LegisLation and standards
advertisement
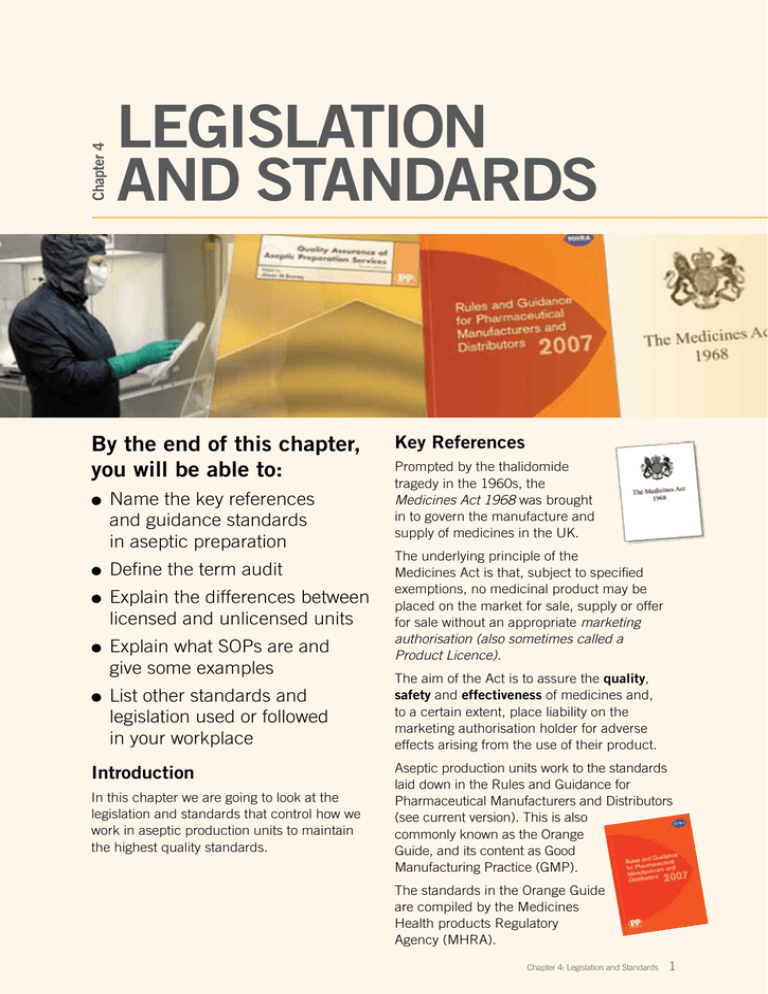
Chapter 4 Legislation and Standards By the end of this chapter, you will be able to: l l l l l Name the key references and guidance standards in aseptic preparation Define the term audit Explain the differences between licensed and unlicensed units Explain what SOPs are and give some examples List other standards and legislation used or followed in your workplace Introduction In this chapter we are going to look at the legislation and standards that control how we work in aseptic production units to maintain the highest quality standards. Key References Prompted by the thalidomide tragedy in the 1960s, the Medicines Act 1968 was brought in to govern the manufacture and supply of medicines in the UK. The underlying principle of the Medicines Act is that, subject to specified exemptions, no medicinal product may be placed on the market for sale, supply or offer for sale without an appropriate marketing authorisation (also sometimes called a Product Licence). The aim of the Act is to assure the quality, safety and effectiveness of medicines and, to a certain extent, place liability on the marketing authorisation holder for adverse effects arising from the use of their product. Aseptic production units work to the standards laid down in the Rules and Guidance for Pharmaceutical Manufacturers and Distributors (see current version). This is also commonly known as the Orange Guide, and its content as Good Manufacturing Practice (GMP). The standards in the Orange Guide are compiled by the Medicines Health products Regulatory Agency (MHRA). Chapter 4: Legislation and Standards 1 Aseptic Processing Edited by Alison Beaney on behalf of the NHS Pharmaceutical Quality Assurance Committee, Quality Assurance of Aseptic Preparation Services (Yellow Guide) gives guidance on all aspects of the principles of Good Manufacturing Practice (GMP). All aseptic preparation units work to the standards set out in Aseptic dispensing for NHS Patients (Farwell Report). This was produced in 1995 by John Farwell and provides guidance to NHS aseptic units on standards of aseptic preparation. Farwell (1995) sets out specific policies for aseptic activity and highlights the need for a quality system. These are observed in all units and should include: l Comprehensive quality assurance with independent approval l Reference to other legislative requirements, where necessary, eg, COSHH, Ionising Radiation Regulations, etc Licensed Units Some hospital manufacturing units hold a Specials Licence granted by the MHRA. This allows the unit to manufacture pharmaceutical products without a product licence or marketing authorisation that are required by industry. Licensed units can: l manufacture products and sell to external customers; l assign extended expiry dates to products, provided they are supported by stability data. Unlicensed Units l Detailed, approved operational procedures to cover all facets of the activity l Defined responsibilities, competencies, training and performance of staff involved in the activity l Control of all materials, including containers, devices and packaging, used in the processes. l preparation is done by or under the supervision of a pharmacist who takes full responsibility for the quality of the product; l Appropriate provision and use of special clothing (for operator and product protection) l the preparation uses closed systems (i.e. not open to the atmosphere) l Provision, maintenance and correct performance of facilities and equipment, including disposables, for the whole range of activities carried out l licensed sterile medicinal products are used as ingredients or the ingredients are manufactured sterile in licensed facilities; l l Consistent approach to product presentation including labelling products will be allocated a shelf life of no more than one week and the shelf life should be supported by stability data l Full documentation of systems and processes and other product-related issues, e.g., customer complaints l all activities should be in accordance with defined NHS guidelines. l Validation of all procedures 2 Chapter 4: Legislation and Standards Aseptic preparation units can operate under an exemption from Section 10 of the Medicines Act, when dispensing directly to named patients. i.e. without a specials licence, providing the following conditions are met: Chapter 4 Legislation and Standards Some differences between aseptic preparations under Section 10 Exemption, compared to specials manufacturing licence Section 10 Exemption Specials Manufacturing Licence Maximum 7-day expiry Expiry limited to stability evidence Prepared or directly supervised by Pharmacist Prepared by suitably trained person following approved procedures Must only be prepared against a legal prescription Can be prepared for stock Final check and release may be done together Final check and release MUST be done by separate people Release may be done by any locally approved Pharmacist Release may only be done by person registered by MHRA, e.g. Pharmacist or Qualified Person (QP) Standards must comply with local and QA regional audit Standards must comply with MHRA inspection which is much more stringent Audits Audits are a process of checks, carried out to ensure that Good Manufacturing Practice standards, such as those laid down in the Orange Guide (see current version), Farwell(1995) and PICS (2008) are upheld. Licensed units are subject to inspection by MHRA GMP inspectors every 2 years. All units, both licensed and unlicensed, must carry out regular internal and external audits. l l Internal audits should be carried out by staff who are part of the management organisational structure of the department. Audits may be carried out internally according to an audit calendar with action taken to rectify any non-conformances as required. External audits should be carried out by staff who are not managerially accountable and are independent of any service provision to the unit. External audits should be carried out at a suitable frequency, at least every 18 months, as required by EL(97)52. For Self Inspection, a self audit programme should be established that monitors the implementation and compliance with the written guidelines for quality assurance and good manufacturing practice, and that considers the type and complexity of operations performed, which includes: l an annual self audit plan with records; l evidence that adequate corrective actions are undertaken. Self audits should be conducted in an independent and detailed way by designated competent people. Records of all auditing should be made, with action plans compiled, completed and re-assessed. Chapter 4: Legislation and Standards 3 Aseptic Processing Standard Operating Procedures (SOPs) l Product sampling and testing l Process validation These are instructions and information on how to carry out a wide range of operations in your unit. SOPs are devised to ensure uniformity in all processes and that the best way of carrying out a task is determined and reproduced consistently. SOPs should cover all areas within the preparation process. l Operation of the Unit l Staff training and testing l Request processing l Action to be taken in case of system failure l Controlled drugs l Storage and distribution of products l Spillage l Product complaints and recalls l Assembly and transfer of ingredients l Laundry These instructions should be followed at all times with no deviation (unless under exceptional circumstances where the deviation is approved by a supervisor, has been evaluated and documented and is known to be safe and does not affect the quality of the product in any way). No operator should rely on word of mouth to transfer information and there should be no individual interpretation of information. If there is doubt about a procedure or policy, the line manager should be contacted and an explanation given. Some examples are: Other General Legislation & Standards Health and Safety at Work Act The Health and Safety at Work Act 1974 identifies the Health and Safety responsibilities of both the employer and the employees. Take care of your own safety and that of others who may be affected by what you do – your acts or omissions. l Management of procedures l Error recording l Cleaning and disinfecting l Fridge validation l Test failure The purpose of the Health and Safety at Work Act etc is to provide the legal framework to promote, stimulate and encourage high standards of health and safety at work. l Unusual event recording Further Reading l Maintenance and repairs l COSHH and Health & Safety l Capacity and planning l Entry and exit from facilities You should read your department Health and Safety procedures and be aware of risks to yourself and others. Some considerations are given below: l Documentation l Environmental monitoring l Labels and labelling l Use of equipment l Waste l Product preparation checks and release 4 Chapter 4: Legislation and Standards Control of Substances Hazardous to Health (COSHH) Using chemicals or other hazardous substances at work can put people’s health at risk, so the law requires employers to control exposure to hazardous substances to prevent ill health. Employers have to protect people Chapter 4 Legislation and Standards who may be exposed, by complying with the Control of Substances Hazardous to Health Regulations 1999 (COSHH). ✔ Know which is the right type of extinguisher to use. ✔ Know where the fire exits are. All places of work must be assessed to establish the risks. You should refer to your own local risk assessments and SOPs. ✔ Know where the fire alarm manual pushes are in your area. ✔ Know the sound of the fire alarm. Where possible, risks to health must be reduced by use of alternative substances or by the use of protective equipment. DON’T COSHH Data Sheets will be available for each substance. These give details such as: l Product Information l Emergency and First Aid Procedures l Health Hazard Information l Effects of Exposure l Handling and Storage ✗ Obstruct access to fire exits. ✗ Store items on top of fire extinguishers. ✗ Lock fire doors. ✗ Get changed from your cleanroom clothes on exit – get out as soon as possible IN THE EVENT OF A FIRE: l Stop what you are doing. Leave it safe. l Start to exit. l Check adjacent rooms for other staff as you exit. l Do NOT get changed. l Do NOT collect personal belongings. l Leave unit by nearest appropriate exit. (Do not use a ‘kick-panel’ if main exit is clear) l Exit the Pharmacy by the most appropriate exit. Manual Handling You should observe your organisations procedures for lifting and handling, and should receive appropriate training – follow your SOPs. In production areas, special care should be taken to check workstations and operator positioning to reduce risks l Check the positioning of your chair before you start work l Report to the senior member of staff for roll-call AND report the unit clear. l Avoid overstretching and twisting l l Take a break from repetitive movements at reasonable intervals to avoid strain DO NOT re-enter until advised by senior member of staff. Dealing with a Product Spillage Fire Safety Make sure you know what to do before you find yourself confronted by a fire. DO ✔ Know your fire instructions. ✔ Know where the fire extinguishers are in your area, how to use the fire extinguishers/ organisations policy on their use See Individual Product Data for Dealing with Spillages. You should: l Minimise the number of people in the area l Restrict access to the area l For cytotoxics use a designated spill kit l Be aware of your spillage SOP Chapter 4: Legislation and Standards 5 Aseptic Processing Reporting of Accidents/incidents For needle stick injuries *Report all accidents/incidents immediately* Individuals are expected to have a duty of care when handling sharps, however injuries may occur. Incidents should be reported on an accident form. These may be assessed by a senior person and action taken as necessary, in accordance with departmental procedures. All accidents/incidents in the work place should be reported to a senior member of staff and an incident form completed immediately, detailing the incident and action taken. First Aid For accidental exposure to drug/cleaning agent see relevant COSHH data sheet. Task There should be a copy of the Yellow Guide (Quality Assurance of Aseptic Preparation Services) available in your unit. Read through Section 16 Internal and External Audits. Make a note below of any additional points about audits that are relevant to your unit and you should be aware of: 6 Chapter 4: Legislation and Standards Chapter 4 Legislation and Standards Test Yourself Write down as many examples of SOPs as you can remember (up to a maximum of 10). Put a tick next to any that you have already followed/used or read in your day-to-day work. Chapter 4: Legislation and Standards 7 Aseptic Processing Questions Q1 How often should licensed units be inspected by MHRA inspectors? (1) Q2 Who should carry out external audits? (2) Q3 What type of audits must be carried out by unlicensed units? (2) 8 Chapter 4: Legislation and Standards Chapter 4 Legislation and Standards Q4 The following publications lay down the standards followed by all aseptic production units. What names are commonly used to refer to them, and what is the purpose of each publication? Official name Common name Purpose Aseptic dispensing for NHS Patients Rules and Guidance for Pharmaceutical Manufacturers and Distributors Quality Assurance of Aseptic Preparation Services (6) Chapter 4: Legislation and Standards 9 Aseptic Processing Q5 What does COSHH stand for? List 5 details that can be found on a COSHH datasheet 1. 2. 3. 4. 5. (6) 10 Chapter 4: Legislation and Standards