- Medgadget
advertisement
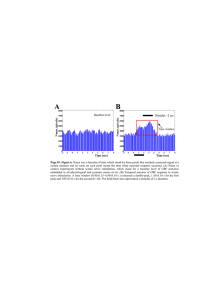
Home Search Collections Journals About Contact us My IOPscience Recruitment and blocking properties of the CardioFit stimulation lead This article has been downloaded from IOPscience. Please scroll down to see the full text article. 2011 J. Neural Eng. 8 034004 (http://iopscience.iop.org/1741-2552/8/3/034004) View the table of contents for this issue, or go to the journal homepage for more Download details: IP Address: 212.143.214.185 The article was downloaded on 05/05/2011 at 13:03 Please note that terms and conditions apply. IOP PUBLISHING JOURNAL OF NEURAL ENGINEERING doi:10.1088/1741-2560/8/3/034004 J. Neural Eng. 8 (2011) 034004 (6pp) Recruitment and blocking properties of the CardioFit stimulation lead Tamar Ahilea Anholt1 , Shai Ayal1 and Joshua A Goldberg2,3 1 BioControl Medical Ltd, Yehud 56100, Israel Department of Physiology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 E-mail: joshua-goldberg@northwestern.edu Received 3 February 2011 Accepted for publication 22 March 2011 Published 5 May 2011 Online at stacks.iop.org/JNE/8/034004 Abstract The CardioFit vagal stimulation system has been developed as a proposed therapy for congestive heart failure (CHF). CardioFit is to be implanted in several hundred CHF patients enrolled in the INOVATE-HF clinical trial, an FDA approved study. The CardioFit stimulation lead (CSL), which is a cuff electrode that delivers stimulation pulses to the right cervical vagus, was designed to recruit efferent cardiac vagal fibers while minimizing unwanted recruitment of other fibers. This paper presents the CSL and measurements of its recruiting and blocking properties when placed on isolated porcine vagus nerves maintained at an elevated temperature in oxygenated artificial cerebrospinal fluid. Using charge balanced quasi-trapezoidal pulses driven through the CSL, we show in eight out of nine nerves a 63% ± 13% (mean ± SD) unidirectional attenuation of the A-fiber compound action potential attained at a current of 3.0 ± 0.8 mA. The threshold for the activation of A- and B-fibers was found to be 0.3 ± 0.17 mA and 2.5 ± 1.1 mA, respectively. The results presented here should help to guide the optimal parameters used in the upcoming deployment of the CardioFit system. in anti-epileptic VNS, is superfluous at best and could induce unwanted side effects (Zagon and Kemeney 2000). The CardioFit system is an implanted VNS system that is approved for marketing in Europe and has been implanted in about 30 patients (De Ferrari and Schwartz 2011). During INOVATE-HF (INcrease Of VAgal TonE in chronic Heart Failure), an FDA approved clinical trial (ClincalTrials.gov 2011), the CardioFit system will be implanted in several hundred patients in the course of the next few years. The main components of the CardioFit system are the CardioFit implantable stimulator (CIS), an implantable pulse generator; the CardioFit stimulation lead (CSL), a nerve stimulation electrode; and an off-the-shelf intra-cardiac sensing electrode (ISE). The CSL safety was demonstrated using histopathological analysis of nerve samples from chronically implanted animals (Cohen and Georgievskaya 2011). The CSL was designed to recruit efferent vagal B-fibers, while minimizing the recruitment of A-fibers, whose activation could potentially have undesired central effects. The purpose of this study was to measure the recruitment and blocking Introduction Vagus nerve stimulation (VNS) is an established and widely used therapy for epilepsy (Handforth et al 1998, Heck et al 2002) and it has also been approved as a therapy for treatment-resistant depression (Rush et al 2005). VNS suitability for several other applications is currently under investigation (Castoro et al 2011). The mechanism of action of VNS for these applications has been investigated using various methodologies (Van Laere et al 2000), yet it is not fully understood. It has been proposed that VNS-induced enhancement of parasympathetic tone could serve to treat congestive heart failure (CHF, Olshansky et al 2008, De Ferrari and Schwartz 2011) as well as other cardiovascular diseases (Bilgutay et al 1968, Vanoli et al 1991, Zhang et al 2002, Tosato et al 2006). In this case, the potential therapeutic effect presumably relies on the propagation of action potentials along the axons of efferent cardiac vagal neurons towards the heart. Any propagation towards the head, particularly along A-fibers, which have been implicated in seizure suppression 3 Author to whom any correspondence should be addressed. 1741-2560/11/034004+06$33.00 1 © 2011 IOP Publishing Ltd Printed in the UK J. Neural Eng. 8 (2011) 034004 T Ahilea Anholt et al to the cardiac R-wave, which is sensed through the ISE. Each burst consists of 1–3 pulses with a programmable inter-pulse interval of 16–350 ms (typically 55 ms). Each pulse is a quasi-trapezoidal (QT) (Accornero et al 1977, van den Honert and Mortimer 1979, Sweeney and Mortimer 1986, Fang and Mortimer 1991, Jones et al 1995, Tosato et al 2007), charge balanced, asymmetric current pulse. The pulse amplitude is programmable with current amplitudes of 0,0.1, . . . ,6 mA and consists of a positive 500 μs plateau followed by an approximately exponential decay with a time constant of 500 μs. This positive phase is followed by a negative discharge phase. The electrode is allowed to discharge with a current limited to an amplitude that is 5% of the amplitude of the positive phase. Discharge continues until the voltage on the electrode vanishes, which takes up to 30 ms. Because the inter-pulse interval within a stimulation burst is longer than the typical nerve refractory time, the neural response for each pulse can be taken as independent of the stimulation history. Hence, characterizing the neural response to single pulses is the relevant information with regard to the efficacy of the device, which delivers only low-frequency bursts. Figure 1. Schematic drawing and electrical wiring diagram of the CSL positioned around the nerve. Silicone is denoted in black. The recessed anode and cathodes are denoted by A, C1 and C2, respectively. The two indifferent contacts are denoted by a ‘0’. One recess, marked ‘E’, is left empty (no contact) to decrease the pressure on the nerve. The widths (in mm) are (from left to right) 0.7, 0.7, 1.4, 1.1, 0.7, and 0.7 for the recesses denoted by 0, A, C2, E, C1, and 0, respectively. The axis of symmetry (center of the nerve) is marked by a dashed arrow pointing in the efferent direction. properties of the CSL as a function of stimulation current and direction. Experiments were conducted on isolated porcine vagus nerves. The neural response to CSL stimulation manifested in the compound action potential (CAP) was recorded and analyzed for relevant stimulation parameters. CSL dimensions and materials The CardioFit stimulation lead (CSL) (figure 1) is a modified bipolar cuff electrode designed primarily for VNS (but it can be applied broadly for peripheral nerve stimulation). The CSL cuff is manufactured using injection press molding from liquid silicone resin (NuSil, Santa Barbara, CA). Recessed into the silicone cuff are five ring-shaped contacts made of platinum– iridium (90%/10%). The contacts consist of one anode, two cathodes (electrically short-circuited to each other) and two neutral contacts (interconnected and otherwise independent Methods The CardioFit system The CIS delivers stimulation bursts to the right cervical vagus nerve using the CSL. The stimulation burst is synchronized 1 0.8 CAP Amplitude [normalized] 0.6 0.4 0.2 0 -0.2 -0.4 0 5 10 Latency [msec] 15 20 Figure 2. A typical CAP response for a 6 mA current pulse. Distinct peaks corresponding to A- and B-fibers can be seen. The A-fibers have a double peak at a latency of less than 5 ms corresponding to the Aβ and Aγ subgroups, and the B-fibers have a peak at a latency of 9 ms. The CAP amplitude is normalized by dividing the signal with the maximal measured A-fiber CAP over all currents. 2 J. Neural Eng. 8 (2011) 034004 T Ahilea Anholt et al of other electrodes in the cuff). The CSL’s cuff length is 12.1 mm, and its outer diameter is 5.9 mm. The CSL comes in four models to ensure a snug fit to the nerve. The models differ only in the cuff’s inner diameter, which can be one of 2.50 mm, 2.75 mm, 3.00 mm or 3.25 mm. (A) Isolated porcine vagus experimental system Animals were supplied by, and the vagus nerve was dissected out at, a local abattoir (Institute of Animal Research, Kibbutz Lahav, Israel). The animals were aged 6 months of mixed Landrace/Large White breed, and weighed approximately 90 kg. Each animal was killed by a stabbing wound to the thorax and was bled. The vagus nerve was removed within 8 min of the stabbing and placed in an ice-cold HEPESbuffered sucrose solution containing (in mM) MgCl2 10, CaCl2 0.5, KCl 3, glucose 11, HEPES 5, sucrose 230, pH = 7.3–7.4 with NaOH, and shipped to our laboratory. The nerve was then transferred into artificial cerebrospinal fluid (ACSF) oxygenated at room temperature in 95% O2 /5% CO2 , which contained (in mM) MgCl2 2, CaCl2 2, KCl 2.5, NaCl 126, glucose 10, NaH2 PO4 ·H2 O 1.25 and NaHCO3 26, and was allowed to equilibrate at room temperature for at least 75 min. After equilibration, the nerve was placed onto an array of silver–silver chloride wires with one end in a small ‘pool’ in which the CSL was fastened around the nerve and submerged in ACSF. The pool, containing the oxygenated ACSF, was kept at 34 ◦ C with a feedback controller to correctly represent the thresholds for blocking and recruitment at a physiological temperature. The rest of the array remained at room temperature (24 ◦ C). In all cases, a CSL with an inner diameter of 2.5 mm was used as it provided a ‘snug’ fit to the porcine vagus. The recording was made through a pair of silver–silver chloride wires from the array. The recording wires had a spacing of 5–10 mm and were at a distance of 50–90 mm from the CSL. The ground terminal was connected to a silver–silver chloride wire, which was located between the CSL and the recording site, and short-circuited to the bath with a silver–silver chloride pellet. To compare activation in the blocking direction versus the non-blocking direction of the CSL, the CSL was removed from the nerve and its direction was reversed. The waveform of the pulse, generated by custom-made software, mimicked the CardioFit pulse waveform. The waveform was fed through a D/A board (National Instruments, Austin, TX) to a linear stimulus isolator (WPI, Sarasota, FL), which was connected to the CSL. The software also controlled an A/D board that recorded 100 ms segments of the signal. The signal was first amplified by a Cyberamp 380 (Molecular Devices, Sunnyvale, CA) amplifier (10 000×– 100 000×) in the differential configuration using a fourthorder (80 dB/decade) low-pass Bessel filter at 6 kHz for antialiasing. It was then sampled at a rate of 50 kHz. The software enabled us to log the CAPs generated by current pulses that varied in amplitude or duration onto a PC. The sequences of pulses with varying parameters were delivered in random order and multiple repetitions were averaged. The latency and amplitude of peaks were determined offline by finding the extrema of the waveform components recorded. 10 20 8 15 6 10 4 Stimulation Current [mA] 2 5 Latency [msec] 00 (B) 10 20 8 15 6 10 4 Stimulation Current [mA] 2 5 Latency [msec] 00 Figure 3. (A) The CAP response for currents ranging from 0.1 to 9 mA in the non-blocking direction. The CAP amplitude is monotonic non-decreasing as a function of current. (B) The CAP response in the blocking direction (the same nerve as in figure 2). A distinct region where the CAP of the A-fibers is attenuated can be seen for currents at or above 4 mA. Results A typical CAP response for a 6 mA current pulse is shown in figure 2. Distinct peaks corresponding to A- and B-fibers may be seen. The A-fibers have a double peak (which are frequently but not always discernable) at a latency of less than 5 ms corresponding to the Aβ and Aγ subgroups, and the B-fibers have a peak at a latency of 9 ms. Typical CAP responses for currents ranging from 0.1 to 9 mA in the nonblocking direction are presented in figure 3(A). The A- and B-fiber CAP amplitudes are either rising or constant as a function of current. In figure 3(B), we show the CAP responses of another nerve in the blocking direction. A distinct region where the CAP of the A-fibers (primarily the Aβ) is attenuated can be seen in the blocking direction for currents at or above 4 mA. The maximal CAP amplitude in the latencies relevant for A-fibers (including both Aβ and Aγ subgroups) and B-fibers 3 J. Neural Eng. 8 (2011) 034004 T Ahilea Anholt et al 1 CAP Amplitude [normalized] 0.8 0.6 0.4 0.2 0 0 1 2 3 4 5 6 7 8 9 Stimulation Current [mA] Figure 4. The maximal CAP amplitude in the latencies 2–6 ms relevant for A- (squares, dashed line) and 6–12 ms relevant for B-fibers (circles, solid line) as a function of stimulation current in the same nerve as used in figures 2 and 3(B). The threshold for A- and B-fiber activations as well as the region of the A-fiber block (marked by a black bar) can be seen. The CAP amplitude is normalized by dividing the signal with the maximal measured A-fiber CAP over all currents. Note that this figure depicts the maximal values detected (algorithmically) for each stimulation, resulting in positive values below threshold due to noise. anode. Elongating the cuff would probably result in a larger A-fiber CAP reduction, but this was impractical because it would also increase the probability of mechanical insult to the nerve. Previous studies of the CAP recorded from the pig vagus in vivo (Tosato et al 2007, Vuckovic et al 2008, Ordelman et al 2010) gave similar results with regard to Aβ, Aγ , and B-fiber components. All of these papers give activation thresholds for the various components of the CAP. These thresholds coincide with our measured thresholds for the Aβ and B CAP components. Tosato et al (2007) report higher currents (10 mA) needed for anodal block with a QT current pulse of the same width or wider, while maximal block at 6.3 ± 2.3 mA was reported by Vuckovic et al (2008) for anodal block with QT pulses of the same width or wider, with a reduction of 60–100% of the maximal CAP amplitude, which is comparable to what the CSL attained. In both Tosato et al (2007) and Vuckovic et al (2008), custommade tripolar cuff electrodes were used. The quantitative differences in percentage blocking and the blocking current results can be attributed to the different electrode shapes and dimensions used in these studies driving a different current distribution through the nerve. Castoro et al (2011) measured the excitation properties of canine vagal fibers using a helical bipolar electrode. The activation thresholds they report for Afibers are similar to those measured here, but their measured B-fiber threshold of 0.5 ± 0.1 mA is much lower than that measured in the pig. Castoro et al (2011) did not report anodal blocking in their measurements. At 6 mA, which is the CIS’s maximal stimulation current, a charge injection of 6 μC/phase at a charge density of 68 μC/cm2 /phase occurs at the anode (which has a smaller as a function of stimulation current in the same recording as shown in figure 3(B) is shown in figure 4. The threshold for A- and B-fiber activations as well as the region of A-fiber block (marked by a black bar) can be seen. In measurements conducted on n = 9 nerves, we found that the threshold for activation of A-fibers was 0.3 ± 0.17 mA (mean ± SD), while the threshold for activation of B-fibers was 2.5 ± 1.1 mA. In eight of the nine measured nerves, A-fiber blocking was observed. In these fibers, maximal block of A-fibers was attained at 3.0 ± 0.8 mA with an average reduction of 63% ± 13% from its initial peak activation, which was attained at 1.2 ± 0.4 mA. Threshold and blocking values are presented in figure 5. Discussion The recruitment and blocking characteristics of the CSL were measured on isolated vagus nerves of the pig. The results show that the CSL, using the QT pulse produced by the CIS, is able to excite A- and B-fibers, and that in one direction a range of currents exists (approximately 3–5 mA) for which the A-fiber CAP is reduced by more than 60%, while the B-fiber CAP attains close to maximal activation. Thus, stimulation by the CSL is B-fiber preferential and directional with regard to Afibers. Such preference toward nerve fiber type and direction is advantageous in applications that require those features, i.e. when organ-specific stimulation is required and the side-effect profile needs to be minimized. A larger reduction in A-fiber CAP was not obtained due to the virtual cathode produced by the current flowing in the indifferent contact nearest to the 4 T Ahilea Anholt et al 60 0 40 1 50 Current [mA] 2 A−fiber max block [%] 3 70 4 J. Neural Eng. 8 (2011) 034004 A−fiber threshold B−fiber threshold A−fiber max block Figure 5. Left: A- and B-fiber thresholds (n = 9) and A-fiber maximum blocking current (n = 8). Right: A-fiber CAP amplitude reduction at maximal blocking as a percentage of the initial peak of A-fiber activation (n = 8, 100% would represent the total block). human subjects will be similar to those measured on isolated nerves and reported here. We should have more definitive data about the recruitment of cardiac fibers in the human right vagus nerve at the conclusion of the INOVATE-HF trial (ClinicalTrials.gov 2011). In conclusion, we show that the CSL, when driven by the CIS, can produce a significant (>60%) reduction in the A-fibers afferent component of the CAP. We believe that these findings will help to guide practitioners to optimal parameter settings to use in the stimulation of the right vagus nerve of the prospective participants in the INOVATE-HF clinical trial (ClinicalTrials.gov 2011). surface area than the cathodes). While this value is above the value used elsewhere (Shannon 1992, Popovic and Sinkjaer 2000), we note that in those studies, a stimulation frequency of 50 Hz for a duration of 7 h was used, while CardioFit is limited to a 9 Hz stimulation frequency at a 25% duty cycle (i.e. stimulation is administered following at most 25% of detected R-waves). As another safety measure, the metal contacts of the CSL are recessed into the silicone so that the nerve does not have mechanical contact with any rigid surface to prevent possible tissue abrasion and damage specific to electrically active biomaterial interfaces caused by the production of free radicals on the electrode surface, resulting in peroxidationmediated injury to membrane lipids (Merrill et al 2005). Indeed, chronic CardioFit stimulation for a duration of 6 months at maximal stimulation parameters was found to be safe, not damaging the nerve fibers (Cohen and Georgievskaya 2011). The human data for activation thresholds in the vagus nerve for comparison to our results are scarce. In Evans et al (2004), results from nine patients show evoked potentials corresponding to A-, B- and C-fibers. Thresholds for activation are not reported. In Koo et al (2001), threshold currents for the activation and conduction velocity of vagal fibers in humans of various ages were measured. For adults, the threshold is below 0.5 mA, which is consistent with our A-fiber results. The conduction velocity of adult vagal fibers as measured in that study is 12 m s−1 , which is slower than the 19 m s−1 measured by Evans et al (2004). Rozman et al (2009) report influences on the heart function of cervical left vagus stimulation in a single human subject. They show that to elicit a significant effect, a current that is above 1.5 mA but below 2.5 mA is needed. This is consistent with our measured threshold for activation of porcine B-fibers. While there are some quantitative differences between our porcine isolated nerve measurements and human measurements, the overall picture of A- and B-fibers seems comparable. This suggests that the recruitment characteristics of the CSL in Acknowledgments The authors would like to thank Rami Biran, Tsachi Czaczkes, Itzhak Sinai, Tamir Ben-David and Ehud Cohen for excellent technical support and valuable discussions. References Accornero N, Bini G, Lenzi G L and Manfredi M 1977 Selective activation of peripheral nerve fibre groups of different diameter by triangular shaped stimulus pulses J. Physiol 273 539–60 Bilgutay A M, Bilgutay I M, Merkel F K and Lillehei C W 1968 Vagal tuning. A new concept in the treatment of supraventricular arrhythmias, angina pectoris and heart failure J. Thorac. Cardiovasc. Surg. 56 71–82 Castoro M A, Yoo P B, Hincapie J G, Hamann J J, Ruble S B, Wolf P D and Grill W M 2011 Excitation properties of the right cervical vagus nerve in adult dogs Exp. Neurol. 227 62–8 ClinicalTrials.gov 2011 http://clinicaltrials.gov/ct2/show/NCT01303718 Cohen M L and Georgievskaya Z 2011 Histopathology of the stimulated vagus nerve: primum non nocere Heart Fail. Rev. 16 163–9 De Ferrari G M and Schwartz P J 2011 Vagus nerve stimulation: from pre-clinical to clinical application: challenges and future directions Heart Fail. Rev. 16 195–203 5 J. Neural Eng. 8 (2011) 034004 T Ahilea Anholt et al Evans M S, Verma-Ahuja S, Naritoku D K and Espinosa J A 2004 Intraoperative human vagus nerve compound action potentials Acta Neurol. Scand. 110 232–8 Fang Z-P and Mortimer J T 1991 Selective activation of small motor axons by quasitrapezoidal current pulses IEEE Trans. Biomed. Eng. 38 168–74 Handforth A, DeGiorgio C M, Schachter S C, Uthman B M, Naritoku D K, Tecoma E S, Henry T R, Collins S D, Vaughn B V, Gilmartin R C, Labar D R, Morris G L 3rd, Salinsky M C, Osorio I, Ristanovic R K, Labiner D M, Jones J C, Murphy J V, Ney G C and Wheless J W 1998 Vagus nerve stimulation therapy for partial-onset seizures: a randomized active-control trial Neurology 51 48–55 Heck C, Helmers S L and DeGiorgio C M 2002 Vagus nerve stimulation therapy, epilepsy, and device parameters: scientific basis and recommendations for use Neurology 59 S31–37 Jones J F, Wang Y and Jordan D 1995 Heart rate responses to selective stimulation of cardiac vagal C fibres in anaesthetized cats, rats and rabbits J. Physiol. 489 203–14 Koo B, Ham S D, Sood S and Tarver B 2001 Human vagus nerve electrophysiology: a guide to vagus nerve stimulation parameters J. Clin. Neurophysiol. 18 429–33 Merrill D R, Bikson M and Jefferys J G 2005 Electrical stimulation of excitable tissue: design of efficacious and safe protocols J. Neurosci. Methods 141 171–98 Olshansky B, Sabbah H N, Hauptman P J and Colucci W S 2008 Parasympathetic nervous system and heart failure: pathophysiology and potential implications for therapy Circulation 118 863–71 Ordelman S C, Kornet L, Cornelussen R, Buschman H P and Veltink P H 2010 An indirect component in the evoked compound action potential of the vagal nerve J. Neural Eng. 7 066001 Popovic D and Sinkjaer T 2000 Control of Movement for the Physically Disabled (London: Springer) Rozman J, Peclin P, Knezevic I, Mirkovic T, Gersak B and Podbregar M 2009 Heart function influenced by selective mid-cervical left vagus nerve stimulation in a human case study Hypertens. Res. 32 1041–3 Rush A J, Marangell L B, Sackeim H A, George M S, Brannan S K, Davis S M, Howland R, Kling M A, Rittberg B R, Burke W J, Rapaport M H, Zajecka J, Nierenberg A A, Husain M M, Ginsberg D and Cooke R G 2005 Vagus nerve stimulation for treatment-resistant depression: a randomized, controlled acute phase trial Biol. Psychiatry 58 347–54 Shannon R V 1992 A model of safe levels for electrical stimulation IEEE Trans. Biomed. Eng. 39 424–6 Sweeney J D and Mortimer J T 1986 An asymmetric two-electrode cuff for generation of unidirectionally propogated action potentials IEEE Trans. Biomed. Eng. 33 541–9 Tosato M, Yoshida K, Toft E, Nekrasas V and Struijk J J 2006 Closed-loop control of the heart rate by electrical stimulation of the vagus nerve Med. Biol. Eng. Comput. 44 161–9 Tosato M, Yoshida K, Toft E and Struijk J J 2007 Quasi-trapezoidal pulses to selectively block the activation of intrinsic laryngeal muscles during vagal nerve stimulation J. Neural. Eng. 4 205–12 Van Den Honert C and Mortimer J T 1979 Generation of unidirectionally propagated action potentials in a peripheral nerve by brief stimuli Science 206 1311–2 Van Laere K, Vonck K, Boon P, Brans B, Vandekerckhove T and Dierckx R 2000 Vagus nerve stimulation in refractory epilepsy: SPECT activation study J. Nucl. Med. 41 1145–54 Vanoli E, De Ferrari G M, Stramba-Badiale H, Hull S S Jr, Foreman R D and Schwartz P J 1991 Vagal stimulation and prevention of sudden death in conscious dogs with a healed myocardial infarction Circ. Res. 68 1471–81 Vuckovic A, Tosato M and Struijk J J 2008 A comparative study of three techniques for diameter selective fiber activation in the vagal nerve: anodal block, depolarizing prepulses and slowly rising pulses J. Neural. Eng. 5 275–86 Zagon A and Kemeney A A 2000 Slow hyperpolarization in cortical neurons: a possible mechanism behind vagus nerve simulation therapy for refractory epilepsy? Epilepsia 41 1382–9 Zhang Y, Mowrey K A, Zhuang S W, Wallick D W, Popovic Z B and Mazgalev T N 2002 Optimal ventricular rate slowing during atrial fibrillation by feedback AV nodal-selective vagal stimulation Am. J. Physiol. Heart Circ. Physiol. 282 H1102–10 6