First-trimester umbilical cord diameter: a novel marker of fetal
advertisement
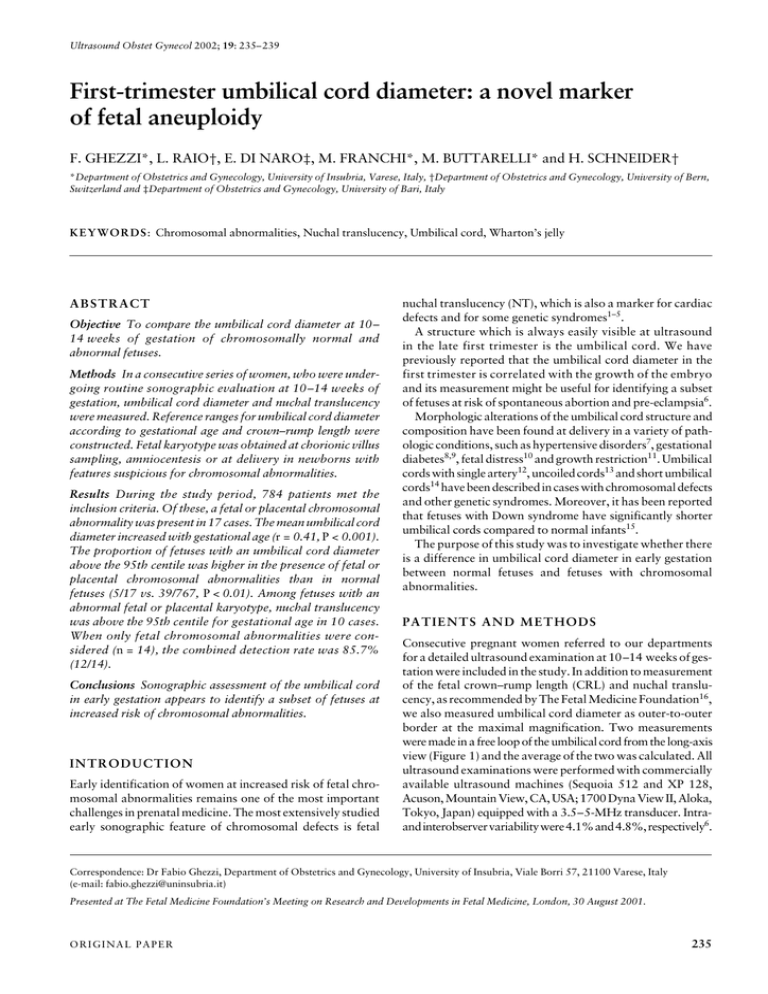
Ultrasound Obstet Gynecol 2002; 19: 235– 239 First-trimester umbilical cord diameter: a novel marker of fetal aneuploidy Blackwell Science Ltd F. GHEZZI*, L. RAIO†, E. DI NARO‡, M. FRANCHI*, M. BUTTARELLI* and H. SCHNEIDER† *Department of Obstetrics and Gynecology, University of Insubria, Varese, Italy, †Department of Obstetrics and Gynecology, University of Bern, Switzerland and ‡Department of Obstetrics and Gynecology, University of Bari, Italy KE YWORDS: Chromosomal abnormalities, Nuchal translucency, Umbilical cord, Wharton’s jelly ABSTRACT Objective To compare the umbilical cord diameter at 10– 14 weeks of gestation of chromosomally normal and abnormal fetuses. Methods In a consecutive series of women, who were undergoing routine sonographic evaluation at 10–14 weeks of gestation, umbilical cord diameter and nuchal translucency were measured. Reference ranges for umbilical cord diameter according to gestational age and crown–rump length were constructed. Fetal karyotype was obtained at chorionic villus sampling, amniocentesis or at delivery in newborns with features suspicious for chromosomal abnormalities. Results During the study period, 784 patients met the inclusion criteria. Of these, a fetal or placental chromosomal abnormality was present in 17 cases. The mean umbilical cord diameter increased with gestational age (r = 0.41, P < 0.001). The proportion of fetuses with an umbilical cord diameter above the 95th centile was higher in the presence of fetal or placental chromosomal abnormalities than in normal fetuses (5/17 vs. 39/767, P < 0.01). Among fetuses with an abnormal fetal or placental karyotype, nuchal translucency was above the 95th centile for gestational age in 10 cases. When only fetal chromosomal abnormalities were considered (n = 14), the combined detection rate was 85.7% (12/14). Conclusions Sonographic assessment of the umbilical cord in early gestation appears to identify a subset of fetuses at increased risk of chromosomal abnormalities. INTRODUCTION Early identification of women at increased risk of fetal chromosomal abnormalities remains one of the most important challenges in prenatal medicine. The most extensively studied early sonographic feature of chromosomal defects is fetal nuchal translucency (NT), which is also a marker for cardiac defects and for some genetic syndromes1–5. A structure which is always easily visible at ultrasound in the late first trimester is the umbilical cord. We have previously reported that the umbilical cord diameter in the first trimester is correlated with the growth of the embryo and its measurement might be useful for identifying a subset of fetuses at risk of spontaneous abortion and pre-eclampsia6. Morphologic alterations of the umbilical cord structure and composition have been found at delivery in a variety of pathologic conditions, such as hypertensive disorders7, gestational diabetes8,9, fetal distress10 and growth restriction11. Umbilical cords with single artery12, uncoiled cords13 and short umbilical cords14 have been described in cases with chromosomal defects and other genetic syndromes. Moreover, it has been reported that fetuses with Down syndrome have significantly shorter umbilical cords compared to normal infants15. The purpose of this study was to investigate whether there is a difference in umbilical cord diameter in early gestation between normal fetuses and fetuses with chromosomal abnormalities. PATIENTS AND METHODS Consecutive pregnant women referred to our departments for a detailed ultrasound examination at 10–14 weeks of gestation were included in the study. In addition to measurement of the fetal crown–rump length (CRL) and nuchal translucency, as recommended by The Fetal Medicine Foundation16, we also measured umbilical cord diameter as outer-to-outer border at the maximal magnification. Two measurements were made in a free loop of the umbilical cord from the long-axis view (Figure 1) and the average of the two was calculated. All ultrasound examinations were performed with commercially available ultrasound machines (Sequoia 512 and XP 128, Acuson, Mountain View, CA, USA; 1700 Dyna View II, Aloka, Tokyo, Japan) equipped with a 3.5–5-MHz transducer. Intraand interobserver variability were 4.1% and 4.8%, respectively6. Correspondence: Dr Fabio Ghezzi, Department of Obstetrics and Gynecology, University of Insubria, Viale Borri 57, 21100 Varese, Italy (e-mail: fabio.ghezzi@uninsubria.it) Presented at The Fetal Medicine Foundation’s Meeting on Research and Developments in Fetal Medicine, London, 30 August 2001. ORIGINAL PAPER 235 First-trimester umbilical cord diameter The fetal karyotype was established by chorionic villus sampling or amniocentesis or at delivery in newborns with features suggestive of chromosomal abnormalities. Each patient was included only once. Since we did not know whether placental chromosomal abnormalities might influence the morphology of the umbilical cord, a separate analysis was conducted, including and excluding cases with confined placental mosaicisms. Informed consent was obtained from all patients and the Human Research Review Committee of the participating institutions approved the study. The data of the first 304 fetuses were utilized in a previously published study6. Statistical analysis Statistical analysis was performed using SPSS for Windows (SPSS Inc., Chicago, IL, USA) and with GraphPad Prism version 3.00 for Windows (GraphPad Software, San Diego, CA, USA). The data were analyzed as previously described by Royston and Wright17. Polynomial regression analysis was performed to identify the regression curves that best fitted the mean and standard deviation (SD) as a function of gestational age and CRL. The SD scores (Z-scores) were calculated using the formula: (Observed umbilical cord diameter – mean umbilical cord diameter)/SD To assess the model fit, the Gaussian distributions of the Zscores were checked using the Kolmogorov–Smirnov test. The 5th and 95th centiles for umbilical cord diameter with gestation and in relation with CRL were obtained as previously described18 using the formula: mean ± 1.645 SD. Spearman rank correlation was used to assess the correlation between umbilical cord measurements and both gestational age and CRL. Fisher’s exact test was used to compare proportions. P < 0.05 was considered statistically significant. RESULTS The entry criteria were met by 784 patients. Of these, chromosomal abnormalities were present in 17 cases. To Ghezzi et al. construct nomograms for the umbilical cord diameter according to gestational age, the analysis was restricted to patients whose fetus had a normal karyotype (n = 767). The clinical characteristics of these patients are summarized in Table 1. A significant correlation was found between umbilical cord diameter and gestational age (r = 0.41, P < 0.001). The regression equation for the mean umbilical cord diameter (y) according to gestational age (x) was y = – 0.4245 + 0.3568x and for the SD (y′) was y′ = 0.001802 + 0.04226x. The normal distribution of Z-scores was confirmed by the Kolmogorov– Smirnov test. Figure 2 shows the umbilical cord diameters observed measurements and the fitted 5th, 50th and 95th centiles. The clinical characteristics of cases with placental or fetal abnormal karyotype are shown in Table 2. In five fetuses (29.4%) with chromosomal abnormalities, the umbilical cord was greater than the 95th centile for gestational age (Figure 3). The proportion of fetuses with an umbilical cord diameter above the 95th centile was higher among those with fetal or placental chromosomal abnormalities compared to normal fetuses (5/17 vs. 39/767, P < 0.01). Three cases of an abnormal karyotype at chorionic villus sampling were confirmed at amniocentesis to have confined placental mosaicisms. When these cases were removed from the analysis, the proportion of chromosomally abnormal fetuses with an umbilical cord diameter above the 95th centile increased from 29.4% to 35.7% (5/14). To explore the significance of an increased umbilical cord diameter, the analysis was further restricted to fetuses with a CRL of 45–85 mm, as recommended for the evaluation of Table 1 Characteristics of patients used for the generation of the umbilical cord diameter nomogram Characteristics n = 767 Maternal age (years) (mean ± SD) Gestational age at examination (weeks) (mean ± SD) Gestational age at delivery (weeks) (mean ± SD) Nulliparous (n), % Birth weight (g) (mean ± SD) Placental weight (g) (mean ± SD) 30.8 ± 6.2 11.7 ± 0.78 39.6 ± 1.7 338 (44.1) 3432 ± 504 593 ± 126 Umbilical cord diameter (mm) 10 9 8 7 6 5 4 3 2 1 0 10 11 12 13 14 Gestational age (weeks) Figure 1 Sonographic measurement of the umbilical cord diameter in the first trimester of pregnancy. 236 Figure 2 Umbilical cord diameter measurements plotted on the estimated centiles for gestational age. Lines represent the 5th, 50th and 95th centile. Ultrasound in Obstetrics and Gynecology First-trimester umbilical cord diameter Ghezzi et al. Umbilical cord diameter (mm) 10 9 8 7 6 5 4 3 2 1 0 10 9 9 7 6 5 4 3 2 55 60 65 70 75 80 85 8 7 6 5 4 3 2 1 1 0 50 Figure 4 Umbilical cord diameter measurements plotted on the estimated centiles for embryonic crown–rump length. Lines represent the 5th, 50th and 95th centile. 10 8 45 Crown–rump length (mm) Umbilical cord diameter (mm) Umbilical cord diameter (mm) nuchal translucency2. In this group of patients, 645 women had a normal fetus while 14 had a fetus with an abnormal karyotype. A significant correlation was found between umbilical cord diameter and CRL (r = 0.35, P < 0.001). The regression equation for the mean umbilical cord diameter (y) according to CRL (x) was y = 2.206 + 0.03002x and for the SD (y′) was y′ = –0.3021 + 0.204x. Figure 4 shows the relationship between the umbilical cord diameter observed measurements and the CRL, as well as the umbilical cord diameter fitted 5th, 50th and 95th centiles. In four out of 14 fetuses with chromosomal abnormalities and with a CRL of 45–85 mm, the umbilical cord diameter was above the 95th centile (28.6%) (Figure 5). The proportion of fetuses with an umbilical cord diameter greater than the 95th centile was higher among those with fetal or placental abnormal karyotype compared to normal fetuses (4/14 vs. 35/631, P < 0.01). When cases with confined placental mosaicism were excluded from the analysis, the proportion of fetuses with abnormal 10 11 12 13 0 14 45 50 55 65 70 75 80 85 Crown–rump length (mm) Gestational age (weeks) Figure 3 Umbilical cord diameter of fetuses with an abnormal karyotype plotted on reference ranges for gestational age. 60 Figure 5 Umbilical cord diameter of fetuses with an abnormal karyotype plotted on reference ranges for crown–rump length. Table 2 Characteristics of fetuses with abnormal karyotype Gestational age at examination (weeks) Umbilical cord diameter (mm) Nuchal translucency (mm) Crown–rump length (mm) Biparietal diameter (mm) Karyotype 10.1 10.4 10.9 11.1 11.4 11.4 11.6 11.6 11.6 11.7 11.9 12.1 12.3 12.4 12.9 14.0 13.0 5.3 3.5 3.0 3.8 3.9 5.0 3.5 3.8 4.1 3.7 9.0 5.1 4.3 3.4 3.6 7.6 3.2 1.8 1.0 2.9 1.1 2.5 9.6 0.5 3.0 3.8 1.6 11.0 2.1 1.0 4.0 4.8 8.0 3.3 36.7 38.0 33.9 55.5 53.0 65.0 53.1 52.3 53.6 55.5 53.0 57.5 56.8 61.3 47.3 80.0 65.4 13.5 15.5 13.6 19.5 18.0 18.2 19.2 19.3 19.0 20.7 19.0 22.1 21.9 19.3 18.5 29.7 28.8 47XX + 21 45XO 47XY + 21 47XXY 47XX + 21 47XY + 21 Confined placental mosaicism 47XY + 21 47XX + 21 Confined placental mosaicism 45XO 47XY + 13 Confined placental mosaicism 47XX + 21 47XX + 18 45XO 47XY + 18 Ultrasound in Obstetrics and Gynecology 237 First-trimester umbilical cord diameter karyotype and an umbilical cord diameter higher than the 95th centile was 36.4% (4/11). Of the 17 fetuses with an abnormal fetal or placental karyotype, the nuchal translucency was above the 95th centile for gestational age in 10 cases. Among the five fetuses with an umbilical cord diameter above the 95th centile, the nuchal translucency was increased in three cases. In our population, combining the measurement of nuchal translucency and umbilical cord diameter, the detection rate of fetal or placental aneuploidies was 70.6% (12/17) with a net increase of 11.8% compared to nuchal translucency alone (10/17; 58.8%). When only fetal chromosomal abnormalities are considered the combined detection rate was 85.7% (12/14). DISCUSSION This study shows that a relationship exists between fetal chromosomal abnormalities and the morphology of the umbilical cord. Although the underlying pathophysiologic mechanism leading to an increased umbilical cord diameter in fetuses with chromosomal abnormalities remains to be explored, certain etiologic mechanisms might explain the increase in both nuchal translucency and umbilical cord diameter. The Wharton’s jelly mainly comprises a ground substance of hyaluronic acid and proteoglycans in an aqueous solution of salts, metabolites and plasma proteins distributed in a fine network of collagen microfibrils19. The most predominant cellular population consists of fibroblasts involved in synthesizing collagen and glycosaminoglycans20. Approximately 70% of the soluble part of the Wharton’s jelly is composed of collagen type IV and hyaluronic acid20 which, in turn, is capable of entrapping large amounts of fluid21. Moreover, several types of collagen (types I, III, IV, V and VI) are found to be homogeneously distributed in the media of the umbilical vessels or in the Wharton’s jelly22,23. The precipitation of collagen, laminin and heparan sulfate has been observed as early as the first trimester around the canalicular-like structure of the Wharton’s jelly22. A number of studies have demonstrated that alterations of the extracellular matrix are present in fetuses affected by trisomy 21, 13 and 1823,24. In fetuses with trisomy 21, the extracellular matrix of the nuchal skin is much richer in glucosaminoglycan, especially hyaluronan, compared to chromosomally normal fetuses23,25. This appears to be the consequence of a decreased degradation of hyaluronan in fetuses with trisomy 21. In the nuchal skin of trisomy 18 fetuses, the distribution and organization of collagen types I and III is different compared to normal fetuses, resembling modification occurring with aging25. Finally, in trisomy 18, most dermal fibroblasts have been found to be laminin positive and in trisomy 13 most dermal fibroblasts are collagen type IV positive23. In gestational age-matched control normal fetuses, this was never found to be the case23. Therefore, an over-expression, as well as an under-expression, of different structural proteins, polysaccharides and proteoglycans of the extracellular matrix, which might result in abnormal accumulation of fluid, could explain both the increased nuchal translucency and increased umbilical cord diameter. 238 Ghezzi et al. Another interesting question is why fetuses with Turner syndrome might have a wider than normal umbilical cord. The most plausible mechanism to explain the hygroma colli generally present in fetuses with Turner syndrome is lymphatic vessel hypoplasia in the upper dermis26. This does not explain the increased umbilical cord diameter in fetuses affected by Turner syndrome because lymphatic vessels are completely absent in the umbilical cord and in the placenta27. However, alterations of proteoglycan expression have been found in the skin of fetuses with Turner syndrome. It has been reported that, in fetuses with Turner syndrome, biglycan, which is encoded on chromosome X, is under-expressed and chondroitin-6-sulfate is over-expressed28. Thus, it reasonable to assume that similar extracellular matrix modifications might also affect the Wharton’s jelly which for a large part is composed of proteoglycans. Another mechanism that might explain the increased umbilical cord size is venous congestion26. Considering that the amount of Wharton’s jelly in the first and early second trimesters is lower than that in the third trimester27, the increase in umbilical cord size in early gestation could either be the consequence of a progressive enlargement of the umbilical cord vessels or an overrepresentation of Wharton’s jelly, or both. Cardiac defects and abnormalities of the great arteries are common findings in fetuses with increased nuchal translucency16. Moreover, an absent or reverse flow during atrial contraction at the level of the ductus venosus has been reported in a very high proportion of chromosomally abnormal fetuses between 11 and 14 weeks of gestation29. As a consequence, umbilical vein congestion may cause umbilical vein dilatation, transudation of fluid into the Wharton’s jelly and enlargement of the umbilical cord size. Noteworthy, it has been demonstrated that Wharton’s jelly is a metabolically active tissue involved in the exchanges between amniotic fluid and the blood in umbilical vessels30. Hence, it is possible that venous congestion, frequently seen in trisomic fetuses, might cause an alteration in the transfer of fluid normally present in the first trimester of gestation31 between Wharton’s jelly and the umbilical vessels. The sonographic counterpart of the abnormal accumulation of fluid in the Wharton’s jelly is an increased umbilical cord size. In conclusion, the results of the present study suggest that umbilical cord size early in gestation is different between normal and chromosomally abnormal fetuses. We hypothesize that the underlying pathophysiologic mechanisms leading to an increase in umbilical cord diameter might be those that also explain the increased nuchal translucency in fetuses with abnormal karyotype, such as alterations of the extracellular matrix components or fetal venous congestion. Larger studies should aim to explore the possible clinical application of routine sonographic evaluation of the umbilical cord in early gestation. REFERENCES 1 Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K. Fetal nuchal translucency: ultrasound screening for chromosomal defects in the first trimester of pregnancy. Br Med J 1992; 304: 867–9 Ultrasound in Obstetrics and Gynecology First-trimester umbilical cord diameter 2 Pandya PP, Brizot ML, Kuhn P, Snijders RJ, Nicolaides KH. Firsttrimester fetal nuchal translucency thickness and risk for trisomies. Obstet Gynecol 1994; 101: 782– 6 3 Hyett J, Perdu M, Sharland G, Snijders R, Nicolaides KH. Using fetal nuchal translucency to screen for major congenital cardiac defects at 10–14 weeks of gestation: population based cohort study. BMJ 1999; 352: 1662 4 Zosmer N, Souter VL, Chan CS, Huggon IC, Nicolaides KH. Early diagnosis of major cardiac defects in chromosomally normal fetuses with increased nuchal translucency. Br J Obstet Gynaecol 1999; 106: 829 –33 5 Souka AP, Krampl E, Bakalis S, Heath V, Nicolaides KH. Outcome of pregnancy in chromosomally normal fetuses with increased nuchal translucency in the first trimester. Ultrasound Obstet Gynecol 2001; 18: 9–17 6 Ghezzi F, Raio L, Di Naro E, Franchi M, Brühwiler H, D’Addario V, Schneider H. First-trimester umbilical cord diameter and the growth of the human embryo. Ultrasound Obstet Gynecol 2001; 18: 348– 51 7 Bankowski E, Sobolewski K, Romanowicz L, Chyczewski L, Jawosrski S. Collagen and glycosaminoglycans of Wharton’s jelly and their alterations in EPH-gestosis. Eur J Obstet Gynecol Reprod Biol 1996; 66: 109 –17 8 Singh SD. Gestational diabetes and its effect on the umbilical cord. Early Hum Dev 1986; 14: 89 –98 9 Weissman A, Jakobi P. Sonographic measurements of the umbilical cord in pregnancies complicated by gestational diabetes. J Ultrasound Med 1997; 16: 691– 4 10 Raio L, Ghezzi F, Di Naro E, Franchi M, Maymon E, Mueller MD, Brühwiler H. Prenatal diagnosis of a lean umbilical cord: a simple marker for fetuses at risk of being small for gestational age at birth. Ultrasound Obstet Gynecol 1999; 13: 176 – 80 11 Bruch JF, Sibony O, Benali K, Challer C, Blot P, Nessmann C. Computerized microscope morphometry of umbilical vessels from pregnancies with intrauterine growth retardation and abnormal umbilical artery Doppler. Hum Pathol 1997; 28: 1139 – 45 12 Persutte WH, Hobbins J. Single umbilical artery: a clinical enigma in modern prenatal ultrasound. Ultrasound Obstet Gynecol 1995; 6: 216 –29 13 Lacro RV, Jones KL, Benirschke K. The umbilical cord twist: origin, direction and relevance. Am J Obstet Gynecol 1987; 157: 933 – 8 14 Gilbert-Barness E, Drut RM, Drut R, Grange DK, Opitz JM. Developmental abnormalities resulting in short umbilical cord. Birth Defects 1993; 29: 113 – 40 15 Moessinger AC, Mills JL, Harley EE, Ramakrishnan R, Berendes HW, Blanc WA. Umbilical cord length in Down’s syndrome. Am J Dis Child 1986; 140: 1276 –7 Ultrasound in Obstetrics and Gynecology Ghezzi et al. 16 Pandya P. Nuchal translucency thickness. In Nicolaides KH, Sebire NJ, Snijders RJM, eds. The 11–14-Week Scan. The Diagnosis of Fetal Abnormalities. Publisher’s location?: Parthenon Publishing, 1999: 14– 8 17 Royston P, Wright EM. How to construct ‘normal ranges’ for fetal variables. Ultrasound Obstet Gynecol 1998; 11: 30– 8 18 Altman DG, Chitty LS. Chart of fetal size: 1. Methodology. Br J Obstet Gynaecol 1994; 101: 29–34 19 Takechi K, Kuwabara Y, Mizuno M. Ultrastructural and immunohistochemical studies of Wharton’s jelly umbilical cord cells. Placenta 1993; 14: 235– 45 20 Vizza E, Correr S, Goranova V, Heyn R, Angelucci PA, Forleo R, Motta PM. The collagen skeleton of the human umbilical cord at term. A scanning electron microscopy study after 2N-NaOH maceration. Reprod Fertil Dev 1996; 8: 885–94 21 Klein J, Meyer F. Tissue structure and macromolecular diffusion in umbilical cord immobilization of endogenous hyaluronic acid. Biochim Biophys Acta 1983; 22: 400–11 22 Nanaev AK, Kohnen G, Milovanov AP, Domogatsky SP, Kaufmann P. Stromal differentiation and architecture of the human umbilical cord. Placenta 1997; 18: 53– 64 23 Von Kaisenberg CS, Krenn V, Ludwig M, Nicolaides KH, Brand-Saberi B. Morphological classification of nuchal skin in human fetuses with trisomy 21, 18 and 13 at 12–18 weeks and in a trisomy 16 mouse. Anat Embryol (Berl) 1998; 197: 105 –24 24 Von Kaisenberg CS, Brand-Saberi B, Christ B, Vallian S, Farzaneh F, Nicolaides KH. Collagen type VI gene expression in the skin of trisomy 21 fetuses. Obstet Gynecol 1998; 91: 319–23 25 Brandt-Saberi B, Epperlein HH, Romanos GE, Christ B. Distribution of extracellular matrix components in nuchal skin from fetuses carrying trisomy 18 and trisomy 21. Cell Tissue Res 1994; 277: 465 –75 26 Von Kaisenberg CS, Nicolaides KH, Brand-Saberi B. Lymphatic vessel hypoplasia in fetuses with Turner syndrome. Hum Reprod 1999; 14: 823– 6 27 Benirschke K, Kaufman P. Pathology of the Human Placenta, 3rd edn. New York: Springer-Verlag, 1995: 323 28 Von Kaisenberg C, Hyett J. Pathophysiology of increased nuchal translucency. In Nicolaides KH, Sebire NJ, Snijders RJM, eds. The 11–14-Week Scan. London: Parthenon Publishing, 1999: 95 –114 29 Matias A, Gomes C, Flack N, Montenegro N, Nicolaides K. Screening for chromosomal abnormalities at 11–14 weeks: the role of ductus venosus blood flow. Ultrasound Obstet Gynecol 1998; 12: 380– 4 30 Gilbert WM, Cheung CY, Brace RA. Rapid intramembranous absorption into the fetal circulation of arginine vasopressin injected intraamniotically. Am J Obstet Gynecol 1991; 164: 1013 –8 31 Gilbert WM, Brace RA. Amniotic fluid volume and normal flows to and from the amniotic cavity. Semin Perinatol 1993; 17: 150 –7 239