CAREFUL ANTIBIOTIC USE IN OTITIS MEDIA
advertisement

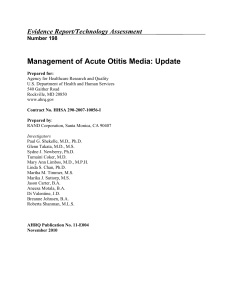
CAREFUL ANTIBIOTIC USE ININ OTITIS CAREFUL ANTIBIOTIC USE OTITISMEDIA MEDIA • Otitis media with effusion does NOT require antibiotic treatment • Acute otitis media does not always require antibiotic treatment Confirm middle ear effusion No effusion NOT OME Or AOM Yes, effusion present Signs/Symptoms of ear pain, fever, or irritability & bulging yellow/red tympanic membrane? Yes No No Acute Otitis Media (AOM) DIAGNOSIS • History of acute onset of signs and symptoms WITH • The presence of middle ear effusion (indicated by bulging of the TM or limited absent TM mobility, otorrhea, or air-fluid level) WITH Signs or symptoms of middle-ear inflammation (indicated by distinct erythema of the TM or distinct otalgia) • Children less than 6 months old: TREATMENT • Treat with antibiotics even when Dx is uncertain. Children aged 6 months to 2 year: • Treat with antibiotics only if severe illness and/or when Dx is confirmed, if Dx is uncertain and/or nonsevere then simply observe without A/B treatment) Children aged 2 year and above: • Treat with antibiotics only if severe illness. if Dx is uncertain or illness is non-severe then simply observe without treatment • Most cases of AOM resolve with symptomatic treatment alone and do not require antibiotics. Managem ent should include assessme nt of pain ¬ if pain is present, clinician should recommend treatment to reduce pain. resolution of OME. PREVENTION . • handwashing • breastfeeding • avoidance of environmental tobacco smoke • avoidance of feeding in a supine, flat position . Presence effusion Otitis of Media with(including Effusionimmobility (OME) of the tympanic membrane) • Presence of effusion (including immobility WITHOUT of the tympanic Signs membrane) or symptoms of acute infection. Nonspecific signs and symptoms (rhinitis, WITHOUT cough, diarrhea) are often present. • Signs or symptoms of acute infection. Nonspecific signs and symptoms (rhinitis, cough, TREATMENT diarrhea) are often present. Antibiotic treatment has not been demonstrated to be effective in long-term • Antibiotic treatment has not been demonstrated to be effective in long-term resolution of OME. • A single course of treatment for 10-14 days may be used when a parent or caregiver expresses a strong aversion to impending surgery. Avoiding unnecessary treatment of just OME would save up to 6-8 million courses of antibiotics each year & help prevent resistance *Management should include assessment of pain—if present, clinician should recommend treatment to reduce pain 97 CONFIDENTIAL Treatment for Acute Otitis Media ISSUES • 1st line agents Amoxicillin • Standard dose 80-90 mg/kg/day PO per day in div doses • Allergy to Penicillin and/or Beta-lactams Azithromycin Clarithromycin 10 mg/kg PO 1st day then 5mg/kg PO daily for 4 days 15 mg/kg/PO div bid for 5 days • Allergy/anaphylaxis w/ beta-lactam (hypersensitivity Type I reaction)*cross-sensitivity possibility still exists in a few patients Cefuroxime axetil Cefprozil 30 mg/kg day PO div bid for 5 days 30 mg/kg day PO div bid for 5 days 2nd-Line Agents This guideline perhaps may not apply to the following types of patients: Failure of Amoxicillin Amoxicillin-clavulanate Cefuroxime axetil Cefprozil 90 mg/kg/day PO div bid (based on amoxicillin)/(use amoxicillin or clavulanate 7:1 formulation) 30 mg/kg/day PO div bid for 10 days 30 mg/kg/day PO div bid for 10 days • infants less than 6 weeks old • premature infants who are hospitalized • children with craniofacial abnormalities such as cleft palate • Clarithromycin • • children who are immunocompromised or have severe underlying systemic disease • children with complications of AOM (e.g., sepsis, mastoiditis) • Also excluded are children with a clinical recurrence of AOM within 30 days or AOM Beta-lactam Allergy Azithromycin Antibiotic prophylaxis is no longer recommended for recurrent AOM A single course of treatment for 10-14 days may be used when a parent or caregiver expresses a strong aversion to impending surgery. Treat symptomatically for 48–72 hours from symptom onset if pain/fever is manageable with systemic analgesics, provided followup can be ensured and provided symptoms don’t worsen earlier. After this timeframe 48–72 hours, antibiotics may be considered for AOM Additionally, in patients with sinus infection, acute bacterial rhinosinusitis should be diagnosed and treated with antibiotics only if no improvement after 10 days or symptoms worsen after five to seven days. 10 mg/kg PO 1st day then 5mg/kg or daily for 4 days 15 mg/kg/PO div bid for 10 days Use a 10-day therapy as standard for children aged 5 years and younger. Use of 5- to 7-day course is appropriate in children aged 6 years and older with mild to moderate disease with underlying chronic OME. • The recommendations in this guideline do not indicate an exclusive course of treatment. Variations, taking into account individual circumstances, may be appropriate. References: 1. CDC website: Pediatric treatment guidelines for upper respiratory tract infections; Otitis Media: Pediatrics Physician Information (Sheet) http://www.cdc.gov/drugresistance/community/healthcare_provider.htm 2. CLINICAL PRACTICE GUIDELINES: American Academy of Pediatrics and American Academy of Family Physicians, Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics 2004;113(5):1451-65. 3. Canadian Clinical Practice Guidelines 2007 from the Alberta Medical Association 4. Dowell SF, Marcy SM, Phillips WR, Gerber MA, Schwartz B. Otitis media-Principles of judicious use of antimicrobial agents. Pediatrics 1998;101(1 Suppl Pt 2):165-71. 5. Stool SE, Berg AO, Berman S, et al. Otitis media with effusion in young children. Clinical practice guideline. AHCPR Publication no 94-0622 1994. 6. American Academy of Family Physicians, American Academy of Otolaryngology-Head and Neck Surgery, American Academy of Pediatrics Subcommittee on Otitis Media with Effusion. Otitis media with effusion. Pediatrics 2004;113(5):1412-29. 7. Wong DM, Blumberg DA, Lowe LG. Guidelines for the use of antibiotics in acute upper respiratory tract infections. Am Fam Physician. 2006 Sep 15;74(6):956-66. 98 CONFIDENTIAL