Serotonin toxicity caused by the interaction of fentanyl and
advertisement

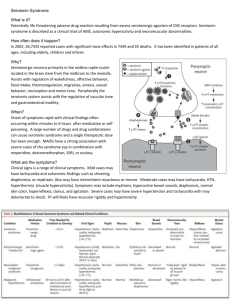
bs_bs_banner Emergency Medicine Australasia (2015) ••, ••–•• doi: 10.1111/1742-6723.12521 CASE LETTER Serotonin toxicity caused by the interaction of fentanyl and serotonergic medications Dear Editor, A 19-year-old woman was transferred to the ED from an external Day Procedure Unit having been emergently intubated following a tonic episode after elective general anaesthesia for molar extraction. Her past medical history included depression, and her regular medications were amitriptyline 25 mg, citalopram 60 mg and pantoprazole 20 mg. General anaesthesia was achieved with sevoflurane and iv fentanyl 75 mcg, propofol 125 mg and midazolam 2 mg with a laryngeal mask airway (LMA). During the case, the patient received iv kefazolin 1 g, dexamethasone 8 mg, paracoxib 40 mg and ondansetron 4 mg, and 15 mL 0.5% bupivocaine was infiltrated locally. On LMA removal post-procedure, she had generalised tonicity with jaw trismus, tachycardia (111/min), hypertension (172/83 mmHg) and oxygen saturations of 88% on room air. She was subsequently intubated with iv fentanyl 100 mcg, propofol 50 mg and rocuronium 50 mg. She received further iv fentanyl 80 mcg and rocuronium 20 mg, and a propofol infusion was commenced prior to transfer to the ED. On arrival in the ED, the patient was sedated with normal haemodynamics. She had signs of neuromuscular excitation with bilateral increased lower limb tone, hyperreflexic knee and ankle jerks with sustained ankle clonus. A computed tomography head scan was normal and an electroencephalogram 4 h after arrival demonstrated severe diffuse encephalopathy consistent with medication effect. The patient was managed in Intensive Care prior to an uneventful extubation, and she was discharged from hospital the following day. The patient’s clinical presentation was consistent with serotonin toxicity from her serotonergic medications (amitriptyline, a tricyclic antidepressant, and citalopram, a selective serotonin re-uptake inhibitor) with the additional administration of fentanyl, a phenylpiperidine opioid, which is also a serotonin re-uptake inhibitor. Differential diagnoses included malignant hyperthermia; however, neuromuscular hyper-reactivity signs including clonus are not consistent with this. Primary seizure was also considered, but this was not consistent with clinical signs or electroencephalogram findings. Her hypoxia was likely a consequence of restricted ventilation due to respiratory muscle spasm, which may have occurred because of serotonin toxicity or fentanyl usage. Serotonin toxicity is a spectrum of clinical signs occurring due to increased serotonin concentrations within the central nervous system. Neuromuscular excitation, autonomic nervous system excitation and mental state changes form the triad of clinical features1 with some neuromuscular changes, for example, clonus or tremor and hyperreflexia being essential for diagnosis of serotonin toxicity.2 A number of drug classes are implicated as causative agents including monoamine oxidase inhibitors, serotonin releasing agents (e.g. serotonin re-uptake inhibitors, tricyclic antidepressants and phenylpiperidine opioids) and miscellaneous drugs including lithium.1 Serotonin toxicity is a concentrationdependent event with onset depending on pharmacokinetics and pharmacodynamics of the specific serotonergic agent. With this case, serotonin toxicity developed rapidly corresponding to the rapid onset of action of parenterally administered fentanyl. Serotonin toxicity has been reported previously where patients treated with serotonergic agents have received fentanyl.3,4 In a retrospective analysis conducted by Koury et al.,5 4538 patients given fentanyl while on a serotonergic drug were compared with a cohort of 107 507 patients on a serotonergic agent who did not receive fentanyl. Although the incidence of serotonin toxicity was low, the rate within the cohort receiving fentanyl was 18 times higher, which was statistically significant. Fentanyl is widely used in a variety of situations within the ED. With increasing usage of serotonin-releasing antidepressants,6 ED staff must be aware of the cumulative impact phenylpiperidone opioids have in precipitating serotonin toxicity. For patients prescribed regular serotonergic agents, alternate opioid classes should be utilised if there is no specific indication for fentanyl. If fentanyl is administered, increased vigilance should be observed for the development of serotonin toxicity. Acknowledgement CBP is supported by a QEMRF Research Fellowship. Competing interests CBP is a section editor for Emergency Medicine Australasia. References 1. 2. 3. 4. Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ 2014; 348: g1626. Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM 2003; 96: 635–42. Ailawadhi S, Sung KW, Carlson LA, Baer MR. Serotonin syndrome caused by interaction between citalopram and fentanyl. J. Clin. Pharm. Ther. 2007; 32: 199–202. Rang S, Field J, Irving C. Serotonin toxicity caused by an interaction © 2015 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine 2 5. 6. CASE LETTER between fentanyl and paroxetine. Can. J. Anesth. 2008; 55: 521–5. Koury KM, Becky BA, Gulur P. Incidence of serotonin syndrome in patients treated with fentanyl on serotonergic agents. Pain Physician 2015; 18: E27–E30. Buckley NA, Whyte IM, Dawson AH, Isbister G. A prospective cohort study of trends in self poisoning, Newcastle, Australia, 1987–2012: plus ça change, plus c’est la même chose. Med. J. Aust. 2015; 202: 438–42. Melanie C ARMITAGE,1 Kathryn I WOOLFIELD1 and Colin B PAGE1,2,3 1 Emergency Department, Princess Alexandra Hospital, Brisbane, Queensland, Australia, 2Clinical Toxicology Research Group, University of Newcastle, Newcastle, New South Wales, Australia, and 3 School of Medicine, University of Queensland, Brisbane, Queensland, Australia © 2015 Australasian College for Emergency Medicine and Australasian Society for Emergency Medicine