Lecture 22: Virus offence meets host defense
advertisement
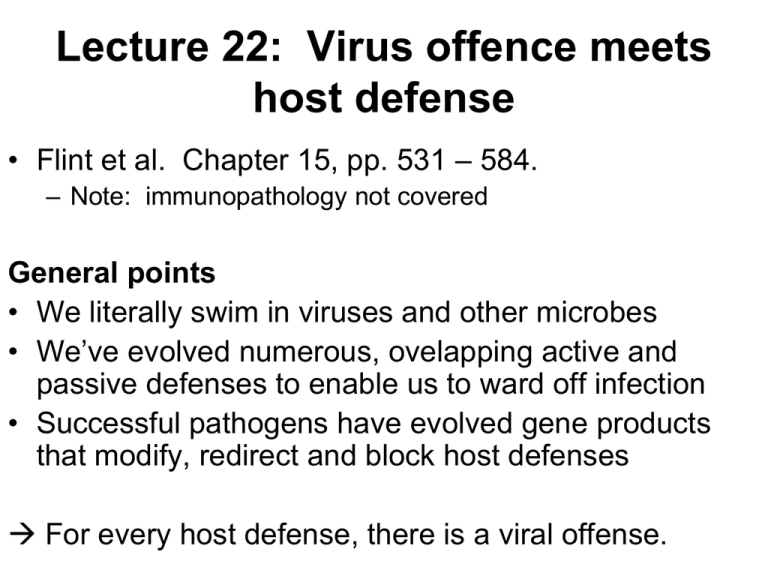
Lecture 22: Virus offence meets host defense • Flint et al. Chapter 15, pp. 531 – 584. – Note: immunopathology not covered General points • We literally swim in viruses and other microbes • We’ve evolved numerous, ovelapping active and passive defenses to enable us to ward off infection • Successful pathogens have evolved gene products that modify, redirect and block host defenses For every host defense, there is a viral offense. Primary physical and chemical defenses • Skin – Largest organ in body – >5 kg for adults – Strong barrier to infection – Inactivates viruses by desiccation, acids, skin cleansing mechanisms, inhibitors made by commensals • Other Epithelial surfaces: inactivates viruses via – – – – Secretions Mucus Tears Acid pH Intrinsic cellular defenses – Intro • Highly conserved, arose early in evolution • Non-specific responses to stresses, e.g. – Starvation – Irradiation – Infection Apoptosis • Programmed cell death • Keeps “wrong” cells from proliferating – “Sacrifice the one for the good of the many” • Promoted by Capsases: Cysteine proteases that cleave after ASPartate residues – Extrinsic pathway: triggered from outside – Intrinsic pathway: triggered from inside • Viruses can alter gene expression inside and outside of cell Fig. 15.1 • Viruses can activate either pathway Viral inhibition of apoptosis Many viral proteins have evolved to inhibit apoptosis by intervening at any one of multiple steps in the pathway. Fig. 15.2 Other intrinsic defenses • Autophagy – Cells cannibalize themselves! – Induced by starvation, viral infection • Nuclear domain 10 (NSD10) bodies – Prevent transcription of “foreign DNA” in nucleus – Defense against DNA viruses • RNA silencing (siRNAs, RNAi) – System recognizes and degrades dsRNAs – Defense against RNA viruses Immune defenses – overview • Highly coordinated • Depends on interplay of secreted proteins, receptor-mediated signaling, and cell-to-cell communication • Three critical steps: recognition, amplification, control. • Can be non-adaptive (innate) or adaptive. Innate immune responses • Cytokines – soluble proteins that act as signals • Sentinel cells – e.g. dendritic cells, patrol local areas • Complement – soluble proteins, poke holes in infected cells • Cytolytic “death star” cells – Natural Killer (NK) cells – Neutrophils, Basophils, Macrophages, other granulocytes. • Pattern recognition receptors – Detection of “non-self” • Toll-like receptors. • Expressed inside and outside of cells • Very ancient – Detection of “missing” or “altered self” • Used mainly by NK T-cells. • Also ancient: similar systems used by insects. Cytokines • Rapid response team: one of the first indicators of infection • Infected cells make cytokines in response to multiple cues – e.g. uncoating of viruses, exposure to foreign DNA/viral proteins, stress such as ER overloaded viral proteins or too much transcription activity. • Divided into three classes: • Proinflammatory – promote immune activation – e.g. IL-1, Tnf, IL-6, IL-12 • Anti-inflammatory – return system to basal activity – e.g. IL-10, IL-4, Tgf-b • Chemokines – Recruit immune cells early in immune response – e.g. IL-8 Cytokines – viral responses • (see Tables 15.6 and 15.7) • Cytokines interact with cells via cytokine receptors • Many viruses have evolved gene products to modulate the immune response • Virokines: Mimic host cytokines. • Viroreceptors: mimic host cytokine receptors. Serve as sinks for cytokines, prevent cytokine activities. Interferons – early warning See Table 15.8 • Produced by infected cells (and immature dendritic cells) • IFN-a: produced by most nucleated cells in response to viral infection, dsRNA • IFN-b: produced by most nucleated cells in response to viral infection, dsRNA • INF-g: Produced by T-cells, NK cells in response to antigens, mitogens, IL-2, 12 • Induce antiviral states – – – – – Apoptosis of infected cells Apoptosis of nearby cells – firewall Block cell proliferation Enhances NK cell activity Alters MHC expression…and many more effects • Very non-specific and toxic…Not the “magic bullet” – However, useful for treatment of many persistent viral infections, e.g. hepatitis B and C Antiviral IFN-induced proteins Pkr (dsRNA activated protein kinase) Activated by dsRNA. Phosphorylates eIF2-a, shutting down translation. Many viral proteins evolved to inactivate or misdirect Pkr. RNase L + 2’-5’ Oligo(A) synthetase Work together to degrade RNAs. Both antiviral and apoptotic Mx proteins In mice, specifically prevents “cap-snatching” by influenza In humans ,can also prevent replications of VSV, Measles, parainfluenza and others. Antiviral IFN-induced proteins P200 proteins Block cell proliferation Inhibit rRNA transcription and ribosome biosynthesis Nitric oxide synthase Directs synthesis of NO in NK cells Cytotoxic Inhibits poxvirus and herpesvirus replication PML Part of the ND10 bodies, prevents transcription of foreign DNA Ubiquitin-proteosome pathway components Proteins tagged with ubiquitin are targeted to the proteosome for degradation Viral gene products that counter IFN response • Viruses have evolved many gene products to counter IFN. Types of modulation include: • Inhibition of IFN synthesis • IFN receptor decoys • Inhibition of IFN signaling • Block functions of IFN-induced proteins • See Table 15.9 Non-specific cellular response • Dendritic cells and macrophages – Sentinel cells: patrol local area for bad guys – Phagocytotic – Present foreign antigen to T-cells • NK cells – Recognize and kill virus infected cells – Detect “altered” or “missing-self” molecules • Altered self: MHC I & II + non-self antigen • Missing self: Lack of MHC I or II, lack of activating receptors. Non-specific cellular response (Figs. 15.9, 15.10) NK cell Dendritic cell Complement • “Complemented by antibody” • 3 pathways: classical, alternative, mannanbinding • Poke holes in infected cells, targets cells for degradation, activates inflammation Complement Pattern Associated Molecular Patterns- PAMPs