Phosphate-induced autophagy, Xiao
advertisement
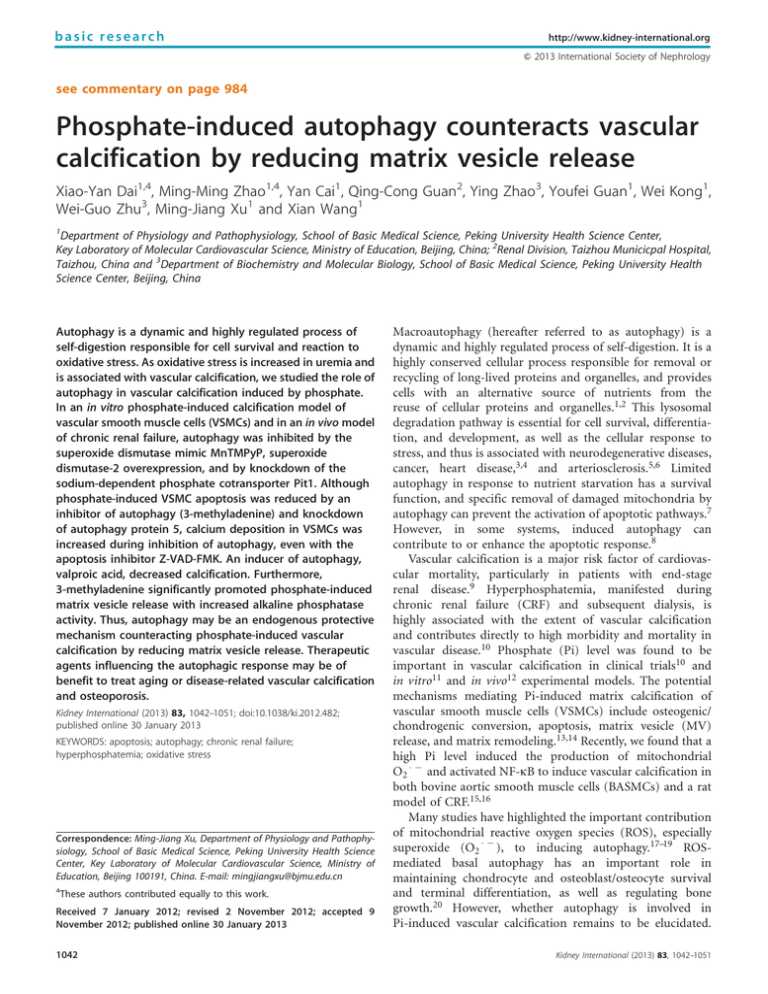
basic research http://www.kidney-international.org & 2013 International Society of Nephrology see commentary on page 984 Phosphate-induced autophagy counteracts vascular calcification by reducing matrix vesicle release Xiao-Yan Dai1,4, Ming-Ming Zhao1,4, Yan Cai1, Qing-Cong Guan2, Ying Zhao3, Youfei Guan1, Wei Kong1, Wei-Guo Zhu3, Ming-Jiang Xu1 and Xian Wang1 1 Department of Physiology and Pathophysiology, School of Basic Medical Science, Peking University Health Science Center, Key Laboratory of Molecular Cardiovascular Science, Ministry of Education, Beijing, China; 2Renal Division, Taizhou Municicpal Hospital, Taizhou, China and 3Department of Biochemistry and Molecular Biology, School of Basic Medical Science, Peking University Health Science Center, Beijing, China Autophagy is a dynamic and highly regulated process of self-digestion responsible for cell survival and reaction to oxidative stress. As oxidative stress is increased in uremia and is associated with vascular calcification, we studied the role of autophagy in vascular calcification induced by phosphate. In an in vitro phosphate-induced calcification model of vascular smooth muscle cells (VSMCs) and in an in vivo model of chronic renal failure, autophagy was inhibited by the superoxide dismutase mimic MnTMPyP, superoxide dismutase-2 overexpression, and by knockdown of the sodium-dependent phosphate cotransporter Pit1. Although phosphate-induced VSMC apoptosis was reduced by an inhibitor of autophagy (3-methyladenine) and knockdown of autophagy protein 5, calcium deposition in VSMCs was increased during inhibition of autophagy, even with the apoptosis inhibitor Z-VAD-FMK. An inducer of autophagy, valproic acid, decreased calcification. Furthermore, 3-methyladenine significantly promoted phosphate-induced matrix vesicle release with increased alkaline phosphatase activity. Thus, autophagy may be an endogenous protective mechanism counteracting phosphate-induced vascular calcification by reducing matrix vesicle release. Therapeutic agents influencing the autophagic response may be of benefit to treat aging or disease-related vascular calcification and osteoporosis. Kidney International (2013) 83, 1042–1051; doi:10.1038/ki.2012.482; published online 30 January 2013 KEYWORDS: apoptosis; autophagy; chronic renal failure; hyperphosphatemia; oxidative stress Correspondence: Ming-Jiang Xu, Department of Physiology and Pathophysiology, School of Basic Medical Science, Peking University Health Science Center, Key Laboratory of Molecular Cardiovascular Science, Ministry of Education, Beijing 100191, China. E-mail: mingjiangxu@bjmu.edu.cn 4 These authors contributed equally to this work. Received 7 January 2012; revised 2 November 2012; accepted 9 November 2012; published online 30 January 2013 1042 Macroautophagy (hereafter referred to as autophagy) is a dynamic and highly regulated process of self-digestion. It is a highly conserved cellular process responsible for removal or recycling of long-lived proteins and organelles, and provides cells with an alternative source of nutrients from the reuse of cellular proteins and organelles.1,2 This lysosomal degradation pathway is essential for cell survival, differentiation, and development, as well as the cellular response to stress, and thus is associated with neurodegenerative diseases, cancer, heart disease,3,4 and arteriosclerosis.5,6 Limited autophagy in response to nutrient starvation has a survival function, and specific removal of damaged mitochondria by autophagy can prevent the activation of apoptotic pathways.7 However, in some systems, induced autophagy can contribute to or enhance the apoptotic response.8 Vascular calcification is a major risk factor of cardiovascular mortality, particularly in patients with end-stage renal disease.9 Hyperphosphatemia, manifested during chronic renal failure (CRF) and subsequent dialysis, is highly associated with the extent of vascular calcification and contributes directly to high morbidity and mortality in vascular disease.10 Phosphate (Pi) level was found to be important in vascular calcification in clinical trials10 and in vitro11 and in vivo12 experimental models. The potential mechanisms mediating Pi-induced matrix calcification of vascular smooth muscle cells (VSMCs) include osteogenic/ chondrogenic conversion, apoptosis, matrix vesicle (MV) release, and matrix remodeling.13,14 Recently, we found that a high Pi level induced the production of mitochondrial O2 and activated NF-kB to induce vascular calcification in both bovine aortic smooth muscle cells (BASMCs) and a rat model of CRF.15,16 Many studies have highlighted the important contribution of mitochondrial reactive oxygen species (ROS), especially superoxide (O2 ), to inducing autophagy.17–19 ROSmediated basal autophagy has an important role in maintaining chondrocyte and osteoblast/osteocyte survival and terminal differentiation, as well as regulating bone growth.20 However, whether autophagy is involved in Pi-induced vascular calcification remains to be elucidated. Kidney International (2013) 83, 1042–1051 X-Y Dai et al.: Autophagy counteracts vascular calcification Here, we examined the induction of autophagy by Piincreased ROS levels, and the role of autophagy in Pi-induced calcification in VSMCs and a rat model of CRF. RESULTS High Pi promotes autophagy in VSMCs To determine whether autophagy is involved in Pi-induced vascular calcification, we first examined the effect of Pi on autophagosome formation in VSMCs. Pi dose dependently (1.5–3 mmol/l) increased the level of the lipid-conjugated form of the autophagosome marker light-chain 3-II (LC3II) in BASMCs (Figure 1a). With lysosome-dependent degradation of LC3II blocked by chlorquinol (25 mmol/l), Pi further increased the LC3II level (Figure 1b). Increased accumulation of LC3 puncta tagged with green fluorescent protein (GFP) indicated Pi induction of autophagosomes (Figure 1c), and the proportion of cells with GFP–LC3 puncta was sustained from 0.5 to 7 days with Pi treatment (Figure 1d). Electron microscopy of typical autophagic structures in BASMCs gave direct evidence of the autophagy activation, and increased autophagic structures were observed in cells exposed to Pi for 12 h (Figure 1e). Increased autophagy was observed in parallel in human aortic VSMCs (HA-VSMCs; Figure 1f and Supplementary Figure S1 online). In addition, immunofluorescence analysis of LC3 puncta revealed autophagosome formation in renal artery walls of a patient with CRF (Figure 1g). Thus, high Pi promoted autophagy in both animal and HA-VSMCs. ROS mediate Pi-induced autophagy in VSMCs Mitochondrial ROS production contributes to autophagosome formation in many conditions, and the superoxide dismutase mimic MnTMPyP reduces Pi-induced calcification by eliminating mitochondrial ROS.15 Here, Pi significantly increased mitochondrial ROS level in BASMCs (Figure 2a). MnTMPyP (25 mmol/l), as well as SOD2 overexpression, significantly decreased Pi-increased LC3II level in BASMCs (Figure 2b and c). These results were further confirmed by MnTMPyP, decreasing the Pi-increased formation of GFP–LC3 puncta from 47.2 to 20.3% in BASMCs (Figure 2d). Therefore, ROS generation mediated Pi-induced autophagy in vitro. In addition, MnTMPyP reduced LC3 level (Figure 2e) and mitochondrial ROS level (Figure 2f) in abdominal aortas of CRF rats with high serum Pi level (2.73±0.10 mmol/l in control group vs. 5.50±0.36 mmol/l in CRF group, Po0.05). Indirect immunofluorescence analysis of LC3 puncta in both calcified and non-calcified regions of the aorta (Supplementary Figure S2 online) further showed that MnTMPyP decreased autophagosome formation in the abdominal aortic wall of CRF rats (Figure 2f). Type III sodium-dependent Pi cotransporter Pit1 mediates Pi-induced autophagy HA-VSMCs were transfected with scramble small interfering RNA (siRNA) or Pit1 siRNA for 48 h; knockdown of Pit1 expression was confirmed by reverse transcriptase PCR Kidney International (2013) 83, 1042–1051 basic research (Figure 3a) and western blot analyses (Figure 3b). Pi increased LC3II level in scramble siRNA–treated HA-VSMCs, and Pit1 knockdown significantly reduced Pi-increased LC3II level (Figure 3c). Similarly, Pit1 knockdown significantly decreased Pi-induced calcium deposition (Figure 3d). Therefore, Pit1 mediated Pi-induced autophagy and calcification in VSMCs. Inhibition of Pi-induced autophagy aggravates calcification To address the potential role of autophagy in Pi-induced calcification in VSMCs, we first used 3-MA (5 mmol/l), a pharmacological inhibitor of autophagy. 3-MA attenuated the Pi-increased LC3II level (Figure 4a) and formation of LC3 puncta (43% reduction) (Figure 4b). To confirm the pharmacological results of 3-MA, siRNA knockdown of autophagy protein 5 (Atg5) expression in rat VSMCs (Figure 4c and Supplementary Figure S3 online) resulted in a significant reduction of LC3 puncta in Pi-treated rat VSMCs (Figure 4d). Alizarin red S staining (Figure 5a) and calcium content assay (Figure 5b) revealed that 3-MA increased calcium deposition in BASMCs pretreated with Pi (3 mmol/l) at 3, 7, and 10 days. Similarly, in HA-VSMCs (Figure 5c) and rat VSMCs (Figure 5d), 3-MA significantly increased Pi-induced calcium deposition. These findings were further confirmed by siRNA knockdown of Atg5, which significantly augmented Pi-induced calcium deposition in both primary rat VSMCs (Figure 5e) and the rat SMC cell line A7r5 (Figure 5f). Furthermore, ex vivo experiments of rat aortic rings showed that 3-MA aggravated Pi-induced calcification (Figure 5g). In contrast, valproic acid (1 mmol/l), a pharmacological inducer of autophagy, significantly ameliorated Pi-induced calcium deposition in both cultured rat aortic rings (Figure 6a) and BASMCs (Figure 6b). Therefore, autophagy ameliorated Pi-induced vascular calcification. The pro-calcification effect of autophagy inhibition does not involve ROS-induced apoptosis Autophagy induction under cellular stress may contribute to cell apoptosis or be a mechanism for cell survival, and VSMC apoptosis is one of the mechanisms of Pi-promoted vascular calcification.21,22 As expected, Pi increased the activity of apoptosis marker–cleaved caspase-3 (Figure 7a) and caspase3/7 (Figure 7b). These increases were reversed by siRNA knockdown of Atg5 and MnTMPyP in rat VSMCs. Consistently, both 3-MA and MnTMPyP reduced the Piincreased apoptosis (indicated by terminal transferase dUTP nick-end labeling staining) (Figure 7c and Supplementary Figure S4 online) and caspase-3/7 activity (Figure 7d) in BASMCs. Interestingly, MnTMPyP and autophagy inhibition by Atg5 siRNA knockdown or 3-MA had a synergistic effect on reducing caspase 3/7 activation and apoptosis (Figure 7b–d). However, the apoptosis inhibitor Z-VAD-FMK (20 mmol/l) significantly ameliorated Pi-induced calcification; 3-MA still significantly aggravated Pi-induced calcification, even in the presence of Z-VAD-FMK (Figure 7e). 1043 basic research X-Y Dai et al.: Autophagy counteracts vascular calcification a b BASMCs Pi (mM) LC3I LC3II 0 1.5 2 2.5 β-Actin LC3II protein level * 3 * 2 1 d BASMCs Ctrl Pi (3 mM) GFP–LC3 Control * 8 * BASMCs Pi (3 mM) % Cells with GFP–LC3 puncta LC3II protein level 4 e Chq+Pi LC3I LC3II β-Actin c BASMCs Pi Chq Ctrl 3 6 * * 4 2 BASMCs 80 Control * Pi (3 mM) * 60 * * 0.5 Days 1 Day 40 20 f Control 3 Days HA-VSMCs 7 Days Pi (3 mM) GFP-LC3 1 μm 1 μm g 2 μm Human renal artery wall Donor CKD 2 μm Figure 1 | Phosphate (Pi) induces autophagy in vascular smooth muscle cells (VSMCs). (a) Western blot analysis of light-chain 3-II (LC3II) levels in bovine aortic smooth muscle cells (BASMCs) treated with Pi at the indicated concentrations for 12 h and (b) in BASMCs pretreated with chloroquine (Chq, 25 mmol/l) for 30 min, then with Pi for 12 h. (c) Confocal microscopy of green fluorescent protein (GFP) in BASMCs transfected with GFP–LC3 plasmids, cultured for 36 h, and then treated with Pi for 12 h. Autophagosomes are indicated by fluorescence puncta. (d) Percentage of BAMSCs with GFP–LC3 puncta after Pi treatment for the indicated durations. *Po0.05 versus corresponding control. (e) Electron microscopy of autophagic structures (arrows) in cells exposed to Pi for 12 h. n ¼ 3–4, one representative image is shown. (f) Confocal microscopy of GFP–LC3 puncta in human aortic VSMCs (HA-VSMCs) transfected with GFP–LC3 plasmids and treated with Pi (3 mmol/l) for 12 h. (g) Immunofluorescence analysis of LC3 puncta in renal artery wall from human organ donor and recipient with chronic kidney disease during renal transplantation. CKD, chronic kidney disease. Thus, the pro-calcification effect of autophagy inhibition may not be associated with ROS-induced apoptosis. Autophagy inhibition increases Pi-induced MV release MVs were isolated from cell lysates by collagenase digestion. Pi significantly increased MV release, from 0.9 to 5.5 mg, and 1044 inhibition of autophagy by 3-MA further promoted Pi-induced MV release, from 5.5 to 9.6 mg, in BASMCs (Figure 8a). Annexin II protein content was significantly increased in MVs from calcified BASMCs, and 3-MA further increased the content (Figure 8b). Furthermore, assay of alkaline phosphatase (ALP) activity as shown by ELF 97 Kidney International (2013) 83, 1042–1051 basic research X-Y Dai et al.: Autophagy counteracts vascular calcification a b BASMCs * 0 3 MnTMPyP LC3I 0 0 15 3 mM 25 μM LC3II Pi (3 mM) LC3I LC3II 5 Control Pi d * * 2.0 1.5 1.0 0.5 % Cells with GFP–LC3 puncta BASMCs Control Pi+MnTMPyP Pi – Ad-SOD2 + – + β-Actin 2.5 LC3II protein level 10 BASMCs Ad-GFP β-Actin LC3II protein level Fluorescence intensity (a.u.) 20 c BASMCs Pi * 1.5 * 1.0 0.5 60 * * 40 20 GFP–LC3 Control e * CRF CRF+MnTMPyP LC3 β-Actin LC3 protein level 3 Control * 2 1 Control f CRF Anti-LC3 CRF+ MnTMPyP % Cells with LC3 puncta * Mitochondrial ROS CRF * 30 20 10 Control Control Pi+ MnTMPyP Pi CRF CRF+ MnTMPyP CRF+MnTMPyP Figure 2 | Reactive oxygen species (ROS) mediate phosphate (Pi)-induced autophagy in vascular smooth muscle cells (VSMCs). (a) Confocal microscopy of fluorescence with control and Pi (3 mmol/l) induction in bovine aortic smooth muscle cells (BASMCs) incubated with MitoTracker Red CM-H2XRos probe for 30 min to indicate mitochondrial ROS level. (b) Western blot analysis of light-chain 3 (LC3)I/II level in BASMCs pretreated with MnTMPyP for 30 min, or (c) infected with adenovirus-expressing green fluorescent protein (GFP) or superoxide dismutase 2 (SOD2) for 24 h, and then treated with Pi for 12 h. (d) Immunofluorescence and percentage of cells with GFP–LC3 puncta in BASMCs treated with Pi (3 mmol/l) and/or MnTMPyP (25 mmol/l) for 12 h. (e) Western blot analysis of LC3 protein level in abdominal aortas of rats with chronic renal failure (CRF) with control, vehicle (CRF), and CRF plus MnTMPyP (CRF þ MnTMPyP) treatment and (f) immunofluorescence of LC3 puncta and MitoTracker Red CM-H2XRos probe (200 nmol/l) for mitochondrial ROS in rat abdominal aorta walls. n ¼ 3–5, *Po0.05. phosphatase substrate activity indicated increased number of ELF 97–positive MVs in calcified BASMCs, which could be further increased by 3-MA treatment (Figure 8c). In addition, ALP activity, considered a marker of MV maturation, was Kidney International (2013) 83, 1042–1051 further increased by 3-MA treatment in calcified BASMCs (Figure 8d), and the release of ALP into the MV fraction, indicated by the ratio of MV ALP to total cellular ALP, was also increased in 3-MA-treated cells (Supplementary 1045 basic research si R N A Pit1/2 protein level β-Actin 1.5 Scramble LC3II protein level 3 0 3 Pit1 siRNA 0 0.5 2 1 * * * 2 40 20 1 Pi Control 3-MA+Pi 200 Atg5 100 β-Actin 1.5 Control Pi Control Pi Scramble Pit1 siRNA Figure S5a and b online). Thus, the pro-calcification effect of autophagy inhibition may contribute to its promotion of MV release. DISCUSSION In this study, we showed that Pi-increased ROS levels potentiated autophagy in cultured VSMCs and aortic walls of a dietary adenine–induced rat CRF model, and the sodium-dependent Pi cotransporter Pit1 mediated the Piinduced autophagy. Inhibition of autophagy by 3-MA or siRNA knockdown of the autophage protein Atg5 significantly aggravated Pi-induced calcium deposition in vitro and ex vivo. However, valproic acid, a pharmacological inducer of autophagy, significantly ameliorated the increased calcification. The underlying mechanisms of the pro-calcification effect of autophagy inhibition involved increased MV release rather than cell apoptosis. Thus, targeting the autophagy pathway may help to prevent or treat vascular calcification in patients with end-stage renal disease. As autophagy is linked to conditions such as neurodegenerative diseases, cancer, and cardiovascular diseases, it is a prime target for developing therapeutic treatments for these diseases.23 Evidence of the importance of hyperphosphatemia as a major inducer of vascular calcification comes from studies of genetic syndromes and diseases of renal insufficiency;13 increased Pi exposure results in the conversion of Rat VSMCs Rat VSMCs Control Scramble Atg5 siRNA * Figure 3 | Type III sodium-dependent phosphate cotransporter Pit1 mediates phosphate (Pi)-induced autophagy in vascular smooth muscle cells (VSMCs). (a) Reverse transcriptase PCR analysis of mRNA levels of Pit1 and Pit2 in human VSMCs (HA-VSMCs) transfected with scramble or Pit1 siRNA for 48 h. (b) Western blot analysis of Pit1/2 protein levels in HA-VSMCs transfected with scramble or Pit1 siRNA for 48 h. (c) Light chain 3 (LC3)I/II protein levels in HA-VSMCs transfected with scramble or Pit1 siRNA for 48 h, then treated with Pi (3 mM) for 12 h. (d) Calcium content assay of HAVSMCs transfected with scramble or Pit1 siRNA for 48 h, then treated with Pi (3 mM) for 10 days. n ¼ 3, *Po0.05. 1046 * * 3 mM 300 * * 3 1.0 0.5 * 50 % Cells with Lc3 puncta Scramble Pi LC3-I LC3-II β-Actin Pit1 siRNA 1.0 Atg5 protein level Control % Cells with GFP–Lc3 puncta β-Actin 1.0 * BASMCs * 60 LC3II Pit1/2 0.5 BASMCs Control Pi 3-MA+Pi LC3I Lc3-II protein level Pit2 Pi t1 l tro C on Pit1 Calcium content mg/g prot Relative mRNA level 1.5 Sc ra m bl e X-Y Dai et al.: Autophagy counteracts vascular calcification * * 40 30 20 10 Scramble Scramble Atg5 siRNA +Pi +Pi Figure 4 | Phosphate (Pi)-induced autophagy is abolished by autophagy inhibition. (a) Western blot analysis of light-chain 3 (LC3)I/II protein levels in bovine aortic smooth muscle cells (BASMCs) pretreated with autophagy inhibitor 3-methyladenine (3-MA 5 mmol/ l) for 30 min, and then with Pi (3 mmol/l) for 12 h. (b) Percentage of cells with green fluorescent protein (GFP)–LC3 puncta in BASMCs treated with Pi (3 mmol/l) or 3-MA þ Pi for 12 h. (c) Western blot analysis of protein level of autophagy protein 5 (Atg5) in rat vascular smooth muscle cells (VSMCs) transfected with scramble or Atg5 small interfering RNA (siRNA) for 48 h. (d) Percentage of GFP–LC3 puncta in rat VSMCs transfected with scramble or Atg5 siRNA for 48 h, and then with Pi for 12 h. n ¼ 3, *Po0.05. contractile VSMCs to osteogenic/chondrogenic cells, cell apoptosis, MV release, and matrix remodeling, followed by vascular calcification.14 Here, we showed that autophagy involved in Pi-induced vascular calcification. Elevated Pi level could induce autophagy, as shown by the formation of GFP–LC3 puncta, increased LC3II level, and electron microscopy of typical autophagic structures in cultured VSMCs and a rat CRF model, as well as the human aortic wall. Our previous report15 showed that elevated Pi level could increase the production of mitochondrial ROS, and scavenging intracellular O2 by MnTMPyP and SOD2 overexpression significantly decreased Pi-induced calcification and autophagy. Thus, increased O2 level has an important role in Pi-induced autophagy. Chen et al.17 also showed that O2 is the major ROS-regulating autophagy. Pit1 was previously found to have an important role in Pi-induced calcification.24 We also demonstrated that Pit1 was the dominant Pi cotransporter in VSMCs. SiRNA knockdown of Pit1 significantly reduced the Pi-induced calcification and autophagy. Thus, Pit1-mediated Pi transport and ROS generation have a vital role in Pi-induced autophagy. High Pi level may be a new inducer of autophagy, in addition to starvation and H2O2, which may help in further exploring the mechanisms of Pi-induced vascular diseases. Autophagy is a multifunctional process involved in various cellular activities23 and is essential for survival, Kidney International (2013) 83, 1042–1051 basic research X-Y Dai et al.: Autophagy counteracts vascular calcification 3-MA+Pi Pi 3-MA * * 300 * 200 100 * 300 Calcium content mg/g prot Pi 400 Calcium content mg/g prot BASMCs Calcium content mg/g prot Control Rat VSMCs 10 days HA-VSMCs 10 days BASMCs 7 days Alizarin red S staining * 200 100 Control 3 Days 7 Days 10 Days Ctrl Pi * 300 200 * 100 3-MA 3-MA+Pi Ctrl Pi 3-MA 3-MA+Pi Calcium content mg/g prot Calcium content mg/g prot 150 A7r5 10 days * 100 * 50 Control Pi Scramble 150 * 100 * 50 Control Pi Scramble Control Pi Atg5 siRNA Control Pi Atg5 siRNA Calcium content mg/g prot Rat aortic ring Rat VSMCs 10 days 10 * 8 6 * 4 2 Control Pi 3-MA 3-MA+Pi Figure 5 | Blockage of autophagy exacerbates phosphate (Pi)-induced calcification. (a–d) Cells were treated with Pi (3 mmol/l) or Pi þ 3methyladenine (3-MA) (5 mmol/l) for the indicated days, and then alizarin red S staining (a) and calcium content assay were performed (b–d). (e) Calcium content assay of rat vascular smooth muscle cells (VSMCs) and (f) A7r5 cells transfected with scramble or autophagy protein 5 (Atg5) small interfering RNA (siRNA) for 48 h, and then treated with Pi for 10 days; (g) rat aortic ring explants treated with Pi (3 mmol/l) and/or 3-MA (5 mmol/l) for 7 days. n ¼ 3–5, *Po0.05. BASMCs, bovine aortic smooth muscle cells; HA-VSMCs, human aortic VSMCs. BASMCs * 3 Calcium content mg/g prot Calcium content mg/g prot Rat aortic ring 4 * 2 1 Ctrl Pi VPA VPA+Pi 1000 * * 800 600 400 200 Ctrl Pi VPA VPA+Pi Figure 6 | Autophagy inducer valproic acid (VPA) reduces calcification. (a) Calcium content assay of rat aortic ring explants and (b) bovine aortic smooth muscle cells (BASMCs) treated with phosphate (Pi) (3 mmol/l) and/or VPA (1 mmol/l) for 7 days. n ¼ 3, *Po0.05. differentiation and development, as well as the cell response to stress.2,25 We wondered whether autophagy functionally contributed to Pi-induced calcification. Autophagy inhibition by both the pharmacological inhibitor 3-MA and siRNA knockdown of Atg5 significantly aggravated Pi-induced calcium deposition in both animal and human aortic cells, including BASMCs, rat VSMCs, HA-VSMCs, and the A7r5 cell line. As expected, the pharmacological autophagy inducer valproic acid had a therapeutic effect on Pi-induced calcification in BASMCs and rat aortic rings. Thus, autophagy may be an endogenous protective mechanism counteracting vascular calcification under hyperphosphatemia. Further research is needed regarding therapeutic agents that influence the autophagic response for treating aging or disease-related vascular calcification. We wondered how autophagy inhibition augmented Pi-induced calcium deposition. VSMC apoptosis is an important mechanism for Pi-promoted vascular calcification, and drugs that inhibit apoptosis can ameliorate Kidney International (2013) 83, 1042–1051 calcification.21,22 Autophagy induction under cellular stress may contribute to cell apoptosis or be a mechanism of cell survival.26 The cytotoxic effects of autophagy may be explained by the direct self-destructive potential of massive autophagy (type II cell death)27 or by hardwiring the autophagic process to pro-apoptotic signals (type I cell death).28 In both scenarios, caspase-3 activity is increased. Atg5 has a dual role in autophagy, and apoptosis is regulated by proteolysis of Atg5; thus, siRNA knockdown of Atg5 was found to abolish autophagy and reduce apoptosis.29 In our study, the Pi-increased caspase-3 activity and terminal transferase dUTP nick-end labeling-positive cells in VSMCs was reversed by the ROS scavenger MnTMPyP. In addition, autophagy inhibition by 3-MA and Atg5 siRNA knockdown reduced the formation of autophagosomes and Pi-increased apoptosis. Finally, autophagy inhibition aggravated Pi-induced calcification even when cell apoptosis was blocked by Z-VAD-FMK. Thus, ROS mediates Pi-induced apoptosis and calcification, but the pro-calcification effect of autophagy inhibition might not involve ROS-mediated VSMC apoptosis. Thus, an additional mineralization-specific mechanism could be involved in autophagy inhibition–aggravated calcification. Growing evidence suggests that membranebound vesicles from cells are involved in both physiological and pathological calcification.30 Calcifying membrane-bound vesicles (here, MVs) released from VSMCs participating in VSMC mineralization have been reported in both human SMCs and BASMCs.31,32 MVs are membrane-enclosed microstructures released from the cell membrane that have a key role in hydroxyapatite formation and the mineralization process, and the release of ALP into the MV 1047 basic research X-Y Dai et al.: Autophagy counteracts vascular calcification a b ! Rat VSMCs – – 0 0 – – 0 3 + – 0 3 – + 0 3 – – 25 μM 3 mM β-Actin 1.0 ! 10 ! ! * 15 – – 0 0 – – 0 3 + – 0 3 – + 0 3 – – 25 μM 3 mM # # 5 # 1 2 3 4 5 0 0 0 0 0 3 5 0 3 0 25 3 5 mM 25 μM 3 mM # 5 # Scramble Atg5 siRNA MnTMPyP Pi 1 2 3 4 + – 0 0 + – 0 3 – + 0 3 + + 25 3 e BASMCs 8 10 # 0.5 * ! 6 # # 4 # 2 3-MA MnTMPyP Pi * 300 ! 1 2 3 4 5 0 0 0 0 0 3 5 0 3 0 25 3 5 mM 25 μM 3 mM 5 – + 25 μM 3 mM BASMCs ! Luminescence (RLU ×10 5) %TUNEL-positive cells # d BASMCs 20 3-MA MnTMPyP Pi 1.5 Scramble Atg5 siRNA MnTMPyP Pi c * * * 2.0 * * Calcium content mg/g prot Scramble Atg5 siRNA MnTMPyP Pi Cleaved caspase-3 Rat VSMCs 15 Luminescence (RLU ×10 4) Cleaved caspase-3 protein level 2.5 200 100 3-MA Z-VAD-FMK Pi 1 2 3 4 5 0 0 0 0 0 3 5 0 3 0 20 3 5 mM 20 μM 3 mM Figure 7 | The pro-calcification effect of autophagy inhibition does not involve reactive oxygen species (ROS)-mediated vascular smooth muscle cell (VSMC) apoptosis. (a) Cleaved caspase-3 and (b) caspase-3/7 activity detected in rat VSMCs transfected with scramble or autophagy protein 5 (Atg5) small interfering RNA (siRNA) for 48 h, and then treated with MnTMPyP and/or phosphate (Pi) as indicated for 10 days. (c) Quantification of terminal transferase dUTP nick-end labeling (TUNEL) staining of apoptotic cells in bovine aortic smooth muscle cells (BASMCs) treated with Pi and/or 3-methyladenine (3-MA) and MnTMPyP as indicated for 7 days. (d) Caspase-3/7 activity and (e) calcium content assay in BASMCs treated with 3-MA, MnTMPyP, Z-VAD-FMK, and/or Pi as indicated for 7 days. n ¼ 3, *Po0.05 versus corresponding group 1 or as indicated; #Po0.05 versus corresponding group 2; !Po0.05 versus corresponding group as indicated. a BASMCs b * BASMCs Pi (3 mM) – + 3-MA (5 mM) – + Annexin II 10 * 5 Ctrl c * 5 Annexin II protein level MV release (μg) 15 Pi 4 3 * 2 1 3-MA 3-MA+Pi BASMCs Ctrl Pi 1 μm 1 μm Pi+3-MA 3-MA ALP activity (IU/mg prot) d BASMCs * 0.3 * 0.2 0.1 Ctrl 1 μm Pi 3-MA 3-MA+Pi 1 μm Figure 8 | Blocking autophagy promotes matrix vesicle (MV) release. (a–c) Bovine aortic smooth muscle cells (BASMCs) were treated with phosphate (Pi) (3 mmol/l) and/or 3-methyladenine (3-MA) (5 mmol/l) for 3 days, MVs were isolated by centrifugation, and then (a) MV release was assessed by total protein content. (b) Western blot analysis of protein level of annexin II (MV marker) in MVs. (c) Alkaline phosphatase (ALP) activity shown by ELF 97 phosphatase substrate in cultured BASMCs. (d) Assay of ALP activity in MVs. n ¼ 4, *Po0.05. 1048 Kidney International (2013) 83, 1042–1051 X-Y Dai et al.: Autophagy counteracts vascular calcification fraction is an important process for MV-mediated mineralization.30–32 Recently, 1,25(OH)2D3 was found to stimulate mineralization by increasing MV production.33 Here, inhibition of autophagy increased Pi-induced MV release and ALP activity, which may be the cause of calcification aggravated by autophagy inhibition. Furthermore, previous works have shown that MV can selectively load ALP in both VSMCs34 and chondrocytes, and actin polymerization inhibited by cytochalasin D can increase the release of ALP into the MV fraction.35,36 In the present study, the ratio of MV ALP to cell ALP indicated increased release of ALP into the MV fraction in 3-MA-treated cells without affecting cellular ALP and osteogenic gene expression, which may indicate that cellular ALP is interrelated with osteogenic differentiation, whereas the release of ALP into the MV fraction involves other mechanisms. The process and mechanism of MV formation and release are not completely understood, but some evidence suggests that the actin cytoskeleton is involved in the release of MVs from chondrocytes/osteoblast-like cells.36–38 Despite the absence of direct evidence of the influence of autophagy on the cytoskeleton, cytoskeletal components contribute to the formation of autophagy,39 and pro-renin receptor knockout can alter the cytoskeleton and lead to the accumulation of LC3-positive vesicles.40 Our results showed that 3-MA markedly decreased SM-a-actin expression (Supplementary Figure 6a online) and affected cell shape and actin/SM-aactin distribution (Supplementary Figure 6b online) but not the expression of Pi-induced osteogenesis genes (Supplementary Figure 6a online). Therefore, we can not exclude the fact that autophagy inhibition may contribute to MV release and load of ALP by regulating the cytoskeleton, which needs further exploration. Several epidemiological studies suggested a relationship between vascular calcification, impaired bone metabolism, and increased mortality, both in patients with chronic kidney disease and the general aging population.41–43 Basal autophagy has an important role in maintaining chondrocyte and osteoblast/osteocyte survival and terminal differentiation, as well as in regulating bone growth.20 With our finding that autophagy is an endogenous protective mechanism counteracting vascular calcification under hyperphosphatemia, therapeutic agents acting on the autophagic response and activities of autophagy-regulating pathways could be developed to treat aging or disease-related vascular calcification and osteoporosis. MATERIALS AND METHODS Animal protocols Abdominal aortas were from the CRF rat model fed with 0.75% adenine and 0.9% phosphorus, as we described previously15 and used for both morphology and western blot analysis. The rat CRF model was confirmed by increased levels of serum creatinine, blood urea nitrogen, and blood Pi in blood samples. MnTmPyP (C44H36Cl5MnN8, 30 nmol/l/day, Calbiochem, Darmstadt, Germany) was given intraperitoneally. Kidney International (2013) 83, 1042–1051 basic research Cell culture and cell calcification model BASMCs and rat VSMCs were isolated and cultured as described.44–46 Briefly, segments of aortas were obtained from prepubertal bovines and rats. The inner portion of the medium was removed and cut into B1-mm2 sections, which were placed in a culture dish with Dulbecco’s modified Eagle’s medium (DMEM) containing 4.5 g/l glucose supplemented with 20% fetal bovine serum (FBS) and 10 mmol/l sodium pyruvate. Cells that migrated from the explants were grown in DMEM plus 15% FBS; cells between passages 3 and 8 were used in experiments. T/G HA-VSMCs were from ATCC (Rockville, MD) and cultured in DMEM plus 10% FBS. For calcification experiments, cells were seeded at a density of 1104 cells/cm2 (day 0) and maintained in 15% FBS–DMEM until confluence (day 6), when calcification was induced by adding 10 mmol/L-b-glycerophosphate or 3 mmol/l Pi (Sigma, St Louis, MO). Calcium deposits were detected by measuring calcium content or by alizarin red staining, as we described.15,46 For treatment with antioxidants or inhibitors, MnTMPyP (25 mmol/l), Z-VAD-FMK (Promega, Madison, WI, 20 mmol/l), autophagy inhibitor 3-MA (Calbiochem, 5 mmol/l), or chloroquine (Sigma, 25 mmol/l) was added with Pi every 3 days. Aortic ring calcification Aortas (from the thoracic to the iliac arteries) were removed in a sterile manner from rats. After the adventitia and endothelium were carefully removed, the vessels were cut into 2- to 3-mm rings and placed in high-Pi (3 mmol/l) or normal culture medium at 37 1C in 5% CO2 for 7 days, with medium changes every 3 days. MV isolation MVs were harvested by following a modified MV isolation protocol.31,47 Confluent BASMCs were washed twice with PBS and transferred to control or high-Pi (3 mmol/l) medium for 3 days, and then the medium was decanted after digestion with collagenase and centrifuged at 10,000 g to remove cells and apoptotic bodies. MVs were then harvested from the supernatant by centrifugation at 100,000 g for 30 min at 4 1C in a Hitachi Ultracentrifuge (Hitachinaka, Ibaraki, Japan). MVs were resuspended with 0.1% HCl or 1% Triton X-100, and protein and ALP activity were determined. An increase in protein level indicated an increased number of MVs. Western blot analysis Cell and aortic extracts were collected after treatment. The protein underwent sodium dodecyl sulfate–polyacrylamide gel electrophoresis and transfer to a nitrocellulose membrane, which was incubated successively with 3% bovine serum albumin and the primary antibodies anti-LC3 (1:1000, CST, Danvers, MA), anti-cleaved caspase 3 (1:1000, CST), anti-Pit1/2, and anti-b-actin (1:500, both Santa Cruz Biotechnology, Santa Cruz, CA), followed by IRDye700or 800–conjugated secondary antibody (1:20,000, Rockland, Gilbertsville, PA) for 1 h. Fluorescence signals were detected by the Odyssey infrared imaging system (LI-COR Biosciences, Lincoln, NE). Immunofluorescence analysis Treated samples were fixed with 4% paraformaldehyde and then rendered permeable by incubation in 0.1% Triton X-100 in 5% bovine serum albumin–phosphate-buffered saline for 15 min; the 1049 basic research samples were then treated with the antibody anti-LC3, actin, or SM-a-actin (1:200) overnight at 4 1C, followed by treatment with secondary antibody Alexa Fluor R488 donkey anti-rabbit IgG (1:500) for 1 h at 37 1C. Nuclei were labeled with Hoechst 33342. Replacing the primary antibody with normal IgG served as a negative control. Alizarin red S staining Cells in 6-well plates were washed three times with PBS and fixed with 10% formaldehyde for 10 min. After three washes with PBS, cells were exposed to 1% Alizarin red S for 30 min and washed with 0.2% acetic acid. Positively stained cells showed a reddish/ purple color. Apoptosis analysis VSMC apoptosis was assessed by measuring caspase 3/7 activity with the use of the Caspase-Glo 3/7 Assay Kit (Promega) and terminal transferase dUTP nick-end labeling assay (Promega). Analysis of autophagy by GFP–LC3 redistribution At 24 h after plating, cells were transfected with GFP–LC3 expression vector (kindly provided by Dr Wei-Gou Zhu, Peking University) by the Lipofectamine 2000 method (Invitrogen, Grand Island, NY). Next, 6 h later, the transfection medium was replaced with DMEM containing 10% FBS. The next day, cells were treated as described. The GFP signal was monitored by confocal laser scanning microscopy (Leica, Bannockburn, IL). The following criteria were used to determine cells with punctuate GFP–LC3 (positive cells): (1) uneven, ring-shaped dots in cytoplasm; (2) mean number of uneven, ring-shaped dots per cell among 500 randomly selected normal cells; and (3) more dots than the mean number of normal cells. The percentage of positive cells was recorded for quantification. RNA interference siRNA against rat Atg5, human type III sodium-dependent Pi cotransporters Pit1 (Slc20a1), and control siRNA were synthesized by Invitrogen. The siRNA sequences for Atg5 were 50 -UUCAGGACC UGGAAAGCCAUUGUUG-30 (sense) and 50 -CAACAAUGGCUUU CCAGGUCCUGAA-30 (antisense); Pit1 50 -GCGCAAUAAUAGCUA UACUTT-30 (sense); and 50 -AGUAUAGCUAUUAUUGCGCTT-30 (antisense). Cells cultured in 6-well plates were transfected with siRNA at a final concentration of 10 nmol/l by the Lipofectamine RNAiMAX Reagent method (Invitrogen), and then incubated for 4 h at 37 1C before the addition of 10% fetal calf serum for 48 h. At the end of treatment, cells were harvested for experiments. Gene knockdown was confirmed by real-time PCR and western blot analyses. The primers for rat Atg5 were 50 -TCAGTGGAGGCAACAG AACC-30 (sense) and 50 -CAGACACGAACTGGCACATT-30 (antisense); Pit1 50 -CCAACTGTGCAGGCATAGAA-30 (sense) and 50 -TT CTTCCTGGTTCGTGCATT-30 (antisense). Electron microscopy Electron microscopy was performed at our institution’s microscopy facility. Briefly, cells were prefixed with 3% glutaraldehyde and postfixed with 2% osmium tetraoxide. After dehydration, cells were embedded in epoxy resin. Ultrathin sections were cut, contrasted with uranyl acetate and lead citrate, and examined under a Zeiss EM-109 electron microscope (Carl Zeiss AG, Carl-Zeiss-Strasse, Oberkochen, Germany). 1050 X-Y Dai et al.: Autophagy counteracts vascular calcification ALP activity ALP activity was measured colorimetrically as the hydrolysis of p-nitrophenyl Pi with the use of an ALP assay kit (Jiancheng Bioengineering, Nanjing, China). Results were normalized to levels of total protein. Cells or aortic rings were homogenized with 1% Triton X-100 in 0.9% saline on ice and centrifuged in a microfuge at 8000 g for 5 min. The supernatant was removed for ALP and protein concentration assay. Statistical analysis Data are reported as mean±s.e.m. Unpaired Student’s t-test was used for analysis of two groups and one-way analysis of variance for three or more groups, followed by Bonferroni’s multiple comparison test as applicable by the use of Prism 5. Po0.05 was considered to be statistically significant. DISCLOSURE All the authors declared no conflict of interest. ACKNOWLEDGMENTS This study was supported by the National Basic Research Program of China (2010CB912504 and 2011CB503904), the National Science & Technology Pillar Program (2012BAI39B03), the National Natural Science Foundation of China (81270370, 30900566, 81170099, 81121061, and 31230035), and the Beijing Natural Science Foundation (Mammalian Target of Rapamycin Complex-1 (mTORC1) Promotes Vascular Smooth Muscle Cell Calcification). SUPPLEMENTARY MATERIAL Figure S1. Pi induced autophagy in T/G human aortic VSMCs (HAVSMCs). Figure S2. LC3 puncta cells were found in both calcified and noncalcified aortic wall in chronic renal failure rats. Figure S3. Knockdown of Atg5 by siRNA. Figure S4. TUNEL staining (red) to identify apoptotic cells. Figure S5. The effects of autophagy inhibition on release of alkaline phosphatase (ALP) into the matrix vesicle (MV) fraction. Figure S6. The effects of autophagy inhibition on VSMC phenotypic transition. Supplementary material is linked to the online version of the paper at http://www.nature.com/ki REFERENCES 1. Meijer AJ. Amino acids as regulators and components of nonproteinogenic pathways. J Nutr 2003; 133: 2057S–2062S. 2. Levine B, Klionsky DJ. Development by self-digestion: molecular mechanisms and biological functions of autophagy. Dev Cell 2004; 6: 463–477. 3. Cuervo AM. Autophagy: in sickness and in health. Trends Cell Biol 2004; 14: 70–77. 4. Shintani T, Klionsky DJ. Autophagy in health and disease: a double-edged sword. Science 2004; 306: 990–995. 5. De Meyer GR, Martinet W. Autophagy in the cardiovascular system. Biochim Biophys Acta 2009; 1793: 1485–1495. 6. Martinet W, De Meyer GR. Autophagy in atherosclerosis: a cell survival and death phenomenon with therapeutic potential. Circ Res 2009; 104: 304–317. 7. Zhang H, Bosch-Marce M, Shimoda LA et al. Mitochondrial autophagy is an HIF-1-dependent adaptive metabolic response to hypoxia. J Biol Chem 2008; 283: 10892–10903. 8. Crighton D, Wilkinson S, O’Prey J et al. DRAM, a p53-induced modulator of autophagy, is critical for apoptosis. Cell 2006; 126: 121–134. 9. London GM, Guerin AP, Marchais SJ et al. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant 2003; 18: 1731–1740. 10. Block GA, Port FK. Re-evaluation of risks associated with hyperphosphatemia and hyperparathyroidism in dialysis patients: recommendations for a change in management. Am J Kidney Dis 2000; 35: 1226–1237. Kidney International (2013) 83, 1042–1051 basic research X-Y Dai et al.: Autophagy counteracts vascular calcification 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. Giachelli CM, Jono S, Shioi A et al. Vascular calcification and inorganic phosphate. Am J Kidney Dis 2001; 38: S34–S37. Ohnishi M, Nakatani T, Lanske B et al. In vivo genetic evidence for suppressing vascular and soft-tissue calcification through the reduction of serum phosphate levels, even in the presence of high serum calcium and 1,25-dihydroxyvitamin D levels. Circ Cardiovasc Genet 2009; 2: 583–590. Giachelli CM. The emerging role of phosphate in vascular calcification. Kidney Int 2009; 75: 890–897. Shanahan CM, Crouthamel MH, Kapustin A et al. Arterial calcification in chronic kidney disease: key roles for calcium and phosphate. Circ Res 109: 697–711. Zhao MM, Xu MJ, Cai Y et al. Mitochondrial reactive oxygen species promote p65 nuclear translocation mediating high-phosphate-induced vascular calcification in vitro and in vivo. Kidney Int 79: 1071–1079. Zhao G, Xu MJ, Zhao MM et al. Activation of nuclear factor-kappa B accelerates vascular calcification by inhibiting ankylosis protein homolog expression. Kidney Int 82: 34–44. Chen Y, Azad MB, Gibson SB. Superoxide is the major reactive oxygen species regulating autophagy. Cell Death Differ 2009; 16: 1040–1052. Chen Y, Gibson SB. Is mitochondrial generation of reactive oxygen species a trigger for autophagy? Autophagy 2008; 4: 246–248. Huang J, Lam GY, Brumell JH. Autophagy signaling through reactive oxygen species. Antioxid Redox Signal 14: 2215–2231. Srinivas V, Bohensky J, Zahm AM et al. Autophagy in mineralizing tissues: microenvironmental perspectives. Cell Cycle 2009; 8: 391–393. Son BK, Kozaki K, Iijima K et al. Statins protect human aortic smooth muscle cells from inorganic phosphate-induced calcification by restoring Gas6-Axl survival pathway. Circ Res 2006; 98: 1024–1031. Proudfoot D, Skepper JN, Hegyi L et al. Apoptosis regulates human vascular calcification in vitro: evidence for initiation of vascular calcification by apoptotic bodies. Circ Res 2000; 87: 1055–1062. Mizushima N, Levine B, Cuervo AM et al. Autophagy fights disease through cellular self-digestion. Nature 2008; 451: 1069–1075. Li X, Yang HY, Giachelli CM. Role of the sodium-dependent phosphate cotransporter, Pit-1, in vascular smooth muscle cell calcification. Circ Res 2006; 98: 905–912. Kiffin R, Bandyopadhyay U, Cuervo AM. Oxidative stress and autophagy. Antioxid Redox Signal 2006; 8: 152–162. Maiuri MC, Zalckvar E, Kimchi A et al. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat Rev Mol Cell Biol 2007; 8: 741–752. Scott RC, Juhasz G, Neufeld TP. Direct induction of autophagy by Atg1 inhibits cell growth and induces apoptotic cell death. Curr Biol 2007; 17: 1–11. Espert L, Denizot M, Grimaldi M et al. Autophagy is involved in T cell death after binding of HIV-1 envelope proteins to CXCR4. J Clin Invest 2006; 116: 2161–2172. Yousefi S, Perozzo R, Schmid I et al. Calpain-mediated cleavage of Atg5 switches autophagy to apoptosis. Nat Cell Biol 2006; 8: 1124–1132. Anderson HC. Matrix vesicles and calcification. Curr Rheumatol Rep 2003; 5: 222–226. Kidney International (2013) 83, 1042–1051 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. Reynolds JL, Joannides AJ, Skepper JN et al. Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD. J Am Soc Nephrol 2004; 15: 2857–2867. Chen NX, O’Neill KD, Chen X et al. Annexin-mediated matrix vesicle calcification in vascular smooth muscle cells. J Bone Miner Res 2008; 23: 1798–1805. Woeckel VJ, Alves RD, Swagemakers SM et al. 1Alpha,25-(OH)2D3 acts in the early phase of osteoblast differentiation to enhance mineralization via accelerated production of mature matrix vesicles. J Cell Physiol 225: 593–600. Chen NX, Kircelli F, O’Neill KD et al. Verapamil inhibits calcification and matrix vesicle activity of bovine vascular smooth muscle cells. Kidney Int 77: 436–442. Dean DD, Schwartz Z, Bonewald L et al. Matrix vesicles produced by osteoblast-like cells in culture become significantly enriched in proteoglycan-degrading metalloproteinases after addition of betaglycerophosphate and ascorbic acid. Calcif Tissue Int 1994; 54: 399–408. Hale JE, Wuthier RE. The mechanism of matrix vesicle formation. Studies on the composition of chondrocyte microvilli and on the effects of microfilament-perturbing agents on cellular vesiculation. J Biol Chem 1987; 262: 1916–1925. Hale JE, Chin JE, Ishikawa Y et al. Correlation between distribution of cytoskeletal proteins and release of alkaline phosphatase-rich vesicles by epiphyseal chondrocytes in primary culture. Cell Motil 1983; 3: 501–512. Thouverey C, Strzelecka-Kiliszek A, Balcerzak M et al. Matrix vesicles originate from apical membrane microvilli of mineralizing osteoblast-like Saos-2 cells. J Cell Biochem 2009; 106: 127–138. Mostowy S, Cossart P. Autophagy and the cytoskeleton: new links revealed by intracellular pathogens. Autophagy 7: 780–782. Riediger F, Quack I, Qadri F et al. Prorenin receptor is essential for podocyte autophagy and survival. J Am Soc Nephrol 22: 2193–2202. Frye MA, Melton LJ III, Bryant SC et al. Osteoporosis and calcification of the aorta. Bone Miner 1992; 19: 185–194. Kiel DP, Kauppila LI, Cupples LA et al. Bone loss and the progression of abdominal aortic calcification over a 25 year period: the Framingham Heart Study. Calcif Tissue Int 2001; 68: 271–276. Rodriguez Garcia M, Naves Diaz M, Cannata Andia JB. Bone metabolism, vascular calcifications and mortality: associations beyond mere coincidence. J Nephrol 2005; 18: 458–463. Ross R. The smooth muscle cell. II. Growth of smooth muscle in culture and formation of elastic fibers. J Cell Biol 1971; 50: 172–186. Shioi A, Nishizawa Y, Jono S et al. Beta-glycerophosphate accelerates calcification in cultured bovine vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 1995; 15: 2003–2009. Cai Y, Xu MJ, Teng X et al. Intermedin inhibits vascular calcification by increasing the level of matrix gamma-carboxyglutamic acid protein. Cardiovasc Res 85: 864–873. Wuthier RE, Chin JE, Hale JE et al. Isolation and characterization of calcium-accumulating matrix vesicles from chondrocytes of chicken epiphyseal growth plate cartilage in primary culture. J Biol Chem 1985; 260: 15972–15979. 1051