Hourly Rounding Skills Labs and Their Impact on HCAHPS Scores
advertisement
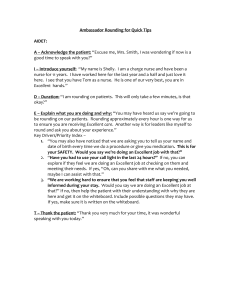
Hourly Rounding Skills Labs and Their Impact on HCAHPS Scores Point of Contact: Janine Diddens, (210) 297-4601, jmdidden@baptisthealthsystem.com Group Involved with the Project. The North Central Baptist Patient Experience Officer, Nursing Directors, and Inpatient Nursing Units Submitted by CPT Nicole M. Lawrence 16 May 2014 Executive Summary: Today, value based purchasing requires that healthcare workers execute high quality care. Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) measures the patients’ perspective of their hospital stay. Organizations such as the Studer Group have completed extensive research on what a patient is looking for during their hospital stay. Quality hourly rounding has been proven to directly impact patient experience scores. At North Central Baptist Hospital (NCBH), Janine Diddens, the Patient Experience Officer, implemented individual hourly rounding skills labs, introduced by the Studer Group, and saw increased patient experience scores as a direct result. 1|Page Objective of the Best Practice: The goal is to sustain North Central Baptist Hospital (NCBH) Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores above the 70th percentile through quality individual hourly rounding skills labs. Background: NCBH HCAHPS scores were unpredictable and rarely in the desired range above the 70th percentile. Monthly scores in the year before implementation of hourly rounding skills labs fluctuated between 35.2 percentile and 79.4 percentile (only once above 70th) with no apparent trend or explanation for the fluctuation. The hospital CEO decided to employ a Patient Experience Officer, Janine Diddens, to work with the nursing directors using evidence based practices to coach the NCBH team and ultimately improve HCAHPS scores. Before implementing the skills labs, the hospital leadership cycled through educating themselves and staff members about HCHAPS scoring, training nurses, setting expectations for hospital staff, and repeating those steps. Janine saw this as insanity, doing the same thing over and over and expecting a different result. In June 2013, she insisted it was time to take it to another level. Individual hourly rounding skills labs create a safe learning environment that allows staff to behaviorally rehearse and transform reliable knowledge into consistent action. This is the time for staff members to see their areas of strength and weakness and practice improving their approach to rounding. The skills lab is an opportunity for the leader of the unit to train their staff and validate their practice. Additionally, the leader’s engagement allows staff to receive meaningful and direct feedback. Literature Review: Why is improving HCAHPS scores important to NCBH? “The FY 2014 Hospital Value-Based Purchasing (Hospital VBP) program links a portion of IPPS [Inpatient Prospective Payment System] hospitals’ payment from CMS to performance on a set of quality measures, which include…the Patient Experience of Care Domain, 30% of TPS…The HCAHPS Survey is the basis of the Patient Experience of Care Domain” (HCAHPS Fact Sheet, 2013, p. 3). In other words, a portion of the hospital’s income depends on HCAHPS scores. First, NCBH must understand HCAHPS. “The intent of the HCAHPS initiative is to provide a standardized survey instrument and data collection methodology for measuring patients’ perspectives on hospital care” (www.hcahpsonline.org/home.aspx, 2014). Every hospital participating in the HCAHPS initiative is up against the same patient scrutiny. “The HCAHPS survey contains 21 perspectives on care and patient rating items that encompass nine key topics: communication with doctors, communication with nurses, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness of the hospital environment, quietness of the hospital environment, and transition of care” (www.hcahpsonline.org/home. aspx, 2014). Different hospitals may struggle in different areas on the survey. At NCBH, there is opportunity for improvement consistently in responsiveness and communication. Quality hourly rounding has been proven to improve nurse and patient satisfaction. The Agency for Healthcare Research and Quality (AHRQ) published a study in November 2011 in which Memorial Health System in Springfield, IL concluded “the rounding program has helped to reduce patient falls, pressure ulcers, and call light use, and contributed to significant improvements in patient satisfaction with nursing” (http://innovations.ahrq.gov/content.aspx?id=3204, 2011). AHRQ is not alone in encouraging hourly rounding. “Studer Group® works with hundreds of healthcare organizations in the United States, Canada, Australia, New Zealand and beyond, teaching them how to achieve, sustain, and accelerate exceptional clinical, operational, and financial outcomes” (https://www.studergroup.com/who-we-are/about-studer-group/). NCBH frequently turns to the Studer Group for guidance on exceptional care. The Studer Group website contains instructional 2|Page videos of hourly rounding skills labs. NCBH skills labs are based off those recommended by Studer Group. Implementation Methods: In congruence with the Studer Group teachings and recommendations, Janine began hourly rounding skills labs. She started with a busy orthopedic inpatient unit, 3E. She worked with the nursing director of the unit to schedule 30 minute appointments with each RN, LPN, and CNA. First, Janine recorded herself conducting an hourly round on a mock patient. She wanted to show staff what “right looks like”. At the nurse’s appointed time, she allowed the staff to view her video prior to their skills lab. Then, Janine used an unoccupied patient room with the nursing director as the patient and recorded on her iPad a mock hourly round performed by the nurse. When they were finished, Janine sat down with the nurse and watched the video. This allowed the nurse to see behaviors he/she may not have realized were happening. Janine filled out a rating sheet that notated behaviors the nurse did well and opportunities for improvement (see Appendix A). She used the remaining time to coach the nurse on scripting techniques and areas for improvement. She chose two goals for each nurse to focus and improve upon and gave the rating sheets to the director for her records. The director now has the responsibility to continue the coaching and mentoring along with direct observations of future hourly rounding to check for learning and further opportunities for improvement. The experience officer uses this time to teach the directors the difference between coaching their staff and cheerleading. A cheerleader is enthusiastic, cheerful, and positive. While a coach does encompass those traits, they are also knowledgeable, focused, and supportive through the learning and growing phases. Results: During the skills labs, Janine consistently discovered and addressed a few “Aha” moments. Many nurses have a habit of saying, “call me if you need anything” before they exit a patient room. Janine helped the nurses to understand that this practice will increase the patient’s use of their call light. Nurses cannot possibly meet the expectation of answering call lights in a timely manner if all of their patients are constantly calling for small requests such as blankets, ice, etc. A better practice is to say, “Here is your call light. It is for your safety. Please, use it if you need something urgently, if you are short of breath or experiencing unfamiliar pain, etc. I will be back in one hour to meet any of your other needs.” Following this statement, it is important that the nurse actually returns in one hour to perform the next hourly round. The rounding also needs to be of high quality to ensure that before the nurse leaves the room the patient has all of their needs met. Another repeated recommendation for many nurses was that they narrate their care. Nurses get in a rush and move about the room without the patient realizing what the nurse is thinking, observing, or doing. If the patient does not know what the nurse is doing, the nurse may not earn appropriate credit they deserve. Janine also stressed the importance of managing up. This is the practice of explaining to the patient that they are in good hands. Nurses can manage themselves up by telling the patient the amount of experience they have or how many patients they have cared for just like them. Nurses can also manage others up by telling the patient all of the desirable traits and experience of another nurse or a physician caring for them. It puts the patient at ease and creates a sense of confidence in their healthcare team. Hourly rounding skills labs on 3E began in July 2013. Janine performed approximately 40 individual skills labs over 4 weeks. NCBH 3E HCAHPS scores in the months leading up to the skills labs implementation were 68th percentile in April 2013, 64.2 percentile in May 2013, and 3|Page 45.4 percentile in June 2013, reflecting a downward trend. Following the skills labs, the scores for the unit reflected an upward trend from 58th percentile in July 2013, to 72nd percentile in August, and 80.8 percentile in September, the highest unit scores for at least the past year. When combining these scores with those from the rest of the units in the hospital, the total hospital scores were impacted positively from 49.6 percentile in May and 56.4 percentile in June to 61.6 percentile in July, 72.2 percentile in August, and 88.4 percentile in September. This was the only instance in the past 16 months of two consecutive months with hospital scores in the desired range above the 70th percentile. Conclusion: This best practice is outcomes-based, adaptable/replicable, sustainable, and innovative. Hourly rounding skills labs effectiveness are measured by communication and responsiveness scores within the HCAHPS scores. Increasing overall hospital HCAHPS scores through diligent hourly rounding skills labs and follow up allows for a return on investment with CMS performance payment. At a lower level, the skills labs increase nursing efficiency during hourly rounding. These skills labs are replicable in any inpatient unit. Hourly rounding is widely accepted as an essential practice to reduce call lights and increase patient satisfaction. Therefore, hourly rounding skills labs are applicable on any unit that is aware of hourly rounding. Following the skills labs with the patient experience officer, the director of the unit is responsible for sustainment and continued observations. The experience officer plans to return to each unit on a yearly basis to perform additional skills labs to any new employees in addition to those the director identifies as needing additional training. Hourly rounding skills labs are an innovative approach to involving the leader in a hands-on coaching opportunity. This practice builds upon the evidence based practice of hourly rounding to ensure quality efficient rounding. 4|Page References HCAHPS Fact Sheet. August 2013. Centers for Medicare & Medicaid Services (CMS), Baltimore, MD USA, www.hcahpsonline.org. http://innovations.ahrq.gov. Hourly Nurse Rounds Help to Reduce Falls, Pressure Ulcers, and Call Light Use, and Contribute to Rise in Patient Satisfaction. AHRQ Health Care Innovations Exchange. November 23, 2011. http://www.hcahpsonline.org. Centers for Medicare & Medicaid Services, Baltimore, MD. May 8, 2014. https://www.studergroup.com. Studer Group, Gulf Breeze, FL. May 8, 2014. 5|Page Appendix A 6|Page