FLUIDS AND ELECTROLYTES FOR SURGEONS Anil S. Paramesh MD, FACS
advertisement
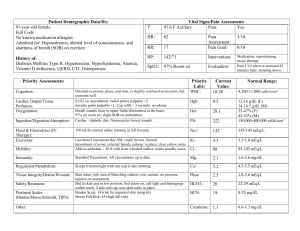
FLUIDS AND ELECTROLYTES FOR SURGEONS Anil S. Paramesh MD, FACS Associate Professor of Surgery, Urology and Pediatrics Why ? Essential for surgeons (and all physicians) Knowledge can diagnose, treat and prevent many of the problems in surgical patients Most abnormalities are relatively simple, and many iatrogenic Fluid Compartments Total Body Water Relatively constant Depends upon fat content and varies with age Men 60% (neonate 80%, 70 year old 45%) Women 50% TOTAL BODY WATER 60% BODY WEIGHT ICF 2/3 (40% BW) H2O ECF 1/3 (20% BW) Predominant solute Predominant solute K+ Na+ 75% interstitial 25% intravascular (5% of BW) It’s All About Balance Gains and Losses Most individuals ingest approx 2 – 2.5 L/day Losses Sensible and Insensible Typical adult, typical day Skin Lungs Kidneys Feces 600 ml 400 ml 1500 ml 100 ml Balance can be dramatically impacted by illness and medical care How much fluid can a patient lose if a patient could lose fluid? Sensible losses Blood (most pts can tolerate 500 cc BL) Sweat (up to 4 L /day) Tears – (diarrhea) Insensible losses Skin 250 cc/day/degree fever Trach/vent – upto 1500 cc/day Peritoneum - > 1/day Third spacing I LOVE SALT WATER! Electrolytes (mEq/L) Na K Ca Mg Cl HCO3 Protein Plasma 140 4 5 2 103 24 16 Intracellular 12 150 0.0000001 7 3 10 40 Gibbs-Donnan equation – product of diffusible an/cations same on both sides of SP membrane Fluid Movement Is a continuous process Diffusion Solutes move from high to low concentration Osmosis Fluid moves from low to high solute concentration. Active Transport Solutes kept in high concentration compartment Requires ATP Movement of Water Osmotic activity Normal around 300 mOsm/L Osmolality determined by concentration of solutes Plasma (mOsm/L) 2 X Na + Glc + BUN 18 2.8 Fluid Status Blood pressure Check for orthostatic changes Physical exam Invasive monitoring Arterial line CVP PA catheter Foley Volume Deficit Most common surgical disorder Signs and symptoms CNS: sleepiness, apathy, reflexes, coma GI: anorexia, N/V, ileus CV: orthostatic hypotension, tachycardia with peripheral pulses Skin: turgor Metabolic: temperature Hypovolemia Acute Volume Depletion Determine etiology Hemorrhage, NG, fistulas, Aggressive diuretic therapy Third space shifting, burns, crush injuries Ascites What kind of fluid are we losing? Sweat – hypotonic (low sodium) Insensible loss is pure water GI loss is usually isotonic Stomach – acid, high CL Pancreas/bile – high HCO3 Saliva – high K IV fluids a la carte NaCl Normal saline (0.9%) has 154 mEq/L Na, 154 mEq Cl ½ Normal has 77 mEq Na/Cl Lactated Ringers Has 130 Na, 109 Cl (also has some K, Ca, lactate) D5Water Good replacement for insensible losses Case 1 6 month old boy, born full-term Developed worsening vomiting during the past week Today he is listless, irritable, not tolerating oral intake Pulse 145, BP 70/50 Diaper is dry, anterior fontanel depressed Case 1 Labs 134 92 12 2.8 40 0.8 12.3 15 45 200 Case 1 F & E Problem List Hypovolemia Hypochloremia Hypokalemia Alkalosis 134 92 12 2.8 40 0.8 Treatment – Patient weight is 12 kg Fluid choice? Replace volume Replace K/Cl How to order “Bolus” Think about rate over time Adequate access important What would maintenance fluid choice and rate be? 4-2-1 rule Acid – Base Balance Acidosis May result from decreased perfusion i.e. decreased intravascular volume K will move out of cells (K+ - H+ exchange) Alkalosis Complex physiologic response to more chronic volume depletion i.e. vomiting, NG suction, pyloric stenosis, diuretics K will move intracellular Paradoxical Aciduria Hypochloremic Hypovolemia Aldosterone activation Na H Na K Loop of Henle Case 1 When should we operate? Need to wait until adequately resuscitated Why Monitor by: Normalized vital signs Good urine output Normalized labs Case 2 64 year old, 50 kg, had colon resection 5 days ago “doing well” ….until…. Suddenly develops atrial fibrillation with rapid ventricular response P 120, irregular; BP 115/70; RR 20 Temp 38.7 Confused, anxious Case 2 Labs 128 100 12 3.0 22 0.8 16.3 8.9 28 180 Mg 1.1 Case 2 Diagnoses? New onset A fib, why? Hypervolemia Hyponatremia Hypokalemia Hypomagnesemia Anemia Case 2 Why does patient have hypervolemia? Increased Antidiuretic Hormone (ADH) Causes Surgical stress (physiologic) Cancers (pancreas, oat cell) CNS (trauma, stroke) Pulmonary (tumors, asthma, COPD) Medications Anticonvulsants, antineoplastics, antipsychotics, sedatives (morphine) Hyponatremia – how to classify Na loss True loss of Na Dilutional (water excess) Inadequate Na intake Classified by extracellular volume Hypovolemic (hyponatremia) Diuretics, renal, NG, burns Isovolemic (hyponatremia) Liver failure, heart failure, excessive hypotonic IVF Hypervolemic (hyponatremia) Glucocorticoid deficiency, hypothyroidism Patient was receiving maintenance fluids D5 0.45NS at 125 ml/hr Case 2 - How to treat A fib: ACLS protocol Correct electrolytes Replace Mg and K Decrease volume, fluid restriction Case 3 23 year old with jejunostomy Had colon and ileum resected due to injury Tolerates some oral nutrition, but has high output from jejunostomy (2.5 liters per day), therefore requires TPN P 118, BP 105/60 Case 3 Labs 154 114 28 3.2 16 2.4 10.3 9.7 28 380 Glucose 213 Mg 1.4 Current Problems Hypovolemia Increased plasma osmolarity 2 X 154 + (213/18) + (28/1.8) = 335 Hypernatremia Renal insufficiency Acidosis Case 3 - Hypovolemia Fistula output High volumes can rapidly lead to dehydration Electrolyte composition can be difficult to estimate Can send aliquot to laboratory May need to be replaced separately from maintenance (TPN) fluids Hyperglycemia Hypernatremia Relatively too little H2O Free water loss (burns, fever, fistulas) Diabetes insipidus (head trauma, surgery, infections, neoplasm) Dilute urine (Opposite of SIADH) Osmotic diuresis Nephrogenic DI Kidney cannot respond to ADH Too much Na, usually iatrogenic Hypernatremia Free water deficit: [0.6 X wt (kg)] X [Serum Na/140 - 1] Example: Na 154, 60 kg person (0.6 X 60) X [(154/140) - 1] 36 X [1.1 -1] 36 X 0.1 = 3.6 Liters Case 3 – How to Treat 154 114 28 3.2 16 2.4 Correct hyperglycemia Replace pre-existing volume deficits Reduce ostomy output if possible What to do with: Acidosis? Hypokalemia? Case 4 58 year old, had a recent kidney transplant Laboratory calls with critical value: Potassium 5.9 What to do? Case 4 Evaluate the patient Exam ECG Order repeat labs Hyperkalemia - Common Causes Hemolyzed specimen Underlying disease Renal failure Rhabdomyolysis Associated medications Too much K+, ACE inhibitors, beta-blockers, antibiotics, chemotherapy, NSAIDS, spironolactone Potassium and Ph Normally 98% intracellular Acidosis Extracellular H+ increases, H+ moves intracellular, forcing K+ extracellular Alkalosis Intracellular H+ decreases, K+ moves into cells (to keep intracellular fluid neutral) Hyperkalemia - Treatment Emergency (> 6 mEq/l) Monitor ECG, VS Calcium gluconate IV (arrhythmias) Insulin and glucose IV Kayexalate, Lasix + IVF, dialysis Mild to Moderate Mild: dietary restriction, assess medications Moderate: Kayexalate Severe: dialysis Pimping Questions on Rounds! Signs of hypo Ca? Chvostek, Trousseau, prolonged QT MCC of Hyper Ca? PTH/metastatic Ca Signs of hyper Mg Loss of DTR Signs of hypo Phos? Difficulty weaning off vent Compl of correcting Na too rapidly? Central Pontine Myelinolysis