Emergency Department and Urgent Care for Children
Excluded From Child Care
WHAT’S KNOWN ON THIS SUBJECT: Previous studies have
revealed that children in child care are frequently ill with mild
illness and are unnecessarily excluded from child care at high
rates.
WHAT THIS STUDY ADDS: Parent race/ethnicity, single parents,
and work-related concerns are associated with increased
emergent/urgent care use for a sick child excluded from child
care, even for mild illnesses.
AUTHORS: Andrew N. Hashikawa, MD, MS,a David C.
Brousseau, MD, MS,b Dianne C. Singer, MPH,c Achamyeleh
Gebremariam, MS,c and Matthew M. Davis, MD, MAPPc,d
aDepartment of Emergency Medicine, cChild Health Evaluation
and Research Unit, University of Michigan Medical School, Ann
Arbor, Michigan; bSection of Pediatric Emergency Medicine,
Department of Pediatrics, Medical College of Wisconsin,
Milwaukee, Wisconsin; and dInstitute of Healthcare Policy and
Innovation and Gerald R. Ford School of Public Policy, University
of Michigan, Ann Arbor, Michigan
KEY WORDS
child care, illness, urgent care, emergency care, policy, survey,
and parents
abstract
BACKGROUND: Children in child care are frequently unnecessarily excluded for illness. We investigated parental use of urgent medical
evaluation for sick children unable to attend child care.
METHODS: In May 2012, authors conducted a nationally representative
survey of parents, who completed online questions regarding child illness causing absence from child care and their medical care-seeking
behavior. Main outcome was parents’ use of emergency department or
urgent care (ED/UC).
RESULTS: Overall survey participation rate was 62%. Of participating
parent cohort with children 0 to 5 years old, 57% (n = 357) required
child care, of which 84% (n = 303) required out-of-home child care.
Over 88% of parents sought acute medical care for their sick children unable to attend child care. Approximately one-third of parents needed a doctor’s note for employers and/or child care. Parents
sought medical evaluation (.1 option possible) from primary care
(81%), UC (26%), or ED (25%). ED/UC use was most common for rash
(21%) and fever (15%). Logistic regression indicated ED/UC use was
significantly higher among single/divorced parents (odds ratio [OR] =
4.3; 95% confidence interval [CI]: 2.5–13.5); African American parents
(OR = 4.2; 95% CI: 1.2–14.6); parents needing a doctor’s note (OR = 4.2;
95% CI: 1.5–11.7); and those with job concerns (OR = 3.4; 95% CI: 1.2–9.7).
CONCLUSIONS: A substantial proportion of parents whose sick children cannot attend child care seek care in ED/UC. Training child
care professionals regarding appropriate illness exclusions may
decrease ED/UC visits by lowering child care exclusions. Pediatrics
2014;134:e120–e127
ABBREVIATIONS
AAP—American Academy of Pediatrics
ACA—Affordable Care Act
aOR—adjusted odds ratio
CI—confidence interval
ED—emergency department
GfK—GfK Custom Research, LLC
NPCH—National Poll on Children’s Health
OR—odds ratio
UC—urgent care
Dr Hashikawa conceptualized and designed the study, helped
with data acquisition, and drafted the initial manuscript;
Dr Brousseau helped conceptualize and design the study,
contributed substantially to data interpretation, and critically
reviewed and revised the manuscript; Ms Singer made
substantial contributions to study design, study analysis and
data interpretation, and critically reviewed the manuscript;
Mr Gebremariam carried out data analysis and interpretation
and critically reviewed the manuscript; Dr Davis made
substantial contributions to study design and development of
data collection instruments and critically reviewed and revised
the manuscript; and all authors approved the final manuscript
as submitted.
www.pediatrics.org/cgi/doi/10.1542/peds.2013-3226
doi:10.1542/peds.2013-3226
Accepted for publication Mar 25, 2014
Address correspondence to Andrew N. Hashikawa, MD, MS,
Department of Emergency Medicine, Children’s Emergency
Services, 2800 Plymouth Rd, Suite G080, NCRC Building 10, Ann
Arbor, MI 48109-2800. E-mail: drewhash@umich.edu
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2014 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have
no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated
they have no potential conflicts of interest to disclose.
e120
HASHIKAWA et al
Downloaded from by guest on October 1, 2016
ARTICLE
More than 80% of the children in the
United States will require nonparental
child care by 6 years of age because of
working parents, welfare reform, and
economic necessity.1–3 Children in child
care center settings have more upper
respiratory infections, diarrheal illness,
ear infections, and myringotomy tube
placement than children who stay at
home exclusively.4–7
Previous research demonstrates that
ill children are routinely excluded from
child care unnecessarily given that
most child care-related illnesses are
minor in severity.8–11 Unnecessary
exclusions place a substantial burden
on working families, businesses, and
health care resources.1,9,12–18 Nationally, an estimated 44 million workers
lack any paid sick leave benefits to
care for sick children, disproportionately affecting poor and minority
families.19
The American Academy of Pediatrics
(AAP), in its publication Caring for Our
Children: National Health and Safety
Performance Standards for Out-ofHome Child Care and Early Education
Programs,20 outlined clear child care
illness exclusion guidelines, particularly
if the child cannot participate comfortably in activities or needs more attention
that staff can provide safely. Several
studies demonstrate that child care
provider adherence to the guidelines is
low, however, and training is unavailable
in most states.8,9,21,22
Consequently, child care providers unaware of AAP national child care recommendations may increase parents’
perceived need for urgent medical
evaluations for nonurgent conditions
to avoid loss of wages or missed time
from work.23–26 An estimated 50% to
80% of the 25 million pediatric visits to
the emergency department are for
nonurgent conditions.27–30 High emergency department (ED) utilization for
nonurgent conditions leads to increased
cost, prolonged wait times, patient dis-
satisfaction, and adverse events.28,31
Studies suggest that most families
seeking nonurgent pediatric ED visits
report having a regular primary care
physician.27,32 Multiple factors associated with pediatric nonurgent ED
utilization have been identified, including single parent status, Medicaid
insurance, lack of convenient/weekend
hours, parent ED utilization, and quality
of relationship with primary care provider.27,28,33,33 Many of these factors are
prominent characteristics of parents
who need child care services. No
studies of pediatric ED or acute care
use, however, have assessed the impact that child care illness might have
on parents’ need for urgent medical
evaluations.
The C.S. Mott Children’s Hospital National Poll on Children’s Health (NPCH)
survey was used to investigate the prevalence and characteristics of parents
who use the ED or urgent care (UC) for
sick children unable to attend child
care.
METHODS
Study Design and Sample
The NPCH, located within the Child
Health Evaluation and Research Unit of
the Division of General Pediatrics at the
University of Michigan, measures perceptions concerning major health care
issues and trends for US children. The
NPCH is conducted in partnership with
the GfK Custom Research, LLC (GfK)
Group’s Web-enabled KnowledgePanel,
a probability-based panel designed to
be representative of the US population.
The KnowledgePanel has served as the
sampling frame for several other peerreviewed studies on health topics related to children.34–37
The NPCH sample includes oversampling
of parents and members of racial and
ethnic minorities to ensure adequate
representation of those groups. Panel
participants were originally chosen
through random selection of telephone
PEDIATRICS Volume 134, Number 1, July 2014
numbers and residential addresses and
were invited by GfK to participate by
telephone or mail. If individuals agree to
participate but do not already have Internet access, GfK provides them a laptop and Internet service connection at no
cost. Panelists receive unique log-in
information for accessing surveys online,
and then are sent emails each month
inviting them to participate in research
ona wide array of topics.After joining the
panel, participants provide individual
and household demographic data, used
for sampling purposes.
The survey for the current study was
piloted in April 2012 by using a separate
convenience sample of 105 KnowledgePanel participants. The process for the
pretest sample is very similar to the
process for the main survey, with identical sample definitions in both samples.
When the survey items were judged by
the investigators to be functioning as
intended, the final survey was fielded in
May 2012. Eligible participants in the
survey were adults 18 years or older. This
study is based on responses of parents
with children 0 to 5 yearsold in child care.
The study was approved by the University
of Michigan Medical School Institutional
Review Board.
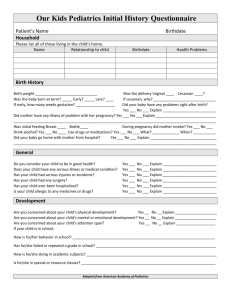
Survey Items
The focus of this study was on parental
responses to 5 questions related to
child care and illness, within a larger
survey of 52 questions on topics including bullying, hearing loss, top child
health concerns in respondents’ communities, and whole genome sequencing. The survey questions related to
child care and illness developed by the
study team are presented in Fig 1: for
purposes of analysis, “child care” also
included “daycare” and “preschool”
settings. Only children who required
care outside their homes were included.
For parents with .1 child, each parent
was asked to select the youngest child
as the index case for purposes of this
study.
e121
Downloaded from by guest on October 1, 2016
FIGURE 1
Survey questions in NPCH survey related to child care illness and management.
e122
HASHIKAWA et al
Downloaded from by guest on October 1, 2016
ARTICLE
Parents completed survey questions
regarding illnesses that caused absence
from child care and medical careseeking behavior when their children
could not attend child care. Five hypothetical vignettes about a child with illness symptoms (cold symptoms without
fever, conjunctivitis, gastroenteritis,
mild fever, and ringworm), adapted
from Copeland et al8 and previously
used by the authors,9,21 were presented
to each respondent (Fig 1). For each of
the illness vignettes, parents chose
whether the child would be a) sent to
child care despite symptoms; b) excluded by child care because of illness;
or c) kept at home even if the child was
allowed at child care. Parents were also
asked if they would take their children
for medical care if their children developed symptoms the evening before
an important parent meeting. The median time to complete the survey was
10 minutes.
Survey Analysis
Deidentified data were presented from
the survey partner to the authors, with
sampling weights on the basis of the US
Census to yield nationally representative estimates. All result data are presented weighted for the US population.
Bivariate analyses (x2 tests) were
conducted for the relationship between parent-reported ED/UC use and
several parent (gender, race, parent
education, household income, house
ownership status, housing type) and
child (insurance status, allergy status,
asthma status, seizure, lung disease
from prematurity, obesity) characteristics. The primary outcome was
parent’s use of either the ED or UC for
their child. Parents’ choices of site of
urgent medical care (ED, UC, or primary care provider) were initially analyzed separately, but UC and ED were
then combined for final analysis, given
the sample size and distribution of
answers.
The authors then applied logistic regression models to examine the associations between parent-reported ED/UC
use and child variables. All variables
achieving a P , .05 level of significance
in bivariate analyses were retained in
our final multivariate model. Descriptive
statistics were used to summarize
responses to vignettes.
RESULTS
Study Participants
Overall survey participation rate was
62%. Among the participating cohort of
parents with children 0 to 5 years old (n =
630), 57% of parents (n = 357) required
child care for at least 1 child, of which
84% (n = 303) of parents had a child
requiring child care outside the home.
Parent and child demographics are
presented in Table 1.
Overall, 38% of parents required
a doctor’s note either for their own
work (20%), and/or so their children
could return to child care (30%). Onethird of parents (33%) were concerned
about loss of job or pay when taking
time off of work to care for their sick
children when those children were
unable to attend child care.
Most parents (88%) took their children
to a medical provider when their sick
children were unable to attend child
care. Although 80% of parents reported
seeking medical care for their sick
child in the past year at a primary care
physician’s office, substantial proportions
of parents also reported choosing UC
(26%) or ED (25%) settings.
Factors Associated With ED/UC
Utilizations: Bivariate Analysis
In bivariate analyses, ED/UC use was
significantly higher among parents
needing a doctor’s note (versus those
who did not), parents with work concerns (versus those without), African
American parents (versus all others),
single/divorced parents (versus married parents); and parents with an-
PEDIATRICS Volume 134, Number 1, July 2014
TABLE 1 Parent and Child Characteristics
Parent and Child Characteristics, N = 303
Parent gender
Women
Men
Parent race/ethnicity
Non-Hispanic white
Non-Hispanic black
Other non-Hispanic
Hispanic
Parent marital status
Married
Living with partner
Never married
Divorced
Separated
Annual household income
,$30K
$30K to $60K
.$60K to #$100K
.$100K
Parent education level
Less than high school
High school
Some college
Bachelor’s degree or higher
Child age
0–11 mo
1y
2y
3y
4y
5y
Time in child care
.30 h per week
10–30 h per week
,10 h per week
Child asthma
Yes
No
Child insurance
Private
Public
None
%
53
47
59
16
6
19
71
13
10
4
2
23
28
27
22
11
21
33
35
7
7
15
18
22
31
31
40
29
8
92
64
33
3
nual household income ,$60 000 (vs
$$60 000). Parent education level,
child insurance status, and other child
variables were not statistically significantly associated with ED/UC use in
our analysis.
Parents’ need for a doctor’s note, parent race/ethnicity, marital status, and
parent work concerns remained statistically significant in multivariate
analyses. ED/UC use was higher among
parents needing a doctor’s note (adjusted odds ratio [aOR] = 4.2; 95% confidence interval [CI]: 1.5–11.7). African
American parents were more likely than
e123
Downloaded from by guest on October 1, 2016
white or Hispanic parents to use the
ED/UC (aOR = 4.2; 95% CI: 1.2–14.6).
Single or divorced parents (aOR = 4.3;
95% CI: 1.4–13.5), and parents with job
concerns (loss of pay or job when taking
time off work to care for a sick child
unable to attend child care; aOR = 3.4;
95% CI: 1.2–9.7) were also more likely
to use the ED/UC.
Vignettes and Medical
Care-Seeking Behavior
Collectively across all vignettes, .85%
of parents would seek acute medical
care for their children for any symptoms
presented. Parent responses to illness
vignettes are presented in Fig 2.
FIGURE 2
Will parents send a child with symptoms to child care?
Parent preference for the type of acute
medical care (primary care provider
versus ED/UC versus no visit) also varied
depending on illness symptom in each
vignette (Fig 3).
DISCUSSION
Our survey is the first study to demonstrate that a high proportion of parents
report seeking medical evaluation in
acute care settings when their children’s
illnesses prevent attendance at child
care. The potential impact of this type of
health care-seeking behavior on health
care resources may be substantial
given the sheer number of children
currently using child care services
nationally. Reasons for seeking acute
medical care for a child excluded
from child care may be multifactorial,
with ED/UC use higher among singleparent households, African American
parents, parents concerned about job
threats to their job or job-related income, and parents in need of a doctor’s
note.
Our results concur with previous studies
that revealed factors associated with
nonurgent pediatric emergency visits
include single-parent status and the
need for convenient before- and afterwork hours.27,33 Our additional findings that parents at higher risk for using
e124
FIGURE 3
Parent preference for acute medical care.
ED/UC settings for child care illnesses
were African American parents and
single parents are also consistent with
previous studies.23,25 Our study did not
find that Hispanic families were at higher
risk for ED/UC use, consistent with
studies revealing that Hispanic families are more dependent on child care
provided by extended families.38,39
Parents without sick leave benefits face
a considerable dilemma as they risk
either loss of wages or loss of a job to
stay home with a sick child excluded
from child care. Parents may view the
HASHIKAWA et al
Downloaded from by guest on October 1, 2016
situation as a socioeconomic emergency, choosing the inconvenience of an
urgent medical evaluation over the inability to return to work in a timely
manner. This choice may partially explain why almost 9 of 10 parents in our
study chose to seek medical evaluation
when their sick child could not attend
child care. Lack of health insurance was
not associated with increased ED/UC
use because the majority of children
in our survey, similar to 2011 national
statistics, had health insurance coverage.40
ARTICLE
Child care illness policies that differ
from AAP child care guidelines may impact parent medical care-seeking behavior. The need for a doctor’s note, as
reported by almost one-third of parents
in our survey, was associated with increased ED/UC use for sick children excluded from child care. Many child care
settings, in contrast to AAP guidelines,
require health care visits before a child
can return to child care.21 National AAP
child care guidelines no longer require
a mandatory health visit for many
symptoms of illness and children can
usually return to child care as long as
general exclusion criteria are resolved,
the child can participate in usual activities, and child care providers can provide and maintain safe staffing ratios.19,41
A previous study revealed that the majority of parents of children excluded
from child care reported they would not
have scheduled the medical visit if it
were not required by child care policies.42 Our study revealed that with almost one-third of parents (for fever,
pink-eye, rash, and gastroenteritis
vignettes) reporting their children
would not be allowed in child care, a
substantial proportion of parents may
be scheduling medical visits on the
basis of unnecessary child care illness
exclusion policies. Interventions targeting child care providers to use AAP
guidelines to make appropriate exclusion and return-to-care decisions may
decrease parents’ need to seek urgent
medical evaluation for nonurgent
child care illnesses.
All the illness symptoms in the vignettes,
per AAP child care guidelines, would not
have required immediate exclusion from
child care settings. In our study, few
parents would send their child with mild
symptoms to child care for ringworm,
gastroenteritis, or fever. Most parents
reported wanting to seek acute medical
care for at least 1 of the illnesses in the
vignettes. Moreover, parents’ decisions
to seek urgent medical evaluation varied
by vignette, suggesting parents are
more concerned about certain symptoms (eg, fever, rash) compared with
others. These findings are consistent
with a previous survey of child care
center directors, which reported that
children with these same symptoms
(rash or fever) would be more likely
than children with other symptoms to
be excluded from child care centers.9
Consistent with previous studies,
parents in our national survey reported
self-excluding their children from child
care, suggesting a lack of knowledge regarding AAP national child care guidelines by parents.1,8 We were surprised
by the proportion of parents who
reported they would seek medical care
for mild upper respiratory symptoms,
with almost one-fifth of parents reporting they would seek primary care provider evaluation for their child. Given
the large number of children in child
care settings, parents with sick children
unable to attend child care seeking
acute medical evaluation may profoundly impact available primary care
resources.
Our study also indicates that “fever
phobia,” described for many years in
the literature, continues to exist among
parents.43 Fever education and anticipatory guidance may benefit parents.44
New parents with young children in
child care should be given regular anticipatory guidance regarding the expected
increase in frequency of infections and
the management of common child care
related illnesses. Targeted parent educational interventions in child care could
help decrease the demand for antibiotics
for viral or respiratory conditions.
It is unclear how implementation of the
Affordable Care Act (ACA) may affect
health care-seeking behavior of parents
forchildren in child care. In this study and
others, most families have primary care
providers for their child, and expansion
of children’s coverage is not a major
focus of the ACA. The ACA’s emphasis on
PEDIATRICS Volume 134, Number 1, July 2014
providing care in patient-centered medical homes may encourage providers to
expand service hours, which can help
decrease ED/UC visits for primary careappropriate conditions.
The child care industry and child care
providers face numerous challengeswith
respect to managing illness in child care
settings. Many child care settings are
facedwithhigh-turnoverofstaff,poorpay,
and lack of available health-related
training; children with mild illness may
place a significant strain on child care
provider ratios. Additionally, child care
providers may face considerable opposition from some parents who feel any
illness should be excluded from child
care. To help child care providers establish policies for safe and appropriate
management of mildly ill children, the
AAP has established national recommendations that include guidelines that
allow for exclusion if staff to child ratio is
not adequate or the child cannot participatecomfortablyinactivities. The AAP
has created a new free online learning
course via PediaLink available through
the AAP’s Healthy Child Care America
Web site (http://www.healthychildcare.
org) for child care providers to learn
how to prevent and manage infectious
diseases in child care settings on the
basis of AAP national child care guidelines. Additionally, the AAP Web site offers
free, in-training materials that health
care trainers can use to teach groups of
child care professionals and parents
about AAP national child care illness
guidelines.45 Widespread dissemination
of AAP child care guidelines at the state
and national level along with active child
care provider training has the potential
to decrease parental work absenteeism
and health resource utilization.
Our study has several potential limitations. First, similar to any survey,
selection bias and response bias may
exist. We used an established survey process recognized as valid and nationally
representative in previous peer-reviewed
e125
Downloaded from by guest on October 1, 2016
publications, but it is possible that unforeseen biases related to the perspectivesofparentswithchildreninchild
caremay haveinfluenced thefindings.34–37
Another limitation in our study design
is the use of vignettes to assess decisions about child care attendance and
care-seeking behavior. It is possible that
parents’ responses may not reflect actual
medical care-seeking behavior. Nevertheless, the vignettes provided a standardized approach to assess parents’
care-seeking behavior tendencies, in
a manner aligned with AAP guidelines.
Another potential limitation is that the
languageandstructureofthesurveyitems
may have been challenging for parents
with low literacy. For this reason, we
designed the survey at a Flesch-Kincaid
reading level of 3.1 (third grade); additionally, the vignette items have been
previously and successfully used in a
survey for parents.8 Finally, the fifth vignette presented a situation that may
potentially represent a bias toward parents in professional job settings. The
scenario, however, was intentionally nonspecific (parent faced with an important
meeting the next day) so that the scenario
could still occur for parents employed in
minimum wage or job-training settings
and not just in professional settings.
CONCLUSIONS
A substantial proportion of parents
seek care in ED/UC settings for children excluded from child care for
nonurgent conditions. Socioeconomic
and parent concerns about loss of pay
or job may be significant contributors
to urgent medical care-seeking behavior among parents with sick children unable to attend child care.
Adoption of national AAP child care
guidelines by states and the training of
child care providers and parents may
reduce the unnecessary exclusion of ill
children and the unnecessary utilization of ED/UC resources.
REFERENCES
1. Copeland KA, Duggan AK, Shope TR. Knowledge and beliefs about guidelines for exclusion of ill children from child care.
Ambul Pediatr. 2005;5(6):365–371
2. Shope TR, Aronson S. Improving the health
and safety of children in nonparental early
education and child care. Pediatr Rev. 2005;
26(3):86–95
3. Liu M, Anderson SG. Neighborhood effects
on working mothers’ child care arrangements. Child Youth Serv Rev. 2012;34(4):740–
747
4. Alexander CS, Zinzeleta EM, Mackenzie EJ,
Vernon A, Markowitz RK. Acute gastrointestinal illness and child care arrangements. Am J Epidemiol. 1990;131(1):124–131
5. Marx J, Osguthorpe JD, Parsons G. Day
care and the incidence of otitis media in
young children. Otolaryngol Head Neck
Surg. 1995;112(6):695–699
6. Pickering LK, Bartlett AV, Woodward WE.
Acute infectious diarrhea among children
in day care: epidemiology and control. Rev
Infect Dis. 1986;8(4):539–547
7. Wald ER, Guerra N, Byers C. Upper respiratory tract infections in young children:
duration of and frequency of complications. Pediatrics. 1991;87(2):129–133
8. Copeland KA, Harris EN, Wang NY, Cheng TL.
Compliance with American Academy of
Pediatrics and American Public Health Association illness exclusion guidelines for
child care centers in Maryland: who follows them and when? Pediatrics. 2006;118
e126
9.
10.
11.
12.
13.
14.
15.
(5). Available at: www.pediatrics.org/cgi/
content/full/118/5/e1369
Hashikawa AN, Juhn YJ, Nimmer M, et al.
Unnecessary child care exclusions in a
state that endorses national exclusion
guidelines. Pediatrics. 2010;125(5):1003–1009
Pappas DE, Schwartz RH, Sheridan MJ,
Hayden GF. Medical exclusion of sick children from child care centers: a plea for
reconciliation. South Med J. 2000;93(6):
575–578
Shapiro ED, Kuritsky J, Potter J. Policies for
the exclusion of ill children from group day
care: an unresolved dilemma. Rev Infect
Dis. 1986;8(4):622–625
Bell DM, Gleiber DW, Mercer AA, et al. Illness associated with child day care: a
study of incidence and cost. Am J Public
Health. 1989;79(4):479–484
Bradley RH; National Institute of Child
Health and Human Development (NICHD)
Early Child Care Research Network. Child
care and common communicable illnesses
in children aged 37 to 54 months. Arch
Pediatr Adolesc Med. 2003;157(2):196–200
Cordell RL, MacDonald JK, Solomon SL,
Jackson LA, Boase J. Illnesses and absence
due to illness among children attending
child care facilities in Seattle-King County,
Washington. Pediatrics. 1997;100(5):850–855
Cordell RL, Waterman SH, Chang A, Saruwatari
M, Brown M, Solomon SL. Provider-reported
illness and absence due to illness among
children attending child-care homes and
HASHIKAWA et al
Downloaded from by guest on October 1, 2016
16.
17.
18.
19.
20.
21.
22.
centers in San Diego, Calif. Arch Pediatr
Adolesc Med. 1999;153(3):275–280
Giebink GS. Care of the ill child in day-care
settings. Pediatrics. 1993;91(1 pt 2):229–233
Lu N, Samuels ME, Shi L, Baker SL, Glover
SH, Sanders JM. Child day care risks of
common infectious diseases revisited.
Child Care Health Dev. 2004;30(4):361–368
Wald ER, Dashefsky B, Byers C, Guerra N,
Taylor F. Frequency and severity of infections in day care. J Pediatr. 1988;112(4):540–
546
National Partnership for Women and Families. Paid sick days. Available at: http://
paidsickdays.nationalpartnership.org/site/
PageServer?pagename=psd_toolkit_factsheets.
Accessed April 15, 2014
American Academy of Pediatrics, American
Public Health Association, National Resource Center for Health and Safety in
Child Care and Early Education. Caring for
Our Children: National Health and Safety
Performance Standards; Guidelines for
Early Care and Education Programs. 3rd
ed. Elk Grove Village, IL: American Academy
of Pediatrics; Washington, DC: American
Public Health Association; 2011
Hashikawa AN, Stevens MW, Juhn YJ, et al.
Self-Report of Child Care Directors Regarding Return-to-Care. Pediatrics. 2012;
130(6):1046–1052
Landis SE, Earp JA. Day care center illness:
policy and practice in North Carolina. Am J
Public Health. 1988;78(3):311–313
ARTICLE
23. Heymann SJ, Earle A. The impact of welfare
reform on parents’ ability to care for their
children’s health. Am J Public Health. 1999;
89(4):502–505
24. Heymann SJ, Earle A, Egleston B. Parental
availability for the care of sick children.
Pediatrics. 1996;98(2 pt 1):226–230
25. Heymann SJ, Toomey S, Furstenberg F. Working parents: what factors are involved in
their ability to take time off from work when
their children are sick? Arch Pediatr Adolesc
Med. 1999;153(8):870–874
26. Voigt RG, Johnson SK, Hashikawa AH, et al.
Why parents seek medical evaluations for
their children with mild acute illnesses.
Clin Pediatr (Phila). 2008;47(3):244–251
27. Phelps K, Taylor C, Kimmel S, Nagel R, Klein
W, Puczynski S. Factors associated with
emergency department utilization for nonurgent pediatric problems. Arch Fam Med.
2000;9(10):1086–1092
28. Mistry RD, Hoffmann RG, Yauck JS, Brousseau
DC. Association between parental and
childhood emergency department utilization. Pediatrics. 2005;115(2). Available at:
www.pediatrics.org/cgi/content/full/115/2/
e147
29. Fong C. The influence of insurance status
on nonurgent pediatric visits to the emergency department. Acad Emerg Med. 1999;6
(7):744–748
30. McCaig LF, Nawar EW. National Hospital
Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data. 2006;
(372):1–29
31. Stanley R, Zimmerman J, Hashikawa C,
Clark SJ. Appropriateness of children’s
nonurgent visits to selected Michigan
emergency departments. Pediatr Emerg
Care. 2007;23(8):532–536
32. Zimmer KP, Walker AR, Minkovitz CS, Zimmer
KP, Walker AR, Minkovitz CS. Maternal and
child factors affecting high-volume pediatric
emergency department use. Pediatr Emerg
Care. 2006;22(5):301–308
33. Doobinin KA, Heidt-Davis PE, Gross TK,
Isaacman DJ. Nonurgent pediatric emergency department visits: Care-seeking
behavior and parental knowledge of insurance. Pediatr Emerg Care. 2003;19(1):
10–14
34. Tarini BA, Singer D, Clark SJ, Davis MM.
Parents’ concern about their own and their
children’s genetic disease risk: potential
effects of family history vs genetic test
results. Arch Pediatr Adolesc Med. 2008;162
(11):1079–1083
35. Dempsey AF, Singer DD, Clark SJ, Davis MM.
Adolescent preventive health care: what do
parents want? J Pediatr. 2009;155(5):689–
694
36. Clark SJ, Butchart A, Kennedy A, Dombkowski KJ. Parents’ experiences with and
preferences for immunization reminder/
recall technologies. Pediatrics. 2011;128
(5). Available at: www.pediatrics.org/cgi/
content/full/128/5/e1100
37. Freed GL, Clark SJ, Butchart AT, Singer DC,
Davis MM. Parental vaccine safety concerns
in 2009. Pediatrics. 2010;125(4):654–659
PEDIATRICS Volume 134, Number 1, July 2014
38. Radey M, Brewster KL. The influence of
race/ethnicity on disadvantaged mothers’
child care arrangements. Early Child Res Q.
2007;22(3):379–393
39. Yesil-Dagli U. Center-based childcare use by
Hispanic families: Reasons and predictors.
Child Youth Serv Rev. 2011;33(7):1298–1308
40. Federal Interagency Forum on Child and
Family Statistics. America’s Children: Key
National Indicators of Well-being, 2013
Health Insurance Coverage. Available at:
www.childstats.gov/americaschildren/care1.
asp. Accessed March 1, 2014
41. Aronson SS. Managing Infectious Diseases
in Child Care and Schools, 2nd ed. Elk
Grove Village, IL: American Academy of Pediatrics; 2009
42. Shope TR, Duggan A, Wilson M. Mandatory
doctor’s visits and notes for mildly ill children excluded from child care centers.
Baltimore, MD: Pediatric Academic Societies; 2001
43. Crocetti M, Moghbeli N, Serwint J. Fever
phobia revisited: have parental misconceptions about fever changed in 20 years?
Pediatrics. 2001;107(6):1241–1246
44. O’Neill-Murphy K, Liebman M, Barnsteiner
JH. Fever education: does it reduce parent
fever anxiety? Pediatr Emerg Care. 2001;17
(1):47–51
45. American Academy of Pediatrics. Healthy
Futures: Improving Health Outcomes for
Young Children. Available at: www.healthychildcare.org/healthyfutures.html. Accessed
April 15, 2014
e127
Downloaded from by guest on October 1, 2016
Emergency Department and Urgent Care for Children Excluded From Child
Care
Andrew N. Hashikawa, David C. Brousseau, Dianne C. Singer, Achamyeleh
Gebremariam and Matthew M. Davis
Pediatrics 2014;134;e120; originally published online June 23, 2014;
DOI: 10.1542/peds.2013-3226
Updated Information &
Services
including high resolution figures, can be found at:
/content/134/1/e120.full.html
References
This article cites 39 articles, 15 of which can be accessed free
at:
/content/134/1/e120.full.html#ref-list-1
Citations
This article has been cited by 2 HighWire-hosted articles:
/content/134/1/e120.full.html#related-urls
Subspecialty Collections
This article, along with others on similar topics, appears in
the following collection(s):
Emergency Medicine
/cgi/collection/emergency_medicine_sub
Adolescent Health/Medicine
/cgi/collection/adolescent_health:medicine_sub
Toxicology
/cgi/collection/toxicology_sub
Advocacy
/cgi/collection/advocacy_sub
Child Care
/cgi/collection/child_care_sub
Permissions & Licensing
Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
/site/misc/Permissions.xhtml
Reprints
Information about ordering reprints can be found online:
/site/misc/reprints.xhtml
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
Grove Village, Illinois, 60007. Copyright © 2014 by the American Academy of Pediatrics. All
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on October 1, 2016
Emergency Department and Urgent Care for Children Excluded From Child
Care
Andrew N. Hashikawa, David C. Brousseau, Dianne C. Singer, Achamyeleh
Gebremariam and Matthew M. Davis
Pediatrics 2014;134;e120; originally published online June 23, 2014;
DOI: 10.1542/peds.2013-3226
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
/content/134/1/e120.full.html
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2014 by the American Academy
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on October 1, 2016