The Accuracy, Precision and Reliability of Measuring Ventilatory
advertisement

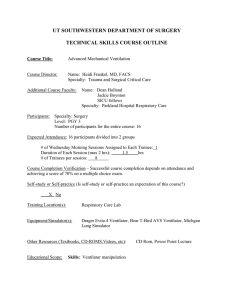
Society for Technology in Anesthesia Section Editor: Maxime Cannesson The Accuracy, Precision and Reliability of Measuring Ventilatory Rate and Detecting Ventilatory Pause by Rainbow Acoustic Monitoring and Capnometry Michael A. E. Ramsay, MD,* Mohammad Usman, PhD,† Elaine Lagow, RN,‡ Minerva Mendoza, RN,§ Emylene Untalan, RN,§ and Edward De Vol, PhD║ BACKGROUND: Current methods for monitoring ventilatory rate have limitations including poor accuracy and precision and low patient tolerance. In this study, we evaluated a new acoustic ventilatory rate monitoring technology for accuracy, precision, reliability, and the ability to detect pauses in ventilation, relative to capnometry and a reference method in postsurgical patients. METHODS: Adult patients presenting to the postanesthesia care unit were connected to a Pulse CO-Oximeter with acoustic monitoring technology (Rad-87, version 7804, Masimo, Irvine, CA) through an adhesive bioacoustic sensor (RAS-125, rev C) applied to the neck. Each subject also wore a nasal cannula connected to a bedside capnometer (Capnostream20, version 4.5, Oridion, Needham, MA). The acoustic monitor and capnometer were connected to a computer for continuous acoustic and expiratory carbon dioxide waveform recordings. Recordings were retrospectively analyzed by a trained technician in a setting that allowed for the simultaneous viewing of both waveforms while listening to the breathing sounds from the acoustic signal to determine inspiration and expiration reference markers within the ventilatory cycle without using the acoustic monitor- or capnometer-calculated ventilatory rate. This allowed the automatic calculation of a reference ventilatory rate for each device through a software program (TagEditor, Masimo). Accuracy (relative to the respective reference) and precision of each device were estimated and compared with each other. Sensitivity for detection of pauses in ventilation, defined as no inspiration or expiration activity in the reference ventilatory cycle for ≥30 seconds, was also determined. The devices were also evaluated for their reliability, i.e., the percentage of the time when each displayed a value and did not drop a measurement. RESULTS: Thirty-three adults (73% female) with age of 45 ± 14 years and weight 117 ± 42 kg were enrolled. A total of 3712 minutes of monitoring time (average 112 minutes per subject) were analyzed across the 2 devices, reference ventilatory rates ranged from 1.9 to 49.1 bpm. Acoustic monitoring showed significantly greater accuracy (P = 0.0056) and precision (P- = 0.0024) for respiratory rate as compared with capnometry. On average, both devices displayed data over 97% of the monitored time. The (0.95, 0.95) lower tolerance limits for the acoustic monitor and capnometer were 94% and 84%, respectively. Acoustic monitoring was marginally more sensitive (P = 0.0461) to pauses in ventilation (81% vs 62%) in 21 apneic events. CONCLUSIONS: In this study of a population of postsurgical patients, the acoustic monitor and capnometer both reliably monitored ventilatory rate. The acoustic monitor was statistically more accurate and more precise than the capnometer, but differences in performance were modest. It is not known whether the observed differences are clinically significant. The acoustic monitor was more sensitive to detecting pauses in ventilation. Acoustic monitoring may provide an effective and convenient means of monitoring ventilatory rate in postsurgical patients. (Anesth Analg 2013;117:69–75) From the *Department Of Anesthesiology and Pain Management, Baylor Research Institute, Baylor University Medical Center, Dallas, Texas; †Masimo Corporation, Irvine, California; ‡Baylor Research Institute and §Post Anesthesia Care Unit, Baylor University Medical Center; and ║Department of Quantitative Sciences, Baylor Health Care System, Dallas, Texas. Accepted for publication February 12, 2013. Funding: Masimo provided equipment and sensors for the study and funded the cost of research personnel who collected study data. Conflict of Interest: See Disclosures at the end of the article. Reprints will not be available from the authors. Address correspondence to Michael A. E. Ramsay, MD, Department Of Anesthesiology and Pain Management, Baylor University Medical Center, 3500 Gaston Ave., 2 Roberts, Dallas, Texas 75246. Address e-mail to docram@baylorhealth.edu. Copyright © 2013 International Anesthesia Research Society. DOI: 10.1213/ANE.0b013e318290c798 July 2013 • Volume 117 • Number 1 T here is an increasing realization in the health care community of the importance of continuous patient monitoring not only in the operating room but also in procedure areas, the postanesthesia care unit (PACU) and general care floor when patients are receiving sedative drugs and postoperative opioids, all which may depress breathing. The ability to detect and respond appropriately Institute for Healthcare Improvement. Rapid Response Teams. Available at: http://www.ihi.org/knowledge/Pages/Tools/HowtoGuideDeployRapidResponseTeams.aspx a b The Joint Commission. 2009 National Patient Safety Goals. Available at: http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals Anesthesia Patient Safety Foundation. Available at: http://www.apsf.org c d American Society of Anesthesiologists. Available at: http://www.asahq.org www.anesthesia-analgesia.org 69 Ventilatory Rate by Rainbow Acoustic Monitoring to the early indicators of physiological deterioration in a patient has become a major initiative for many nationally recognized health care organizations such as the Institute for Healthcare Improvement,a the Joint Commission,b the Anesthesia Patient Safety Foundation,c and the American Society of Anesthesiologists.d While early warning scoring systems along with the notification of rapid response teams are becoming widely implemented as a means of identifying and intervening early in patients at risk for an adverse event and readmission to the intensive care unit (ICU) or death, they cannot replace continuous monitoring. Changes in physiological variables such as ventilatory rate, oxygen saturation, exhaled carbon dioxide (CO2), and heart rate have been shown to be early indicators of a patient’s deteriorating condition.1–4 Earlier activation of the rapid response team may be possible if these variables could be monitored continuously and alarms transmitted to the caregiver.5 There is a need for a continuous monitor of ventilatory rate in spontaneously breathing patients at risk for ventilatory depression. This is particularly important in patients undergoing deep or moderate sedation and in patients at risk for ventilatory depression secondary to the administration of postoperative opioids. There is a significant risk of patient morbidity and mortality in the postoperative period due to ventilatory depression after administration of neuraxial opioids, intermittent parenteral injections of opioids, or IV patient-controlled analgesia (PCA), especially continuous infusions of opioids.6 Patients with obstructive sleep apnea (OSA), morbid obesity, or the elderly appear to be at higher risk for opioid-induced ventilatory depression.7,8 The Anesthesia Patient Safety Foundationc and the American Society of Anesthesiologistsd advocate the routine use of continuous postoperative ventilatory monitoring in at-risk patients receiving postoperative opioids including PCA or neuraxial opioids. Manual methods of determining ventilatory rate such as intermittent auscultation are time consuming, unreliable, and often poorly documented.9 Continuous methods of monitoring ventilatory rate such as capnometry have known limitations that can affect accuracy and patient tolerance.10 Capnometry measures the fractional CO2 in patient exhalations by infrared light absorption, mass spectrometry, and other methods. Side-stream capnometry, the method most commonly used in postoperative, nonventilated patients, uses a facemask or a nasal cannula for collection of exhaled gases, both of which may be bothersome to patients and can become dislodged. The nasal cannula has the further limitation of being inaccurate during mouth breathing, airway obstruction, or when oxygen is administered through the cannula.8,10,11 Additionally, variation from baseline of end-tidal carbon dioxide (EtCO2) is an important observation. Hypoventilation may cause the EtCO2 to decrease, because there is inadequate mixing of alveolar gas. Therefore, a low EtCO2 may be as important as a high EtCO2 when assessing for hypoventilation.12 There has been a great deal of interest in the development of a noninvasive bioacoustic sensor for ventilatory rate monitoring. Previous attempts to introduce the technology have been largely unsuccessful due to problems with ambient noise and motion artifacts. Recently, a method for the noninvasive measurement of ventilatory rate using 70 www.anesthesia-analgesia.org a contact piezoelectric sensor received Food and Drug Administration 510 (k) clearance and CE Mark and has become commercially available. The technology detects, amplifies, and processes the biological sounds and vibrations associated with ventilation through a disposable sensor placed on the neck. The purpose of this study was to determine the accuracy and reliability of this new bioacoustic sensor technology for the measurement of ventilatory rate and detection of cessation of breathing (pause in ventilation) in adult postsurgical patients when compared with side-stream capnometry, and with a reference standard. We are aware of 1 study that has systematically evaluated the use of continuous pulse oximetry monitoring in postsurgical patients on the general floor for its ability to affect clinical outcomes.13 This study used measure-through motion and low perfusion pulse oximetry (Masimo SET®, Masimo, Irvine, CA) to minimize false alarms and enhance detection of true alarms. In a cohort evaluated before and after the implementation of continuous pulse oximetry monitoring, there was a decrease in rescue events from 3.4 to 1.2 per 1000 patient discharges and ICU transfers from 5.6 to 2.9 per 1000 patient days. In contrast, 2 other cohorts without implementation of pulse oximetry showed no difference during the same time periods. While there was a dramatic decrease in rescue events and ICU transfers, it is possible that the addition of ventilatory rate monitoring could have provided an earlier notification of ventilatory depression, signaled by a decreasing ventilatory rate or pause in ventilation. Earlier notification might have allowed earlier or additional intervention in many of the at-risk subjects and further improved patient safety. Overdyk et al.14 demonstrated that continuous monitoring of postoperative patients with pulse oximetry and EtCO2 identified prolonged periods of hypoxia and apnea. Of a total of 178 patients studied, 12% had incidences of oxygen desaturation <90%, and 41% had periods of bradypnea <10 bpm for at least 3 minutes. One patient in the study had to be rescued with bag-mask ventilation. Abnormal ventilatory rate has been shown to be a common clinical feature in patients before a major clinical event such as cardiac arrest, onset of sepsis, and in patients experiencing shock, pain, asthma, sepsis, and respiratory infection.15,16 Despite the strong correlation between ventilatory rate changes and physiological deterioration, there is poor compliance in ventilatory rate charting.17 Because of this, ventilatory rate has been referred to as “the neglected vital sign.”18 This is probably because, unlike arterial blood pressure and heart rate, this variable is not usually recorded automatically. METHODS An observational study of adult patients presenting to the PACU of an academic tertiary care facility (Baylor University Medical Center, Dallas, TX) was conducted after IRB approval and obtaining written informed consent. On arrival in the PACU, a convenience sample of surgical patients was connected to a Pulse CO-Oximeter with Rainbow® acoustic monitoring (RAM) technology (Rad87, version 7804, Masimo) through an adhesive bioacoustic sensor (RAS-125, rev C) applied to the subject’s neck, lateral anesthesia & analgesia to the cricoid cartilage, following the manufacturer’s directions for use. Each subject was also fitted with a nasal cannula connected to a bedside capnometer (Smart Capnoline adult CO2 oral/nasal sampling set with Capnostream20, version 4.5, Oridion, Needham, MA). The oxygen flow rate through the cannula was 2 L/min. We chose to use nasal capnometry because that is what is typically used at our institution. The acoustic monitor and capnometer were connected to a computer with software (ADC, Masimo) for continuous waveform and parameter recording. The capnometer waveform data were collected at 20 Hz and the ventilatory rate at 1 Hz; the acoustic monitor outputs data at 2000 Hz and the ventilatory rate value at 0.5 Hz, so ventilatory rate data at 1 Hz were used for comparison. The ventilatory rate resolution for both monitors was 1 breath per minute, i.e., integer values. For the reference ventilatory rate, acoustic and EtCO2 waveform files were retrospectively analyzed by a trained technician using a specialized LabVIEW-based software program developed by Masimo (TagEditor, Masimo). LabVIEW allows simultaneous viewing of both waveforms while listening to the breathing sounds from the acoustic signal to manually determine and annotate inspiration and expiration reference markers within the ventilatory cycle independent of the acoustic monitor- or capnometer-calculated ventilatory rates. An additional technician was used to validate the reference markers, and if there was disagreement between technicians, a third technician was used to adjudicate. This was very rarely necessary as there were a small number of contentious events. Technicians were respiratory therapists or medical doctors trained to use the TagEditor program and contracted by Masimo. The reference ventilatory rate was then automatically calculated by the software program based on 30 seconds averaged period from the manual annotation of the data. The averaged ventilation period was calculated every 2 seconds using a sliding window and was equal to the mean period of all valid inspiration to inspiration and expiration to expiration periods for about the last 30 seconds, based on manual annotation. Figure 1 shows a screen shot of the TagEditor program patient file of the acoustic monitor and capnometry waveforms with manual markings during inspiration, expiration, and a respiratory pause. Ventilatory rates from the acoustic monitor and capnometer were compared with their respective reference methods at each time point, and absolute deviations (i.e., the absolute value of the difference from reference) in breaths per minute (bpm) were calculated. As a measure of accuracy, absolute deviations were calculated as a percent of reference. The process for calculation of accuracy is illustrated in Figure 2. Percent absolute deviations were averaged for each subject yielding overall measures of accuracy. For comparison of the accuracy of capnometry to that of RAM, the individual percent absolute deviations (RAM and capnometry) were compared for each monitoring time point (when both were present) by subtracting one from the other (capnometry minus RAM) and then averaged within subject. A 1-sample t test was used to evaluate significance across subjects. To measure the precision of each device for each subject, the standard deviation of percent deviations (in nonabsolute value) were calculated. The precisions of the 2 devices were compared through a paired t test of the subject-specific standard deviations of the 2 devices’ percent deviations from reference. The ability of both methods to detect ventilatory pauses was assessed. Ventilatory pause was defined as Figure 1. Screen shot of patient file as displayed by TagEditor program showing acoustic monitoring waveform (upper trace, 1) and capnometry (lower trace, 2) with manual markers for inspiration (A) and expiration (B). July 2013 • Volume 117 • Number 1 www.anesthesia-analgesia.org 71 Ventilatory Rate by Rainbow Acoustic Monitoring Figure 2. Calculation of accuracy for each device. RAM = Rainbow® acoustic monitoring; EtCO2 = end-tidal carbon dioxide. no inspiration or expiration activity in the ventilatory cycle measured by the reference method for ≥30 seconds. For the purposes of the study, a true positive (TP) was defined as no inspiration or expiration for ≥30 seconds by the reference method when the test method detected no inspiration and expiration during the same ≥30-second period. A false negative (FN) was defined as no inspiration or expiration for >15 seconds as determined by the reference method when the test method showed at least 1 inspiration or expiration during the same >15-second period. The sensitivity of each device was calculated as TP/(TP+FN) (%). This calculation was made across all the pauses for the 33 patients. Counts were recorded in a matched sample table and sensitivities compared with a Fisher exact test. These type of data do not lend themselves to an estimation of specificity, as distinct periods of no ventilatory pauses cannot be defined. Last, reliability of both devices was assessed by reviewing the number of time points each device displayed a value during the total monitoring time, and calculating a drop-out rate (percent of time points when the monitoring device failed to provide data) and lower bound tolerance intervals.19 RESULTS Thirty-three adults (73% female) with age of 45 ± 14 years and weight 117.4 ± 42.2 kg were enrolled. A total of 3712 minutes of monitoring time (average 112 minutes per subject) were analyzed. The range of monitoring time for patients was 20 to 259 minutes. Patient characteristics and surgical procedures are shown in Table 1. All patients were recovering from major surgery requiring PCA pumps, intermittent narcotics, or both. At least 35% of patients were diagnosed with OSA before enrollment, but this group of patients was 72 www.anesthesia-analgesia.org not analyzed separately. Ventilatory rate range by the reference method was 1.9 to 49.1 bpm for capnography and 4.0 to 41.5 bpm for RAM. On average, each of the devices displayed data over 97% of the monitored time (97.2% for capnometry and 98.4% for acoustic monitoring [P = 0.3750]). There were 2 patients for whom the capnometer was not reliably functioning, about 20% dropouts in one and 35% dropouts in the other. The largest drop-out rate for acoustic monitoring across the 33 patients was 8.5%. The (0.95, 0.95) lower tolerance limits for the acoustic monitor and capnometer were 94% and 84%, respectively. That is, with 95% confidence, 95% of acoustic monitor devices will return a ventilatory rate at least 94% of the time within a patient. Ninety-five percent of capnometers will return a rate at least 84% of the time within a patient. Tables 2 and 3 show the accuracy and precision estimates for both the capnometer and the RAM. On average, the capnometer deviated by 13% from its reference ventilation rate, whereas the RAM deviated by 10%. Table 4 shows the comparative analysis of accuracy and precision between the 2 devices. Larger values for the average columns reflect less accuracy and less precision. As the comparative analysis is based on the capnometer value minus the RAM value, then a positive value would indicate less accuracy/precision for the capnometer relative to the RAM, and a negative value would indicate less accuracy/precision for the RAM relative to the capnometer. The results show the RAM to be statistically more accurate (Fig. 3, P = 0.0056) and precise (Fig. 4, P = 0.0024). Table 5 illustrates the results of the sensitivities of the 2 devices to detect the 21 occurrences of respiratory pause that occurred across the 33 patients. Acoustic monitoring trended a higher sensitivity (P = 0.0461), 17 detected (81%) vs 13 detected (62%). Not all subjects had a ventilatory anesthesia & analgesia pause period of ≥30 seconds, and some subjects had several pauses in ventilation ≥30 seconds. DISCUSSION We present results of 33 PACU patients exhibiting a wide range of ventilation rates while being treated with intermittent narcotics, IV PCA pumps, or both. On average, the reliability of the 2 devices was high. The results suggest that Table 1. Patient Characteristics, Postoperative Analgesia, and Procedures 33 45 (±14) 24 (72) 118 ± 42 41 ± 13 112 ± 71 19.8–258.8 N Age (y) Female gender (%) Weight (kg) Body mass index Monitoring time (min) Range (min–max) Diagnosed obstructive sleep apnea Yes (%) No (%) Unknown (%) Postsurgical analgesia Prescribed PCA (%) Prescribed narcotics PRN Yes (%) No (%) Unknown (%) Procedures Laparoscopic gastric bypass Laparoscopic gastric sleeve Laparoscopic cholecystectomy Herniorraphy Cystoscopy and ureteroscopy Other 12 (40) 18 (60) 3 15 (45) 30 (97) 1 (3) 2 11 (33) 5 (15) 5 (15) 2 (6) 2 (6) 8 (24) Data are mean (±SD) or number (%). PCA = patient-controlled analgesia; PRN = as needed. the capnometer is about 3% less precise than the RAM (95% confidence interval, 0.9%–4.8%). The study did not address whether the better accuracy and precision of RAM was clinically significant. An important issue in the monitoring of ventilation of such patients is the ability to detect pauses in ventilation. Twentyone such events occurred among the 33 patients followed. Acoustic monitoring showed a statistically higher sensitivity for detecting these events (81% vs 62% for capnometry). Specificity was not assessed, because the nature of the monitoring (measured every 2 seconds) and the definition of a pause in ventilation (no breathing for 30 seconds) precluded counting true negatives (needed for estimating specificity). There are several limitations to our study. First, although both capnometry and acoustic monitoring provided data during the vast majority of the monitoring time (drop-out rates for both methods was <2%), we did not document and analyze the factors associated with the loss of data. We also did not analyze the main causes of inaccurate readings that are likely to be different for capnometry and acoustic monitoring. Perhaps the most important limitation to the study is that we could only evaluate 21 respiratory pause events, and the analyses involved the assumption that these were independent events. Larger studies may increase the understanding of factors associated with data loss, inaccurate readings, and false alarms. For example, observation of what specific patient events (e.g., coughing, speaking, snoring) result in inaccurate readings, or data loss could lead to a better understanding of the performance and limitations of acoustic monitoring. We tested acoustic monitoring in the PACU only, and since this technology is acoustic-based, it may perform differently in care areas with higher or different types of ambient noise. Ventilatory rate is an important vital sign. Current methods of continuous monitoring have significant drawbacks. Table 2. Summary Estimates of Accuracy for Ventilatory Rate (Relative to the Respective Reference) Across 33 Patients Accuracy measure |capnometer–reference|/reference |RAM–reference|/reference Average of patient averages 0.13 0.10 SD of patient averages 0.09 0.09 95% CI (N = 33) 0.10–0.16 0.07–0.13 CI = confidence interval; RAM = Rainbow acoustic monitoring Table 3. Summary Estimates of Precision for Ventilatory Rate (Relative to the Respective Reference) Across 33 Patients Precision measure SD ([capnometer–reference]/reference) SD ([RAM–reference]/reference) Average SD of percent bias 0.21 0.16 SD of SD of percent bias 0.14 0.12 95% CI (N = 33) 0.16–0.26 0.12–0.20 CI = confidence interval; RAM = Rainbow acoustic monitoring. Table 4. Accuracy and Precision Comparisons Between Capnometry and Acoustic Monitoring Measure Accuracy Precision Capnometer percent absolute deviation–RAM percent absolute deviation SD(capnometer percent bias)–SD(RAM percent bias) Average of patient average differences 0.028 SD of patient average differences 0.055 95% CI P 0.009–0.048 0.0056 0.050 0.088 0.019–0.081 0.0024 CI = confidence interval; RAM = Rainbow acoustic monitoring. July 2013 • Volume 117 • Number 1 www.anesthesia-analgesia.org 73 Ventilatory Rate by Rainbow Acoustic Monitoring Figure 3. Pairwise comparison of accuracy for each of 33 patients. RAM = Rainbow® acoustic monitoring. correlates well with capnometry. This confirms an analysis by Mimoz et al.22 The addition of a combination of continuous oxygenation monitoring with pulse oximetry and continuous ventilatory rate monitoring may provide a safety net for postsurgical patients receiving opioids. Therefore, a welltolerated patient monitoring technology that accurately, automatically, and continuously tracks ventilatory rate has the potential to greatly improve the timeliness of response to a failing patient and improve patient safety and outcomes. CONCLUSION Figure 4. Pairwise comparison of precision for each of 33 patients. RAM = Rainbow® acoustic monitoring. The data from this study demonstrate that acoustic monitoring provides a very reliable noninvasive, continuous method for estimating ventilatory rate in postsurgical patients at risk for ventilatory compromise. Relative to capnometry, it demonstrated greater accuracy, precision, and sensitivity to pauses in ventilation. The clinical significance of this will need to be determined by a larger study. In addition, the utility of these findings in patients with OSA should be prospectively assessed. Acoustic monitoring may provide a reliable means for tracking ventilation status in patients at risk for ventilatory depression. E DISCLOSURES Table 5. Matched Sample Data for Comparison of Sensitivities for Detection of 21 Respiratory Pauses Across 33 Patients (P = 0.0461) RAM Positive Negative Positive 11 2 13 Capnometry Negative 6 2 8 17 4 21 RAM = Rainbow acoustic monitoring They are either not accurate or are not well tolerated by patients.20,21 The development of an acoustic transducer that can be integrated into an adhesive patch that is applied to the patient’s neck may offer a good alternative for monitoring respiratory rate continuously. This study demonstrates that this technology monitors respiratory rate that 74 www.anesthesia-analgesia.org Name: Michael A. E. Ramsay, MD. Contribution: This author helped design and conduct the study, has seen the original study data, reviewed the analysis of the data and helped write the manuscript. Affiliation: Michael A. E. Ramsay approved the final manuscript. He attests to the integrity of the original data and the analysis reported in this manuscript. Michael A. E. Ramsay is the archival author. Conflict of Interest: This author receives research funds from Masimo Corporation and is a Speaker Board member and Advisory Board member for Masimo Corporation. Name: Mohammad Usman, PhD. Contribution: This author helped design the study, analyze the data, and write the manuscript. Affiliation: Mohammad Usman approved the final manuscript. Conflict of Interest: This author is an employee of Masimo Corporation. anesthesia & analgesia Name: Elaine Lagow, RN. Contribution: This author helped conduct the study and approved the final manuscript. Conflict of Interest: This author is funded in part from research funds from Masimo Corporation. Name: Minerva Mendoza, RN. Contribution: This author helped conduct the study and approved the final manuscript. Conflict of Interest: The author has no conflicts of interest to declare. Name: Emylene Untalan, RN. Contribution: This author helped conduct the study and approved the final manuscript. Conflict of Interest: The author has no conflicts of interest to declare. Name: Edward De Vol, PhD. Contribution: This author completed the review and revision of the statistical analysis. He approved the final manuscript. This author also attests to the integrity of the original data, having reviewed the original data and the analysis reported in this manuscript. Conflict of Interest: The author has no conflicts of interest to declare. This manuscript was handled by: Steven L. Shafer, MD. REFERENCES 1.Hagle ME, Lehr VT, Brubakken K, Shippee A. Respiratory depression in adult patients with intravenous patient-controlled analgesia. Orthop Nurs 2004;23:18–27 2.Hammond NE, Spooner AJ, Barnett AG, Corley A, Brown P, Fraser JF. The effect of implementing a modified early warning scoring (MEWS) system on the adequacy of vital sign documentation. Aust Crit Care 2013;26:18–22 3. Churpek MM, Yuen TC, Huber MT, Park SY, Hall JB, Edelson DP. Predicting cardia carrest on the wards. Chest 2012;141:1170–6 4. Cuthbertson BH, Boroujerdi M, McKie L, Aucott L, Prescott G. Can physiological variables and early warning scoring systems allow early recognition of the deteriorating surgical patient? Crit Care Med 2007;35:402–9 5.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA 2008;300:2506–13 6. George JA, Lin EE, Hanna MN, Murphy JD, Kumar K, Ko PS, Wu CL. The effect of intravenous opioid patient-controlled analgesia with and without background infusion on respiratory depression: a meta-analysis. J Opioid Manag 2010;6:47–54 7. Kasuya Y, Akça O, Sessler DI, Ozaki M, Komatsu R. Accuracy of postoperative end-tidal Pco2 measurements with mainstream July 2013 • Volume 117 • Number 1 and sidestream capnography in non-obese patients and in obese patients with and without obstructive sleep apnea. Anesthesiology 2009;111:609–15 8. Maddox RR, Williams CK, Oglesby H, Butler B, Colclasure B. Clinical experience with patient-controlled analgesia using continuous respiratory monitoring and a smart infusion system. Am J Health Syst Pharm 2006;63:157–64 9.Hogan J. Why don’t nurses monitor the respiratory rates of patients? Br J Nurs 2006;15:489–92 10. Friesen RH, Alswang M. End-tidal PCO2 monitoring via nasal cannulae in pediatric patients: accuracy and sources of error. J Clin Monit 1996;12:155–9 11. Gaucher A, Frasca D, Mimoz O, Deboene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask in intubated patients receiving supplemental oxygen after surgery. Br. J. Anaesth 2012;108:316–20 12 Godwin SA, Caro DA, Wolf SJ, Jagoda AS, Charles R, Marett BE, Moore J; American College of Emergency Physicians. Clinical policy: procedural sedation and analgesia in the emergency department. Ann Emerg Med 2005;45:177–96 13. Taenzer AH, Pyke JB, McGrath SP, Blike GT. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology 2010;112:282–7 14.Overdyk FJ, Carter R, Maddox RR, Callura J, Herrin AE, Henriquez C. Continuous oximetry/capnometry monitoring reveals frequent desaturation and bradypnea during patientcontrolled analgesia. Anesth Analg 2007;105:412–8 15. Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest 1990;98:1388–92 16. Mailey J, Digiovine B, Baillod D, Gnam G, Jordan J, Rubinfeld I. Reducing hospital standardized mortality rate with early interventions. J Trauma Nurs 2006;13:178–82 17.McBride J, Knight D, Piper J, Smith GB. Long-term effect of introducing an early warning score on respiratory rate charting on general wards. Resuscitation 2005;65:41–4 18. Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust 2008;188:657–9 19.Beyer WH, ed. Handbook of Tables for Probability and Statistics. Cleveland, OH: Chemical Rubber Company, 1966:362 20.Wilkinson JN, Thanawala VU. Thoracic impedance monitoring of respiratory rate during sedation–is it safe? Anaesthesia 2009;64:455–6 21. Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask® in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth 2012;108:316–20 22. Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth 2012;108: 872–5 www.anesthesia-analgesia.org 75