, 1.96 mmol) was dissolved in 15 ml of N,N-dimethylformamide. Benzyl bromide (1.1 Eq) was then added, and the solution was stirred and heated to 70°C. When TLC indicated that the starting material had all been consumed, the reaction mixture was added to 50 ml of water, and the solution was extracted three times with ethyl acetate. The combined extracts were washed with 5% NaOH, water, and brine and then dried over MgSO4. The N-3-benzyl-phenobarbital was purified from the N,N-1,3-dibenzyl derivative by silica gel chromatography with hexane/ethyl acetate (9:1, v/v), and both products were characterized by 1H NMR. The early eluting fraction was identified as N,N-1,3-dibenzyl-phenobarbital. Yield: 0.235 g, 37%. TLC: Rf 0.67. 1H NMR (DMSO-d6): ␦ 0.9 (t, 3H, -CH2-CH3), 2.5 (m, 2H, CH2-CH3), 5.1 (m, 4H, -CH2-Ph), 7.3 (m, 15H, Ph). The later eluting fraction was identified as N-3-benzyl-phenobarbital (0.105 g, 17%). TLC: Rf 0.58. 1H NMR (DMSO-d6): ␦ 0.9 (t, 3H, -CH2-CH3), 2.5 (m, 2H, -CH2-CH3), 5.1 (m, 2H, -CH2-Ph), 7.3 (m, 10H, Ph), 8.2 (s, 1H, NH). Separation and Optical Rotation of Enantiomers. The enantiomers of N-3-benzyl-nirvanol were separated by HPLC using an (R,R) Whelk-O1 column (10.0-mm i.d. ⫻ 250 mm; Regis Technologies, Inc., Morton Grove, IL) with 3% isopropanol in hexane at a flow rate of 5 ml/min with UV detection at 254 nm. (⫹)-N-3-Benzyl-nirvanol and (⫺)-N-3-benzyl-nirvanol were eluted at 6.1 and 11.8 min, respectively. The enantiomers of N-3-benzylphenobarbital were separated using a CHIRALCEL OJ column (4.6-mm i.d. ⫻ 250 mm; Daicel Chemical Industries, Ltd., Tokyo, Japan) with 10% acetonitrile in ethanol at a flow rate of 1 ml/min. (⫹)-N-3-Benzyl-phenobarbital and (⫺)-N-3-benzyl-phenobarbital were eluted at 5.0 and 12.0 min, respectively. Individual peak fractions were collected, and the organic solvent was evaporated to dryness under reduced pressure. The purity of the resulting enantiomers was greater than 95% enantiomeric excess. Optical rotations were obtained using a Jasco P-1030 polarimeter (Jasco Co, Tokyo, Japan): (⫹)-N3-benzyl-nirvanol [␣]D20, ⫹52.0° (methanol; concentration, 10 mg/ml); (⫺)N-3-benzyl-nirvanol [␣]D20, ⫺45.2° (methanol; concentration, 10 mg/ml); (⫹)-N-3-benzyl-phenobarbital [␣]D20, ⫹43.9° (methanol; concentration, 10 mg/ml); (⫺)-N-3-benzyl-phenobarbital [␣]D20, ⫺43.3° (methanol; concentration, 10 mg/ml). Enzyme Sources. CYP2C19 cDNA (Romkes et al., 1991) was obtained from Dr. J. A. Goldstein (NIEHS, Bethesda, MD) in the vector pBlueScript SK⫹/⫺. This cDNA was inserted into the pBacPAK8 transfer vector on an XhoI/XbaI fragment behind the polyhedrin promoter to create pBP2C19. Cotransfection of insect cells with Bsu36I-digested BacPAK6 viral DNA, and the pBP2C19 was carried out with reagents and procedures provided by CLONTECH Laboratories, Inc. (Palo Alto, CA) to generate recombinant viral particles for expression. Suspension cultures of Trichoplusia ni insect cells were infected with recombinant viruses for CYP2C19 and CYP2C9, and the two hemoproteins were purified to near homogeneity by procedures detailed previously (Haining et al., 1996). For some experiments, Supersomes (GENTEST) were used. Recombinant rat NADPH-P450 oxidoreductase and human cytochrome b5 were expressed and purified from bacterial cultures in a manner described previously by Chen et al. (1998). Human liver tissue was obtained from the Human Liver Bank established in the Departments of Medicinal Chemistry and Pharmaceutics at the University of Washington. Details concerning the acquisition, storage, and preparation of the human liver microsomes used in these experiments have been described (Rettie et al., 1989). Assay for MFL Demethylation. The activity of reconstituted recombinant CYP2C19 was determined by measuring MFL demethylation activities. The incubation mixtures were in a final volume of 200 l and contained 2.5 pmol of purified CYP2C19, 5 pmol of P450 reductase, 2.5 pmol of cytochrome b5, 5 g of L-␣-dilauroyl-sn-glycero-3-phosphocholine, 1 mM NADPH, 50 mM potassium phosphate buffer, pH 7.4, and MFL (1, 2, and 4 M). The reaction was initiated by the addition of reconstituted enzymes. Incubations were carried out at 37°C for 20 min and terminated by adding 200 l of 40 nM 2,7-dichlorofluorescein in acetonitrile as an internal standard and 10 l of 10% perchloric acid. After centrifugation at 8000g for 2 min, the supernatant was analyzed by HPLC using an XTerra RP18, 5-m column (4.6-mm i.d. ⫻ 150 mm; Waters Co., Milford, MA), attached to a guard column (3.9-mm i.d. ⫻ 20 mm). The column was eluted with a linear gradient of acetonitrile/10 mM potassium phosphate buffer, pH 8.0, that changed from a ratio of 15:85 to 35:65 over 10 min at a flow rate of 1 ml/min. Metabolites were detected fluorometrically with the excitation wavelength set at 490 nm and emission wavelength at 525 nm. Assay for (S)-Mephenytoin 4ⴕ-Hydroxylation by Human Liver Microsomes. Ki values for the inhibition of (S)-mephenytoin 4⬘-hydroxylation were assessed using three individual human liver microsomal preparations (HL134, male, 7 years, Caucasian; HL143, male, 48 years, Caucasian; and HL164, female, 50 years, Caucasian). The incubation mixtures for (S)-mephenytoin 4⬘-hydroxylation were in a final volume of 200 l and contained 50 pmol of human liver microsomal P450, 1 mM NADPH, 50 mM potassium phosphate buffer, pH 7.4, and (S)-mephenytoin (20, 40, and 80 M). The reaction was initiated by the addition of microsomes. Incubations were carried out at 37°C for 30 min and terminated by adding 50 l of 5 M phenobarbital in acetonitrile as an internal standard. The samples were then centrifuged at 8000g for 2 min, and 4⬘-hydroxymephenytoin in the supernatant was analyzed by HPLC using an XTerra RP18, 5-m column (4.6-mm i.d. ⫻ 150 mm) attached to a guard column (3.9-mm i.d. ⫻ 20 mm). The column was eluted with a linear gradient of acetonitrile/10 mM potassium phosphate buffer, pH 3.0, that changed from 25:75 to 30:70 over 10 min, and then isocratically with a 50:50 mix from 10 to 15 min. The flow rate was 1 ml/min with UV detection at 204 nm. 237 SELECTIVE, POTENT CYP2C19 INHIBITORS TABLE 1 Incubation conditions, HPLC assay conditions, and Km values for cDNA-expressed P450 isoform (Supersomes) activities P450 Isoform Substrate Enzyme (pmol P450/inc) Metabolite Internal Standard (200 l of Acetonitrile) CYP1A2 CYP2A6 CYP2C8 CYP2C9 CYP2C19 CYP2D6 CYP2E1 CYP3A4 2.5 M CEC 0.5 M Coumarin 0.5 M DBF 35 M MFL 1.5 M MFL 5.0 M MAMC 100 M MFC 0.5 M DBF 0.5 0.4 2.5 2.5 2.5 2.5 5.0 0.5 CHC HC FL FL FL HAMC HFC FL 0.5 M HMC 0.1 M HMC 40 nM DCFL 40 nM DCFL 40 nM DCFL 0.1 M HC 0.25 M HC 40 nM DCFL Mobile Phase Acetonitrile/10 mM Potassium Phosphate Buffer (pH 8.0) Excitation Emission nm 0–10 min; 20:80–70:30 linear gradient 0–5 min; 20:80–30:70 linear gradient, 5–10 min; 30:70 0–5 min; 15:85–32:68 linear gradient, 5–12 min 70:30 0–10 min; 15:85–35:65 linear gradient 0–10 min; 15:85–35:65 linear gradient 0–10 min; 10:90–30:70 linear gradient 0–10 min; 20:80–70:30 linear gradient 0–5 min; 15:85–32:68 linear gradient, 5–12 min 70:30 408 368 490 490 490 370 385 490 450 456 525 525 525 470 502 525 CHC, 3-cyano-7-hydroxycoumarin; HC, 7-hydroxycoumarin; FL, fluorescein; HAMC, 7-hydroxy-4-(aminomethyl)coumarin; HFC, 7-hydroxy-4-(trifluoromethyl)coumarin; HMC, 7-hydroxy4-methylcoumarin; DCFL, 2,7-dichlorofluorescein. Results Inhibition of CYP2C19 by N-3-Benzyl-Nirvanol, N-3-BenzylPhenobarbital, and Mephenytoin Enantiomers. All six compounds inhibited recombinant CYP2C19 in a competitive manner (data not shown). Ki values for the inhibition of CYP2C19-dependent MFL activity by each of these compounds are shown in Table 2. As expected, (S)-mephenytoin was a much more potent inhibitor than (R)-mephenytoin (8-fold), although the affinity of the (S)-enantiomer for CYP2C19 was not particularly strong (Ki ⫽ 29.5 M). Replacement of the N-3 methyl group of the mephenytoin enantiomers with a benzyl moiety resulted in a dramatic enhancement in affinity for CYP2C19 (45- to 118-fold). Expansion of the five-membered hydantoin nucleus to a six-membered barbiturate ring with retention of the N-3 benzyl moiety resulted in further increases in inhibitor potency such that the Ki value for the most potent inhibitor examined, (⫺)- TABLE 2 Ki values for the inhibition of CYP2C19 by mephenytoin, N-3-benzyl-nirvanol, and N-3-benzyl-phenobarbital enantiomers CYP2C19 activity was measured as MFL demethylation using reconstituted recombinant enzymes, as described under Materials and Methods. K i values were determined by nonlinear regression with SYSTAT Statistics ver 5.0 using the competitive inhibition equation. Data are expressed as means of two or three experiments. Compound Ki Inhibitor Potency Relative to (S)Mephenytoin M (R)-(⫺)-Mephenytoin (S)-(⫹)-Mephenytoin (⫺)-N-3-Benzyl-nirvanol (⫹)-N-3-Benzyl-nirvanol (⫹)-N-3-Benzyl-phenobarbital (⫺)-N-3-Benzyl-phenobarbital 237.0 29.5 5.3 0.25 4.7 0.079 0.12 1.0 5.6 118.0 6.3 373.0 N-3-benzyl-phenobarbital, dropped to 79 nM—an increase in affinity for CYP2C19 of 373-fold relative to (S)-mephenytoin. Inhibition of (S)-Mephenytoin 4ⴕ-Hydroxylation in Human Liver Microsomes by (ⴙ)-N-3-Benzyl-Nirvanol and (ⴚ)-N-3-Benzyl-Phenobarbital. Representative Dixon plots for the inhibition of human liver microsomal (S)-mephenytoin 4⬘-hydroxylation by (⫹)N-3-benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital are shown in Fig. 2. Both (⫹)-N-3-benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital were found to be potent competitive inhibitors of native microsomal CYP2C19 activity, exhibiting mean Ki values obtained from three separate microsomal preparations of 0.24 and 0.085 M, respectively (Table 3). These data are in good agreement with the Ki values obtained from the inhibition of MFL demethylation catalyzed by reconstituted recombinant CYP2C19. Inhibitory Effects of (ⴙ)-N-3-Benzyl-Nirvanol and (ⴚ)-N-3Benzyl-Phenobarbital on the Activities of Heterologously cDNAExpressed Human P450 Isoforms. To probe the P450 isoform selectivity of these two potent CYP2C19 inhibitors, their inhibitory effects on the activities of the major isoforms relevant to human liver drug metabolism were determined using commercially available Supersomes. These screening experiments were performed with single inhibitor concentrations equal to ⬃4 times the respective Ki values for CYP2C19, i.e., 1 M for (⫹)-N-3-benzyl-nirvanol and 0.3 M for (⫺)-N-3-benzyl-phenobarbital. In preliminary experiments, we determined the Km of each metabolic reaction catalyzed by the recombinant P450 and then selected this value for the final substrate concentration to be used in each inhibition experiment (Table 1, column 2). An exception was CYP2E1, in which the substrate concentration was set at 100 M, since determination of an accurate Km value for MFC was precluded by its limited solubility. Nonetheless, it was clear that MFC demethylation catalyzed by CYP2E1 was not saturated at this substrate concentration. Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2016 Ki Determination. Inhibitors were dissolved in methanol such that the final concentration of solvent in the incubation mixture was 1.0% v/v. The rate data were analyzed graphically by Dixon plots to obtain approximate kinetic constants and to determine the nature of the inhibition. Ki values were determined by nonlinear regression with SYSTAT Statistics version 5.0 (SYSTAT, Inc., Evanston, IL) using the competitive inhibition equation. Inhibition Studies by cDNA-Expressed Human P450 Isoforms. Baculovirus-infected insect cell microsomes, which contained heterologously overexpressed CYP1A2, 2A6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4 (Supersomes; GENTEST), were used as the source of enzymes. The activities were determined by measuring CEC deethylation for CYP1A2, coumarin 7-hydroxylation for CYP2A6, DBF debenzylation for CYP2C8 and CYP3A4, MFL demethylation for CYP2C9 and CYP2C19, MAMC demethylation for CYP2D6, and MFC demethylation for CYP2E1, using fluorometric HPLC assays. Details concerning the final substrate concentration, P450 content, detected metabolite, internal standard, mobile phase for HPLC elution, and fluorescence detection used in these experiments are summarized in Table 1. Incubation mixtures contained cDNA-expressed P450 microsomes, 1 mM NADPH, 50 mM potassium phosphate buffer, pH 7.4, the appropriate substrate, and inhibitor in a final volume of 200 l. The final substrate concentrations were chosen to be approximately the apparent Km values determined by preliminary kinetics studies, except for CYP2E1. The final concentrations of the inhibitors (⫹)-N3-benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital were set at 1 and 0.3 M, respectively. Incubations were carried out at 37°C for 20 min and terminated by adding 200 l of acetonitrile containing the appropriate internal standard. Aliquots of these reaction mixtures, except for MAMC demethylation and DBF debenzylation, were then acidified by adding 10 l of 10% perchloric acid. For DBF debenzylation, reaction mixtures were further incubated at 37°C for 2 h, after adding 10 l of 6 M sodium hydroxide to achieve benzyl ester hydrolysis and then acidified by the addition of 10 l of 70% perchloric acid. All samples were centrifuged at 8000g for 2 min, and the supernatant analyzed fluorometrically by HPLC using an XTerra RP18 column with various ratios of acetonitrile/10 mM potassium phosphate buffer, pH 8.0, as indicated in Table 1. 238 SUZUKI ET AL. FIG. 2. Representative Dixon plots for the inhibition of microsomal (S)mephenytoin 4⬘-hydroxylation by (⫹)-N-3-benzyl-nirvanol (A) and (⫺)-N-3benzyl-phenobarbital (B). TABLE 3 Ki values for the inhibition of (S)-mephenytoin 4⬘-hydroxylation by (⫹)-N-3benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital in human liver microsomes The activities of (S)-mephenytoin 4⬘-hydroxylation in three different human liver microsomal preparations were analyzed as described under Materials and Methods. K i values were determined by nonlinear regression with SYSTAT Statistics using the competitive inhibition equation. Ki Enzyme Source (⫹)-N-3-Benzyl-Nirvanol (⫺)-N-3-Benzyl-Phenobarbital M HL134 HL143 HL164 Mean ⫾ S.D. 0.23 0.28 0.21 0.24 ⫾ 0.04 0.071 0.094 0.089 0.085 ⫾ 0.012 Under these conditions, (⫹)-N-3-benzyl-nirvanol inhibited CYP2C19 by 80% with only a modest degree of inhibition (16%) toward the next most susceptible isoform, CYP3A4 (Fig. 3A). (⫺)N-3-Benzyl-phenobarbital also markedly inhibited CYP2C19 activity but without significantly affecting the metabolic activities of the other P450 isoforms tested, including CYP3A4 (Fig. 3B). In separate experiments using reconstituted preparations of CYP2C9 and an (S)flurbiprofen 4⬘-hydroxylase reporter assay, the Ki values of the two most potent CYP2C19 inhibitors, (⫹)-N-3-benzyl-nirvanol and (⫺)N-3-benzyl-phenobarbital against CYP2C9 were determined to be 83 and 16 M, respectively (data not shown), further demonstrating the selectivity of (⫹)-N-3-benzyl-nirvanol and (⫺)-N-3-benzylphenobarbital for inhibition of CYP2C19. Discussion Numerous studies conducted in recent years (Newton et al., 1995; Bourrie et al., 1996; Ono et al., 1996; Zhang et al., 2001) have established the use of a variety of specific, high-potency inhibitors for all of the major (and several minor) human P450 isoforms, with the notable exception of CYP2C19. Omeprazole and tranylcypromine, with Ki values of 4.1 and 8.7 M, respectively (VandenBranden et al., 1996; Wienkers et al., 1996), have occasionally been used as CYP2C19 inhibitors, but both compounds also inhibit CYP3A4 and CYP2A6 with Ki values of 79 and 0.04 M, respectively (Lampen et al., 1995; Draper et al., 1997), and therefore do not demonstrate high selectivity. The most potent inhibitors for CYP2C19 found to date are probably norfluoxetine and ticlopidine with Ki values of 1.1 and 1.2 The effects of 1 M (⫹)-N-3-benzyl-nirvanol and 0.3 M (⫺)-N-3-benzylphenobarbital were determined on CEC deethylation for CYP1A2, coumarin 7-hydroxyation for CYP2A6, DBF debenzylation for CYP2C8 and 3A4, MFL demethylation for CYP2C9 and 2C19, MAMC demethylation for CYP2D6, and MFC demethylation for CYP2E1. Data are expressed as the percentage of the control velocities. Each value is the mean ⫾ standard deviation of three different incubations. M, respectively (Kobayashi et al., 1995; Ko et al., 2000). However, both drugs are also potent inhibitors of CYP2D6 (Stevens and Wrighton, 1993; Ko et al., 2000). Therefore, to our knowledge, no highly potent and isoform-specific inhibitors of CYP2C19 have been described. CYP2C19 and CYP2C9 are the most highly conserved isoforms among the human CYP2C subfamily, exhibiting 91% amino acid identity (Romkes et al., 1991) and yet having distinctive substrate, product, and inhibitor specificities. For example, sulfaphenazole is a nanomolar potency inhibitor of CYP2C9 but is not a marked inhibitor of CYP2C19 (Ono et al., 1996). CYP2C19 and CYP2C9 both metabolize phenytoin to 5-(4-hydroxyphenyl)-5-phenylhydantoin but with different prochiral stereoselectivities. Phenytoin is stereospecifically oxidized on the pro-(S)-phenyl ring by CYP2C9, whereas CYP2C19 exhibits low prochiral selectivity (Bajpai et al., 1996). However, if phenytoin is methylated at the N-3 position on the hydantoin ring, the resulting N-3-methyl-phenytoin is still metabolized by CYP2C19 but apparently is no longer a substrate for CYP2C9 (Schellens et al., 1990). Furthermore, it was demonstrated recently in vitro that (R)mephobarbital, [(⫺)-N-3-methyl-phenobarbital] but not its (S)-antipode, is preferentially metabolized by CYP2C19 (Kobayashi et al., 2001). Since (S)-mephenytoin, which is also N-3-methylated on the hydantoin ring, has long been considered to be the prototypic substrate for CYP2C19, it seems clear that alkylation at the N-3 positions on hydantoin and barbiturate rings is an important structural modification that differentiates CYP2C9 and CYP2C19 substrates. Moreover, the absolute configuration of the substrate would appear also to be an essential determinant of high-affinity binding to CYP2C19. Based on the above considerations, we prepared several enantiomerically pure N-3 substituted nirvanol and phenobarbital derivatives and tested their binding affinities for CYP2C19, as reflected in the magnitude of Ki values toward CYP2C19-dependent catalytic reactions. From these studies, (⫹)-N-3-benzyl-nirvanol and (⫺)-N-3-benzyl-phenobarbital emerged as highly potent and selective inhibitors for native and recombinant CYP2C19. Each compound exhibited a Ki value for CYP2C19 that is more than 2 orders of magnitude lower than that obtained with (S)-mephenytoin. Moreover, the antipodes of these two nanomolar inhibitors were 20- to 60-fold less potent as CYP2C19 inhibitors, and the Ki values for (⫺)-N-3-benzyl-phenobarbital and (⫹)-N-3-benzyl-nirvanol against the closely related enzyme Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2016 Human liver microsomes (HL164) were used as the enzyme source. Incubations were carried out at three different (S)-mephenytoin concentrations of 20 M (closed circles), 40 M (open circles), and 80 M (closed squares), as described under Materials and Methods. V, velocity of 4⬘-hydroxymephenytoin formation. FIG. 3. Inhibitory effects of (⫹)-N-3-benzyl-nirvanol (A) and (⫺)-N-3-benzylphenobarbital (B) on the activities of heterologously cDNA-expressed human P450 isoforms. SELECTIVE, POTENT CYP2C19 INHIBITORS References Bajpai M, Roskos LK, Shen DD, and Levy RH (1996) Role of cytochrome P4502C9 and cytochrome P4502C19 in the stereoselective metabolism of phenytoin to its major metabolite. Drug Metab Dispos 24:1401–1403. Bertz RJ and Granneman GR (1997) Use of in vitro and in vivo data to estimate the likelihood of metabolic pharmacokinetic interactions. Clin Pharmacokinet 32:210 –258. Bourrie M, Meunier V, Berger Y, and Fabre G (1996) Cytochrome P450 isoform inhibitors as a tool for the investigation of metabolic reactions catalyzed by human liver microsomes. J Pharmacol Exp Ther 277:321–332. Chen W, Koenigs LL, Thompson SJ, Peter RM, Rettie AE, Trager WF, and Nelson SD (1998) Oxidation of acetaminophen to its toxic quinone imine and nontoxic catechol metabolites by baculovirus-expressed and purified human cytochromes P450 2E1 and 2A6. Chem Res Toxicol 11:295–301. Draper AJ, Madan A, and Parkinson A (1997) Inhibition of coumarin 7-hydroxylase activity in human liver microsomes. Arch Biochem Biophys 341:47– 61. Haining RL, Hunter AP, Veronese ME, Trager WF, and Rettie AE (1996) Allelic variants of human cytochrome P450 2C9: baculovirus-mediated expression, purification, structural characterization, substrate stereoselectivity, and prochiral selectivity of the wild-type and I359L mutant forms. Arch Biochem Biophys 333:447– 458. Jung F, Richardson TH, Raucy JL, and Johnson EF (1997) Diazepam metabolism by cDNAexpressed human 2C P450s: identification of P4502C18 and P4502C19 as low Km diazepam. N-demethylases. Drug Metab Dispos 25:133–139. Ko JW, Desta Z, Soukhova NV, Tracy T, and Flockhart DA (2000) In vitro inhibition of the cytochrome P450 (CYP450) system by the antiplatelet drug ticlopidine: potent effect on CYP2C19 and CYP2D6. Br J Clin Pharmacol 49:343–351. Kobayashi K, Kogo M, Tani M, Shimada N, Ishizaki T, Numazawa S, Yoshida T, Yamamoto T, Kuroiwa Y, and Chiba K (2001) Role of CYP2C19 in stereoselective hydroxylation of mephobarbital by human liver microsomes. Drug Metab Dispos 29:36 – 40. Kobayashi K, Yamamoto T, Chiba K, Tani M, Ishizaki T, and Kuroiwa Y (1995) The effects of selective serotonin reuptake inhibitors and their metabolisms on S-mephenytoin 4⬘hydroxylase activity in human liver microsomes. Br J Clin Pharmacol 40:481– 485. Lampen A, Christians U, Guengerich FP, Watkins PB, Kolars JC, Bade A, Gonschior AK, Dralle H, Hackbarth I, and Sewing KF (1995) Metabolism of the immunosuppressant tacrolimus in the small intestine: cytochrome P450, drug interactions, and interindividual variability. Drug Metab Dispos 23:1315–1324. Lin JH and Lu AY (1998) Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet 35:361–390. Nelson DR, Koymans L, Kamataki T, Stegeman JJ, Feyereisen R, Waxman DJ, Waterman MR, Gotoh O, Coon MJ, Estabrook RW, et al. (1996) P450 superfamily: update on new sequences, gene mapping, accession numbers and nomenclature. Pharmacogenetics 6:1– 42. Newton DJ, Wang RW, and Lu AYH (1995) Cytochrome P450 inhibitors: evaluation of specificities in the in vitro metabolism of therapeutic agents by human liver microsomes. Drug Metab Dispos 23:154 –158. Ono S, Hatanaka T, Hotta H, Satoh T, Gonzalez FJ, and Tsutsui M (1996) Specificity of substrate and inhibitor probes for cytochrome P450s: evaluation of in vitro metabolism using cDNAexpressed human P450s and human liver microsomes. Xenobiotica 26:681– 693. Pelkonen O, Mäenpää J, Taavitsainen P, Rautio A, and Raunio H (1998) Inhibition and induction of human cytochrome P450 (CYP) enzymes. Xenobiotica 28:1203–1253. Rettie AE, Eddy AC, Heimark LD, Gibaldi M, and Trager WF (1989) Characteristics of warfarin hydroxylation catalyzed by human liver microsomes. Drug Metab Dispos 17:265–270. Romkes M, Faletto MB, Blaisdell JA, Raucy JL, and Goldstein JA (1991) Cloning and expression of complementary DNAs for multiple members of the human cytochrome P450IIC subfamily. Biochemistry 30:3247–3255. Schellens JHM, van der Wart JHF, and Breimer DD (1990) Relationship between mephenytoin oxidation polymorphism and phenytoin, methylphenytoin and phenobarbitone hydroxylation assessed in a phenotyped panel of healthy subjects. Br J Clin Pharmacol 29:665– 671. Stevens JC and Wrighton SA (1993) Interaction of the enantiomers of fluoxetine and norfluoxetine with human liver cytochromes P450. J Pharmacol Exp Ther 266:964 –971. Suzuki H, Kneller MB, Rao S, Jones JP, Trager WF, and Rettie AE (2000) Hydantoin and barbiturate inhibitors of CYP2C19 and CYP2C9. Drug Metab Rev 32 (Suppl 2):218. Thummel KE, Kunze KL, and Shen DD (2000) Metabolically-based drug-drug interactions: principles and mechanisms, in Metabolic Drug Interactions (Levy RH, Thummel KE, Trager WF, Hansten PD, and Eichelbaum M eds) pp 3–19, Lippincot Williams and Wilkins, Philadelphia, PA. VandenBranden M, Ring BJ, Binkley SN, and Wrighton SA (1996) Interaction of human liver cytochromes P450 in vitro with LY307640, a gastric proton pump inhibitor. Pharmacogenetics 6:81–91. von Moltke LL, Greenblatt DJ, Giancarlo GM, Granda BW, Harmatz JS, and Shader RI (2001) Escitalopram (s-citalopram) and its metabolites in vitro: cytochromes mediating biotransformation, inhibitory effects, and comparison to r-citalopram. Drug Metab Dispos 29:1102–1109. Wedlund PJ (2000) The CYP2C19 enzyme polymorphism. Pharmacology 61:174 –183. White RE (2000) High-throughput screening in drug metabolism and pharmacokinetic support of drug discovery. Annu Rev Pharmacol Toxicol 40:133–157. Wienkers LC, Wurden CJ, Storch E, Kunze KL, Rettie AE, and Trager WF (1996) Formation of (R)-8-hydroxywarfarin in human liver microsomes: a new metabolic marker for the (S)mephenytoin hydroxylase, P4502C19. Drug Metab Dispos 24:610 – 614. Wrighton SA and Stevens JC (1992) The human hepatic cytochromes P450 involved in drug metabolism. Crit Rev Toxicol 22:1–21. Wu ZL, Huang SL, Ou-Yang DS, Xu ZH, Xie HG, and Zhou HH (1998) Clomipramine N-demethylation metabolism in human liver microsomes. Zhongguo Yao Li Xue Bao 19:433– 436. Zhang W, Kilicarslan T, Tyndale RF, and Sellers EM (2001) Evaluation of methoxsalen, tranylcypromine and tryptamine as specific and selective CYP2A6 inhibitors in vitro. Drug Metab Dispos 26:897–902. Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2016 CYP2C9 were 200- to 300-fold higher than for CYP2C19. Studies with a panel of recombinant P450s at inhibitor concentrations equivalent to ⬃4 times Ki demonstrated very high inhibitor selectivity toward CYP2C19, particularly with (⫺)-N-3-benzyl-phenobarbital. As noted under Materials and Methods, synthesis of racemic N-3benzyl-nirvanol could be achieved in high yield (90%) compared with racemic N-3-benzyl-phenobarbital (17%). This was due to the preferred formation of the dibenzyl derivative in the latter reaction, which necessitated an additional column chromatography step. Accordingly, (⫹)-N-3-benzyl-nirvanol, albeit a slightly less potent and less selective inhibitor of CYP2C19 than (⫺)-N-3-benzyl-phenobarbital, may be a more attractive synthetic target in many laboratories, particularly since it can also be prepared by direct benzylation of (S)-(⫹)-nirvanol, which is easily obtained by fractional crystallization. In conclusion, we report that (⫹)-N-3-benzyl-nirvanol and (⫺)-N3-benzyl-phenobarbital are potent, selective inhibitors of CYP2C19. Both novel inhibitors should prove useful in the assessment of the contribution of CYP2C19 to drug metabolism in human liver microsomes. Future studies are aimed at incorporating these inhibitors and other congeners into a comparative molecular field analysis model for CYP2C19 and to use them further to delineate active-site features of the enzyme that promote high-affinity binding of N-3-alkylated hydantoins and barbiturates. 239