Photosensitive diseases
advertisement
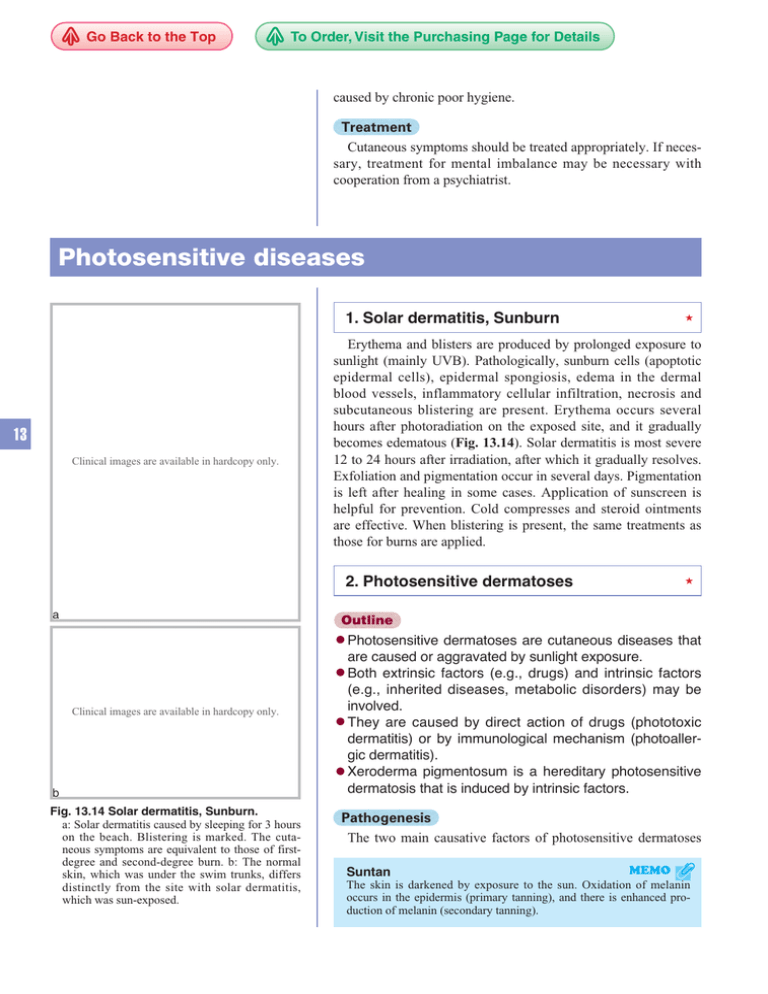
Go Back to the Top To Order, Visit the Purchasing Page for Details caused by chronic poor hygiene. Treatment Cutaneous symptoms should be treated appropriately. If necessary, treatment for mental imbalance may be necessary with cooperation from a psychiatrist. Photosensitive diseases 1. Solar dermatitis, Sunburn Erythema and blisters are produced by prolonged exposure to sunlight (mainly UVB). Pathologically, sunburn cells (apoptotic epidermal cells), epidermal spongiosis, edema in the dermal blood vessels, inflammatory cellular infiltration, necrosis and subcutaneous blistering are present. Erythema occurs several hours after photoradiation on the exposed site, and it gradually becomes edematous (Fig. 13.14). Solar dermatitis is most severe 12 to 24 hours after irradiation, after which it gradually resolves. Exfoliation and pigmentation occur in several days. Pigmentation is left after healing in some cases. Application of sunscreen is helpful for prevention. Cold compresses and steroid ointments are effective. When blistering is present, the same treatments as those for burns are applied. 13 Clinical images are available in hardcopy only. 2. Photosensitive dermatoses a b c d e f g hOutline i j k l m n o p q ● Photosensitive Clinical images are available in hardcopy only. a b c d e f g h Fig. 13.14 Solar dermatitis, Sunburn. a: Solar dermatitis caused by sleeping for 3 hours on the beach. Blistering is marked. The cutaneous symptoms are equivalent to those of firstdegree and second-degree burn. b: The normal skin, which was under the swim trunks, differs distinctly from the site with solar dermatitis, which was sun-exposed. dermatoses are cutaneous diseases that are caused or aggravated by sunlight exposure. ● Both extrinsic factors (e.g., drugs) and intrinsic factors (e.g., inherited diseases, metabolic disorders) may be involved. ● They are caused by direct action of drugs (phototoxic dermatitis) or by immunological mechanism (photoallergic dermatitis). ● Xeroderma pigmentosum is a hereditary photosensitive p q j i dermatosis kthat is linduced m by intrinsic n ofactors. r Pathogenesis The two main causative factors of photosensitive dermatoses MEMO The skin is darkened by exposure to the sun. Oxidation of melanin occurs in the epidermis (primary tanning), and there is enhanced production of melanin (secondary tanning). Suntan r Photosensitive diseases / 2. Photosensitive dermatoses 195 Table 13.4 Main drugs that induce photosensitive dermatosis. Drug Classification Drugs Psychoactive Chlorpromazine, promethazine, diazepam, carbamazepin, imipramine Muscle relaxant Afloqualone Antihistamine Diphenhydramine, mequitazine Antibacterial agent Nalidixic acid, enoxacin, ofloxacin, ciprofloxacin, lomefloxacin, sparfloxacin, fleroxacin, tosufloxacin, tetracycline, doxycyclin Antifungal agent Griseofulvin, flucytosine, itraconazole Antiinflammatory Ketoprofen, tiaprofenic acid, suprofen, piroxicam, ampiroxicam, actarit, diclofenac, naproxen Antihypertensive agent Hydrochlorothiazide, trichlormethiazide, meticrane, clofenamide, tripamide, metolazone, furosemide, tilisolol HCl, pindolol, diltiazem HCl, nicardipine HCl, nifedipine, captopril, lisinopril Antidiabetic Tolbutamide, chlorpropamide, glibenclamide, carbutamide, glymidine sodium Antipodagric Benzbromarone Antitumor agent 5-FU, tegafur, dacarbazine, flutamide Lipid-lowering drug Simvastatin Prostatomegaly therapeutic agent Tamsulosin Photochemistry therapeutic agent 8-Methoxypsoralen, trioxypsoralen, hematoporphyrin derivative Vitamin Etretinate, pyridoxine, VB12 Antirheumatic Sodium aurothiomalate, methotrexate (Based on: Kamide R. Photosensitive dermatosis caused by extrinsic photosensitizing substance. In: Tamaoki K, editor. New Dermatology Vol. 16. Nakayama Shoten; 2003: 293-300). Table 13.5 Classification of photosensitive dermatosis. Classification Cause Drug Extrinsic photosensitive dermatosis Diagnostic name Phototoxic dermatitis Chapter 13 Photoallergic dermatitis Chapter 13 Pellagra Accumulation Intrinsic photosensitive of chromophore Porphyria in skin dermatosis DNA repair defect Described in... Xeroderma pigmentosum (XP) Chapter 17 Chapter 17 Chapter 13 Cackayne syndrome Bloom syndrome Decrease of melanin Albinism Chapter 16 Phenylketonuria Chapter 17 Unknown Hydroa vacciniforme Chapter 13 Solar urticaria Chapter 13 Polymorphous light eruption Chapter 13 Chronic actinic dermatitis (CAD) Chapter 13 are extrinsic chemicals and intrinsic factors (Tables 13.4 and 13.5). This section describes photosensitive dermatoses that are caused by extrinsic factors. Extrinsic photosensitive dermatosis is inflammation of skin caused by the excitation of chromophores by daily exposure to radiation (mainly UVA). Chromophores reach the skin either from outside (skin lotion, perfume, fruit juice, tar) to induce photocontact dermatitis or from within the body (drugs, food). The mechanisms of inflammation are phototoxic Photosensitive drug eruption MEMO In addition to phototoxic condition or photoallergy, drug intake may induce intrinsic photosensitive diseases (e.g., porphyria, lupus erythematosus). 13 196 13 Physiochemical Injury and Photosensitive Diseases sunlight (UVA) chromophores ②Chromophores convert into photoallergens. ①Contact is made with a causative substance, or there is intake of such substance. photoallergens ③The photoallergens connect with biologic proteins. biologic proteins ④Macrophages and Langerhans cells phagocytose the conjugates of photoallergens and biologic proteins. in the lymph nodes or intradermal area intradermal area lymph ducts ⑤The photoallergens in macrophages and Langerhans cells are presented to T cells, and sensitization occurs. regional lymph nodes 13 ①Macrophages and Langerhans cells recognize photoallergens themselves. primary intake of causative substance (sensitization) ②The photoallergens are presented to effector T cells, causing inflammation that peaks 48 hours after presentation. secretion of various cytokines, localized inflammation secondary and further intake of the causative substance Fig. 13.15 Mechanism of photoallergic reaction. Table 13.6 Phototoxic reaction and photoallergic reaction. Phototoxic reaction Photoallergic reaction Incidence May occur in anybody Immunologically mediated (Type IV) only More than one exposure to agent required? No Yes (the excited substance itself becomes toxic) and photoallergic (the excited substance becomes an allergen that induces inflammation by immunoreaction) (Fig. 13.15, Table 13.6). 1) Phototoxic dermatitis Outline ● Phototoxic Onset of reaction hours to 1 after exposure to day agent and light 24-72 hours Dermatitis Clinical features Exaggerated sunburn Distribution Sun-exposed Sun-exposed skin skin Spread to unexposed areas? No Pathologic feature Spongiosis, Necrosis of epidermal cell eczema (sunburn) Yes (possible) Almost never Yes Cross reaction (sometimes) caused by similar compounds? Amount of agent Large required for photosensitivity Small dermatitis may occur in anyone by the combination of a certain dose of drugs and sun exposure. ● It may occur even at the first irradiation (usually by UVA), without any latency. ● The main causative drugs are psoralen, coal tar, thiazide drugs, and tetracycline. Clinical features Sunburn-like symptoms are mainly seen. That is, erythema and edema are followed by exfoliation and pigmentation. Perfume may cause both allergic contact dermatitis and phototoxic dermatitis (Berloque dermatitis) on the neck, especially the sides. MEMO The skin comes into direct contact with the causative agent. Subsequent exposure to light of a certain wavelength causes photocontact dermatitis. It is classified by onset mechanism as phototoxic or photoallergic. Photocontact dermatitis 197 Photosensitive diseases / 2. Photosensitive dermatoses Pathogenesis Drugs that accumulate in the skin absorb light at a certain wavelength. Exposure to light at that wavelength causes phototoxic dermatitis. Each drug affects a particular site. 1. A test substance is adhered to the back for 24 hours. Treatment Intake of the causative substance should be discontinued. Sunlight is avoided by sunscreen and a hat. The treatments are the same as those for contact dermatitis. 2. Half of the patch site is exposed to a slightly smaller amount of UVB than for the first MED exposure (about 70% of MED). If the not substance is not a exposed cause of to UVB photoallergic dermatitis in the patient, no skin lesion or erythema will appear. exposed to a small amount of UVB 2) Photoallergic dermatitis Outline ● Photoallergic dermatitis is photosensitive dermatitis that is caused by a type IV allergy reaction, which is induced by sun exposure after topical application or intake of a drug. ● Erythema and blistering are the main symptoms. ● Chlorpromazine, thiazide drugs and oral antidiabetics are the main causative drugs. Clinical features Erythema and serous papules occur on the sun-exposed site, progressing to edema blistering, and erosion. Pathogenesis Chromophores that somehow attach to the skin react to exposure to light of a certain wavelength (mostly UVA, sometimes visible light) to become allergenic, or they may convert into haptens, connect with biologic proteins and become photoallergenic. After sensitization, the causative substance is re-exposed to light when it reaches the skin surface, where it induces type IV allergic reaction (Fig. 13.15). This reaction does not occur without sensitization; that is, inflammation is not caused by the first exposure, nor does allergic reaction occur in everyone. A person who has been sensitized is prone to light-induced inflammation even from a minute amount of the substance. Laboratory findings, Diagnosis Photo-patch test: The test substance is patched as in the usual patch test. The minimal erythema dose (MED) of the patient is also determined. After 24 hours, half of the patch site is exposed to a slightly smaller amount of UV than that of the first MED exposure. The other half is left unexposed. The result is determined 48 hours after exposure (Figs. 13.16 and 13.17). Photo-drug test: Application of the suspected drug is discontinued for at least 20 days. A normal dose of a test drug is applied for 2 days. The diagnosis is photoallergic dermatitis if an eruption is produced by exposure to light. 3. The patch is removed after 48 hours. The site is examined after a short time passes. 13 Fig. 13.16 Photo-patch testing. 60 50 40 70 30 80 20 90 10 100 mJ/cm2 Fig. 13.17 Determination of minimal erythema dose (MED). UVB from 0 mJ/cm2 to 100 mJ/cm2 is irradiated in increments of 10 mJ/cm 2 on areas of the patient’s back where no eruptions have been produced. The MED in this case is 30 mJ/cm2. 198 13 Physiochemical Injury and Photosensitive Diseases Treatment Intake of the causative substance and sunlight exposure should be avoided. The treatment is the same as that for contact dermatitis. A photosensitive disease called “persistent light reaction,” which is categorized as a chronic actinic dermatitis (CAD), may remain after discontinuation of the causative substance. 3. Solar urticaria Clinical images are available in hardcopy only. a 13 a b c d e f g Clinical images are available in hardcopy only. b c d e f g h Definition, Pathogenesis, Clinical features An allergen is intrinsically produced in skin by exposure to light, against which type I allergy is induced. Several minutes after light exposure (mostly the visible spectrum, but also UVA and UVB in some cases), extremely itchy urticaria occurs; however, it disappears in several hours. Anaphylactic shock may be p q j h i rare cases. k l m n o caused in Diagnosis, Examinations Solar urticaria is generally diagnosed from the recurring eruptions caused by exposure to sunlight or to artificial light. However, wheals may be produced or aggravated by light shielding in some cases; certain wavelengths in the light are thought to inhibit wheals. In young patients, differential diagnosis from erythropoietic protoporphyria may be necessary. i j k l m n o p q r Treatment The patient is shielded from the sun, and antihistamines are applied as a symptomatic treatment. PUVA treatment may be performed as a desensitization treatment. Immunosuppressants and plasma exchange have been reported to be effective in severe cases. Clinical images are available in hardcopy only. 4. Chronic actinic dermatitis (CAD) b c d e f g h i Fig. 13.18-1 Chronic actinic dermatitis. a: Intractable eczema presents as lichenified plaques that progress slowly. b: The skin lesion improved significantly after topical application of tacrolimus for several months. c: The skin lesion recurred after sun exposure. Clinical features, Pathogenesis Chronic actinic dermatitis (CAD) most frequently occurs in pchangeq whoser main j k l intractable m n eczematous o adult males. An symptom is slowly progressing lichenoid plaques occurs on exposed areas of the body and becomes chronic (Figs. 13.18-1 and 13.18-2). In some cases, the lesions progress to erythroderma, leading to cutaneous lymphoma-like subcutaneous nodules, thickening of the skin, or facies leontina. It is hypothesized that intrinsic antigens are produced by light exposure for some reason; however, the details of the onset mechanism are unknown. Photosensitive diseases used to be called “persistent light reaction” “actinic reticuloid” or “photosensitivity dermatitis.” Now these are categorized as forms of CAD. r 199 Photosensitive diseases / 6. Hydroa vacciniforme Pathology Eczematous lesions are the main symptom of CAD. As CAD progresses, lymphocytic infiltration and atypical cells are seen in all dermal layers, and Pautrier microabscess-like lesions may occur in the epidermis (actinic reticuloid). Laboratory findings, Diagnosis, Treatment The minimal erythema dose (MED) for UVB is greatly reduced. The MED for UVA and visible light is also reduced in some cases. For differential diagnosis, the skin is subjected to repeated UVB exposure and if eczematous lesions appear then the diagnosis is CAD. Topical steroids are helpful. Complete a b c light shielding is essential. Tacrolimus ointment is also useful. Oral steroids and immunosuppressants are effective in severe cases. Clinical images are available in hardcopy only. d e f g h i j k 5. Polymorphous light eruption Clinical features Polymorphous light eruption occurs most commonly in women between the ages of 10 to 30. Itchy erythema and papular eruptions appear at sun-exposed sites. They become chronic and tend to gradually worsen. The condition also worsens in summer and subsides in winter. Pathogenesis, Diagnosis Polymorphous light eruption is thought to be an allergic reaca bdiseases c withd tion to light. In practice, all photosensitive unknown causes and without specific symptoms of other photosensitive diseases are considered to be polymorphous light eruption. It requires reconsideration as to whether it is an independent disease. 6. Hydroa vacciniforme Outline ● Hydroa vacciniforme is a rare intrinsic photosensitive disease seen in infants. ● Blisters with concave centers form at sun-exposed sites on the face and dorsa of the hands. ● Epstein-Barr viruses are involved. The disease resolves naturally at puberty. ● Sun shading is important. Clinical features, Pathogenesis Hydroa vacciniforme first appears in infants 2 to 3 years of age and resolves naturally at puberty. It occurs more often in males. Erythema and blisters with concave centers are produced by exposure to sunlight or UVB, and crusts form later on. These Clinical images are available in hardcopy only. e f g h i j 13 k Fig. 13.18-2 Chronic actinic dermatitis (CAD). d, e: Chronic eczematous skin lesion accompanied by intense itching on the occipital region and dorsum of hand of a man in his 50s. It worsened with exposure to the sunlight. Oral cyclosporine improved it markedly. l 200 13 Physiochemical Injury and Photosensitive Diseases Clinical images are available in hardcopy only. leave atrophic scarring when they heal. They mostly occur in the face, auriculae, and dorsa of hands (Fig. 13.19). The lesions are sensitive to light and tend to worsen in summer. When the EB virus is involved, the condition may progress to lymphoma. The onset mechanism is unknown, and hereditary predispositions are not usually found. In cases with the involvement of the EB virus, natural killer-cell lymphoma may develop. Diagnosis, Examinations, Treatment Hydroa vacciniforme is diagnosed by laboratory findings. The symptoms may resemble those of porphyria; however, the porphyria level in hydroa vacciniforme is within the normal range. Direct sun exposure is avoided. Sunscreen is helpful. 7. Xeroderma pigmentosum (XP) Clinical images are available in hardcopy only. Outline ● XP 13 Fig. 13.19 Hydroa vacciniforme. Clinical images are available in hardcopy only. Fig. 13.20 Xeroderma pigmentosum (group D). Pigmentation on the face of a woman in her 20s. The cutaneous symptoms are mild. occurs in persons with congenital failure in the DNA repair process. The cells are easily damaged by UV. Sunburn frequently occurs. ● All types are autosomal recessive inherited. ● A malignant tumor may occur as a complication with age. ● Complete shading of light is an effective treatment. Classification, Pathogenesis Patients with xeroderma pigmentosum (XP) have a congenital failure in repairing and eliminating DNA that is damaged by UV exposure. The failure results in severe photosensitive symptoms. UV causes a replication fork bypass of a pyrimidine (thyminethymine) dimer. XP is classified by unscheduled DNA synthesis (UDS), a classification index, into 8 subtypes: groups A to G, and a variant group (Table 13.7). Group A is the severest, and the variant group is the mildest. In the variant group, UDS is normal; however, there is failure in DNA modification after synthesis. Group A and the variant group are the most frequently occurring in Japan, together accounting for 80% of all XP cases. All groups are autosomal recessive and occur in 1 person out of 100,000 to 1.5 persons out of 100,000. About 30% of patients with XP are born from consanguineous marriages. The main genes responsible for XP have been identified (Chapter 29). Clinical features Abnormalities are not found at birth; however, intense and delayed sunburn in 1- to 2-month-old infants may be recognized as the onset of XP group A. Extremely intense and persistent sunburn recurs on sun-exposed sites such as the face and dorsa of hands and forearms. As sunburn recurs, the skin dries and coarsens, presenting an unwashed appearance with ephelides-like pigmented patches, exfoliation, hypopigmented macules and 201 Photosensitive diseases / 7. Xeroderma pigmentosum (XP) Table 13.7 Comparison between types of xeroderma pigmentosum. Severity of skin manifestation Neurological manifestation Average age of skin cancer development UDS (%) Onset Reduced <5 Babyhood Reduced 3-7 Babyhood C Normal 10-25 Babyhood Severe None 10.5 D Reduced 25-50 Babyhood Moderate Sometimes 35.5 E Reduced 40-60 Babyhood and infancy Mild None 41.0 F Reduced 10-20 Early childhood Mild None 47.7 G Normal <25 Early childhood Mild Sometimes 32 Variant Normal 100 Early childhood (about 5 years old) Moderate None 41.0 Group MED A B Severe, carcinogenesis Appears at about 1 year old telangiectasia (Fig. 13.20). Seborrheic keratosis, small tumors, and ulcers occur in succession at the base of these lesions in childhood. Basal cell carcinoma, squamous cell carcinoma, keratoacanthoma and malignant melanoma occur subsequently. Eye symptoms such as photophobia, blepharitis, dacryorrhea, and conjunctivitis occur in childhood and progress to ectropion, blindness, and malignant tumor in the terminal stages. Progressive neurological symptoms occur 6 months after birth, leading to articulatory disorder, gait disorder and intellectual impairment. Disturbance in growth, such as dwarfism and spondyloschisis, also occur. Groups E, F, and G are often overlooked due to their mild symptoms. The carcinogenic period is the third decade of life. Eye symptoms and neurological symptoms are rarely found in these groups. Nevertheless, cutaneous symptoms and neurological symptoms in some cases of groups E, F, and G closely resemble those found in group A (Fig. 13.21). In the variant group, MED is almost normal, but ephelides gradually appears after childhood. Although eye symptoms and neurological symptoms are rarely seen, basal cell carcinoma or squamous cell carcinoma occurs in adulthood. 9.2 Sometimes Severe MEMO UDS (unscheduled DNA synthesis), a test for xeroderma pigmentosum (XP), shows the potential degree of recovery from DNA damage under UV exposure, expressed as a percentage compared to normal controls. Cells are scattered in a petri dish and exposed to UV. When cultured in [3H] thymidine solution, damaged DNA is repaired, and the cells absorb [3H] thymidine. The amount of [3H] thymidine is measured by autoradiography for comparison with normal cases; patients with XP have reduced UDS values. UDS value Clinical images are available in hardcopy only. Laboratory findings, Diagnosis XP diagnosis is confirmed by the MED level, DNA and RNA syntheses after UV exposure, measurement of UDS, and gene test. Treatment Sunlight should be thoroughly avoided by limiting outings in daytime, wearing clothes that cover the body thoroughly, keeping the hair long, wearing UV-screening eyeglasses, sticking UVscreening film on windows, applying shades to fluorescent lamps, and applying sunscreen. Early detection and treatment of cutaneous malignant tumor are important. Neurological disorders are treated by regular listening-comprehension tests, speech training, and motor ability retention training. Go Back to the Top Clinical images are available in hardcopy only. Fig. 13.21 Xeroderma pigmentosum (Group F). Basal cell carcinoma on the dorsum of the nose of a man in his 20s. To Order, Visit the Purchasing Page for Details 13