Telomere Length Inversely Correlates With Pulse
advertisement

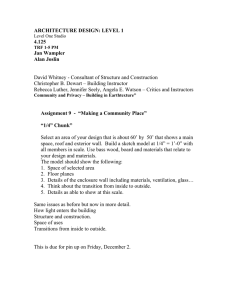
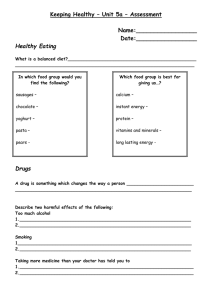
Telomere Length Inversely Correlates With Pulse Pressure and Is Highly Familial Elisabeth Jeanclos, Nicholas J. Schork, Kirsten O. Kyvik, Masayuki Kimura, Joan H. Skurnick, Abraham Aviv Abstract—There is evidence that telomeres, the ends of chromosomes, serve as clocks that pace cellular aging in vitro and in vivo. In industrialized nations, pulse pressure rises with age, and it might serve as a phenotype of biological aging of the vasculature. We therefore conducted a twin study to investigate the relation between telomere length in white blood cells and pulse pressure while simultaneously assessing the role of genetic factors in determining telomere length. We measured by Southern blot analysis the mean length of the terminal restriction fragments (TRF) in white blood cells of 49 twin pairs from the Danish Twin Register and assessed the relations of blood pressure parameters with TRF. TRF length showed an inverse relation with pulse pressure. Both TRF length and pulse pressure were highly familial. We conclude that telomere length, which is under genetic control, might play a role in mechanisms that regulate pulse pressure, including vascular aging. (Hypertension. 2000;36:195-200.) Key Words: blood pressure 䡲 pulse 䡲 age 䡲 twins T biological aging of replicating somatic cells in different organ systems of humans? A related question is: Is the aging of tissues from persons who are genetically endowed with long telomeres likely to occur later in life or at a slower pace than of tissues from persons who inherit short telomeres? Second, which biological parameters can serve as indicators of aging in human beings, since for obvious reasons chronological age (which is determined by calendar time) is a poor criterion for biological aging? In light of these considerations, this work had 2 goals. The first goal was driven by the following concept. Since in industrialized nations pulse pressure increases with age,13 pulse pressure might serve as a phenotype of cardiovascular aging. We therefore examined whether pulse pressure correlates with telomere length. The second goal was to examine whether telomere length is familial. elomeres, the ends of chromosomes, undergo attrition (shortening) in their length with each replicative cycle of cultured somatic cells (reviewed in References 1 through 4). This process also occurs in vivo because an inverse relation exists between telomere length in replicating somatic cells and the age of human beings who have donated these cells (References 5 through 9; reviewed in References 1 through 4). Thus, the replicative history of somatic cells is a major determinant of telomere length. Another determinant of telomere length is heredity, since the high variability in this parameter among human beings is to a large extent genetically determined.5 Recent experimental data support the concept that telomeres might serve as “biological clocks,” pacing not only life span at the cellular level but also aging at the systemic level. These data show that (1) the prevention of telomere attrition by the forced expression in cultured somatic cells of the catalytic component of telomerase, the reverse transcriptase that adds telomere repeats onto the ends of chromosomes, postpones replicative senescence10,11 and (2) the “knockout” of telomerase in the mouse amplifies some characteristics associated with systemic aging in later generations of mice that exhibit substantially shortened telomere length.12 At least 2 fundamental questions therefore arise with respect to the clinical implications of telomere biology. First, can the length of telomeres serve as an in vivo indicator of Methods Subjects DNA samples from white blood cells (WBCs) of 98 healthy twins (10 monozygotic and 39 dizygotic twin pairs) from the Danish Twin Register14 were selected to be studied. The ages of the subjects were 18 to 44 years. The twin pairs were identified in 1994 by responses to a questionnaire. They were selected for further investigation after they reported negative history for major metabolic, cardiovascular, and chronic inflammatory and infectious diseases. Clinical evaluation of and blood collection from Received December 20, 1999; first decision January 11, 2000; revision accepted February 29, 2000. From the Hypertension Research Center (E.J., M.K., A.A.) and the Department of Preventive Medicine and Community Health (J.H.S.), University of Medicine and Dentistry of New Jersey, New Jersey Medical School, Newark; the Department of Epidemiology and Biostatistics (N.J.S.), Case Western Reserve University, Cleveland, Ohio; the Program for Population Genetics and Department of Biostatistics (N.J.S.), Harvard University School of Public Health, Boston, Mass; the Jackson Laboratory (N.J.S., J.H.S.), Bar Harbor, Maine; and the Danish Twin Register (K.O.K.), Genetic Epidemiology Research Unit, Institute of Community Health, Odense University, Denmark. Correspondence to Abraham Aviv, Room F-464, MSB, Hypertension Research Center, University of Medicine and Dentistry of New Jersey, 185 S Orange Ave, Newark, NJ 07103-2714. E-mail avivab@umdnj.edu © 2000 American Heart Association, Inc. Hypertension is available at http://www.hypertensionaha.org 195 196 Hypertension August 2000 the co-twins of each twin pair were done on the same day. Evaluation included a physical examination with measurements of height, weight, and blood pressure. Blood pressure was carefully measured by a standard mercury sphygmomanometer, and the mean of 3 measurements was taken. Measurements were performed in a sitting position after 5 minutes of complete rest. Zygosity was established by HLA-typing and by serological analyses of blood enzyme systems. Approval to perform this research was obtained from the Danish Central Scientific Ethics Committee. Consent to send DNA to the United States was provided by the regional ScientificEthics Committee. Approval to perform the research was also granted by the Institutional Review Board of the University of Medicine and Dentistry of New Jersey–New Jersey Medical School. Measurement of Terminal Restriction Fragment Length DNA samples were coded in Odense University by means of numbers and the letters A and B, denoting the 2 co-twins of each twin pair. No other information (ie, zygosity, blood pressure, age, gender) was revealed by the code. The samples were digested overnight with restriction enzymes Hinf I (10 U) and RsaI (10 U) (Boehringer Mannheim). Eighteen DNA samples (⬇5 g each) from different individuals and 4 DNA ladders (1 kb DNA ladder plus 1 DNA/Hind III Fragments; GIBCO Life Technologies) were resolved in a 0.5% agarose gel (20⫻20 cm) at 50 V (GNA-200 Pharmacia Biotech). Duplicates from the same samples were resolved on different gels. The letter coding (ie, A and B) enabled the running of DNA samples from each twin pair on the same gel. After 16 hours, the DNA was depurinated for 30 minutes in 0.25N HCl, denatured for 30 minutes in 0.5 mol/L NaOH/1.5 mol/L NaCl, and neutralized for 30 minutes in 0.5 mol/L Tris, pH 8, 1.5 mol/L NaCl. The DNA was transferred for 1 hour to a nylon membrane, positively charged (Boehringer Mannheim) with the use of a vacuum blotter (Appligene, ONCOR). The membranes were then hybridized at 65°C with the telomeric probe (digoxigenin 3⬘-end labeled 5⬘-[CCCTAA]3) overnight in 5⫻SSC, 0.1% Sarkosyl, 0.02% SDS and 2% Blocking reagent (Boehringer Mannheim). The membranes were washed at room temperature, 3 times in 2⫻SSC, 0.1% SDS each for 15 minutes and once in 2⫻SSC for 15 minutes. The digoxigenin-labeled probe was detected by the digoxigenin luminescent detection procedure (Boehringer Mannheim) and exposed on x-ray film. The mean terminal restriction fragment (TRF) length was measured as described before.15 After completion of all TRF measurements in all samples, the numbers were decoded for data analysis. Data Analysis To assess the relation of measured factors (eg, gender, blood pressure, age) with telomere length while controlling for gross genetic effects on these phenotypes, we used a linear model with random effect or “variance component” terms (eg, see References 16 through 18). Let y1 and y2 denote telomere length values collected from a twin pair. Assume that the twin pair trait value vector, Y⫽[y1,y2], can be modeled with an appropriate bivariate distribution (eg, bivariate normal) with mean vector, , and variance-covariance matrix, ⍀, which can be partitioned in the following way: (1) ⍀⫽2K 2a⫹I2r where 2a and 2r are estimable variance components terms characterizing gross additive genetic effects (ie, aggregate additive effects of many loci), and random or “error” effects, respectively. The coefficient terms preceding these variance terms are 2⫻2 coefficient matrices relating the variance components to the twin pair trait values. Thus, K is the kinship coefficient matrix with off-diagonal elements equaling 1.0 for MZ twins and 0.5 for DZ twins, and I is the identity matrix. Assume further that can be modeled as ⫽f(X B), where X is vector of covariates (ie, gender, age) and B is an estimable regression parameter vector. For gender, men were assigned a value of 1.0 and women a value of 0.0. We assumed a linear relation between Y and X. The variance component terms and the parameter vector B can be estimated by maximum likelihood. Since we assumed bivariate normality of telomere length among twins and a linear relation between Y and X, the relevant log-likelihood equation is: (2) L(B, 2a,2r Y,X)⫽⫺(1/ 2)log ⍀ ⫺(1/ 2)(Y⫺BX)⬘⍀⫺1(Y⫺BX) Because more than 1 twin pair was collected, the log-likelihood equation was determined as the sum of the individual loglikelihood for each twin pair. Thus, our proposed model is essentially a standard regression model with dependent (paired) observations and special covariance structure. To test the relation of a measured factor, for example, pulse pressure, with telomere length, we tested the significance of the regression coefficient for that factor by using likelihood ratio tests. To safeguard against robustness issues, log-transformed variables were also tested. Note that heritability can be estimated as H⫽2a/(2a⫹2r). Because our model can accommodate multiple factors in the analysis, we also performed stepwise regressions that could determine the set of factors related to a chosen dependent variable that are statistically optimal and independent in their effects.19 It must be emphasized that by not directly testing other sources of “familial aggregation” beyond additive genetic effects (eg, shared diets, lifestyles, housing), any estimate of heritability from our analysis probably is biased. This is true for all twin and standard estimators of heritability that are not exhaustive in terms of the influences that they model. Results Table 1 summarizes general characteristics of the subjects, ignoring the relatedness of the twins. Reliability of the measurements of TRF length is described in Figure 1, which provides a scatterplot of the 2 TRF determinations and a plot of their difference versus the mean of the determinations. Table 2 describes the results of the analysis of the relation between each of the measured factors and TRF length, systolic blood pressure, diastolic blood pressure, and pulse pressure in univariate or pairwise settings. We also present the estimated percentage of variation in each primary variable that was explained by additive genetic random effects, after accounting for the effect of the measured factor. There was no significant correlation between TRF length and age within the age range of subjects in this group. However, gender showed a significant relation with TRF length in that women had longer TRF (also see Table 1). Of the blood pressure parameters, pulse pressure, which was correlated with age, showed the strongest relation with TRF length. TRF length was correlated positively with diastolic blood pressure but negatively with systolic blood pressure (Table 2), which is consistent with a negative relation between TRF length and pulse pressure. In addition, TRF length and pulse pressure were found to be highly heritable. The most parsimonious multivariate model (from the use of a stepwise regression analysis) for TRF length included only pulse pressure (slope⫽⫺0.01 kb/mm Hg, P⬍0.01; first row of Table 3). The most parsimonious multivariate model for pulse pressure included gender, age, and TRF length, which suggests that the relation between TRF length and pulse pressure is independent of gender and age. Jeanclos et al TABLE 1. Variable Gender, M/F Age Height Telomeres and Pulse Pressure 197 Characteristics of Subjects Participating in the Study Overall Mean⫾SD n Men, Mean⫾SD n 38/60 98 36.98⫾7.95 171.81⫾9.17 Women, Mean⫾SD 98 37.52⫾6.51 38 36.63⫾77 60 96 179.63⫾7.22 38 166.69⫾6.23 58 n Weight 72.24⫾18.06 96 83.42⫾20.31 38 64.91⫾11.76 58 BMI 24.47⫾0.37 96 25.17⫾0.41 38 26.72⫾0.29 58 SBP 115.07⫾17.52 96 125.21⫾19.99 38 108.43⫾11.84 58 DBP 64.56⫾9.72 96 65.75⫾9.32 38 63.78⫾9.97 58 PP 50.51⫾17.44 96 59.45⫾19.58 38 44.65⫾13.04 58 TRF 8.73⫾0.79 98 8.51⫾0.88 38 8.87⫾0.71 60 BMI indicates body mass index; SBP and DBP, systolic and diastolic blood pressure, respectively; PP, pulse pressure (ie, SBP⫺DBP); TRF, terminal restriction fragment. Units: Height (in cm), weight (in kg), BMI (in kg/m2), SBP and DBP (in mm Hg), and TRF (in kb). n is the number of individuals with nonmissing values used in the calculations. There were 10 monozygotic twins and 39 dizygotic twins. Figure 2 offers a graphical depiction of the relation between TRF length and pulse pressure, ignoring the relatedness of the twins. The parameters of the linear regression are Pulse Pressure⫽107.57⫺6.54 TRF (r⫽⫺0.30, P⫽0.0032). The parameters of the regression describing the relation between TRF length and pulse pressure in which average measures for each twin pair are plotted against each other are as follows: Pulse Pressure⫽111.0⫺6.93 TRF (r⫽⫺0.33, P⫽0.024). We note that for the multivariate models whose results are described in Table 3, some variables were not considered as potential predictor variables because of collinearity with other variables. Thus, systolic blood pressure and diastolic blood pressure were not considered in analyses involving pulse pressure because pulse pressure is defined by systolic and diastolic blood pressure values. We also note that the correlation between mean arterial pressure and TRF Figure 1. Scatterplot showing relation between first and second TRF length measurements made on each subject. The 2 measurements were performed 3 months apart. Dashed line represents line of identity. Solid line is regression line taking second measurement as a function of first measurement (equation: TRF2⫽0.136⫹0.985 TRF1 (r⫽0.963). Inset shows difference between first and second measurements plotted against mean of the 2 measurements. Solid line indicates mean difference (⫺0.009 kb). Dotted lines represent mean⫾2 SD (SD⫽0.296 kb). was negligible (r⫽0.07). The consequence is that in multiple regression models, pulse pressure was a significant predictor of TRF but mean arterial pressure was not. When pulse pressure and TRF were adjusted for mean arterial pressure, the partial correlation of pulse pressure and TRF (Figure 2) was actually stronger (r⫽⫺0.33). Although height was correlated with pulse pressure in this cohort (r⫽0.37, P⫽0.0002), height was not correlated with TRF (r⫽0.11, P⫽0.27). Height thus had little impact on the explanatory relation between TRF and pulse pressure; the partial correlations coefficient of pulse pressure and TRF after adjustment for height was r⫽⫺0.28, P⫽0.0005. Finally, analyses of the variables after log-transformation did not change the results appreciably (data not shown). Discussion The main finding of this work was that pulse pressure was inversely correlated with the TRF length in WBCs. This finding suggests that individuals who are endowed with relatively longer telomeres manifest a relatively narrow pulse pressure. In addition, this work showed that the mean length of telomeres and pulse pressure were highly familial. Our findings are discussed below. In industrialized nations, systolic blood pressure continuously rises throughout life (Reference 20; reviewed in Reference 13). Diastolic blood pressure also rises in early life, but it tends to level off or even decline in older persons. Hence, pulse pressure manifests progressive widening as a function of age. Arterial aging, particularly expressed by stiffness of central elastic arteries, is a major but not the only factor that determines pulse pressure; other determinants include left ventricular ejection rate and stroke volume. Perhaps the most important variable that determines central arterial stiffness is chronological age.20 –22 However, factors that might enhance the biological aging of the vasculature, including essential hypertension,23 non–insulin-dependent diabetes mellitus,24 and a high salt intake,25 have been independently shown to increase arterial stiffness. Collectively, these observations suggest that aortic pulse pressure might serve as a phenotype of biological aging of central arteries 198 Hypertension TABLE 2. August 2000 Pairwise Relations Between TRF Length, Blood Pressure, and Concomitant Factors Factor Cff TRF Gen N-t TRF – – – SBP ⫺0.01 Cff ⫺3.51 SBP Gen N-t 0.sx DBP Gen N-t Cff PP Gen N-t 90.7 47 2.73 79.2 48 ⫺6.11‡ 85.6 47 0.17* 95.9 47 – – – 79.5 47 0.83† 79.3 47 0.01* 95.8 48 0.33* 88.8 47 – – – ⫺0.66‡ 88.8 47 PP ⫺0.01‡ 96.4 47 0.72† 85.7 47 ⫺0.28‡ 85.7 47 – – – Gender ⫺0.40* 95.1 49 87.8 47 1.82 79.7 48 12.6‡ 82.9 47 DBP 14.1‡ BMI 0.00 95.7 48 6.80† 88.0 47 4.42* 81.5 48 3.39 82.3 47 Age ⫺0.01 95.4 49 0.74‡ 88.8 47 0.01 79.9 48 0.75‡ 83.3 47 Cff indicates maximum likelihood estimate of the regression coefficient for the listed factor (*P⬍0.05; †P⬍0.01; ‡P⬍0.005) by likelihood ratio test based on 2 with 1 degree of freedom; gender was coded as 0⫽female, 1⫽male; Gen, percentage of residual variation caused by genetic factors (see text); and N-t, sample size (number of twin pairs). Dash indicates that the factor was not tested. TRF indicates terminal restriction fragment; SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure (ie, PP⫽SBP⫺DBP). Note: After TRF and PP were log-transformed, they were still highly negatively correlated (⬍0.01). (for review, see Reference 26) and is a predictor of cardiovascular mortality and morbidity.27–30 We note, however, that the subjects in our study were as young as 18 years old. Therefore, their brachial pulse pressure was probably higher than that of their aortic or carotid pulse pressure, given their increased heart rate and amplification of the brachial systolic blood pressure.22,26 In addition, it is well established that height is a major determinant of the relation between pulse pressure and heart rate.26,31,32 Although in our cohort, height did not provide an explanation for the relation between pulse pressure and TRF length, height (and body mass index) must be evaluated as confounding factors in large-scale examinations of the TRF and pulse pressure. Some variations may exist in telomere length among somatic cells, probably as the result of different proliferative rates of tissues. Yet, in comparison to other persons, persons who exhibit either relatively short or long telomeres in one type of a proliferative somatic cell, respectively, express relatively short or long telomeres in other somatic cells (Reference 33; also K. Okuda and A. Aviv, unpublished data). Thus, the relation between TRF length and pulse pressure in the brachial artery might hold not only for telomeres in WBCs but also for telomeres in other replicating cells, including vascular endothelial cells8 and vascular smooth muscle cells.34 These cells play a pivotal function in blood pressure control and vascular aging. In addition, it is unlikely that height is a factor in heritability of TRF length, since no relation was observed in our cohort between TRF length and height. Not only pulse pressure but also the TRF changes with age.5–9 It appears, however, that different phases in the rate of telomere attrition exist throughout life.35 The initial phase (ie, birth to 5 years) is marked by a relatively high rate of telomere attrition. The subsequent phase that includes adolescence and young adulthood is marked by an apparent stabilization of telomere length. Thereafter, telomere attrition resumes at a slower rate than during the first 5 years of life. The majority of subjects we studied were within the age range in which the rate of telomere attrition slows down or levels off altogether, accounting for the lack of correlation between the telomere length and age in this group. In this study, we found that the TRF length in WBCs was highly familial, for example, confirming observations by Slagboom et al5 showing heritability of TRF length in lymphocytes. There is evidence that the TRF length differs among subpopulations of WBCs (eg, References 7 and 36), but as indicated earlier, the differences in the TRF length TABLE 3. Most Parsimonious Multiple Regression Models for TRF Length and Blood Pressure N-t Gender BMI PP Age TRF Gen. Ran TRF 47 NS NS ⫺0.01† NS – 84.0 16.0 SBP 47 13.83† NS – 0.72† NS 85.2 14.8 DBP 47 NS 4.52* – NS 2.78* 79.3 20.7 PP 47 10.82† NS – 0.70† ⫺4.24* 81.1 18.9 Each row corresponds to the model fitting results for the variable listed in the first column. Gender was coded as 0⫽female, 1⫽male; TRF, terminal restriction fragment; SBP, systolic blood pressure; DBP, diastolic blood pressure; and PP, pulse pressure (SBP⫺DBP). Entries are the maximum likelihood estimates of regression coefficients for the factors’ contribution to the model for which the variable listed in the first column was taken as the dependent variable, except for the “Gen” and “Ran” columns, which give the estimated fraction of residual variation explained by genetic and random factors, respectively. NS indicates not significant and therefore the factor was not included in the final model (ie, P⬎0.05), all listed coefficients were significant (*P⬍0.05); †P⬍0.01). Dash indicates that the factor was not tested in the model. N-t is the number of twin pairs with nonmissing values of all relevant variables. Jeanclos et al Telomeres and Pulse Pressure 199 References Figure 2. Relation between pulse pressure and TRF length. Regression line represents best-fit linear regression of pulse pressure on TRF. within subpopulations of somatic cells are far smaller than differences in the TRF length among persons of the same age. For instance, in the same donor, differences in telomere length between naı̈ve and memory T lymphocytes could at most reach 2 kb,7 whereas differences in WBCs or lymphocytes among donors of the same age could be as high as 5 kb.5,37 Thus, the respective findings by Slagboom et al5 and us in lymphocytes and WBCs indicate that high heritability of TRF length is likely to be expressed in all cell types. This conclusion was also reached by Martens et al.33 There are substantial data about heritabilities of systolic and diastolic blood pressures (reviewed in Reference 38) but little information about heritability of pulse pressure.39 Heritabilities of systolic and diastolic blood pressures in this study were higher than in previous reports.38 This may be due to the fact that our model did not accommodate other unmeasured factors, such as shared diets, living conditions, and so forth, which could contribute to similarity in twin values and be erroneously attributed to genetic effects. We propose that to gain a better appreciation of the link between telomere biology and vascular aging in human beings, large-scale investigations should be undertaken to explore further the relation between telomere length and pulse pressure at a wide age range. Acknowledgments Elisabeth Jeanclos is a postdoctoral fellow of the American Heart Association, Northeastern Consortium, Heritage Affiliate; Nicholas J. Schork is supported in part by National Institute of Health grants RR03655-11 from NCRR and HL-94011 and HL-54998 from the National Heart, Lung, and Blood Institute; Kirsten O. Kyvik was supported by the Danish Diabetes Association, Novo Nordic Foundation, and Sygekassernes Helsefond; Masayuki Kimura was partially supported by a grant-in-aid from the American Heart Association; and Abraham Aviv was partially supported by National Institutes of Health grant HL-47906. We thank Dr Anthanase Benetos for reading the manuscript and for his valuable comments. 1. Greider CW. Telomeres and senescence: the history, the experiment, the future. Curr Biol 1998; 8:R178 –R181. 2. Blackburn EH. Telomeres: no end in sight. Cell. 1994;77:621– 623. 3. Broccoli D, Cooke H. Aging, healing, and the metabolism of telomeres. Am J Hum Genet. 1993;52:657– 660. 4. Harley CB. Telomere loss: mitotic clock or genetic time bomb? Mutat Res. 1991;256:271–282. 5. Slagboom PE, Droog S, Boomsma DI. Genetic determination of telomere size in humans: a twin study of 3 age groups. Am J Hum Genet. 1994; 55:876 – 882. 6. Vaziri H, Schachter F, Uchida I, Wei L, Zhu X, Effros R, Choen D, Harley CB. Loss of telomeric DNA during aging of normal and trisomy 21 human lymphocytes. Am J Hum Genet. 1993;52:661– 667. 7. Weng NP, Levine BL, June CH, Hodes RJ. Human naive and memory T lymphocytes differ in telomeric length and replicative potential. Proc Natl Acad Sci U S A. 1995;92:11091–11094. 8. Chang E, Harley CB. Telomere length and replicative aging in human vascular tissues. Proc Natl Acad Sci U S A. 1995;92:11190 –11194. 9. Effros RB. Replicative senescence in the immune system: Impact of the Hayflick limit on T-cell function in the elderly. Am J Hum Genet. 1998;62:1003–1007. 10. Bodnar AG, Quellete M, Frolkis M, Holt SE, Chiu CP, Morin GB, Harley CB, Shay JW, Lichtsteiner S, Wright HE. Extension of life-span by introduction of telomerase into normal human cells. Science. 1998;279: 349 –352. 11. Morales CP, Holt SE, Quellete M, Kaur KJ, Yan Y, Wilson KS, White MA, Wright WE, Shay JW. Absence of cancer-associated changes in human fibroblasts immortalized with telomerase. Nat Genet. 1999;21: 115–118. 12. Rudolph KL, Chang S, Lee HW, Blasco M, Gottlieb GJ, Greider C, DePinho RA. Longevity, stress response, and cancer in aging telomerasedeficient mice. Cell. 1999;96:701–712. 13. Whelton PK, He J, Klag MJ. Blood pressure in Westernized population. In: Swales JD, ed. Textbook of Hypertension. London, UK: Blackwell Scientific Publications; 1994:11–21. 14. Kyvik KO, Green A, Beck-Nielsen H. The New Danish Twin Register: establishment and analysis of twinning rates. Int J Epidemiol. 1995;24: 589 –596. 15. Harley CB, Futcher AB, Greider CW. Telomeres shorten during aging of human fibroblasts. Nature. 1990;345:458 – 460. 16. Schork NJ. The design and use of variance component models in the analysis of human quantitative pedigree data. Biometrical J. 1993;4: 387– 405. 17. Schork NJ. Extended multipoint identity-by-descent analysis of human quantitative traits: efficiency, power, and modeling considerations. Am J Hum Genet. 1993;53:1306 –1319. 18. Searle SR, Casella G, McCulloch CE. Variance Components. New York, NY: John Wiley; 1992. 19. Neter J, Wasserman W, Kutner MH. Applied Linear Statistical Models. Homewood, Ill: Richard D. Irwin; 1985. 20. Franklin SS, Gustin W IV, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure: the Framingham Heart Study Circulation. 1997;96:308 –315. 21. Bramwell JC, Hill AV, McSwiney BA. The velocity of the pulse wave in man in relation to age as measured by the hot-wire sphygmograph. Heart. 1923;10:233–255. 22. Avolio AP, Deng FQ, Li WQ, Luo YF, Huang ZD, Xing LF, O’Rourke MF. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985;71:202–210. 23. Gribbin B, Pickering TG, Sleight P. Arterial distensibility in normal and hypertensive man. Clin Sci. 1979;56:413– 417. 24. Salomaa V, Riley W, Kark JD, Nardo C, Folsom AR. Non–insulindependent diabetes mellitus and fasting glucose and insulin concentrations are associated with arterial stiffness indexes: the ARIC study: Atherosclerosis Risk in Communities Study. Circulation. 1995;91: 1432–1443. 25. Avolio AP, Clyde KM, Beard TC, Cooke HM, Ho KK, O’Rourke MF. Improved arterial distensibility in normotensive subjects on a low salt diet. Arteriosclerosis. 1986;6:166 –169. 26. Nichols WW, O’Rourke MF. McDonald’s Blood Flow in Arteries. Theoretical, Experimental and Clinical Principles. 4th ed. London/Sydney/ Auckland; Arnold: 1998:347–376. 27. Darne B, Girerd X, Safar M, Cambien F, Guize L. Pulsatile versus steady component of blood pressure: a cross-sectional analysis on cardiovascular mortality. Hypertension. 1989;13:392– 400. 200 Hypertension August 2000 28. Benetos A, Rudnichi A, Safar M, Guize L. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32:560 –564. 29. Verducchia P, Schillaci C, Borgioni C, Ciucci A, Pede S, Procellati C. Ambulatory pulse pressure: a potent predictor of cardiovascular risk in hypertension. Hypertension. 1998;32:983–988. 30. Domanski MJ, Davis BR, Pfeffer MA, Kastantin M, Mitchell GF. Isolated systolic hypertension: prognostic information provided by pulse pressure. Hypertension. 1999;34:375–380. 31. Westerhof N, Elzinga G. Normalized input impedance and arterial decay-time over heart period are independent of animal size. Am J Physiol. 1991;261:R126 –R133. 32. Milnor WR. Aortic wavelength as a determinant of the relation between heart rate and body size in mammals. Am J Physiol. 1979;237:R3–R6. 33. Martens UM, Zijlmans JM, Poon SS, Dragowska W, Yui J, Chavez EA, Ward RK, Lansdorp PM. Short telomeres on human chromosome 17p. Nat Genet. 1998;18:76 – 80. 34. Okuda K, Khan MY, Skurnick J, Kimura M, Aviv H, Aviv A. Telomere attrition of the human abdominal aorta: relationship with age and atherosclerosis. Atherosclerosis. In press. 35. Frenck RW Jr, Blackburn EH, Shannon KM. The rate of telomere sequence loss in human leukocytes varies with age. Proc Natl Acad Sci U S A. 1998;95:5607–5610. 36. Weng NP, Granger L, Hodes RJ. Telomere lengthening and telomerase activation during human B cell differentiation. Proc Natl Acad Sci U S A. 1997;94:10827–10832. 37. Jeanclos E, Krolewski A, Skurnick J, Kimura M, Aviv H, Warram JH, Aviv A. Shortened telomere length in white blood cells of patients with IDDM. Diabetes. 1998;47:482– 486. 38. Ward R. Familial aggregation and genetic epidemiology of blood pressure. In: Laragh JH, Brenner BM, eds. Hypertension: Pathophysiology, Diagnosis, and Management. New York, NY: Raven Press; 1990:81–100. 39. Darlu P, Sagnier PP, Bois E. Evidences pour une transmission genetique de la pulsatilte arterielle. C R Acad Sci III. 1994;317:62– 69.