MLAB 1415- HEMATOLOGY Myelodysplastic Syndromes KERI BROPHY-MARTINEZ
advertisement

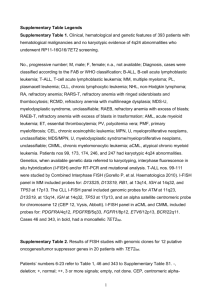
MLAB 1415- HEMATOLOGY KERI BROPHY-MARTINEZ Myelodysplastic Syndromes MYELODYSPLASTIC SYNDROMES • Acquired clonal hematologic disorders characterized by progressive cytopenias in the peripheral blood, reflecting defects in erythroid, myeloid and/or megakaryocytic maturation. • Impaired hematopoiesis. • Disrupted apoptosis • Bone marrow is hyperplastic • The origin is currently unknown Terms used to describe MDS • Preleukemic leukemia or syndrome • Chronic refractory anemia with sideroblasts • Smoldering leukemia Risk factors • Age • Occur primaroy over the age of 50 • Genetic predisposition • Chromosomes 5,7 and 8 • Down’s, Fanconi’s • Environmental exposures • benzene • Prior therapy • Radiation • Chemotherapy Clinical findings • Symptoms are related to progressive bone marrow failure • Infections • Bleeding • Anemia- fatigue/weakness • Death usually occurs from infection and/or bleeding or from leukemia if transformation occurs. Key Lab Features of MDS • Dysmyelopoiesis • Dyserthropoiesis • Dysmegakaryopoiesis Dysmyelopoiesis- PB Dyserthropoiesis- PB Dimorphic erythrocyte population Oval macrocytes Dysmegakaryopoiesis- PB Abnormal platelet granulation Micromegakaryocyte FAB classification • Five MDS subtypes: • Refractory anemia (RA) • Refractory anemia with ringed sideroblasts (RARS) • Refractory anemia with excess blasts (RAEB) • Refractory anemia with excess blasts in transformation (RAEB-t) • Chronic myelomonocytic leukemia (CMML) WHO classification- 2008 • Refractory anemia (RA) with unilineage dysplasia • Refractory anemia with ringed sideroblasts (RARS) • Refractory cytopenia with multilineage dysplasia (RCMD) • RA with excess blasts (RAEB) • MDS with isolated deletion of 5q • MDS, unclassifiable • Childhood MDS MDS/MPD Diseases • Clonal hematopoietic neoplasms that at initial presentation have some clinical, laboratory or morphological findings of both a MDS/MPD • Abnormalities in the regulation of myeloid proliferation, maturation and cell survival • Diseases • CMML associated with persistent monocytosis • Atypical Chronic Myeloid Leukemia • Juvenile Myelomonocytic Leukemia • MDS/MPD, unclassifiable Chronic Myelomonocytic Leukemia (CMML) • Monocytosis • Dysplasia in one or more myeloid lines • Bone marrow hypercellular • Splenomegaly may be present Therapy • Currently, there is no really good treatment for MDS, therefore most therapy is supportive, such as transfusion of blood components and antibiotics. • The only effective treatment is bone marrow transplant, but most patients are too old to survive the rigors of this treatment. • Immunosuppressive therapy decreases the chance of leukemic transformation. References • McKenzie, Shirlyn B., and J. Lynne. Williams. "Chapter 21." Introduction. Clinical Laboratory Hematology. Boston: Pearson, 2010. Print • Rodak, Bernadette F., Fritsma, George, and Elaine Keohane. "Chapter 35." Myelodysplastic Syndrome. Hematology Clinical Principles and Applications. St. Louis: Elsevier, 2012. Print