SMALL, SMALLER, SMALLEST– SILVER- RUSSELL TO
advertisement

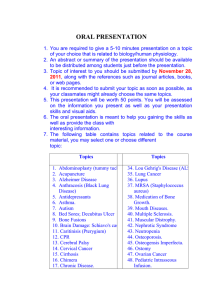
SMALL, SMALLER, SMALLEST– SILVERRUSSELL TO PRIMORDIAL DWARFISM Dr. Judith G. Hall, OC, MD The University of British Columbia Vancouver, BC Canada CAUSES OF GROWTH RESTRICTION ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Bone disorders - chonrdrodysplasias, rickets Nutritional - chronic infection, Celiac disease, Crohn’s disease, malabsorption Congenital anomalies - cardiac, renal, CNS Metabolic - renal acidosis, glycogen storage disease, etc. Emotional - psychosocial dwarfism Endocrine - hypothyroidism, hypopituitarism, Cushing’s disease Intrauterine growth retardation - Turner syndrome, small for dates, many syndromes, infection, chromosomal anomalies Normal variation - familial short stature, constitutional delay HOW TO APPROACH SHORT STATURE? 1. 2. 3. 4. 5. Present at birth vs. later onset (i.e., IUGR, SGA, primordial) Proportionate vs. non-proportionate – relative to what? How short is short? When falls off centiles in utero Growth pattern after birth IUGR – Intrauterine Growth Retardation SGA – Small for Gestational Age PRIMORDIAL – Prior to Birth ¾ IUGR = SGA = PRIMORDIAL ¾ Below the 3rd centile for gestational age ¾ How far below? ¾ Relative centiles of OFC, length, and weight NATURE’S RULE OF THUMB OFC > LENGTH > WEIGHT i.e., Preserve the brain if you can RELATIVE TO WHAT AT WHAT AGE? ¾ OFC, length/height, weight FOR AGE (and to each other) ¾ OFC, length/height, weight FOR HEIGHT AGE ¾ OFC, length/height, weight FOR BONE AGE PROPORTIONAL VS. NON-PROPORTIONATE (MIDGET) (DWARF) ¾ Length/height compared to span ¾ Upper/lower segment ¾ Proximal, middle, distal HERE WE ARE TALKING ABOUT: ¾ IUGR/SGA (prenatal) ¾ Relatively proportionate short stature postnatally ¾ Very, very small types of syndromes Centiles have little meaning way, way, way, below 3rd centile! >>>3rd centile Significant IUGR Relatively PROPORTIONATE/POST NATAL SHORT STATURE DISORDERS 1. 2. 3. 4. 5. 6. 7. 8. Bloom* Dubowitz Floating Harbor MOPD II* Mulibrey* Silver-Russell/Russell-Silver*** SHORT 3-M* Also: Chromosomal, CPM, and teratogens A B C TERM DELIVERY ADULT HEIGHT OFC FLOATING HARBOR 2460 gm 46.8 cm 130 cm-140 cm Slow growth OFC wnl for age Mild MR MULIBREY 2400 gm 45 cm 2nd best 150 cm Relative macrocephalic DUBOWITZ 2300 gm 45 cm 4th best 146 cm MR 75% Microcephaly 100% SHORT 2200 gm 45 cm 154 cm Best growth OFC about 10% for age 3 -M 2100 gm 40 cm 120 cm-136 cm Relative macrocephaly BLOOM 1850 gm 44 cm 3rd best 148 cm Mild MR Mild microcephaly R -S 1200 gm – 2500 gm 150 cm males heterogenous 35 cm – 50 cm 140 cm females Relative macrocephaly MOPD II Start off proportionate become 1000 gm 35 cm 100 cm Worst!! RUSSELL-SILVER/SILVER-RUSSELL PHENOTYPE Silver et al 1953, Russell 1954 (no asymmetry) ¾ Small body compared to head; head is normal for age; and therefore, big relative to body ¾ Pseudohydrocephaly, “macrocephaly” ¾ Relatively underweight ¾ Asymmetry ~ 50% (hemihypotrophy) ¾ Delayed bone age, but grow parallel to 3rd centile RUSSELL-SILVER/SILVER-RUSSELL PHENOTYPE - 2 OFTEN PRESENT ¾ High forehead ¾ Triangular shaped face ¾ Clinodactyly ¾ Café au lait spots ¾ Special education needs 35% RUSSELL-SILVER/SILVER-RUSSELL PHENOTYPE - 3 OCCASSIONAL - ? REFLECT HETEROGENEITY ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Syndactyly 20% Hypoglycemia (45% of non UPD) Excessive sweating, tachycardia Congenital dislocated hip 12% Hypospadias, cryptorchidsm in 20% males Scoliosis 36% Bluish sclerae Apparently low set ears WEIGHT < HEIGHT < OFC ¾ Programming ¾ Nutrition ¾ Fetal survival Placental deficiency/insufficiency z Placental (CPM) mosaicism ¾ Imprinting/epigenetic z ¾ ¾ ¾ Chromosome 7 z Mat UPD 7 z 7p11.2-13 mat dUp and other z 7q11q1-p14 translocations z 7q25 translocation z Pat 7q32 disruptions z Mat 7q32 UPD Trisomy 7 mosaicism 11p15 demethylation z Mat duplication z Opposite of BWS ¾ 15q26.1 – qter deletions z Rings ¾ ¾ 17q22-q24, pat deletion 17q25 10% 1% (x 11) 30% 2% 1x ¾ ¾ ¾ AR, AD families Chromosome 8, 15, 17, 18 Discordant MZ twins z ? All 11p15? ¾ Unknown _______ 50% 50% WHAT WE HAVE LEARNED ABOUT IMPRINTING? ¾ Deletion ¾ UPD (milder) ¾ Point mutation ¾ Duplications ¾ Imprinting control center change ¾ Methylation changes (LOI) ¾ Tissue specific expression RS/SR Imprinted genes normal expression 7 UPD mat p11.1-p14 Mat UPD (?1GFBP1↑) Pericentric inversion Point mutation q32 Mat dup and UPD 11p15 Mat dysfunction Mat UPD Loss of paternal methylation DMR FOX2 pat FOX2 pat GRB10 pat GRB10 pat (C7oef10-11) PEG/MIST mat PEG/MIST (CoPg2 Copg2AS, and MITI, IMP3?) H19 mat H19 H19 15q26.1-qter IGFIR ? 17q23.3-q25 CHS1 ? KPN2 GRB2 and 7 Disruption ↓ ↓ -- ↑ ↑ CHROMOSOME 7 ¾ ¾ ¾ ¾ ¾ Mat UPD 7 5%-10% z Special education z Speech delay (absence of FOXP2) z Fewer minor dysmorphic features z No asymmetry z Recessive disorders z Mat iso 3:5 hetero 7p11.2-p14 – mat duplication (GRB10 paternally imprinted – point mutations) z (3 AD families) z TX and pericentric 7q mat UPD 13 – qter (PEG1/MEST maternally imprinted) 7q32 translocation breakpoint and ∂2-COP Trisomy 7 rescue with residual T7 cells CHROMOSOME 11P15 – 40% ¾ ¾ ¾ ¾ ¾ ¾ Demethylation of ICR and pat H19 z regulation of IGF2 expression, biallelic z expression of H19 – with hypomethylation H19 Opposite of BWS Asymmetry frequent (fibroblast studies important) ? Cancer risk (small) Mat duplication 11p15 (35% of the 40%) also UPD Discordant MZ twins CHROMOSOME 15 ¾ 15q26.1-qter deletions and rings apparently loss of functional IGF1R CHROMOSOME 17 ¾ 17q24.1-q25 translocations, 2% deletions z Apparently pat CSH1 expression lost RS/S/R PRACTICAL ASPECTS ¾ Early feeding problems Hypoglycemia ? GH therapy, androgenic hormone Leg lengthening discrepancy (> 3 cm) Cryptorchidism for males Speech/language development ¾ Hundreds of cases reported ¾ ¾ ¾ ¾ ¾ ¾ Very rarely familial RUSSELL-SILVER/SILVERRUSSELL DIFFERENTIAL DIAGNOSIS ¾ DNA repair ¾ Partington 3-M syndrome Fetal alcohol syndrome IMAGe syndrome Chromosomal Diploid/triploid mixoploidy Mosaic Turner syndrome Y q deletions Trisomy 18 and 18p - ¾ ¾ ¾ ¾ Fanconi anemia Nijmegen breakage Bloom syndrome X-linked with hyperpigmental skin RUSSELL-SILVER/SILVER-RUSSELL REFERENCES ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Bailey W et al. Monozygotic twins discordant for the Russell-Silver syndrome. Am J Med Genet 1995;58:101-105. Bliek J et al. Hypomethylation of the H19 gene causes not only Silver-Russell synrome (SRS) but also isolated asymmetry or an SRS-like phenotype. Am J Hum Genet 2006; 78:604-614. Dupont JM et al. Familial Reciprocal Translocation t(7;16) associated with maternal uniparental disomy 7 in a Russel-Silver patient. Am J Med Genet 2002;111:405408. Font-Montgomery E et al. Clinical outcome and follow-up of the first reported case of Russell-Silver syndrome with the unique combination of maternal uniparental heterodisomy 7 and mosaic trisomy 7. Birth Defects Res A 2005; 73:577-582. Gicquel C et al. Epimutation of the telomeric imprinting center region on chromosome 11p15 in Silver-Russell syndrome Nat Genet 2005; 37:1003-1007. Hannula K et al. Do patients with maternal uniparental disomy for chromosome 7 have a distinct mild Silver-Russell phenotype?. J Med Genet 2001;38:273-278. Hitchins MP et al. Investigation of the GRB2, GRB7, and CSH1 genes as candidates for the Silver-Russell syndrome (SRS) on chromosome 17q. J Med Genet 2002;39:E13. Kotzot D et al. Maternal uniparental disomy 7 - review and further delineation of the phenotype. Eur J Pediatr 2000;159:247-256. Matsumoto N. A 4-Mb critical region for intrauterine growth retardation at 15q26. Clin Genet 2002; 62:340-342. Monk D et al. Chromosome 7p disruptions in Silver Russell syndrome: delineating an imprinted candidate gene region. Hum Genet 2002;111:376-387. Schonherr N et al. The centromeric 11p15 imprinting centre is also involved in SilverRussell syndrome. J Med genet 2007; 44:59-63. Tamura T et al. Ring chromosome 15 involving deletion of the insulin-like growth factor 1 receptor gene in a patient with features of Silver-Russell syndrome. Clin Dysmorphol 1993;2:106-113. MULIBREY NANISM Muscle Liver Brain Eye Perhentupa et al 1970 - Finnish ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Large dolicocephalic cranium with high prominent forehead Triangular shaped face Depressed bridge of nose 90% Muscle wasting Hands & feet appear large Yellowing of retina with yellow spots 80% Constrictive pericarditis 35% - (congestive heart failure) Enlarged liver with prominent veins 45% Long shallow sella turcica (J shaped) MULIBREY NANISM- 2 ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Hypotonia 70 % Thin long bones with narrow medullary canal 100% Fibrous dysplasia of tibia 25% High pitched voice 96% Nevus flammeus 65% Ovarian stromal tumors Wilms tumor 4% Incomplete breast development in females Premature ovarian failure & subsequent infertility in females MULIBREY NANISM- 3 ¾ ¾ ¾ ¾ Autosomal recessive – with consanguinity Over 80 reported cases Finland (85%) and Egypt, France, Turkey, Argentina, Spain Mutations occur in TRIM 37 – 17q21 - q24 • Encodes peroxisomal protein whose function is unknown – it shows a granular cytoplasmic pattern in cells • It is a RING – B – box-wild-coil protein • Ubiqutin E3 ligase MULIBREY NANISM- 4 MANAGEMENT ¾ Feeding problems early ¾ Pericardiectomy often necessary ¾ GH therapy little increase in ultimate weight ¾ Females have spontaneous puberty, then ovarian failure, oligomenorhea, and infertility MULIBREY NANISM- 5 DIFFERENTIAL DIAGNOSIS ¾ Russell-Silver syndrome ¾ 3-M syndrome ¾ Meier Gorlin syndrome MULIBREY NANISM- 6 REFERENCES ¾ ¾ ¾ ¾ ¾ ¾ ¾ Avela K et al. Gene encoding a new RING-B-box-Coiled coil protein is mutated in mulibrey nanism. Nature Genetics 2000;25:298- 301. Balg S et al. Mulibrey nanism. Clin Dysmorphol 1995;4:63-69. Hamalainen RH et al. Wilms’ tumor and novel TRIM37 mutations in an Australian patient with mulibrey namism. Clin Genet 2006 70:473479. Jagiello P et al. A novel splice site mutation in the TRIM37 gene causes mulibrey nanism in a Turkish family with phenotypic heterogeneity. Hum Mutat 2003; 21:630-635. Karlberg N et al. Mulibrey nanism: clinical features and diagnostic criteria. J Med Genet 2004;41:92-98. Karlberg N e al. Failure of sexual maturation in mulibrey nanism. NEJM 2004; 351:2559-2560. Lapunzina P et al. Mulibrey nanism: three additional patients and a review of 39 patients. Am J Med Genet 1995;55:349-355. 3–M Miller McKusick Malvaux et al. 1975 ¾ ¾ ¾ ¾ ¾ ¾ Relatively large head, dolicocephaly, with frontal bossing, 50th centile for age Short broad neck with prominent trapezius, square shoulders Deformed sternum, short thorax Transverse grooves on anterior chest, flaring of bottom of chest, transverse ribs Square shoulders with winged scapulae Triangular face, hypoplastic midface, long philtrum, prominent lips, “gloomy facies” 3 – M – (2) ¾ Full eyebrows ¾ Prominent ears ¾ Fleshy nose tip ¾ Crowded teeth, V-shaped dental arch ¾ Short fifth finger ¾ Hypospadius and hypogonadism in males 3 – M – (3) Miller McKusick Malvaux et al. 1975 ¾ Hyperlordosis ¾ Loose joints ¾ Slender long bone with diaphyseal constriction and flared metaphyses ¾ Tall vertebrae ¾ Thoracic kyphoscoliosis ¾ ? CNS aneurysms 3 – M – (4) TREATMENT ¾ Feeding problems ¾ Male cryptorchidism, infertility ¾ Watch for kyphoscolosis 3 – M – (5) ¾ Autosomal recessive, increased consanguinity ¾ Heterozygotes may have minor clinical features ¾ About 100 cases reported ¾ Cullin 7 gene, 25 different mutations in 29 families ¾ CUL7 assembles an E3 ubiquitin ligase complex 3 – M – (6) Miller McKusick Malvaux et al. 1975 DIFFERENTIAL DIAGNOSIS ¾ Russell-Silver syndrome ¾ Bloom syndrome ¾ Mulibrey Nanism 3 – M – (7) REFERENCES ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Hennekam RCM et al. Further delineation of the 3-M syndrome with review of the literature. Am J Med Genet 1987;28:195-209. Huber C et al. Identification of mutations in CUL7 in 3-M syndrome. Nature Genet 2005;37:1119-1124. Le Merrer M et al. Dwarfism with gloomy face: a new syndrome with features of 3-M syndrome. J Med Genet 1991;28:186-191. Maksimova N et al. Clinical, molecular and histopathological features of short stature syndrome with novel CUL7 mutation in Yakuts: new population isolate in Asia. J Med genet 2007;44:772-778. Miller JD et al. The 3-M syndrome: a heritable low birthweight dwarfism. BDOAS 1975;11(5):39-47. Mueller RF et al. The 3-M syndrome: risk of intracerebral aneurysm?. J Med Genet 1992;29:425-427. van der Wal G et al. 3-M syndrome: description of six new patients with review of the literature. Clin Dysmorphol 2001;10:241-252. Winter RM et al. The 3-M syndrome. J Med Genet 1984;21:124-128. SHORT SYNDROME (Gorlin et al and Sensenbrenner et al, 1975) ¾ Short stature ¾ Hyperextensible joints/inguinal hernia ¾ Ocular depression (deep set, large appearing eyes) ¾ Rieger anomaly (megalocornea, anterior segment dystrophy, glaucoma, and lens opacities) ¾ Teething delay (small teeth, enamel hypoplasia, malocclusion) SHORT SYNDROME - 2 Speech delay (36 months) with normal intelligence ¾ Triangular shaped face z Broad forehead, small chin, small facial bones z Telecanthus, deep set eyes, Reiger anomaly z Hypoplastic alae, broad nasal bridge ¾ Micrognathia, dimple in chin ¾ Dental eruption delay and bone age delay ¾ SHORT SYNDROME - 3 ¾ ¾ ¾ ¾ ¾ ¾ Feeding problems (V & D) and FTT Decreased subcutaneous fat, lipodystrophy – dystrophy of face & upper limbs and subcutaneous pits in elbows, and buttocks DM related to insulin resistance after puberty & GH RX Thin hair & skin transparent Occasional neurosensory deafness Ears – relatively larger, parallel creases, apparently posterior angle SHORT SYNDROME - 4 ¾ Hyperextensible hands ¾ Clinodactyly 5th ¾ Large & cone shaped epiphyses ¾ Thin, gracile, long bones SHORT SYNDROME - 5 ¾ ¾ ¾ ¾ 20 cases ? 2 AR families; ?4 AD with non penetrance Equal males and females Translocation 1q31.2/4q25, ? PITX2 mutation SHORT SYNDROME – 6 DIFFERENTIAL DIAGNOSIS ¾ GMS ¾ DeHawere syndrome ¾ Russell-Silver syndrome ¾ Polycystic ovary disease SHORT SYNDROME – 7 REFERENCES Bankier A et al. Absent iris stroma, narrow body build and small facial bones: a new association or variant of SHORT syndrome?. Clin Dysmorphol 1995;4:304-312. Brodsky MC et al. Rieger anomaly and congenital glaucoma in the SHORT syndrome. Arch Ophthal 1996;114:1146-1147. Haan E et al. SHORT syndrome: distinctive radiographic features. Clin Dysmorphol 1998;7:103-107. Joo SH et al. Case report on SHORT syndrome. Clin Dysmorphol 1999;8:219-221. Koenig R et al. SHORT syndrome. Clin Dysmorphol 2003;12:45-50. Lipson AH et al. The SHORT syndrome: further delineation and natural history. J Med Genet 1989;26:473-475. Schwingshandl J et al. SHORT syndrome and insulin resistance. Am J Med Genet 1993;47:907-909. Sorge G et al. SHORT syndrome: a new case with probable autosomal dominant inheritance. Am J Med Genet 1996;61:178-181. FLOATING HARBOR SYNDROME Boston Floating Hospital – Harbor General Hospital (Pelletier et al 1973, Leisti et al 1974) Developmental delay, particularly speech 100% z Mild MR, some with hyperactivity ¾ Craniofacial – triangular face (round in infancy) z Broad nose, bulbous with prominent nasal bridge z Prominent eyes early, deep set later z Wide mouth, thin lips z Broad columella z Smooth and short philtrum z Large nares, hypoplastic alae z Posteriorly rotated ears, appear lowset ¾ ¾ Head circumference normal for age FLOATING HARBOR SYNDROME - 2 ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Clinodactyly of 5th (nail hypoplasia), brachydactyly, broad thumbs, Appear proportionate Decreased subcutaneous tissue Short neck, with low hairline Hirsuitism and long eye lashes Joint laxity – 50% Trigonencephaly Celiac disease Occasional high pitched voice Tethered cord x1 FLOATING HARBOR SYNDROME - 3 ¾ Delayed BA 100% - but puberty on time ¾ Clinodactyly of 5th in 75% and coned epiphyses ¾ Brachydactyly 50% ¾ Finger clubbed 45% ¾ Pseudoarthrosis of clavicle FLOATING HARBOR SYNDROME – 4 ¾ About 20 cases ¾ Mostly sporadic M:F – 1:2 ¾ Consanguinity, 1 set of female sibs ¾ Advanced paternal age in most ¾ x 3 mother daughter affected – doubtful ¾ Gene Unknown FLOATING HARBOR SYNDROME – 5 DIFFERENTIAL DIAGNOSIS ¾ Silver – Russell syndrome ¾ Shprintzen syndrome ¾ 3-M syndrome ¾ Dubowitz syndrome ¾ Rubinstein – Taybi syndrome FLOATING HARBOR SYNDROME - 6 REFERENCES Ala-Mello S et al. The first Finnish patient with the Floating-Harbor syndrome: the follow-up of eight years. Am J Med Genet 2004;130A:317-319. Davalos IP et al. Floating-Harbor syndrome. A neuropsychological approach. Genetic Counseling 1996;7:283-288. Feingold M. Thirty-two year follow-up of the first patient reported with the Floating-Harbor syndrome. Am J Med Genet 2006;140A: 782-784. Hersh JH et al. Changing phenotype in Floating-Harbor syndrome. Am J Med Genet 1998;76:58-61. Lacombe D et al. Floating-Harbor Syndrome: description of a further patient, review of the literature, and suggestion of autosomal dominant inheritance. Eur J Pediatr 1995;154:658-661. Patton MA et al. Syndrome of the month: Floating-Harbor syndrome. J Med Genet 1991;28:201-204. Rosen AC et al. A further report on a case of Floating-Harbor Syndrome in a mother and daughter. J Clin Exp Neuropsychol 1998;20:483-495. Wiltshire E et al. Floating-Harbor syndrome complicated by tethered cord: A new association and potential contribution from growth hormone therapy. Am J Med Genet 2005;136A:81-83. BLOOM SYNDROME (Bloom 1954, German F/U) ¾ ¾ ¾ ¾ ¾ Microcephaly – mildly/small for size Malar mypoplasia Telangiectasia and erythema of face (butterfly distribution) Pigment abnormalities and atrophic scars (photosensitivity by 2 years) Increased risk of tumors: leukemia, lymphoma, adenocaricoma, squamous cell, carcinoma, and Wilm’s (at least 44% affected, mean age of onset 25 years) BLOOM SYNDROME – 2 ¾ High squeaky voice ¾ Immune deficiency and reduced 1gA, 1gG, 1gM ¾ Chronic infections (particularly chronic lungs 20%) ¾ Male infertility with small testes, females fertile with premature menopause BLOOM SYNDROME - 3 ¾ Delayed puberty (and BA) ¾ DM 16% - type 2 after puperty ¾ Mild MR – normal IQ with learning disability ¾ Feeding problems in infancy ¾ Male infertility with small testes, females fertile with early menopause BLOOM SYNDROME - 4 ¾ Increase sister chromatid exchange (SCE) breakage, dicenrics, tetraradials BLOOM SYNDROME - 5 ¾ ¾ ¾ ¾ ¾ ¾ Autosomal recessive Mutations in BML (15q26.1) which is a protein homolous to REC Q helicase 64 mutations, 2 Ashkenazi mutations Ashkenazi Jew carrier rate about 1% Unwinds DNA in 3’ to 5’ direction along bound strand, nuclear cell cycle regulator Other DNA helicase disorders - Werner, Rothman Thompson Bloom syndrome registry ~ 150 patients maintained by German & Passarge - Helps to clarify the natural history BLOOM SYNDROME - 7 DIFFERENTIAL DIAGNOSIS ¾ Russell Silver syndrome ¾ Rothmund Thompson syndrome ¾ Cockayne syndrome ¾ Ataxia Teliangectasia ¾ Fanconi Anemia BLOOM SYNDROME - 8 REFERENCES Auerbach AD et al. Disorders of DNA replication and repair. Curr Opin Pediatr 1997;9:600-616. Chisholm CA et al. Successful pregnancy in a woman with Bloom syndrome. Am J Med Genet 2001;102:136-138. Ellis NA et al. Molecular genetics of Bloom's syndrome. Hum Mol Genet 1996;5:1457-1463. Ellis NA et al. The Bloom's sydrome gene product is homologous to RecQ helicases. Cell 1995;83:655-666. Mohaghegh P et al. DNA helicase deficiencies associated with cancer predisposition and premature ageing disorders. Hum Mol Genet 2001;10:741-746. Passarge E. Bloom's syndrome: the German experience. Ann Genet (Paris) 1991;34:179-197. DUBOWITZ SYNDROME - 1 Dubowitz 1965 ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ DD & MR – mild – moderate (72%) Hyperactivity 70% Shy, short attention span Speech delay 67% High pitched voice 55%, hoarse cry 30% Microcephaly, high sloping forehead 80%, flat superorbital ridges 90%, present at birth Exzema – like skin disorder on face & flexion areas, 60% from birth, clears 2 – 4 years Space hair, especially frontal 70% and lateral eyebrows 45% DOBOWITZ SYNDROME – 2 ¾ ¾ ¾ ¾ ¾ ¾ FTT - Muscular hypotonia 40% Delayed BA 50% Faces become triangular Broad nasal tip 50% and broad base to nose Telecanthis with prominent epicanthal folds, ptosis 65%, blepharophimosis 80% Apparently low set, prominent, dysmorphic ears 75% DOBOWITZ SYNDROME – 3 ¾ Small chin 80%, with age becomes long square chin ¾ Clinodactyly of fifth - 50% and syndactyly 20% ¾ Males hypospadias, cryptorchidism 50% ¾ Leukemia, lymphoma, neuroblastoma, and aplastic anemia have been reported DOBOWITZ SYNDROME – 4 ¾ ¾ ¾ ¾ 150 cases AR many with consanguinity ? Subtypes • ? Anorectal & craniosynostosis subtypes • Immune deficiency and frequent infection • Low cholesterol Gene unknown DOBOWITZ SYNDROME – 5 DIFFERENTIAL DIAGNOSIS ¾ FAS syndrome ¾ Bloom syndrome ¾ Smith-Lemli-Opitz syndrome ¾ 22q- syndrome DOBOWITZ SYNDROME – 6 REFERENCES Hansen KE et al. Dubowitz syndrome: long-term follow-up of an original patient. Am J Med Genet 1995;55:161-164. Ilyina HG et al. Dubowitz syndrome: possible evidence for a clinical subtype. Am J Med Genet 1990;35:561-565. Moller KT et al. The Dubowitz syndrome: a retrospective. J Cranio Gen Dev Bio 1985;5:283-286. Parrish JA et al. Studies of the density and the properties of the hair in a new inherited syndrome of hypotrichosis. Ann Hum Genet 1972;35:349-356. Tsukahara M et al. Dubowitz syndrome: review of 141 cases including 36 previously unreported patients. Am J Med Genet 1996;63:277-289. Winter RM. Syndrome of the month: Dubowitz syndrome. J Med Genet 1986;23:11-13. MAJEWSKI (MICROCEPHALIC) OSTEODYSPLASTIC PRIMORDIAL DWARFISM II Majewski et al 1982 ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Severe IUGR < 1000 gm at term Severe postnatal short stature – around 100 cm as adult At birth, proportionate OFC (28 weeks at term) Progressive relative true microcephaly Forehead lacks posterior slant, in fact tall, forehead Small dysplastic teeth (or absent) compared to mouth size High squeaky voice Prominent nose and eyes MOPD II - 2 ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Progressive bony changes and loose jointedness with disproportionate shortening of mesomelic segment Brachydactyly Bowed legs Develop café au lait spots May have depigmentation spots Develop dark pigment with some acanthesis around neck & axilla Far sighted, short globe Pleasant personality MOPD II - 3 ¾ Develop intracranial aneurysm ¾ Develop truncal obesity ¾ Rarely DM ¾ Cutis mamorata seen ¾ Males cryptorchidism, hypospadias, micropenis ¾ Reduced life expectancy – oldest 40 years old ¾ No increase in cancer noted MOPD II – 4 MANAGEMENT ¾ Feeding problems ¾ Little or no response to GH ¾ Scoliosis may develop ¾ CNS aneurysm need to be screened for ¾ Avoid sun ¾ Watch for dislocation radius & knees ¾ Danger from being so small ¾ Watch for DM MOPD II - 5 ¾ Autosomal recessive with consanguinity ¾ Increase among Mediterranean countries ¾ Variability in same family ¾ About 100 cases reported MOPD II - 6 ¾ Percentrin (PCNT) mutations ¾ Component of centrosome complex ¾ Role in cell division (mitosis) ¾ Helps to organize mitotic spindle for segregation and anchoring of spindle ¾ Giant coiled coil protein localized to centrosome througout cell cycle ¾ 21q22.3 MOPD II - 7 ¾ Meier-Gorlin syndrome ¾ Floating Harbor syndrome ¾ 3 – M syndrome ¾ SHORT syndrome ¾ Seckels syndrome ¾ MOPD I and III MOPD II – 8 REFERENCES ¾ ¾ ¾ ¾ ¾ ¾ ¾ Brancati F et al. Majewski osteodysplastic primordial dwarfism type II (MOPD II) complicated by stroke: Clinical report and review of cerebral vascular anomalies. Am J Med Genet 2005;139A:212-215. Hall JG et al. Majewski osteodysplastic primordial dwarfism type II (MOPD II): natural history and clinical findings. Am J Med Genet 2004;130A:55-72. Kannu P et al. Microcephalic osteodysplastic primordial dwarfism type II: a child with cafe au lait lesions, cutis marmorata, and moyamoya disease. Am J Med Genet 2004;128A:98-100. Nishimura G et al. Microcephalic osteodysplastic primordial short stature type II with cafe-au-lait spots and moyamoya disease. Am J Med Genet 2003;117A:299-301. Ozawa H et al. Pachygyria in a girl with microcephalic osteodysplastic primordial short stature type II. Brain Dev 2005;27:237-240. Rauch A et al. Mutations in the pericentrin (PCNT) gene cause primoridal dwarfism. Science 2008;319:816-819. Young ID et al. Microcephalic osteodysplastic primordial short stature type II with cafe-au-lait spots and moyamoya disease: another patient. Am J Med Genet 2004;127A:218-220. SUMMARY 1 ALL PROPORTIONATE, IUGR, AND POSTNATAL SHORT STATURE ¾ Bloom syndrome z Mild microcephaly, malar hypoplasia z Telangectasia erythemations rash on cheeks and with sun exposure ¾ Floating Harbor syndrome z Speech delay - mild MR z Changing face – prominent nose, short philtrum z BA delay, but puberty on time ¾ SHORT z Riegers (lens opacity, glaucoma), eyes large appearing, then deepset z Lipodystrophy of face and upper torso z Speech delay – IQ okay z Hypoplastic alae, prominent nose as adults ¾ SUMMARY 2 ALL PROPORTIONATE, IUGR, AND POSTNATAL SHORT STATURE Dubowitz syndrome z Relative microcephaly z Eczema z Sparce lateral eyebrows z Telecanthus, prominent epicanthal folds ¾ Russell-Silver/Silver-Russell z Normal size head (pseudohydrocephaly) z Relatively underweight z 50% asymmetric z BA delay, late puberty ¾ Mulibrey Nanism z Large, long head with triangular face with depressed bridge of nose z Constructive pericarditis and heart failure with liver enlargement z Yellow pigment and spots in retina z Fibrosis of ovaries, fibrodysplasia of tibia SUMMARY 3 ALL PROPORTIONATE, IUGR, AND POSTNATAL SHORT STATURE ¾ 3-M z Short thorax with sternal deformity, transverse ribs, rib groove z Broad neck, square shoulders, prominent trapezius z Triangular face, full lips, hypoplastic midface, long philtrum ¾ MOPD II z Severe pre & postnatal growth z Progressive microcephaly, high forehead z Prominent nose, small teech, squeaky voice z Progressive boney dysplasia SEVERE IUGR ¾ Epigenetic control of growth ¾ Ubiquinoation ¾ Peroxisomal function ¾ Centrosomal functiion – mitotic spindle ¾ DNA repair ¾ Chromosomal aberrations ¾ Teratogens ¾ Placental function COMMON AND OVERLAPPING FEATURES ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ Large appearing head Triangular shaped face Decreased subcutaneous fat Delayed bone age Feeding difficulties as an infant High pitched voice Infertility Clinodactyly of the fifth finger Pigment abnormalities Bone changes of disuse (tall vertebrae, dolicocephaly, thin ribs, and long bones) “A” LIST 1. 2. 3. 4. 5. 6. 7. 8. Bloom* Dubowitz Floating Harbor MOPD II* Mulibrey* Silver-Russell/Russell-Silver*** SHORT 3-M* Also: Chromosomal, CPM, and teratogens “B” LIST Gorlin/Smith/Jones ¾ Aarskog Sx ¾ de Lange Sx ¾ Hallerman Streiff Sx ¾ Meire-gorlin Sx ¾ Rubinstein Taybi Sx ¾ Seckel’s Sx Hall 2004 article on MOPD II ¾ Toriello 1986 ¾ Saul Wilson Hersh 1990 & 1994 ¾ Hurst 1988 ¾ Sdfs ¾ Bangstad 1989, Salerno 2003, Scott 1969 ¾ Bluebel 1996 ¾ Cervenka 1979 ¾ Frias 2005 REFERENCES ¾ ¾ ¾ ¾ ¾ Gorlin RJ, Cohen Jr. MM, Hennekam RCM. Syndromes of the head and neck, 4th ed. Oxford University Press, NY, 2001. Jones KL. Smith’s recognizable patterns of human malformations, 6th edition. WB Saunders, Philadelphia, 2006. Winter-Baraitser Dysmorphology Database, version 1.0. In Winter RM & Baraitser M (eds.) London Medical Databases, Oxford University Press, Oxford, UK, 2005. OMIM (Online Mednelian Inheritance in Man) http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=OMIM Genetest/GeneClinics http://www.genetests.org