skeletal, dentoalveolar, and soft tissue changes in class ii, division 2
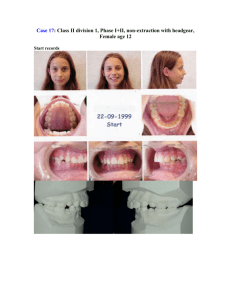
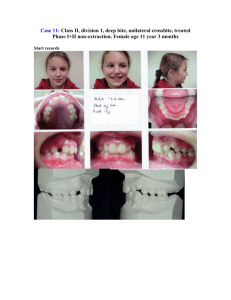
advertisement

SKELETAL, DENTOALVEOLAR, AND SOFT TISSUE CHANGES IN CLASS II, DIVISION 2 MALOCCLUSIONS TREATED BY NON-EXTRACTION WITH FULL APPLIANCES AND THE FORSUS Alan D. Larkin, D.M.D. Thesis Presented to the Graduate Faculty of Saint Louis University in Partial Fulfillment of the Requirements For the Degree of Master of Science in Dentistry 2012 Abstract Objective: To better understand skeletal, dentoalveolar, and soft tissue changes in treated Class II, division 2 malocclusions compared to an untreated matched control group. Materials and Methods: A study group of 29 cephalograms of Class II, division 2 subjects treated by nonextraction therapy, full appliances, and the use of the Forsus appliance were compared to a control sample of Class II, division 2 untreated patients matched for age and sex. Pretreatment (T1) and post treatment (T2) cephalograms were analyzed. An x-y reference plane of SN-7 (x-axis) and a line perpendicular to this passing through sella (y-axis) was used. A total of 30 variables (27 measurements and 3 angular) were evaluated and independent t-tests of the changes between the treated and untreated groups were performed. Results: Vertical facial height did not change with treatment. In the treated group maxillary and mandibular incisors were proclined significantly, 12.3 and 11.3 degrees respectively, however the upper lip showed a decrease in protrusion while the lower lip showed significantly more protrusion. Overbite was reduced from 6.3 mm to 2.5 mm and the mandibular plane angle did not change with treatment. Conclusions: Compared with the untreated control sample, anterior vertical facial height 1 did not change with treatment, the maxillary and mandibular central incisors were proclined significantly with treatment, the SN to GoGn angle did not change with orthodontic treatment, and the treatment effect was limited to the lower lip. Overbite was corrected by relative intrusion of the maxillary and mandibular central incisors, as well as by proclination of the maxillary and mandibular central incisors. 2 SKELETAL, DENTOALVEOLAR, AND SOFT TISSUE CHANGES IN CLASS II, DIVISION 2 MALOCCLUSIONS TREATED BY NON-EXTRACTION WITH FULL APPLIANCES AND THE FORSUS Alan D. Larkin, D.M.D. Thesis Presented to the Graduate Faculty of Saint Louis University in Partial Fulfillment of the Requirements For the Degree of Master of Science in Dentistry 2012 COMMITTEE IN CHARGE OF CANDIDANCY: Professor Eustaquio A. Araujo, Chairperson and Advisor Professor Rolf G. Behrents Adjunct Professor Peter H. Buschang i DEDICATION I dedicate this thesis to my wife, Nicole, who has supported me while I have been in school, which has been our entire married life up to this point. Her optimism and can-do attitude have been a constant enrichment to me each day. I also dedicate this to our five children: Aubrie, Derek, Amalie, Chace, and Branson. My parents, Mark and Lou Ann Larkin, who have made emotional, physical, and financial sacrifices in hopes that I can succeed in whatever field I pursue. ii ACKNOWLEDGEMENTS I would like to thank my committee for their help. Dr. Araujo who has a unique talent of seeing uncovered potential in anyone he comes in contact with, and then being able to help bring that out. patience, motivation, and guidance. Thank you for your To Dr. Behrents, who is the best problem solver I have ever met. always believing in me. Thank you for To Dr. Buschang, thank you for providing a control sample and statistical help. To Dr. Lisa Alvetro, thank you for going out of your way to provide a sample of Class II, division 2 patients who were all treated with the Forsus. iii TABLE OF CONTENTS List of Tables............................................vi List of Figures..........................................vii CHAPTER 1 : INTRODUCTION Description of the Problem.......................1 CHAPTER 2 : REVIEW OF THE LITERATURE Normal Occlusion.................................2 Definition..................................2 Prevalence..................................3 Class II, Division 2 Malocclusion................4 Definition..................................4 Prevalence..................................5 Etiology....................................6 Skeletal Characterizations.................11 Untreated Developmental Characteristics....12 Soft Tissue in Normal Occlusion.................14 Soft Tissue in Class II, division 2.............15 Deep Bite Correction............................18 Forsus..........................................19 Purpose.........................................21 References......................................22 CHAPTER 3 : JOURNAL ARTICLE Abstract........................................28 Literature Review...............................29 Materials and Methods...........................31 Treated Sample.............................31 Untreated Control Sample...................32 Methodology................................33 Statistical Analyses.......................40 Results.........................................43 Horizontal Measurements....................43 Vertical Measurements......................44 Angular Measurements.......................45 Discussion......................................47 Hard Tissue................................47 Soft Tissue................................49 Angular Changes............................51 iv Conclusions.....................................52 Skeletal...................................52 Dentoalveolar..............................53 Soft Tissue................................53 References......................................54 Appendix..................................................56 Vita Auctoris.............................................60 v LIST OF TABLES Table 2.1 – Stellzig et al results of untreated Class II, division 2 changes ...........................16 Table 2.2 – Stellzig et al results of different extraction patterns on the face in Class II, division 2 patients .....................................16 Table 3.1 – Age and gender distribution of study sample...33 Table 3.2 – Landmarks and definitions.....................34 Table 3.3 – Method error results..........................42 Table 3.4 – Changes in cephalometric horizontal measurements..................................43 Table 3.5 – Changes in cephalometric vertical measurements..................................44 Table 3.6 – Changes in cephalometric angular values.......45 Table A.1 – Changes in soft tissue pronasale and gnathion.56 Table A.2 – Horizontal descriptive statistics.............57 Table A.3 – Vertical descriptive statistics...............58 Table A.4 – Angular descriptive statistics................59 vi LIST OF FIGURES Figure 2.1 – Dental appearance of Class II, division 2.....5 Figure 3.1 – Landmarks located............................35 Figure 3.2 – Reference planes.............................36 Figure 3.3 – Vertical soft tissue measurements............37 Figure 3.4 – Vertical hard tissue measurements............37 Figure 3.5 – Horizontal soft tissue measurements..........38 Figure 3.6 – Horizontal hard tissue measurements..........38 Figure 3.7 – Angular measurements and vertical facial height ......................................39 Figure 3.8 – Changes from T1 to T2 for the Untreated Control (left) and Treated (right/dotted lines) ......................................46 vii CHAPTER 1: INTRODUCTION Description of the Problem Throughout the years since orthodontics was first described as a specialty, the definition of an ideal result has changed. Different practitioners have different feelings on what aspects of the teeth, jaw, and face should be changed or enhanced with orthodontic treatment. One area often debated concerns the patient’s lips. Over the past century, many researchers and clinicians have looked at the effects that repositioning of incisors has on the lips. However, most of the effort and studies are focused on the retraction of lips and few look at the effects of protracting the lips. Thus, there is a need to address this void in the literature. 1 CHAPTER 2: REVIEW OF THE LITERATURE Normal Occlusion Definition A little over one-hundred years ago, Angle first described the characteristics of a normal occlusion. Using the maxillary first molars as his “key” he went on to explain that when the mesiobuccal cusp occluded with the buccal groove of the lower molar, a normal occlusion had occurred.1 In addition, the teeth needed to exhibit a relationship in which they were aligned in a smooth curving line of occlusion. A very basic, but profound explanation as this statement has now proved to be correct for more than 100 years. Angle classified malocclusions into the following categories: Class III. Class I, Class II (divisions 1 and 2) and Each category, or classification, was based on the relationship of the first molars and the alignment, or lack thereof, of the other teeth. The definition of normal occlusion proposed by Angle did not consider all aspects of an excellent occlusion. In “The six keys to normal occlusion” published by Andrews in 1972, new insights were given analyzing six significant characteristics observed in a study of 120 casts of 2 non-orthodontic individuals with normal occlusion. The characteristics included proper molar relationship, proper crown angulation, proper crown inclination, no rotations, tight contacts, and a flat occlusal plane.2 These six keys outline the foundation of ideal orthodontic treatment that result in a desirable normal occlusion. Prevalence There is a large range concerning the prevalence of a normal occlusion within the United States. This may be due, in part, to the varying definitions of what can be considered normal or abnormal. Massler and Frankel in 1951 looked at 2,758 children 14 to 18 years old and concluded that only 18% of them had a normal occlusion.3 Their definition of normal was any child that had less than 10 mildly malposed teeth which did not require orthodontic correction. Ast et al found similar results of 4.7% for normal occlusion.4 When the definition of normal is broadened to include Class I malocclusion the percent among United States children who are classified as having a normal occlusion increases to 69.9%.4 For every 44 children who present with a normal, or Class I malocclusion, there will be 15 children who have a Class II malocclusion and 1 child who has a Class III malocclusion.4 3 Class II, Division 2 Malocclusion Definition In 1907 Angle defined the categories, or classifications, of different malocclusion. Class II malocclusion is distal occlusion of the teeth. More specifically it is characterized by distal occlusion of the teeth in both lateral halves of the lower dentition, indicated by the mesiodistal relations of the first permanent molars. To further divide this malocclusion, Angle created the Class II, division 2 malocclusion which focuses on the retrusion instead of the protrusion (as seen in Division 1) of the maxillary incisors.1 Angle described additional features of Class II, division 2 malocclusions. He stated this classification is seen when the lower jaw and chin recessed, caused by the distal position of the mandible and lack of vertical growth below the nose. He also observed an abnormal overbite and the maxillary incisors dipped down and lingually. 4 Figure 2.1 Dental appearance of Class II, division 2 Prevalence The 1966-70 survey mentioned earlier found 54% of children in the United States to be a Class I normal occlusion, also found 32% of the children to have a distocclusion, or Class II (Division 1 or 2) malocclusion.5 Of this percentage, Class II, division 2 malocclusion represents an even smaller part as little as 3% to 4%.3 Studies have cited the prevalence within the Caucasian population to be between 2.3% and 5%.3,4,6 Other ethnic groups have been studied as well and Class II, division 2 malocclusion has been reported to range from 1% to 12% in various racial and ethnic groups.7–11 5 Etiology Many theories exist as to why this malocclusion exists. A key finding is the lingual tipping of the mandibular incisors and the maxillary incisors. Angle said this was because the molars did not erupt to their normal vertical height.1 Strang said faulty growth was the cause for a decreased vertical growth below the nose and heredity was a key factor.12 Like Strang, Graber stated that there is in fact a hereditary pattern to Class II, division 2 malocclusion. He said the tongue interferes with the eruption of the posterior teeth by filling the interocclusal spaces.13 As the posterior teeth are prevented from erupting to their full potential the face becomes shortened. There was a group called The Eastern Component Group of the Angle Society that thought the mandible was in a normal position but a failure in metabolic or developmental process resulted in less than normal vertical growth of the posterior teeth. This failure, combined with hypertrophied sucking muscles due to habits, produced pressure on the anterior part of the mandible in a distal direction which produced less forward growth resulting in a distal locking of the mandibular molar teeth.14 6 According to their observations, they listed the following aspects as possible etiologies for Class II, division 2: (a) Dysfunctional activity of the muscles of the lips causing a backward driving force (b) Excessive action of the mentalis muscles (c) Abnormal swallowing function, especially the first stage, in the form of exaggerated sucking action (d) Premature loss of deciduous molars (e) Hypertoned, tense musculature of lips (f) Hypertrophy of the musculature of the cheeks (g) Nervous, high strung temperament (h) Malnutrition in early infancy (pointing to disturbance of calcium metabolism) (i) Hypertrophy of the mentalis muscles (j) Distal pull by muscles attached to hyoid bone (k) Posture habit (l) Retarded forward growth of the mandible due to muscular pressure They also noted a lack of vertical growth of the mandible, particularly in the molar and the premolar areas, which they speculate was due to a developmental process in early childhood from malnutrition. 7 Based on a clinical impression, Strang believed that heredity was an important factor for the occurrence of Class II, division 2 malocclusions. The faulty growth patterns of facial and cranial structures were caused by the lack of vertical growth below the nose and by the distal positioning of the mandible. Strang also believed that a dysfunction in muscular activity, causing pressure against the maxillary central incisors, combined with the deep bite, were mechanical factors that needed to be considered in the distal positioning of the mandible.12 In another study involving a small sample of only 15 patients, Hedges concluded that Class II, division 2 was not a specific stereotyped clinical syndrome. He believed that the problem develops as the result of compensatory variation, eruptive disharmony and muscular pressure, all combined to form the malocclusion.15 Peck et al found that tooth size plays a large role in Class II, division 2 malocclusion etiology. The investigation found that Class II, division 2 patients’ mesio-distal tooth diameters for the maxillary and mandibular incisors were significantly smaller than the teeth of subjects with normal occlusion. This suggests the genetic influence of tooth size is a strong trait associated with Class II, division 2 malocclusions.16 8 This heritable trait of small teeth has also been found by others.17,18 This heritable trait refers to the general width of the maxillary and mandibular four incisors with all eight incisors being smaller than normal. It was found by Araujo and Souki among the Brazilian population that Class II malocclusion was the least common to have a Bolton discrepancy.19 He found Class I and Class III malocclusions display an anterior Bolton discrepancy more so than Class II malocclusion. Robertson and Hilton measured the crown thickness of central incisors of Class II, division 2 patients and found the labiopalatal width to be decreased in these patients.18 Others looked into this more and found not only the labiopalatal thickness to be reduced, but also found the maxillary central incisor to be shaped significantly different than central incisors in all other maloclussions. Grant concluded there is axial bending of the central incisor, along with a shorter root and longer crown in Class II, division 2 malocclusion.18,20,21 In 1975, Proffit et al said the tongue and lip pressure have a greater influence than the cheek pressure on influencing the position of the teeth.22,23 Perhaps the lips were pushing more forcefully on the incisors and causing them to retrude. 9 Lapatki et al wanted to understand the pressure on central incisors of Class II, division 2 patients better. Within his sample the lower lip in Class II, division 2 patients was 5.1 mm above the maxillary central incisor, whereas in a Class I group the mandibular incisors were only 2.7 mm above the incisal edge. This caused greater pressure on the incisal edge when compared to the cervical portion of the central incisor. They concluded the higher the lip line the greater the incisal force, leading to a more upright central incisor. In fact, a high lip line has higher resting pressure of approximately 2.5 times greater than normal.24,25 Lapatki et al concluded the high lip line and greater pressure on the maxillary central incisors was the cause for cover-bite, a unique parameter often seen in Class II, division 2 patients. Cover-bite is estimated to occur in 2% of the United States population today.3,16 Cover-bite is classified as skeletofacial hypodivergence, mandibular dentoalveolar retrusion, bony chin projection, reduced mesiodistal tooth size, maxillary incisor retroclination, and 100% or greater overbite. Walkow and Peck took cover-bite, or “duckbiss” as it is known in older literature, into consideration and did a study to see how these characteristics affect the dental 10 arch width. They concluded arch width in the posterior was normal in both the maxilla and mandible at the level of the molars. However, in the anterior mandible from canine to canine arch width was significantly less than normal.26 Mandibular intercanine collapse is likely a cause for incisor crowding. All in all, the etiology of Class II, division 2 malocclusion is uncertain. Proffit has stated that the research findings consistently have shown that there is no simple explanation for malocclusion in terms of oral function and that mouth breathing, tongue thrusting, soft diet, or sleeping posture cannot be regarded as the sole or even the major reason for most malocclusions.27 Proffit continues to point out that research has not yet clarified the precise role of heredity as an etiologic agent for malocclusion and that etiology of most orthodontic problems are difficult because several interacting factors probably play a role. Skeletal Characterization Whether patients demonstrating a clinical Class II, division 2 malocclusion have an underlying skeletal or dentoalveolar pattern is an ongoing debate in the literature. Some researchers say the maxilla is too 11 prognathic while others say it is too retrognathic when compared with mandibles in Class I malocclusions. Brezniak et al did a cephalometric study and found no data that showed the maxilla is either prognathic or retrognathic. However, he did find data which shows the mandible in Class II, division 2 patients is shorter than a Class I mandible but longer than a Class II, division 1 mandible.28 However, the data was not statistically significant and so the debate continues. There is an item throughout the literature for which there seems to be no disagreement and that is that Class II, division 2 patients have a vertical discrepancy. Vertically, Class II, division 2 patients are seen to have a hypodivergent facial pattern as seen in an acute gonial angle and enlarged posterior facial height.28 The Peck et al study concluded Class II, division 2 malocclusion has an excessive bony chin projection.16 Perhaps the projection of the bony chin could be the reason researchers claim Class II, division 2 malocclusion is a dentoalveolar problem and not a skeletal problem. Untreated Developmental Characteristics In order to understand differences in Class II, division 2 malocclusion it is important to understand the 12 skeletal and dental differences in untreated and normal occlusion. In 1983, Bjork and Skieller studied the aspects of craniofacial growth through an implant study.29,30 At about the same time these studies were going on for normal occlusion, Fischer-Brandies et al conducted a study which followed Class II, division 2 adult subjects.31 The results showed the pogonion in a normal position with the B-point retropositioned. Thus, the length of the mandible in a Class II, division 2 patient compared to a normal Class I patient is only slightly diminished, if not the same size. Fischer-Brandies et al concludes that in adults, where mandibular growth is completed, there is no significant difference in skeletal structure between Class II, division 2 and a normal Class I occlusion.31 Isik et al found similar results in 2006 and concluded that Class II, division 2 subjects are skeletally similar to Class I subjects.32 In 2009, Al-Khateeb and Al-Khateeb studied 551 cephalograms consisting of Class I, Class II division 1 and 2 adults and children. From this they concluded the mandible of Class II, division 2 malocclusion is orthognathic.33 13 Soft Tissue in Normal Occlusion A long asked question in orthodontics is “how does the face change over time and how is it affected by incisor position.” Facial convexity increases with age but without factoring in the nose the face over time tends to take on a less convex profile.34,35 Between the ages of 9 and 13 facial convexity remains stable and then starting at age 13 the convexity starts to decrease.35 As the patient grows the maxilla becomes less protrusive all the while the chin takes on a more forward position relative to the forehead.34 The facial skeleton becomes flat and the soft tissue becomes less convex. The alveolar process and teeth become more upright in position with growth. The nose grows forward more than the chin grows forward, thus the lips may appear to recede in relation to the profile.34 Without orthodontic treatment, the maxillary and mandibular lips maintain the same position relative to each other. Tissue thickness varies in the face. In 1961 Subtelny found that the nose, A point, vermillion of the upper and lower lip, B point, and pogonion will increase in tissue thickness with age.34,36 Then in 1990 Nanda et al looked at children between the ages of 7 and 18 years old with Class I normal occlusion to further investigate how the untreated soft tissue changes. Their conclusions agreed with that of 14 Subtelny in that parts of the face increase in thickness over time. In addition, Nanda et al found that the tissue over A and B point increase more so than the tissue over the lip vermillion.37 Soft Tissue in Class II, division 2 Few articles compare treatment of Class II, division 2 to a control sample of untreated Class II, division 2 patients. Even fewer studies compare soft tissue changes of this malocclusion to a control sample of the same malocclusion. Stellzig et al, researchers in Germany, used a sample of untreated Class II, division 2 patients from the Belfast Growth Study and compared these to Class II, division 2 patients who had undergone extraction treatment.38 Their control samples were untreated Class I and Class II, division 2 patients between the ages of 9 and 15 yrs old who had cephalograms taken every two years. The study found in untreated patients of Class II, division 2 malocclusion the U1-SN value increased 2 degrees. When examining the lips to the Esthetic plane, “E-plane”, as described by Ricketts, Labial Superiorus changed from -1.1 mm to -2.9 mm during the six years and the Labial Inferiorus changed from -0.8 mm to -2.1 mm behind the E-plane. The Rickett’s Esthetic Plane accounts for the 15 nose and so one must factor into these results that the nose and chin are growing during this time. For ease of comparison Stellzig et al’s results are in a table below. Table 2.1 Stellzig et al38 results of untreated class II, division 2 changes Class II, div 2 Class I Ls-E plane Proclination of 2.3 degrees Retrusion of 1.8 mm Proclination of 1.5 degrees Protrusion of 2.5 mm Li-E plane Retrusion of 1.3 mm Retrusion of 1.8 mm Interincisal angle No change (within 0.5 degree change) No change (within 0.5 degree change) 1-SN Stellzig et al’s study also looked at lip response to anterior segmental distalization after extractions in Class II, division 2 malocclusion. Table 2.2 Their results are below: Stellzig et al38 results of different extraction patterns on the face in Class II, division 2 patients Maxillary and Mandibular first bicuspid extraction Maxillary second molar extraction 1-SN Increase of 5.4 degrees Increase of 8.5 degrees Ls-E plane Retrusion of -3.4 mm Retrusion of -1.6 mm Li-E plane Retrusion of 2.4 mm Retrusion of 0.7 mm This study shows that in untreated Class II, division 2 patients the profile will flatten during the growth period between 9-15 years of age, with the significance of 16 profile flattening being found by a decrease in protrusion of the upper lip.38 However, a weakness to the Stellzig and coworker’s study was the small sample size of untreated controls. Flaring of the incisors has been looked at by others. Honn et al used the Holdaway angle as a reference and found when the maxillary incisors were proclined between 4.4 and 6.2 degrees and the mandibular incisors were proclined between 1.1 and 5.5 degrees the lips protruded more.39 Honn et al found that Class II, division 2 patients attained the standard value according to Holdaway and lip position showed a marked improvement. Rains and Nanda found the upper lip was not only responsive to maxillary incisor movement, but also responded to mandibular incisor movement, mandibular rotation, and the lower lip.40 Leaver studied Class II, division 2 patients treated by non-extraction and extraction therapy and found the upper lip protruded less than expected in the non-extraction group.41 17 Deep Bite Correction As mentioned earlier, a consistent finding in Class II, division 2 malocclusion is that of a deep bite. Deep bite is noted by some authors as the most difficult of goals to achieve in orthodontic therapy.42,43 Several factors related to the development of deep bite coincide with Class II, division 2 malocclusion: a) Infraocclusion of mandibular molars and supraocclusion of maxillary incisors.44 b) Incisor angulation: Overbite decreases as the interincisal angle decreases below 180 degrees, and increases rapidly as exceeds 180 degrees.44 There are multiple techniques to correct a deep bite but all involve intrusion of the maxillary or mandibular incisors, extrusion of the maxillary or mandibular posterior teeth, mandibular incisor proclination, or an increase of the lower face height.45–47 A retrospective study done by Parker et al found side effects for opening the bite in Class II, division 2 malocclusions. The total face height increases by 6.12 mm, maxillary incisor to SN increases by 14.66 degrees, and the IMPA increases an average of 7.91 degrees.48 However this study incorporated both extraction and nonextraction cases and there was no consistency of mechanics for how the deep 18 bite was corrected. Depending on the treatment to correct the deep bite the literature shows a lower face height increase in Class II, division 2 malocclusion between 0.7 mm and 3.20 mm.48,49 However, this increase is consistent with normal growth. In another study which used an activator to correct the Class II, division 2 malocclusion the author noticed an increase of facial height of 7.2 mm from N-Me after treatment, however the author did not record soft tissue change.50 Talass et al commented on vertical facial height and its relationship to soft tissue changes. They found that increasing vertical facial height was not an important factor in upper lip retraction, but attributed this finding to the fact that a minimal amount of facial height increase was found in his particular sample.51 Rains and Nanda used the mandibular position to evaluate the vertical facial height and concluded that mandibular rotation was one of the more significant variables predicting vertical and/or horizontal changes in the upper and lower lips.40 Forsus Surgery, selective extraction patterns, intra-arch, inter-arch, and extra-oral appliances are some of the various techniques orthodontic practitioners have developed 19 over the years to correct Class II, division 2 malocclusions. Intermaxillary elastics are a typical and commonly used method for Class II, division 2 correction. There are several benefits and disadvantages explained in the literature with using inter-arch elastics and they include mesial movements of the mandibular molars, distal movements and tipping of the maxillary incisors, clockwise rotation of the occlusal plane, tipping of the mandibular incisors, extrusion of the mandibular molars and maxillary incisors, and a clockwise rotation of the mandibular plane.27,52–54 However, the side effects, whether good or bad, require the patient to be compliant with the use of elastics or treatment time is lengthened and results compromised.55,56 In an effort to overcome compliance from the patient some orthodontists use other intraoral techniques. The Forsus has been widely accepted in orthodontic therapy. The Forsus does cause palatal tipping and extrusion of the maxillary incisors, protrusion and intrusion with labial tipping of mandibular incisors, distal tipping of maxillary molars, and mesial movement and tipping of the mandibular molars.57,58 The Forsus has shown similar results to elastics and has been deemed an acceptable substitute to inter-arch elastics.57 20 Purpose One of the many goals in orthodontic treatment is to finish the patient with a balanced facial profile. Orthodontic treatment does not solely change the shape of the nose and chin, but because of the close proximity the lips are with their dentoalveolar counterparts, the lips can be modified greatly with orthodontic treatment. Researchers have attempted to study the changes of lips when teeth are proclined in Class II, division 2 malocclusions but few have compared the results with a control sample of the same malocclusion and even fewer have looked at cases treated by non-extraction therapy. The purpose of this study is to provide the orthodontist with data useful in determining the skeletal, dentoalveolar, and soft tissue changes in Class II, division 2 malocclusions treated by non-extraction therapy. 21 References 1. Angle EH. Treatments of Malocclusion of the Teeth. 7th ed. Philadelphia: SS White Dent Mfg Co; 1907. 2. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972;62:296–309. 3. Massler M, Frankel JM. Prevalence of malocclusion in children aged 14 to 18 years. Am J Orthod. 1951;37:751–68. 4. Ast DB, Carlos JP, Cons NC. The prevalence and characteristics of malocclusion among senior high school students in upstate New York. Am J Orthod. 1965;51:437–45. 5. Kelly JE. An assessment of the occlusion of the teeth of youths 12-17 years. Vital Health Stat 11. 1977;162:1–65. 6. Taylor AT. A study of the incidence and manifestations malocclusion and irregularity of the teeth. D J Australia. 1935;7:650. 7. Altemus LA. Frequency of the incidence of malocclusion in American Negro children aged twelve to sixteen. Angle Orthod. 1959;29:189–200. 8. Steigman S, Kawar MJ, Zilberman Y. Prevalence and severity of malocclusion in Israeli Arab urban children 13 to 15 years of age. Am J Orthod. 1983;84:337–43. 9. Perng C, Lin J. Preliminary study of malocclusion of pedodontic patients in Veterans General Hospital. Taiwan Clin Dent. 1983;3:19–26. 10. Markovic MD. A genetic study of Class II, division 2 malocclusions. Eur J Orthod. 2000;22:453–4. 11. De Bruyne I. Prevalence and characteristics of malocclusion in a Belgian orthodontic population. Eur J Orthod. 2000;22:575. 12. Strang RH. Class II, division 2 malocclusion. Angle Orthod. 1958;28:210–4. 22 13. Graber TM. The “three m’s”: muscles, malformation, and malocclusion. Am J Orthod. 1963;49:418–50. 14. Eastern Component Group. A clinical study of cases of malocclusion in Class II, division 2. Angle Orthod. 1935;5:87–106. 15. Hedges RB. A cephalometric evaluation of Class II, division 2. Angle Orthod. 1958;28:191–7. 16. Peck S, Peck L, Kataja M. Class II, division 2 malocclusion: a heritable pattern of small teeth in well-developed jaws. Angle Orthod. 1998;68:9–20. 17. Beresford J. Tooth size and class distinction. Dental Pract. 1969;20:113–20. 18. Robertson NR, Hilton R. Features of the upper central incisors in Class II, division 2. Angle Orthod. 1965;35:51–3. 19. Araujo EA, Souki MQ. Bolton anterior tooth size discrepancies among different malocclusion groups. Angle Orthod. 2003;73:307–13. 20. Delivanis HP, Kuftinec MM. Variation in morphology of the maxillary central incisors found in Class II, division 2 malocclusions. Am J Orthod. 1980;78:438–43. 21. McIntyre GT, Millett DT. Crown-root shape of the permanent maxillary central incisor. Angle Orthod. 2003;73:710–5. 22. Proffit WR, McGlone RE, Barrett MJ. Lip and tongue pressures related to dental arch and oral cavity size in Australian aborigines. J Dent Res. 1975;54:1161–72. 23. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978;48:175–86. 24. Lapatki BG, Mager AS, Schulte-Moenting J, Jonas IE. The importance of the level of the lip line and resting lip pressure in Class II, division 2 malocclusion. J Dent Res. 2002;81:323–8. 23 25. Lapatki BG, Klatt A, Schulte-Mönting J, Jonas IE. Dentofacial parameters explaining variability in retroclination of the maxillary central incisors. J Orofac Orthop. 2007;68:109–23. 26. Walkow TM, Peck S. Dental arch width in Class II, division 2 deep-bite malocclusion. Am J Orthod Dentofacial Orthop. 2002;122:608–13. 27. Proffit, WR. Contemporary Orthodontics. 4th ed. Saint Louis, MO: Mosby/ Elsevier; 2007. 28. Brezniak N, Arad A, Heller M, Dinbar A, Dinte A, Wasserstein A. Pathognomonic cephalometric characteristics of Angle Class II, division 2 malocclusion. Angle Orthod. 2002;72:251–7. 29. Bjork A. Variations in the growth pattern of the human mandible: longitudinal radiographic study by the implant method. J Dent Res. 1963;42:400–11. 30. Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5:1–46. 31. Fischer-Brandies H, Fischer-Brandies E, König A. A cephalometric comparison between Angle Class II, division 2 malocclusion and normal occlusion in adults. Br J Orthod. 1985;12:158–62. 32. Isik F, Nalbantgil D, Sayinsu K, Arun T. A comparative study of cephalometric and arch width characteristics of Class II, division 1 and division 2 malocclusions. Eur J Orthod. 2006;28:179–83. 33. Al-Khateeb EA, Al-Khateeb SN. Anteroposterior and vertical components of Class II, division 1 and division 2 malocclusion. Angle Orthod. 2009;79:859–66. 34. Subtelny JD. The soft tissue profile, growth and treatment changes. Angle Orthod. 1961;31:105–22. 35. Bishara SE. Longitudinal soft-tissue profile changes: A study of three analysis. Am J Orthod. 1985;88:209–23. 24 36. Subtelny JD. A Longitudinal study of soft tissue facial structures and their profile characteristics, defined in relation to underlying skeletal structures. Am J Orthod. 1959;45:481–507. 37. Nanda RS, Meng H, Kapila S, Goorhuis J. Growth changes in the soft tissue facial profile. Angle Orthod. 1990;60:177–90. 38. Stellzig A, Basdra EK, Kube C, Komposch G. Extraction therapy in patients with Class II/2 malocclusion. J Orofac Orthop. 1999;60:39–52. 39. Hönn M, Schneider C, Dietz K, Godt A, Göz G. Treating Class II patients with removable plates and functional orthopedic appliances-the importance of anterior tooth inclination and direction of growth on treatment outcome. J Orofac Orthop. 2006;67:272–88. 40. Rains MD, Nanda R. Soft-tissue changes associated with maxillary incisor retraction. Am J Orthod. 1982;81:481–8. 41. Leaver SF. Incisor protraction, increased vertical facial height and their treatment effects on the soft tissue profile in a Class II division 2 malocclusion. MS Thesis – CADE, Saint Louis University 2002. 42. Grieve GW. The most difficult problem in orthodontia--the elimination of the deep overbite. Dental Cosmos. 1928;19:704–7. 43. Mershon JV. Possibilities and limitations in the treatment of closed-bites. Int J Orthod Oral Surg. 1937;23:581–9. 44. Prakash P, Margolis, HI. Dento-Craniofacial relations in varying degrees of overbite. Am J Orthod. 1952;38:657–73. 45. Burstone CR. Deep overbite correction by intrusion. Am J Orthod. 1977;72:1–22. 46. Ball JV, Hunt NP. The effect of Andresen, Harvold, and Begg treatment on overbite and molar eruption. Eur J Orthod. 1991;13:53–8. 25 47. Otto RL, Anholm JM, Engel GA. A comparative analysis of intrusion of incisor teeth achieved in adults and children according to facial type. Am J Orthod. 1980;77:437–46. 48. Parker CD, Nanda RS, Currier GF. Skeletal and dental changes associated with the treatment of deep bite malocclusion. Am J Orthod Dentofacial Orthop. 1995;107:382–93. 49. Dake ML, Sinclair PM. A comparison of the Ricketts and Tweed-type arch leveling techniques. Am J Orthod Dentofacial Orthop. 1989;95:72–8. 50. Demisch A, Ingervall B, Thüer U. Mandibular displacement in angle Class II, division 2 malocclusion. Am J Orthod Dentofacial Orthop. 1992;102:509–18. 51. Talass MF, Talass L, Baker RC. Soft-tissue profile changes resulting from retraction of maxillary incisors. Am J Orthod Dentofacial Orthop. 1987;91:385–94. 52. Ellen EK, Schneider BJ, Sellke T. A comparative study of anchorage in bioprogressive versus standard edgewise treatment in Class II correction with intermaxillary elastic force. Am J Orthod Dentofacial Orthop. 1998;114:430–6. 53. Nelson B, Hansen K, Hägg U. Class II correction in patients treated with Class II elastics and with fixed functional appliances: a comparative study. Am J Orthod Dentofacial Orthop. 2000;118:142–9. 54. Remmer KR, Mamandras AH, Hunter WS, Way DC. Cephalometric changes associated with treatment using the activator, the Fränkel appliance, and the fixed appliance. Am J Orthod. 1985;88:363–72. 55. Beckwith FR, Ackerman RJ Jr, Cobb CM, Tira DE. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;115:439–47. 56. Skidmore KJ, Brook KJ, Thomson WM, Harding WJ. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;129:230–8. 26 57. Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus resistant device versus intermaxillary elastics. Angle Orthod. 2008;78:332–8. 58. Aras A, Ada E, Saracoğlu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–25. 27 CHAPTER 3: JOURNAL ARTICLE Abstract Objective: To better understand skeletal, dentoalveolar, and soft tissue changes in treated Class II, division 2 malocclusions compared to an untreated matched control group. Materials and Methods: A study group of 29 cephalograms of Class II, division 2 subjects treated by nonextraction therapy, full appliances, and the use of the Forsus appliance were compared to a control sample of Class II, division 2 untreated patients matched for age and sex. Pretreatment (T1) and post treatment (T2) cephalograms were analyzed. An x-y reference plane of SN-7 (x-axis) and a line perpendicular to this passing through sella (y-axis) was used. A total of 30 variables (27 measurements and 3 angular) were evaluated and independent t-tests of the changes between the treated and untreated groups were performed. Results: Vertical facial height did not change with treatment. In the treated group maxillary and mandibular incisors were proclined significantly, 12.3 and 11.3 degrees respectively, however the upper lip showed a decrease in protrusion while the lower lip showed significantly more protrusion. Overbite was reduced from 6.3 mm to 2.5 mm and the mandibular plane angle did not change with treatment. Conclusions: 28 Compared with the untreated control sample, anterior vertical facial height did not change with treatment, the maxillary and mandibular central incisors were proclined significantly with treatment, the SN to GoGn angle did not change with orthodontic treatment, and the treatment effect was limited to the lower lip. Overbite was corrected by relative intrusion of the maxillary and mandibular central incisors, as well as by proclination of the maxillary and mandibular central incisors. Literature Review One of the many goals with orthodontic treatment is to finish the patient with a balanced facial profile. Orthodontic treatment cannot solely change the shape of the nose and chin. However, the lips, primarily in the vermillion area, are positioned in close correlation to the underlying dental and alveolar structures.1 Therefore, the lips can be modified greatly with orthodontic treatment.1 In 1907 Angle classified the types of malocclusion.2 Among them is a division of Class II where the incisors are consistently upright and there is a deep overbite. Often, in a Class II, division 2 malocclusion two goals of treatment are to 1) procline the maxillary and mandibular incisors and 2) correct the deep bite. 29 The correction of these two problems cause changes in the position of the lips.3–6 Researchers have attempted to study the changes of lips when teeth are proclined in Class II, division 2 malocclusions, but few have compared the results with an untreated control sample of the same malocclusion and even fewer have looked at cases treated by non-extraction therapy.3,5–9 Several lines of reference have been developed in order to study how, through orthodontic treatment, lips change with treatment. The Z-angle, H-angle, E-line, and S-line are some of the many references commonly used in orthodontic literature to evaluate profile and soft tissue changes.7,10 Much of the research done today compares changes in lips relative to these lines of reference. But all these lines use the nose and chin to relate how the lips are moving throughout orthodontic treatment. A problem that arises, is the nose and chin are continually growing and concern as to whether these planes should be used to measure lip changes has risen.10 Recently, Buschang et al has concluded an SN-7 x-y reference plane more accurately reflects the magnitude of change in the lips.10 A study by Leaver used this SN-7 reference plane to compare soft tissue changes in extraction verse non-extraction Class II, division 2 patients.6 30 Tadic and Woods used a similar x-y reference plane to look at soft tissue thickness in Class II, division 1 and 2 extraction patients.11 However, neither of these two studies had available a control sample of untreated Class II, division 2 patients to compare with. There is a need in the literature for a study that uses an SN-7 x-y reference plane and an untreated control sample to compare changes in Class II, division 2 malocclusions which have occurred due to full appliance orthodontic treatment. Materials and Methods Treated Sample A sample of 29 Class II, division 2 patients between the ages of 11 and 17 were selected. All were treated by non-extraction and had a Forsus for the correction of the anteroposterior discrepancy. male and 20 female. Of the 29 patients nine were Twenty-three were treated by the same orthodontist and the remaining six came from the files at Saint Louis University Center for Advanced Dental Education. All were treated in a single phase of treatment only and had never worn orthodontic appliances prior to the start of this study. The start (T1) cephalogram was taken 31 within one month of having the full maxillary and mandibular appliances placed. After leveling and aligning the teeth, and while still in full appliances a Forsus appliance was placed from the distal of the mandibular canines to the maxillary first molars. When the anteroposterior correction was resolved the Forsus appliance was removed and treatment continued until the orthodontic practitioner deemed treatment complete, at which time all appliances were removed and the final (T2) cephalogram was taken. All cephalograms had to show good soft tissue definition and contain all of the landmarks necessary for the analysis in order to be included in this study. Untreated Control Sample The untreated Class II, division 2 sample consisted of 18 subjects, nine male and nine female, all of which were from the Human Growth Study of the University of Montreal. All had cephalograms taken yearly starting at age 11 and ending at age 17. Two cephalograms, a (T1) and (T2) were matched with the age and sex of the treated samples pre (T1) and post (T2) treatment times. The overall average age of the treated and untreated samples were also matched 32 (Table 3.1). The untreated subjects were selected based on Class II, division 2 malocclusion, no prior orthodontic treatment, no orthodontic treatment during the years of cephalogram recordings, and no major craniofacial anomalies. Table 3.1 Group Untreated Treated Age and gender distribution of study sample Males:Females 9:9 9:20 T1 age Mean Age ± SD (Range) 13.0 ± 1.0 (11y-14y) 12.96 ± 1.0 (11y1m-14y9m) T2 age Mean Age ± SD (Range) 15.56 ± 1.0 (14y-17y) 15.45 ± 0.9 (13y9m-16y9m) Methodology For each of the cephalograms, 18 hard and soft tissue anatomical landmarks were located. Their definitions are in table 3.2 and a diagram of their corresponding location is seen in figure 3.1. These landmarks were traced for both the untreated and treated samples at both time points (T1 and T2), then digitized using Dentofacial Planner 7.0 software. 33 Table 3.2 Landmarks and Definitions. Abbreviation Gn Landmark Gnathion Gn’ Soft Tissue Gnathion Gonion Go L1 LL Lmf Mandibular Incisor Incisal Edge Mandibular Central Incisor Apex Lower Lip Labiomental Fold Me Menton N Nasion Pog Pogonion Pog’ Soft Tissue Pogonion Pronasale Subnasale L1a Prn Sbn S Sls Sella Superior Labial Sulcus U1 Maxillary Incisor Incisal Edge Maxillary Central Incisor Apex Upper Lip U1a UL Definition The most anterior and inferior midline point on the external contour of the symphysis of the mandible The most anterior and inferior point on the contour of the chin The point on the curvature of the mandible located by bisecting the angle formed by the lines tangent to the posterior ramus and the inferior border of the mandible The incisal tip of the mandibular central incisor The root tip of the mandibular central incisor The most anterior part of the lower lip The deepest point in the concavity between labrale inferius and soft tissue pogonion The most inferior midline point on the symphyseal outline of the mandible The most anterior point of the frontonasal suture The most prominent or anterior point on the symphysis of the mandible in the median plane. The most anterior point on the contour of the chin Most anterior point on the nasal tip The point where the lower margin of the nasal septum is confluent with the integumental upper lip The center of the pituitary fossa The deepest point in the concavity of the upper lip, midway between subnasale and labrale superius The incisal tip of the maxillary central incisor The root tip of the maxillary central incisor The most anterior point on the upper lip 34 Figure 3.1 Landmarks located Within Dentofacial Planner, two reference planes were constructed in order to create an x-y coordinate grid. A horizontal line was created parallel to the sella-nasion line minus 7 degrees (SN-7) and a vertical line was created perpendicular to this line (SN-7) passing through the landmark sella. This is diagrammed in Figure 3.2. 35 Figure 3.2 Reference Planes The measurements were broken up into (1) vertical soft and hard tissue, (2) horizontal soft and hard tissue, and (3) angular measurements as explained in Figures 3.3 to 3.7 below. 36 Figure 3.3 Vertical soft tissue measurements Figure 3.4 Vertical hard tissue measurements 37 Figure 3.5 Horizontal soft tissue measurements Figure 3.6 Horizontal hard tissue measurements 38 Figure 3.7 Angular measurements and vertical facial height The U1-SN (U1 to SN) refers to the angle where a line drawn through the long axis of the maxillary central incisor intersects with a line connecting landmarks sella and nasion. The L1-GoGn (L1 to GoGn) refers to the angle made when a line drawn through the long axis of the manidubular central incisor intersects with the mandibular plane. For this study, the mandibular plane is a line connecting landmarks gonion and gnathion. Magnification was considered for both samples. All cephalograms in the untreated control sample were taken using the same machine and values were multiplied by a 39 correction factor of .89 to account for magnification. For the treated sample, there were two separate cephalogram machines used. At the time of exposure, a 50 mm ruler was placed next to the patient’s head which subsequently was included in the radiograph. The 50 mm ruler was measured on each of the treated patient’s cephalograms and the machine’s magnification calculated. For the treated group, a correction factor of .90 and .76 were equated and corresponding measurements were multiplied based on the machine used to take that individual cephalogram. The correction factors were used to give all measurements in the treated and untreated groups a 0% enlargement (i.e. life size). Since magnification does not affect angular measurements, all angles in both the treated and untreated group in this study were excluded from being multiplied by a correction factor. Statistical Analyses All measurements were done on both group’s T1 and T2 cephalograms. Descriptive data was obtained and statistical analysis was performed using the Statistical Package for the Social Science (SPSS) version 20 (IBM). Independent t-tests were performed with a set significance level of p≤.05 to appraise the difference between groups at 40 T1 and T2 and change scores between groups. Soft tissue pronasale and gnathion were taken out of the results section due to their small sample size. be found in table A.1 of the appendix. Their values can For accuracy, ten (33%) randomly chosen cephalograms from the treated group were chosen and at a separate time retraced. To account for human error the measurements and angles for the ten cephalograms were compared to the original measurements and a method error was calculated. The method error ranges from .28 mm to .71 mm for linear measurements and .34 to 1.42 degrees for angular measurements. Subnasale was the least consistent location with the largest vertical and horizontal discrepancy. None of the method error measurements, including subnasale, were found to be statistically significant. In table 3.3 below are the systematic probability and method error results. 41 Table 3.3 Method error results Error Hard Tissue Soft Tissue Hard Tissue Soft Tissue Angular Changes Vertical Measurements Horizontal Measurements Variable Systematic Probability 0.49 0.62 0.51 0.90 0.74 0.90 0.66 0.79 0.75 0.96 0.93 0.35 0.77 0.62 0.62 0.47 0.57 0.82 0.45 0.45 0.76 0.67 0.11 Maxillary Central Mandibular Central Pogonion Gnathion Menton Subnasale Superior Labial Sulcus Upper Lip Lower Lip Labiomental Fold Pogonion Maxillary central Mandibular central Pogonion Gnathion Menton Overbite Subnasale Superior Labial Sulcus Upper Lip Lower Lip LabiomentalFold Pogonion Method Error 0.39 0.51 0.50 0.47 0.57 0.65 0.28 0.39 0.39 0.41 0.50 0.39 0.49 0.55 0.42 0.43 0.36 0.71 0.34 0.34 0.55 0.53 0.70 mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm mm U1 to SN 0.40 0.95 degrees L1 to GoGn 0.50 1.42 degrees SN to GoGn 0.22 0.35 degrees 42 Results Horizontal Measurements There were three measurements in the horizontal axis that showed significant changes (p≤.05): maxillary central incisors, mandibular central incisors, and the lower lip. The items with the least amount of change were menton and subnasale. Table 3.4 Details are below in Table 3.4. Changes in cephalometric horizontal measurements Horizontal Changes Group Treated (in millimeters) Control (in millimeters) Soft Tissue Hard Tissue Variable Mean SD Mean SD Maxillary Central 2.83 2.17 1.31 2.14 Mandibular Central 3.98 1.97 1.33 2.17 Pogonion 2.58 2.19 2.04 3.22 Gnathion 2.56 2.24 2.19 3.31 Menton 2.23 2.31 2.43 3.21 Subnasale 2.14 2.49 2.30 2.66 Superior Labial Sulcus 1.56 2.19 2.34 2.58 Upper Lip 1.77 2.54 2.36 2.96 Lower Lip 2.82 2.25 1.24 2.81 Labiomental Fold 2.84 2.04 1.57 2.94 Pogonion 2.69 2.15 2.18 3.82 Bold*= Statistically significant (prob ≤.05) change over time 43 Group Difference Sig. <.03* <.01* .50 .65 .80 .83 .29 .48 .05* .11 .61 Vertical Measurements There were four measurements in the vertical axis that showed significant changes (p≤.05): maxillary central incisors, mandibular central incisors, overbite, and subnasale. The item with the least amount of change was soft tissue pogonion. Table 3.5 Details are below in Table 3.5. Changes in cephalometric vertical measurements Vertical Changes Group Treated (in millimeters) Control (in millimeters) Soft Tissue Hard Tissue Variable Mean SD Mean SD Maxillary Central 1.36 1.98 2.85 2.16 Mandibular Central 5.20 1.74 2.73 2.17 Pogonion 4.17 2.87 5.12 3.97 Gnathion 4.43 2.98 4.77 3.79 Menton 4.70 3.10 5.21 3.92 Overbite -3.86 1.30 0.09 0.79 Subnasale 1.43 1.98 2.66 1.67 Superior Labial Sulcus 2.13 2.16 3.04 1.91 Upper Lip 1.85 2.01 2.62 2.04 Lower Lip 3.57 2.70 3.30 2.82 Labiomental Fold 3.93 2.28 4.15 2.78 Pogonion 5.03 3.27 4.76 4.64 Bold*= Statistically significant (prob ≤.05) change over time 44 Group Difference Sig. <.02* <.01* .35 .74 .62 <.01* <.05* .16 .22 .76 .79 .82 Angular Measurements Two of the three angular measurements calculated in this study showed a significant change (p≤.05): U1 to SN, and L1 to GoGn. The third angle measured, SN to GoGn showed a minimal change between T1 and T2 for both the control and the treated sample. Details are below in Table 3.6. Table 3.6 Changes in cephalometric angular values Angular Changes Group Treated (in degrees) Control (in degrees) Group Difference Variable Mean SD Mean SD U1 to SN 12.33 7.70 -1.04 3.81 L1 to GoGn 11.29 7.79 0.22 4.68 SN to GoGn -0.77 1.97 -0.82 2.76 Bold*= Statistically significant (prob ≤.05) change over time 45 Sig. <.01* <.01* .94 In figure 3.8 below is a scale drawing comparing changes between the two groups. Descriptive statistics for all measurements can be found in tables A.2 to A.4 in the appendix section. Figure 3.8 Changes from T1 to T2 for the untreated control (left) and treated (right/dotted lines) groups 46 Discussion Hard Tissue The maxillary central incisors moved 1.52 mm forward with treatment. The total forward distance the maxillary central incisors moved with treatment was 2.83 mm. This is consistent with Leaver that found 3.88 mm total forward movement in non-extraction treatment.6 The maxillary central incisors had a significantly less vertical movement with treatment, implying that a relative intrusion of the maxillary central incisors had occurred. This is not consistent with Aras et al who found that with the use of the Forsus maxillary incisor extrusion occured.12 The mandibular central incisors moved forward 2.65 mm more with treatment. This is consistent with mandibular incisor proclination seen with use of the Forsus.12 In this study the mandibular central incisors total forward movement of 3.98 mm is larger than the change of 2.57 mm Leaver found in their non-extraction treatment group.6 Vertically, the mandibular central incisors had a significant amount of relative intrusion with treatment. They relatively intruded 2.47 mm more than the control sample. This helped with correction of the overbite in the treated group. The use of the Forsus in the treated group may have aided in the relative intrusion as other studies 47 have found mandibular incisor intrusion with use of the Forsus.12 Vertical facial height increased in both groups as was expected with growth during the years of 11 to 17. There was no significant change in vertical facial height between the control and the treated sample, but the increase was less in the treated sample. Parker et al did find a 2.0 mm larger increase in vertical facial height with treatment than this study did.8 In Leaver’s study, the Forsus was not used and the non-extraction vertical facial height change was a difference of only 0.2 mm compared with this study. Leaver had a 4.9 mm change, whereas this study had a 4.7 mm change.6 Regarding the overbite, an increase in vertical facial height as a cause for overbite correction can be ruled out since there was no significant change in vertical facial height with treatment. The deep bite therefore was corrected by relative intrusion of the maxillary and mandibular central incisors and also by proclination of the maxillary and mandibular central incisors. Hard tissue pogonion, gnathion, and menton did not show a significant change in horizontal and vertical measurements between groups. All these points showed normal changes that are consistent with growth. 48 Soft Tissue The upper lip had less protrusion with treatment, even though the maxillary central incisors were proclined 12.33 degrees with treatment. With treatment, there was a non-significant change of 0.59 mm less forward movement in the upper lip. This may have been caused by the fact that in Class II, division 2 malocclusions the maxillary lateral incisors are more proclined prior to treatment than the central incisors. Another way of saying this is the upper lip does not come forward with proclination of maxillary central incisors because at the start of treatment the lateral incisors are already positioned near the place the central incisors will eventually end. However, a conclusion of this cannot be made from this study as the changes in the maxillary lateral incisors were not recorded. It would be expected that if the maxillary incisors were proclined 12.3 degrees than the upper lip would increase more than was found in this study. Talass et al contributes the low degree of predictability found in the upper lip to a result of the complex anatomy and dynamics of the upper lip.5 In the untreated control group, the upper lip had more protrusion over time, whereas in the treated group the upper lip had marked retrusion over time. 49 Rains and Nanda found the upper lip to be responsive to maxillary incisor movement in treatments using extractions and anterior retraction.4 In this study, even though non-extraction treatment was used, the upper lip responded to maxillary central incisor proclination by retracting slightly. The lower lip responds to non-extraction treatment with no change vertically but a large change horizontally. Forward movement of the lower lip increased by a statistically significant 1.58 mm with treatment. Total forward movement in the treated sample was 2.82 mm which is larger than the 0.72 mm forward movement Leaver found in non-extraction treatment.6 To conclude the large change in lower lip protrusion with treatment as a result of mandibular incisor proclination is difficult since Leaver and this study had similar mandibular incisor proclination but differing lower lip protrusion. Subnasale did not change horizontally with treatment, but did have a statistically less vertical movement with treatment in this study. The cause is difficult to say as subnasale had a large method error calculation, implying that there may have been more error in the treated group with locating this landmark. 50 The labiomental fold, soft tissue pogonion, and gnathion moved forward and downward consistently in both groups, which is consistent with a natural downward and forward growth. Angular Changes The SN to GoGn angle had no changes with or without treatment. The angular measurements of U1 to SN and L1 to GoGn showed a significant increase in proclination with treatment. These are expected as other studies have also seen an increase in these angles with treatment. This study found a mean change in L1 to GoGn of 11.29 degrees with treatment, which is similar to the 11.07 degree change Leaver found with non-extraction treatment.6 This study’s findings were not consistent with what Parker et al found in their study, which was a mean change of 7.9 degrees.8 But Parker et al’s results mixed both extraction (11 patients) and non-extraction (34 patients) Class II, division 2 together.8 Leaver and Parker et al did use a different mandibular plane (lower border of the mandible) than this study (Go to Gn) which has to be taken into consideration and will account for a small amount of difference. 51 The U1 to SN increased 12.33 degrees in this study, which is only slightly less than the 14.66 degrees seen in Aras et al’s study and the 14.01 degrees found in Leaver’s study.6,12 Conclusions According to the results of this study, Class II, division 2 subjects between the ages of 11-17 years of age who were treated with non-extraction therapy and who all used the Forsus for anteroposterior correction presented with the following: Skeletal 1) Compared with the untreated control sample, anterior vertical facial height did not change with treatment. 2) The SN to GoGn angle did not change with orthodontic treatment. 52 Dentoalveolar 3) Compared to the untreated control sample, maxillary and mandibular central incisors were proclined significantly during treatment. 4) Overbite was corrected by relative intrusion of the maxillary and mandibular central incisors, as well as by proclination of the maxillary and mandibular central incisors. Soft Tissue 5) Compared to the untreated control sample, treatment effect was limited to the lower lip. 53 References 1. Subtelny JD. The soft tissue profile, growth and treatment changes. Angle Orthod. 1961;31:105–22. 2. Angle EH. Treatments of Malocclusion of the Teeth. 7th ed. Philadelphia: SS White Dent Mfg Co; 1907. 3. Hönn M, Schneider C, Dietz K, Godt A, Göz G. Treating Class II patients with removable plates and functional orthopedic appliances-the importance of anterior tooth inclination and direction of growth on treatment outcome. J Orofac Orthop. 2006;67:272–88. 4. Rains MD, Nanda R. Soft-tissue changes associated with maxillary incisor retraction. Am J Orthod. 1982;81:481–8. 5. Talass MF, Talass L, Baker RC. Soft-tissue profile changes resulting from retraction of maxillary incisors. Am J Orthod Dentofacial Orthop. 1987;91:385–94. 6. Leaver SF. Incisor protraction, increased vertical facial height and their treatment effects on the soft tissue profile in a Class II division 2 malocclusion. MS Thesis – CADE, Saint Louis University 2002. 7. Stellzig A, Basdra EK, Kube C, Komposch G. Extraction therapy in patients with Class II/2 malocclusion. J Orofac Orthop. 1999;60:39–52. 8. Parker CD, Nanda RS, Currier GF. Skeletal and dental changes associated with the treatment of deep bite malocclusion. Am J Orthod Dentofacial Orthop. 1995;107:382–9. 9. Remmer KR, Mamandras AH, Hunter WS, Way DC. Cephalometric changes associated with treatment using the activator, the Fränkel appliance, and the fixed appliance. Am J Orthod. 1985;88:363–72. 10. Buschang PH, Fretty K, Campbell PM. Can commonly used profile planes be used to evaluate changes in lower lip position. Angle Orthod. 2011;81:557–63. 54 11. Tadic N, Woods MG. Incisal and soft tissue effects of maxillary premolar extraction in Class II treatment. Angle Orthod. 2007;77:808–16. 12. Aras A, Ada E, Saracoğlu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–25. 55 Appendix Table A.1 Changes in soft tissue pronasale and gnathion Horizontal and Vertical Changes Group Variable Treated (in millimeters) Mean SD Control (in millimeters) Mean SD Horizontal Pronasale 3.51 2.96 1.13 Measurements Gnathion 2.54 2.26 -0.57 Vertical Pronasale 1.55 1.55 1.42 Measurements Gnathion 4.91 3.17 2.98 Bold*= Statistically significant (prob ≤.05) change over 56 0.33 0.89 0.92 1.76 time Group Difference Sig. <.01* <.01* .88 .25 Table A.2 Horizontal descriptive statistics Horizontal (in millimeters) Group Treated Time Variable Soft Tissue Hard Tissue Maxillary Central Mandibular Central Pogonion Gnathion Menton Pronasale Subnasale Superior Labial Sulcus Upper Lip Lower Lip Labiomental Fold Pogonion Gnathion n= sample size Control T1 T2 T1 T2 n Mean SD Mean SD n Mean SD Mean SD 29 29 29 29 29 29 29 29 29 29 29 29 29 65.38 61.64 58.39 56.98 53.50 93.28 80.40 78.04 80.14 75.70 67.61 69.52 66.85 5.25 4.54 5.65 5.65 5.69 3.46 3.69 4.07 4.28 4.48 5.08 6.05 6.61 68.22 65.61 60.97 59.54 55.72 96.79 82.54 79.60 81.91 78.52 70.45 72.22 69.39 4.67 4.68 5.96 6.03 5.94 5.02 4.81 4.78 5.10 5.27 5.43 6.56 6.94 18 18 18 18 18 4 15 17 17 14 14 18 4 64.72 62.03 59.43 56.73 52.82 89.94 78.97 77.72 80.27 76.96 69.42 71.24 69.97 4.24 4.13 5.06 5.12 5.00 3.35 3.21 4.11 4.75 5.54 4.65 5.18 5.73 66.02 63.37 61.48 58.92 55.26 93.18 80.95 79.43 81.93 78.11 70.80 73.42 72.03 4.67 4.24 6.19 6.43 6.44 4.98 4.17 4.31 4.47 5.33 4.95 6.48 7.92 57 Table A.3 Vertical descriptive statistics Vertical(in millimeters) Group Treated Time Variable Soft Tissue Hard Tissue Maxillary Central Mandibular Central Pogonion Gnathion Menton Overbite Pronasale Subnasale Superior Labial Sulcus Upper Lip Lower Lip Labiomental Fold Pogonion Gnathion n= sample size Control T1 T2 T1 T2 n Mean SD Mean SD n Mean SD Mean SD 29 29 29 29 29 29 29 29 29 29 29 29 29 29 74.09 67.78 96.80 100.39 102.67 6.31 41.05 52.31 59.38 64.65 76.19 84.20 93.57 101.40 4.82 4.25 5.71 5.87 5.99 1.43 4.04 4.16 5.10 4.87 5.14 5.04 5.99 6.26 75.44 72.98 100.97 104.82 107.37 2.45 42.60 53.74 61.51 66.50 79.75 88.13 98.60 106.31 4.23 4.30 6.02 6.24 6.37 0.64 3.83 3.73 4.73 4.77 4.87 5.04 6.07 1.18 18 18 18 18 18 18 4 15 17 17 14 14 18 4 64.71 59.33 91.68 94.64 94.31 5.40 32.70 41.89 48.03 55.61 66.64 74.85 88.83 91.02 3.79 3.64 6.09 5.99 5.98 1.25 2.12 2.46 3.02 3.02 4.64 5.04 5.40 5.09 67.56 62.06 96.80 99.41 99.52 5.49 34.93 44.02 50.81 58.02 69.52 78.42 93.59 94.15 4.69 4.55 7.85 7.53 7.72 1.43 2.29 2.36 3.10 3.64 4.85 5.26 6.18 4.49 58 Table A.4 Angular descriptive statistics Angles (in degrees) Group Treated Time Angles Variable T1 n Mean Control T2 SD T1 Mean SD n T2 Mean SD Mean SD U1 to SN 29 94.86 9.86 107.19 6.48 18 96.79 6.10 95.76 5.61 L1 to GoGn 29 98.89 8.23 110.19 8.55 18 91.39 7.36 91.61 7.89 SN to GoGn 29 27.41 4.24 26.65 4.87 18 30.71 4.37 29.88 4.97 n= sample size 59 Vita Auctoris Alan Larkin was born in Las Vegas, Nevada to Mark and Lou Ann Larkin. He is the third of four children. He was raised in Las Vegas and graduated from Green Valley High School. He attended Brigham Young University in Utah for one year prior to serving a proselytizing mission for The Church of Jesus Christ of Latter-day Saints in Seoul, Korea for two years. Upon completion of his missionary work he returned to Brigham Young University and later earned his Bachelor of Science degree in Biology. He then attended the University of Louisville Dental School in Louisville, Kentucky where he graduated Magna Cum Laude with his Doctor of Dental Medicine degree. Dr. Larkin expects to receive a Master of Science in Dentistry degree from Saint Louis University in December of 2012. He and his wife are the proud parents of five wonderful children. 60