Gzrdiovascular
Research
ELSWIER
Cardiovascular
Research
32(1996)901-908
Does parallel conductance vary during systole in the human right
ventricle?
P.A. White a, R.R. Chaturvedi a, A.J. Bishop b, C.I.O. Brcmkes b, P. J. Older&w
A.N. Redington a7*
b,
a Depurtment of Paediatric Cardiology, Royal Brompton Hospital, Sydney Street, London, SW3 6NP, UK
b Department of Adult Cardiology, Royal Brompton Hospital, Sydney Street, London, SW3 6NP, UK
Received7 February1996; accepted3 I May 19%
Abstract
Keywords: Parallel conductance; Conductance catheter; Human; Pressure-volume area
Right ventricular (RV) contractile performance remains
poorly characterised, particularly in humans. Measurement
of ventricular volume is important in the investigation of
ventricular function and the description of changes in left
ventricular volume related to time and pressure has been
fundamental in the development of current concepts of left
ventricular performance. Numerous techniques have been
used to measure right ventricular volume [l-5], but most
require geometric assumptions and labour intensive off-line
image contouring. The conductance technique has been
developed to enable a real time, beat to beat assessment of
left ventricular volume [6-91 and is a potentially useful
technique for continuous measurement of right ventricular
volume.
Corresponding author. Tel. (+44-171)
351-8545.
Time for primary
1. Introduction
l
351-8546; Fax (+44-171)
OCO8-6363/%/$15.00 Copyright 0 1996 Elsevier Science B.V. All rights reserved.
PII SOOOS-6363(96)00132-O
review 36 days.
Downloaded from by guest on September 30, 2016
Objectives: Right ventricular (RV) contractile performance remains poorly characterised, particularly in humans. Conductance
catheter techniques have the potential to overcome the geometric difficulties in RV volume measurementthat have hindered systematic
studies of RV pressurevolume relations. The present study examines changes in parallel conductance(Vc) that may occur during the
cardiac cycle in the human right ventricle. Methods: Using signals obtained from custom-built conductance catheters, six iscchronal
systolic values of Vc (Vc(t)) were measuredduring hypertonic saline wash-in. Studies were performed in nine patients undergoing right
heart catheterisation.Their agesranged from 7 to 39 years (median = 16) and their weights ranged from 20.3 to 84.7 kg (median = 50.0
kg). Measurementsof mean Vc and isochronal Vc(t) and its variability during systole were assessed.Mean Vc was measuredusing the
Baan technique (Vc(Baan)), Vc(t) was measuredfrom six systolic isochrones obtained during the same period of hypertonic saline
wash-in. Results: The temporal changes in Vc(t) were small (mean 5.8%, median = 4.4%, range = 0.6-17.9%) of total corrected
end-diastolic volume (mean maximal variation of 7.7 ml). The value of Vc(t) obtained at dp/df,,
(mean - 99.1 ml; median - 104.75
ml; range 20.15-196.7 ml) was not significantly different to that obtained at dp/dt,,
(mean = 100.0 ml; median = 110.87 ml;
range = 20.0-204.2 ml) (P > 0.05), but both were higher than the single Vc measurement(Vc(Baan)) obtained using the standard
approach(P = 0.02). The correlation betweenVc(Baan) and Vc(t) for group data; (Vc(Baan) = 89.69 ml, s.d. = 43.73 ml; vc(t7 = 98.16
ml, s.d. = 50.16 ml) produces a regressionslope of 0.99 for all studies (P = 0.02). Conclusion: We conclude that parallel conductance
does vary during systole in the human right ventricle of adults and older children after repair of congenital abnormalities but there is no
significant difference in Vc(t) at dp/dr,i, and d p/dr,.
However, there was a significant difference when the isochronal Vc(t)
measurementis comparedwith the standardsingle value technique (Vc(Baan)) obtained using the hypertonic saline wash-in method.The
excellent correlation between Vc(t) and Vc(Baan) suggeststhat the correction of Vc for the phaseof the cardiac cycle is unnecessaryfor
most purposeswhen studying the human right ventricle.
PA. White et al./ Cardiovascular Research 32 (1996) 901-908
902
A
.,, ._ ,.. 4
_..._.....__._......-............_.._._...._.__._..._.__..........~~~~~
._...__............-................._.__....._.............~
::.::,..:.:*I :.: :.:._ :.:.. :.:.: :.: : :iseo,
ECG (BPW
. ...
85
Volume (ml)
80
__.....-..
I
__ .__.._
__.
_.
Pressure (mmHg)
Pressure / Volume
Time (Set)
B
End Diastolic Volume (ml)
End Systolic Volume (nil)
Downloaded from by guest on September 30, 2016
20.84
PA. White et al. /Cardiovascular
We have previously shown that a conductancecatheter
can reliably measurethe volume of right ventricular models made from human post-mortem hearts [lo]. A drawback of this technique in vivo is that structures such as the
myocardium and left ventricular blood pool also conduct
current, a phenomenon known as parallel conductance
(Vc). There is no systematicevaluation of Vc in the human
left or right ventricle and validation is neededto determine
its stability during the cardiac cycle. The hypertonic saline
wash-in technique for determining parallel conductance
has been widely reported for the left ventricle in animal
models [8,11]. This technique yields a single value for
parallel conductancevolume, Vc(Baan), i.e., it assumesno
significant variation during the cardiac cycle. Animal studies have suggestedthat any such variation is insignificant
in the left ventricle [ 12,131but there are no data currently
available for the right.
In this study we present a method of determining
parallel conductance throughout the systolic phase of the
cardiac cycle to investigate the potential variation of Vc in
the human right ventricle.
2.1. Preparation
Studies were performed in nine patients undergoing
cardiac catheterisation for a variety of clinical conditions.
Their agesranged from 7 to 39 years (median = 16 years)
and their weights ranged from 20.3 to 84.7 kg (median =
50.0 kg). There were seven males and two females. All
patients were in sinus rhythm. Patient characteristics are
detailed in Table 1. All had undergone surgical or tranTable 1
Patient demographicsand clinical condition
Patient Age (years) Weight (kg) Sex Clinical condition (repaired)
1
2
3
4
5
6
7
8
9
15
16
I
18
30
21
39
16
14
40.95
50.00
20.30
59.15
84.70
80.10
38.05
60.00
46.00
M
M
M
M
M
F
F
M
M
PA + VSD
PS+PR
AVSD + fallots
Fallots
Fallots + PS+ PR
Fallots
PS+ fallot + VSD
Fallots
PS+ pulmonary valvotomy
PA = pulmonary atrcsia; VSD = ventricular septal defect; PS =
pulmonary stenosis; PR = pulmonary regurgitation; AVSD =
atriovennicular septal defect; Fallots = tetralogy of fallot.
903
scatheter treatment of congenital heart defects and were
being re-evaluated as part of their routine follow-up. None
had any evidence of residual intra- or extracardiac shunting, outflow tract obstruction, atrioventricular valve regurgitation or myocardial dysfunction. This study was approved by the hospital ethics committee and informed
written consentwas obtained from all patients. The investigation conforms with the principles outlined in the Declaration of Helsinki [14]. All subjects were sedated, intubated and receiving intermittent positive pressure ventilation at the time of study. A 2.5 French Millar micromanometer (Millar Instruments Inc., Houston, TX, USA)
and a 5 or 7 French custom-built “8-electrode” conductance catheter (Cordis-Webster, Roden, The Netherlands)
with an appropriate total interelectrode distance to match
the length from the apex to the tricuspid valve (range 5-8
cm), was advanced via the femoral vein into the right
ventricle and positioned with the distal end in the apex.
The catheter size was selected so that the most proximal
electrode of the conductance catheter was at the level of
the tricuspid valve. Correct placement of the conductance
catheter was achieved mainly by fluoroscopy and verified
by monitoring segmental volume phase relationships and
counterclockwise pressure-volumeloop genesis. The conductance catheter was connected to a Sigma 5 DF signal
conditioning and processing unit (Cardiodynamics, The
Netherlands). Analogue signals representing the five segmental conductances, left ventricular pressure and ECG
were digitised (12 bit, 250 Hz), monitored on line and
stored on a microcomputer for later analysis using custom
software.
2.2. Conductance catheter
The principles of the conductancetechnique to estimate
ventricular volume have been described in detail elsewhere
and extensively evaluated in the left ventricle [7-91.
Briefly, the conductance catheter method to determine
ventricular volume is based on the measurementof the
electrical conductanceof blood in a ventricular cavity. The
conductance catheter used in all measurementshad eight
equally spacedplatinum ring electrodes.
An electric current of 20 kHz and 30 PA is applied
between the two outermost electrodes(electrodes 1 and 8)
to generate an intracavitary electric field. The remaining
electrodesare used to measurethe potential difference and
therefore derive the time varying conductance(Gt) of five
ventricular segments.Total right ventricular conductanceis
calculated as the sum of the segmentalconductances.The
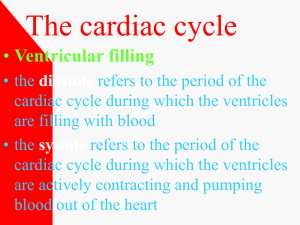
Fig. 1. Determination of Vc(Baan) from the human right ventricle. (A) Data obtained dur!ng hypertonic saline wash-m. The hypertonic saline mixes with
blood in the right ventricle producing a gradual transient increasein volume while true volume and pressureremain constant.(B) Regressionusing paired
minimal versus maximal volumes generatesa linear relation between observedvolumes as a function of changing blood conductivity. Extrapolation to the
line of identity (correspondingto o = 0) gives Vc(Baan) = 59.7 ml, R = 0.%9.
Downloaded from by guest on September 30, 2016
2. Method
Research 3;? (1996) 901-908
PA. White ef al. / Cardiovascular Research 32 (1996) 901-908
904
relationship between time varying volume (Vt) with Gt is
given by the simple formula [7]:
Vt = l/a.
L2 p(Gt - Gp)
(1)
Where (Y is the dimensionless slope factor, p is the
specific conductivity of blood measured from a blood
sample, L is the interelectrode distance and Gp is the
parallel conductance.Left and right ventricular tissue, fluid
and the associatedpericardial tissues also contribute to the
total measuredconductance.The offset volume, Vc, caused
by the parallel conductance,Gp, is equal to
Vc = ( 1/cz)(L2. p)Gp
(2)
Fig. 2. Pressurevolume loops obtained during a saline wash-in technique.
The perceived volume increase is due to the increasing conductivity
created by hypertonic saline.
2.3. Vc estimation
V,, = mV,, + b
(3)
Where V,, = end systole and V,, = end diastole, m =
slope, b = y-intercept.
As actual stroke volume is constant, changes in these
conductance values are due to altered blood conductivity
and not volume. V,,, is plotted against the subsequent
Vminof each beat during the ascendingphaseof the saline
wash-in. The theoretical relationship between EDV and
ESV represents a straight line thus we perform linear
regression analysis on ESV and EDV. This line is used to
extrapolate to the line of identity (A’). The volume at this
point representsVc(Baan) (B’) (Fig. 1B). This volume is
the result of current conducted through structures surrounding the right ventricle equals (Vc(Baan)) by:
Vc(Baan) = b/( 1 - m)
(4)
where Vc(Baan) = parallel conductance, b = y-intercept,
m = slope
2.4. Vcfd
The method describedby Baan et al. [6] yields a single
value based on measurementstaken at end systole and
diastole. This does not take into account potential changes
during the cardiac cycle. To assessvariability of parallel
conductancein the right ventricle multiple estimateswere
obtained during systole using a method previously described in dogs and mini-pigs in the left ventricle [ 12,131.
Briefly, the systolic portion of four consecutive cardiac
cycles from a hypertonic saline wash-in was divided into
six equal time intervals (isochrones) from dp/dt,,,
to
dp/dt,,,,, and the apparent ventricular volume of each
point was obtained by interpolation from the raw data.
The data were then plotted as ventricular volume versus
stroke volume for each cardiac cycle. Thus ventricular
volume at each isochronal point can be linearly regressed
against stroke volume. The volume where the regression
line intercepts the y-axis corresponding to zero stroke
volume or conductivity correspondsto the parallel conductance volume at each time interval (Vc(t)). If there were no
change in Vc(t) then the intercept would be identical for
each isochrone.
2.5. Protocol
Arterial, right atria1and pulmonary artery pressuresand
ECG were continuously monitored. Having obtained an
optimum conductancecatheter position in the right ventricle, blood resistivity, p, was measuredand entered into the
signal conditioning and processing unit along with the
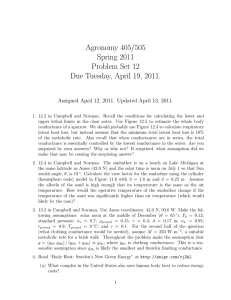
Fig. 3. Isochronal plots for each of the six time intervals in each patient. Isochrones l-6 representequally spacedisochronesfrom maximum dp/dr to
minimum dp/dr and the numerical value is reflected by the y-intercept for each regressionline.
Downloaded from by guest on September 30, 2016
Determination of a value for the volume offset due to
parallel conductance(Vc(Baan)) was performed by a dilution technique previously described by Baan et al. [6],
whereby the conductivity of the blood was transiently
increasedby a bolus injection of hypertonic saline (1-3 ml
of 10%) into the femoral vein. After a short period of time
the blood-saline mixture entered the right ventricle causing
an increase in the right ventricular conductance and perceived increase in amplitude of the volume signal (Fig.
1A). The principal assumption inherent in this method is
that infusion of a small bolus of hypertonic saline increasesthe blood conductivity but not the volume of blood
in the right ventricular cavity, while the conductivity of
surrounding structures remains constant. From the conductance signal, the two most easily identified points from
each successivecycle are the points of maximum (V,,, or
end-diastolic) and minimum (V,,,i, or end-systolic) volume
according to
PA. White et al. /Cardiovascular
Research 32 (1996) 901-908
905
Patient 3
Patient 1
______
Vc@un)-IOS.4ml
&.a l-126.32ml
6
lo
Patient 4
30
20
strolks
volva
6
I
2
(WI]
3
Sxoka
‘
Voluma
5
6
7
(mll
Patient 6
Patient 5
00
Lsa 3=63.84d
Is0 4=63 mm1
3
00
Downloaded from by guest on September 30, 2016
5
Is0 6==62.94ml
s
a
:
2
2
5
Q
70
Patient 7
Patient 8
Patient 9
40
Is0 I -I 32.39d
LoZ-123.6Lhl
Lua44-117.3Sml
20
lo
0
str.A.
lrochtone
ea lrochrone
q
1
2
o lrochrone
o ltochrons
3
4
o lrochrons
o lrochrone
20
“oluan
5
6
(ml,
30
-0
1
2
3
S,rLa.
‘
v.aluala
5
6
(“0
7
6
906
PA. White et al. / Cardiovascular
interelectrode distance. Parallel conductancewas measured
during the injection of 3 ml of 10% saline into the femoral
vein during continuous data acquisition. If ectopy occurred
during data collection, we performed another injection in
order to obtain at least two acceptable recordings. If
changesin heart rate or ventricular pressurewere apparent
during the saline injection, the injection was repeatedwith
a smaller volume. Each dataset was acquired for approx.
20 s during suspendedventilation.
2.6. Data analysis/statistics
The significance of variation from the mean of six
isochronal values of Vc(t> during systole was assessed
using analysis of variance. The Vc(t) values obtained at
were also compared directly to those at
dp/%,,
dp/dtmi, using a paired sample t-test. The possibility of a
relationship between the absolute measurement of
Vc(Baan) and its deviation during the cardiac cycle was
assessedby linear regression. The null hypothesis was
rejected when P < 0.05.
Fig. 2 shows an example of the pressurevolume loops
recorded after injecting 3 ml of hypertonic saline into the
femoral vein. The single value technique yielded values of
Vc(Baan) which ranged from 19 to 166.4 ml (median = 99
ml, s.d. = 43.75 ml). The correlation coefficients (r) of the
relationship when V,,,,, is plotted against the subsequent
Vminto obtain Vc(Baan) ranged from 0.80 to 0.99 (mean =
0.93, s.d. = 0.07).
The time varying Vc(t) determination was obtained
from each of six isochrones during the systolic portion of
the cardiac cycle (Fig. 3). Each of the lines displayed on
the graph represents one of the isochrones ranging from
minimum to maximum dp/dt and the numerical value is
reflected by the y-intercept for each regression line.
Isochrone 1 represents maximum positive dp/dt and
isochrone 6, minimum dp/dt. Each isochrone in between
can be identified from its y-intercept. The six Vc(t)
values, Vc(t) at dp/d&
and dp/dr,,,, and from the
normal saline technique (Vc(Baan)) are summarised in
Table 2. The close correlation betweenVc(Baan) and Vc( t)
for group data (Vc(Baan) = 89.69 ml, s.d. = 43.74 ml;
Vc( t) = 98.16 ml, s.d. = 50.16 ml) producesa regression
slope of 0.99 and an intercept of - 3.93 ml (P = 0.02).
Fig. 3 details the changesin Vc(t> that occurred during
cardiac systole in all nine patients. The mean initial value
for group data, at dp/dt,,,, of 0.96 + 4.36 ml above the
mean decreased to a minimum of - 2.60 I!I 5.30 ml at
midsystole changing at d p/d tmin to 1.90 f 4.37 ml. However, the value at dp/dr,,, was not significantly different
from that at dp/dt,i, (P > 0.05) but both exceededmean
Vc(Baan) (P = 0.02).
Table 2
Mean Vc(Baan) determined by hypertonic saline with mean Vdt)
nine patients
Patient
Vc(Baan)
vc(t)
Vdt) (dp/dr,,,)
Vc(t) (dp/dr,,,)
1
2
3
4
5
6
7
8
9
Mean (ml)
s.d. (ml)
P
105.4
85.7
46.6
59.7
101.2
166.4
124.2
99.0
19.0
89.7
43.7
0.02
121.7
93.6
48.0
62.8
111.1
192.3
123.5
109.8
20.8
98.2
50.2
121.5
92.4
46.9
62.9
110.9
204.2
129.1
112.4
20.0
100.1
53.7
ns.
126.3
90.0
47.3
63.1
111.3
196.7
132.4
104.7
20.2
99.1
52.3
for
Vc(Baan), single value parallel conductance; vc(t), mean of time varying
parallel conductance from dp/dt,,,
to dp/dt,,;
Vc(t) dp/dt,i,,
mean parallel conductance at dp/dr,,,;
V&j dp/dt,,,,
mean parallel
conductance at dp/dr,,,.
Comparison of Vc(Baan) with vc(t) and
Vc(t) dp/dt,i,
to V&) dp/dr,,,
was by a paired I-test (P-values
shown).
There was a significant relationship (r = 0.59, P < 0.05)
with the difference between maximum and minimum Vc(t)
[AVc(t)] and the Vc( t) averaged from all of the six
isochrones.This suggeststhat the magnitude of variability
is proportional to the amount of parallel conductanceitself.
However, overall the Vc(t) averaged for the group represented 5.73% (s.d. = 5.75%) of total corrected end-diastolic volume (mean maximal variation of 7.66 ml), and
2.47% (s.d. = 2.23%) as a percentageof Vc(t).
4. Discussion
The conductancetechnique has been widely applied to
the study of left ventricular pressure-volumerelationships
in animals [8,15,16] and adults with a variety of heart
diseases[7,11]. Extensive validation has been published
and it has been recently demonstratedthat left ventricular
parallel conductance remains fairly constant during the
cardiac cycle [ 12,131.There is no theoretical reason why
this technique should not be applied to study human right
ventricular function. A prerequisite of this technique is the
determination of the parallel conductanceor volume offset
(Vc) due to the conductivity of tissues surrounding the
ventricular blood pool. Early studies assumedthis offset to
be constant [6,17], but there are several potential sources
of Vc variability including respiration, atria1 filling, right
ventricular ejection, and myocardial blood volume changes.
Of these, in clinical practice, changeswith respiration are
the largest and were even more marked in this study of
right ventricular volumes than we have seen in the left
ventricle. For this reason all measurementsmadeusing this
technique should be recorded during suspendedventilation.
Downloaded from by guest on September 30, 2016
3. Results
Research 32 (1996~901-908
PA. White et al./Cardiovascular
907
lished b,y Szwarc et al. [13] in the much smaller left
ventricle of anaesthetisedclosed chest mini-pigs. In this
study a small but significant variation in Vc(t) was found
using the isochronal method in the left ventricle of closed
chest pigs, although there was no significant difference
between Vc(t> at dp/dt,,,
and dp/dr,,,,. However, a
comparison with the single value method was not made in
their study.
Implicit in our analysis is an unchanged gain constant
(a) throughout the cardiac cycle. There are remarkably
few data in this regard. Most investigators, in left ventricular studies, like us in the right ventricle either ignore ct
(assuming it to be constant even over a wide range of
conditions [8,17]) or calibrate the conductancesignal using
angiographic [7] or thermodilution measurements[7,1l]
(both of which have inherent limitations). In a novel study,
examining (Y and its potential variation throughout the
cardiac cycle and over a broad volume range, Stamatoet
al. [20] examined seven open and closed chest pigs. The
gain constant, cx, did not change significantly during the
cardiac cycle. However, when stroke volume was compared with that obtained by either thermodilution or pulmonary flow probe (in the open chest animal), over a wide
range of volumes, an inverse relation was observed between right ventricular volume and o. Although the exact
relationship between a variable 01 and a variable Vc has
not been definitively described, no matter what this relationship, the overall effect is small when assessedin this
clinical preparation.
The effects of hypertonic saline in the myocardial blood
vessels were overcome by taking systolic isochronesduring the ascending limb of the saline wash-in. This is
important, as Baan et al. [7] showed that a transient
decreasein left ventricular pressure and in maximal left
ventricular dp/dt occurred when 1.5 ml of 0.6 M of
saline was injected directly into the main stem left coronary artery of dogs. Furthermore, there was a transient
increase in left ventricular diameter and conductance,
amounting to 2% of end-diastolic dimension. Lankford et
al. [ 121 <andApplegate et al. [21] also observed that the
descendingphase of the saline wash-in is often accompanied by a slight fall in left ventricular pressure,presumably
becauseof the myocardial depressanteffect of the concentrated saline. To avoid these changes,apparently causedby
an effect on the myocardium, Vc was measuredduring the
rising limb of the hypertonic saline wash-in in all right
ventricular parallel conductancemeasurementsas penetration of salt into the wall during this period is limited.
Our results are important in a number of respects.The
temporal variation in Vc(t) in the right ventricle is small
and appearsto be of the same order of magnitude as that
seenin the left ventricle [ 12,131,although it is theoretically
possible that we did not detect larger changesby examining only six isochrones. Nonetheless,despite the potential
effects of right atria1 filling, varying right ventricular
chamber geometry during systole and left sided events,
Downloaded from by guest on September 30, 2016
We have previously shown that a conductancecatheter
can reliably measurethe volume of human right ventricular casts[lo], and Dickstein et al. [ 181in a recent study in
open chest pigs suggestedthe technique may be particularly useful for the study of RV function in vivo. In their
study a consistent change in RV end-systolic P-V relationships with loading and inotropic intervention was shown.
Parallel conductancein the study of Dickstein et al. [ 181
was measuredusing the single value, linear technique first
describedby Baan et al. (Vc(Baan)) [7]. Validation studies
in animals [ 18,191with structurally normal right ventricles
suggestthat Vc measuredusing Baan’s technique is relatively stable over a wide volume range. This commonly
usedmethod of estimating Vc has the theoretical disadvantage of utilising only two points in the cardiac cycle and
does not, therefore, allow for change in Vc that may occur
between these times. Parallel conductance determination
tends to be higher in the right ventricle [ 181,presumably
reflecting a greater current leakage through the thin wall
and proximity to mediastinal structures. This may introduce the potential for a greater error in absolute volume
determination. Furthermore, the thin ventricular wall makes
Vc measurementsmore sensitive to changes that occur
within the cardiac cycle, e.g., atria1filling and LV ejection.
To date, however, there are no animal or human data
concerning right ventricular parallel conductance during
the cardiac cycle.
Lankford et al. [12] devised a method for estimating
changesin Vc during the cardiac cycle which, they argue,
is more robust and less susceptible to noise within the
system. By using 20 isochrones throughout systole they
were able to demonstrate, in the isolated heart, minimal
changesin left ventricular Vc(t), although there were more
marked changes which approximated 4% of the end-diastolic volume, in the in situ preparations. Despite this
temporal variation there remained an extremely good correlation between Vc(Baan) and Vc(t). It was also shown
that the conductance volume signal was only minimally
sensitive to changesin the blood content of the surrounding myocardium.
We used a similar method to examine changesin Vc(t)
that occur during the cardiac cycle in the human right
ventricle. Our data show that small changes in parallel
conductanceoccur during systole, representing 6% of the
end-diastolic volume, but no significant difference between
Vc(t) at dp/dr,,, and dp/d&.
Interestingly, in common with the study of left ventricular parallel conductance
by Lankford et al. [ 121,the parallel conductanceat both of
thesepoints and the Vc( t) from the six systolic isochrones
exceededthat obtained using the single value Baan technique (Vc(Baan)). Importantly, however, there was a close
linear relationship between Vc(t) and Vc(Baan) (r = 0.99).
Thus for most clinical and experimental preparations,where
relative volume is important, either method will allow
durable, repeatableand comparable results.
These findings are very similar to those recently pub-
Research 32 (1996) 901-908
908
PA.
White et al. / Cardiovascular
Acknowledgements
This work was supportedby the Scott Rhodes Research
Fund and Clinical Research Committee, Royal Brompton
Hospital NHS Trust. Thanks must also be given to Dr. R.
Szwarc for provision of the analysis software used in this
paper.
References
111 Ferlinz J. Measurement of right ventricular volumes in man from
single plane cineangiograms. A comparison to the biplane approach.
Am. Heart J 19749487-96.
121 Redington A, Gray H, H&on M, Rigby M, Oldershaw P. Characterisation of the normal right ventricular pressure-volume relation by
biplane angiography and simultaneous micromanometer pressure
measurements. Br. Heart J 1988;59:23-30.
[3] Foale R, Nihoyannopoulos P, Mckenna W, et al. Echocardiographic
measurement of the normal adult right ventricle. Br. Heart J
1986;56:33-44.
[4] Markiewicz W, Sechtem U, Higgins C. Evaluation of the right
ventricle by magnetic resonance imaging. Am Heart J 1987;113:815.
[5] Schnjen F, Herringuez A, Renondo J, Poincelot F, Pichene M. Inter-
32 (1996) 901-908
and intrasubject variability of the thermodilution measurement of
right ventricular ejection fraction and volume in patients with chronic
obstructive pulmonary disease. Cardiovasc Res 1990;24:33-36.
t61Baan J, Jong TTA, Kerkhof PLM, Moene RJ, Van Dijk AD, Van
der Velde ET, Koops J. Continuous stroke volume and cardiac
output from intra-ventricular dimensions obtained with impedance
catheter. Cardiovasc Res 1981;15:328-334.
[71 Baan J, Van der Velde ET, Hein G, et al. Continuous measurement
of left ventricular volume in animals and humans by conductance
catheter. Circulation 1984;70(5):812-823.
h31Burkhoff D, Van der Velde ET, Kass D, Baan J, Maughan WL,
Sagawa K. Accuracy of volume measurement by conductance
ejecting
canine hearts. Circulation
catheter in isolated,
1985;72(2):440-447.
191 Baan J, Van der Velde ET, Steendijk P, Koops J. Calibration and
application of the conductance catheter for ventricular volume measurement. Automedica 1989;11:357-365.
[IO1White PA, Bishop AJ, Conroy B, Otdershaw PJ, Redington AN. The
determination of volume of right ventricular casts using a conductance catheter. Eur Heart J 1995; 16: 1425- 1429.
llll Kass DA, Midei M, Graves W, Brinker JA, Maughan WL. Use of a
conductance (volume) catheter and transient inferior caval occlusion
for rapid determination of pressure-volume relationships in man.
Cathet Cardiovasc Diag 1988; 15: 192-202.
l121Lankford EB, Kass DA, Maughan WL, Shoukas AA. Does volume
catheter parallel wall conductance vary during the cardiac cycle. Am
J. Physiol 1990;258 (Heart Circ PhysiolU):Hl9331942.
1131 Szwarc RS, Mickleborough LL, Mizuno SI, Wilson GJ, Liu P,
Mohamed S. Conductance catheter measurements of left ventricular
volume in the intact dog: parallel conductance is independent of left
ventricular size. Cardiovasc Res 1994;28(2):252-258.
[141 Declaration of Helsinki. Br Med J 1964;ii: 177.
1151 Kass DA, Yamazaki T, Burkhoff D, Maughan WL, Sagawa K.
Determination of left ventricular end-systolic pressure-volume relationships by the conductance (volume) catheter technique. Circulation 1986;73:586-595.
1161McKay RG, Miller MJ, Ferguson JJ, et al. Assessment of left
ventricular end-systolic pressure-volume relations with an impedance
catheter and transient inferior vena cava occlusion: use of this
system in the evaluation of the cardiotonic effects of dobutamine,
mihinone, posicor, and epinehrine. J Am Co11Cardiol 1986,8: 11521160.
[171 Mckay RG, Spears JR, Aroesty JM, et al. Instantaneous measurement of left and right ventricular stroke volume and pressure-volume
relationships with an impedance catheter. Circulation 1984;69:703710.
[18] Dickstein ML, Yano 0, Spotnitz HM, Burkhoff D. Assessment of
right ventricular contractile state with the conductance catheter
technique in the pig. Cardiovasc Res 1995;29:820-826.
[19] Wocdard JC, Bertram CD, Gow BS. Detecting right ventricular
volume
changes using the conductance
catheter. Pace
1992;15:2283-2294.
[20] Stamato TM, Szwarc RS, Benson LN. Measurement of right ventricular volume by conductance catheter in closed-chest pigs. Am J
Physiol 1995;269 (Heart Circ Physiol 38):H869-H876.
[21] Applegate RJ, Cheng CP, Little WC. Simultaneous conductance
catheter and dimension assessment of left ventricle volume in the
intact animal. Circulation 1990;81:638-648.
[22] Bohwood CM, Appleyard RF, Glantz SA. Left ventricular volume
measurement by conductance catheter in intact dogs: parallel conductance volume depends on left ventricular size. Circulation
1989;80:1360- 1377.
[23] White PA, Chaturvedi RR, Bishop AJ, Redington AN. Development
and validation of a conductance technique for measuring pulmonary
valve regurgitation. In: Proceedings of the Institution of Physics and
Engineering in Medicine and Biology, 1st Annual Scientific Conference, 1995;98 (Abstr.).
Downloaded from by guest on September 30, 2016
Vc(t) remains reasonably constant, and so estimations of
Vc in the right ventricle should be as accurate as those in
the left ventricle. Although these results are encouraging it
must be realised that they do not imply that Vc remains
constant under all conditions. Indeed Boltwood et al. [22]
have demonstrateda significant fall in Vc during extreme
off-loading in the canine left ventricle, while Applegate et
al. [21] observed a greater decreasein conductancevolume
as compared to ultrasonic volume during caval occlusion,
implying that Vc decreasedwith extreme preload reduction. However, we have found no significant change in Vc
under the more physiological changes seen during fluid
loading in humans [23]. Until these findings have been
investigated further it remains important, therefore,to make
repeatedmeasurementsof Vc during acute interventions.
In conclusion we have shown that while Vc(t) varies
throughout the cardiac cycle in the human right ventricle
of adults and older children after repair of congenital
abnormalities, there is no significant difference in Vc(t) at
dP/dtmin ad dP/dtrnax- The fact that the small changes
observedin Vc(t) during systole are similar in both the RV
and LV suggests that the anatomy of the RV does not
preclude the use of conductancecathetertechnology in the
assessmentof RV function. Finally, the excellent correlation between Vc(Baan) and Vc(t) suggeststhat the correction of Vc for the phaseof the cardiac cycle is unnecessary
for the purposesof most data analysis.
These results provide further evidence that the application of conductancetechnology to the study of human right
ventricular function is both possible and useful.
Research