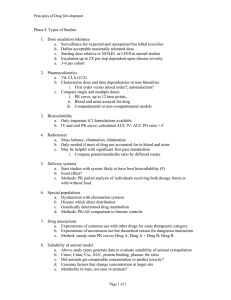
Introduction to Pharmacokinetics
advertisement

Introduction to Pharmacokinetics David Karhu AMWA 75th Annual Meeting, San Antonio, October 3, 2015 Introduction to Pharmacokinetics Objectives Define pharmacokinetics (PK) Principles of ADME Noncompartmental PK Compartmental PK 2 Introduction to Pharmacokinetics “I learned very early the difference between knowing the name of something and knowing something.” - Richard Feynman 3 Introduction to Pharmacokinetics What is pharmacokinetics? “What the body does to the drug” Assesses rate of movement of drugs in body; ie, study of mathematical relationships between administered dose of a drug and its resulting concentrations ADME: Absorption, Distribution, Metabolism, Excretion 4 Introduction to Pharmacokinetics Fundamental tenet: there is a relationship between blood concentrations and pharmacological effect Ref: Mehrotra, et al. Int J Impot Res 2007;19(3):253-64 5 ADME Absorption Process by which unchanged drug enters systemic circulation following administration by an extravascular route (eg, PO, SC, transdermal, inhalation) Bioavailable fraction (f) Bioavailability (F) is 100% following IV dosing http://usmle1-general-pharmacology-2.html 6 ADME Factors affecting absorption Physicochemical properties of drug (solubility, permeability) http://usmle1-general-pharmacology-2.html 7 ADME Factors affecting absorption Extent of first-pass metabolism http://usmle1-general-pharmacology-2.html 8 ADME Factors affecting absorption Splanchnic blood flow http://usmle1-general-pharmacology-2.html 9 ADME Factors affecting absorption Gut motility http://usmle1-general-pharmacology-2.html 10 ADME Factors affecting absorption Transport back to intestinal lumen (eg, P-glycoprotein efflux) http://usmle1-general-pharmacology-2.html 11 ADME Factors affecting absorption Fed versus fasting state (food slows rate of stomach emptying; rate of splanchnic blood flow increases) http://usmle1-general-pharmacology-2.html 12 ADME Distribution Reversible process by which drug moves between intravascular space (blood) and extravascular space (other tissues) Elimination Irreversible loss of drug from site of measurement (eg, blood) Metabolism Excretion 13 ADME Metabolism Biochemical modification of drugs, usually through specialized enzymatic systems (eg, cytochrome P450 oxidases) Most drugs are weak acids or weak bases (partially ionized) Lipophilic in un-ionized form; can readily diffuse across membranes Transformed (eg, hydroxylation, conjugation) to more polar, water-soluble products to facilitate renal excretion Some metabolites are active (have pharmacological effects); some are inactive Metabolism is primarily hepatic, although most tissues have some metabolic activity 14 ADME Excretion Removal of unchanged drug and metabolites from the body Major routes renal (urine) to a lesser extent, biliary (feces) Minor routes Sweat, tears, saliva, milk 15 ADME Enterohepatic recycling http://quizlet.com/10071850/pharm1-block3-general-flash-cards/ 16 17 Noncompartmental PK Common parameters Calculation Interpretation 18 Therapeutic range In general, dosage regimen (ie, dose and dosing interval) is adjusted so that both Cmax,ss and Cmin,ss are within therapeutic range Drug Concentration vs Time Plot 240 Drug Concentration (ng/mL) Toxicity 200 Cmax,ss 160 Therapeutic range 120 Cmin,ss 80 Dose 40 0 Dose 0 Dose Dose Dose Lack of efficacy Dose 10 20 30 40 50 Time (h) 19 60 70 80 Area Under the Concentration vs Time Curve (AUC) Measure of extent of absorption (total systemic exposure) AUC0-n, where n is any sampling time AUC0-t, where t is time of last sample collection AUC0-∞, extrapolation to infinity AUC0-τ, where τ is a dosing interval at steady state 20 AUC0-t The trapezoidal rule is used to calculate AUC0-t: AUC0t = C1 n C2 2 ( t 2 - t1) + C2 C3 2 ( t3 - t 2) …Cn1 C n ( t n - t n -1) 2 Drug Concentration vs Time Plot C5 30 Drug Concentration (ng/mL) (C5 + C6)/2 = average C = height 25 C6 20 15 10 5 0 0 t6 – t5 = width 2 4 6 Time (h) 8 21 10 12 AUC0-∞ Semilog plot - concentrations in terminal phase decline linearly Drug Concentration vs Time Plot 100 Drug Concentration (ng/mL) 10 1 0 2 4 6 Time (h) 8 22 10 12 AUC0-∞ Slope of regression line = terminal elimination rate constant, or λz To calculate AUC0-∞, extrapolate area from time = t to infinity and add to AUC0-t Ct/λz, where Ct is last observed nonzero conc (FDA) Cz/λz where Cz is estimated conc from the regression line at time = t (Health Canada) Drug Concentration vs Time Plot Drug Concentration (ng/mL) 100 slope = λz 10 Extrapolated area 1 0 2 4 6 Time (h) 8 23 10 12 AUC0-τ Dose Dose Dose Dose Dose Dose Note: If CL does not change with multiple dosing1, AUC0-∞ (single dose) = AUC0-τ (at steady state) 1 Autoinduction or autoinhibition may cause CL to change 24 Bioavailability (F) Absolute bioavailability Relative amount of extravascularly-administered drug that reaches systemic circulation unchanged For IV dose, F = 100% Absolute bioavailability following PO dose: F Eg: AUC AUC PO IV D D IV PO AUCPO = 75 ng·h/mL; AUCIV = 100 ng·h/mL; DIV = DPO = 1 mg = 1 000 000 ng F 75 ng h/mL 1 000 000 ng 100 75% 100 ng h/mL 1 000 000 ng 25 Bioavailability (F) Relative bioavailability Determined against reference standard (eg, oral solution, innovator product, old formulation) Relative bioavailability: Frel AUC AUC Test Reference DReference D Test 26 Maximum observed concentration (Cmax) Read directly from concentration data Estimate of maximum systemic exposure Following IV dosing, Cmax typically occurs at end of injection or infusion Following extravascular dosing, Cmax occurs when rate of absorption = rate of elimination Am J Physiol Endocrinol Metab 2007;292:E1829–E1836 http://www.xenogesis.com/services-3/in-vivo/pharmacokinetics-pk/ 27 Time of maximum observed concentration (tmax) Read directly from data Following extravascular dosing, maximum drug effects and adverse events are likely to occur at or around tmax 28 Terminal elimination rate constant (λz) Common abbreviations: k, kel, or λz Fraction of drug eliminated per unit time Depends on 2 parameters volume of fluid cleared per unit time (ie, clearance) volume to be cleared (ie, volume of distribution) z V d Also related to half-life z CL ln 2 t 1/ 2 λz can also be determined from slope of regression line at terminal phase of log concentration vs time curve 29 Terminal elimination half-life (t1/2) Time it takes for concentration in terminal elimination phase (linear portion of a semi-log plot) to decrease by half t1/ 2 ln 2 z Used to estimate dosing interval, time to steady state, or time needed for drug concentration to return to safe level following overdose A drug is considered essentially eliminated after 5 half-lives 1 half-life: 50% 2 half-lives: 75% 3 half-lives: 88% 4 half-lives: 94% 5 half-lives: 97% 30 Clearance (CL) Most important PK parameter Volume of fluid from which drug is completely removed in a given time period Units: L/h or mL/min Measure of the ability of the body to eliminate a drug dX Eliminatio n rate dt CL Concentration in blood C Integrating from 0∞, CL 0 dX dt dt Cdt 0 where 0 and dX dt dt Cdt = total amount eliminated (ie, Doseiv) = AUC0-∞ 0 Therefore CL D AUC iv 0 31 Clearance (CL) For extravascular dose, CL CL / f f D AUC 0 D AUC 0 CL/f is the apparent clearance CL is used to calculate dosing rate for long-term drug administration: Dosing rate = CL Css where Css is the desired steady-state concentration 32 Clearance Calculated for organs responsible for clearing drug: kidney (renal clearance, CLR), liver (hepatic clearance, CLH), or other organs Renal clearance, CLR A AUC e ( 0 n ) 0 n where Ae(0-n) is amount of drug excreted unchanged over a specified time interval Ae(0-n) = Cu(0-n) Vu(0-n) where Cu(0-n) and Vu(0-n) are concentration and volume of urine, respectively, over collection interval (0-n) 33 Clearance Reasons CL can decrease Renal or hepatic impairment Enzyme inhibition Age Reasons CL can increase Enzyme induction 34 Volume of distribution (Vd) Proportionality constant linking amount of drug in body to measured concentration Vd does not represent a physiologic volume 35 Volume of distribution (Vd) 36 Volume of distribution (Vd) Add known amount of soluble substance (eg, 1000 mg), mix well, determine concentration (eg, 10 mg/L) Then, Volume 37 Amt 1000 mg 100 L Conc 10 mg / L Volume of distribution (Vd) Now, imagine that the added substance binds to rocks on bottom of pond so that measured concentration is 1 mg/L Then, Volume 1000 mg 1000 L 1 mg / L Note: Volume has not changed, but apparent volume has 38 Volume of distribution (Vd) Immediately after IV dose, V c Dose C 0 where Vc is the volume in central (sampling) compartment, and C0 is maximal concentration C0 corresponds to initial plasma concentration resulting from total drug mixing in blood before any distribution or elimination Vc can be viewed as the apparent volume from which drug elimination occurs, because kidney and liver are wellperfused tissues and belong to central compartment 39 Volume of distribution (Vd) Immediately after an IV bolus, Vc = DoseIV/C0 Vd (L) Vc VC Vp Time postdose (h) Vc is volume of central compartment Vp is volume of peripheral compartment 40 Volume of distribution (Vd) Soon thereafter, drug begins to be distributed and eliminated Vd (L) Vc Vp Vc Time postdose (h) Vc is volume of central compartment Vp is volume of peripheral compartment 41 Volume of distribution (Vd) Vd increases to an asymptotic value (Varea) when equilibrium of distribution is attained Once equilibrium attained, net exchange between plasma (central compartment) and tissues (peripheral compartments) is null Varea Vc Vd (L) Vc Time postdose (h) Vc is volume of central compartment Vp is volume of peripheral compartment 42 Vp Volume of distribution (Vd) After this, any decrease of plasma concentration is due to irreversible drug elimination V area Amt of drug in body during terminal phase Plasma concentration during terminal phase CL λ z Dose AUC 0 λz For extravascular dose, the amount of drug accessing systemic circulation is unknown; thus V area f Dose AUC0 λz V area f Dose AUC V/f is the apparent volume of distribution Ref: J Vet Pharmacol Therap 2004;27:441-53 43 0 λz Volume of distribution (Vd) Some drugs distribute primarily in plasma Tightly bound to plasma proteins (eg, warfarin) Highly hydrophilic (eg, gentamicin) These drugs have low Vd (eg, ≤ 0.25 L/kg) Other drugs bind extensively to tissues outside of blood, eg adipose tissue, muscle eg, chloroquine These drugs have a high Vd (eg, > 200 L/kg) 44 Compartmental PK Not always possible to use noncompartmental PK Drug not eliminated (eg, IV iron) Extensive blood sampling not feasible (eg, infants, cancer patients) Use compartmental PK to construct model based on differential equations to explain change in drug concentrations over time Use simplest model that explains data 45 Compartmental PK One-compartment model Monoexponential decay Toxicol Appl Pharmacol. 2013;271(2):216-228 46 Compartmental PK Two-compartment model Biexponential decay Toxicol Appl Pharmacol. 2013;271(2):216-228 47 Compartmental PK 48 Noncompartmental vs Compartmental Noncompartmental PK Based on algebraic equations Sensitive to sampling frequency Simple Reproducible Does not require specialized software Compartmental PK Based on linear or nonlinear differential equations Useful when sampling is sparse Fitting compartmental models can be complex and lengthy process Requires specialized software 49 Questions? 50