Charnley low-frictional torque arthroplasty in patients under the age
advertisement

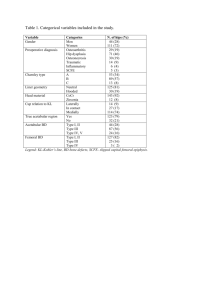
Charnley low-frictional torque arthroplasty in patients under the age of 51 years FOLLOW-UP TO 33 YEARS B. M. Wroblewski, P. D. Siney, P. A. Fleming From Wrightington Hospital, Wigan, England etween November 1962 and December 1990 a group of 1092 patients, 668 women and 424 men, under the age of 51 years at the time of surgery, underwent 1434 primary Charnley low-frictional torque arthroplasties and are being followed up indefinitely. Their mean age at operation was 41 years (12 to 51). At the latest review in June 2001 the mean follow-up had been for 15 years 1 month. Of the 1092 patients 54 (66 hips) could not be traced, 124 (169 hips) were known to have died and 220 (248 hips) had had a revision procedure. At a mean follow-up of 17 years and 5 months, 759 patients (951 hips) are still attending. In this group satisfaction with the outcome is 96.2%. The incidence of deep infection for the whole group was 1.67%. It was more common in patients who had had previous surgery (hemi- and total hip arthroplasties excluded), 2.2% compared with 1.5% in those who had not had previous surgery, but this difference was not statistically significant (p = 0.4). There were fewer cases of deep infection if gentamicin-containing cement was used, 0.9% compared with 1.9% in those with plain acrylic cement, but this was not also statistically significant (p = 0.4). There was a significantly higher rate of revision in patients who had had previous hip surgery, 24.8% compared with 14.1% in those who had not had previous surgery (p < 0.001). At the latest review, 1.95% are known to have had at least one dislocation and 0.4% have had a revision for dislocation. The indication for revision was aseptic loosening of the cup (11.7%), aseptic loosening of the stem (4.9%), a fractured stem (1.7%), deep infection (1.5%) and dislocation (0.4%). B B. M. Wroblewski, FRCS, Professor of Orthopaedic Biomechanics, Consultant Orthopaedic Surgeon P. D. Siney, BA, Senior Research Fellow P. A. Fleming, Research Assistant The John Charnley Research Institute, Wrightington Hospital, Hall Lane, Appley Bridge, Nr Wigan WN6 9EP, UK. Correspondence should be sent to Professor B. M. Wroblewski. ©2002 British Editorial Society of Bone and Joint Surgery 0301-620X/02/410293 $2.00 540 With revision for any indication as the endpoint the survivorship was 93.7% (92.3 to 95.0) at ten years, 84.7% (82.4 to 87.1) at 15 years, 74.3% (70.5 to 78.0) at 20 years and 55.3% (45.5 to 65.0) at 27 years, when 55 hips remained ‘at risk’. J Bone Joint Surg [Br] 2002;84-B:540-3. Received 17 June 1999; Accepted after revision 12 October 2001 When Charnley introduced the low-frictional torque arthroplasty (LFA) into clinical practice he selected a group of patients who were to be followed up indefinitely. He initiated this prospective study in November 1962, when highmolecular-weight polyethylene (HMWPE) was first introduced as material for the socket. The series was closed 1 at the end of December 1965. Although popularly known as the ‘first 500’ it included all operations carried out during this period of 38 months. There were 905 primary LFAs: 426 were primary LFAs, 336 had a cemented stem with an uncemented metal-backed press-fit cup, 22 had a polytetrafluoroethylene (PTFE) cup with a cemented stem revised to an uncemented metal-backed cup and 121 had a PTFE cup revised to a cemented cup. With time as the numbers dwindled it became clear that a new group of younger patients had to be introduced prospectively. This 2 decision, taken in 1974, proved to be correct because when Charnley published his results at 12 to 15 years in 1979 only 77 LFAs (8.5%) of the original ‘first 500’ group 3 could be reviewed, and by 1983 only 42 (4.6%) remained. Patients and Methods Patients undergoing a Charnley LFA between November 1962 and December 1990 were included in an indefinite follow-up study in which the only criterion was age less than 50 years at the time of LFA. All revisions from hemiand total hip arthroplasties were excluded, as were the patients in whom either the design, material or surgical technique did not conform to the standard protocol as practised at that stage of the evolution of the operation. Routine follow-up was at three months and then annually, but with increasing follow-up and experience it was possible to ‘tailor’ the review for individual patients according THE JOURNAL OF BONE AND JOINT SURGERY CHARNLEY LOW-FRICTIONAL TORQUE ARTHROPLASTY IN PATIENTS UNDER THE AGE OF 51 YEARS 4,5 to the radiological appearances, the level of activity of 6 7 the patient or the rate of wear of the cup measured as 8 penetration. The clinical outcome was graded as described 9 by Merle d’Aubigné and Postel and modified by Charn10 ley. Over time a number of aspects became apparent. The collection and processing of the information were becoming a daunting task, and a dedicted unit, the John Charnley Research Institute, was established for the purpose. When the information revealed specific issues such as fracture of 11 7 the stem or wear of the cup and loosening, each resulting modification of materials, design or surgical technique became the basis of a separate prospective study requiring an increasing period of follow-up. Two further aspects of this study must be appreciated. First, the numbers in this group were dwindling and secondly the volume of information available could not be presented in either a single communication or in a simple form. We therefore present the clincal results and survivor12 ship analysis. Since we are continuing our policy of 13 advising early revision for failure we have used this as the endpoint in the survivorship analysis, defining it as exchange or removal of one or both components. The results are reliable since there remain, as recommended by 14 Lettin, Ware and Morris, more than 40 hips still at risk at the endpoint of the survivorship curve. Results There were 668 women and 424 men with a mean age of 41 years (12 to 51) and a mean weight of 65 kg (30 to 108). They had 1434 LFAs. Of the 342 patients (31.3%) who had bilateral LFAs, in 98 (9%) both hips had been replaced under the same general anaesthetic while in 244 (22.3%) both had been replaced by December 1990. The underlying pathology of the hip and the type of previous operations are shown in Table I. All LFAs had been carried out in a cleanair enclosure using total-body-exhaust suits, the development of which had been finalised in 1970. The transtrochanteric approach was used routinely. The surgeons carrying out the operations were recorded as Professor Sir John Charnley 13%, the senior author (BMW) 40%, and senior residents 47%. At the latest review in June 2001, the mean follow-up was 15 years 1 month. A total of 54 patients (4.9%, 66 LFAs, 4.6%) could not be traced, 124 (11.4%; 169 LFAs, 11.8%) were known to have died, 220 (20.1%; 248 LFAs, 17.3%) had had a revision and 759 (69.5%; 951 LFAs, 66.3%) continued to attend. The mean follow-up of the attending patients was 17 years 5 months. Clinical. Assessment at the latest follow-up, at the last follow-up before death or on readmission for a revision, has shown that 90.3% were satisfied with the outcome, 80.5% were free from pain and 9.8% had occasional discomfort. A total of 68% had normal or nearly normal function and 68.5% had a full or nearly full range of movement of the VOL. 84-B, NO. 4, MAY 2002 541 Table I. The underlying hip pathology (some patients had more than a single disorder) and previous hip surgery (excluding hemi- and total hip arthroplasty) in 1092 patients who had a Charnley LFA Number of hips Diagnosis Primary osteoarthritis Congenital dislocation/subluxation Perthes' disease Slipped upper femoral epiphysis Trauma Septic arthritis Chronic sepsis (tuberculosis) Quadrantic head necrosis Rheumatoid arthritis Ankylosing spondylitis Fractured neck of femur Paget's disease Fusion for unspecified pathology Protrusio acetabuli Unspecified Previous hip surgery None Osteotomy: femoral/pelvic Cup arthroplasty Open reduction Fusion/attempted fusion Pin, plate or screw fixation Other (soft-tissue procedures) Percentage 298 395 77 55 85 5 37 68 292 91 38 1 18 47 10 20.79 27.55 5.37 3.84 5.93 0.35 2.58 4.74 20.36 6.35 2.65 0.07 1.26 3.28 0.70 1164 139 15 42 36 4 78 81.17 9.69 1.05 2.93 2.51 0.28 5.44 Table II. Complications after 1434 Charnley low LFAs observed within one year of surgery, or during follow-up including revisions shown in Table III Number Complications of hips Percentage Within one year of surgery Local Haematoma Delayed wound healing Trochanteric nonunion Dislocation Infection General Deep-vein thrombosis (clinical) Pulmonary embolism (non-fatal) Cardiovascular Abdominal Urinary Other During follow-up Dislocation Deep infection Loose cup Loose stem Fractured stem Other (including trochanteric explorations) Unexplained pain 14 3 34 5 9 1.0 0.2 2.4 0.4 0.6 26 45 3 5 28 10 1.8 3.1 0.2 0.4 2.0 0.7 24 24 261 93 25 69 3 1.7 1.7 18.2 6.3 1.7 4.8 0.2 Table III. Indication for revision of a Charnley LFA. Some patients had more than a single indication for revision Number Indication of hips Percentage Infection 22 1.53 Dislocation 6 0.42 Loose cup 152 10.6 Loose stem 70 4.9 Fractured stem 22 1.7 Unexplained pain 2 0.14 Socket wear 15 1.1 Other (includes removal of trochanteric wires) 20 1.4 542 B. M. WROBLEWSKI, P. D. SINEY, P. A. FLEMING Table IV. Wear of the UHMWPE cup measured by penetration, migration and revision for aseptic loosening Cup penetration (mm) Number Number migrating % migrating Number revised % revised 0 73 0 0.0 0 0.0 0.1 to 1.0 754 108 14.3 42 5.5 1.1 to 2.0 261 76 29.1 33 12.6 2.1 to 3.0 195 71 36.4 36 18.5 Table V. Survivorship analysis of 1434 Charnley LFAs taking Follow-up Number (yrs) at start Withdrawn Failure 0 1434 0 0 1 1434 0 0 2 1434 27 3 3 1404 25 4 4 1375 13 5 5 1357 19 4 6 1334 23 10 7 1301 22 6 8 1273 26 16 9 1231 30 12 10 1189 37 20 11 1132 73 20 12 1039 64 16 13 959 58 24 14 877 66 8 15 803 82 15 16 706 59 22 17 625 64 7 18 554 56 9 19 489 67 8 20 414 55 10 21 349 44 4 22 301 53 4 23 244 54 6 24 184 57 5 25 122 26 0 26 96 28 4 27 64 18 3 28 43 13 3 29 27 9 0 30 18 7 0 31 11 7 0 32 4 2 0 33 2 0 0 34 2 2 0 hip. Of the 759 patients (951 LFAs) who have not had a revision, 96.2% are satisfied with the outcome, 88% are free from pain and 8.2% have occasional discomfort. A total of 78.7% have normal or nearly normal function and 75.7% have a full or nearly full range of movement. The complications within one year of surgery and those occurring during the period of follow-up including revisions are shown in Table II. Complications. Deep infection occurred in 24 LFAs (1.67%) and was slightly more common in patients who had had previous hip surgery (6/270; 2.2%) than in those who had not (18/1164; 1.55%); this was not significantly different (p = 0.4). Plain acrylic cement had been used in 1092 (76.2%) hips and deep infection occurred in 21 (1.9%); 20 (1.8%) have been revised. Gentamicin-containing cement had been used in 342 (23.8%) and deep infec- 3.1 to 4.0 91 43 47.3 21 23.1 4.1 to 5.0 40 24 60 13 32.5 5.1 to 6.0 10 5 50 3 30 revision for any reason as the endpoint Number Cumulative at risk success rate (%) 1434 100.00 1434 100.00 1420.5 99.79 1391.5 99.50 1368.5 99.14 1347.5 98.84 1322.5 98.08 1290 97.62 1260 96.35 1216 95.36 1170.5 93.65 1095.5 91.83 1007 90.24 930 87.66 844 86.71 762 84.74 676.5 81.49 593 80.31 526 78.60 455.5 76.84 386.5 74.25 327 73.03 274.5 71.57 217 68.81 155.5 65.59 109 65.59 82 60.71 55 55.26 36.5 47.04 22.5 47.04 14.5 47.04 7.5 47.04 3 47.04 2 47.04 1 47.04 6.1 to 7.0 10 7 70 4 40 95% confidence limits 100.00 to 100.00 100.00 to 100.00 99.55 to 100.00 99.13 to 99.87 98.65 to 99.62 98.27 to 99.41 97.35 to 98.81 96.80 to 98.44 95.33 to 97.36 94.21 to 96.52 92.30 to 95.00 90.27 to 93.38 88.50 to 91.98 85.68 to 89.64 84.58 to 88.84 82.39 to 87.09 78.85 to 84.13 77.44 to 83.18 75.49 to 81.70 73.45 to 80.24 70.50 to 78.01 68.92 to 77.14 67.06 to 76.09 63.70 to 73.92 59.55 to 71.64 58.37 to 72.82 52.48 to 68.95 45.49 to 65.03 35.94 to 58.15 32.90 to 61.19 29.42 to 64.66 22.54 to 71.54 8.30 to 85.78 0.00 to 94.49 0.00 to 100.00 tion occurred in three (0.9%), two of which have been revised (p = 0.2). Various methods of trochanteric re-attachment have been used. Trochanteric nonunion occurred in 34 LFAs (2.4%). There were no dislocations or revisions for dislocation in this group of patients. There were five dislocations (0.35%) within one year of surgery and none required revision. By the latest review 28 (1.95%) are known to have had at least one dislocation and six (0.42%) had been revised for dislocation. Other indications for revision are shown in Table III. Wear of the UHMWPE cup. Wear was measured as penetration using the method which has been previously 8 described. The mean rate of penetration for the whole group was 0.1 mm/year (0.01 to 0.67) and the mean total penetration was 1.4 mm (0.1 to 7). The correlation between THE JOURNAL OF BONE AND JOINT SURGERY CHARNLEY LOW-FRICTIONAL TORQUE ARTHROPLASTY IN PATIENTS UNDER THE AGE OF 51 YEARS 543 Fig. 1 Survivorship analysis of 1434 Charnley LFAs taking revision for any reason as the endpoint. the depth of penetration, the incidence of migration of the cup and revision for aseptic loosening of the cup is shown in Table IV. Survivorship analysis. Taking revision for any reason as the endpoint, the survivorship was 93.7% (92.3 to 95.0) at ten years, 84.7% (82.4 to 87.1) at 15 years, 74.3% (70.5 to 78.0) at 20 years, and 55.3% (45.5 to 60.5) at 27 years when 55 hips remained ‘at risk’ (Table V, Fig. 1). Discussion The long-term clinical results of the Charnley LFA remain excellent even in young patients. Consistency of materials, design and surgical technique, the availability of large numbers of patients with long-term follow-up and regular review have allowed a meaningful study of various parameters to be made and improvements to be introduced while continuing the clinical practice. In order to contribute to the understanding of the long-term results the selection of young patients for an indefinite follow-up was essential. Such a decision imposed demands on the skills of the surgeon and the durability of the arthroplasty and is probably the most severe test of both, since it inevitably involves patients whose level of activity and life expectation are high and includes a large percentage of patients with developmental disorders of the hip and rheumatoid arthritis. The long-term problem of wear and loosening of the cup 7 is highlighted. It is in this area that further progress is to be expected. A combination of ceramic and cross-linked 15 polyethylene gives excellent results at 12 years. If the rate of wear is reduced the effects of wear particles, as a possible cause of loosening of the component, may become of academic interest only. Two other aspects must be borne in mind when considering the clinical results. First, they may not reflect the 16 mechanical state of the arthroplasty, hence follow-up with radiographs of good quality and continuity of the methods used to record the data are essential. Secondly, the implant cannot be considered to become an integral part of the skeleton. The surgeon therefore has a continuing responsibility to monitor this as it changes with age. The surgeon must also understand patients’ expectations, the patient VOL. 84-B, NO. 4, MAY 2002 must accept the limitations of the operation and the system using the procedure as a measure of ‘quality of outcome’ must be prepared to accept its share of responsibility. This research was supported by the Peter Kershaw and John Charnley Trusts. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. References 1. Charnley J. Low friction arthroplasty of the hip: theory and practice. Berlin, etc: Springer-Verlag, 1979:20-90. 2. Wroblewski BM, Fleming PA, Hall RM, Siney PD. Stem fixation in the Charnley low friction arthroplasty in young patients using an intramedullary bone block. J Bone Joint Surg [Br] 1998;80-B:273-8. 3. Charnley J. Low friction arthroplasty of the hip: theory and practice. Springer-Verlag, Berlin, etc. 1979:42. 4. Pacheco V, Shelley P, Wroblewski BM. Mechanical loosening of the stem in Charnley arthroplasties: identification of the “at risk” factors. J Bone Joint Surg [Br] 1988;70-B:596-9. 5. Hodgkinson JP, Shelley P, Wroblewski BM. The correlation between the roentgenographic appearance and the operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop 1988;228:105-9. 6. Feller JA, Kay PR, Hodgkinson JP, Wroblewski BM. Activity and socket wear in the Charnley low-friction arthroplasty. J Arthroplasty 1994;9:341-5. 7. Wroblewski BM. Charnley low friction arthroplasty in patients under the age of 40 years. In: Sevastik J, Goldie I, eds. The young patient with degenerative hip disease. Stockholm: Almqvist & Wiksell, 1985:197-201. 8. Griffith MJ, Seidenstein MK, Williams D, Charnley J. Socket wear in Charnley low friction arthroplasty of the hip. Clin Orthop 1978;137:37-47. 9. Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg [Am] 1954;36-A:451-75. 10. Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg [Br] 1972;54-B:61-76. 11. Charnley J. Fracture of femoral prostheses in total hip replacement. Clin Orthop 1975;111:105-20. 12. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457-81. 13. Wroblewski BM. Revision surgery in total hip arthroplasty: surgical technique and results. Clin Orthop 1982;170:56-61. 14. Lettin AWF, Ware HS, Morris RW. Survivorship analysis and confidence intervals: an assessment with reference to the Stanmore total knee replacement. J Bone Joint Surg [Br] 1991;73-B:729-31. 15. Wroblewski BM, Siney PD, Fleming PA. Low-friction arthroplasty of the hip using alumina ceramic and cross-linked polyethylene: a tenyear follow-up report. J Bone Joint Surg [Br] 1999;81-B:54-5. 16. Wroblewski BM, Fleming PA, Siney PD. Charnley low-frictional torque arthroplasty of the hip: 20-30 year results. J Bone Joint Surg [Br] 1999;81-B:427-30.