Is Inhibitor of differentiation 3 involved in human primary Sjo¨gren`s
advertisement
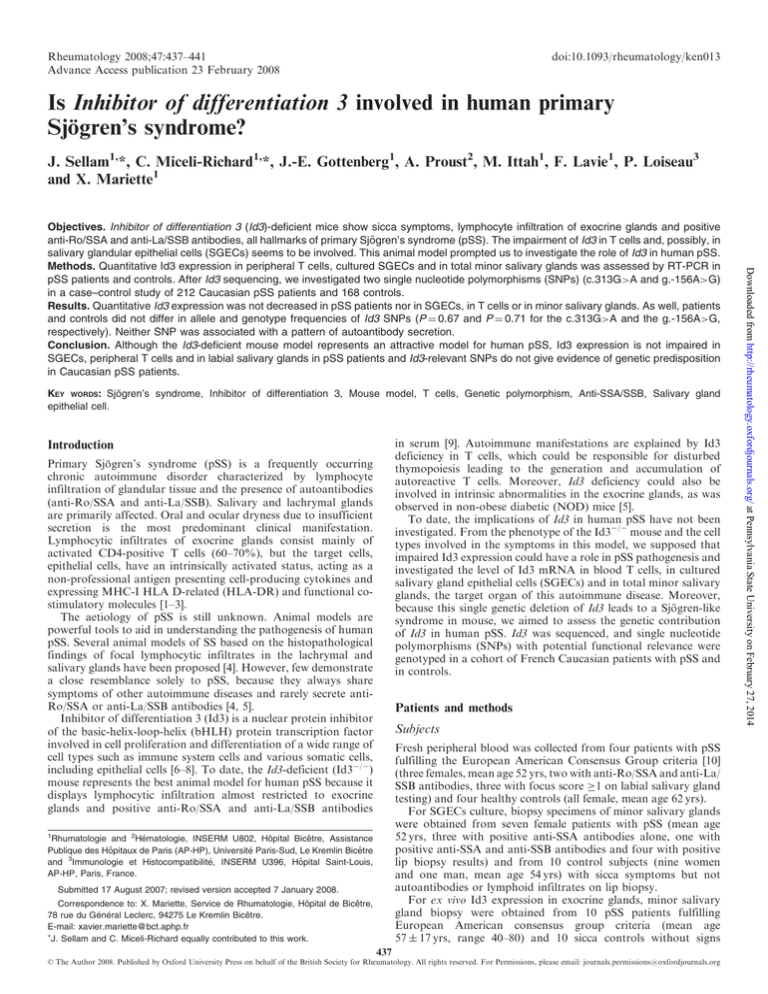
Rheumatology 2008;47:437–441 Advance Access publication 23 February 2008 doi:10.1093/rheumatology/ken013 Is Inhibitor of differentiation 3 involved in human primary Sjögren’s syndrome? J. Sellam1,*, C. Miceli-Richard1,*, J.-E. Gottenberg1, A. Proust2, M. Ittah1, F. Lavie1, P. Loiseau3 and X. Mariette1 KEY WORDS: Sjögren’s syndrome, Inhibitor of differentiation 3, Mouse model, T cells, Genetic polymorphism, Anti-SSA/SSB, Salivary gland epithelial cell. in serum [9]. Autoimmune manifestations are explained by Id3 deficiency in T cells, which could be responsible for disturbed thymopoiesis leading to the generation and accumulation of autoreactive T cells. Moreover, Id3 deficiency could also be involved in intrinsic abnormalities in the exocrine glands, as was observed in non-obese diabetic (NOD) mice [5]. To date, the implications of Id3 in human pSS have not been investigated. From the phenotype of the Id3/ mouse and the cell types involved in the symptoms in this model, we supposed that impaired Id3 expression could have a role in pSS pathogenesis and investigated the level of Id3 mRNA in blood T cells, in cultured salivary gland epithelial cells (SGECs) and in total minor salivary glands, the target organ of this autoimmune disease. Moreover, because this single genetic deletion of Id3 leads to a Sjögren-like syndrome in mouse, we aimed to assess the genetic contribution of Id3 in human pSS. Id3 was sequenced, and single nucleotide polymorphisms (SNPs) with potential functional relevance were genotyped in a cohort of French Caucasian patients with pSS and in controls. Introduction Primary Sjögren’s syndrome (pSS) is a frequently occurring chronic autoimmune disorder characterized by lymphocyte infiltration of glandular tissue and the presence of autoantibodies (anti-Ro/SSA and anti-La/SSB). Salivary and lachrymal glands are primarily affected. Oral and ocular dryness due to insufficient secretion is the most predominant clinical manifestation. Lymphocytic infiltrates of exocrine glands consist mainly of activated CD4-positive T cells (60–70%), but the target cells, epithelial cells, have an intrinsically activated status, acting as a non-professional antigen presenting cell-producing cytokines and expressing MHC-I HLA D-related (HLA-DR) and functional costimulatory molecules [1–3]. The aetiology of pSS is still unknown. Animal models are powerful tools to aid in understanding the pathogenesis of human pSS. Several animal models of SS based on the histopathological findings of focal lymphocytic infiltrates in the lachrymal and salivary glands have been proposed [4]. However, few demonstrate a close resemblance solely to pSS, because they always share symptoms of other autoimmune diseases and rarely secrete antiRo/SSA or anti-La/SSB antibodies [4, 5]. Inhibitor of differentiation 3 (Id3) is a nuclear protein inhibitor of the basic-helix-loop-helix (bHLH) protein transcription factor involved in cell proliferation and differentiation of a wide range of cell types such as immune system cells and various somatic cells, including epithelial cells [6–8]. To date, the Id3-deficient (Id3/) mouse represents the best animal model for human pSS because it displays lymphocytic infiltration almost restricted to exocrine glands and positive anti-Ro/SSA and anti-La/SSB antibodies Patients and methods Subjects Fresh peripheral blood was collected from four patients with pSS fulfilling the European American Consensus Group criteria [10] (three females, mean age 52 yrs, two with anti-Ro/SSA and anti-La/ SSB antibodies, three with focus score 1 on labial salivary gland testing) and four healthy controls (all female, mean age 62 yrs). For SGECs culture, biopsy specimens of minor salivary glands were obtained from seven female patients with pSS (mean age 52 yrs, three with positive anti-SSA antibodies alone, one with positive anti-SSA and anti-SSB antibodies and four with positive lip biopsy results) and from 10 control subjects (nine women and one man, mean age 54 yrs) with sicca symptoms but not autoantibodies or lymphoid infiltrates on lip biopsy. For ex vivo Id3 expression in exocrine glands, minor salivary gland biopsy were obtained from 10 pSS patients fulfilling European American consensus group criteria (mean age 57 17 yrs, range 40–80) and 10 sicca controls without signs 1 Rhumatologie and 2Hématologie, INSERM U802, Hôpital Bicêtre, Assistance Publique des Hôpitaux de Paris (AP-HP), Université Paris-Sud, Le Kremlin Bicêtre and 3Immunologie et Histocompatibilité, INSERM U396, Hôpital Saint-Louis, AP-HP, Paris, France. Submitted 17 August 2007; revised version accepted 7 January 2008. Correspondence to: X. Mariette, Service de Rhumatologie, Hôpital de Bicêtre, 78 rue du Général Leclerc, 94275 Le Kremlin Bicêtre. E-mail: xavier.mariette@bct.aphp.fr J. Sellam and C. Miceli-Richard equally contributed to this work. 437 ß The Author 2008. Published by Oxford University Press on behalf of the British Society for Rheumatology. All rights reserved. For Permissions, please email: journals.permissions@oxfordjournals.org Downloaded from http://rheumatology.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014 Objectives. Inhibitor of differentiation 3 (Id3)-deficient mice show sicca symptoms, lymphocyte infiltration of exocrine glands and positive anti-Ro/SSA and anti-La/SSB antibodies, all hallmarks of primary Sjögren’s syndrome (pSS). The impairment of Id3 in T cells and, possibly, in salivary glandular epithelial cells (SGECs) seems to be involved. This animal model prompted us to investigate the role of Id3 in human pSS. Methods. Quantitative Id3 expression in peripheral T cells, cultured SGECs and in total minor salivary glands was assessed by RT-PCR in pSS patients and controls. After Id3 sequencing, we investigated two single nucleotide polymorphisms (SNPs) (c.313G>A and g.-156A>G) in a case–control study of 212 Caucasian pSS patients and 168 controls. Results. Quantitative Id3 expression was not decreased in pSS patients nor in SGECs, in T cells or in minor salivary glands. As well, patients and controls did not differ in allele and genotype frequencies of Id3 SNPs (P ¼ 0.67 and P ¼ 0.71 for the c.313G>A and the g.-156A>G, respectively). Neither SNP was associated with a pattern of autoantibody secretion. Conclusion. Although the Id3-deficient mouse model represents an attractive model for human pSS, Id3 expression is not impaired in SGECs, peripheral T cells and in labial salivary glands in pSS patients and Id3-relevant SNPs do not give evidence of genetic predisposition in Caucasian pSS patients. 438 J. Sellam et al. of autoimmunity (mean age 56 10 yrs, range 37–70) already described elsewhere [11]. Among the 10 pSS patients, 9 of them had a focus score >1, 7 had anti-SSA antibodies and 4 had antiSSB autoantibodies. For Id3 genetic study, we included a cohort of 209 unrelated patients with pSS according to the European American consensus group criteria (40% without autoantibodies, 28% with anti-SSA antibodies only and 32% with both anti-SSA and anti-SSB antibodies) and 168 healthy blood donors. All patients and controls were Caucasians. The study received approval from the local ethics committee, and informed consent was obtained from all subjects. Blood T-cell isolation SGECs culture and characterization Primary cultures of SGECs were established from minor salivary glands as previously described [12]. In brief, each lobule was cut into small fragments and set in six 75-cm2 flasks with basal epithelial medium (a 3 : 1 mixture of Ham’s F-12 and DMEM) supplemented with 2.5% fetal calf serum, epidermal growth factor (10 ng/ml), hydrocortisone (0.4 g/ml), insulin (0.5 g/ml), penicillin (100 IU/ml) and streptomycin (100 g/ml) and incubated at 378C under 5% CO2. After 4–5 weeks’ culture at 70–80% confluence, cells were dissociated with a 0.125% trypsin–EDTA solution for real-time quantitative RT-PCR. To exclude cell dedifferentiation during primary culture or contamination by fibroblastic cells, morphological characteristics and cytokeratin-7 staining for ductal SGECs were evaluated. As reported previously [12], all tested samples were 95–100% positive for cytokeratin-7, -19 and -903 but not for cytokeratin-20, which confirm the ductal epithelial origin of these cells and exclude the fibroblastic nature. Moreover, complementary staining with MPO, CD20, CD3, CD45 and smooth muscle actin excluded the possibility of contamination with myeloid cells, B cells, T cells or myoepithelial cells. RNA isolation from minor salivary glands After minor labial salivary glands were dissected from the lower lip of the subjects, RNA extraction, cRNA production and cDNA synthesis and amplification were performed as described previously [11]. Id3 mRNA quantitation Total RNA was isolated from isolated T cells and cultured SGECs by use of the RNeasy Mini kit (Qiagen, Courtaboeuf, France). cDNA synthesis involved use of Enhanced Avian HS RT-PCR (Sigma-Aldrich, Saint Quentin Fallavier, France). Id3 and -actin cDNA levels were determined by use of Light Cycler-based kinetic quantitative PCR (Roche Diagnostics, Meylan, France). Id3 and -actin PCR products were detected by use of LightCycler FastStart DNA Master SYBR Green I (Roche Diagnostics). To correct for variations in mRNA recovery and reverse transcription yield, the amount of Id3 cDNA was normalized to that of -actin. Amplification primers for the human genes were as follows: Id3, forward 50 -CTGAGCTTGCTGGACGACA-30 and reverse 30 -ATGTAGTCGATGACGCGCTGTA-50 ; and -actin, forward Sequencing analysis of Id3 Because Id3 polymorphisms have never been studied in Caucasian patients, Id3 was sequenced with genomic DNA isolated from PBMCs of six patients with pSS and six healthy controls. Polymorphism screening included the 3 exons, the intron–exon junction boundaries and the 50 flanking region, thus including the putative promoter region of Id3 (2200 bp upstream of the transcription initiation site). Putative functional consequences of the identified polymorphisms in the promoter region were assessed using AliBaba 2.1, a program for predicting transcription factorbinding sites [13]. Case–control study of SNPs Among the four SNPs identified, two with potential functional relevance were genotyped. The c.313G>A SNP was genotyped by the PCR restriction fragment-length polymorphism method in 209 patients with pSS (126 with positive autoantibodies, including 58 with anti-Ro/SSA only and 68 with anti-Ro/SSA and anti-La/SSB antibodies and 83 without autoantibodies) and 168 healthy French blood donors. PCR was performed in a 20-ml final reaction volume with PTC 200 (Peltier Thermal Cycler) with use of 100 ng DNA, 1.25 U AmpliTaq Gold (Applied Biosystems, CA, USA), the appropriate buffer supplied by the manufacturer (Tampon GeneAmp 1) and MgCl2 (1.5 mM). Cycle conditions were 958C for 12 min, then 30 cycles of 958C for 30 s, 588C for 30 s and 728C for 30 s, then a final extension at 728C for 7 min. The g.-156A>G SNP was genotyped by competitive allelespecific PCR by use of fluorescence resonance energy transfer (FRET) technology. Statistical analysis Quantitative results are expressed as means S.E.M. For quantitative comparison of results between patients and controls, Mann–Whitney U-test was used. All genotyped SNPs were in Hardy–Weinberg equilibrium. Comparisons of allelic and genotypic frequencies of c.313G>A and g.-156A>G polymorphisms between patients and controls involved two-sided chi-square test. A Bonferroni correction was applied for two tested SNPs. Both unadjusted and adjusted (denoted by Pa) P-values are reported. A P < 0.05 was considered significant. Results Quantitative Id3 mRNA expression in human pSS Because total Id3 deficiency in the mouse model leading to a Sjögren-like syndrome is related to a specific Id3 impairment in Downloaded from http://rheumatology.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014 Peripheral blood mononuclear cells (PBMCs) were obtained by centrifugation with Ficoll gradient (PAA Laboratories, Pasching, Austria). T cells were negatively separated from other PBMCs by use of a Pan T-Cell Isolation Kit II and magnetic-activated cellsorting columns (Miltenyi Biotec, Bergish Gladbach, Germany). T-cell purity was assessed by flow cytometry performed with use of an EPICS XL device (Beckman Coulter), showing <0.2% CD14þ cells and <5% CD22þ cells by use of anti-CD14 FITC, anti-CD22 PC5 antibodies or appropriate isotype-matched control (Becton Dickinson). 50 -GCTGTGCTACGTCGCCCT-30 and reverse 50 -AAGGTAGT TTCGTGGATGCC-30 . Each sample was processed in duplicate, with initial incubation at 968C for 10 min, then 40 cycles of 958C for 10 s, 608C for 15 s and 728C for 20 s. For each run, serially diluted cDNA of human B cells infected with EBV (B EBV cells) were used for quantitative standards. We determined the cell equivalence (CE) number of Id3 and -actin mRNA in each sample according to the standard curve generated from values obtained with B EBV cells. The unit number showing relative Id3 mRNA level in each sample was determined as a value of Id3 CE normalized to -actin CE. Melting-curve analysis was performed to assess the specificity of PCR product. For ex vivo Id3 expression in total exocrine glands, quantitative RT-PCR was performed as described elsewhere [11] using the Id3 primer sequences described above. Normalization of amount of Id3 cDNA was performed using the amount of cDNA hypoxanthine phosphoribosyltransferase (HPRT) sequences. HPRT PCR primers were: 50 -TGACACTGGCAAAACAATGCA-30 and reverse, 50 -GGTCCTTTTCACCAGCAAGCT-30 . Id3 and primary Sjögren’s syndrome T cells, we investigated the mRNA expression of Id3 in peripheral T cells of patients with pSS and healthy donors but found no difference in Id3 expression between the groups (ratio Id3/-actin 1.2 0.09 in pSS patients and 1.1 0.01 in controls; P ¼ 0.38) (Fig. 1A). Also, because the abnormal phenotype of SGECs in pSS could be related to an intrinsic Id3 impairment in these cells, we further investigated the expression of Id3 mRNA in cultured SGECs of 7 patients with pSS and 10 with sicca symptoms without autoimmunity. Id3 expression in SGECs was not decreased in pSS NS Id3 gene sequencing 1.2 1.0 0.8 0.6 0.4 Id3 gene polymorphism analysis 0.2 The allele and genotype frequency of c.313G>A and g.-156A>G in patients and controls are reported in Tables 2 and 3. All genotyped SNPs were in Hardy–Weinberg equilibrium. pSS patients and controls did not differ in allele and genotype frequencies of polymorphisms. For the c.313G>A, G and A allelic frequency were 79 and 21%, respectively, in pSS patients vs 81 and 19%, respectively, in controls (P ¼ 0.67). For the g.-156A>G, A and G allelic frequency were 52 and 48%, respectively, in pSS patients vs 53 and 47%, respectively, in controls (P ¼ 0.71). Allelic and genotypic distributions of c.313G>A and g.-156A>G according to the profile of antibody secretion are reported in Tables 2 and 3. Both SNPs were not associated with a specific pattern of autoantibody secretion: adjusted P-value (Pa) ¼ 0.34 and Pa ¼ 0.10 for c.313G>A and Pa ¼ 0.09 and Pa ¼ 0.14 for g.-156A>G (for allelic and genotypic frequencies, respectively). 0 Controls n =4 pSS n =4 NS B 1.8 1.6 1.4 1.2 1.0 0.8 0.6 0.4 0.2 0 Controls n =10 pSS n =7 Discussion FIG. 1. RT-PCR results of quantitative Id3 mRNA expression in pure cell populations from pSS patients and controls. Results are expressed as mean (solid histograms) and S.E.M (vertical lines). (A) Id3 expression in blood T cells. (B) Id3 expression in SGECs. NS, non significant. Since the Id3-knockout mouse was described as an animal model of pSS, we aimed to investigate the role of Id3 in human pSS. Here, we demonstrate that the mRNA expression of Id3 is not TABLE 1. Sequence variations of human Id3 gene with the corresponding minor allele frequencies Sequence variations c.313G>A c.331T>G g.-156A>G g.-234G>A g.-386_-387insG g.-1962T>C g.-2085(GAA)5-6 0.16 0.055 0.42 0.08 0.18 0.46 0.045 Minor allele frequency The genotyped SNPs are represented in bold. The reference sequence is provided by Ensembl database (http://www.ensembl.org) (OTTHUMG00000003229). TABLE 2. Allelic and genotypic frequencies of Id3 gene c.313G/A polymorphism in pSS patients and controls and according to the presence of autoantibodies c.313G/A SS (n¼209) Allele frequenciesa G 332 (79) A 86 (21) Genotype frequencies GG 131 (63) GA or AAb 78 (37) pSS without auto-Ab (n ¼ 83) pSS with anti-SSA only (n ¼ 58) pSS with anti-SSA and anti-SSB (n ¼ 68) Controls (n ¼ 168) OR (95% CI) pSS vs controls P-value 129 (78) 37 (22) 99 (85) 17 (15) 104 (76) 32 (24) 271 (81) 65 (19) 0.93 (0.65,1.33) 1.08 (0.75,1.55) 0.67 0.67 47 (57) 36 (43) 44 (76) 14 (24) 40 (59) 28 (41) 111 (66) 57 (34) 0.86 (0.56, 1.32) 1.16 (0.76, 1.77) 0.49 0.49 a The allelic frequencies are calculated on 418 chromosomes for patients and 336 chromosomes for controls. bDue to the low number of AA genotype carriers, AA and AG genotypes were analysed together. Results are expressed as number of patients (%). pSS, primary Sjögren’s syndrome; auto-Ab, auto-antibody; NA, not applicable; OR, odds ratio. Downloaded from http://rheumatology.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014 1.4 Id3/β-actin patients as compared with control subjects (ratio Id3/-actin 1.4 0.07 vs 1.5 0.05; P ¼ 0.5) (Fig. 1B). As culture procedure could change the expression of Id3 in SGECs, we performed Id3 RNA quantification in vivo from total labial salivary glands biopsy in 10 patients and 10 sicca controls subjects without signs of autoimmunity. Id3 expression was increased in pSS patients compared with controls (ratio Id3/ HPRT 2.8 2.3 in pSS patients vs 1.0 0.8 in controls; P ¼ 0.03). Using genomic DNA of six healthy controls and six patients, five SNPs were identified as well as one insertion and a variability of a short sequence repeats (Table 1). We genotyped two SNPs with minor allele frequency higher than 10% and potential functional relevance: one located in the promoter region (g.-156A>G) modifying putative Sp1 transcription factor-binding sites and the other (c.313G>A), a non-synonymous SNP (A105T) located in the second exon. Using a program for predicting transcriptionbinding site, the other identified polymorphisms were not functionally relevant. Among the genotyped SNPs, c.313G>A was already reported in public databases (http://www.ncbi.nlm. nih.gov/projects/SNP). A 1.6 Id3/β-actin 439 J. Sellam et al. 440 TABLE 3. Allelic and genotypic frequencies of Id3 gene g.-156A>G polymorphism in pSS patients and controls and according to the presence of autoantibodies g.-156A>G pSS (n ¼ 212) Allele frequenciesa A 220 (52) G 204 (48) Genotype frequencies AA 55 (26) AG 110 (52) GG 47 (22) pSS without auto-Ab (n ¼ 77) pSS with anti-SSA only (n ¼ 63) pSS with anti-SSA and anti-SSB (n ¼ 72) Controls (n ¼ 154) Odds ratio (95% CI) pSS vs controls P-value 70 (45) 84 (55) 64 (51) 62 (49) 86 (60) 58 (40) 164 (53) 144 (47) 0.94 (0.71, 1.27) 1.06 (0.79, 1.42) 0.71 0.71 14 (18) 42 (55) 21 (27) 18 (29) 28 (44) 17 (27) 23 (32) 40 (56) 9 (12) 43 (28) 78 (51) 33 (21) 0.90 (0.57, 1.44) AA vs AG or GG 0.67 1.04 (0.63, 1.73) GG vs AA or AG 0.86 a The allelic frequencies are calculated on 424 chromosomes for patients and 308 chromosomes for controls. Results are expressed as number of patients (%); pSS, primary Sjögren’s syndrome; auto-Ab, auto-antibody; NA, not applicable; OR, odds ratio. human pSS [20] probably through collaboration between T and B cells [21]. All these results prompted us to investigate the presence of impaired expression of Id3 in human pSS. Since adoptive transfer of T cells is responsible for the development of the disease and Id3/ mice with T cell deficiency show no infiltrates, we quantified Id3 expression in blood T cells in pSS patients and healthy controls but found no difference in mRNA expression between the two groups. However, we cannot eliminate that Id3 expression is disturbed only in a subgroup of T cells such as tissueinfiltrating T cells, autoreactive T cells or regulatory T cells. In pSS, the target cells SGECs are primarily affected and could drive the immune response in exocrine tissue [1, 22]. Id3 deficiency could be involved in this functional impairment, thus facilitating the autoantigen presentation [5]. However, we found no difference between patients and controls in Id3 expression in SGECs. Nevertheless, the level of expression of Id3 in SGECs could be modified by the culture conditions and time, and we could not eliminate a dysregulation of Id3 in vivo. Thus, we performed Id3 mRNA quantification using cDNA from total labial salivary glands in 10 pSS patients and 10 controls. Interestingly, we have found a significant higher expression of Id3 in patients compared with controls. But, it could be only related to the greater number of inflammatory cells present in biopsies from patients who could express more Id3. Finally, our study still has some limitations. First, quantification of Id3 was performed on mRNA and the possibility of a defect of the protein in pSS patients remains possible but not assessed here. Lastly, we cannot exclude an Id3 defect during organogenesis, which could disappear during the life. Whatever it is, Id3 expression does not seem to be quantitatively decreased in human pSS. However, although the Id3 mRNA level was not impaired in peripheral T cells, SGECs and exocrine glands, defective function of Id3 could relate to Id3 polymorphisms. Since Id3 gene polymorphisms have not been extensively studied in humans, we first carried out Id3 gene sequencing in 12 subjects and identified 2 SNPs with potential functional relevance. Interestingly, no significant association was found between these two SNPs and pSS. Moreover, since most of the genetic predisposition to pSS is related to the pattern of autoantibody secretion [23] and since the Id3 knockout mouse has anti-Ro/SSA and anti-La/SSB antibodies, we studied the association between Id3 polymorphisms and autoantibody secretion but found no significant association with pattern of autoantibody secretion. In conclusion, although the Id3/ mouse shows clinical and biological symptoms very close to those observed in human pSS, Id3 is not down-regulated in blood T cells and SGECs of patients with pSS, the target cells of the disease. Moreover, the two relevant polymorphisms of Id3 are not involved in genetic predisposition to human pSS in a Caucasian population. Thus, Id3 seems to be not involved in the pathogenesis of human pSS. These results illustrate the difference between disease in animal models and in humans. Downloaded from http://rheumatology.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014 decreased in blood T cells, cultured SGECs and in minor salivary glands in patients with pSS as compared with healthy controls. Moreover, Id3 is not associated with a genetic predisposition to the disease or to a specific pattern of autoantibody secretion. Human pSS is considered as a multigenic and multifactorial autoimmune disease of unknown origin. Mouse models are of great value for studying the pathogenesis of SS, especially because they allow for investigating the initiation phase of the autoimmune process, which is not possible in humans. Among such models, NOD, MRL/lpr, NFS/sld and B-cell activating factor transgenic mice have been extensively studied as models of SS [4, 14]. However, the models may differ from human pSS and imperfectly reflect the manifestations observed in humans. Indeed, these mice are not models of pSS, because they also show characteristic features of other autoimmune diseases such as diabetes mellitus, RA and SLE. Moreover, secretory function is not always altered, as in the MRL/lpr mouse, and the autoantibody profile can differ from human disease, as in the NOD mouse, in which no anti-La/SSB antibodies are detected [4]. Interestingly, Li et al. [9] reported that the unique deletion of one gene, Id3, in mouse resulted in symptoms very similar to those observed in human pSS. Id3 is a member of the inhibitor of differentiation family of transcription factors, up-regulated in a broad range of cell types to regulate cell proliferation and differentiation [15]. The primary function of the Id3 protein is to inhibit bHLH transcription factors, thus preventing the DNA binding of bHLH and activating the transcription of target genes [16, 17]. The interaction between Id3 and bHLH proteins could be a key regulatory event leading to cellular proliferation and inhibition of differentiation in somatic cells. In general, the expression of Id genes is high in proliferating cells and low in differentiating and quiescent cells. The authors first reporting on the Id3-deficient mouse described impaired T-cell-dependent and -independent immune response and disturbed cell proliferation after B-cell antigen receptor (BCR) stimulation, thus revealing a specific role for Id3 in mediating signals from BCR to cell cycle progression during the humoral immune response [18, 19]. However, this mouse, at 10 weeks of age, exhibited no particular abnormalities in appearance, general behaviour, body and organ size or mortality rate. The same group reported that at 6–8 months of age, mice showed symptoms mimicking human pSS (sialadenitis, keratitis, sicca syndrome, salivary gland infiltrates and anti-Ro/SSA and anti-La/SSB antibodies) [9]. Notably, symptoms occurred when the mice reached an age comparable with middle age in humans, which is the usual time of development of human pSS. Id3/ mice show no significant elevated urine protein level, no hyperglycaemia and the lymphocyte infiltration is mainly observed in exocrine glands, with occasional immune cells in lung or kidney. These data are consistent with this mouse model being exclusively a model of SS not associated with another autoimmune disease. Moreover, Id3/ mice respond to treatment with anti-CD20 monoclonal antibody, which also suggests a role of B cells like in Id3 and primary Sjögren’s syndrome Rheumatology key messages Although Id3/ mouse represents the best animal model for human pSS, Id3 mRNA is not quantitatively decreased in the human pSS in blood T cells and SGECs. Genetic polymorphisms of Id3 do not predispose to pSS in Caucasian population. Id3 seems to be not involved in human pSS pathogenesis, illustrating the difference between autoimmune disease in animal models and in humans. Acknowledgements We thank Xavier Puéchal, Le Mans, France and Eric Hachulla, Lille, France, who helped collect DNA from patients. Disclosure statement: The authors have declared no conflicts of interest. References 1 Mitsias DI, Kapsogeorgou EK, Moutsopoulos HM. The role of epithelial cells in the initiation and perpetuation of autoimmune lesions: lessons from Sjogren’s syndrome (autoimmune epithelitis). Lupus 2006;15:255–61. 2 Moutsopoulos HM. Sjogren’s syndrome: autoimmune epithelitis. Clin Immunol Immunopathol 1994;72:162–5. 3 Moutsopoulos HM, Kordossis T. Sjogren’s syndrome revisited: autoimmune epithelitis. Br J Rheumatol 1996;35:204–6. 4 van Blokland SC, Versnel MA. Pathogenesis of Sjogren’s syndrome: characteristics of different mouse models for autoimmune exocrinopathy. Clin Immunol 2002;103:111–24. 5 Versnel MA. Id3 knockout mice as a new model for Sjogren’s syndrome: only a T cell defect or more? Immunity 2004;21:457–8. 6 Christy BA, Sanders LK, Lau LF, Copeland NG, Jenkins NA, Nathans D. An Id-related helix-loop-helix protein encoded by a growth factor-inducible gene. Proc Natl Acad Sci USA 1991;88:1815–9. 7 Asirvatham AJ, Schmidt MA, Chaudhary J. Non-redundant inhibitor of differentiation (Id) gene expression and function in human prostate epithelial cells. Prostate 2006;66:921–35. 8 Everly DN Jr, Mainou BA, Raab-Traub N. Induction of Id1 and Id3 by latent membrane protein 1 of Epstein-Barr virus and regulation of p27/Kip and cyclin-dependent kinase 2 in rodent fibroblast transformation. J Virol 2004;78:13470–8. 9 Li H, Dai M, Zhuang Y. A T cell intrinsic role of Id3 in a mouse model for primary Sjogren’s syndrome. Immunity 2004;21:551–60. 10 Vitali C, Bombardieri S, Jonsson R et al. Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the AmericanEuropean Consensus Group. Ann Rheum Dis 2002;61:554–8. 11 Gottenberg JE, Cagnard N, Lucchesi C et al. Activation of IFN pathways and plasmacytoid dendritic cell recruitment in target organs of primary Sjogren’s syndrome. Proc Natl Acad Sci USA 2006;103:2770–5. 12 Ittah M, Miceli-Richard C, Eric Gottenberg J et al. B cell-activating factor of the tumor necrosis factor family (BAFF) is expressed under stimulation by interferon in salivary gland epithelial cells in primary Sjogren’s syndrome. Arthritis Res Ther 2006;8:R51. 13 Grabe N. AliBaba2: context specific identification of transcription factor binding sites. In Silico Biol 2002;2:S1–15. 14 Groom J, Kalled SL, Cutler AH et al. Association of BAFF/BLyS overexpression and altered B cell differentiation with Sjogren’s syndrome. J Clin Invest 2002;109:59–68. 15 Jan YN, Jan LY. HLH proteins, fly neurogenesis, and vertebrate myogenesis. Cell 1993;75:827–30. 16 Jen Y, Manova K, Benezra R. Expression patterns of Id1, Id2, and Id3 are highly related but distinct from that of Id4 during mouse embryogenesis. Dev Dyn 1996;207:235–52. 17 Sun XH, Copeland NG, Jenkins NA, Baltimore D. Id proteins Id1 and Id2 selectively inhibit DNA binding by one class of helix-loop-helix proteins. Mol Cell Biol 1991;11:5603–11. 18 Pan L, Sato S, Frederick JP, Sun XH, Zhuang Y. Impaired immune responses and B-cell proliferation in mice lacking the Id3 gene. Mol Cell Biol 1999;19:5969–80. 19 Rivera RR, Johns CP, Quan J, Johnson RS, Murre C. Thymocyte selection is regulated by the helix-loop-helix inhibitor protein, Id3. Immunity 2000;12:17–26. 20 Seror R, Sordet C, Guillevin L et al. Tolerance and efficacy of rituximab and changes in serum B cell biomarkers in patients with systemic complications of primary Sjogren’s syndrome. Ann Rheum Dis 2007;66:351–57. 21 Hayakawa I, Tedder TF, Zhuang Y. B-lymphocyte depletion ameliorates Sjogren’s syndrome in Id3 knockout mice. Immunology 2007;122:73–9. 22 Manoussakis MN, Moutsopoulos HM. Sjogren’s syndrome: autoimmune epithelitis. Baillieres Best Pract Res Clin Rheumatol 2000;14:73–95. 23 Gottenberg JE, Busson M, Loiseau P et al. Association of transforming growth factor beta1 and tumor necrosis factor alpha polymorphisms with anti-SSB/La antibody secretion in patients with primary Sjogren’s syndrome. Arthritis Rheum 2004;50:570–80. Downloaded from http://rheumatology.oxfordjournals.org/ at Pennsylvania State University on February 27, 2014 Funding: The authors received a grant from Fondation pour la Recherche Médicale, Agence Nationale pour la Recherche to carry out the study. 441