Making a decision about living organ and tissue
advertisement

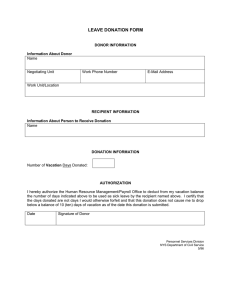
MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION W O R K I N G T O B U I L D A H E A L T H Y A U S T R A L I A MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION Endorsed 15th March 2007 This booklet is derived from Living Organ and Tissue Donation: Guidelines for Ethical Practice for Health Professionals, which was developed by the National Health and Medical Research Council in 2006. The booklet aims to help people think through some ethical issues and make decisions about living organ and tissue donation. If you are thinking of making a living donation, the doctors caring for you can give you more information that is relevant to your situation. © Australian Government 2007 Paper-based publication This work is copyright. Apart from any use permitted under the Copyright Act 1968, no part may be reproduced by any process without written permission from the Commonwealth available from the Attorney-General’s Department. Requests and inquiries concerning reproduction and rights should be addressed to the Commonwealth Copyright Administration, Attorney-General’s Department, Robert Garran Offices, National Circuit, Canberra, ACT, 2600 or posted at: http://www.ag.gov.au/cca ISBN Print: 1864963174 © Australian Government 2007 Electronic documents This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use, or use within your organisation. Apart from any use as permitted under the Copyright Act 1968, all other rights are reserved. Requests for further authorisation should be directed to the Commonwealth Copyright Administration, Attorney-General’s Department, Robert Garran Offices, National Circuit, Canberra, ACT, 2600 or posted at: http://www.ag.gov.au/cca Online: 1864963239 To obtain information regarding NHMRC publications contact: Email: nhmrc.publications@nhmrc.gov.au Phone: Toll free 13 000 NHMRC (13 000 64672) or call 02 6217 9000 Internet: http://www.nhmrc.gov.au Contents Contents 1Living organ and tissue donation — an overview 1 2 The ethics of living donation 4 Principles of ethical living donation 5 Emerging ethical concerns 6 3What is the process of donation? 7 How are donors assessed? 7 Decision-making — balancing the needs of everyone involved 9 Deciding on behalf of a child or dependent adult 10 Continuing care of donors 11 4different decisions about living donation 14 5 15 Before you decide MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION iii Living organ and tissue donation — an overview 1Living organ and tissue donation — an overview The NHMRC has developed this booklet to help people to think through the ethical issues and make decisions about living donation of organs and tissues. Why are organs and tissues needed? Transplants of organs (heart, lung, liver, kidney, pancreas) and tissues (bone marrow, corneas, heart valves, skin, bone) can save lives and improve health. Transplant operations have been taking place in Australia for decades. Many people are living longer and enjoying better quality of life as a result. As medical advances continue, the need for transplants keeps growing. Most transplanted organs and tissues come from people who have died but there are not as many organs available to be transplanted as there are people who need them. Living donation is an option for some patients who are on the waiting list for an organ or tissue from a donor who has died. Donation of certain organs and tissues by living donors is well-established in Australia. This booklet discusses the main ethical issues involved in living donation. It focuses on the types of living donation currently being carried out in Australia. This includes whole organs (eg kidneys), parts of organs (eg parts of the liver) and tissues (eg bone marrow). The NHMRC has also developed a booklet about the main ethical issues involved in deceased organ donation. How is living donation possible? Living donation is only possible if the person who donates (the donor) can still live healthily without that organ or tissue. Many types of living donation are of regenerative tissue. This type of tissue grows back naturally after some of it is removed. Bone marrow is a commonly donated tissue of this type. Blood is also regenerative, but is not discussed in this booklet as blood donation does not involve an operation. Non-regenerative tissue does not grow back again once it is removed. Kidney donation is the most common form of this type of donation. Most people have two kidneys. If one is donated, the remaining one (as long as it is healthy) can carry out the normal functions of both kidneys. It is also possible to transplant a part of the liver. This is because the liver is able to do the extra work necessary so that both the donor and the person who has had the transplant (the recipient) can be healthy. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION Living organ and tissue donation — an overview Different types of donation Currently in Australia, more than one-third of kidney donations are from living donors. The rest are from people who have died. Most living organ donors are relatives of the person receiving the transplant (eg a parent, brother or sister). Recent advances in medicine have also made it possible for people who are not related to the person who needs a transplant (eg a spouse, partner or friend) to make a donation. Living donation by a relative or friend is called directed donation. Living donation can also be non-directed. Donations of bone marrow by volunteers are a common form of this type of donation. Non-directed kidney donation is a new practice worldwide. It is still rare in Australia and is only possible at some Australian hospitals. In these cases, a person decides to donate a kidney to help whoever is on the waiting list. The donor has no say in who will or will not receive the kidney. Care is taken to protect the privacy of this type of donor. Living donation is a good option for most patients who need a kidney transplant. A living donation keeps the person off the waiting list and is likely to work better and last longer than a kidney from a dead donor. Who can be a living donor? To be a living donor, a person must be in good physical and mental health. They also need to be free from diseases that may affect the health of the person who receives the transplant. Living donors are usually aged between 18 and 60 years old. In some cases, children may donate regenerative tissue, such as bone marrow, to a close relative. The donor and recipient usually have matching blood groups and tissue types. A test using the donor’s blood can also show whether the recipient’s immune system is likely to reject the transplant. New techniques and drugs have made it possible to transplant non-matched organs and tissues. This process is more complex. The person receiving the transplant is more likely to have health problems than they would after a matched transplant. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION Living organ and tissue donation — an overview How does living donation affect donors? The effect that donation has on the donor depends on which organ or tissue they donate. In Australia, kidney or bone marrow donation are the most common forms of living donation. This may change as medical advances increase the types of donation possible. Bone marrow — A bone marrow transplant is most likely to succeed if bone marrow from a relative is used. But sometimes no match can be found in the family. Bone marrow registers help people to find a match from an unrelated volunteer. The risks from donating bone marrow are the same as those with any general anaesthetic. The chance of a serious complication is very low. After the bone marrow is removed, donors can return to normal activity, including work, within days. Kidney — The operation to remove a kidney lasts about three hours. Donors usually spend another four or five days in hospital. There can be complications from the operation but donors usually return to their normal routine, including work, within six to eight weeks. Kidney donation is not likely to cause health problems unless the remaining kidney is injured or becomes diseased in the future. Liver — In living liver donation, a part of the liver is removed from the donor. A smaller part of the liver is taken if the transplant is for a child. The operation to remove the part of the liver usually lasts five to eight hours. The donor usually then spends another seven days in hospital. There is some risk of complications from the operation. Donors usually return to all normal activities within three to six months. “My brother told me that he had kidney failure at the end of last year. I’m not certain he even asked me to donate. I just knew that I would help if I could. My wife and children completely supported my decision.This was really important to the whole process because inevitably everyone becomes involved.” Lung — Living lung donation is a complex process that has not yet been performed in Australia but has been carried out overseas. It requires two donors. One donor gives a part of the left lung. The other donor gives a part of the right lung. The two segments of lung are transplanted into a single recipient at the same time. As the lungs do not grow back, the donors lose some of their lung function. This would not normally be noticed by the donor. Other organs — Some other types of living donations have been undertaken overseas. These include a part of the intestine or the pancreas. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION The ethics of living donation 2 The ethics of living donation Each type of living donation involves asking ethical questions. This is because the treatment affects not only the people in need of transplants but also the healthy individuals who volunteer to donate. Living donors have operations that do not benefit them and may even cause them harm. What are ethics? Ethics are about your personal beliefs, and about the way we think and behave as a community. Ethics are about the rules of behaviour and human duty, morals and values — that is, understanding right and wrong, justice and injustice, good and bad, and doing the right thing. Before living donation can go ahead, the person who wishes to donate must understand that the donation may affect their physical health and their mental wellbeing. The chances of there being problems after donation will depend on the type of donation. For example, the chances of problems after bone marrow donation are quite small. Kidney or liver donation involve a more serious operation so it is more likely that there could be problems afterwards. The bigger the risk of harm to the donor, the greater the ethical concern. There are important ethical standards that must be met before living donation can go ahead: • donors must understand and accept the risk to themselves; • t here must be a very low chance of harm to the donor’s physical or mental health, straight away or in the future; and • t here must be a very high chance that the transplant will be successful. “After we learnt that Glenn’s liver was failing, I think it was hardest for Margaret. She was the only member of the family who was a matched donor.We tried to help her come to a decision. In the end the final choice had to be hers.The counsellor helped Margaret to accept that it was okay to say no as she was scared of the operation and what might happen to her.We were lucky that a liver from a dead donor became available.” Overall, the wellbeing of the donor must be considered above the health of the person who needs the transplant. Living donation by children and adults who cannot make their own decisions is even more difficult. This is because: • c hildren and dependent adults are very vulnerable and must be protected; • it may be difficult to make sure they understand what is involved; and • p arents or guardians may be in the situation where they are making decisions for the donor and the recipient. Because of these difficulties, an independent team needs to decide whether the donation would be in the child or dependent adult’s best interests. Deciding on behalf of children and dependent adults is discussed in Section 3. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION The ethics of living donation Principles of ethical living donation People must be in good physical and mental health before they can become living donors. There are some important principles that must be followed as well, to make sure that every living donation is ethically acceptable. Living donation must be altruistic Altruism means that the donor is thinking only about the other person and is not expecting to receive rewards. The decision to donate must be free and voluntary People should not be forced or influenced by emotional pressures or promises of rewards like money. It is illegal in Australia to provide an organ in exchange for money. Because it might be seen as an incentive, there can be no reimbursement to living donors for loss of wages or other expenses. Both donors and recipients must be fully informed Donors and recipients need clear information so that they can understand what the risks are and what might happen in the future. Everyone involved in the decision-making process must be treated with respect and care Whether a donation goes ahead or not, the donor assessment and transplant teams follow the ethical principles outlined in this booklet and work towards the best possible results for the donor and recipient. Cultural issues must be considered in planning programs and working with families Translators are important to give information to people whose first language is not English. The health professionals involved need to understand and be sensitive to the ways in which culture and beliefs can influence decisions about donation. “Although we tried to explain, Kassiani did not really understand what was being asked of her or what would happen. The hospital helped us by getting an interpreter. They even found some brochures about kidney donation that were written in Greek. In the end, she decided not to donate but we felt better knowing that she had been given all the information she needed to make her own decision. ” MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION The ethics of living donation Emerging ethical concerns The ethical and legal implications of newer practices in living donation are still being thought through. These emerging issues need to be considered and discussed within the community. PAIRED DONATION Recipient Pair 2 Pair 1 Donor The growing demand for organs and tissues means that waiting lists are getting longer. The wait for an organ can be long and sometimes life-threatening for someone without a friend or relative who can make a donation. A number of new practices have developed overseas to help people without suitable living donors. aired donation aims to help people go through with living • P donation even when the kidney donor and potential recipient are not matched. The unmatched pair is combined with another unmatched pair. The two pairs ‘exchange’ organs (see diagram) and both avoid the waiting list. Paired donation currently takes place in the US and the Netherlands. In Australia, this type of donation is only legal in WA. • L ist exchange acts as an organ ‘matching’ service. A donor who does not have a match with his or her intended recipient offers to donate to a stranger on the waiting list. In return, the intended recipient is given priority for an organ from a deceased donor. This practice does not currently occur in Australia. There are ethically unacceptable practices that provide other sources of organs. These include internet sites that match donors and recipients for a profit, appeals by organisations (eg community groups) on behalf of recipients, and potential recipients advertising for organs through the media (eg placing advertisements, generating news stories). These practices are unethical because: • t hey favour people who have access to a particular media or group; • they may involve costs; and • they do not take account of who needs the organ most. There are also organ ‘black markets’, where people in developing countries sell their organs to foreigners who want to bypass the waiting list in their own country. This takes advantage of donors, many of whom are poor and helpless. Because there may not be a full assessment before donation, it can lead to serious health problems for both donors and recipients (eg the person receiving the transplant becoming infected with a disease from the donor). MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION What is the process of donation? 3What is the process of donation? Special care is taken to make sure that the process of organ and tissue donation meets strict ethical and legal requirements. This chapter discusses the process of living organ and tissue donation, including who is involved and what happens afterwards. How are donors assessed? The assessment for living donation depends on the organ or tissue to be donated. For bone marrow donation, tests are done to check for medical suitability and matching with the recipient. Possible donors are told about the bone marrow donation process. Then they have a medical examination and counselling session. After these steps, the person makes the decision, usually with the support of friends and family, about whether to become a bone marrow donor or not. For living kidney or liver donation, the assessment and consent process is much more complex. It may take three to nine months and involves: The donor’s transplant team The transplant team is made up of many people who work together to support and educate the donor and his or her family. These include: • specialist physician • b lood and tissue testing to see whether the donor and recipient are matched; • surgeon • assessment of the potential donor’s mental health; •psychiatrist or psychologist • transplant coordinator • social assessment; and • nursing staff • m any stages of medical assessment, including further tests for matching. • social worker Assessment is a two-way process. It is a chance for health professionals to make sure that the person is suitable to donate. It also gives the person a chance to learn as much as possible about donation before making a decision. Donors are given detailed information about possible physical or mental health problems after the donation. • pharmacist • dietitian • physiotherapist • pain team. Each donor has at least one private session with a specialist doctor. The specialist, or another doctor such as the patient’s GP, acts as an advocate, or supporter, for the donor and can help them with making their decision. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION What is the process of donation? If the health professionals agree that the donor is suitable, he or she is asked to give consent. People who are thinking about being donors can change their minds at any time. Tests may show that donation is likely to make the person ill or cause too much stress, or the donor may realise that they cannot afford the time off work. If donation does not go ahead, the person’s reasons are kept completely private. Whether donation is urgent or not, donors have the right to: •medical information about the donation and its short and long-term risks •information about the likely benefits to the recipient •independent medical advice •counselling to discuss the possible mental health and social consequences of the decision to donate •as much time as possible to make the decision Donors also have the right to decide not to donate, or to change their minds about donating. Their reasons will be kept private. Mental health assessment The mental health assessment helps health professionals to make sure that every living donor is making a free and informed decision and that the donation is unlikely to have a harmful effect on his or her mental health. In directed donation, it is important to assess whether potential donors: • a re under emotional pressure (eg a young woman’s parents begging her to donate a kidney to a sick brother or sister); or • f eel obliged to donate, even if it involves risks to themselves (eg a father with very high blood pressure donating a kidney to try to save the life of his child). In non-directed donation, the person’s reason for donating is usually a true wish to help a stranger in need. However, the reason may also be a need for attention, or wanting to get something out of the donation in some way. The process for non-directed organ donation involves intense mental health screening, and a cooling-off period of several months. The mental health assessment is carried out by qualified and experienced psychiatrists or psychologists. They help potential donors think through the decision about whether or not to donate. They can also give advice on common feelings after donation, including feelings the donor might have if the transplant is not successful (eg depression). Whether the person goes ahead with donation or not, counselling continues to be available. Social assessment The hospital social worker talks to potential donors about the effects of the donation on their social wellbeing. For example, he or she may ask whether someone is available to assist with daily activities after the surgery and how they will manage financially while recovering. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION What is the process of donation? Medical assessment The medical assessment is important for both the donor and the recipient. Tests are carried out to make sure that: • d onation will have a minimal effect on the donor’s future health; and • the donor does not have any illnesses that could be passed on to the recipient through the donation. Decision-making — balancing the needs of everyone involved “After all the time I spent talking to different people at the hospital, and then the tests as well, we finally heard that I could be a donor for my aunty. It felt good to know that everything was fine and I felt confident that I would be okay with just one kidney.That was 5 years ago now and we are both feeling great.” For some people making the choice to donate may be quite easy. Others may feel caught in a very difficult situation. They may feel uncomfortable about donating, or the family relationship may make the situation so emotional that it is difficult to think clearly and decide freely. The pressure can be more intense and potential donors may feel there is no choice but to agree if: • m edical testing shows that they are the only matching donor in the family; • family member is likely to die unless transplant goes ahead; and • f amily members apply pressure through emotional ‘blackmail’, threats of disapproval or even the promise of favours. It is very important that potential donors decide for themselves and are not influenced by others. It is usually possible to take some time to come to a decision. Counselling is available during the decisionmaking process to help everyone involved. Before the potential donor is asked to make a final decision, he or she can discuss all of the reports with the doctor who is acting as their advocate. The advocate can give them confidential advice and help them to think about all of the important issues. “I don’t mind admitting that I was scared when they told me I could be a donor for Sally. Still, the doctors and nurses were very supportive and the surgery and recovery weren’t as bad as I expected. I still go back to the hospital for regular check-ups. Sometimes Sally and I go together and I am proud to know that I have helped Sally become healthy again.” The surgeon who will do the operation has to be sure that it is safe to do the surgery. Finally, if all agree, the donor is asked to sign the papers for consent to the operation. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION What is the process of donation? The person who needs the transplant also has to give consent to receiving the organ or tissues before surgery goes ahead. The recipient may not wish to get an organ from a living donor. If this happens, they keep their place on the waiting list for an organ from a donor who has died. If the potential donor decides not to donate or if there are other reasons why the transplant will not proceed, counselling is available. Medical or mental health care is also given if a disease or other health problem is identified during assessment. In most Australian States, children can be living donors for a sibling or a parent only, and may donate only regenerative tissue (eg bone marrow). Deciding on behalf of a child or dependent adult In some cases, a child or an adult who cannot make a decision for themselves (eg due to mental illness, brain injury or dementia), may be the only good match for a transplant. The health care team help parents or guardians to find the best way to make a decision about donation. This takes into account the welfare of the donor and the person who needs the transplant. It is important for older children to think about donation and take part in the decision. In some cases, the potential donor may suffer more from the loss of a parent or brother or sister (should the transplant not go ahead) than they would from the donation. Health professionals help parents or guardians to make sure that the potential donor under­stands as much as possible about what will happen to them and what the transplant will mean for the recipient. In all cases of donation by a child or dependent adult, an independent team makes a decision about whether the donation should be allowed to go ahead. They try to do what is best for the potential donor. Parents or donors are then asked to give their consent for the donation. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 10 What is the process of donation? Decisions to allow a child or dependent adult to become a living donor are only ethically right when: • no other suitable donors are available; • the risks and discomforts to the donor are minimal; • the person receiving the transplant is a close relative; • the donation is a last resort in treatment and is expected to be of great benefit to the recipient; • an independent team considers that on balance the donation is in the donor’s best interests; • the parents or guardians consent and the donor agrees (if she or he is able to do so); and • where required by law, authorisation has been obtained. “The only compatible donor for Jamie was his twin brother Andy. The boys were only 8 at the time and didn’t really understand what bone marrow donation would mean for them. It was a hard road for us all but it helped that so many people were involved in the decision-making. The hospital ethics committee took the final decision on whether or not we could go ahead with the donation.” Continuing care of donors All donors are offered medical and mental health care for at least one year after the donation or longer if there are any complications. The staff member who supported the donor through the donation process is usually involved in follow-up care. Contact details for organisations that can provide information and resources about donation and continuing care are given in Section 5 of this booklet. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 11 What is the process of donation? Living organ and tissue donation for adults* Potential donor considers donation Potential donor learns about assessment If consent to assessment given Medical assessment • Donor is compatible with recipient • Potential donor is making a free choice to donate • There are minimal known medical or surgical problems • It is unlikely that donation will have a harmful effect on the person’s mental wellbeing • There is minimal risk of infection to the recipient If minimal risk of physical harm Social assessment Psychological assessment • Employment or studies will not be unreasonably affected by donation elp with daily activities • H will be available during recovery period • Person is able to manage financially during recovery If minimal risk of psychological harm If minimal risk of social harm Donor advocate advice on donation If no barriers to donation Surgical team decision on donation If no unreasonable risk to donor Donor gives written, informed consent to donation If consent is not given, donation does not proceed and reasons for withdrawal remain confidential Donation and transplantation proceed Ongoing care of donor • Medical review • Mental health review • Counselling and support *This framework is meant as a guide only. The actual sequence of events will depend on individual circumstances. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 12 What is the process of donation? Living organ and tissue donation for children or dependent adults* Person is identified as a potential donor Person’s family learn about the assessment process If family consents to assessment Medical assessment • Donor is compatible with recipient • There are no known medical/ surgical problems • There is minimal risk of infection to the recipient If minimal risk of physical harm Social assessment Psychological assessment • Potential donor understands • Appropriate care will the process as far as is be available after the possible donation • As far as he or she understands, the potential donor agrees to donate • L ikelihood of harm to potential donor’s wellbeing is greater from not donating than from donating If minimal risk of psychological harm If minimal risk of social harm Legal and ethical assessment • Ethical principles have been followed in process of consent • There are no ethical reasons not to proceed • There are no legal reasons not to proceed If potential donation is ethically and legally acceptable Independent team decision on donation If donation is considered to be in the person’s best interests Surgical team decision on donation If there is no unreasonable risk to the donor Parent/guardian gives consent to donation If consent is not given, donation does not proceed and reasons for withdrawal remain confidential Donation and transplantation proceed Ongoing care of donor • Medical review • Mental health review • Counselling and support *This framework is meant as a guide only. The actual sequence of events will depend on individual circumstances. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 13 Different decisions about living donation 4different decisions about living donation People choose to be living donors, or choose not to be, for different kinds of reasons or a mixture of reasons. Some examples of these are given below. For: • The donation may improve the quality of life for the recipient. • The potential risks of donating are outweighed by the potential benefits to the person needing a transplant. • The transplant can take place while the person who needs it is still quite healthy. • Living donation by a relative increases the likelihood that the recipient will receive a well-matched organ or tissue. • In living donation, the transplant operation can take place straight after the donation operation. This means that the transplanted organ starts working again more quickly. • Transplants from living donors usually work better than from dead donors. • Living donation can be a rewarding experience for both donor and recipient. Against: • There is a risk that the transplanted organ will be rejected or won’t work or that a bone marrow transplant will be unsuccessful. • The donor will need to take time out from their normal routine to have tests, to undergo surgery and during the recovery period. • The operation, like any surgery, has risks even though every effort is made to minimise these risks. There are also risks of illness or death after donation. • The donor may feel unhappy about the way that the recipient treats the organ. • The donor may not like the feeling that the organ now belongs to someone else. • The donor may feel responsible if the recipient becomes sicker or dies. • The relationship between the donor and the recipient may change. • The donor may incur expenses such as travel costs and accommodation. • There are different ways of helping others that may be preferable. MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 14 Before you decide 5 Before you decide This booklet has been designed to guide you through some of the issues to consider when making a decision about living organ and tissue donation. Here are some questions to ask yourself as you decide. Have I been given enough information to understand the donation procedure, the possible risks involved and what happens afterwards? Am I aware of the chance of success of the transplant and the likely benefits to the recipient? If I decide not to donate, what is the alternative for the recipient and how long is he or she likely to have to wait for an organ from a dead donor? Further information Websites Australian Bone Marrow Donor Registry www.abmdr.org.au Australia and New Zealand Dialysis and Transplant Registry www.anzdata.org.au How will I feel if the recipient of my organ continues to have ill health or dies after the transplantation? Australians Donate www.organdonation.org.au How will I cope with changes to my own health if there are problems after the donation? HealthInsite healthinsite.gov.au How will I feel knowing that my organ is inside someone else’s body? How will the donation affect my relationship with the recipient? How will my family react to my decision? How will I feel if I choose not to donate? How do I feel about making a decision on behalf of my child or a dependent adult in my care? Kidney Health Australia www.kidney.org.au Publications Kidney Donation by Live Donors www.health. nsw.gov.au or from the Renal Resource Centre on 1800 257 189 Living Donor Kidney Transplantation Donor and Recipient Perspectives www.uktransplant.org.uk MAKING A DECISION ABOUT LIVING ORGAN AND TISSUE DONATION 15